Abstract
We report a rare clinical case of hemosiderotic dermatofibroma in a 36-year-old female patient. The main dermatoscopic finding was represented by homogeneous blue-gray pigmentation. The aim of this report is to demonstrate the rarity of the lesion and the dermatoscopic importance it assumes by sharing a blue-gray homogeneous pattern with other benign and malignant lesions.
Keywords: Benign fibrous histiocytoma, dermoscopy, differential diagnosis
INTRODUCTION
Dermoscopy is a useful noninvasive technique, mainly used to aid in the diagnosis of pigmented, melanocytic, and non-melanocytic lesions, according to specific criteria.1 Dermatofibroma (DF) is a benign skin tumor, usually diagnosed without much difficulty by clinical history and typical dermatoscopic findings. However, DFs have a wide range of clinical and dermatoscopic variants. Atypical or rare variants may mimic other skin tumors.2-4
We report a case of hemosiderotic DF with a homogeneous blue-gray pigmentation pattern, indistinguishable from other benign or malignant skin lesions. Such dermoscopic finding makes differential diagnosis with melanoma necessary.
CASE REPORT
We report the case of a 36-year-old female patient with a single plaque-like asymptomatic pigmented lesion on her right breast for 11 months. The lesion had progressively enlarged during the last three months. She had negative personal and family history of melanoma or other skin tumors. Dermatological examination revealed a blue-gray hard plaque with a hypochromic halo on the right breast (Figure 1).
Figure 1.

Blue-gray hard plaque with a hypochromic halo on the right breast
Dermoscopic examination showed only a blue-gray homogeneous pattern (Figure 2). We performed a total excision of the lesion with a 2-mm margin. The material was sent for histopathological examination. Histological sections stained with hematoxylin-eosin showed epidermis with acanthosis and dermis with proliferation of elongated cells showing brown pigmentation or involving thickened collagen fibers (Figures 3 and 4). Perls' staining technique revealed blueness in correspondence to the brown pigment, compatible with hemosiderin (Figure 5).
Figure 2.
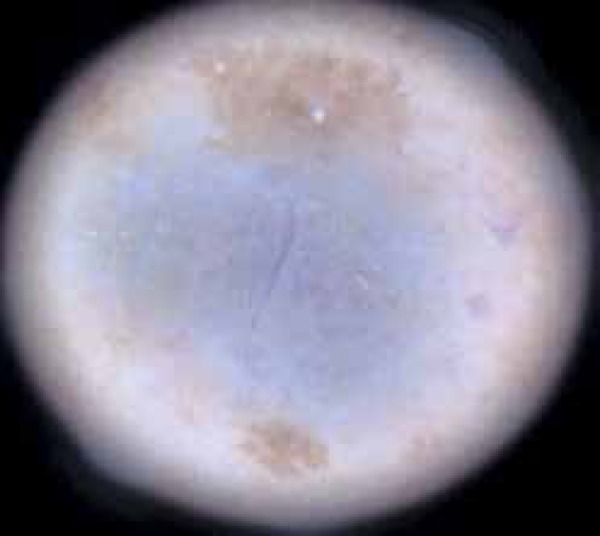
Dermatoscopic examination revealed a homogeneous blue-gray area and collision of freckles at the periphery of the lesion
Figure 3.
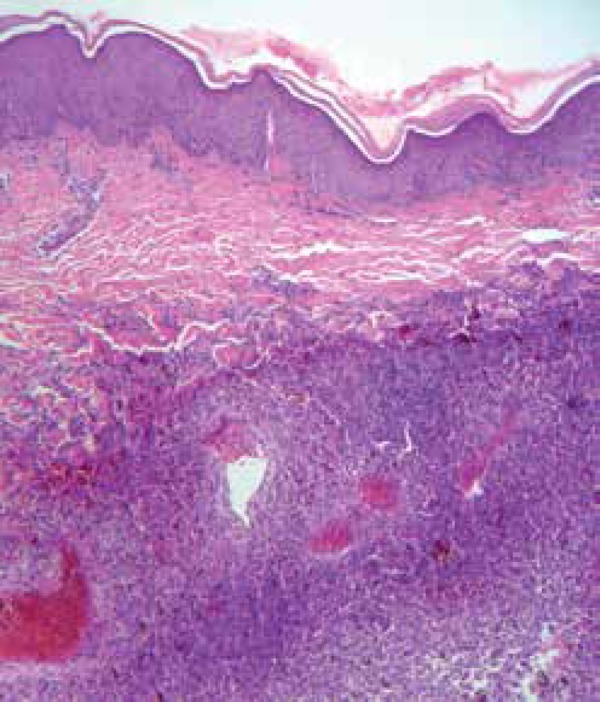
Histopathology: dermal involvement represented by the proliferation of cells, some showing brown pigmentation and other involving thickened collagen fibers (Hematoxylin & eosin x100)
Figure 4.
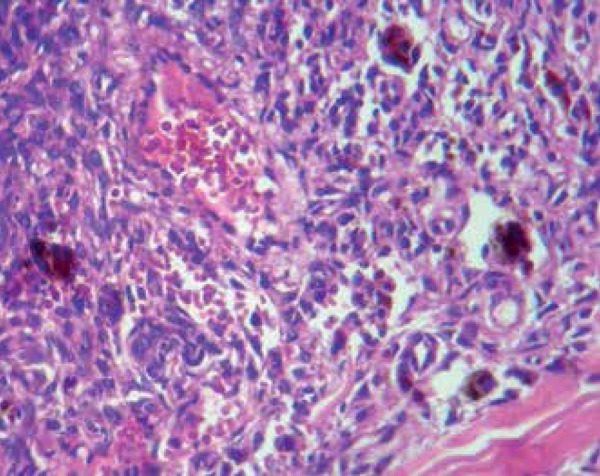
High magnification: detail of the brown pigment retention by proliferated stellate cells. Dilated vessels filled with red blood cells in between stellate cells (Hematoxylin & eosin x400)
Figure 5.
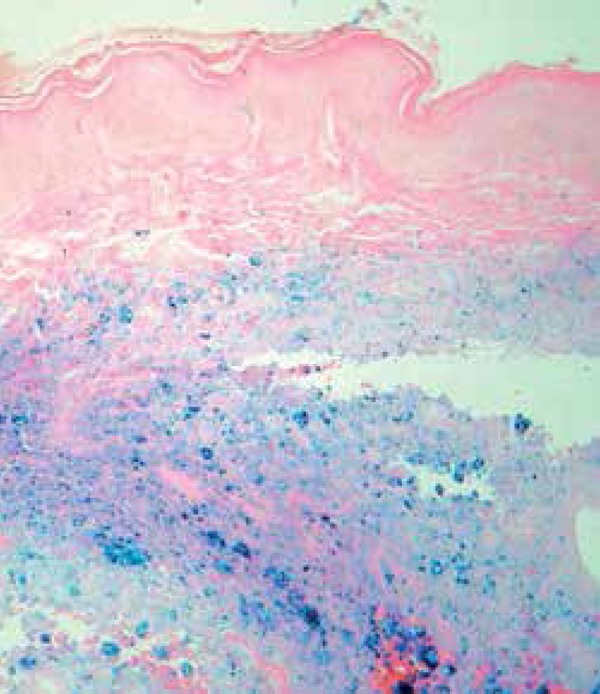
Perls’ staining revealing bluish intracellular iron storage in the form of hemosiderin (Hematoxylin & eosin x100)
Considering the clinical characteristics and dermoscopic and histopathological findings, the lesion was diagnosed as hemosiderotic DF.
DISCUSSION
DF is a benign tumor of uncertain histogenesis, probably fibrohistiocytic, more commonly observed on the lower extremities of young adults, with a slight predilection for females. It manifests as a papule, plaque, or hardened nodule, which may exist with a variable degree of pigmentation, from light brown to blackish-brown. It is usually asymptomatic and may be solitary or multiple.1,2,5 The classically described dermoscopic finding is a scarring plaque with central clearing surrounded by a thin, peripheral pigment network. This pattern is observed in 36%-80% of DFs, which enables a rapid and accurate diagnosis in most cases.1-4,6 However, cases with atypical clinical presentations or histologic variants (aneurysmal, hemosiderotic, epithelioid, and atrophic DFs, or DF with sebaceous component) may raise doubts about the diagnosis.3,4 Therefore, in such cases, the correlation between clinical findings, dermoscopy, and histopathology becomes essential.
The hemosiderotic variant represents approximately 2% of DFs.2-4 Dermoscopic findings reveal an homogeneous area of blue or bluish-red pigmentation in the center of the lesion. This pigmentation is histopathologically correlated to proliferation of macrophages (multinucleated histiocytes) containing hemosiderin within the cytoplasm.2 It is believed that erythrocytes extravasate from small vessels, with subsequent production of hemosiderin, which would be engulfed by the tumorous cells.2,7
Santa Cruz and Kyriakos postulated that the slow and continuous extravasation of blood from intratumoral capillaries would form some vascular spaces. That would lead to the loss of stromal support and the consequent increase in tumor internal pressure, causing cavity dilatation lacking an endothelial lining.2,8 At this stage, aneurysmal DFs would be formed. Therefore, hemosiderotic DF would be the initial phase of aneurysmal DFs. The etiology of these aneurysmal cavities is unknown. For some authors, this phenomenon could occur in hypercellularity regions with poor reticulin network or as a result of traumas or repetitive microtraumas, which would precipitate micro-haemorrhages as described before.2,8,9
In hemosiderotic or aneurysmal DFs, other dermoscopic structures can be observed in association with homogeneous blue or bluish-red areas, such as a fine peripheral pigmented network, bright white linear structures (chrysalis-like structures), and different vascular structures, determining a multicomponent pattern.2
The dermoscopic examination of this case only showed a homogeneous blue-gray area, which seems to be - as believed by other authors - due to the hemosiderin deposit contained in tumor cells. The blue-gray homogeneous pattern has been cited in the literature as a dermoscopic feature of rare variants of DF.2-4 However, this pattern is nonspecific and can be seen in melanocytic lesions, including melanoma and blue nevus, as well as in non-melanocytic neoplasms such as vascular tumors, tumor of the appendages, and cysts.
Therefore, in such cases, biopsy and histopathological examination are mandatory to confirm the diagnosis. An exception to this rule is the blue nevus, whose diagnosis can be made by the association of the homogeneous blue pattern with medical history of long-term stability of the lesion. In such cases, tumor removal is not necessary.10
Footnotes
Conflict of Interest: None
Financial Support: None
Work performed at Institute of Dermatology Professor Rubem David Azulay at Santa Casa de Misericordia do Rio de Janeiro (IDPRDA-SCMRJ) - Rio de Janeiro (RJ), Brazil.
References
- 1.Argenziano G, Soyer HP, De Giorgi V, Piccolo D, Carli P, Delfino M, et al. Dermoscopy: A Tutorial. Milan: EDRA Medical Publishing & New Media; 2000. [Google Scholar]
- 2.Zaballos P, Llambrich A, Ara M, Olazarán Z, Malvehy J, Puig S. Dermoscopic findings of haemosiderotic and aneurysmal dermatofibroma: report of six patients. Br J Dermatol. 2006;154:244–250. doi: 10.1111/j.1365-2133.2005.06844.x. [DOI] [PubMed] [Google Scholar]
- 3.Kilinc Karaarslan I, Gencoglan G, Akalin T, Ozdemir F. Different dermoscopic faces of dermatofibromas. J Am Acad Dermatol. 2007;57:401–406. doi: 10.1016/j.jaad.2006.10.984. [DOI] [PubMed] [Google Scholar]
- 4.Puig S, Romero D, Zaballos P, Malvehy J. Dermoscopy of dermatofibroma. Arch Dermatol. 2005;141:122–122. doi: 10.1001/archderm.141.1.122. [DOI] [PubMed] [Google Scholar]
- 5.Lourival Lopes Filho L, de Oliveira de Avelar Alchorne A. Pre-operative evaluation of the visible and palpable diameters of dermatofibroma. Int J Dermatol. 2003;42:736–737. doi: 10.1046/j.1365-4362.2003.01910.x. [DOI] [PubMed] [Google Scholar]
- 6.Ferrari A, Soyer HP, Peris K, Argenziano G, Mazzocchetti G, Piccolo D, et al. Central white scarlike patch: A dermatoscopic clue for the diagnosis of dermatofibroma. J Am Acad Dermatol. 2000;43:1123–1125. doi: 10.1067/mjd.2000.109842. [DOI] [PubMed] [Google Scholar]
- 7.Ozdemir F, Kilinc I, Akalin T. Homogeneous blue pigmentation in dermatofibroma. J Eur Acad Dermatol Venereol. 2006;20:733–734. doi: 10.1111/j.1468-3083.2006.01633.x. [DOI] [PubMed] [Google Scholar]
- 8.Santa Cruz DJ, Kyriakos M. Aneurysmal ('angiomatoid') fibrous histiocytoma of the skin. Cancer. 1981;47:2053–2061. doi: 10.1002/1097-0142(19810415)47:8<2053::aid-cncr2820470825>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 9.Pegas JR, Santos BA, Tebcherani AJ, Cade KV. Dermatofibroma aneurismático. Surg Cosmet Dermatol. 2010;2:225–227. [Google Scholar]
- 10.Zalaudek I, Docimo G, Argenziano G. Using Dermoscopic Criteria and Patient-Related Factors for the Management of Pigmented Melanocytic Nevi. Arch Dermatol. 2009;145:816–826. doi: 10.1001/archdermatol.2009.115. [DOI] [PMC free article] [PubMed] [Google Scholar]


