Abstract
Background
Collaborative learning models were designed to support quality improvements, such as innovation implementation by promoting communication within organizational teams. Yet the effect of collaborative learning approaches on organizational team communication during implementation is untested.
Purpose
This study explores change in communication patterns within teams from children’s mental health organizations during a year-long learning collaborative focused on implementing a new treatment. We adopt a social network perspective to examine intra-organizational communication within each team and assess change in: (1) the frequency of communication among team members, (2) communication across organizational hierarchies, and (3) the overall structure of team communication networks.
Methodology/Approach
A pretest posttest design compared communication among 135 participants from 21 organizational teams at the start and end of a learning collaborative. At both time points, participants were asked to list the members of their team, and rate the frequency of communication with each along a 7 point Likert scale. Several individual, pair-wise, and team-level communication network metrics were calculated and compared over time.
Findings
At the individual level, participants reported communicating with more team members by the end of the learning collaborative. Cross-hierarchical communication did not change. At the team-level, these changes manifested differently depending on team size. In large teams, communication frequency increased, and networks grew denser and slightly less centralized. In small teams, communication frequency declined, growing more sparse and centralized.
Practice Implications
Results suggest that team communication patterns change minimally, but evolve differently depending on size. Learning collaboratives may be more helpful for enhancing communication among larger teams, thus managers might consider selecting and sending larger staff teams to learning collaboratives. This study highlights key future research directions that can disentangle the relationship between learning collaboratives and team networks.
Key Terms: Organizational communication, social networks, quality improvement, learning collaboratives
Within healthcare organizations, poor communication can lead to errors, compromise care coordination, and limit service effectiveness (IOM, 2001). As organizations address these quality problems, poor communication especially across levels of the organizational hierarchy, can also constrain organizations’ capacity to design and carry out planned change and quality improvement efforts (Bae, Nikolaev, Seo, & Castner, 2015). Through formal and informal interactions, professionals transfer knowledge, provide social support, and build shared meaning and expectations (Tenkasi & Chesmore, 2003). Thus, strong communication among clinicians, supervisors, and senior leaders is necessary for promoting organizational learning, and quality improvement success (Bae et al 2015; Cunningham et al., 2012).
Large group interventions that promote team work, information sharing, and buy-in for quality improvement and other planned organizational changes have the potential to build robust communication networks (Bae et al., 2015; Chambers, Wilson, Thompson, & Harden, 2012). For instance, collaborative learning models, including the Institute for Healthcare Improvement’s Breakthrough Series Collaborative (IHI, 2003; Kilo, 1998), show promise for creating strong organizational communication networks (Nembhard, 2012). Learning collaborative models are popular quality improvement strategies that facilitate ongoing dialogue and interaction among senior leaders, supervisors, and clinicians. Enhanced organizational communication networks might be one unintended but positive consequence of learning collaboratives. To contribute to the literature on large group interventions that support quality improvement and organizational change in health care, our study explores the utility of learning collaboratives for building strong communication networks within organizational teams.
Theoretical Background - Team Communication Networks and Organizational Change
Drawing from social network theory and approaches, communication ties among organizational members diffuse information, influence, and social support (Valente, 2010). These ties also constitute the network structure, and the assessment of structural features can be used to draw inferences about the strength and flow of communication among team members (Valente, 2010). Dense organizational networks, where professionals are well-connected with one another via frequent and reciprocal social relationships, indicate strong, cohesive, but potentially redundant communication. In contrast, sparse networks have fewer direct communication ties that are infrequent and often unreciprocated. Sparse networks indicate weak and fragmented communication within and across sub-groups within a team. Though weak communication ties can facilitate organizational innovation by connecting individuals to new information and resources beyond their immediate group (e.g. Hansen, 1999), strong and dense communication within an organization is critical for large scale, planned organizational changes—such as quality improvement and innovation implementation initiatives—that are intended to modify group behavior and norms) (Tenkasi and Chesmore, 2003; Ditty, Landes, Doyle, & Beidas, 2015).
Although cohesive social networks can foster groupthink and resistance to change (especially during the early change stages), once organizational members buy into the planned change, strong communication enables successful quality improvement (Garcia, 2007). Frequent and strong communication among team members diffuses information quickly and facilitates knowledge transfer and collective learning as organizational members build shared meaning, expectations, social norms, and accountability (Tenkasi & Chesmore, 2003). This shared commitment and social support promotes integration of new knowledge gained by individuals during quality improvement efforts (Powell, Hausmann-Stabile, & McMillen, 2013), especially when implementing complex tasks (Hansen, 1999) in newly formed groups (Balkundi & Harrison, 2006).
Because quality improvement often requires administrative, supervisory, and practice-level changes, strong reciprocal communication that is decentralized and flows across hierarchical units is also important for diffusing information, conveying clear expectations for change, and identifying and addressing administrative barriers (Mohrman, Tenkasi & Mohrman, 2003). However, research on social networks within healthcare settings suggests that most networks and communication patterns are hierarchical (Bae et al., 2015; Cott, 1997), in which communication occurs within, rather than across levels (Creswick, Westbrook, & Braithwaite, 2009). Additionally, highly centralized networks, where communication ties are clustered around one or few team members, reflect hierarchy, power, and control over information and learning (Valente, 2010). As a result, centralized communication can hinder shared understanding and interactions that engage staff across levels, thus impeding quality improvement (Mohrman, Tenkasi, & Mohrman, 2003) and performance (Sparrowe et al. 2001).
Communication Network-Building Interventions - Learning Collaboratives
Building densely connected and decentralized communication networks that bridge hierarchies could facilitate quality improvement efforts that depend on coordination among organizational administrators, supervisors, and clinicians. Prior research in the broader organizational development and workforce management literatures suggest that group interventions emphasizing collaborative planning and implementation of change can build communication ties among organizational members (Clarke, 2005). These types of interventions build communication ties among organizational members by facilitating information sharing, commitment, and buy-in for the planned change (Garcia, 2007).
Made popular by the Institute for Healthcare Improvement’s (IHI) Breakthrough Series, learning collaboratives are one such group intervention used worldwide to improve care quality in a variety of healthcare contexts (Nadeem et al., 2013; IHI, 2003). Within behavioral health, learning collaboratives have been used to integrate depression treatment into primary care settings (e.g. Katzelnick, et al, 2005), improve mental health service engagement among low income youth (e.g. Caveleri et al, 2006), and disseminate and implement trauma-focused care for children (e.g. Ebert, Amaya-Jackson, Markiewicz, Kisiel, & Fairbank, 2012).
Although evidence supporting their effectiveness for improving quality and implementation success is mixed (Nadeem, Olin, Hill, Hoagwood, & Horwitz, 2014; Schouten, Hulscher, van Everdingen, Huijsman, & Grol, 2008), learning collaboratives may promote knowledge sharing and social support within organizational teams. Specific learning collaborative components and structure often vary across setting and purpose, however most incorporate a core set of activities (Nadeem et al, 2013) that target participants’ skills, attitudes, and perceptions, and foster a shared understanding of interdependence. Over 8 to12 months, teams from multiple units or organizations engage in a structured series of intensive and collaborative learning, planning, and application activities intended to promote learning within and across organizational teams. Organizational teams participate in two to three in-person learning sessions with didactic training provided by faculty leaders. In between the learning sessions, teams return to their home organization to complete plan-do-study-act (PDSA) cycles where teams conduct and assess small tests of change, and collect data to track the team’s progress. Throughout the process, teams are supported by the learning collaborative faculty leaders who facilitate monthly conference calls and provide coaching.
These activities provide structure for team members to interact with one another. In fact, prior evidence suggests that advice-sharing and communication patterns change over the duration of learning collaboratives (Bunger, Hanson, Doogan, Powell, Cao, & Dunn, 2016) and other types of organizational quality improvement initiatives (Rangachari et al., 2014, 2015). The learning sessions, PDSA cycles, regular group calls, and consultation activities bring team members together and promote communication with one another about quality improvement and organizational learning (Nembhard 2009; 2012). As a result, team members might build new ties with their colleagues, and communicate more frequently with one another across the organizational hierarchy.
Study Purpose
Although the importance of communication for organizational change and quality improvement success is well established, little is known about strategies and interventions for developing robust communication networks within organizations where communication flows frequently and reciprocally across hierarchical levels (Bae et al, 2015; Chambers, Wilson, Thompson, & Harden, 2012). Given the emphasis on shared learning and structured opportunities for intensive team collaboration around planning and implementation, we posit that learning collaboratives have potential for strengthening team communication networks in several ways, but to date, this relationship has not been tested (Nadeem et al., 2014; Schouten et al., 2008).
The present study explores change in communication patterns within organizational teams participating in a learning collaborative focused on implementing a treatment innovation (one type of planned organizational change to improve care quality). Using a social network approach, we describe changes in team communication patterns at multiple levels and address three aims. First, at the individual level, participants might build new ties with team members and communicate with them more frequently than before the learning collaborative began. Therefore, we assess changes in the number of ties and frequency of communication among team members over the course of the learning collaborative (Aim 1). Second, within each organizational team, opportunities for intensive interaction throughout the learning collaborative may lead to new or stronger communication ties across the hierarchy. Thus, we examine change in communication across hierarchical levels in each team, focusing on pair-wise communication ties across clinicians, supervisors, and senior leaders (Aim 2). Third, these subtle changes may result in a shift in the structure of the overall communication network, creating more densely connected networks, with strong communication ties that are less centralized around a few key members. Therefore, we describe changes in the overall structure of team communication networks by assessing measures of connectedness, strength, and centralization (Aim 3).
Methods
Study Context
This community-based study examines change in communication patterns within teams from children’s mental health organizations who participated in a year long learning collaborative focused on implementing trauma-focused cognitive behavioral therapy (TF-CBT). TF-CBT is a manualized treatment for post-traumatic stress disorder symptoms among children and youth, with strong evidence for its effectiveness (Cary & McMillen, 2012). As part of a naturally occurring regional initiative to expand availability of high quality trauma-informed mental health services, a large Midwestern county government agency contracted with a local university based mental health treatment center to design and lead the learning collaborative. The design was based on the National Center for Child Traumatic Stress (NCCTS) Learning Collaborative model which integrates the core IHI Breakthrough Series Collaborative components with clinical training and coaching (Ebert et al., 2012; Improvement, 2003). The specific components of the learning collaborative have been described and specified in detail elsewhere (Bunger, Hanson, Doogan, Powell, Cao, & Dunn, 2016).
Behavioral health agencies funded by the county government were invited to send formal implementation teams. Consistent with the NCCTS model, agencies had discretion over team membership, but were instructed by the learning collaborative leadership to form teams comprised of three to ten employees including at least one senior leader (a high level leader with administrative authority such as an executive or clinical director), supervisor (who will manage and support clinicians), and clinician (who will deliver TF-CBT directly to children and families). Out of 44 agencies invited, 32 volunteered and selected a total of 206 individuals to attend. To accommodate community interest, four staggered learning collaboratives were conducted beginning in April 2011. By the end of the learning collaboratives in September 2012, 145 individuals (70%) remained. The external research team was invited to observe this initiative – timed to coincide with the learning collaboratives, we overlaid a pretest posttest design to explore change in teams’ communication. Institutional Review Boards at the first author’s former and current institutions approved this study.
Participants and Data Collection
Study participants include 135 individuals (94% of learning collaborative completers) from 21 organizational teams. To be included in the study sample, teams had to have at least three members who completed the learning collaborative, who also provided complete responses to two surveys administered in person during the first and third learning sessions (about nine months later). Because this study focuses on change in team communication over time, our analyses do not include participants who completed the learning collaborative but did not respond to both surveys (n=8) or were from teams with fewer than three participants (n=2). Most participants were clinicians (60%), followed by supervisors (23%), and senior leaders (14%). Unlike traditional medical settings where the term “clinician” may encompass a range of roles and professional backgrounds, clinicians at the frontlines of mental health organizations are a fairly homogenous group, typically comprised of individuals with master’s level training in social work or counseling. Nearly all of the participants had masters’ degrees or higher (98%), in a range of disciplines including social work (42%), addictions (20%), counseling (18%), and psychology (9%). Participants reported extensive field experience (65% reported more than five years of field experience), although nearly 40% were employed by their organization for less than a year at the start of the learning collaborative (Table 1).
Table 1.
Participant Characteristics (n=135)
| n | % | |
|---|---|---|
| Job Role | ||
| Clinician | 82 | 60.74 |
| Supervisor | 32 | 23.70 |
| Senior leader | 19 | 14.07 |
| Missing | 2 | 1.48 |
| Education | ||
| Bachelor’s degree | 3 | 2.22 |
| Master’s degree | 125 | 92.59 |
| Doctoral degree or equivalent | 5 | 3.70 |
| Missing | 2 | 1.48 |
| Discipline* | ||
| Social work | 76 | 43.43 |
| Psychology | 16 | 9.14 |
| Education | 6 | 3.43 |
| Medicine | 3 | 1.71 |
| Admin./mgmt. | 7 | 4.00 |
| Addictions counseling | 35 | 20.00 |
| Counseling | 32 | 18.29 |
| Experience in the field | ||
| Less than 3 years | 25 | 18.52 |
| 3–5 years | 18 | 13.33 |
| More than 5 years | 90 | 66.67 |
| Missing | 2 | 1.48 |
| Experience in current job | ||
| 0–6 months | 25 | 18.52 |
| 6–11 months | 31 | 22.96 |
| 1–3 years | 20 | 14.81 |
| 3–5 years | 18 | 13.33 |
| More than 5 years | 39 | 28.89 |
| Missing | 2 | 1.48 |
Sum is greater than sample size because some participants indicated more than one disciplinary background.
Measures, Metrics, and Analysis
Data on organizational team communication networks were gathered using an ego-network (nomination) approach. Due to the lack of participant information available prior to the start of the study, and turnover over its duration, an ego-centric nomination approach was used at both time points. At both survey time points, respondents (egos) listed each of their implementation team members (alters). For each team member, respondents noted the alter’s position and answered the question: “In the past 6 months, how frequently have you communicated or been in contact with this person via in-person contact, telephone, or email?” using a seven-point Likert scale ranging from “Not once” (1) to “Many times daily” (7). Of those who participated in the survey, 111 provided complete responses to the communication items. Responses were used to calculate and compare several metrics. Although we do not have responses from all learning collaborative completers, we do have their colleagues’ reports about communication with them – therefore we include data about ties with team members (alters) who did not respond to one or both surveys. Because our data represent valued ties (as opposed to binary reports of communication ties), we incorporate weighted metrics when possible. Missing communication frequency values were replaced with the team median, consistent with other team network research (Sparrowe, Liden, Wayne, & Kraimer, 2001).
Individual Communication Frequency
First, to examine change in communication frequency, four individual-level metrics were calculated at both time points. The number of outgoing (out-degree) and incoming communication ties (in-degree) represent the number of team members with whom each participant interacts. Because communication within a relationship could be unbalanced (e.g. A communicates with B more often than B communicates with A), the average communication frequency reported by (weighted out-degree) and with (weighted in-degree) each participant was also calculated. Change over time was examined using paired samples t-tests using Stata 14.
Communication Across Hierarchical Levels
Second, we examined change in communication across hierarchical levels (between clinicians and supervisors, supervisors and senior leaders, etc.) in two ways. First, we compared the E-I index at pretest and posttest for each team. The E-I index is a measure of homophily, or tendency to connect with members of similar social groups, and is calculated as a proportion of within-group to total ties (Krackhardt & Stern, 1988). A positive E-I index indicates heterophily, or the tendency to communicate with colleagues across the hierarchy, whereas a negative E-I index indicates homophily, or the tendency to communicate within colleagues in similar roles. Second, we focused on communication with pairs (dyads). For each team, the number of ties and average communication frequency within several types of dyads were compared: between clinicians, between clinicians and supervisors, between clinicians and senior leaders, between supervisors and senior leaders. Average communication frequency is the sum of communication frequency scores per team as a fraction of the total reported number of ties for that team. Given the small number of teams, and skewed distribution of these measures, we used Wilcoxon signed rank tests to test for significance differences using Stata 14.
Team Communication Network Structure
Third, to explore network structural changes, eleven network metrics used for understanding relationship dynamics were calculated for each team (Valente, 2010; Wasserman & Faust, 1994). For each team, two basic features were calculated: the total number of individual members on the agency team (network size), and the total number of ties reported among team members (number of ties within teams). Because examining the net change in ties can mask more nuanced changes, three measures were calculated to assess tie churning (Sasovova, Mehra, Borgatti, & Schippers, 2010): percentage of maintained ties (communication ties observed at both time points), percentage of dissolved ties (ties observed at pretest but not at posttest), and the percentage of new ties (ties observed at posttest but not at pretest). Two measures of overall communication and connectedness were calculated: average team communication frequency, which represents the average communication frequency within each team, and network density, a measure of overall team connectedness, calculated as the percentage of potential pair-wise ties reported by team members. Higher scores reflect denser, more connected networks.
Additionally, we calculated two measures of relationship strength: reciprocity, the percentage of mutual communication ties among team members, and weighted reciprocity, the proportion of communication frequency that was reciprocated, which accounts for the valued ties (Squartini, Picciolo, Ruzzenenti, & Garlaschelli, 2013). Higher reciprocity metrics indicate that a higher proportion of ties and overall amount of communication is reciprocated among team members, suggesting strong communication within the network.
We also assessed two centralization metrics that account for clustering of communication within networks around one or a few team members: in-degree centralization ranges from zero (where team members have an equal number of incoming communication ties) to one (one member receives all incoming communication ties), and weighted in-degree centralization which captures the proportion of communication centralized around members (thus accounts for the communication frequency scores, and the amount of communication each member receives). Higher centralization scores suggest that communication ties, or frequent communication is more clustered around key members, whereas lower scores suggest that communication is diffused among team members. Network metrics were calculated using UCINET vs 6.232 (Borgatti, Everett, & Freeman, 2002). Metrics were averaged across teams and compared over time. However, network metrics are often sensitive to size, complicating comparisons across differently sized teams (Dunn & Westbrook, 2011). Therefore, to detect subtle structural differences based on team size, the teams were divided based on median number of team members (median=5) into small (n=11) and large teams (n=10).
Results
Change in Individual Communication Frequency
Table 2 presents results of a paired samples t-tests comparing participants’ number of ties (in- and out-degree), and communication frequency (weighted in- and out-degree) with their team members at the beginning and end of the learning collaborative. At the start of the learning collaborative, participants’ average out-degree was 4.4 (SD = 1.5) of their team members, and the average frequency of their communication with their team members (weighted out-degree) was 5.1 (SD=1.4) which represents “about once per week” on the response scale. However, participants were the recipients of communication (in-degree) from an average of 5.5 (SD=2.6) team members, and the average frequency of their communication was 5.8 (SD=.09), which represents “about daily” on the response scale.
Table 2.
Participants’ Average Ties and Communication Over Time (n=111)
| Pre | Post | ||||
|---|---|---|---|---|---|
| M | SD | M | SD | T-Test | |
|
| |||||
| Participants’ Reported Communication with Team Members (Out-Going Ties) | |||||
| Out-degree | 4.43 | 1.53 | 5.08 | 2.04 | t(110)=4.01, p=.0001 |
| Weighted Out-degree | 5.14 | 1.36 | 5.18 | 1.15 | t(110)=.41, p=.34 |
| Team Members’ Communication With Participants (In-Coming Ties) | |||||
| In-Degree | 5.54 | 2.574 | 5.39 | 2.31 | t(110)=−.79, p=.43 |
| Weighted In-Degree | 5.75 | 0.09 | 5.73 | 0.09 | t(110)=−.28, p=.61 |
By the end of the learning collaborative, participants’ average out-degree increased to 5.1 (SD=2.0) team members which was significantly higher than at the beginning of the learning collaborative [t(110)=4.01, p<.001], suggesting an increase in number of team members with whom participants communicated. However, there were no significant changes in the number of team members who reported communicating with each participant (in-degree), or communication frequency with team members (weighted out- and in-degree). An increase in out-degree but a static average communication frequency at post-test suggests that individuals communicate as frequently as in the pre-test, but with a greater number of team members.
Change in Communication Across Hierarchical Levels
Table 3 presents results of Wilcoxon signed-rank tests comparing the E-I index and the number and average communication frequency of cross-hierarchical ties, within each team over time. At the beginning of the learning collaborative, teams’ median E-I index was positive (median=.40) suggesting a fair degree of heterophily, or tendency to communicate across hierarchical roles. Ties between clinicians and their supervisors (median=6.5) were the most commonly reported within each team followed by ties among clinicians (median=6.0), clinicians and senior leaders (median=4.0), and supervisors and senior leaders (median=2.0). However, average communication was frequent (about daily) within cross-hierarchical ties, including those between senior leaders and supervisors (median=6.0), and supervisors and clinicians (median=5.8). Communication among clinicians (median=5.1) and between clinicians and senior leaders (median=4.5) was less frequent, occurring about every week or two.
Table 3.
Change in Cross-Hierarchical Ties Within Teams (n=21)
| Pre | Post | Wilcoxon Signed-Rank | |||||
|---|---|---|---|---|---|---|---|
| M | Mdn | SD | M | Mdn | SD | ||
|
| |||||||
| E-I Index | .386 | .400 | .263 | .377 | .364 | .277 | z=1.33, p=.18 |
| Dyads | |||||||
| Clinician <--> Clinician | |||||||
| Ties | 9.09 | 6.00 | 9.54 | 10.21 | 4.50 | 14.22 | z=−.746, p=.46 |
| Communication Freq. | 4.60 | 5.09 | 2.27 | 4.79 | 5.20 | 2.28 | z=1.72, p=.09 |
| Clinician <--> Supervisor | |||||||
| Ties | 7.68 | 6.50 | 5.57 | 6.95 | 5.50 | 5.54 | z=1.26, p=.21 |
| Communication Freq. | 5.33 | 5.75 | 1.47 | 5.37 | 5.70 | 1.02 | z=−.14, p=.89 |
| Clinician <--> Senior Leader | |||||||
| Ties | 4.77 | 4.00 | 4.61 | 3.86 | 2.50 | 4.70 | z=1.91, p=.06 |
| Communication Freq. | 3.84 | 4.50 | 2.45 | 3.66 | 4.50 | 2.32 | z=.34, p=.74 |
| Supervisor <--> Senior Leader | |||||||
| Ties | 2.27 | 2.00 | 2.05 | 1.54 | 1.00 | 1.68 | z=2.75, p=.01 |
| Communication Freq. | 4.54 | 6.00 | 2.81 | 4.10 | 5.50 | 2.84 | z=1.51, p=.13 |
At the end of the learning collaborative, teams’ E-I index, and tendency to communicate across the hierarchy remained somewhat stable and heterophilic (median=.36), suggesting that there was little change in team members’ tendency to communicate with their colleagues across the hierarchy. Teams reported a significant decrease in ties between supervisors and senior leaders (median = 1.0, z = 2.8, p < .01). No significant differences were observed in the number of ties among clinicians, between clinicians and their supervisors, or between clinicians and senior leaders. Nor were there significant differences in communication frequency within the four dyad types, suggesting that participants continued to communicate just as frequently as in the beginning of the learning collaborative.
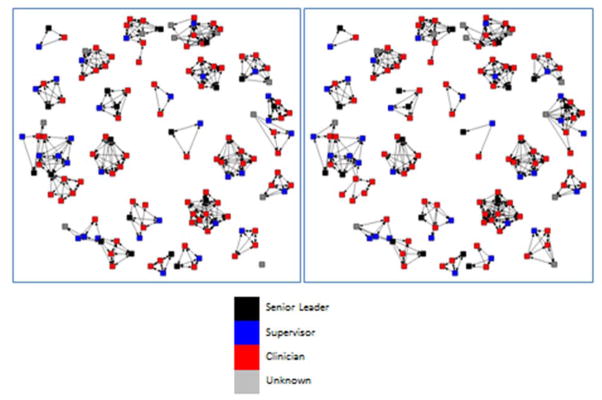
Change in Team Communication Network Structure
Changes in participants’ ties and communication frequency could shift the structure of the network resulting in changes in overall connectedness, strength, and centralization. Table 4 summarizes and compares the structural features of small and large team communication networks at the beginning and end of the learning collaborative, and Figure 1 depicts the structure of the 21 teams at pre and posttest. Across all 21 teams, results suggest that the structural features of the communication networks changed little over the duration of the learning collaborative. However, network structure and change over time appears to vary by team size.
Table 4.
Team Communication Network Characteristics at Baseline and Follow Up [Average (Standard Deviation)]
| Small Teams (n=11) | Large Teams (n=10) | All Teams (n=21) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pretest | Posttest | Change | Pretest | Posttest | Change | Pretest | Posttest | Change | |
|
|
|
|
|||||||
| Basic Team Features | |||||||||
| Size | 4.45 (.69) | 4.36 (.81) | −0.09 | 9.60 (2.12) | 9.60 (2.12) | 0.00 | 6.90 (3.03) | 6.86 (3.09) | −0.04 |
| Number of Ties | 14.36 (5.35) | 11.09 (4.99) | −3.27 | 43.80 (14.40) | 46.30 (19.68) | 2.50 | 28.38 (18.29) | 27.86 (22.61) | −0.52 |
| Tie Churn | |||||||||
| Proportion of Ties Maintained | - | - | .67 | - | - | .658 | - | - | .670 |
| Proportion of Ties Dissolved | - | - | .22 | - | - | .147 | - | - | .182 |
| Proportion of New Ties | - | - | .11 | - | - | .170 | - | - | .143 |
| Overall Connectedness | |||||||||
| Team Communication Frequency | 5.76 (.82) | 5.63 (.83) | −0.13 | 4.75 (1.02) | 4.90 (.93) | 0.15 | 5.28 (1.04) | 5.28 (.94) | 0.00 |
| Density | .91 (.17) | .73 (.16) | −0.18 | .55 (.23) | .59 (.27) | 0.04 | .74 (.27) | .66 (.23) | −0.08 |
| Tie Strength | |||||||||
| Reciprocity | .87 (.26) | .54 (.24) | −0.33 | .69 (.20) | .63 (.25) | −0.06 | .78 (.24) | .58 (.24) | −0.20 |
| Weighted Reciprocity | .78 (.28) | .64 (.20) | −0.14 | .74 (.15) | .70 (.18) | −0.04 | .76 (.22) | .67 (.19) | −0.09 |
| Centralization | |||||||||
| In-degree (ties) | .07 (.13) | .35 (.27) | 0.28 | .22 (.18) | .20 (.12) | −0.02 | .14 (.17) | .28 (.22) | 0.14 |
| In-degree (weighted) | .15 (.10) | .26 (.29) | 0.11 | .27 (.13) | .21 (.12) | −0.06 | .21 (.13) | .24 (.22) | 0.03 |
Figure 1.
Team Communication Networks at Baseline and Follow-up
Among small teams, the number of ties declined from baseline (M=14.36, SD = 5.35) to follow up (M=11.09, SD=4.99). On average, small teams maintained 67% of the ties reported across both time points. Among ties that changed over time, a greater proportion of ties were dissolved (22.3%) than formed (10.7%); thus, although new ties were formed during the learning collaborative, more ties dissolved resulting in a net decrease in communication ties within small teams. Overall connectedness also declined among small teams: average communication frequency declined slightly from the beginning (M=5.76, SD=0.82) to the end of the learning collaborative (M=5.63, SD=0.83), and fell between “about weekly” and “about daily” on the response scale. Average network density, which is the percentage of communication ties present, also decreased from 91% to 73% indicating that the team communication networks became sparser over time. Overall relationship strength also declined: the average percentage of reciprocated ties decreased from 87% to 54%, indicating that within small teams, relationships became more unidirectional over time. The weighted reciprocity also decreased, but to a lesser extent (from 78% to 64%). These changes resulted in more centralized networks; both in-degree and weighted in-degree centralization increased over time (from 0.07 to .35, and from .15 to .26, respectively) suggesting that communication became more clustered around one or more few central team members in small teams.
Unlike the small teams, large teams experienced an expansion over time. Large teams reported an increase in number of ties from baseline (M=43.80, SD=14.40) to follow-up (M=46.30, SD=19.68), although this change is small (about three ties). Similar to small teams, large teams maintained about 66% of their ties over time. However, a greater percentage of ties were formed (17%), than dissolved (14.7%). Thus, although small teams experienced a net decrease in communication ties, large teams observed a net increase. Compared to small teams, large teams reported a lower baseline average communication frequency (M=4.75, SD=1.02; representing “about weekly” on the response scale) which increased slightly over time (M=4.9, SD=.93). Large team communication networks had lower density scores, but unlike small teams (which became more sparse), large teams grew denser over time (from 55% to 59% connected). Both reciprocity measures remained fairly constant suggesting that relationship strength did not change. In terms of centralization, large teams were more centralized at baseline (in-degree centralization M=.22, weighted in-degree centralization M=.27) than small teams (in-degree centralization M=.07, in-degree weighted centralization M=.15). Although small teams became more centralized over time, centralization in large teams remained somewhat constant. In-degree centralization declined (from .22 to .20) as well as weighted in-degree centralization (from .27 to .21) indicating communication became less clustered, although the change is small.
Discussion
With an emphasis on team building and shared learning, learning collaborative models have potential for strengthening communication within organizational teams, which is necessary for successful quality improvement efforts including implementation of evidence-based practices. Our study is one of the first to explore whether and how organizational team communication patterns change during participation in learning collaboratives. Using a social network approach that examines change at multiple levels, results suggest that team communication patterns change over time. At the individual level, participants communicated with more of their team members by the end of the learning collaborative, but there was no evidence suggesting learning collaboratives built new or more frequent communication ties across organizational hierarchies. Although few, these new communication ties produced denser team network structures, although this difference was small and occurred in larger teams. Smaller teams, on the other hand, grew sparser and more centralized suggesting that teams may differentially benefit from learning collaboratives depending on their size.
At the beginning of the learning collaboratives, team members were communicating with one another weekly or daily. By the end of the learning collaborative, participants communicated with more of their team members, while maintaining the same frequency of communication. Communicating with additional colleagues can be time consuming, therefore individuals can be constrained in the number of colleagues with whom they communicate frequently (Roberts, Dunbar, Pollet, & Kuppens, 2009). As participants expanded their networks to include additional colleagues, they could have accommodated these new communication demands by reducing their overall communication frequency or intensity. However, in this study, results indicate that participants continued to communicate just as intensively within their teams throughout the duration of the learning collaborative, suggesting that participants can accommodate additional communication demands without sacrificing intensity.
Although learning collaboratives are expected to build and strengthen cross-hierarchical communication ties within an organization, our results indicate little change in the tendency to communicate with others in different team roles. In fact, the number of ties between supervisors and senior leaders declined over time. Unlike the hierarchical communication patterns observed in other studies of healthcare organizations (Bae et al., 2015; Cott, 1997), teams in this study began the learning collaborative with fairly frequent communication across the organizational hierarchy as indicated by the E-I index. In fact, the most frequent communication was observed between senior leaders and supervisors, and between supervisors and clinicians. Over time, few changes in cross-hierarchical communication relationships were observed suggesting that participants maintained intensive communication across hierarchical levels.
Together these results might be seen as a challenge to claims that learning collaboratives build strong communication within implementation teams. However, communication in general, and across hierarchical levels was high at the beginning of the learning collaborative, perhaps due to the relatively high proportion of relatively new employees. Nearly half of the participants began working at their agency within a year of the learning collaborative, and may have relied on frequent communication with their colleagues and supervisors to learn their new job at baseline. Also, other studies (Rangachari et al, 2014) suggest that communication among team members can fluctuate over the duration of quality improvement initiatives, peaking after the launch and declining over time to return to initial levels, perhaps reflecting a shift from initial innovation adoption to sustainment phases. As participants became more proficient in their jobs, and integrated the new intervention into their daily practice, the need for communication may have decreased over time. Or, communication may reach a threshold and decline as a result of fatigue and disengagement with the learning collaborative.
Nonetheless, these small adjustments to communication patterns at the individual and dyadic-levels produced some observable changes in the structure of team’s communication networks, although change manifested differently depending on team size. Among small teams, communication frequency declined over time. Additionally, networks became more sparse and centralized, with fewer strong reciprocated ties. Yet, large teams’ communication networks grew slightly more dense and strong. Our results extend existing findings that team size matters for cohesion and organizational change efforts. Compared to large teams, small teams tend to cohere faster and require communication and dialogue among fewer members to share their collective knowledge (Thompson, 2015). However, with each additional member, teams accumulate a variety of skills, expertise, and resources. The diversity found among larger teams stimulates interaction and can strengthen communication, which is essential for solving complex problems, such as quality improvement or implementation challenges. As a result, large teams benefit from their collective knowledge and skills, and this has been positively associated with team performance (Thompson et al 2015), innovation (Hulsheger, et al 2009), and implementation (Ditty et al 2015).
Implications for Healthcare Leaders and Managers
In light of our findings, learning collaborative leaders might consider adjusting the components expected to strengthen communication among team members. While the in-person learning sessions might bring teams together for collaborative planning every few months, promoting strong and meaningful team communication might require more structured and continuous opportunities to interact back at the home agency. Thus, learning collaborative leaders might focus on providing greater support for the model components that are focused on internal quality improvement, such as PDSA cycles, and other quality monitoring activities. Ongoing support for bringing clinicians, supervisors, and senior leaders together to communicate regularly and intensively about implementation could help build and maintain strong ties among team members, especially across the hierarchy.
Additionally, organizational leaders who will be participating in a learning collaborative might consider sending larger teams. Findings related to differential change in communication by team size suggest that learning collaborative models may be less beneficial for enhancing communication among small teams. Although taking more professional staff “offline” for training can present challenges for managers (especially smaller agencies with fewer staff to maintain service levels), developing a critical mass of individuals who are adopting an innovation generates a more supportive organizational climate for implementation (Powell, Hausmann-Stabile, & McMillen, 2013).
Limitations & Agenda for Future Research
First, although this study includes a substantial number of organizational teams compared to other network studies, the number (21 teams) precludes significance testing at the team level. Second, our focus on children’s mental health organizations in a single region limits the generalizability. Generalizability of this study’s findings may also be limited by selection bias. Organizations that participated in the learning collaborative and in the study likely include those that were interested in implementing TF-CBT. Communication in these organizations may differ from those that declined to participate because they already implemented TF-CBT, perceived TF-CBT was a poor fit for their agency, and/or lacked the resources necessary to support this intervention. Furthermore, generalizability may be constrained by the relatively high level of attrition. A substantial number of clinicians (n=61) dropped out of the learning collaborative - although not uncommon among frontline staff, we are not able to examine how this turnover and attrition influences organizational communication. Third, findings are based upon participant self-reports which may introduce social desirability and/or recall bias. Fourth, the lack of a control or comparison group prohibits causal inferences about the impact of learning collaboratives on communication networks. Fifth, although this study benefits from a high response rate from learning collaborative completers, missing data from non-responders or non-completers likely produces underestimates of the number of ties, communication frequency, and network metrics. Sixth, this study assesses frequency of communication with organizational team members, but does not explore the content of what was discussed among team members and how this may have changed over time. Finally, in the absence of implementation or treatment outcome data, we cannot examine whether change in communication networks or learning collaborative participation leads to quality improvement..
However, our findings generate new insights related to research questions, designs, and methods for advancing research on the impact of learning collaboratives and other large group implementation interventions. Future studies examining evolution of communication and other professional networks may require data collection at multiple time points especially since Rangachari et al (2014), noted that change in team communication may peak during the early stages of the initiative prior to declining. Furthermore, because communication patterns can vary based on content (about implementation, treatment, etc.), future studies might adopt a more refined measurement approach, complemented by qualitative data, to better understand the nature of and change in team communication.
Although this study explored changes among teams’ internal communication patterns, structured opportunities to learn from other organizational teams and the learning collaborative faculty leaders can also broker new relationships between teams. External relationships spanning structural holes between groups transfer new information that stimulates change and innovation (Hansen, 1999). Small teams, with few members to shoulder the burden of participation, and quality improvement might especially benefit from these opportunities. Additional research examining the evolution and interaction of internal and external social relationships among small and large teams would be helpful for assessing the effectiveness of learning collaboratives for building both types of ties. Finally, more rigorous studies with comparison conditions are needed to assess the impact of learning collaboratives on communication patterns, improvement, and client outcomes.
Acknowledgments
This research was supported in part by a National Research Service Award Postdoctoral Traineeship (T32 MH019117)(AB) from the National Institute of Mental Health. Preparation of this article was also supported by the Implementation Research Institute (IRI) at the George Warren Brown School of Social Work, Washington University in St. Louis; through an award from the National Institute of Mental Health (R25 MH080916-01A2), and the Department of Veterans Affairs, Health Services Research and Development Service, Quality Enhancement Research Initiative (QUERI) (AB). The authors gratefully acknowledge Dr. Tom Valente for his valuable consultation on network data management and assistance calculating network metrics, and Drs. Natasha Bowen and Njeri Kagotho for their helpful comments on an earlier draft.
Contributor Information
Alicia C. Bunger, Assistant Professor, College of Social Work, Ohio State University, 1947 College Road, Columbus, Ohio 43210, Phone: 614-688-8366; Fax: 614-292-7522.
Rebecca Lengnick-Hall, Doctoral Student. School of Social Work, University of Southern California.
References
- Bae SH, Nikolaev A, Seo JY, Castner J. Healthcare Provider Social Network Analysis: A Systematic Review. Nursing Outlook. 2015;63(5):566–584. doi: 10.1016/j.outlook.2015.05.006. http://doi.org/10.1016/j.outlook.2015.05.006. [DOI] [PubMed] [Google Scholar]
- Balkundi P, Harrison DA. Ties, Leaders, and Time in Teams: Strong Inference About Network Structure’s Effects on Team Viability and Performance. Academy of Management Journal. 2006;49(1):49–68. http://doi.org/10.5465/AMJ.2006.20785500. [Google Scholar]
- Borgatti SP, Everett MG, Freeman LC. Ucinet for Windows: Software for Social Network Analysis. Harvard, MA: Analytic Technologies; 2002. [Google Scholar]
- Bunger AC, Hanson RJ, Doogan NJ, Powell BJ, *Cao Y, Dunn J. Can Learning Collaboratives Support Implementation By Rewiring Networks? Administration and Policy in Mental Health and Mental Health Services Research. 2016:79–92. doi: 10.1007/s10488-014-0621-x. http://dx.doi.org/10.1007/s10488-014-0621-x. [DOI] [PMC free article] [PubMed]
- Cavaleri MA, Gopalan G, Mckay MM, Appel A, Bannon WMJ, Bigley MF, … Thalor S. Impact of a learning collaborative to improve child mental health service use among low-income urban youth and families. Best Practices in Mental Health. 2006;2(2):67–79. [Google Scholar]
- Cary CE, McMillen JC. The data behind the dissemination: A systematic review of trauma-focused cognitive behavioral therapy for use with children and youth. Children and Youth Services Review. 2012;34(4):748–757. http://doi.org/10.1016/j.childyouth.2012.01.003. [Google Scholar]
- Chambers D, Wilson P, Thompson C, Harden M. Social network analysis in healthcare settings: A systematic scoping review. PLoS ONE. 2012;7(8) doi: 10.1371/journal.pone.0041911. http://doi.org/10.1371/journal.pone.0041911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke N. Transorganization Development for Network Building. The Journal of Applied Behavioral Science. 2005;41(1):30–46. http://doi.org/10.1177/0021886304272655. [Google Scholar]
- Cott C. “We decide, you carry it out”: A social network analysis of multidisciplinary long-term care teams. Social Science & Medicine. 1997;45(9):1411–1421. doi: 10.1016/s0277-9536(97)00066-x. http://doi.org/10.1016/S0277-9536(97)00066-X. [DOI] [PubMed] [Google Scholar]
- Creswick N, Westbrook JI, Braithwaite J. Understanding communication networks in the emergency department. BMC Health Services Research. 2009;9:247. doi: 10.1186/1472-6963-9-247. http://doi.org/10.1186/1472-6963-9-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham FC, Ranmuthugala G, Plumb J, Georgiou A, Westbrook JI, Braithwaite J. Health professional networks as a vector for improving healthcare quality and safety: a systematic review. BMJ Quality & Safety. 2012;21(3):239–49. doi: 10.1136/bmjqs-2011-000187. http://doi.org/10.1136/bmjqs-2011-000187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ditty MS, Landes SJ, Doyle A, Beidas RS. It Takes a Village: A Mixed Method Analysis of Inner Setting Variables and Dialectical Behavior Therapy Implementation. Administration and Policy in Mental Health. 2015;42(6):672–81. doi: 10.1007/s10488-014-0602-0. http://doi.org/10.1007/s10488-014-0602-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn AG, Westbrook JI. Interpreting social network metrics in healthcare organisations: a review and guide to validating small networks. Social Science & Medicine (1982) 2011;72(7):1064–8. doi: 10.1016/j.socscimed.2011.01.029. http://doi.org/10.1016/j.socscimed.2011.01.029. [DOI] [PubMed] [Google Scholar]
- Ebert L, Amaya-Jackson L, Markiewicz JM, Kisiel C, Fairbank JA. Use of the Breakthrough Series Collaborative to Support Broad and Sustained Use of Evidence-Based Trauma Treatment for Children in Community Practice Settings. Administration and Policy in Mental Health and Mental Health Services Research. 2012;39(3):187–199. doi: 10.1007/s10488-011-0347-y. http://doi.org/10.1007/s10488-011-0347-y. [DOI] [PubMed] [Google Scholar]
- Garcia SK. Developing Social Network Propositions to Explain Large-Group Intervention Theory and Practice. Advances in Developing Human Resources. 2007;9(3):341–358. http://doi.org/10.1177/1523422307304100. [Google Scholar]
- Hansen MT. The Search-Transfer Problem: The Role of Weak Ties in Sharing Knowledge across Subunits Organization. Administrative Science Quarterly. 1999;44:82–111. [Google Scholar]
- Hülsheger UR, Anderson N, Salgado JF. Team-level predictors of innovation at work: A comprehensive meta-analysis spanning three decades of research. Journal of Applied Psychology. 2009;94(5):1128–1145. doi: 10.1037/a0015978. doi.org/10.1037/a0015978. [DOI] [PubMed] [Google Scholar]
- Institute for Healthcare Improvement. The Breakthrough Series: IHI’s Collaborative Model for Achieving Breakthrough Improvement. Cambridge, MA: IHI Innovation Seies White Paper; 2003. [Google Scholar]
- IOM. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- Katzelnick DJ, Von Korff M, Chung H, Provost LP, Wagner EH. Applying depression-specific change concepts in a collaborative breakthrough series. Joint Commission Journal on Quality and Patient Safety. 2005;31(7):386–397. doi: 10.1016/s1553-7250(05)31052-x. [DOI] [PubMed] [Google Scholar]
- Kilo CM. A Framework for Collaborative Improvement: Lessons from the Institute for Healthcare Improvement’s Breakthrough Series. Quality Management in Health Care. 1998;8(4):1–13. doi: 10.1097/00019514-199806040-00001. [DOI] [PubMed] [Google Scholar]
- Krackhardt D, Stern RN. Informal Networks and Organizational Crises: An Experimental Simulation. Social Psychology Quarterly. 1988;51(2):123–140. [Google Scholar]
- Mohrman Sa, Tenkasi RV, Mohrman AM., Jr The Role of Networks in Fundamental Organizational Change: A Grounded Analysis. Journal of Applied Behavioral Science. 2003;39(3):301–323. http://doi.org/10.1177/0021886303258072. [Google Scholar]
- Nadeem E, Olin SS, Hill LC, Hoagwood KE, Horwitz SM. Understanding the components of quality improvement collaboratives: a systematic literature review. The Milbank Quarterly. 2013;91(2):354–94. doi: 10.1111/milq.12016. http://doi.org/10.1111/milq.12016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadeem E, Olin SS, Hill LC, Hoagwood KE, Horwitz SM. A literature review of learning collaboratives in mental health care: Used but untested. Psychiatric Services. 2014;65(2):1088–1099. doi: 10.1176/appi.ps.201300229. http://doi.org/10.117/appi.ps.201300229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nembhard IM. Learning and improving in quality improvement collaboratives: which collaborative features do participants value most? Health Services Research. 2009;44(2 Pt 1):359–78. doi: 10.1111/j.1475-6773.2008.00923.x. http://doi.org/10.1111/j.1475-6773.2008.00923.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nembhard IM. All teach, all learn, all improve? The role of interorganizational learning in quality improvement collaboratives. Health Care Management Review. 2012;37(2):154–164. doi: 10.1097/HMR.0b013e31822af831. http://doi.org/10.1097/HMR.0b013e31822af831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nembhard IM, Alexander JA, Hoff TJ, Ramanujam R. Why does the quality of health care continue to lag? Insights from management research. Academy of Management Perspectives. 2009;23(1):24–42. [Google Scholar]
- Powell BJ, Hausmann-Stabile C, McMillen JC. Mental health clinicians’ experiences of implementing evidence-based treatments. Journal of Evidence-Based Social Work. 2013;10(5):396–409. doi: 10.1080/15433714.2012.664062. http://doi.org/10.1080/15433714.2012.664062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rangachari P, Madaio M, Rethemeyer RK, Wagner P, Hall L, Roy S, Rissing P. Role of Communication Content and Frequency in Enabling Evidence-Based Practices. Quality Management in Health Care. 2014;23(1):43–58. doi: 10.1097/QMH.0000000000000017. http://doi.org/10.1097/QMH.0000000000000017. [DOI] [PubMed] [Google Scholar]
- Rangachari P, Madaio M, Rethemeyer RK, Wagner P, Hall L, Roy S, Rissing P. The evolution of knowledge exchanges enabling successful practice change in two intensive care units. Health Care Management Review. 2015;40(1):65–78. doi: 10.1097/HMR.0000000000000001. http://doi.org/10.1097/HMR.0000000000000001. [DOI] [PubMed] [Google Scholar]
- Roberts SG, Dunbar RI, Pollet TV, Kuppens T. Exploring variation in active network size: Constraints and ego characteristics. Social Networks. 2009;31(2):138–146. doi: 10.1016/j.socnet.2008.12.002. [DOI] [Google Scholar]
- Sasovova Z, Mehra A, Borgatti SP, Schippers MC. Network churn: The effects of self-monitoring personality on brokerage dynamics. Administrative Science Quarterly. 2010;55(4):639–670. [Google Scholar]
- Schouten LMT, Hulscher MEJL, van Everdingen JJE, Huijsman R, Grol RPTM. Evidence for the impact of quality improvement collaboratives: systematic review. BMJ (Clinical Research Ed.) 2008;336(7659):1491–4. doi: 10.1136/bmj.39570.749884.BE. http://doi.org/10.1136/bmj.39570.749884.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparrowe RT, Liden RC, Wayne SJ, Kraimer ML. Social Networks and the Performance of Individuals and Groups. Academy of Management Journal. 2001;44(2):316–325. http://doi.org/10.2307/3069458. [Google Scholar]
- Squartini T, Picciolo F, Ruzzenenti F, Garlaschelli D. Reciprocity of weighted networks. Scientific Reports. 2013;3 doi: 10.1038/srep02729. http://doi.org/10.1038/srep02729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenkasi RV, Chesmore MC. Social Networks and Planned Organizational Change: The Impact of Strong Network Ties on Effective Change Implementation and Use. Journal of Applied Behavioral Science. 2003;39(3):281–300. http://doi.org/10.1177/0021886303258338. [Google Scholar]
- Thompson BM, Haidet P, Borges NJ, Carchedi LR, Roman BJB, Townsend MH, … Levine RE. Team cohesiveness, team size and team performance in team-based learning teams. Medical Education. 2015;49(4):379–85. doi: 10.1111/medu.12636. http://doi.org/10.1111/medu.12636. [DOI] [PubMed] [Google Scholar]
- Valente TW. Social networks and health: models, methods, and applications. Oxford University Press; 2010. [Google Scholar]
- Wasserman S, Faust K. Social Network Analysis: Methods and Applications. New York: Cambridge University Press; 1994. [Google Scholar]