Abstract
The Barriers to Smoking Cessation Scale (BCS) was developed to assess global and specific perceived barriers that may interfere with the quit process. Although the BCS is widely used in the literature, little scientific work has been devoted to examining the psychometric properties of the measure. Thus, the present study sought to address this gap by evaluating the BCS in a sample of 497 treatment-seeking smokers. The current study examined the factor structure of the BCS, measurement invariance of the BCS subscales across sex and over two time points, and evaluated construct validity. Results indicated that the BCS was best modeled by a higher-order factor structure wherein the originally proposed three-factor solution (Addiction, External, and Internal) constituted the lower-order and a global factor constituted the higher-order factor. The higher-order BCS structure demonstrated partial measurement invariance across sex and full measurement invariance from baseline to quit day among treatment seeking smokers. Additionally, expected relations were observed between the BCS subscales and similar and divergent constructs, and predictive validity was partially supported. The current findings provide novel empirical evidence that the BCS is a reliable measure of perceived barriers to smoking cessation across multiple domains and is related to several affective and smoking processes the may interfere with the process of quitting.
Keywords: Smoking, Barriers to Cessation, Tobacco, Measurement, Addiction
The efficacy of pharmacological and psychosocial treatments for smoking cessation has been well-established (Fiore et al., 2008). Approximately 70% of current adult smokers are motivated to quit (CDC, 2010). However, in spite of the efficacious intervention programs and high rate of motivation to quit, less than 10% of smokers utilize smoking cessation treatments. Moreover, less than 40% of smokers who engage in treatment adhere to treatment protocol (Sabaté, 2003), and only 10–40% achieve long-term abstinence (CDC, 2010). Such large inconsistencies between motivation to quit and engagement in treatment suggest substantial barriers to initiating and adhering to smoking cessation efforts. Indeed, numerous barriers to smoking cessation have been identified, including policy, environmental, and financial factors (Rosenthal et al., 2013; Twyman, Bonevski, Paul, & Bryant, 2014). Yet, comparatively little empirical work has explored individual differences in perceived barriers for smoking cessation.
Perceived barriers for smoking cessation refers to individual differences in perceptions of smoking cessation stressors that interfere with one’s ability to engage in quitting behavior (Macnee & Talsma, 1995a). To our knowledge, the only available measure to assess perceived barriers for smoking cessation is the Barriers to Cessation Scale (BCS; Macnee & Talsma, 1995a). The BCS was developed to assess processes related to barriers to cessation. Within the theoretical framework of the Transactional Model of Stress (Lazarus & Folkman, 1984), the BCS was designed to evaluate both primary (e.g., recognition of aspects of smoking cessation as threatening) and secondary (e.g., perceived inability to cope with threats to cessation) cognitive appraisals of stressors associated with cessation. Indeed, this measure addressed a significant gap in the literature by recognizing that perceived inability to cope with perceived barriers may negatively impact a smoker’s interest in, motivation for, and ultimate quit success (Macnee & Talsma, 1995a).
The BCS is a 19-item measure that was initially evaluated on a sample of 186 individuals from three studies combined to represent one sample. Participants from these studies included smokers: (a) in the process of quitting, (b) enrolled in a pilot study for smoking cessation trial, and (c) who engaged in actions to quit during an observational study. Findings from this work suggests that the BCS maintains a global score wherein all the items are summed and three lower-order factors using 18 items (omitting a ‘Weight gain’ item because it has previously been found to not load onto any of the three factors; Macnee & Talsma, 1995a). The three lower-order factors capture tobacco addiction stressors, such as “Thinking about cigarettes all the time” (Addiction subscale); external stressors, such as peer pressure to smoke (External subscale); and internal stressors, such as anxiety or irritability (Internal subscale).
Theoretical and empirical evidence implicates perceived barriers to cessation in behavior related to smoking maintenance and quit processes. Theoretically, because smoking may alleviate negative affective states (Kassel, Stroud, & Paronis, 2003), persons with greater perceived barriers or stressors about quitting may be more apt to regulate their stress by smoking, which in turn, may increase their vulnerability to smoking persistence and dependence (West, Hajek, & Belcher, 1989). Thus, perceived barriers for quitting may play a central role in theoretical models of smoking maintenance and relapse. Consistent with this perspective, the BCS total score is associated with numerous aspects of smoking behavior, including tobacco dependence and cigarettes smoked per day (El-Shahawy & Haddad, 2015; Mahaffey et al., 2015). Moreover, the BCS total score is related to other smoking-based processes that may interfere with cessation, including smoking outcome expectancies (Foster, Zvolensky, Garey, Ditre, & Schmidt, 2014; Johnson, Farris, Schmidt, & Zvolensky, 2012; Peasley-Miklus, McLeish, Schmidt, & Zvolensky, 2012), smoking-specific experiential avoidance (i.e., avoidance or inflexibility in the presence of uncomfortable or difficult sensations or thoughts related to smoking (i.e., avoidance or inflexibility in the presence of uncomfortable or difficult sensations or thoughts related to smoking; Foster et al., 2014), severity of quit problems (i.e., weight gain, nausea, headache; Farris, Langdon, DiBello, & Zvolensky, 2015; Mahaffey et al., 2015), and commitment to quitting (Moore et al., 2013). The BCS total score is also associated with several affective processes, including dysphoria (Buckner et al., 2015) and negative affect (Foster et al., 2014; Gregor, Zvolensky, McLeish, Bernstein, & Morissette, 2008; Zvolensky et al., 2007). Regarding quit behavior, the BCS total score has been found to differentiate and successfully classify quitters and non-quitters following a quit attempt (Macnee & Talsma, 1995a). Extant work also indicates the BCS as a useful assessment tool to identify smokers who may have more or less difficulty quitting by virtue of how stressful they perceive quitting to be and also help gauge (indirectly) motivation to quit (e.g., greater perceived obstacles may be related to lesser motivation to quit; Macnee & Talsma, 1995b).
Comparatively, work with the BCS subscales has been limited. Of the available work, the Addiction and External subscales have demonstrated some initial clinical utility to differentiate exclusive cigarette smokers from smokers who use multiple tobacco products (El-Shahawy et al., 2015) as well as identify a smoker’s stage of change and readiness to change (Haddad & Petro-Nustas, 2006). Other work has found that the Addiction and Internal subscales assessed at quit day are related to abstinence at 1-month post quit (Albanese et al., 2016).
Despite the apparent clinical utility of the BCS, little scientific work has been devoted to examining the psychometric properties of the measure. There has only been one psychometric evaluation of the scale completed as part of its original development (Macnee & Talsma, 1995a). As a result, there are numerous central gaps in knowledge about the psychometric performance of the BCS despite its use in clinical and research settings. First, the psychometric qualities and structure of this measure have not been well established. Indeed, although the BCS is most widely used under the working assumption that it is a unidimensional construct (e.g., the total score is utilized), the overall fit for a one-factor model has yet to be examined. Thus, it is presently unknown if a one-factor BCS composite adequately captures the covariance between items on the measure. Moreover, the assumed three-factor structure has not been evaluated in an independent sample of smokers. Indeed, the sample size-to-item ratio (approximately 10:1) in the original principal components factor analysis (Macnee & Talsma, 1995a) suggests that the final factor structure and indicators of each component may possibly yield less than ideal reliable results (Costello & Osborne, 2011), and warrants replication. Similarly, while purported to be a valid and clinically important construct in the context of smoking cessation (Macnee & Talsma, 1995a), the psychometric properties of the BCS beyond internal consistency have not been evaluated in a large sample of treatment-seeking smokers. Thus, it is presently unknown how a one-factor solution fits BCS data obtained from a smoking cessation trial, and how this solution may compare to a three-factor solution.
Second, it is possible that the best fitting solution for the BCS may be a higher-order factor structure in which the observed variables load onto the originally proposed subscales (i.e., first order factors) and the first order factors load onto a higher, second order general factor. A higher-order factor structure is appropriate when there is evidence that first order factors are highly correlated (Reise, Moore, & Haviland, 2010), which has been observed with the BCS. Indeed, the BCS subscales were rotated using an oblique rotation in the initial investigation of the BCS structure because they were theorized to correlate. Subsequent empirical work has corroborated the theorized correlation across the subscales (Macnee & Talsma, 1995a). Considering the common use of a total score and the high correlation across subscales, it may be that covariance between items and subscales is best captured by a higher-order factor structure. Yet, no extant work has examined a higher-order factor structure for the BCS.
Third, no study has assessed reliability or measurement invariance of the BCS across sex or over time. Reliability evidence provides important information about the general psychometric attributes of a measure (Vandenberg & Lance, 2000), yet no study has examined reliability of the BCS beyond internal consistency at a single time point. Similarly, measurement invariance, or stability of the construct, across sex or longitudinally (Vandenberg et al., 2000), has not been assessed for the BCS. Measurement invariance assesses if indicators load onto underlying factors the same way across groups or over time and provides empirical evidence that the fundamental meaning of a construct is not confounded by differences (across sex) or changes (across time) in perceptions or other variables (Little, Preacher, Selig, & Card, 2007; Vandenberg et al., 2000). Without establishing measurement invariance, bias may be introduced into the examination of the construct and interpretation of results (McHorney & Fleishman, 2006) and differences cannot be “unambiguously interpreted” (Horn & McArdle, 1992). Thus, testing and establishing measurement invariance is necessary for future researchers to accurately conclude that observed differences in the BCS across sex and changes in the BCS over time are due to true changes in the construct.
Finally, limited work has examined the relation between BCS and abstinence or severity of withdrawal symptoms. Although the BCS has been found to differentiate quitters from non-quitters after a quit attempt (Albanese et al., 2016; Macnee & Talsma, 1995a), this work has focused on post-treatment assessments of BCS to predict abstinence at the same or later time point. Thus, it remains unknown if pre-treatment BCS scores might have clinical utility to identify smokers who may experience more difficulty quitting. Additionally, given the robust association between withdrawal severity and relapse (Piasecki et al., 2000), understanding predictors of withdrawal severity is paramount to treatment development that integrates perceived barriers to cessation processes. Lastly, although theoretically (Kassel et al., 2003) BCS may relate to abstinence though negative mood states or affect, this model has not been empirically examined. Despite the BCS capturing elements that may interfere with cessation, no study has examined the BCS or its subscales as predictors of withdrawal severity or pathways through which BCS may contribute to abstinence.
Together, the current study sought to address a number of notable, clinically-relevant gaps related to the psychometric evaluation of the BCS. Specifically, the BCS was evaluated for its factor structure, internal consistency, measurement invariance, associations with similar and divergent measures, and predictive validity among a sample of treatment seeking smokers. To evaluate the factor structure of the BCS, we examined model fit for one-, three-, and higher-order factor models of the BCS using baseline data. We hypothesized that the three-, and higher-order factor models would demonstrate superior fit relative to the one-factor model structure, and that the higher-order factor would demonstrate comparable fit to the three-factor model considering that there are only three first-order factors. Additionally, we evaluated the internal consistency of each BCS subscale and the total score at baseline and quit day. We hypothesized that the subscales and total score would demonstrate acceptable internal consistency. Next, we examined measurement invariance of the BCS at baseline across sex to ensure that the structural organization of the BCS is consistent for men and women. After establishing measurement invariance across sex, we examined measurement invariance of the BCS between baseline and quit day (measured at 4 weeks post baseline appointment) to ensure that the structural organization of the BCS is stable over time. We hypothesized that the BCS would demonstrate at least partial measurement invariance across both sex and time.
We further evaluated the construct validity of the BCS by examining associations between BCS subscales and total score and affective and smoking processes posited to relate to BCS, including dysphoria (Buckner et al., 2015), negative affect (Foster et al., 2014), social anxiety (Buckner, Zvolensky, Jeffries, & Schmidt, 2014), smoking outcome expectancies (Foster, Zvolensky, et al., 2014) as well as positive affect (Minami, Yeh, Bold, Chapman, & McCarthy, 2014) and well-being (Macnee & Talsma, 1995a). We hypothesized that all BCS subscales and the total score would positively correlate with dysphoria, negative affect, social anxiety, and smoking outcome expectancies. We also hypothesized, based on extant theoretically-driven empirical work (Macnee & Talsma, 1995a), that BCS subscales and total score would negatively relate to positive affect and well-being.
Moreover, we examined whether the BCS differentiated quitters from non-quitters at quit day, as well as the construct validity of the BCS to predict quit day withdrawal severity among successful quitters and lapse and relapse after a successful quit attempt. We hypothesized that smokers who were unsuccessful at quitting on quit day would have reported greater pre-quit barriers to cessation across the three BCS subscales and total score relative to smokers who successfully quit on quit day. Further, we hypothesized that greater scores on the BCS subscales and total score at the pre-quit assessment would relate to more severe withdrawal symptoms on quit day. Finally, informed by theory (Kassel et al., 2003), we hypothesized that great BCS across the subscales and total score would indirectly predict lapse and relapse through greater negative affectivity.
METHODS
Participants
A sample of 497 treatment-seeking adult smokers who responded to study advertisements (e.g., flyers, newspaper ads, radio announcements; 47.9% female; Mage = 36.9; SD = 13.5) were included in the study. Exclusion criteria included suicidality and psychosis. The racial/ethnic distribution of this sample was as follows: 84.5% White/Caucasian; 8.9% Black/Non-Hispanic; 0.6% Black/Hispanic; 2.6% Hispanic; 1.0% Asian; and 2.4% ‘Other.’ At least one current (past year) Axis I diagnosis was endorsed by 45.1% of the sample, most commonly social anxiety disorder (10.5%), generalized anxiety disorder (5.0%), current major depressive episode (4.4%), and posttraumatic stress disorder (3.0%). On average, participants reported smoking 16.6 cigarettes per day (SD = 10.0), had been a daily smoker for 18.5 years (SD = 13.3), and had an average expired carbon monoxide level of 19.13 parts per million (SD = 11.91); 27 participants did not provide a carbon monoxide sample. A moderate level of tobacco dependence was observed within the sample based on the Fagerström Test for Nicotine Dependence (M = 5.2, SD = 2.3; Heatherton, Kozlowski, Frecker, & Fagerström, 1991).
Measures
Demographics Questionnaire
Demographic information collected included gender, age, and race. Information collected via the demographics questionnaire was used to describe the sample.
Barriers to Cessation Scale (BCS)
The BCS (Macnee & Talsma, 1995a) is a 19-item self-report assessment of perceived barriers to or stressors resulting from smoking cessation (e.g., “Feeling less in control of your moods”). Responses are provided on a 4-point Likert scale ranging from ‘not a barrier’ (0) to ‘large barrier’ (3). The BCS has three subscales as originally developed: Addictive Barriers, External Barriers, and Internal Barriers. In the current study, the ‘Weight gain’ item was administered last.
Inventory of Depression and Anxiety Symptoms (IDAS)
The IDAS (Watson et al., 2007) is a 64-item self-report assessment of depression and anxiety symptoms (e.g., “I felt inadequate”) in which responses are provided on a 5-point scale ranging from ‘not at all’ (1) to ‘extremely’ (5). The IDAS contains 12 subscales, with some subscales sharing overlapping items: general depression (20 items), dysphoria (10 items), well-being (8 items), anxious arousal (8 items), lassitude (6 items), insomnia (6 items), suicidality (6 items), social anxiety (5 items), ill temper (5 items), traumatic intrusions (4 items), appetite loss (3 items), and appetite gain (3 items). The IDAS subscales have shown good internal consistency (α = .80 to .89) and convergent validity with other measures of depression and anxiety (Watson et al., 2007). The present study utilized the dysphoria (α = .92), social anxiety (α = .88), and well-being (α = .91) subscales.
Positive and Negative Affect Schedule (PANAS)
The PANAS (Watson, Clark, & Tellegen, 1988) is a self-report assessment of the degree to which participants usually experience 20 different positive (e.g., excited, proud) or negative affective states (e.g., afraid, distressed). Responses are provided on a Likert scale ranging from ‘very slightly or not at all’ (1) to ‘extremely’ (5). The PANAS yields two factors, positive affect (PA) and negative affect (NA), which have shown good internal consistency (PA: α = .86; NA: α = .90) and validity (Watson et al., 1988). The present study utilized both subscales. Internal consistency was excellent for both subscales (PA: α = .90; NA: α = .90).
Smoking Consequences Questionnaire (SCQ)
The SCQ (Brandon & Baker, 1991) is a 50-item assessment of smoking outcome expectancies (e.g., “cigarettes taste good”). Response options range from ‘completely unlikely’ (0) to ‘completely likely’ (9). The SCQ produces four subscales: Negative Consequences, Positive Reinforcement-Sensory Satisfaction, Negative Reinforcement-Negative Affect Reduction, and Appetite-Weight Control. In previous research, the SCQ has demonstrated excellent internal consistency (α > .90) on all subscales (Brandon et al., 1991) and convergent validity with criterion variables (e.g., smoking status; Copeland, Brandon, & Quinn, 1995). Internal consistency was good across subscales for the present study (Negative Consequences: α = .89; Positive Reinforcement-Sensory Satisfaction: α = .89; Negative Reinforcement-Negative Affect Reduction: α = .94; and Appetite-Weight Control: α = .91).
Carbon Monoxide
Biochemical verification of smoking status was assessed by expired carbon monoxide (CO) analysis of breath samples collected using a CMD/CO Carbon Monoxide Monitor (Model 3110; Spirometrics, Inc.). A cut-off of 4 ppm has demonstrated excellent properties at distinguishing smokers from nonsmokers (Perkins, Karelitz, & Jao, 2013). In the present study, the CO sample was used to describe the sample as well as classify quitters (e.g., nonsmokers) and non-quitters (e.g., smokers) on quit day.
The Minnesota Nicotine Withdrawal Scale (MNWS)
The Minnesota Nicotine Withdrawal Scale (Hughes & Hatsukami, 1986) is an 8-item measure of nicotine withdrawal symptoms, which are rated on a 4-point Likert-type scale, ranging from 0 = Not present to 3 = Severe (e.g., insomnia, irritability/frustration, difficulty concentrating, and restlessness). The MNWS assessed severity of withdrawal symptoms on quit day. The present study utilized the MNWS total score (α = .84).
Timeline Followback Interview (TLFB)
A modified smoking version of the TLFB (Sobell & Sobell, 1980) was measure used to collect daily smoking behavior. The TLFB has demonstrated good reliability and validity for this purpose (Brown et al., 1998). Outcome analyses focused on early (i.e., first 2 weeks post-quit; Zvolensky, Stewart, Vujanovic, Gavric, & Steeves, 2009) smoking (a) lapse and (b) relapse among those who successfully quit on quit day. Consistent with past work, lapse was defined as smoking any amount following quit day and relapse was defined as smoking at least 5 cigarettes per day on at least three consecutive days following quit day (Shiffman et al., 1996).
Smoking History Questionnaire (SHQ)
The SHQ is a self-report assessment of smoking history (e.g., onset of daily smoking) and pattern (e.g., smoking rate; Brown, Lejuez, Kahler, & Strong, 2002). In the present study, the SHQ was used to describe the sample on smoking history and patterns of use.
Fagerström Test for Nicotine Dependence (FTND)
The FTND is a 6-item assessment of an individual smoker’s tobacco dependence (Heatherton et al., 1991). Total scale scores range from 0–10, with higher scores reflecting high levels of physiological tobacco dependence. The FTND has shown adequate internal consistency (α = .61), good convergent validity with key smoking variables (e.g., saliva cotinine), and high test-retest reliability (Heatherton et al., 1991). In the present study, the FTND total score was used to describe the smoking severity of the sample and included as a covariate in differential and predictive validity analyses (α = .57).
Structured Clinical Interview-Non-Patient Version for DSM-IV (SCID-N/P)
Diagnostic assessments were performed using the SCID-N/P (First, Spitzer, Gibbon, & Williams, 2007). The interviews were administered by trained staff and supervised by independent doctoral-level psychologists. All interviews were audio-taped and the reliability of a random selection of approximately 12.5% of interviews were checked (MJZ) for accuracy; no cases of diagnostic coding disagreement were noted. The SCID was used to describe psychopathology in the sample.
Procedure
Data for the present study was collected during a large, multi-site randomized controlled clinical trial examining the efficacy of two smoking cessation interventions described in detail elsewhere (Schmidt, Raines, Allan, & Zvolensky, 2015). Interested persons responding to community-based advertisements (e.g., flyers, newspaper ads, radio announcements) contacted the research team and were provided with a detailed description of the study via phone. Participants were then screened for initial eligibility, and if eligible, scheduled for an appointment. Eligibility included: (a) being between ages 18–65, (b) reporting smoking eight or more cigarettes per day, and (c) reporting motivation to quit rated as at least 5 or higher on a 10-point scale. After providing written informed consent, participants were interviewed using the SCID-I/NP and completed a computerized self-report assessment battery as well as biochemical verification of smoking status.
The current study is based on secondary analyses of baseline and quit day data for a subset of the sample, which was selected on the basis of complete data for primary variables of interest at baseline. At baseline, 497 cases were retained for analyses (i.e., those who provided complete baseline data for variables in the current study, regardless of parent-study eligibility). The inclusion of participants regardless of eligibility for the larger trial is consistent with past psychometric work conducted in the context of a smoking cessation trial (see Farris et al., 2015). Of the 497 cases, 426 were randomized to treatment; 71 cases did not meet eligibility criteria as outlined above. Of those randomized, 244 provided complete data for the BCS at quit day. All study procedures were approved by the Institutional Review Boards.
Data Analytic Strategy
Analyses were first conducted to examine if those who provided data at quit day and those who did not significantly differed on demographics and study variables at baseline. Next, the factor structure at baseline was examined using structural equation modeling (confirmatory factor analysis; CFA; Brown, 2015). Single factor, three-factor, and higher-order models were analyzed using baseline data (n = 497). Analyses were conducted using Mplus Version 7.1 (Muthén & Muthén, 1998–2012). Considering that the distribution of select BCS items was determined to be outside the range of normal (skewness range [in absolute value]: 0.10–2.08; kurtosis range [in absolutes value]: 0.31–3.49), maximum likelihood robust (MLR) estimation was employed (Muthén & Muthén, 1998–2012). With respect to model fit, several tests were used to evaluate the models. First, the model fit was evaluated using the root mean square error of approximation (RMSEA), with values of less than .08 indicating reasonable fit and values above .10 suggesting poor fit (Browne, Cudeck, Bollen, & Long, 1993). Second, the comparative fit index (CFI; Bentler, 1990) was also used, with values between 0.95 and 1.00 indicating excellent fit and values between .90 and .95 indicating acceptable fit (Hu & Bentler, 1999). Third, the standardized root mean square residual was evaluated, with values less than .08 indicating acceptable fit (Hu et al., 1999). Finally, modifications consistent with empirical work were employed to improve model fit, if necessary (Steenkamp & Baumgartner, 1998). Modified CFA models were evaluated for improved model fit using the Akaike information criterion (AIC), with smaller AIC values indicating better fit (Kline, 2011) and the aforementioned model fit statistics.
Cronbach’s alpha was used to document internal consistency of factor items. Measurement invariance (Meredith, 1993) was then assessed across sex and time with the higher-order factor structure (Chen, Sousa, & West, 2005). Specifically, configural, metric, and scalar invariance were assessed by constraining parameters and comparing nested models. Specifically, Model 1 (configural invariance) assesses for similar factor-indicator patterns across groups. Model 2 (metric invariance at the item level) assesses for consistency in the strength of the association between items and lower-order factors across groups. Model 3 (metric invariance at the lower-order factor level) assesses for consistency in the strength of the association between lower-order factors and the higher-order factor across groups. Model 4 (scalar invariance at the item level) assesses for consistency in item means. Model 5 (scalar invariance at the lower-factor level) assesses for consistency in lower-order, latent means. A non-significant difference in model comparison indicates model invariance for the more constrained model (Anderson & Gerbing, 1988). The Sattora-Bentler scaled X2 difference test was employed to assess differences in model fit (Satorra & Bentler, 2001). Considering the X2 difference tests are susceptible to similar problems as the X2, including sample size dependency (Kline, 2015), additional fit indices were used to evaluate difference in model fit. Specifically, CFI change of less than 0.010 and RMSEA change of less than 0.015 (Chen, 2007) provided statistical evidence for invariance between the less constrained and more constrained model; in instances wherein a discrepancy for invariance was observed across evaluative statistics, CFI change and RMSEA change were considered more accurate tests for model comparison and used as primary indicators of invariance.
Zero-order correlations were computed between the BCS factors and dysphoria, negative affect, social anxiety, smoking outcome expectancies, positive affect, and well-being at baseline to evaluate associations with similar and dissimilar constructs. Alpha values for correlations were adjusted based on the Holm-Bonferroni method (Holm, 1979).
Next, an analysis of covariance (ANCOVA) was conducted to examine differences in the baseline BCS among quitters and non-quitters at quit day after controlling for factors that influence quit success, including gender (Shiffman, Brockwell, Pillitteri, & Gitchell, 2008), tobacco dependence (Zhou et al., 2009), and treatment condition. Only participants who were randomized to treatment were included in these analyses (n = 423); three did not provide complete data for the tobacco dependence measure and were excluded. As with smoking cessation work, an intent-to-treat analytic approach was utilized such that smokers who dropped out prior to quit day were classified as smokers (Hughes & Carpenter, 2005; Lichtenstein & Glasgow, 1992).
Additionally, four hierarchical multiple regressions (Cohen & Cohen, 1983) were conducted to examine BCS total score and subscales assessed at baseline as predictors of withdrawal severity at quit day among successful quitters. Covariate entered at step 1 for all regressions included gender, tobacco dependence, and treatment condition. Additionally, condition was examined as a potential moderator of baseline BCS total score and subscale effects on quit day withdrawal severity.
Finally, mediation analyses were conducted using bootstrapping techniques through PROCESS, a conditional modeling program that tests for both direct and indirect effects (Hayes, 2013). An indirect effect is the product of path from the predictor to the mediator (path a) and path from the mediator to the outcome (path b) and is assumed to be significant if the confidence intervals (CIs) around their product do not include zero (Preacher & Hayes, 2008; Zhao, Lynch, & Chen, 2010). Four models were conducted with lapse as the outcome, baseline negative affectivity (PANAS-NA) as the mediator, and BCS subscales and total score as independent predictors. Four models were conducted with relapse as the outcome, baseline negative affectivity (PANAS-NA) as the mediator, and BCS subscales and total score as independent predictors. Consistent with past work, lapse was defined as smoking any amount in the first 2 weeks following quit day and relapse was defined as smoking at least 5 cigarettes per day on at least three consecutive days in the first 2 weeks following quit day (Shiffman et al., 1996). Conservative confidence intervals (99%) were specified to adjust for Type I error rate inflation (Hayes & Preacher, 2014). Covariates included gender, tobacco dependence, and treatment condition.
Results
Attrition Analyses
Participants who provided complete quit day data for variables of interest (n = 244) and those who did not (n = 253) significantly differed in terms of gender (X2[1] = 5.58, p = .02). Specifically, more women provided quit day data (n = 130) compared to men (n = 114). Participants who did not provide quit day data reported being a regular, daily smoker for significantly fewer years than those who provided quit day data (M = 16.26; SD = 12.45 versus M = 20.79; SD = 13.75; t[494] = −3.85, p < .001). Moreover, participants who did not provide quit day data reported significantly more dysphoric symptoms (M = 20.60; SD = 8.35 versus M = 18.15; SD = 7.46) and negative affectivity (M = 20.04, SD = 7.80 versus M = 18.21; SD = 6.71) than those who provided quit day data (Dysphoria: t[495] = 3.45, p = .001; PANAS-NA: t[495] = 2.80, p = .01). No other differences were observed between participants who provided quit day data and those who did not.
Confirmatory Factor Analysis
First, a one-factor model was examined at baseline. The one-factor model yielded poor model fit statistics (X2[152] = 1111.01, p < .001; RMSEA = .11 [90% CI: .11, .12]; CFI = .71; SRMR = .10). Suggested modifications for correlated residual variances that were conceptually logical were examined. Fit statistics for the one-factor model did not substantively improve after correlating residual variances between items 1 (e.g., ‘No encouragement or help from friends’) and 7 (e.g., ‘No encouragement or help from family members or significant others’), and items 2 (e.g., ‘Having strong feelings such as anger, or feeling upset when you are by yourself) and 8 (e.g., ‘Having strong feelings such as anger, or feeling upset when you are with other people’; (X2[150] = 800.84, p < .001; RMSEA = .09 [90% CI: .09, .10]; CFI = .80; SRMR = .09).
Second, the assumed three-factor model was examined at baseline. The three-factor model yielded marginal fit statistics (X2[132] = 606.61, p < .001; RMSEA = .09 [90% CI: .08, .09]; CFI = .85; SRMR = .09). Modification indices suggested that item 17 (e.g., ‘Seeing things or people which remind you of smoking’) should load onto the Addiction subscale. The inclusion of this item on the Addiction subscale was conceptually logical, and therefore, explored. The modified model produced a lower AIC value relative to the original model (21873.07 and 22038.45, respectively) and demonstrated improved overall model fit (X2[132] = 461.21, p < .001; RMSEA = .07 [90% CI: .06, .08]; CFI = .90; SRMR = .06).
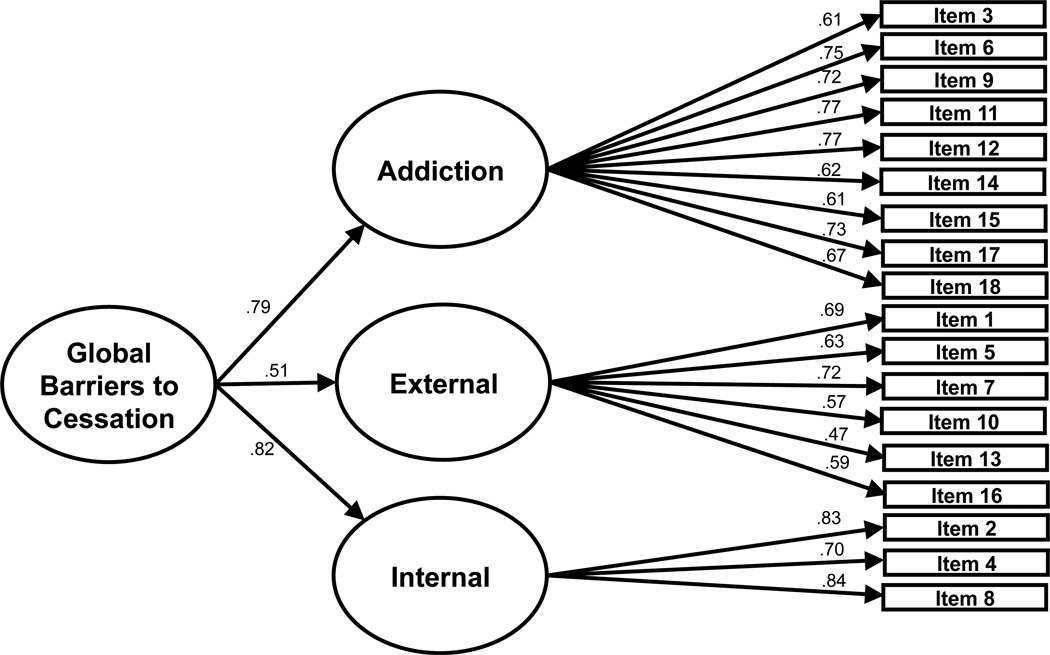
Third, the higher-order structure was examined using the modified factor structure and produced fit statistics identical to the three-factor solution (X2[132] = 461.22, p < .001; RMSEA = .07 [90% CI: .06, .08]; CFI = .90; SRMR = .06). See Figure 1 for final model structure and factor loadings for the higher-order solution. The modified BCS subscales and total score demonstrated good internal consistency at baseline and quit day (α’s: .78 to .90; see Table 1).
Figure 1. Confirmatory factor analysis of higher-order BCS structure at baseline.
Note: Standardized coefficients are presented in the figure. All factor loadings were significant (all p’s < .001).
Table 1.
Internal consistency of the BCS subscales at baseline and quit day
| Variable | Mean (SD) | Cronbach’s Alpha |
|---|---|---|
| Baseline (n = 497) | ||
| BCS Addiction | 15.6 (6.7) | .89 |
| BCS External | 3.7 (3.8) | .78 |
| BCS Internal | 4.4 (2.8) | .83 |
| BCS Total Score | 24.7 (11.2) | .89 |
| Quit Day (n = 244) | ||
| BCS Addiction | 12.9 (6.7) | .90 |
| BCS External | 4.3 (4.6) | .87 |
| BCS Internal | 3.9 (2.7) | .83 |
Note. BCS = Barriers to Cessation Scale (Macnee & Talsma, 1995a).
Test of Measurement Invariance by Sex
Configural invariance was assessed by examining if the same factors and pattern of factor loadings emerged across sex. The higher-order BCS structure demonstrated configural invariance across sex. Next, metric invariance of the items was examined by constraining factor loading for the same items across sex to be equal. The BCS items demonstrated metric invariance across sex. To examine metric invariance of the first order factors, factor loading for the same factors were constrained to be equal across sex. The BCS items demonstrated metric invariance of the first order factors across sex. To examine scalar invariance for items, intercepts for same items were constrained across sex to be equal. The scalar invariance model for items fit was significantly worse than the metric invariance model for first order factors. The modification indices suggested that item 15 (e.g., ‘Fear of failing to quit’) intercept was the largest source of the misfit and should be allowed to vary across sex. After freeing the intercept for item 15, fit indices indicated that the partial scalar invariance model did not fit significantly worse than the metric invariance model for first order factors. Lastly, partial scalar invariance of the first order factors was examined. For this model, first order factor model intercepts were all constrained to be zero, and the intercept for item 15 remained unconstrained. The BCS demonstrated partial scalar invariance of the first order factors across sex. Thus, the higher-order BCS structure demonstrated partial measurement invariance after freeing one of the item intercepts. Table 2 displays findings for measurement invariance models.
Table 2.
Measurement invariance of the BCS across sex.
| Models | χ2 | df | CFI | RMSEA | SRMR | ΔCFI | ΔRMSEA | ΔSBχ2 | Δdf | p |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Configural | 617.53 | 264 | .89 | .07 | .07 | -- | -- | -- | -- | -- |
| 2. Metric: Item Level |
642.07 | 279 | .89 | .07 | .07 | .003 | .001 | 24.51 | 15 | .06 |
| 3. Metris: First Order Level |
645.65 | 281 | .89 | .07 | .07 | .000 | .000 | 3.52 | 2 | .17 |
| 4a. Scalar: Item Level |
699.21 | 296 | .87 | .07 | .07 | .013 | .002 | 55.23 | 15 | <.001 |
| 4b. Partial Scalar: Item Levela |
687.12 | 295 | .88 | .07 | .07 | .009 | .001 | 42.32 | 14 | <.001 |
| 5. Partial Scalar: Second Order Levela |
694.16 | 297 | .88 | .07 | .08 | .002 | .000 | 7.21 | 2 | .03 |
Note. Intercepts for 15 allowed to vary. df = degrees of freedom; CFI = comparative fit index; RMSEA = root mean square error of approximation; SRMR = standardized root-mean-square residual; ΔCFI = change in comparative fit index from previous model; ΔRMSEA = change in root mean square error of approximation from previous model; ΔSBχ2 = change in Sattora-Bentler scaled X2 from previous model; Δdf = change in degrees of freedom from previous model.
Test of Measurement Invariance Over time
Configural invariance was assessed by examining if the same factors and pattern of factor loadings emerged over time. The higher-order BCS structure demonstrated configural invariance over time. Next, metric invariance of the items was examined by constraining factor loading for the same items across time points to be equal. The higher-order BCS structure demonstrated metric invariance at the item level. To examine metric invariance of the first order factors, factor loading for the same factors were constrained to be equal across time. The BCS demonstrated metric invariance of the first order factors over time. To examine scalar invariance for items, intercepts for same items were constrained across time points to be equal. The BCS items demonstrated scalar invariance of the items across time. Finally, scalar invariance of the first order factors was examined. For this model, first order factor model intercepts were all constrained to be zero over time. The BCS demonstrated scalar invariance of the first order factors across time. Thus, the higher-order BCS structure demonstrated full measurement invariance over time. Table 3 displays findings for measurement invariance models.
Table 3.
Measurement invariance of the BCS from baseline to quit day
| Models | χ2 | df | CFI | RMSEA | SRMR | ΔCFI | ΔRMSEA | ΔSBχ2 | Δdf | p |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Configural | 1281.14 | 569 | .88 | .05 | .08 | -- | -- | -- | -- | -- |
| 2. Metric: Item Level |
1296.66 | 584 | .88 | .05 | .08 | .000 | .000 | 14.43 | 15 | .49 |
| 3. Metric: First Order Level |
1301.42 | 586 | .88 | .05 | .08 | .000 | .000 | 4.95 | 2 | .08 |
| 4. Scalar: Item Level |
1341.69 | 601 | .88 | .05 | .08 | .005 | .000 | 40.79 | 15 | <.001 |
| 5. Scalar: First Order Level |
1364.60 | 603 | .87 | .05 | .08 | .003 | .000 | 61.06 | 2 | <.001 |
Note. df = degrees of freedom; CFI = comparative fit index; RMSEA = root mean square error of approximation; SRMR = standardized root-mean-square residual; ΔCFI = change in comparative fit index from previous model; ΔRMSEA = change in root mean square error of approximation from previous model; ΔSBχ2 = change in Sattora-Bentler scaled X2 from previous model; Δdf = change in degrees of freedom from previous model.
Associations among the BCS and affective and smoking processes
Table 4 displays the associations among BCS subscales and total score with dysphoria, negative affect, social anxiety, smoking outcome expectancies, positive affect, and well-being at baseline. Associations were all in the expected directions. The Addiction subscale was significantly correlated with dysphoria, social anxiety, both positive and negative affect, and all SCQ subscales. Observed effect sizes ranged from small to large ([absolute value] r’s = 0.14 to 0.50). The External subscale was significantly correlated with dysphoria, negative affect, social anxiety, and the positive and negative reinforcement SCQ subscales. Observed effect sizes were small (r’s = 0.18 to 0.21). The Internal subscale was significantly correlated with dysphoria, social anxiety, both positive and negative affect, all SCQ subscales, and well-being. Observed effect sizes ranged from small to large ([absolute value] r’s = 0.22 to 0.57). The BCS total score was significantly correlated with dysphoria, social anxiety, both positive and negative affect, all SCQ subscales, and well-being. Observed effect sizes ranged from small to large ([absolute value] r’s = 0.16 to 0.51).
Table 4.
Associations among BCS subscales and affective and smoking processes at baseline
| Variable | Mean (SD) | Range | BCS Addiction |
BCS External |
BCS Internal |
BCS Total Score |
|---|---|---|---|---|---|---|
| Related Constructs | ||||||
| Dysphoria | 19.40 (8.01) | 10–46 | 0.34*a | 0.19*a | 0.46*a | 0.40*a |
| PANAS-NA | 19.15 (7.33) | 10–48 | 0.29*a | 0.21*a | 0.48*a | 0.38*a |
| Social Anxiety | 8.06 (3.74) | 5–25 | 0.23*a | 0.18*a | 0.31*a | 0.29*a |
| SCQ-NC | 6.53 (1.30) | 0–9 | 0.40*a | 0.08 | 0.29*a | 0.37*a |
| SCQ-PR | 5.66 (1.54) | 0–9 | 0.50*a | 0.20*a | 0.30*a | 0.45*a |
| SCQ-NR | 5.64 (1.83) | 0–9 | 0.48*a | 0.19*a | 0.57*a | 0.51*a |
| SCQ-Appetite | 4.12 (2.38) | 0–9 | 0.24*a | 0.10 | 0.24*a | 0.29*a |
| Divergent Constructs | ||||||
| PANAS-PA | 32.29 (7.23) | 11–50 | −0.14*b | −0.07 | −0.22*a | −0.17*a |
| Well-Being | 22.68 (6.93) | 8–40 | −0.10 | −0.06 | −0.27*a | −0.16*a |
Note. p < .001 and Holm-Bonferroni corrected significance range from p = .001−.007
p = .002 and Holm-Bonferroni corrected significance p = .008. BCS = Barriers to Cessation Scale (Macnee & Talsma, 1995a); Dysphoria = Inventory of Depression and Anxiety Symptoms Dysphoria Subscale (Watson et al., 2007); PANAS-NA= Positive and Negative Affect Schedule-Negative Affect (Watson et al., 1988); Social Anxiety = Inventory of Depression and Anxiety Symptoms Social Anxiety Subscale (Watson et al., 2007); SCQ = Smoking Consequences Questionnaire (Brandon et al., 1991); PANAS-PA= Positive and Negative Affect Schedule-Positive Affect (Watson et al., 1988); Well-Being = Inventory of Depression and Anxiety Symptoms Well-Being Subscale (Watson et al., 2007).
Mean differences in BCS across quitters and non-quitters
Four separate ANCOVAs were performed to compare smokers who quit (n = 91) and did not quit on quit day (n = 335) on the BCS total score and subscales, controlling for gender, tobacco dependence (e.g., FTND total), and condition assignment. Quitters and non-quitters did not differ on their baseline BCS total score or any BCS subscales.
Predictive validity
Baseline BCS Addiction, Internal and total score emerged as significant predictors of quit day withdrawal severity among quitters after controlling for gender, FTND total, and condition. Indeed, Step 2, wherein the BCS construct was entered, accounted for greater statistical variance relative to Step 1 wherein only covariates were entered across these three models. See Table 5. Regarding tests of condition assignment as a moderator, condition significantly moderated the relation between baseline External subscale and quit day withdrawal severity (F(70,1) = 5.77, ΔR2 = .07, p = .02), such that perceived external barriers to cessation was unrelated to withdrawal severity at quit week among those in the treatment condition, but positively related to withdrawal severity at quit week among smokers in the active condition. Condition did not moderate the association between baseline Addiction, Internal and total score and quit day withdrawal severity (p’s > .05).
Table 5.
Hierarchical regression analyses predicting withdrawal severity among quitters from BC Addiction, External, Internal and Total Score while controlling for covariates.
| Step | Predictor | B | SE | t | β | Adj R2 | F |
|---|---|---|---|---|---|---|---|
| Step 1: Covariates |
Gender | 1.82 | 1.13 | 1.61 | 0.19 | 0.00 | 0.38 |
| FTND | −0.06 | 0.25 | −0.23 | −0.03 | |||
| Condition | 0.87 | 1.10 | 0.79 | 0.09 | |||
| Step 2: Covariates and BCS-Addiction |
Gender | 1.24 | 1.09 | 1.14 | 0.13 | 0.10 | 2.97* |
| FTND | −0.22 | 0.25 | −0.89 | −0.10 | |||
| Treatment | 1.01 | 1.05 | 0.97 | 0.11 | |||
| BCS-Addiction | 0.25 | 0.09 | 2.91 | 0.33** | |||
| Step 2: Covariates and BCS-External |
Gender | 1.85 | 1.12 | 1.65 | 0.19 | 0.02 | 1.38 |
| FTND | −0.09 | 0.25 | −0.34 | −0.04 | |||
| Condition | 1.23 | 1.12 | 1.10 | 0.13 | |||
| BCS-External | 0.22 | 0.14 | 1.54 | 0.18 | |||
| Step 2: Covariates and BCS-Internal |
Gender | 0.66 | 1.10 | 0.61 | 0.07 | 0.14 | 4.09** |
| FTND | −0.22 | 0.24 | −0.93 | −0.10 | |||
| Condition | 0.85 | 1.02 | 0.83 | 0.09 | |||
| BCS-Internal | 0.68 | 0.19 | 3.57 | 0.41*** | |||
| Step 2: Covariates and BCS-Total |
Gender | 0.97 | 1.08 | 0.91 | 0.10 | 0.14 | 4.08** |
| FTND | −0.26 | 0.24 | −1.07 | −0.12 | |||
| Condition | 1.29 | 1.03 | 1.26 | 0.14 | |||
| BCS-Total | 0.18 | 0.05 | 3.56 | 0.41*** | |||
Note. N = 76
p < .001
p < .01
p < .05.
Step 1 is only presented once because it is the same for all models. A total of 14 participants provided carbon monoxide (CO) on quit day, but did not provide any self-report data on quit day. One person was excluded due to missing data on the Fagerström Test for Nicotine Dependence at baseline. BCS= Barriers to Cessation Scale (Macnee & Talsma, 1995a); FTND = Fagerström Test for Nicotine Dependence (Heatherton et al., 1991).
The independent indirect effects of the Addiction subscale and total score on lapse through PANAS-NA were significant (Addiction: ab = .004, SE = .02, CI99% = .006, .131; total score: ab = .035, SE = .02, CI99% = .001, .088). The Internal subscale had a significant indirect effect on lapse when CIs were relaxed to 95% (ab = .182, SE = .09, CI95% = .032, .373), but not at the 99% CIs level (ab = .182, SE = .09, CI95% = −.007, .473). All independent indirect effects models for relapse were non-significant. The Addiction subscale had a significant indirect effect on relapse when CIs were relaxed to 95% (ab = .034, SE = .02, CI95% = .006, .072).
Discussion
The current study examined the BCS factor structure, measurement invariance of the BCS subscales across sex and over two time points, and evaluated construct validity by investigating associations among BCS subscales and affective and smoking processes proposed to be related to and distinct from BCS subscales. Results indicated that the BCS is a reliable measure of perceived barriers to smoking cessation. Extending prior work, the BCS was best modeled by a higher-order factor structure and demonstrated properties of measurement invariance across sex and from baseline to quit day among treatment seeking smokers. Additionally, the BCS subscales and total score related in the expected directions with similar and divergent constructs. Finally, predictive validity for the BCS subscales and total score was partially supported.
The majority of work with the BCS has utilized a total score summary statistic (Johnson et al., 2012; Macnee & Talsma, 1995a). The current findings provide empirical support for the use of the BCS total score as well as the subscales. Regarding the total score, while the one-factor model resulted in an overall poor factor solution for the BCS, the higher-order factor structure provided a parsimonious, well-fitting measurement model that explained unique covariance between items and subscales. The first-order structure was slightly modified based on findings from the three-factor comparison model and prior research (Albanese et al., 2016). Specifically, the current three-factor model deviated slightly from the original model (Macnee & Talsma, 1995a), such that item 17 (“Seeing things or people which remind you of smoking”) loaded poorly on the External subscale and was better accounted for by the Addiction subscale. This change in model structure was included when evaluating the higher-order structure. As expected, when comparing a three-factor model with correlated factors and a higher-order model that explains the covariance between three lower-order factors, fit indices were identical for these models. Considering that the higher-order model explains covariance between factors and the three-factor solution does not (Reise et al., 2010), this higher-order factor solution offers a more parsimonious measurement model to explain covariance between BCS items and subscale. Together, the present findings support the use of both individual BCS subscales as well as a global total score. The indicators for two of the first-order factors, however, differ slightly from prior work and warrant further independent replication. Additionally, the higher-order model evinced acceptable fit at baseline and the total score, as well as subscales, demonstrated excellent internal reliability at both baseline and quit week, providing further support for the reliability of the total score and subscales.
The higher-order model demonstrated partial measurement invariance across sex and full measurement invariance between baseline and quit day. Indeed, configural, metric, and partial scalar invariance was observed at the item and first order level across sex, and full configural, metric, and scalar was observed at the item and first order level over time. These findings suggest that (a) the BCS is similar at the item and first order structure across sex and over time (e.g., the same factor-indicator pattern); (b) the strengths of the relations between each indicator and its associated factor as well as each first order factor and a global factor is equal over time (e.g., the factor loading for each item did not significantly differ across time); and (c) item and first order factor means are equivalent across sex and over time (e.g., the item intercepts did not differ), with the exception of item 15 across sex.
Although full scalar invariance was not demonstrated across sex, partial scalar invariance was met after un-constraining only one item intercept. This potentially problematic item was observed to have varying intercepts across sex. The identification of this item is a ‘first-step’ toward correcting partial scalar invariance and developing a modified measure that demonstrates full scalar invariance across sex. Despite this limitation, the BCS presently demonstrates partial measurement invariance that supports meaningful interpretations of latent means. Indeed, extant work suggests that valid inferences regarding construct means can be made if there are at least two indicators with equal factor loading and intercepts across groups or over time (Byrne, Shavelson, & Muthén, 1989). Thus, the present work provides initial evidence that differences across sex as well as over time of the BCS result from substantive differences in the trait rather than an artifact of measurement bias. Together, the BCS total score and subscales demonstrated properties that suggest it is a valid measure with factor stability across sex and over time.
Beyond the factor structure, observed associations between the BCS subscales and total score and affective and smoking processes as well as predictive associations provide construct validity for the BCS. Each BCS subscale and the total score positively correlated with constructs that reliably interfere with smoking cessation (Buckner et al., 2015; Carmody, Vieten, & Astin, 2007; Copeland et al., 1995; Leventhal et al., 2013). Additionally, all BCS subscales and the total score were negatively associated with or unrelated to constructs that may promote smoking cessation success (Bränström, Penilla, Pérez-Stable, & Muñoz, 2010; Day, Clerkin, Spillane, & Kahler, 2014). Observed relations among the Addiction Internal subscales and total score were identical across measures examined to support convergent and discriminant validity; yet, the magnitude of these associations varied across these three measures of perceived barriers. Thus, although these two subscales and a global barrier to cessation factor may relate to similar constructs, the strength of their associations identifies the unique contribution of each. Moreover, slightly different observations were observed regarding the External measure, providing evidence for the uniqueness of this subscale. Notably, the External subscale captures perceived barriers to cessation pertaining to lack of relationship support. Thus, conceptual content supports the observed association between this subscale and internal, negatively-valenced risk processes (e.g., dysphoric mood, perceived smoking consequences), as well as the lack of association between this subscale and internally-focused, positively-valenced protective processes (e.g., positive affect). Together, findings support that affective (e.g., dysphoric mood) and cognitive (e.g., smoking consequences) smoking processes are related to each subscale of the BCS.
Unlike prior work (Albanese et al., 2016; Macnee & Talsma, 1995a), the BCS did not differentiate quitters from non-quitters. Indeed, quitters and non-quitters at quit day reported similar baseline scores across the BCS total score and its subscales, after controlling for gender, baseline tobacco dependence, and condition. Thus, although post-treatment BCS assessment relates to quit behavior after smoking cessation treatment (Albanese et al., 2016; Macnee & Talsma, 1995a), the current findings did not support a relation between pre-treatment, or baseline, assessment and abstinence at quit day. Future work might, however, consider evaluating the relation between BCS and quit patterns, such as time to lapse or relapse.
Despite the non-significant association between BCS and abstinence, the positive relation between the BCS Addiction, Internal, and total score and withdrawal severity at quit week as well as the indirect effect of BCS Addiction and total score on lapse through negative affectivity provides further evidence for construct validity and the clinical utility of the perceived barriers for cessation construct. Indeed, these novel findings provide empirical evidence for (a) a relation between perceived barriers at pre-treatment and withdrawal severity at quit day and (b) a pathway through which BCS Addiction and total score relate to lapse among successful quitters. Given the robust association between drug use to avoid or escape negative mood or affective states, such as withdrawal symptoms, and cessation (see Baker, Piper, McCarthy, Majeskie, & Fiore, 2004), elucidating pre-treatment predictors of withdrawal severity provides important information that has the potential to impact treatment development. Consistent with this theoretical model, identifying pre-treatment predictors, such as BCS dimensions, that directly or indirectly relate to early quit failure may help clinicians identify treatment-seeking smokers at greater risk for lapse or relapse.
Clinically, the psychometric properties demonstrated by the BCS suggest that it may be advisable for clinicians to continue to administer the BCS as a way to inform treatment and track perceived barriers to cessation, particularly for smokers interested in or attempting to quit. Given that the BCS taps into multiple domains of perceived barriers for cessation, clinicians may be able to isolate particular areas in which barriers may most interfere with quitting. This approach would allow for a more individualized treatment plan that may promote greater quit success. Further, the present results suggest that difference in BCS subscale latent means across time is attributable to changes in the construct. Thus, the BCS appears to be a suitable measure to document changes in perceived barriers over time.
There are a number of study limitations. First, the sample was largely comprised of a relatively homogenous group of treatment-seeking smokers, and therefore, it will be important for future studies to recruit a more ethnically/racially diverse sample of smokers. Second, the sample included treatment-seeking smokers. Thus, the current findings cannot be extrapolated to all smokers. Future work may consider replicating the present study with a sample of smokers from the general population not presently interested in quitting. Third, although guided by prior work and content evaluation (Albanese et al., 2016; Steenkamp & Baumgartner, 1998), modification indices were utilized to assist with improving model fit and demonstrating measurement invariance. Considering that the data was modified and then re-analyzed, there is an increased likelihood of sampling error. To combat this limitation, future research should examine the overall fit indices for the suggested modified models in an independent sample of smokers. Fourth, although most of the fit statistics used to evaluate measurement invariance of the BCS demonstrated acceptable fit, the CFI was consistently outside the range of acceptable scores. In light of the clinical utility of the BCS and controversy surrounding following suggested ‘rules of thumb’ too stringently (Hopper, Coughlan, Mullen, et al., 2008), we opted to continue with the analyses. For the limitations cited above and the current limitation, it would prove fruitful for further work to examine measurement invariance of the BCS across sex and over time in an independent sample of smokers. Finally, although the rate of attrition observed in the current study is not atypical of smoking cessation trials (see Belita & Sidani, 2015), observed differences between participants who provided quit day data and those who did not may have influenced the relative generalizability of findings. Therefore, the current findings warrant future replication in an independent sample of smokers interested in cessation.
Overall, the present study provides additional support for a global higher-order factor and lower-order constituent factors structure of the BCS. Additionally, current findings highlight the BCS as a theoretically relevant smoking construct that is associated with, and potentially impacts, smoking behavior as well as processes that may interfere with quitting or promote more problematic use. In light of the current findings and extant work, it is advisable for future work utilizing this measure to assign item 17 to the Addiction subscale instead of the External subscale. Additionally, the present study provides further support for the continued use of a global assessment of BCS as captured by a total score. Consistent with these recommendations, the current study extends prior research on the psychometric properties of the BCS by establishing partial measurement invariance across sex and full measurement invariance across time for the higher-order factor structure, in addition to evaluating associations among the BCS modified subscales and total score and cognitive processes that may interfere with smoking cessation. Together, the BCS evinced properties that suggest it is a stable construct that assesses perceived barriers to cessation across multiple domains and is related to several affective and smoking processes the may interfere with cessation.
REFERENCES
- Centers for Disease Control & Prevention (CDC) How tobacco smoke causes disease: The biology and behavioral basis for smoking-attributable disease: A report of the surgeon general. 2010 Centers for Disease Control and Prevention (US) [PubMed] [Google Scholar]
- Albanese BJ, Allan NP, Boffa JW, Chavarria J, Raines AM, Zvolensky MJ, et al. Suicidality prospectively predicts greater urges to smoke following a cessation attempt: Mediation through perceived barriers to cessation. Journal of Affective Disorders. 2016;190:221–226. doi: 10.1016/j.jad.2015.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin. 1988;103(3):411. [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychological review. 2004;111(1):33. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Belita E, Sidani S. Attrition in smoking cessation intervention studies: A systematic review. Canadian Journal of Nursing Research. 2015;47(4):21–40. doi: 10.1177/084456211504700402. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological bulletin. 1990;107(2):238. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Brandon TH, Baker TB. The Smoking Consequences Questionnaire: The subjective expected utility of smoking in college students. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3(3):484–491. [Google Scholar]
- Bränström R, Penilla C, Pérez-Stable EJ, Muñoz RF. Positive affect and mood management in successful smoking cessation. American Journal of Health Behavior. 2010;34(5):553–562. [PubMed] [Google Scholar]
- Brown RA, Burgess ES, Sales SD, Whiteley JA, Evans DM, Miller IW. Reliability and validity of a smoking timeline follow-back interview. Psychology of Addictive Behaviors. 1998;12(2):101–112. [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology. 2002;111(1):180–185. [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research: Guilford Publications. 2015 [Google Scholar]
- Browne MW, Cudeck R, Bollen KA, Long JS. Alternative ways of assessing model fit. Sage Focus Editions. 1993;154:136–136. [Google Scholar]
- Buckner JD, Farris SG, Zvolensky MJ, Shah SM, Leventhal AM, Minnix JA, et al. Dysphoria and smoking among treatment seeking smokers: the role of smoking-related inflexibility/avoidance. American Journal Of Drug & Alcohol Abuse. 2015;41(1):45–51. doi: 10.3109/00952990.2014.927472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Zvolensky MJ, Jeffries ER, Schmidt NB. Robust impact of social anxiety in relation to coping motives and expectancies, barriers to quitting, and cessation-related problems. Experimental and clinical psychopharmacology. 2014;22(4):341. doi: 10.1037/a0037206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne BM, Shavelson RJ, Muthén B. Testing for the equivalence of factor covariance and mean structures: The issue of partial measurement invariance. Psychological bulletin. 1989;105(3):456. [Google Scholar]
- Carmody TP, Vieten C, Astin JA. Negative affect, emotional acceptance, and smoking cessation. Journal of Psychoactive Drugs. 2007;39(4):499–508. doi: 10.1080/02791072.2007.10399889. [DOI] [PubMed] [Google Scholar]
- Chen FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Structural equation modeling. 2007;14(3):464–504. [Google Scholar]
- Chen FF, Sousa KH, West SG. Teacher’s corner: Testing measurement invariance of second-order factor models. Structural equation modeling. 2005;12(3):471–492. [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression for the behavioral sciences. 2nd. Mahwah, New Jersey: Lawrence Erlbaum Associates, Inc; 1983. [Google Scholar]
- Copeland AL, Brandon TH, Quinn EP. The Smoking Consequences Questionnaire-Adult: Measurement of smoking outcome expectancies of experienced smokers. Psychological Assessment. 1995;7(4):484–494. [Google Scholar]
- Costello A, Osborne J. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Practical Assessment, Research & Evaluation. 2011;10:7. [Google Scholar]
- Day AM, Clerkin EM, Spillane NS, Kahler CW. Adapting positive psychology for smoking cessation. In: Parks AC, Schueller SM, editors. The Wiley Blackwell handbook of positive psychological interventions. Wiley-Blackwell: 2014. pp. 358–370. [Google Scholar]
- El-Shahawy O, Haddad L. correlation between nicotine dependence and barriers to cessation between exclusive cigarette smokers and dual (water pipe) smokers among Arab Americans. Substance abuse and rehabilitation. 2015;6:25. doi: 10.2147/SAR.S72360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farris S, Langdon K, DiBello A, Zvolensky M. Why Do anxiety sensitive smokers perceive quitting as difficult? The role of expecting “interoceptive threat” during acute abstinence. Cognitive Therapy and Research. 2015;39(2):236–244. [Google Scholar]
- Farris SG, DiBello AM, Allan NP, Hogan J, Schmidt NB, Zvolensky MJ. Evaluation of the Anxiety Sensitivity Index-3 among treatment-seeking smokers. Psychological Assessment. 2015;27(3):1123–1128. doi: 10.1037/pas0000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz N, Curry SJ. Treating tobacco use and dependence: 2008 update U.S. Public Health Service Clinical Practice Guideline executive summary. Respir Care. 2008;53(9):1217–1222. [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-TR Axis I disorders, research version, non-patient edition (SCIDI/NP) New York, NY: Biometrics Research, New York State Psychiatric Institute; 2007. [Google Scholar]
- Foster DW, Zvolensky MJ, Garey L, Ditre JW, Schmidt NB. Relationships between drinking motives and smoking expectancies among daily smokers who are also problem drinkers. Journal of dual diagnosis. 2014;10(3):118–129. doi: 10.1080/15504263.2014.926759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregor KL, Zvolensky MJ, McLeish AC, Bernstein A, Morissette S. Anxiety sensitivity and perceived control over anxiety-related events: associations with smoking outcome expectancies and perceived cessation barriers among daily smokers. Nicotine & Tobacco Research. 2008;10(4):627–635. doi: 10.1080/14622200801978706. [DOI] [PubMed] [Google Scholar]
- Haddad LG, Petro-Nustas W. Predictors of intention to quit smoking among Jordanian university students. Canadian Journal of Public Health/Revue Canadienne de Sante’e Publique. 2006:9–13. doi: 10.1007/BF03405204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. Methodology in the social sciences. New York, NY: The Guilford Press; 2013. [Google Scholar]
- Hayes AF, Preacher KJ. Statistical mediation analysis with a multicategorical independent variable. British Journal of Mathematical and Statistical Psychology. 2014;67(3):451–470. doi: 10.1111/bmsp.12028. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction to Alcohol and Other Drugs. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Holm S. A simple sequentially rejective multiple test procedure. Scandinavian journal of statistics. 1979:65–70. [Google Scholar]
- Horn JL, McArdle JJ. A practical and theoretical guide to measurement invariance in aging research. Experimental aging research. 1992;18(3):117–144. doi: 10.1080/03610739208253916. [DOI] [PubMed] [Google Scholar]
- Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: a multidisciplinary journal. 1999;6(1):1–55. [Google Scholar]
- Hughes JR, Carpenter MJ. The feasibility of smoking reduction: an update. Addiction. 2005;100(8):1074–1089. doi: 10.1111/j.1360-0443.2005.01174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Archives of General Psychiatry. 1986;43(3):289–294. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- Johnson KA, Farris SG, Schmidt NB, Zvolensky MJ. Anxiety sensitivity and cognitive-based smoking processes: Testing the mediating role of emotion dysregulation among treatment-seeking daily smokers. Journal of addictive diseases. 2012;31(2):143–157. doi: 10.1080/10550887.2012.665695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassel JD, Stroud LR, Paronis CA. Smoking, stress, and negative affect: correlation, causation, and context across stages of smoking. Psychol Bull. 2003;129(2):270–304. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles And Practice Of Structural Equation Modeling. 3rd. New York: Guilford; 2011. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. Guilford publications: 2015. [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer Pub. Co; 1984. [Google Scholar]
- Leventhal AM, Greenberg JB, Trujillo MA, Ameringer KJ, Lisha NE, Pang RD, et al. Positive and negative affect as predictors of urge to smoke: Temporal factors and mediational pathways. Psychology of Addictive Behaviors. 2013;27(1):262–267. doi: 10.1037/a0031579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenstein E, Glasgow RE. Smoking cessation: what have we learned over the past decade? Journal of consulting and clinical psychology. 1992;60(4):518. doi: 10.1037//0022-006x.60.4.518. [DOI] [PubMed] [Google Scholar]
- Little TD, Preacher KJ, Selig JP, Card NA. New developments in latent variable panel analyses of longitudinal data. International Journal of Behavioral Development. 2007;31(4):357–365. [Google Scholar]
- Macnee CL, Talsma A. Development and testing of the barriers to cessation scale. Nurs Res. 1995a;44(4):214–219. [PubMed] [Google Scholar]
- Macnee CL, Talsma A. Predictors of progress in smoking cessation. Public Health Nursing. 1995b;12(4):242–248. doi: 10.1111/j.1525-1446.1995.tb00143.x. [DOI] [PubMed] [Google Scholar]
- Mahaffey BL, Gonzalez A, Farris SG, Zvolensky MJ, Bromet EJ, Luft BJ, et al. Smoking to regulate negative affect: Disentangling the relationship between posttraumatic stress and emotional disorder symptoms, nicotine dependence, and cessation-related problems. Nicotine & Tobacco Research. 2015 doi: 10.1093/ntr/ntv175. [DOI] [PubMed] [Google Scholar]
- McHorney CA, Fleishman JA. Assessing and understanding measurement equivalence in health outcome measures: issues for further quantitative and qualitative inquiry. Medical care. 2006;44(11):S205–S210. doi: 10.1097/01.mlr.0000245451.67862.57. [DOI] [PubMed] [Google Scholar]
- Meredith W. Measurement invariance, factor analysis and factorial invariance. Psychometrika. 1993;58(4):525–543. [Google Scholar]
- Minami H, Yeh VM, Bold KW, Chapman GB, McCarthy DE. Relations among affect, abstinence motivation and confidence, and daily smoking lapse risk. Psychology of Addictive Behaviors. 2014;28(2):376–388. doi: 10.1037/a0034445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore LC, Clark PC, Lee S-Y, Eriksen M, Evans K, Smith CH. Smoking cessation in women at the time of an invasive cardiovascular procedure and 3 months later. Journal of Cardiovascular Nursing. 2013;28(6):524–533. doi: 10.1097/JCN.0b013e31826620d4. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s guide. Seventh. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- Peasley-Miklus CE, McLeish AC, Schmidt NB, Zvolensky MJ. An examination of smoking outcome expectancies, smoking motives and trait worry in a sample of treatment-seeking smokers. Addictive Behaviors. 2012;37(4):407–413. doi: 10.1016/j.addbeh.2011.11.037. doi: http://dx.doi.org/10.1016/j.addbeh.2011.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins KA, Karelitz JL, Jao NC. Optimal carbon monoxide criteria to confirm 24-hr smoking abstinence. Nicotine & Tobacco Research. 2013;15(5):978–982. doi: 10.1093/ntr/nts205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piasecki TM, Niaura R, Shadel WG, Abrams D, Goldstein M, Fiore MC, et al. Smoking withdrawal dynamics in unaided quitters. Journal Of Abnormal Psychology. 2000;109(1):74–86. doi: 10.1037//0021-843x.109.1.74. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Reserch and Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Reise SP, Moore TM, Haviland MG. Bifactor models and rotations: Exploring the extent to which multidimensional data yield univocal scale scores. Journal of personality assessment. 2010;92(6):544–559. doi: 10.1080/00223891.2010.496477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal L, Carroll-Scott A, Earnshaw VA, Sackey N, O’Malley SS, Santilli A, et al. Targeting cessation: Understanding barriers and motivations to quitting among urban adult daily tobacco smokers. Addictive Behaviors. 2013;38(3):1639–1642. doi: 10.1016/j.addbeh.2012.09.016. doi: http://dx.doi.org/10.1016/j.addbeh.2012.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabaté E. Adherence to long-term therapies: evidence for action. World Health Organization: 2003. [Google Scholar]
- Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66(4):507–514. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt NB, Raines AM, Allan NP, Zvolensky MJ. Anxiety sensitivity risk reduction in smokers: A randomized control trial examining effects on panic. Behaviour Research and Therapy. 2015;77:138–146. doi: 10.1016/j.brat.2015.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Brockwell SE, Pillitteri JL, Gitchell JG. Use of smoking-cessation treatments in the United States. American Journal of Preventive Medicine. 2008;34(2):102–111. doi: 10.1016/j.amepre.2007.09.033. doi: http://dx.doi.org/10.1016/j.amepre.2007.09.033. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Gnys M, Richards TJ, Paty JA, Hickcox M, Kassel JD. Temptations to smoke after quitting: a comparison of lapsers and maintainers. Health Psychology. 1996;15(6):455–461. doi: 10.1037//0278-6133.15.6.455. [DOI] [PubMed] [Google Scholar]
- Sobell L, Sobell M. Convergent validity: An approach to increasing confidence in treatment outcome conclusions with alcohol and drug abusers. Evaluating alcohol and drug abuse treatment effectiveness: Recent advances. 1980:177–183. [Google Scholar]
- Steenkamp JBEM, Baumgartner H. Assessing measurement invariance in cross-national consumer research. Journal of consumer research. 1998;25(1):78–107. [Google Scholar]
- Twyman L, Bonevski B, Paul C, Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: a systematic review of the qualitative and quantitative literature. BMJ Open. 2014;4(12):e006414. doi: 10.1136/bmjopen-2014-006414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandenberg RJ, Lance CE. A review and synthesis of the measurement invariance literature: Suggestions, practices, and recommendations for organizational research. Organizational research methods. 2000;3(1):4–70. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Watson D, O’Hara MW, Simms LJ, Kotov R, Chmielewski M, McDade-Montez EA, et al. Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS) Psychological Assessment. 2007;19(3):253–268. doi: 10.1037/1040-3590.19.3.253. (Supplemental) [DOI] [PubMed] [Google Scholar]
- West RJ, Hajek P, Belcher M. Severity of withdrawal symptoms as a predictor of outcome of an attempt to quit smoking. Psychol Med. 1989;19(4):981–985. doi: 10.1017/s0033291700005705. [DOI] [PubMed] [Google Scholar]
- Zhao X, Lynch JG, Chen Q. Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research. 2010;37(2):197–206. [Google Scholar]
- Zhou X, Nonnemaker J, Sherrill B, Gilsenan AW, Coste F, West R. Attempts to quit smoking and relapse: Factors associated with success or failure from the ATTEMPT cohort study. Addictive Behaviors. 2009;34(4):365–373. doi: 10.1016/j.addbeh.2008.11.013. doi: http://dx.doi.org/10.1016/j.addbeh.2008.11.013. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Stewart SH, Vujanovic AA, Gavric D, Steeves D. Anxiety sensitivity and anxiety and depressive symptoms in the prediction of early smoking lapse and relapse during smoking cessation treatment. Nicotine & Tobacco Research. 2009;11(3):323–331. doi: 10.1093/ntr/ntn037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Vujanovic AA, Miller MO, Bernstein A, Yartz AR, Gregor KL, et al. Incremental validity of anxiety sensitivity in terms of motivation to quit, reasons for quitting, and barriers to quitting among community-recruited daily smokers. Nicotine & Tobacco Research. 2007;9(9):965–975. doi: 10.1080/14622200701540812. [DOI] [PubMed] [Google Scholar]