Abstract
This study characterizes the personality disorder (PD) symptoms of patients who endorse a perplexing combination of low desire and high plans for suicide. Five PD (antisocial, narcissistic, borderline, dependent, avoidant) symptoms were examined at the junction of two suicide risk factors: a) suicidal desire/ideation and b) resolved plans/preparations. Participants (N=250) were recruited from U.S. Army Medical Center affiliated sites, including two outpatient clinics, an inpatient facility, and emergency room. Self-report measures of PD and suicide symptoms were administered. The interaction of desire and plans was entered into multiple regression equations predicting PD symptoms. Patients endorsing low desire and high plans for suicide reported significantly more antisocial and narcissistic, and fewer borderline, avoidant, and dependent PD symptoms. Our findings support the existence of patients who endorse suicide plans in the absence of strong suicidal desire, and suggest they display antisocial and narcissistic personality characteristics. Future directions and clinical implications are discussed.
Empirical findings suggest that suicidal symptoms may be represented by a multidimensional structure (Joiner, Walker, Rudd, & Jobes, 1999; Joiner et al., 2003). Specifically, suicidal symptoms can be adequately explained by a two-factor model consisting of a) suicidal desire and ideation (e.g., wish to die and not to live), and b) resolved plans and preparations (e.g., specificity of suicide plan; Beck, Brown, & Steer, 1997; Joiner, Rudd, & Rajab, 1997; Joiner et al., 2003). These findings have been useful both empirically and clinically as they suggest that suicide risk is dependent, in part, upon the individual’s levels on both factors (Joiner et al., 1999; see also Joiner, 2005). Therefore, those exhibiting low and high levels of both factors are considered at low and high risk for suicide, respectively, and high suicidal desire in the absence of particularly prominent symptoms of resolved plans and preparation does not indicate especially high risk for suicide (Joiner et al., 1999; 2003). What about the individuals with little desire for suicide and highly specific and detailed plans for suicide?
One would presume that these individuals are at high risk for suicide as notable symptoms of resolved plans and preparation are a more pernicious indicator of risk than the presence of suicidal desire and ideation. This is because resolved plans and preparations encompasses a host of particularly worrisome risk factors that contribute to the ability for suicide (e.g., specific plans, actual preparatory behaviors, access to means for suicide; confidence in their ability to enact lethal self-harm; Joiner et al., 1999; 2003; Van Orden et al., 2010). This has been supported by research showing that suicide plan specificity, and not desire, is a main predictor of suicide attempt history and future suicidal behavior (Joiner et al., 1997, 2003). The interpersonal theory of suicide, which has garnered empirical support, is based on a similar factor structure of suicidal desire and ability for suicide (see Van Orden et al., 2010 for details). These findings suggest that though both significant desire and plans are predictors of death by suicide, notable symptoms of resolved plans and preparation is a more pernicious indicator of risk. From this perspective, high levels of the resolved plans and preparation factor and the lack of significant symptoms of suicidal desire and ideation should confer elevated risk for suicide.
However, conceptually, this is somewhat counterintuitive. One would expect individuals not desiring to kill themselves to not act against their desires, particularly if the act is extremely difficult and fearsome, and therefore, not be at a great risk for suicide. If the individual does not desire suicide strongly, what is the purpose of reporting a specific and detailed plan for suicide?
One possibility is that these individuals utilize the reporting of detailed plans for suicide, in the absence of actual suicidal desire, as an instrument for personal gain. For example, an incarcerated individual may present with specific plans and preparations for a suicide attempt, not with the desire to die, but rather in an effort to obtain a desired outcome, such as a change in accommodation or prescribed medications. Alternatively, individuals may present with high plans and low desire for a suicide attempt due to a genuine sense of fearlessness about injury, including self-injury. For example, such individuals may adopt the perspective that if they wanted to die by suicide, they would be capable of such an act, apart from whether they desire death.
These patterns of behavior are consistent with the personality patterns of individuals with high levels of antisociality, borderline, and narcissistic PD, which are all significant risk factors for suicide (Blasco-Fontecilla et al., 2009; Ronningstam & Weinberg, 2013; Verona, Patrick, & Joiner, 2001). These three personality patterns share characteristic deficits in their ability to empathize with others, exaggerated, arrogant, or unstable self-view, excessive engagement in risk-taking behaviors, antagonism characterized by hostility or grandiosity, and an increased likelihood of engaging in deceitful and/or exploitive behaviors to manipulate others for personal gain (APA, 2013). For individuals with high levels of these traits, the effect of their behavior on others (e.g., attention from others; sense of excitement from interpersonal drama) is rewarding. The distinct presentation of both low desire and high plans for suicide may be a manifestation of the manipulation that is consistent with the nature of these psychopathologies.
To the authors’ knowledge, no research, to date, has examined the existence and characteristics of this subset of individuals expressing high plans and low desire for suicide. Greater understanding of the characteristics of this unique subset will be vital to clinicians assessing suicide risk during risk assessments. Findings will also impact our understanding of suicide risk factors as the two-factor model of suicidal desire and plans serves as the foundation of many models of suicide, including the interpersonal theory of suicide (Joiner, 2005) and the integrated motivational-volitional model of suicidal behavior (O’Connor, 2011), and suicide risk assessment (Chu et al., 2015; Joiner et al., 1999).
Given the high base rates of suicide attempts and death by suicide and personality psychopathology in military populations (LeardMann et al., 2013), a young adult U.S. military personnel sample was selected as the foundation for examining this unique population. The primary goal of this study was to identify and characterize the antisocial, borderline, and narcissistic personality psychopathology of military members who endorse a unique combination of low desire and high plans for suicide. Avoidant and dependent PD are phenotypically distinct from antisocial, borderline, and narcissistic PD (Trull et al., 2012). Thus, avoidant and dependent PD were compared to antisocial, borderline, and narcissistic PD to determine whether it is the presence of PD symptoms or, more specifically, antisocial, borderline, and narcissistic PD that accounts for the presence of low desire and high plans for suicide. We hypothesized that compared to individuals who endorse other combinations of suicide desire and planning, individuals presenting with low desire and high plans for suicide would display more symptoms of antisocial, borderline, and narcissistic PD than avoidant and dependent PD.
Methods
Participants
Participants were 250 military members (82% male) with an average age of 22.2 years (SD = 2.77) recruited from four U.S. Army Medical Center affiliated sites (i.e., 2 outpatient clinics, an inpatient facility, and an emergency room) for a treatment efficacy study. The study targeted young adults at high risk for suicidality – individuals whose referrals were precipitated by a suicide attempt, and/or those suffering from a mood disorder, adjustment disorder, or alcohol use disorder with concurrent suicidal ideation (Rudd et al., 1996). Data regarding the amount of time spent in military service were unavailable. The participants were primarily non-Hispanic White (60%), 25.3% African American, 10.5% Hispanic, 1.5% Native American, and 1.2% Asian American. Based on the Diagnostic Interview Schedule (DIS; Blouin et al., 1988), the diagnostic breakdown was as follows: 40% major depressive disorder, 15% bipolar spectrum disorders, 13% anxiety disorders, and 5% schizophrenia spectrum disorders. 20% of the participants had comorbid posttraumatic stress disorder, and 20% had comorbid substance use disorder (mean diagnoses = 3). 61.6% reported a history of at least one suicide attempt (n = 154) with the number of previous attempts ranging from 0 to 50 (M = 1.23, SD = 3.52).
Procedures
Internal Review Board approval was obtained for this study. Patients were informed of the study objectives, screened and assigned into a treatment group. Following the provision of full, written, and informed consent, baseline data and assessment, which included the completion of self-report measures and diagnostic interviews, was conducted over the course of one to two days. Follow-up assessments were completed at 1, 6, 12, 18, and 24-months. Presentation at baseline was reflective of individuals in crises and not indicative of typical functioning, thus distorting presentation of personality psychopathology. As such, data from the first follow-up time point (one month post baseline) were used. Patients were interviewed and evaluated by a consistent team of trained clinical staff, which included two licensed, doctoral-level psychologists, three licensed masters-level professionals, and one advanced-level doctoral student who provided no direct clinical care. For details, refer to Rudd et al. (1996).
Millon Clinical Multiaxial Inventory (MCMI; Millon, 1983)
The MCMI contains 175 true-false items designed to assess psychopathology in psychiatric patients. These items correspond to 24 clinical scales. Millon (1983) established adequate test-retest reliability (.88-.93) and validity (alpha = .67-.89) for the MCMI scales; others have reported good convergent validity (Craig & Olson, 2001) and utility in a variety of settings, including the military (Choca, Shanley & Van Denburg, 1992; Rudd & Orman, 1996). This study examined symptoms of five PDs: avoidant, dependent, borderline, antisocial, and narcissistic PD. All participants produced a valid MCMI profile. Notably, the DIS, which includes antisocial PD as a diagnosis, correlated strongly with MCMI antisocial scores (r = .89).
Modified Scale for Suicidal Ideation (MSSI; Miller, Norman, Bishop, & Dow, 1986)
Based on Beck, Kovak, and Weissman’s Scale for Suicidal Ideation, the MSSI is an 18-item clinician-administered measure assessing suicidal symptoms that occurred in the last year. Total scores range from 0 to 54 and higher scores indicate greater suicidal symptoms. Miller and colleagues (1986) reported adequate reliability (alpha coefficient = .94), construct validity, and inter-rater reliability. Factor analyses conducted by Joiner, Rudd, and Rajab (1997) revealed two factors, Suicidal Desire and Ideation, and Resolved Plans and Preparation, as well as good psychometric properties (alpha coefficients = .88, .79, respectively). Symptoms comprising the suicidal desire factor include reasons for living (reversed), wish to die and not to live, frequency of ideation, passive attempt, desire for suicide, and talk of death or suicide (9 items, max = 27). In contrast, symptoms comprising the suicidal plans factor reflect a readiness to die by suicide and intense, acute ideation (e.g., sense of fearlessness about suicide, available means, preparation for an attempt, specificity of suicide plan; 7 items, max = 21). In this study, inter-rater reliability for the MSSI was unavailable due to limitations in resources. However, MSSI desire and plans showed positive correlations with self-reported depressive symptoms (BDI; r = .47, .42, respectively, both p <.001) and hopelessness (BHS; r = .43, .35, respectively, both p <.001), which were expected based on previous research (Miller, Norman, Bishop, & Dow, 1986).
Beck Depression Inventory (BDI; Beck & Steer, 1987)
The BDI is a 21-item inventory measuring depressive symptoms. The BDI possesses good psychometric properties, high levels of concurrent and construct validity, and high internal consistency (alpha coefficients = .81-.86; Beck & Steer, 1987). The BDI correlates highly with the newer version of this inventory, the BDI-II (Beck, Steer, Ball, & Ranieri, 1996). Coefficient alpha for the present study was .92.
Statistical Approach
SPSS Statistics 22 was used. Given that this study was interested in individuals endorsing varying levels of desire and plans, the simple interaction effects of desire at high levels of plans were tested in relation to personality psychopathology. First, multiple regression analyses were used to examine the interaction between MSSI desire and plans for suicide as a predictor of five PD subscales of the MCMI: antisocial, borderline, narcissistic, dependent, and avoidant PDs. The interaction term was generated from MSSI desire and MSSI plans, both centered at their median. Significant interactions were interpreted post-hoc (Aiken & West, 1991). Specifically, the simple effects of MSSI desire at high (1SD above the median) levels of plans were probed. Predicted values of high and low MSSI desire and plans were generated from unstandardized regression coefficients. In all analyses, the following covariates were controlled: gender, age, and depressive symptoms. Expectation-maximization was used to handle missing data, which were minimal (5% missing).
Results/Discussion
Multicollinearity was examined for all regression equations; tolerance and variance inflation factor values were within acceptable range (>.10 or < 10, respectively). Suppression was also examined for all regression equations; beta values were within acceptable range (Beta < zero-order correlation). All variables evidenced acceptable skew and kurtosis values. Univariate outliers (median +/− 2 interquartile ranges) were identified for antisocial PD and BDI total score. Outliers were addressed by bringing the score in question to the next highest value within two interquartile ranges. No bivariate outliers were identified. Of note, analyses were conducted with the outliers included and the pattern of findings remained the same. A post-hoc power analysis conducted using G*Power (Faul et al., 2007) indicated that this study, which had a sample size of 250, had sufficient power (.81) to detect a small effect size (f2 = .04).
Means, standard deviations, and intercorrelations between main study variables are presented in Table 1. Multiple regression analyses are summarized in Table 2. Overall, results indicated that MSSI desire and plans significantly interacted to predict MCMI antisocial (β = .62, p = .001),1 narcissistic (β = .71, p <.001), borderline (β = −.37, p = .04), dependent (β = −.51, p = .006), and avoidant (β = −.41, p <.001) PDs.
Table 1.
Means, Standard Deviations, and Correlations between Key Study Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | M | SD | |
|---|---|---|---|---|---|---|---|---|---|
| 1. MSSI Desire | - | 6.97 | 5.24 | ||||||
| 2. MSSI Plan | .66** | - | 10.44 | 4.64 | |||||
| 3. Avoidant PD | .33** | .25* | - | 57.61 | 30.84 | ||||
| 4. Dependent PD | .12 | .10 | .55** | - | 55.94 | 28.93 | |||
| 5. Narcissistic PD | −.18 | −.12 | −.70** | −.50** | - | 67.54 | 24.08 | ||
| 6. Antisocial PD | −.13 | −.16 | −.42** | −.65** | .75** | - | 67.95 | 23.33 | |
| 7. Borderline PD | .35** | .30** | .64** | .41** | −.43** | −.26** | - | 54.80 | 16.86 |
| 8. BDI | .40** | .37** | .64** | .29** | −.53** | −.26** | .61** | 10.03 | 9.80 |
Note.
p <.05;
p <.01
PD = Millon Clinical Multiaxial Inventory personality disorder. BDI = Beck Depression Inventory total score. N ranged from 245 to 250 due to missing values.
Table 2.
Summary of Regression Analyses with MSSI Desire and MSSI Plans as Predictors of MCMI Personality Psychopathology
| MSSI Desire Main Effect |
MSSI Plans Main Effect |
Desire × Plans Interaction |
Model Summary |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| MCMI PD | Beta | p | pr | Beta | p | pr | Beta | p | pr | R2 |
| Avoidant | .49 | <.001 | .06 | .31 | .008 | .03 | −.41 | <.001 | .05 | .220 |
| Dependent | .46 | .01 | .03 | .28 | .03 | .02 | −.51 | .006 | .03 | .087 |
| Narcissistic | −.77 | <.001 | .08 | −.31 | .009 | .03 | .71 | <.001 | .07 | .199 |
| Antisocial | −.52 | .003 | .04 | −.40 | .001 | .04 | .62 | .001 | .05 | .142 |
| Borderline | .51 | .003 | .04 | .27 | .03 | .02 | −.37 | .04 | .02 | .183 |
Note.
Beta = standardized regression coefficients; pr = partial r2
MSSI = Modified Scale for Suicidal Ideation. MCMI PD = Millon Clinical Multiaxial Inventory (MCMI) Personality Psychopathology Subscales. In all regression equations, age, gender, and depressive symptoms were entered as covariates.
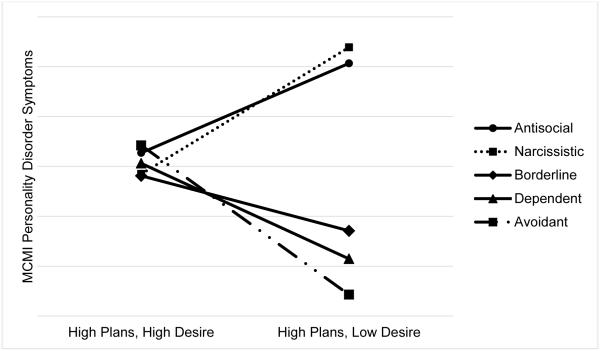
All significant interactions were probed. Results showed that decreases in desire are associated with significantly increased antisocial PD at high plans (β = −.29, p =.03, partial r2 (pr) = .02), and increased narcissistic PD at high plans (β = −.49, p <.001, pr = .06). Decreases in desire are associated with significantly decreased borderline PD at high plans (β = .37, p = .004, pr = .03), decreased dependent PD at high plans (β = .26, p = .05, pr = .02), and decreased avoidant PD at high plans (β = .49, p <.001, pr = .06). Predicted PD values at the junction of MSSI desire and plans are presented (Table 3; Figure 1). Of note, item-level analyses indicated that items reflecting fearlessness and capacity for suicide loaded on MSSI plans, which supports our interpretations of low desire and high plans as a form of manipulation.
Table 3.
Predicted values at low (−1SD from median) and high (+1SD from median) MSSI desire and MSSI plans.
| MCMI Personality Disorder Symptoms | |||||
|---|---|---|---|---|---|
|
| |||||
| Groups | Antisocial | Narcissistic | Borderline | Dependent | Avoidant |
| Low Desire Low Plans |
71.31 | 79.23 | 48.11 | 51.03 | 42.88 |
| Low Desire High Plans |
101.34 | 107.78 | 34.14 | 22.92 | 8.52 |
| High Desire Low Plans |
57.92 | 55.29 | 60.57 | 66.19 | 72.81 |
| High Desire High Plans |
65.42 | 56.98 | 56.22 | 61.22 | 68.40 |
Note.
MCMI = Millon Clinical Multiaxial Inventory. MSSI = Modified Scale for Suicidal Ideation.
Multiple regression analyses were used to examine whether the interaction of MSSI desire and MSSI plans, both centered at the median, predicted MCMI PD symptoms, controlling for age, gender, and depressive symptoms. Significant interactions were probed and predicted values were generated based on unstandardized regression coefficients.
Figure 1.
Modified Scale for Suicidal Ideation (MSSI) Suicidal Desire and Ideation, and Resolved Plans and Preparations Factors, and Millon Clinical Multiaxial Inventory (MCMI) Personality Psychopathology Subscales. Graph depicts the predicted MCMI subscale scores by the interaction between MSSI Desire and MSSI Plans. Lines represent the five MCMI personality psychopathology subscales at high plans/high desire and high plans/low desire.
Given that one would expect individuals who report highly detailed and specific suicide plans to simultaneously reveal a strong desire for suicide, the notion of an individual presenting with highly detailed suicide plans, but low suicidal desire is somewhat counterintuitive. This presentation of high plans and low desire may make the assessment of suicide risk – an already daunting task – even more challenging for clinicians. Greater understanding of the personality characteristics of this subset may help clinicians better assess and manage suicide risk. Thus, this study sought to characterize the personality psychopathology of inpatients and outpatients presenting with low desire and high plans for suicide in a high-risk military sample. Consistent with expectations, results revealed significantly higher levels of antisocial and narcissistic PD symptoms among patients endorsing low desire and high plans for suicide. As predicted, this subset of individuals reported significantly fewer symptoms of avoidant and dependent PD. However, contrary to our hypothesis, this subset displayed significantly fewer symptoms of borderline PD – a point to which we will return.
These findings suggest that individuals demonstrating antisocial and narcissistic symptoms, and simultaneously presenting with low desire and high plans for suicide may do so to manipulate others for personal gain. If indeed manipulation is the explanation for the current findings, then one may wonder why this subset chooses to endorse a suicide plan when claiming ideation/desire may be an easier and, perhaps, equally effective, means of manipulating others. Given that many individuals exhibiting antisocial or narcissistic symptoms also exhibit erratic behavioral tendencies (Crawford, Cohen, & Brook, 2001), one hypothesis is that these individuals are attempting to gain some form of attention using suicide and are not fully informed about suicidality. In this case, a pattern where marked (salient and severe, i.e., plan for a suicide attempt) symptoms of suicidality are endorsed more than are less marked symptoms (i.e., desire not to live) is conceivable. Although the answer remains to be determined with further research, these individuals may present with high plans but relatively low desire.
Alternatively, this pattern of low desire and high plans may present among individuals suffering from a debilitating mental or physical condition, particularly those in the initial phases of the condition. In this case, while individuals may not desire death, they may view death by suicide as a preferable outcome to future suffering, and thus, develop a plan for suicide. These individuals may also present with lower levels of suicidal desire and significant suicide plans. Although this study examines manipulative personality traits as an explanation for this phenomenon, future studies exploring alternative explanations, such as the diagnosis of a terminal illness, are needed to draw conclusions regarding individuals presenting with this unique suicide risk profile.
Contrary to expectations, results indicated that individuals endorsing low desire and high plans for suicide did not report significantly greater symptoms of borderline PD. Though contrary to expectations, one possibility is that suicidality among individuals with symptoms of borderline PD tends to be genuine. Borderline PD is one of the strongest predictors of suicidal behavior: approximately half of borderline PD patients have a minimum of one very severe suicide attempt, and the average number of lifetime suicide attempts is more than three (Joiner, Brown, & Wingate, 2005). Further, some research suggests that individuals with borderline PD symptoms exhibited little to no impairments in their ability to accurately judge others’ emotions (Wagner & Linehan, 1999), which indicates that borderline PD may be associated with fewer deficits in empathy compared to other PDs in cluster B. Additionally, research from the perspective of the Five Factor Model of Personality suggests that borderline personality disorder shares the same configuration of features (i.e., high neuroticism, low agreeableness, low conscientiousness) with cluster C PDs, including avoidant PD (Morey et al., 2002). Consistent with this research, the pattern of results for borderline PD appear to be more similar to that of cluster C avoidant and dependent PDs. Overall, these findings suggest that individuals with borderline PD symptoms may be less likely to report low desire and high plans for suicide as a means for manipulation and more likely to report genuine (and often high; Blasco-Fontecilla et al., 2009) desire for suicide.
While the findings from the present study support the existence of this subset, these findings should be interpreted in the context of limitations. For one, future studies would benefit from the use of measures of personality psychopathology symptoms that are consistent with the latest version of diagnostic criteria. Additionally, while the limited sample size of the population of interest is, in and of itself, informative, a larger sample is necessary to provide adequate power to test hypotheses regarding suicide risk. Relatedly, caution is warranted in generalizing the present findings beyond young adults in the military. Replication of these findings, not only in military samples, but also other, high-risk samples (e.g., prison inmates, civilian inpatients) would be useful for determining whether these findings are sample-specific.
It is important to note that the current study did not compare suicide risk associated with the low desire/high plans presentation. In line with features associated with antisocial and narcissistic PD, including a sense of fearlessness, it is possible to imagine that such individuals adopt the perspective of “I could die by suicide, if I wanted to.” This unpredictable nature, which is associated with the nature of their personality psychopathology (APA, 2013), may suggest lower suicide risk, as they do not report the desire to die. However, their psychopathology and the availability of a suicide plan, which suggest high risk, make it difficult to predict suicide risk. Thus, should this subset of individuals exist in other samples, it would be useful for future studies to examine whether those who endorse low desire and high plans for suicide are at greater risk for engaging in suicide-related behaviors than those presenting with other combinations of suicidal desire and plans.
This was the first preliminary investigation to highlight a subgroup of individuals who exhibit characteristics that are important to acknowledge when examining suicide-related behaviors in civilian and military populations. This study was strengthened by the use of a multi-method assessment approach (i.e., self-reported personality disorder symptoms, clinician-rated suicidality). Further, given that suicide risk is typically elevated in military personnel, the use of a high-risk, clinical, military sample in the present study is notable.
Crucially, this research may be implemented into clinical practice and existing suicide risk assessment protocols. The presence of significantly detailed plans and low desire for suicide should alert the clinician consider the patients presentation thoroughly, including the possibility of secondary gains, before concluding that the patient is at high risk for risk. This unique presentation may indicate the need for more thorough assessment and management of both personality disorder symptoms and suicide risk. Clinicians confronted with this seemingly counterintuitive suicide presentation may also find it useful to assess imminent suicide risk factors that have less face validity, and are therefore less susceptible to manipulation, such as agitation, marked irritability, sleep disturbances, significant weight loss, and social withdrawal (Busch Fawcett, & Jacobs, 2003; Robins, 1981). Appropriate actions may include the management of suicide risk and adjunctive treatments for PD symptoms.
The present study represents an effort to highlight the presence of select individuals who present with a unique constellation of suicide risk factors, namely low desire and high plans for suicide, and document their pattern of personality psychopathology. This study found that the presentation of low desire and high plans for suicide is associated with higher levels of antisocial and narcissistic PD symptoms. These findings directly impact suicide prevention and treatment protocol as knowledge of characteristics associated with low desire and high plans for suicide is important for clinical decision-making (i.e., risk assessment) and improving the specificity and efficacy of risk assessments in clinical health systems. As this is the first study to examine this subset of individuals, we look forward to further research efforts to determine the replicability and generalizability of these findings.
Acknowledgments
This research was supported, in part, by grants from the National Institute of Mental Health to Carol Chu (5 T32 MH093311-04), Jennifer M. Buchman-Schmitt (5 T32 MH093311-04), and from the National Institute of Mental Health, Prevention Research Branch (MH48097). This article was also supported by grants awarded to the Denver VA Medical Center and to Florida State University by the Department of Defense. The Department of Defense had no further role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication. The content of this paper is solely the responsibility of the authors and the views and opinions expressed do not necessarily represent those of the Department of Veterans Affairs, the Department of Defense, or the United States Government.
Footnotes
Of note, the pattern of findings remained the same when DIS antisocial PD score was entered into a regression equation as the dependent variable (β = .58, p = .002).
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; Newbury Park, London: 1991. [Google Scholar]
- American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders. 5th American Psychiatric Publishing; Arlington, VA: 2013. [Google Scholar]
- Beck AT, Brown GK, Steer RA. Psychometric characteristics of the Scale for Suicide Ideation with psychiatric outpatients. Behaviour Research and Therapy. 1997;35(11):1039–1046. doi: 10.1016/s0005-7967(97)00073-9. doi: 10.1111/j.1943-278X.1999.tb00758.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. BDI, Beck Depression Inventory: Manual. Psychological Corporation; San Antonio, TX: 1987. [Google Scholar]
- Beck AT, Steer RA, Ball R, Ranieri WF. Comparison of Beck Depression Inventories-IA and-II in psychiatric outpatients. Journal of Personality Assessment. 1996;67(3):588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Blasco-Fontecilla H, Baca-Garcia E, Dervic K, Perez-Rodriguez MM, Saiz-Gonzalez MD, Saiz- Ruiz J, Oquendo MA, De Leon J. Severity of personality disorders and suicide attempt. Acta Psychiatrica Scandinavica. 2009;119(2):149–155. doi: 10.1111/j.1600-0447.2008.01284.x. doi: 10.1111/j.1600-0447.2008.01284.x. [DOI] [PubMed] [Google Scholar]
- Blouin A, Perez E, Blouin J. Computerized administration of the Diagnostic Interview Schedule. Psychiatry Research. 1988;23:335–344. doi: 10.1016/0165-1781(88)90024-8. doi: 10.1016/0165-1781(88)90024-8. [DOI] [PubMed] [Google Scholar]
- Busch KA, Fawcett J, Jacobs DG. Clinical correlates of inpatient suicide. The Journal of Clinical Psychiatry. 2003;64:14–9. doi: 10.4088/jcp.v64n0105. [DOI] [PubMed] [Google Scholar]
- Choca JP, Shanley LA, Van Denburg E. Interpretative guide to the Millon Clinical Multiaxial Inventory. American Psychological Association; 1992. [Google Scholar]
- Craig RJ, Olson RE. Adjectival descriptions of personality disorders: A convergent validity study of the MCMI-III. Journal of Personality Assessment. 2001;77(2):259–271. doi: 10.1207/S15327752JPA7702_09. [DOI] [PubMed] [Google Scholar]
- Crawford TN, Cohen P, Brook JS. Dramatic-erratic personality disorder symptoms: I. Continuity from early adolescence into adulthood. Journal of Personality Disorders. 2001;15(4):319–335. doi: 10.1521/pedi.15.4.319.19182. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Brown JS, Wingate LR. The psychology and neurobiology of suicidal behavior. Annual Review of Psychology. 2005;56:287–314. doi: 10.1146/annurev.psych.56.091103.070320. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Rudd MD, Rajab MH. The Modified Scale for Suicidal Ideation: factors of suicidality and their relation to clinical and diagnostic variables. Journal of Abnormal Psychology. 1997;106(2):260–265. doi: 10.1037//0021-843x.106.2.260. doi: 10.1037/0021-843X.106.2.260. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Steer RA, Brown G, Beck AT, Pettit JW, Rudd MD. Worst-point suicidal plans: a dimension of suicidality predictive of past suicide attempts and eventual death by suicide. Behaviour Research and Therapy. 2003;41(12):1469–1480. doi: 10.1016/s0005-7967(03)00070-6. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Walker RL, Rudd MD, Jobes DA. Scientizing and routinizing the assessment of suicidality in outpatient practice. Professional Psychology: Research and Practice. 1999;30(5):447–453. doi: 10.1037/0735-7028.30.5.447. [Google Scholar]
- LeardMann CA, Powell TM, Smith TC, Bell MR, Smith B, Boyko EJ, Hooper TI, Gackstetter GD, Ghamsary M, Hoge CW. Risk factors associated with suicide in current and former US military personnel. JAMA: The Journal of the American Medical Association. 2013;310(5):496–506. doi: 10.1001/jama.2013.65164. doi:10.1001/jama.2013.65164. [DOI] [PubMed] [Google Scholar]
- Miller IW, Norman WH, Bishop SB, Dow MG. The Modified Scale for Suicidal Ideation: reliability and validity. Journal of Consulting and Clinical Psychology. 1986;54(5):724–725. doi: 10.1037//0022-006x.54.5.724. doi: 10.1037/0022-006X.54.5.724. [DOI] [PubMed] [Google Scholar]
- Millon T. Millon Clinical Multiaxial Inventory manual. Interpretative Scoring Systems; Minneapolis, MN: 1983. [Google Scholar]
- Morey LC, Gunderson JG, Quigley BD, Shea MT, Skodol AE, McGlashan TH, Zanarini MC. The representation of borderline, avoidant, obsessive-compulsive, and schizotypal personality disorders by the five-factor model. Journal of Personality Disorders. 2002;16(3):215–234. doi: 10.1521/pedi.16.3.215.22541. [DOI] [PubMed] [Google Scholar]
- O’Connor RC. International handbook of suicide prevention: Research, policy and practice. John Wiley & Sons, Ltd; Chichester, UK: 2011. Towards an integrated motivational–volitional model of suicidal behaviour; pp. 181–198. [Google Scholar]
- Robins E. The Final Months: A Study of the Lives of 134 Persons Who Committed Suicide. Oxford University Press; Oxford, UK: 1981. [Google Scholar]
- Ronningstam E, Weinberg I. Narcissistic Personality Disorder: Progress in Recognition and Treatment. FOCUS: The Journal of Lifelong Learning in Psychiatry. 2013;11(2):167–177. doi:10.1176/appi.focus.11.2.167. [Google Scholar]
- Rudd MD, Orman DT. Millon Clinical Multiaxial Inventory profiles and maladjustment in the military: preliminary findings. Military Medicine. 1996;161(6):349–351. [PubMed] [Google Scholar]
- Rudd MD, Rajab H, Orman D, Stulman D, Joiner T, Dixon W. Effectiveness of an outpatient problem-solving intervention targeting suicidal young adults: Preliminary results. Journal of Consulting and Clinical Psychology. 1996;64:179–190. doi: 10.1037//0022-006x.64.1.179. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The interpersonal theory of suicide. Psychological Review. 2010;117(2):575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verona E, Patrick CJ, Joiner TE. Psychopathy, antisocial personality, and suicide risk. Journal of Abnormal Psychology. 2001;110(3):462–470. doi: 10.1037//0021-843x.110.3.462. [DOI] [PubMed] [Google Scholar]
- Wagner AW, Linehan MM. Facial expression recognition ability among women with borderline personality disorder: implications for emotion regulation? Journal of Personality Disorders. 1999;13(4):329–344. doi: 10.1521/pedi.1999.13.4.329. [DOI] [PubMed] [Google Scholar]