Abstract
The aim of this study is to evaluate the benefits of laparoscopic Doppler ultrasound (LDU) application during laparoscopic varicocelectomy (LV), and to compare the surgical outcomes and complications between LDU-assisted LV (LDU-LV) and conventional LV for infertile patients with varicoceles; 147 infertile patients were randomly divided into two groups. Operative and postoperative parameters, semen parameters, and the pregnancy rate were compared. There were no differences in baseline demographics. The operative time was significantly longer in LDU-LV group than LV group. The incidence of postoperative hydrocele was 1.4% (1/72) in LDU-LV group versus 10.7% (8/75) in LV group, which showed a significant difference (P < 0.05). However, other surgical outcomes, such as postoperative hospital stay, postoperative recurrence, and testicular atrophy, were similar between the two groups. Sperm concentration and sperm motility were significantly increased in both groups at 3, 6, and 12 months after surgery (P < 0.01), and they were higher in LDU-LV than LV group in 12 months after surgery (34.21 ± 6.36 vs 29.99 ± 6.04 for concentration, P < 0.05; 40.72 ± 8.12 vs 37.31 ± 6.12 for motility, P < 0.05). Sperm morphology was comparable between the two groups. The pregnancy rate showed no significant difference (44.4% of the LDU-LV vs 37.3% of the LV, P > 0.05). In conclusion, compared with LV, LDU-LV could safely and effectively ligate all spermatic veins and preserve spermatic arteries without leading to high varicocele recurrence and postoperative hydrocele. Given the benefits that sperm counts as well as sperm motility favoring LDU-LV, we recommend that LDU should be routinely used as an effective tool to improve outcomes and safety of laparoscopic varicocelectomy.
Keywords: Doppler ultrasound, laparoscopic varicocelectomy, varicocele
INTRODUCTION
Varicocele is a palpable dilation in the pampiniform plexus of veins in the scrotal sac secondary to retrograde flow of blood to the testicle.1 Varicoceles are present in 10%–15% of the general male population, in approximately 35%–50% of men with primary infertility and up to 81% of patients with secondary infertility.2 Varicocelectomy can be performed by various methods and techniques, which can improve semen parameters and increase the spontaneous pregnancy rates as well as resolve testicular pain effectively.3 With the extensive application of laparoscopic technique, laparoscopic varicocelectomy (LV) was widely employed due to its rapid, safe, effective, and minimally invasive features.4
There was much debate regarding the significance of artery sparing when performing an LV. Several studies found that no differences in semen parameters and pregnancy rates were detected between internal spermatic arteries (ISAs) sparing and ligation;5,6 and higher recurrent rate and persistence of varicocele in ISAs preservation patients were reported.7,8,9 Conversely, other reports indicated that ISAs-sparing procedure was significantly superior in improvement of sperm concentration, motility, morphology than ligation.10 In addition, there was a study with ISAs and lymphatic vessels preserved reporting a low recurrent rate (1.2%).11 The above inconsistency may partly arise from the ambiguity of ISAs preservation due to the poor identification. Higher recurrence of varicocele after ISAs preservation may be attributed to the concurrent preservation of the accompanying veins. Compared with microsurgical varicocelectomy, it was even harder to identify the ISAs precisely and separate them from the adherent veins during LV due to the lower magnification of vasculature under laparoscope and the relatively rough surgical tools. It was common that the veins were left out because of fear of injury to the artery during attempts to ensure ISAs preservation. In addition, due to the poor identification, arteries that were supposedly spared might not be preserved actually. Therefore, techniques that can identify the ISAs and isolate the vascular structures precisely during LV will be rewarded.
Since Fukuda and colleagues used Doppler Ultrasound to evaluate hepatic tumors during laparoscopic surgery in 1982,12 intraoperative ultrasound technology has been widely used to facilitate recognition and dissection of vascular and nonvascular structures in laparoscopic surgery.13,14 Our previous study indicated that Doppler ultrasound-assisted microsurgical varicocelectomy had better outcomes for semen parameters improvement.15 In the present study, a prospective evaluation of the application of laparoscopic Doppler technology during ISAs preservation LV versus conventional LV was conducted in infertile men with varicoceles. We hypothesized that the assistance of laparoscopic Doppler ultrasound (LDU) could help identify and preserve arteries/lymphatics precisely, thus improving semen qualities as well as pregnancy rates.
MATERIALS AND METHODS
Study design
The study was prospectively conducted at the authors’ institution between October 2012 and February 2014. This study received ethics committee approval with the written informed consent obtained from each participant before enrollment and was registered in the Chinese Clinical Trial Registry (http://www.chictr.org.cn/) (Identifier: ChiCTR-IOR-15007561). Infertile patients with uni- or bi-lateral clinically palpable varicoceles were selected based on the following inclusion and exclusion criteria. Infertility is defined as the inability of a sexually active, noncontracepting couple to achieve spontaneous pregnancy in 1 year. Patient's inclusion criteria were as follows: (1) 20–39-year-old with infertility for more than 1 year; (2) impaired semen quality including sperm concentration <15 × 106 ml−1 or total motility <40% or normal morphology <4%; (3) normal serum hormones level including FSH, LH, thyroid hormones, and PRL; and (4) female partner is healthy and has normal reproductive functions evaluated by gynecologist and endocrinologist prior to male partner enrollment. Exclusion criteria were as follows: (1) refusing to enter randomization; (2) subclinical varicoceles, recurrent varicoceles, and normal semen analyses; (3) other reasons of infertility in addition to varicoceles; (4) patient's spouse older than 35 years; (5) abnormal serum hormone levels; (6) female factor infertility; (7) significant surgical diseases, congenital diseases, or endocrine diseases; and (8) with previous inguinal surgery. Before the randomization, all eligible cases received standardized information about the trial from the clinician, orally and in written. Patients were randomly allocated to two groups through a computer randomization program. A simple random allocation sequence was generated and concealed by a trained nurse. Only the surgeon and his assistants knew that the surgical procedures and investigators were blinded to the procedures. The current study was reported according to the CONSORT guidelines.
Varicoceles classification
Varicoceles were classified into three grades according to the criteria proposed by Dubin and Amelar:16 Grade I (palpable only with the Valsalva maneuver), Grade II (palpable without the Valsalva maneuver), and Grade III (visible through the scrotal skin). Ultrasonography was also used to define varicocele as a spermatic venous diameter of >3.7 mm with an increased diameter on the Valsalva maneuver and venous reflux detected by Doppler.17
Surgical procedures
The expert surgeon (Dr. Yuan) had performed at least 80 LV procedures before starting the study. The Laparoscopic Doppler Ultrasound (LDU) probe (Vascular Technology Inc., Nashua, NH, USA) with 5-mm diameter is disposable and is 20-MHz enhanced.
All procedures were performed under general anesthesia, with the patient in the trendelenburg position. The first 10-mm port was inserted with a modified open access technique just below the umbilicus under direct vision. The pneumoperitoneum was established by a veress needle at a maximum intra-abdominal pressure of 12 cm H2 O and a gas flow rate of 1–2 L min−1. The other two 5-mm ports were placed in the right and left lower quadrants under laparoscopic vision. The peritoneal window was made at the level of dilated spermatic vessels at a distance of 3–5 cm from the internal inguinal ring. In the conventional LV group, the spermatic vessels were mass clipped and completely ligated. However, in the LDU-assisted LV group (LDU-LV), all enlarged arteries and veins were consecutively mobilized, identified in the middle. The Laparoscopic vascular Doppler flow detector was connected to the monitor and directed laparoscopically onto the vessels. The ISAs were identified by the characteristic high-pitched pulsatile arterial flow sound; thus, the ISAs were meticulously identified and preserved. The engorged ISVs were then identified, dissected, and ligated. The remaining tissues including lymphatics were also preserved. The venous ligation was performed by a free-hand intracorporeal knot tying technique with 3-0 silk ligature. No electrocautery was used during the whole operation to avoid thermal injury to the spermatic cord and adjacent tissues. At the end of the operation, carbon dioxide was expelled and the 3 small incisions were closed with absorbable sutures.
Evaluations
Intraoperative assessment
Baseline characteristics including patient age, incidence of bilateral varicocele, hormone level, and varicocele grade between the two groups were recorded. The hormones included testosterone, estradiol, FSH, LH, and PRL. Operation time was also recorded.
Postoperative assessment
We calculated the following parameters after surgery: the incidence of postoperative scrotal pain, postoperative scrotal hematoma and hydrocele, recurrent rate, testicular atrophy, hospital stay period, and time to return to normal activity. All patients were followed with visits at 1, 3, 6, and 12 months after surgery. Testicular volume was assessed pre- and post-operatively from ultrasound measurements performed by a single experienced ultrasonographer using the following formula: volume = 0.71 × length × width × depth. Testicular hypotrophy was defined as 20% volume or greater differential between testicles. Recurrent varicocele was diagnosed clinically and by ultrasonography. The presence or absence of a hydrocele was noted for every patient at each visit. Patients with a hydrocele only on scrotal ultrasound but not palpable on physical examination were excluded.
Sperm parameters assessment
Semen parameters including sperm count, sperm motility, and sperm morphology were checked before and at 3, 6, and 12 months after surgery. The pregnancy rate was calculated at 1 year of follow-up.
Primary and secondary outcomes
The primary outcome measures included improvement in semen parameters and pregnancy rates. The secondary outcome measures included operating time, hospital stay period, time to return to normal activity, and postoperative complications.
Statistical analysis
Student's t-test was performed to analyze the normally distributed continuous variables while Chi-square test was used to compare the categorical variables. Two-way repeated measures ANOVA followed by Holm–Sidak test was performed to evaluate changes of sperm parameters after surgery and different impacts of the two surgical procedures on sperm parameters. All analyses were performed with PASW statistics version 18.0 software (IBM SPSS Inc., Chicago, IL, USA), and P < 0.05 was considered statistically significant. The sample size calculation was based on estimated 1-year pregnancy rates of 55% for LDU-LV and 30% for LV based on previous meta-analysis that compared LV with other varicolectomy.18 To detect a difference in the outcome at the 5% statistical significance level and with 90% power, a minimum sample size of 134 patients was required. Therefore, we recruited 160 patients to allow for a 15% dropout rate.
RESULTS
Initially, 160 patients were enrolled in this study. Thirteen patients were excluded postoperatively because ten of them could not be reached in the follow-up, and three patients achieved pregnancy with assisted reproductive techniques, leaving the final number analyzed at 147 patients (75 in LV group and 72 in LDU-LV group) (Figure 1). The median follow-up period was 20 months (range 14–30 months). There were no statistically significant differences in the patient age, preoperative hormone level, testicular volume, the incidence of bilateral varicocele, and varicocele grade between the two groups (Table 1).
Figure 1.
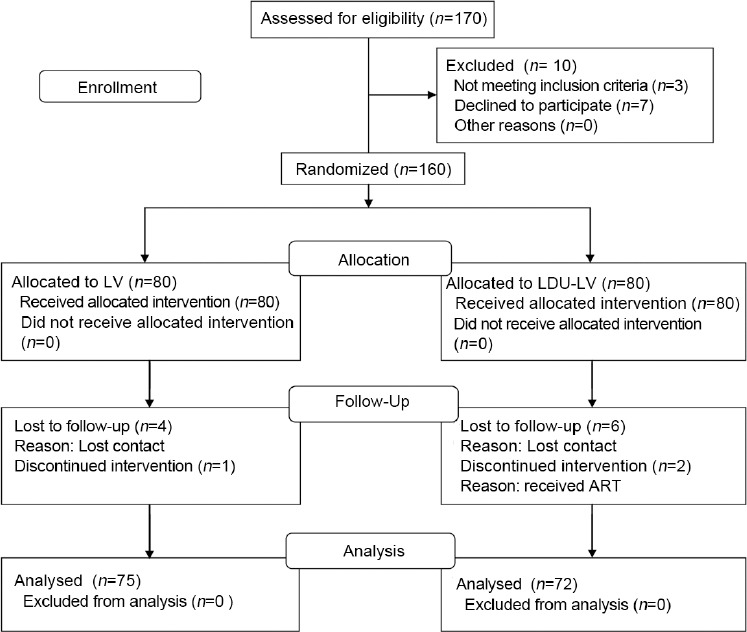
Consolidated standards of reporting trials flowchart for the trial.
Table 1.
Comparison of the preoperative patient characteristics and perioperative outcomes between the two groups
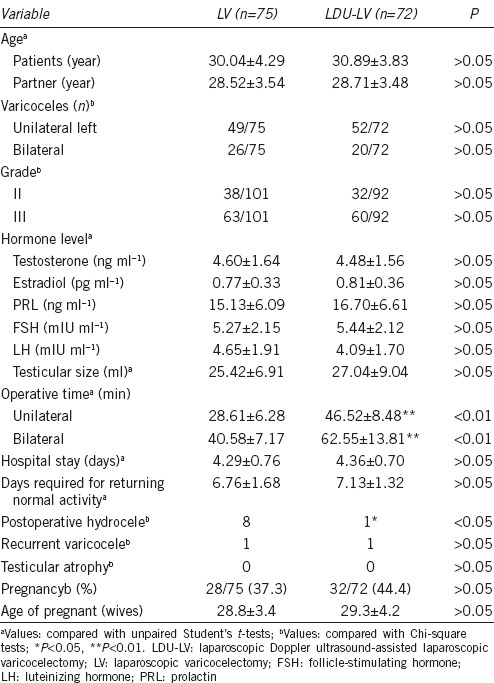
Comparison of intraoperative outcomes
The procedures in the two groups were completed satisfactorily, without intraoperative complications. Both unilateral and bilateral varicoceles’ operative time were significantly longer in the LDU-LV group than LV group (46.52 ± 8.48 vs 28.61 ± 6.28 min for unilateral, 62.55 ± 13.81 vs 40.58 ± 7.17 min for bilateral, Table 1).
Comparison of postoperative outcomes and complications
The hospital stay and time to return to normal activity were little longer for LDU-LV group but did not show statistically significant difference between the two groups (P > 0.05, Table 1). At follow-up, 1 of 72 (1.4%) patients in the LDU-LV group developed a postoperative hydrocele, while it was observed in 8 of 75 (10.7%) in the LV group, which showed a significant difference (P < 0.05, Table 1). Seven of nine postoperative hydroceles were settled spontaneously, and only two patients required intervention. Palpable recurrences were detected in two patients (one in LV and one in LDU-LV), which were confirmed by color Doppler ultrasound (Table 1). The incidence of recurrence was not significantly different between the two groups (Table 1). Testicular atrophy was not detected during the follow-up (Table 1).
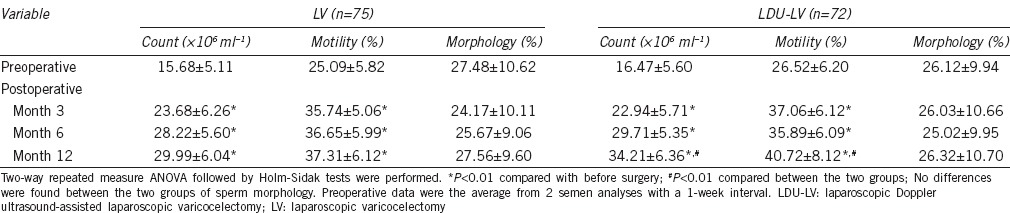
Comparison of the impacts on semen parameters
Semen parameters were measured before surgery and at 3, 6, and 12 months after surgery. There were significant improvements in sperm count and motility after surgery in both groups (Table 2). However, no significant changes of sperm morphology were observed (Table 2). The increase in mean sperm count and sperm motility at 12 months after surgery was greater in LDU-LV than LV group (P < 0.01 for sperm count; P < 0.01 for sperm motility, Table 2).
Table 2.
Pre-and post-operative sperm count/sperm motility/sperm morphology
Spontaneous pregnancy was achieved in 37.3% of the LV group compared to 44.4% of the LDU-LV group, which showed no significant difference (P > 0.05). The mean age of wives who achieved pregnancy was 28.8 ± 3.4 years of age in LV group versus 29.3 ± 4.2 years of age in the LDU-LV group with no significant difference (P > 0.05, Table 1).
DISCUSSION
Precise dissection and preservation of the vessels during suprainguinal laparoscopic varicocelectomy are challengeable due to the complex and adjacent relationship between internal spermatic veins and arteries. Identification of ISAs usually depends on pulsatile movement or evidence of antegrade. However, reasons such as anatomical structure variations or blood pressure fluctuations may make the identification of ISAs and distinction with ISVs very difficult. Furthermore, aggressive manipulation of the vessels during dissection can lead to spasm, making it even harder to distinguish arteries from veins. In the present study, LDU-assisted LV was performed to identify ISAs precisely as expected. The possibility of missing ISVs in division was minimized; even the small periarterial vena comitans that were too tiny to be grasped by conventional laparoscopic instruments were easily dissected and divided. The low recurrent rate in LDU-LV group (1/72) proved that LDU-assisted laparoscopic technique was as effective as the mass ligation LV for the delicate ligating of ISVs.
Nevertheless, with more steps and the use of LDU, the operative time is expected to be longer, which has been proved in our study. More operative time was associated with more efforts to identify vessels, particularly the tiny veins accompanied with the ISAs repeatedly. Similar to microsurgical varicocelectomy, LV was usually performed as an outpatient procedure in other countries; however, in China, most patients preferred to be hospitalized instead of in the clinics. In thirty patients who underwent microsurgical repair in our department, the hospital stay was 4.74 ± 0.81 days, which did not show significant difference with either LDU-LV or conventional LV (P > 0.05).
Currently, microsurgical technique remains the gold-standard procedure for varicocele repair with excellent efficacy rates and low morbidity. However, microsurgical varicocelectomy should be performed by a highly skilled and experienced surgeon to deal with a large number of internal spermatic vessels encountered and the great risks of arterial injury. Nevertheless, this level of skill and experience is not easily achieved among general urologists. With the extensive application of laparoscopic technique, laparoscopic varicocelectomy was widely employed due to the relative shorter operative time for patients, the shorter learning curve for urologists, and a comparable pregnancy rate, which was confirmed by Sami and colleagues who performed an RCT comparing open, laparoscopic and microsurgical approaches of varicocelectomy.19
Previous studies have conflicts regarding the value of preserving the testicular artery in laparoscopic varicocelectomy. Several reports have found a higher rate of persistent or recurrent varicocele when the artery was spared.9,10,20 Conversely, there have been several series reporting no difference in recurrent rate with a loupe-assisted or microsurgical technique, where the testicular artery and lymphatic vessels were preserved.11,21,22 The higher recurrent rate in LV with ISAs preservation may be caused by the failure to isolate small venous channels of ISVs.
Mass ligation of the spermatic vessels allowed for a higher risk of postoperative hydrocele.23 A recent meta-analysis conducted by Liang and colleagues showed that lymphatic sparing LV was associated with a lower incidence of hydrocele formation than lymphatic nonsparing LV.24 Being consistent with the above conclusion, we noted a significant difference of secondary hydrocele formation in LDU-LV group versus LV group. Hydrocele remained one of the common complications of varicocelectomy, and various methods including the use of dye or microsurgery to reduce its occurrence have been suggested. In recent years, with the improvement in laparoscopic equipment and better magnification, the lymphatics can be identified as colorless tubular structures and preserved without dye. We combined the technique reported by Kocvara et al.25 with the application of LDU and were able to identify lymphatics in patients in LDU-LV group without the need of staining. Although most hydroceles resolved spontaneously, postoperative testicular edema induced by lymphatic channel division might lead to decreased testicular function.26 Besides, the increased hydrocele pressure might result in malfunction of spermatogenesis and testicular hypoxia,11 which might be a factor contribute to the decreased sperm count and mobility at 12 months as well as the relative lower pregnancy rate in LV group after surgery compared to LDU-LV group in our study (Table 2).
Testicular atrophy is a rare but dreaded complication of varicocelectomy, especially for approaches above the internal ring-like LV.27 In a retrospective study comparing 41 patients with artery sparing LV and 312 patients with artery ligation LV, no patients experienced testicular atrophy.20 In the current study, we did not found testicular atrophy occurred in either LV or LDU-LV group, suggesting that artery ligation does not compromise the safety of laparoscopic approach, mainly because the interruption of the ISAs above the internal ring would still allow for adequate arterial supply to the testes from the cremasteric or vassal arteries. Nevertheless, there has always been a concern about the blood supply of testes with ISAs ligation during varicocelectomy that may adversely affect the surgical outcomes, especially for those who have had previous inguinal surgery or patients who developed complications after varicocelectomy and required further surgery.20,28,29 There may already be impairments to the collateral supply to the testis for these patients, and the risk of testicular atrophy would be greatly increased.
In agreement with the conclusions of several meta-analyses that indicating varicocele treatment resulted in significant improvement in semen parameters,30,31 we found that sperm counts and sperm motility were improved in both LDU-LV and LV groups. These improvements were observed as early as 3 months postoperatively and were durable at 6–12 months. Moreover, we found that sperm counts and sperm motility in LDU-LV group were significantly higher than LV group at 12 months postoperatively. Excellent preservation of the ISAs and internal spermatic lymphatics in LDU-LV group may contribute to the differences. These findings matched those of previous studies, indicating that patients who underwent artery-preservation LV had better postoperative semen parameters than those who underwent artery-ligation LV.10
Pregnancy is the ultimate goal for infertility patients; thus, we adopted spontaneous pregnancy rate as the primary outcome measure. In our study, with a comparable mean age among females capable of conceiving in both arms, spontaneous pregnancy rate showed no significant difference (37.3% in LV vs 44.4% in LDU-LV) at the end of the 12-month study period. The relative shorter follow-up duration may be one of the reasons for the failure to demonstrate the difference. Similar pregnancy rate (24%–71%) was reported by previous studies,32,33,34 which together with our results support the benefits of varicocele repair in infertile patients.
CONCLUSION
Our results demonstrated that LDU-assisted LV could safely and effectively ligate all spermatic veins, preserve spermatic arteries, and lymphatics without leading to high varicocele recurrence though may consume more operative time. Given the demonstrated benefits of sperm counts as well as sperm motility favoring LDU-LV, we now recommend LDU-LV for the treatment of varicoceles.
AUTHOR CONTRIBUTIONS
MZY and STZ participated in the design of the study. YQL and WDS performed the statistical analysis. LQG and XLZ collected the data, and participated in the design, coordination and drafted the manuscript. All authors read and approved the final manuscript.
COMPETING INTERESTS
None of the authors have conflicts of interest with any people or organization.
ACKNOWLEDGMENTS
We appreciate Chanjuan Zhang for her help in patient allocation and analysis of the data. We also thank Dr. William C. de Groat from the University of Pittsburgh for his assistance in editing the article. This study was supported by the grant from Shandong Province Science and Technology Development Program (2014GSF118079), The Fundamental Research Funds of Shandong University (2014JC03D), and Jinan Clinical Medical Technology Innovation Program (201602147;201602149).
REFERENCES
- 1.Simforoosh N, Ziaee SA, Behjati S, Beygi FM, Arianpoor A, et al. Laparoscopic management of varicocele using bipolar cautery versus open high ligation technique: a randomized, clinical trial. J Laparoendosc Adv Surg Tech A. 2007;17:743–7. doi: 10.1089/lap.2006.0174. [DOI] [PubMed] [Google Scholar]
- 2.Diagnosis and Treatment of Early Melanoma. NIH Consensus Development Conference. 27-29 January, 1992. Consensus statement / NIH Consensus Development Conference. National Institutes of Health Consensus Development Conference. 1992;10:1–25. [PubMed] [Google Scholar]
- 3.Abdel-Meguid TA, Al-Sayyad A, Tayib A, Farsi HM. Does varicocele repair improve male infertility. An evidence-based perspective from a randomized, controlled trial? Eur Urol. 2011;59:455–61. doi: 10.1016/j.eururo.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 4.Nyirady P, Kiss A, Pirot L, Sarkozy S, Bognar Z, et al. Evaluation of 100 laparoscopic varicocele operations with preservation of testicular artery and ligation of collateral vein in children and adolescents. Eur Urol. 2002;42:594–7. doi: 10.1016/s0302-2838(02)00470-0. [DOI] [PubMed] [Google Scholar]
- 5.Matsuda T, Horii Y, Yoshida O. Should the testicular artery be preserved at varicocelectomy? J Urol. 1993;149:1357–60. doi: 10.1016/s0022-5347(17)36391-7. [DOI] [PubMed] [Google Scholar]
- 6.Student V, Zatura F, Scheinar J, Vrtal R, Vrana J. Testicle hemodynamics in patients after laparoscopic varicocelectomy evaluated using color Doppler sonography. Eur Urol. 1998;33:91–3. doi: 10.1159/000019517. [DOI] [PubMed] [Google Scholar]
- 7.Kattan S. The impact of internal spermatic artery ligation during laparoscopic varicocelectomy on recurrence rate and short post operative outcome. Scand J Urol Nephrol. 2001;35:218–21. doi: 10.1080/003655901750291999. [DOI] [PubMed] [Google Scholar]
- 8.Borruto FA, Impellizzeri P, Antonuccio P, Finocchiaro A, Scalfari G, et al. Laparoscopic vs. open varicocelectomy in children and adolescents: review of the recent literature and meta-analysis. J Pediatr Surg. 2010;45:2464–9. doi: 10.1016/j.jpedsurg.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 9.Kim KS, Lee C, Song SH, Cho SJ, Park S, et al. Impact of internal spermatic artery preservation during laparoscopic varicocelectomy on recurrence and the catch-up growth rate in adolescents. J Pediatr Urol. 2014;10:435–40. doi: 10.1016/j.jpurol.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 10.Zampieri N, Zuin V, Corroppolo M, Chironi C, Cervellione RM, et al. Varicocele and adolescents: semen quality after 2 different laparoscopic procedures. J Androl. 2007;28:727–33. doi: 10.2164/jandrol.107.002600. [DOI] [PubMed] [Google Scholar]
- 11.Chung SD, Wu CC, Lin VC, Ho CH, Yang SS, et al. Minilaparoscopic varicocelectomy with preservation of testicular artery and lymphatic vessels by using intracorporeal knot-tying technique: five-year experience. World J Surg. 2011;35:1785–90. doi: 10.1007/s00268-011-1115-6. [DOI] [PubMed] [Google Scholar]
- 12.Fukuda MMF, Nakano Y. Studies on echolaparoscopy. Scan J Gastroenterol. 1982;17:186. [Google Scholar]
- 13.Roayaie S, Jossart G, Gitlitz D, Lamparello P, Hollier L, et al. Laparoscopic release of celiac artery compression syndrome facilitated by laparoscopic ultrasound scanning to confirm restoration of flow. J Vasc Surg. 2000;32:814–7. doi: 10.1067/mva.2000.107574. [DOI] [PubMed] [Google Scholar]
- 14.Neff M, Cantor B, Koren J, Geis WP, Curtiss S, et al. Application of Doppler technology as an aid in identifying vascular structures during laparoscopy. JSLS. 2004;8:259–61. [PMC free article] [PubMed] [Google Scholar]
- 15.Guo L, Sun W, Shao G, Song H, Ge N, et al. Outcomes of microscopic subinguinal varicocelectomy with and without the assistance of Doppler ultrasound: a randomized clinical trial. Urology. 2015;86:922–8. doi: 10.1016/j.urology.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 16.Dubin L, Amelar RD. Varicocele size and results of varicocelectomy in selected subfertile men with varicocele. Fertil Steril. 1970;21:606–9. doi: 10.1016/s0015-0282(16)37684-1. [DOI] [PubMed] [Google Scholar]
- 17.Cina A, Minnetti M, Pirronti T, Vittoria Spampinato M, Canade A, et al. Sonographic quantitative evaluation of scrotal veins in healthy subjects: normative values and implications for the diagnosis of varicocele. Eur Urol. 2006;50:345–50. doi: 10.1016/j.eururo.2006.02.055. [DOI] [PubMed] [Google Scholar]
- 18.Cayan S, Shavakhabov S, Kadioglu A. Treatment of palpable varicocele in infertile men: a meta-analysis to define the best technique. J Androl. 2009;30:33–40. doi: 10.2164/jandrol.108.005967. [DOI] [PubMed] [Google Scholar]
- 19.Al-Said S, Al-Naimi A, Al-Ansari A, Younis N, Shamsodini A, et al. Varicocelectomy for male infertility: a comparative study of open, laparoscopic and microsurgical approaches. J Urol. 2008;180:266–70. doi: 10.1016/j.juro.2008.03.050. [DOI] [PubMed] [Google Scholar]
- 20.Fast AM, Deibert CM, Van Batavia JP, Nees SN, Glassberg KI. Adolescent varicocelectomy: does artery sparing influence recurrence rate and/or catch-up growth? Andrology. 2014;2:159–64. doi: 10.1111/j.2047-2927.2013.00142.x. [DOI] [PubMed] [Google Scholar]
- 21.Goldstein M, Gilbert BR, Dicker AP, Dwosh J, Gnecco C. Microsurgical inguinal varicocelectomy with delivery of the testis: an artery and lymphatic sparing technique. J Urol. 1992;148:1808–11. doi: 10.1016/s0022-5347(17)37035-0. [DOI] [PubMed] [Google Scholar]
- 22.Hsieh ML, Chang PL, Huang ST, Wang TM, Tsui KH. Loupe-assisted high inguinal varicocelectomy for sub-fertile men with varicoceles. Chang Gung Med J. 26:479–84. [PubMed] [Google Scholar]
- 23.Hassan JM, Adams MC, Pope JC, Demarco RT, Brock JW., 3rd Hydrocele formation following laparoscopic varicocelectomy. J Urol. 2006;175:1076–9. doi: 10.1016/S0022-5347(05)00402-7. [DOI] [PubMed] [Google Scholar]
- 24.Liang Z, Guo J, Zhang H, Yang C, Pu J, et al. Lymphatic sparing versus lymphatic non-sparing laparoscopic varicocelectomy in children and adolescents: a systematic review and meta-analysis. Eur J Pediatr Surg. 2011;21:147–53. doi: 10.1055/s-0031-1271733. [DOI] [PubMed] [Google Scholar]
- 25.Kocvara R, Dolezal J, Hampl R, Povysil C, Dvoracek J, et al. Division of lymphatic vessels at varicocelectomy leads to testicular oedema and decline in testicular function according to the LH-RH analogue stimulation test. Eur Urol. 2003;43:430–5. doi: 10.1016/s0302-2838(03)00051-4. [DOI] [PubMed] [Google Scholar]
- 26.Kocvara R. Division of lymphatic vessels at varicocelectomy leads to testicular oedema and decline in testicular function according to the LH-RH analogue stimulation test. Eur Urol. 2003;43:430–5. doi: 10.1016/s0302-2838(03)00051-4. [DOI] [PubMed] [Google Scholar]
- 27.Diamond D. Adolescent versus adult varicoceles - How do evaluation and management differ? J Urol. 2009;181:2418–9. doi: 10.1016/j.juro.2009.03.031. [DOI] [PubMed] [Google Scholar]
- 28.Barqawi A, Furness P, 3rd, Koyle M. Laparoscopic Palomo varicocelectomy in the adolescent is safe after previous ipsilateral inguinal surgery. BJU Int. 2002;89:269–72. doi: 10.1046/j.1464-4096.2001.01623.x. [DOI] [PubMed] [Google Scholar]
- 29.Woldu SL, Van Batavia JP, Poon SA, Raimondi PM, Glassberg KI. Is adolescent varicocelectomy safe after previous inguinal surgery? J Urol. 2010;184:1716–21. doi: 10.1016/j.juro.2010.03.123. [DOI] [PubMed] [Google Scholar]
- 30.Baazeem A, Belzile E, Ciampi A, Dohle G, Jarvi K, et al. Varicocele and male factor infertility treatment: a new meta-analysis and review of the role of varicocele repair. Eur Urol. 2011;60:796–808. doi: 10.1016/j.eururo.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 31.Schauer I, Madersbacher S, Jost R, Hubner WA, Imhof M. The impact of varicocelectomy on sperm parameters: a meta-analysis. J Urol. 2012;187:1540–7. doi: 10.1016/j.juro.2011.12.084. [DOI] [PubMed] [Google Scholar]
- 32.Al-Kandari AM, Shabaan H, Ibrahim HM, Elshebiny YH, Shokeir AA. Comparison of outcomes of different varicocelectomy techniques: open inguinal, laparoscopic, and subinguinal microscopic varicocelectomy: a randomized clinical trial. Urology. 2007;69:417–20. doi: 10.1016/j.urology.2007.01.057. [DOI] [PubMed] [Google Scholar]
- 33.Vermeulen A, Vandeweghe M, Deslypere JP. Prognosis of subfertility in men with corrected or uncorrected varicocele. J Androl. 1986;7:147–55. doi: 10.1002/j.1939-4640.1986.tb00899.x. [DOI] [PubMed] [Google Scholar]
- 34.Lund L, Larsen SB. A follow-up study of semen quality and fertility in men with varicocele testis and in control subjects. Br J Urol. 1998;82:682–6. doi: 10.1046/j.1464-410x.1998.00850.x. [DOI] [PubMed] [Google Scholar]


