Abstract
Background
Proximal femoral nail anti-rotation (PFNA) is a standard femoral intertrochanteric fracture operation. Iatrogenic vascular injury, although uncommon, is a reported complication of PFNA surgery as well as a complication of hip fracture surgery. This study aimed to compare the safety and best use of the distal locking screw in 170 mm PFNA and 240 mm PFNA devices, and to determine the safe region for placement of the distal locking screw in PFNA surgery.
Material/Methods
A retrospective analysis of 100 patients with 170 mm PFNA and 80 patients with 240 mm PFNA were retrospectively analyzed. Two levels of PFNA distal locking screws were equally divided into three planes: I, II, III, for 170 mm PFNA devices and i, ii, iii for the 240 mm PRNA devices. The medial half of the femur was equally divided into eight regions: A to H. The distance between the outer femur and the superficial, the deep and the perforating femoral arteries (SFAs, DFAs, and PFAs), and angles between the reference line and the connection line between the femur center to each artery were measured.
Results
SFAs and DFAs but not PFAs were found in risky or hazardous regions, and DFAs were obviously closer to the femur than SFAs and PFAs at the same level. In the region within 10 mm of the femur, no SFAs were found. The short nails (170 mm PFNA-II devices) were the closest to the DFAs region, indicating that the 170 mm PFNA-II nails are most likely to cause special vessel injury. The short nails were relatively more distant from the SFAs, which were located posteriorly to the long nails (240 mm PFNA-II).
Conclusions
The distal locking screw of the 170 mm PFNA device was more prone to damage the femoral deep artery when the two types of PFNA devices are compared in patients who were candidates for both types of devices.
MeSH Keywords: Bone Screws, Femoral Artery, Femoral Fractures, Safety
Background
As the percentage of older people and people with osteoporosis increases each year, more elderly people will be at risk of intertrochanteric hip fractures [1]. Intertrochanteric hip fractures increase the risk of morbidity and mortality. Many surgical options are used to treatment hip fractures. But for now, interlocked intramedullary nailing, especially proximal femoral nail anti-rotation (PFNA), is considered the ideal method to treat intertrochanteric fracture. A meta-analysis of current evidence indicates that PFNA may be a better choice than dynamic hop screw (DHS) procedures in the treatment of intertrochanteric fractures [2]. PFNA is a commonly performed procedure for internal fixation of intertrochanteric femoral fractures. And unfortunately, iatrogenic pseudo aneurysms are a regularly reported complication of a femoral intramedullary nail [3], with a reported rate of 0.2% [4]. Pseudo aneurysm and intramuscular hematoma are limb- and life-threatening [5]. Pseudo aneurysms most commonly involve the deep femoral artery, (DFA) likely related to its close relationship to the femur in the subtrochanteric region [6]. Iatrogenic injury to the profunda femoris artery or one of its branches and resultant pseudo aneurysm formation has also been documented. To the best of our knowledge, there has been only one study about the relationship between the distal screw placement and the femoral artery. The short nails (200 mm PFNA-II) most likely cause DFAs injuries, and the long nails (300 mm PFNA-II) seem less likely to cause vascular trauma [7]. There are no published studies that have looked at the relationship between profunda femoris arteries and distal screws of different short nails. Our study aimed to compare the artery-based security of 170 mm PFNA-II and 240 mm PFNA-II in a Chinese population, as choosing an appropriate length for PFNA-II can prevent vascular injuries during surgery.
In this study, we measured the range of the distal locking screw of 170 mm PFNA-II and 240 mm PFNA-II using plain radiography. We analyze the relationship between profunda femoris artery (PFA) and the femur and we measured the screw ranges with computed tomography angiography (CTA).
Material and Methods
We obtained the consent of the institutional review board. Retrospective studies included postoperative plain radiography of femoral intertrochanteric fractures with 170 mm PFNA-II or 240 mm PFNA-II devices from January 2012 to December 2014. The study protocol and amendments were approved by local institutional review boards. All participants provided written informed consent prior to participation. Inclusive criteria included: 1) intact lesser trochanter without injury, and 2) the affected limb had no history of fractures. Patients with lower limb deformities were excluded. One hundred patients were enrolled who had 170 mm PFNA-II device surgery. There were 48 male and 52 female patients (52% females), with the mean age of 72.4 years old (range 55–83 years), with an average height of 172 cm (range 153–190 cm). Eighty patients were enrolled who had 240 mm PFNA-II device surgery (45 male and 35 female patients (43.75% females), with the mean age of 62.4 years old (range 24–73 years), with an average height of 175 cm (range 165–187 cm). The distance from the lesser trochanter to the tip of distal locking screw was measured. The distance for the 170 mm PFNA-II device was recorded as D1, and the distance for the 240 mm PFNA-II devise was recorded as D2. The anteverted angle of the femoral neck was also measured.
Thirty patients (15 female and 15 male patients) who underwent lower extremity CTA for evaluation of vascular diseases from January 2012 to December 2014 were included in this study. The average age, weight, and height of all patients were: 68.9 years old (range 63–74 years), 62.7 kg (range 53–80 kg) and 158.9 cm (range 150–170 cm). Those with suspicious lower extremity deformity, vascular diseases of the profunda femoral artery, or fracture history were excluded.
CTA examination was performed using the 16-slice CT scanner (SOMATOM Perspective 16, Siemens Inc., New York, USA) with the standard algorithm using a high-speed scan mode (120.0 kV, 348 mA). Then the CTA radiology images were reformatted at 5 mm intervals in regular axial plane, and final 3-dimensional reconstructions image from the set of the axial source images were performed by utilizing the standard workstation (Siemens Inc., New York, USA). Lower extremity CTA radiology image data were acquired by the GE Medical Systems/Light Speed VCT (Siemens Inc., New York, USA) with the same scanning parameters: voltage 120 Kv, electricity 264 mA, image resolution 0.4 mm/pixel and reconstruction interval 0.625 mm. The images were transmitted to personal graphics workstation in DICOM format through PACS after being produced with a standard algorithm.
The regions of D1 were divided into three levels from I to III, those of D2 were divided into three levels from i to iii (Figure 1). The medial half of femur was divided into ten sections according to the specified angle. Three arcs are made at the same distance from the outer border of the prescribed femur: 1 cm, 2 cm, and 3 cm. At each level, the position of the DFA was evaluated (Figure 2).
Figure 1.
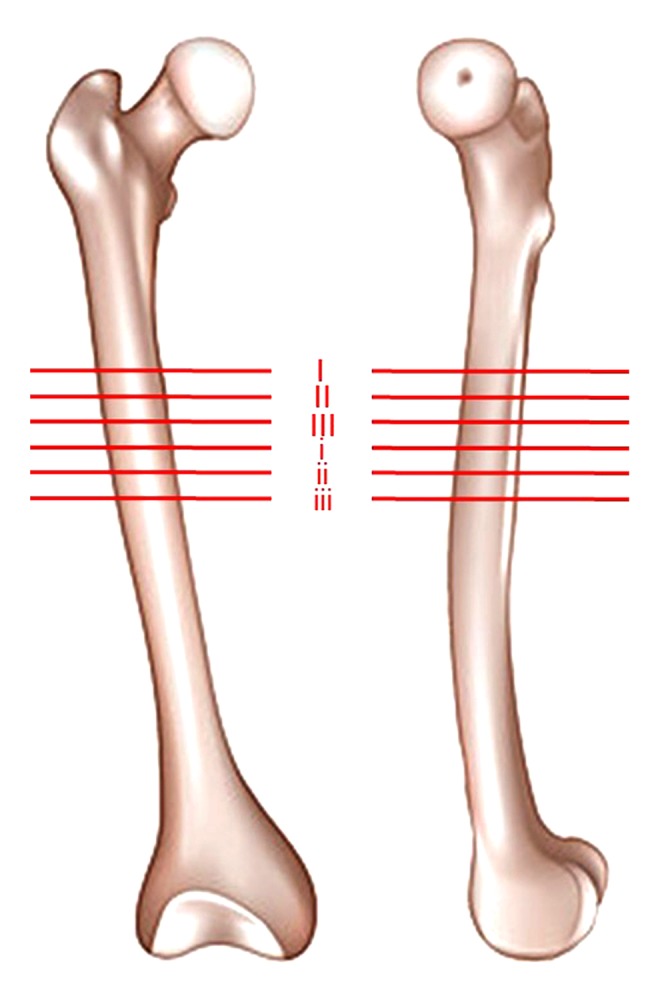
The possible area of distal screw placement was divided into six levels in antero-posterior view and lateral view. The distance from the lesser trochanter to the levels I, II, III, i, ii, and iii’ was 75 mm, 80 mm, 90 mm, 100 mm, 110 mm, and 120 mm, respectively.
Figure 2.
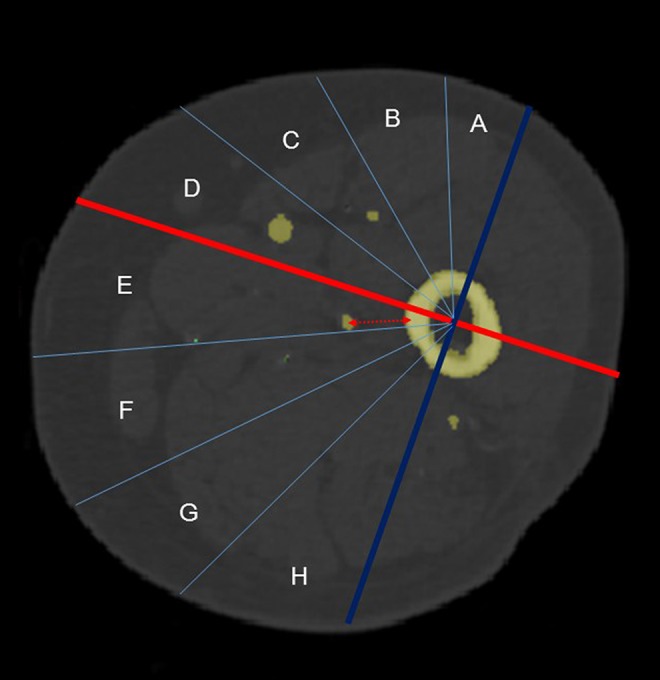
Sectional view of the femur illustrating the measurement of the length from the femur to the deep femoral artery. Medial half of the femur was divided into eight sections. Each section was assigned a letter from A to H, from anterior to posterior.
Results
The region of distance from the lesser trochanter to the tip of distal locking screw was 70–90 mm for the 170 mm PFNA-II devices and for the 240 mm PFNA-II devices, it was 100–120 mm. So the three levels I, II and III were 70 mm, 80 mm, and 90 mm, respectively. The three levels i, ii, and iii were 100 mm, 110 mm, and 120 mm, respectively. For the 170 mm PFNA-II devices, the DFA was positioned at D–G. For 240 mm PFNA-II devices, the DFA was positioned at E–H. There were 27/90 DFAs in the hazardous area for 170 mm PFNA-II devices and there were 10/90 DFAs in the hazardous area for 240 mm PFNA-II devices. The difference was statistically significant (p<0.05). For the three levels I, II, and III, the quantitative proportion of DFAs in the hazardous area was 13/30, 9/30, and 5/30, respectively. For the three levels i, ii, and iii’, the quantitative proportion of DFAs in the hazardous area was 6/30, 3/30, and 1/30, respectively. Statistically significant differences between these levels was found (p<0.05).
We experienced two cases with a deep femoral artery pseudo aneurysm in the locking screw position after insertion of the 170 mm PFNA-II device (Synthes, Solothurn, Switzerland). In one case, pseudo aneurysm presented one week following surgery as a result of gradual erosion from a protruding distal interlocking screw, resulting in compartment syndrome after one month. The major cause of false aneurysms was over penetration of the drill bit or irritation of protruding distal interlocking screw.
A 50-year-old woman presented to the emergency department with an intertrochanteric fracture (Figure 3). After relevant inspection, surgery was performed using a PFNA-II device (within two days of admission). The operation went smoothly, without intraoperative complications. About a week later, her upper and inner fractured thigh began to swell and was suddenly very painful. After positive treatment, her pain was reduced gradually. But just over a month later, again swelling of the involved limb was extremely significance with needle-like pain. This would likely have led to thigh compartment syndrome if left untreated. CTA identified a 4×4 cm pseudo aneurysm of the profunda femoral artery at the level of the locking screw that demonstrated the tip of the distal locking screw penetrating the swollen area. This finding was also confirmed by using medical ultrasonic Doppler imaging. The distal locking screw was noted to be longer than was necessary. We took immediate action, for example, we used surgical debridement to eliminate hematomas and necrotic muscle tissue, resectioned the aneurysm and ligated the profunda femoral artery, and most critically, reset the distal locking screw. The swelling of the mid-thigh shrank with time. The patient recovered well after surgery and was discharged about one month after surgery.
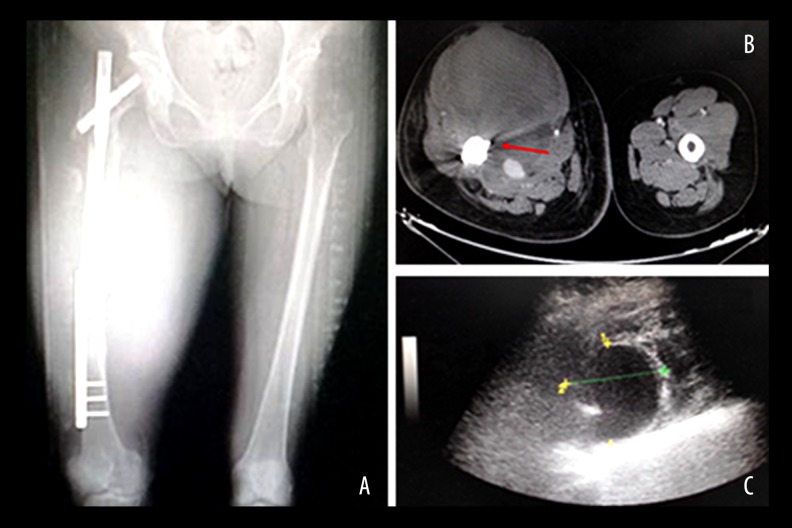
Figure 3.
A week after operation, the upper and inner fracture thigh of a 50-year-old woman with an intertrochanteric fracture became swollen and suddenly very painful. CT and Doppler ultrasonic imaging revealed that profunda femoris artery hemangioma was the cause of the swelling and pain.
In another case, an 81-year-old lean man suffering from femoral intertrochanteric fracture underwent an operation on the second day after admission (Figure 4). The operation appeared to go smoothly, however, the patient noticed immediate postoperative pain and swelling. His hemoglobin dropped from 128 g/L preoperatively to 86 g/L postoperatively, and progressively declined to 68 g/L on the third postoperative day. The perimeter of the affected proximal thigh was 10 cm longer than that of unaffected (normal) thigh. After a blood transfusion, his hemoglobin rose to 10 g/L. Medical ultrasonic Doppler imaging revealed that a profunda femoris artery hemangioma was the cause of the swelling and pain. Based on our experience, we concluded the pseudo aneurysm was caused by the deep drill bit. The patient refused further medical examination and treatment. Fortunately, the size of the lump (hemangioma) was no longer expanding. So the patient’s condition became stable afterwards, and the swelling did not re-accumulate. The patient was discharged from the hospital. On day 23 his general condition deteriorated.
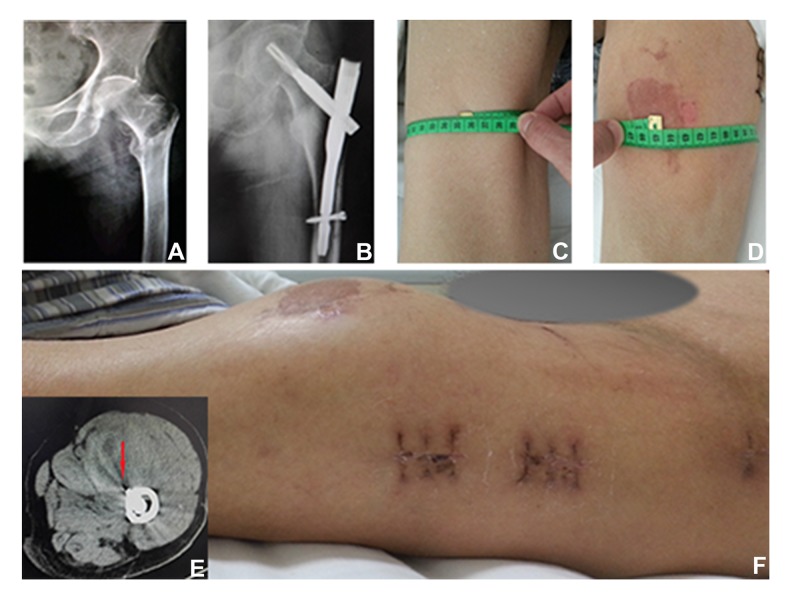
Figure 4.
An 81-year-old lean man with intertrochanteric fracture suffered immediate postoperative pain and swelling. CT revealed a profunda femoris artery hemangioma was the cause of the swelling and pain.
Discussion
DFAs arise at the posterolateral aspect of the femoral artery, starting anteromedially and then posteriorly to the femoral shaft. It runs down the thigh closer to the femur than the femoral artery. In femoral intertrochanteric fractures, PFNA-II devices have been generally used in the Asian population. Although PFNA-II devices have a reliable clinical effect, reports of pseudo aneurysm of the DFA are not rare. It was first reported in 1964 [8]. PFNA devices vary in average length from 18 cm to 24 cm, and the level of the interlocking holes of short Asian-type hip nails are generally close to the third hole and the fourth hole in the side plate with sliding hip screws [9]. The level of the interlocking holes in short Asian-type hip nails and standard nails are quite different. Thus, the longer the hip nails, the lower the risk from the distal interlocking holes. In general, selection of different lengths depends on the location and severity of the trochanteric fracture.
The screw blade of PFNA devices are located in the center of the femoral neck in lateral projection, so the entry angle of the distal screw is the equivalent of the anteverted angle of the femoral neck. When the profunda femoris artery is in the angle range, called dangerous angle, it is more easily destroyed.
Iatrogenic profunda femoris artery injury is usually caused by excessive length of the distal screws, over penetration of a drill bit, or inadvertent deep placement of retractors or clamps. Different occurrence time of symptoms is often a result of the type of arterial injury repair mechanisms. The appearance time of symptoms can be from days to years after PFNA surgery. The onset of symptoms is more acute when the arterial injury is caused by spikes of fractured bone during injury and manipulation, or by over-penetration by a drill bit, retractor, or screw. Delayed onset is usually secondary to arterial wall erosion by constant friction and erosion from a protruding screw, particularly seen in arteries with atherosclerotic plaques. Femoral vessels significantly abut the femur at the levels of interlocking holes when a patient is lean [9]. The internal and adduction rotation of the limb during the procedure may reduce the distance between the femur and artery at the proximal thigh, and the distance increases when there is swelling. The swelling of hip soft-tissue around a trochanteric fracture location could provide a reasonable explanation for pseudo aneurysm after the internal fixation surgery.
The entry angle and the depth of the distal screw must be accurate. In order to reduce the risk of profunda femoral artery injury, the position of the injured limb should be maintained in a neutral position during drilling for an interlocking hole. Using the drill guide and a stop unit is also recommended to prevent over penetration of the drill bit. It is necessary to pay special attention to lean patients. This report stresses the point made by other authors that the screws should be just long enough to penetrate the far cortex, but no longer. The likelihood of iatrogenic injuries may be minimized by using a guarded drill bit, careful tap, correct size of screws, and careful placement of retractors and clamps during surgery [10].
Conclusion
The distal locking screw of 170 mm PFNA device was found to be more prone to damage the femoral deep artery when comparing 120 mm PFNA devices and 170 mm PFNA devices in patient cases where both sizes devices were options. So when you have to use a 170 mm PFNA device, try to make the distal locking nail deeper in order to avoid deep femoral artery injury.
Footnotes
Source of support: This work was supported by the Natural Science Foundation of Shanghai, China (grant no. 14ZR1432600)
Competing interests
The authors declare that they have no competing interests.
References
- 1.Sheehan SE, Shyu JY, Weaver MJ, et al. Proximal femoral fractures: What the orthopedic surgeon wants to know. Radiographics. 2015;35(5):1563–84. doi: 10.1148/rg.2015140301. [DOI] [PubMed] [Google Scholar]
- 2.Zhang K, Zhang S, Yang J, et al. Proximal femoral nail vs. dynamic hip screw in treatment of intertrochanteric fractures: A meta-analysis. Med Sci Monit. 2014;20:1628–33. doi: 10.12659/MSM.890962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bose D, Hauptfleisch J, McNally M. Delayed pseudoaneurysm caused by distal locking screw of a femoral intramedullary nail: A case report. J Orthop Trauma. 2006;20(8):584–86. doi: 10.1097/01.bot.0000245003.83245.58. [DOI] [PubMed] [Google Scholar]
- 4.Lazarides MK, Arvanitis DP, Dayantas JN. Iatrogenic arterial trauma associated with hip joint surgery: An overview. Eur J Vasc Surg. 1991;5(5):549–56. doi: 10.1016/s0950-821x(05)80343-3. [DOI] [PubMed] [Google Scholar]
- 5.Chan WS, Kong SW, Sun KW, et al. Pseudoaneurysm and intramuscular haematoma after dynamic hip screw fixation for intertrochanteric femoral fracture: A case report. J Orthop Surg (Hong Kong) 2010;18(2):244–47. doi: 10.1177/230949901001800222. [DOI] [PubMed] [Google Scholar]
- 6.Rajaesparan K, Amin A, Arora S, et al. Pseudoaneurysm of a branch of the profunda femoris artery following distal locking of an intramedullary hip nail: An unusual anatomical location. Hip Int. 2008;18(3):231–35. doi: 10.1177/112070000801800308. [DOI] [PubMed] [Google Scholar]
- 7.Han CD, Lee YH, Yang KH, et al. Relationship between distal screws and femoral arteries in closed hip nailing on computed tomography angiography. Arch Orthop Trauma Surg. 2013;133(3):361–66. doi: 10.1007/s00402-012-1674-5. [DOI] [PubMed] [Google Scholar]
- 8.Wolfgang GL, Barnes WT, Hendricks GJ. False aneurysm of the profunda femoris artery resulting from nail-plate fixation of intertrochanteric fracture. A case report and review of the literature. Clin Orthop Relat Res. 1974;(100):143–50. [PubMed] [Google Scholar]
- 9.Yang KH, Park HW, Park SJ. Pseudoaneurysm of the superficial femoral artery after closed hip nailing with a Gamma nail: Report of a case. J Orthop Trauma. 2002;16(2):124–27. doi: 10.1097/00005131-200202000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Fordyce A. False aneurysm of the profunda femoris artery following nail and plate fixation of an intertrochanteric fracture. Report of a case. J Bone Joint Surg Br. 1968;50(1):141–43. [PubMed] [Google Scholar]