Abstract
The molecular and cellular mechanisms underlying plaque destabilization remain obscure. We sought to elucidate the correlation between NO, H2S and CO-generating enzymes, nitro-oxidative stress and plaque stability in carotid arteries. Carotid atherosclerotic plaques were collected from 62 patients who had undergone endarterectomy due to internal artery stenosis. Following histological evaluation the plaques were divided into stable and unstable ones. To investigate the impact of simvastatin we divided patients with stable plaques, into those receiving and to those not receiving simvastatin. Expression and/or levels of p-eNOS/eNOS, pAkt/t-Akt, iNOS, cystathionine beta synthase (CBS), cystathionine gamma lyase (CSE), heme oxygenase-1(HO-1), soluble guanyl cyclase sGCα1, sGCβ1, NOX-4 and HIF-1α were evaluated. Oxidative stress biomarkers malondialdehyde (MDA) and nitrotyrosine (NT) were measured. NT levels were decreased in stable plaques with a concomitant increase of eNOS phosphorylation and expression and Akt activation compared to unstable lesions. An increase in HIF-1α, NOX-4, HO-1, iNOS, CBS and CSE expression was observed only in unstable plaques. 78% of patients under simvastatin were diagnosed with stable plaques whereas 23% of those not receiving simvastatin exhibited unstable plaques. Simvastatin decreased iNOS, HO-1, HIF-1α and CSE whilst it increased eNOS phosphorylation. In conclusion, enhanced eNOS and reduced iNOS and NOX-4 were observed in stable plaques; CBS and CSE positively correlated with plaque vulnerability. Simvastatin, besides its known effect on eNOS upregulation, reduced the HIF-1α and its downstream targets. The observed changes might be useful in developing biomarkers of plaque stability or could be targets for pharmacothepary against plaque vulnerability.
Keywords: Carotid plaques, Nitro-oxidative stress, Nitric oxide, Hydrogen sulfide, Heme oxygenase-1
1. Introduction
The presence of atherosclerotic disease in the carotid arteries creates a significant risk for cerebrovascular events, with reported annual ischemic stroke rates ranging from 0.35% to 1.3% in asymptomatic patients with moderate stenosis [1] and from 0.5% to approximately 5% for severe asymptomatic carotid artery stenosis [2]. Around 20% of ischemic strokes appear to originate from carotid plaques [3]. Understanding of atherosclerosis progression and characterization of the role of plaque instability in the pathogenesis of acute ischemic syndromes have been major goals of cardiovascular research during the previous decades. However, the complex molecular and cellular mechanisms underlying plaque destabilization remain largely obscure, and the distinct mechanism through which stabilization of atheroma is achieved is still under investigation [4].
Nitro-oxidative stress, characterized by overproduction of reactive oxygen (ROS) and nitrogen (RNS) species, with a concomitant endothelial dysregulation being manifested through the impairment of nitric oxide (NO) homeostasis, are key factors for plaque formation and instability. Increased expressions of enzymes that promote ROS production, such as NADPH oxidases (NOX), contribute to atherosclerosis. Additionally, upregulation or activation of pro-survival kinases such as protein kinase B (PKB/Akt) or endogenous antioxidant mechanisms, can lead to improved atherosclerotic lesion stability and prognosis in various in vivo models and in clinical trials. However the elucidation of the actual mechanism of the above findings is still under investigation [5].
In addition to NO, studies have revealed another two gasotransmitters, namely hydrogen sulfide (H2S) and carbon monoxide (CO), to be vital signaling molecules in vascular cells, contributing to the protection of the cardiovascular system through activation of various antiapoptotic and antioxidant pathways [6]. NO is produced in most of the mammalian tissues and cells by both enzymic [neuronal nitric oxide sythase (nNOS), endothelial nitric oxide synthase (eNOS), inducible nitric oxide synthase (iNOS)] and non-enzymic reactions (reduction of nitrite/nitrate from dietary and endogenous sources) [6]. H2S is generated from cysteine by cystathionine β-synthase (CBS), cystathionine γ-lyase (CSE) and 3-mercaptopyruvate sulphurtransferase (3-MST) [7], [8], [9]. Reduced levels of H2S have been linked with various cardiovascular disease states that are associated with endothelial dysfunction, including atherosclerosis [10]. Endogenous CO is liberated from heme oxygenases (HO-1 and HO-2) as a result of heme degradation, which along with biliverdin that is rapidly reduced to bilirubin, exhibit antioxidant properties [6]. However, although some information on the role of endogenous NO in atherosclerotic plaques is available [11], the effects of endogenous CO and H2S on plaque stability remain obscure.
To date, several population-based preventive programs aimed at cardiovascular risk reduction were able to substantially abate cardiovascular morbidity and mortality; most importantly the introduction of statin therapy was able to reduce cardiovascular mortality by over one-third [12]. Besides their hypolipidaemic activity, it is already proven that statins exhibit pleiotropic activities, with anti-inflammatory, antioxidant and anti-thrombotic properties being well established [13]. While it is already shown that statins can improve NO homeostasis through upregulation and activation of eNOS and can induce plaque stabilization in patients, the actual underlying mechanism and their effect on the enzymes that generate H2S and CO has not been accessed [14].
Considering the translational importance of understanding and targeting the underlying signaling cascade responsible for atheroma stability, we sought to investigate the intraplaquely interplay between NO, H2S and CO generation enzymes and associate their expression with biomarkers and signaling molecules of nitro-oxidative stress. Moreover, we investigated the effect of simvastatin on plaque stability and unraveled the possible underlying mechanisms of protection.
2. Materials and methods
2.1. Tissue collection
Since 2015, carotid plaques were prospectively collected from 62 random patients, who had internal carotid artery stenosis 70% and underwent carotid endarterectomy. Extent demographic and clinical data, medication, risk factors, and vascular comorbidities were recorded (Table 1). Neurological evaluation of all patients was performed preoperatively in order to classify them as symptomatic (presence of stroke, brain infarcts, transient ischemic attacks and amaurosis fugax) and asymptomatic. Arteriographical evaluation of the carotid bifurcation stenosis was performed in all patients for this study. Degree of luminal stenosis was determined according to North American Symptomatic Carotid Endarterectomy Trial (NASCET) criteria [15]. Based on these measurements, stenotic lesions were divided into two groups, namely asymptomatic patients with stable plaques (stable), and symptomatic patients with unstable plaques (unstable). Moreover according to whether patients were under simvastatin administration or not, patients were divided in four subgroups, namely asymptomatic patients with stable plaques under simvastatin therapy (s/st), asymptomatic patients with stable plaques not receiving simvastatin (s/nost), symptomatic patients with unstable plaques under simvastatin therapy (u/st) and symptomatic patients with unstable plaques not receiving simvastatin (u/nost). The present study has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki). The study protocol was approved by the Institutional Ethics Committee and all patients enrolled gave their informed consensus.
Table 1.
Clinical and Demographic Data collected from patients, who underwent endoartetectomy.
| Patients: | Overall | Simvastatin Therapy | Non simvastatin therapy (non statin) |
|---|---|---|---|
| Demographic data | |||
| No | 62 | 31 | 31 |
| Mean age (range) | 71.05 (55–85) | 71 | 71.06 |
| Male /female | 48/14 | 28/7 | 20/7 |
| Smoking | 40 | 19 | 21 |
| (current/past smokers) | 26/14 | 10/9 | 12/9 |
| Clinical data | |||
| Hypertension | 58 | 31 | 27 |
| Diabetes | 23 | 15 | 8 |
| Hyperlipidemia | 42 | 31 | 11 |
| Ischemic heart disease | 38 | 30 | 8 |
| Aneurysm | 3 | 2 | 1 |
| Peripheral arterial occlusive disease | 24 | 18 | 6 |
| Clinical symptoms | 31 | 9 | 22 |
| Stroke | 12 | 4 | 8 |
| TIA | 11 | 1 | |
| Amaurosis fugax | 8 | 4 | 4 |
| Angiographic carotic stenosis | |||
| <90% | 24 | 10 | 14 |
| ≥90 | 38 | 18 | 20 |
| Plaque histopathology status | |||
| Unstable | 33 | 11 | 22 |
| Stable | 29 | 20 | 9 |
| Medications | |||
| Antiplatelets | 57 | 31 | 26 |
| ACE inhibitors | 30 | 14 | 16 |
| b-blockers | 28 | 18 | 10 |
2.2. Tissue preparation
All carotid plaque specimens were removed in the operating room and were divided into two parts. One part was fixed immediately in 10% neutral-buffered solution with 4% formaldehyde for 24 h, and embedded in paraffin. The second portion was immediately stored at −80 °C for further analysis of malondialdehyde (MDA), nitrotyrosine (NT), immunohistochemical and immunoblotting analysis.
2.3. Histology
Hematoxylin and eosin staining was performed for histological evaluation of the specimens. Two pathologists, blinded to the clinical data, examined each specimen to assess atheromatous plaque morphology, using the American Heart Association classification of atherosclerotic plaques [16]. According to this classification, carotid plaques were assigned as fibroatherotic (type V) and complicated unstable (intraplaque hemorrhage, ulcer, or thrombus) (type VI).
2.4. Immunohistochemistry
-
a.
Antibodies: For immunohistochemical analysis the following antibodies were used: anti-eNOS (6H2) mouse monoclonal antibody at a 1:100 dilution (Cell Signaling Technology, Beverly, MA, USA), anti- NOX4 (IgG rabbit polyclonal; epitope: a synthetic peptide made to an internal region of the human NOX4 protein (between residues 100–200)) at a 1:50 dilution (Novus-Biologicals, Europe), anti iNOS (Ab-1) (IgG rabbit polyclonal; epitope: purified enzyme from mouse macrophages (RAW 264.7) cells) in dilution 1:100 (Cayman Chemicals, Lab Supplies Greece).
-
b.
Method: Immunohistochemistry was performed according to the indirect streptavidin-biotin-peroxidase method. In brief, 5 µm paraffin sections were placed on poly-L-lysine-coated slides, dewaxed, rehydrated and incubated for 30 min with 0.3% hydrogen peroxide to quench the endogenous peroxidase activity. Unmasking of the related proteins was carried out. The sections were incubated with the primary antibody at 4 °C overnight. Biotin-conjugated secondary antibody was added at 1:200 dilutions for 1 h at room temperature (RT). The next stage comprised 30 min incubation in StreptAB Complex (1:100 stock biotin solution, 1:100 stock streptavidin-hyperoxidase solution) (Dako, Greece). For color development we used 3,3′-diaminobenzidine tetrahydrochloride (DAB, Sigma-Hellas, Greece) and hematoxylin as a counterstain.
-
c.
Evaluation: The staining pattern was considered positive only if cytoplasmic signal was discerned. Images were obtained with a Zeiss-Axiolab microscope (Carl Zeiss GmbH, Germany), employing video analysis software as previously described [17]. We used 8 samples of each group for immunohistochemical analysis.
2.5. Western blot analysis
Tissues from the atherosclerotic plaques were pulverized and the powder was homogenized in lysis buffer (1% Triton X-100, 20 mM Tris pH 7.4–7.6, 150 mM NaCl, 50 mM NaF, 1 mM EDTA,1 mM EGTA, 1 mM Glycerolphosphatase, 1% SDS, 100 mM PMSF, and 0.1% protease phosphatase inhibitor cocktail). After centrifugation at 11,000g for 15 min at 4 oC, supernatants were used for protein analysis as previously described [18]. Subsequently the following primary antibodies were used: phospho-eNOS (S1177), eNOS, iNOS, p-Akt (S473), Akt, GADPH, β-actin and β-tubulin (Cell Signaling Technology, Beverly, MA, USA), CBS (Abnova, Germany), CSE (Protein Tech Group, Inc., Rosemont, USA), anti-HO-1, HIF-1α (Santa-Cruz, Inc, UK), NOX-4 (Novus-Biologicals, Europe), and sGC α1, sGCβ1 (Abcam, USA). Membranes were then incubated with secondary antibodies for 2 h at room temperature (goat anti-mouse and goat anti-rabbit HRP; Cell Signaling Technology, Beverly, MA, USA) and developed using the GE Healthcare ECL Western Blotting Detection Reagents (Thermo Scientific Technologies, Bioanalytica, Athens, Greece). Relative densitometry was determined using a computerized software package (NIH Image, National Institutes of Health, USA), and ratios HIF-1α/β-tubulin, phospho-eNOS/eNOS, eNOS/β-actin, iNOS/β-actin, phospho-Akt/Akt, Akt/β-αctin, NOX-4/β-actin, sGCα1/β-actin, sGCβ1/β-actin, HO-1/β-actin, CBS/GADPH and CSE/GADPH were used for statistical analysis.
2.6. Measurement of plaque Malondialdehyde (MDA) and Nitrotyrosine (NT)
Human carotid samples were frozen at −80 °C until the assay. On analysis, tissue samples were washed in ice-cold NaCl 0.9%, blotted on absorbent paper, and weighed. Each sample was minced in ice-cold 20 mM Tris-HCl buffer pH 7.4, in a 1:10 wt/volume ratio, and homogenized using a Teflon pestle. After centrifugation at 3000g for 10 min at 4 °C, the supernatant was used for the biochemical assay. MDA concentration was determined spectrophotometrically at 586 nm and expressed in μΜ (Oxford Biomedical Research Colorimetric Assay for lipid peroxidation) with some modifications as previously described [19]. NT, a biomarker of nitrosative stress, was determined by ELISA according to the manufacturers’ instructions (Bioxytech, Nitrotyrosine-EIA; Oxis Research, Beverly Hills, Calif), as we have previously described [19]. The detection limit of the assay was 2 nM. Protein concentration of the supernatants was determined based on the Lowry assay (DC protein assay, BIORAD, UK). Measurements of each group were performed in triplicate.
2.7. Data analysis and statistics
Differences between different study groups were estimated with the unpaired t-test with Welch correction or the Mann-Whitney test/Kruskal-Wallis test (nonparametric analysis of variance) for variables with significant differences in their SDs. All calculations were performed with the GraphPad Prism 4 software (GraphPad Software Inc). Values of p<0.05 were considered statistically significant.
3. Results
3.1. NO, H2S and CO generating enzymes, nitro-oxidative stress and stability of carotid plaques
3.1.1. Nitro-oxidative stress biomarkers and HIF-1α transcription factor are associated with plaque instability
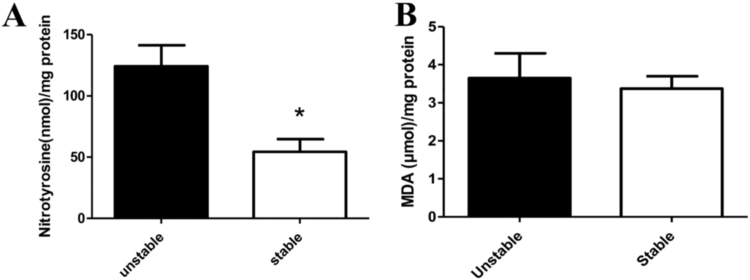
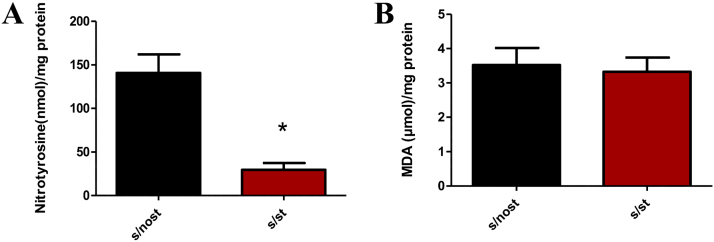
In order to investigate the association of nitro-oxidative stress with plaque stability we measured malondialdehyde (MDA) and nitrotyrosine (NT) levels. We observed that nitrotyrosine was statistically significantly reduced in the stable group (n=25) vs unstable group (n=30) (p<0.05), (Fig. 1A), whilst no change in lipid peroxidation product MDA was observed (Fig. 1B). Hypoxia-inducible factor (HIF)−1α has been shown to positively associate with plaque instability [20], [21], [22]. In line with these observations, we have found that HIF-1α is upregulated in unstable vs stable lesions (p<0.05) (Fig. 2A).
Fig. 1.
Intraplaque nitro-oxidative stress biomarkers: A. Nitrotyrosine levels (nmol/mg protein) of unstable (n=30) and stable groups (n=25), (*p<0.05 vs unstable). B. MDA levels (μΜ/mg protein) of unstable (n=33) and stable groups (n=29) (p=NS).
Fig. 2.
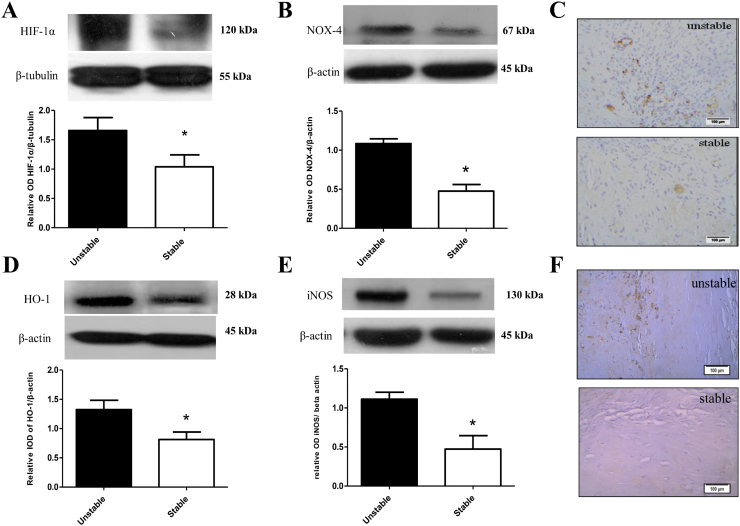
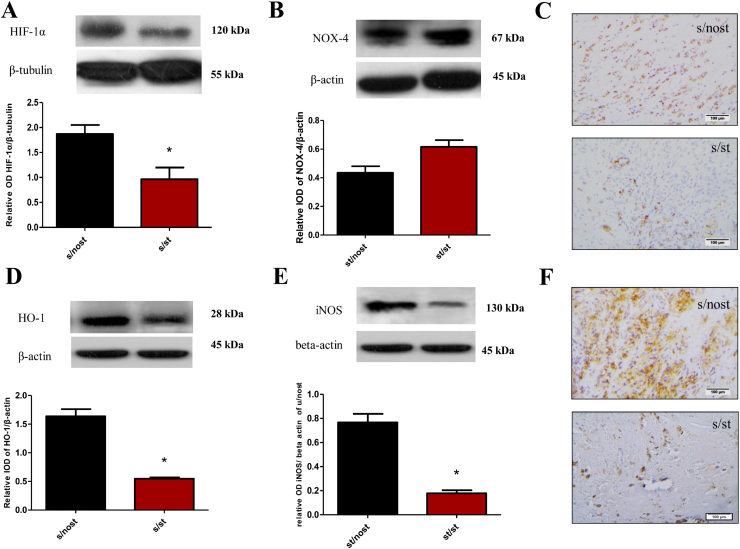
Changes in HIF-1α and its downstream targets NOX-4, HO-1 and iNOS in human atherosclerotic plaques. Representative western blots and relative densitometric analysis of Α. HIF-1α/β-tubulin B. NOX-4/β-actin C. Immunohistochemical (IHC) analysis of NOX-4 in serial sections from stable (n=8) and unstable plaques (n=8) D. HO-1/β-actin E. iNOS/β-actin F. Immunohistochemical (IHC) analysis of iNOS in serial sections from stable (n=8) and unstable plaques (n=8) (*p<0.05 vs Unstable). For IHC purposes, frames in 200x magnification pictures represent the areas of 400x magnification.
3.1.2. NOX-4, HO-1 and iNOS, downstream targets of HIF-1α are differentially expressed in stable vs unstable plaques
HIF-1α is known to upregulate the transcription of a wide variety of genes, including NOX-4, HO-1 and iNOS [23], [24], [25]. NOX-4 mRNA expression is observed under carotid artery injury [26], [27] therefore we initially determined the expression of NOX-4, as nitro-oxidative stress producing enzyme. By using Western blot analysis and immunohistochemistry, we observed that NOX-4 was upregulated in the unstable (n=33) vs stable group (n=29) (p<0.05) (Fig. 2B), contributing to the fact that unstable plaques exhibit increased oxidative stress. Moreover immunohistochemical analysis revealed that NOX-4 was expressed in stromal cells, predominantly in vascular smooth muscle cells (VSMC) and macrophages (Fig. 2C).
Although one of the major enzymes generating CO, heme oxygenase-1 (HO-1) has been implicated in protection against atherogenesis, its role in vulnerable plaques remains to be fully elucidated [28]. Additionally, so far, multiple mechanisms of antioxidant action of HO-1 have been described [29]. We observed a decrease in HO-1 in stable (p<0.05) vs unstable lesions (Fig. 2D). In agreement with previous experimental studies which showed that induction of HO-1 does occur in atherosclerotic lesions, our findings suggest that HO-1 induction may serve to slow the progression or limit the extent of atherosclerosis [30].
iNOS derived peroxynitrite is proven to be a key mediator in atherosclerosis progression as it increases formation of lipid hydroperoxides and nitrosative stress intraplaquely [31]. Our results show that in the stable group, iNOS intraplaque expression is downregulated (p<0.05) vs the unstable group, supporting our idea that plaque stabilization is HIF-1α-dependent (Fig. 2E). Immunohistochemical analysis revealed that iNOS was mainly expressed in VSMC and macrophages (Fig. 2F).
3.1.3. Stable atherosclerotic lesions display an improved profile of NO homeostasis
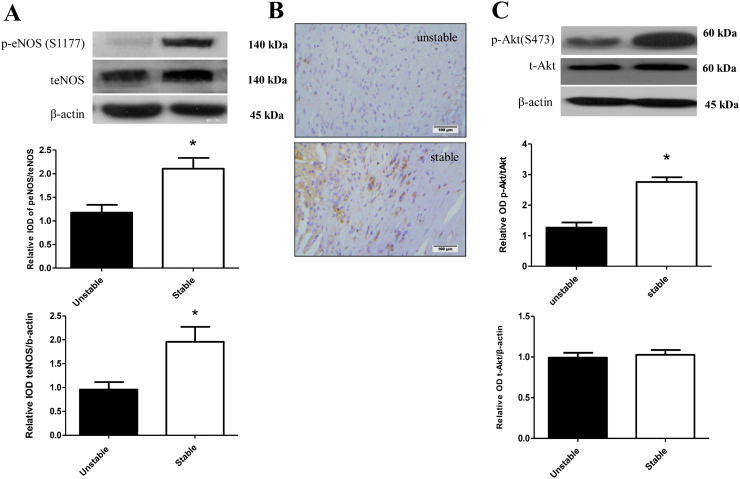
Since endothelial homeostasis is linked to increased eNOS activity while endothelial dysfunction is accompanied by an increase in iNOS expression [32], we determined the phosphorylation and expression of eNOS and iNOS in stable and unstable carotid plaques. We observed that in the stable group (n=29) there is increased phosphorylation of eNOS at Ser1177, the main activator site of the enzyme [33], and upregulated eNOS expression (Fig. 3A). A parallel decrease in iNOS expression was observed in the same group compared to the unstable group (n=29) (p<0.05) (Fig. 2 E and F). Immunohistochemical analysis deduced that eNOS was mainly expressed in endothelial cells and macrophages (Fig. 3B), while iNOS was mainly expressed in VSMC and macrophages (Fig. 2F).
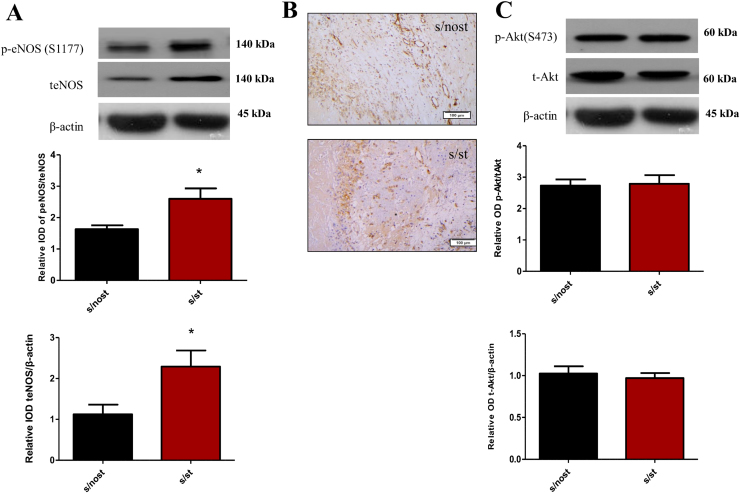
Fig. 3.
eNOS and Akt phosphorylation and expression correlate with atheroma stability. Representative western blots and relative densitometric analysis of Α. p-eNOS/t-eNOS and t-eNOS/β-actin B. Immunohistochemical (IHC) analysis of eNOS in serial sections from stable (n=8) and unstable plaques (n=8). For IHC purposes, frames in 200x magnification pictures represent the areas of 400x magnification. C. p-Akt (S473)/t-Akt and t-Akt/β-actin (*p<0.05 vs Unstable).
3.1.4. Changes in Akt and soluble guanyl cyclase (sGC) expression associated with plaque stability
The serine/threonine kinase Akt, a major upstream activator of eNOS [33], is a multifunctional kinase implicated with a broad range of cellular functions. Studies have shown that absence of Akt1 in atherosclerosis-prone apolipoprotein E (ApoE) knockout mice induce features of plaque vulnerability [34]. We have found that Akt phosphorylation increased significantly in the stable (n=29) vs unstable group (n=33) (p<0.05) (Fig. 3C), whereas Akt expression remains unchanged between the two groups (Fig. 3C). Our findings indicate that stable atherosclerotic lesions are characterized by a favorable biochemical profile consistent with improved endothelial function.
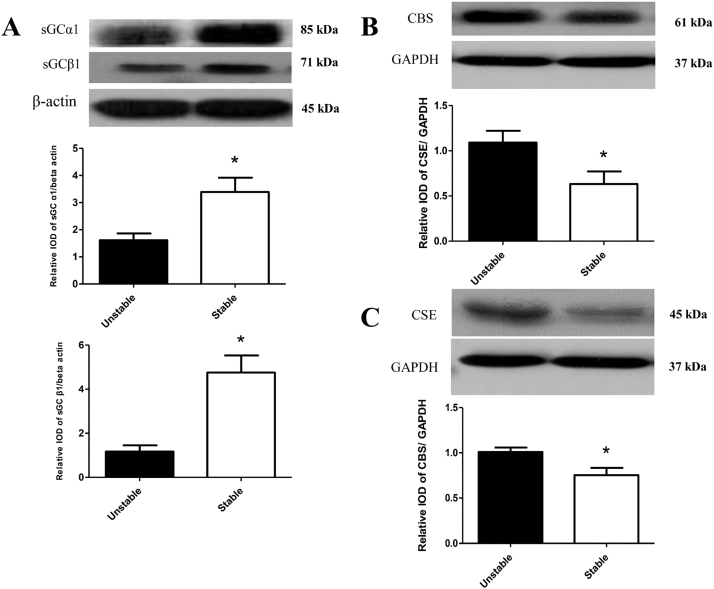
Soluble Guanyl Cyclase(sGC) is a downstream target for endothelium-derived NO and its activation leads to smooth muscle relaxation and improved vascular function [35]. We found that both sGC subunits are upregulated in stable (n=29) vs unstable plaques (n=33) (p<0.05) (Fig. 4A).
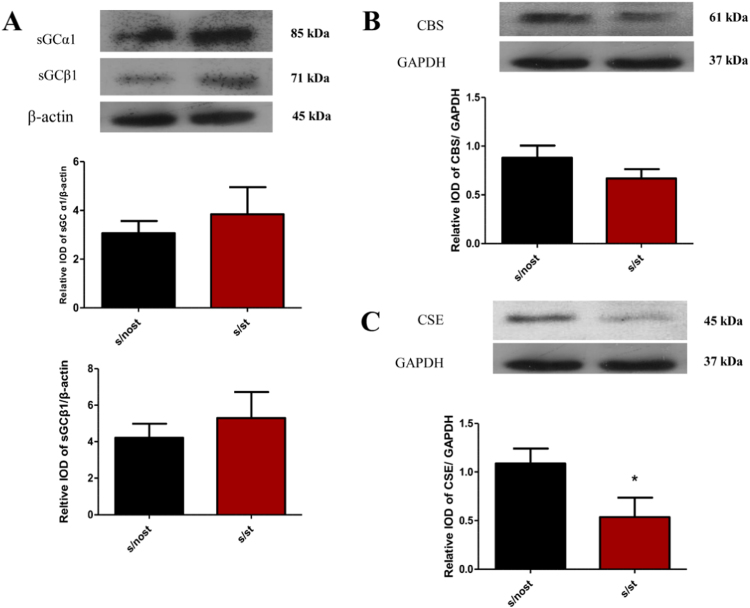
Fig. 4.
sGC subunits, CBS and CSE are upregulated in stable atherosclerotic plaques. Representative western blots and relative densitometric analysis of Α. sGCα1/β-actin and sGCβ1/β-actin B. CBS/GAPDH C. CSE/GAPDH (*p<0.05 vs unstable).
3.1.5. Increased expression of H2S generating enzymes is associated with plaque instability
The role of H2S generating enzymes within atherosclerotic plaques is still unknown. We, thus, sought to investigate the expression of two H2S-generating enzymes that are abundantly expressed in the cardiovascular system, namely CBS and CSE [6]. We observed that the expression of both enzymes is decreased in stable (n=29) vs unstable plaques (n=33) (p<0.05) (Fig. 4 B, C), indicating that increased expression of CBS and CSE might contribute to plaque instability.
3.2. Effects of simvastatin treatment in stable plaques
78% of patients under simvastatin treatment were diagnosed with stable atherosclerotic plaques, whereas 23% of those not receiving simvastatin exhibited unstable plaques. Subsequently we compared atherosclerotic lesions originating from patients with stable plaques, who did not receive simvastatin (or any other statin), with those of patients under simvastatin therapy, in order to investigate the additional protective effects bestowed by simvastatin.
3.2.1. Simvastatin exerts additional antioxidant effects on stable lesions
In order to elucidate any additional mechanism of simvastatin induced atheroma stabilization we assessed the levels of MDA and nitrotyrosine in tissue homogenates. We have found that although simvastatin did not significantly inhibit MDA, it reduced NT levels reflecting the known antioxidant properties of simvastatin (p<0.05) (Fig. 5A and B).
Fig. 5.
Simvastatin treatment exerts antioxidant effects in stable plaques. A. Nitrotyrosine levels (nmol/mg protein) of s/nost (n=9), s/st (n=20) (p<0.05 vs s/nost), B. MDA levels (μΜ/mg protein) of s/nost (n=9), s/st (n=20) (p=NS).
3.2.2. Simvastatin reduces the expression of HIF-1α in stable lesions
As HIF-1α contributes to plaque instability, we sought to evaluate the effect of simvastatin on HIF-1α expression. We observed that HIF-1α levels were reduced in s/st plaques compared to s/nost ones (p<0.05), revealing that HIF-1α represents an important target regulated by simvastatin treatment (Fig. 6A).
Fig. 6.
Simvastatin treatment reduces HIF-1α expression and its downstream targets HO-1 and iNOS promoting atheroma stability. Representative western blots and relative densitometric analysis of Α. HIF-1α/β-tubulin B. NOX-4/β-actin C. Immunohistochemical (IHC) analysis of NOX-4 in serial sections from s/nost (n=8) and s/st (n=8) groups D. HO-1/β-actin E. iNOS/β-actin F. Immunohistochemical (IHC) analysis of iNOS in serial sections from s/nost (n=8) and s/st (n=8) groups. For IHC purposes, frames in 200x magnification pictures represent the areas of 400x magnification.
3.2.3. Simvastatin downregulates HO-1 and iNOS, downstream targets of HIF-1α in stable lesions
Further investigating the effect of simvastatin on HIF-1α’s downstream targets HO-1, NOX-4 and iNOS we have observed that the expression of HO-1 and iNOS (Fig. 6D, E, F) was decreased in s/st group vs s/nost in line with HIF-1α expression (p<0.05). However, NOX-4 expression remained unchanged between groups (p=NS) (Fig. 6B, C).
3.2.4. Simvastatin induces eNOS phosphorylation and expression in stable lesions
Taking under consideration that restoring NO signaling plays a vital role in vascular function and exerts anti-atherosclerotic effects, we investigated the effect of simvastatin on eNOS phosphorylation and expression. We have observed an increase in both eNOS phosphorylation on S1177 and eNOS expression in s/st group (p<0.05), in parallel with reduced iNOS expression (Fig. 7A and B).
Fig. 7.
Simvastatin induces eNOS expression and phosphorylation independently of Akt. Representative western blots and relative densitometric analysis of Α. p-eNOS/t-eNOS and t-eNOS/β-actin B. Immunohistochemical (IHC) analysis of eNOS in serial sections from s/nost (n=8) and s/st (n=8) groups For IHC purposes, frames in 200x magnification pictures represent the areas of 400x magnification. C. p-Akt (S473)/t-Akt and t-Akt/β-actin (*p<0.05 vs s/nost).
3.2.5. Simvastatin does not exert additional effect on Akt phosphorylation and expression or sGC subunit expression in stable lesions
To investigate the upstream and downstream eNOS targets, Akt and sGC respectively, we determined the effect of simvastatin on Akt phosphorylation (S473) and expression (Fig. 7C), as well as the effect of this statin on sGC subunit expression (Fig. 8A). Whilst we had previously observed that both Akt and sGC are upregulated in stable plaques we have found no differences in Akt and sGC regulation between s/nost and s/st groups.
Fig. 8.
Simvastatin downregulates CSE but does not affect expression of CBS and sGC subunits. Representative western blots and relative densitometric analysis of Α. sGCα1/β-actin and sGCβ1/β-actin B. CBS/GAPDH C. CSE/GAPDH (*p<0.05 vs s/nost).
3.2.6. Simvastatin reduces expression of CSE but does not affect CBS expression in stable lesions
Taking under consideration that intraplaque H2S production by CBS and CSE would be associated with increased plaque vulnerability due to the angiogenic properties of H2S [36], we evaluated the effect of simvastatin on the aforementioned enzymes expression. Simvastatin reduced CSE expression in s/st group (p<0.05) while CBS expression remained unchanged (Fig. 8B and C).
To aid the reader in integrating the above-mentioned findings regarding the biochemical changes observed among the different groups studied, a summary of our findings is presented in Table 2.
Table 2.
Summary of biochemical changes in atheromas.
| Unstable | Stable | Stable/no Simvastatin | Stable/Simvstatin | |
|---|---|---|---|---|
| HIF-1α | ↑ | ↓ | ↓ | ↓↓ |
| ΝΟΧ-4 | ↑ | ↓ | ↓ | ↓ |
| ΗΟ-1 | ↑ | ↓ | ↓ | ↓↓ |
| iNOS | ↑ | ↓ | ↓ | ↓↓ |
| eNOS | ↓ | ↑ | ↑ | ↑↑ |
| phospho-eNOS (S1177) | ↓ | ↑ | ↑ | ↑↑ |
| Akt | – | – | – | – |
| phospho-Akt (S473) | ↓ | ↑ | ↑ | ↑ |
| sGC-α1 | ↓ | ↑ | ↑ | ↑ |
| sGC-β1 | ↓ | ↑ | ↑ | ↑ |
| CBS | ↑ | ↓ | ↓ | ↓ |
| CSE | ↑ | ↓ | ↓ | ↓↓ |
4. Discussion
The results of the present study indicate that reduced nitrosative stress and restored eNOS function favor plaque integrity. In addition to improved NO homeostasis (increased eNOS expression and phosphorylation) we report that simvastatin promotes plaque stability and this coincides with reduced expression of HIF-1α, with a parallel decrease in H2S producing enzymes expression.
Atherosclerosis is a multifactorial disease and the mechanisms includes among others, excess ROS and RNS formation, apoptosis and necrosis, angiogenesis, thrombosis and endothelial dysregulation [5]. There is a complex interplay between these processes and a variable importance of each factor in the development, progression and morphology of the atheroma, leading to variable clinical results. Most plaques remain asymptomatic (subclinical disease), some cause luminal obstruction (stable angina), and others may be ruptured leading to an acute coronary syndrome (ACS) (Reviewed in 1). We have previously shown that NT was specifically related to plaque instability in human carotid plaques versus control samples [19]. In agreement to the above, we found that NT levels were decreased in asymptomatic patients with stable plaques versus patients with unstable atheromas. However MDA levels did not differ among groups. The above findings reinforce the notion that plaque stability is associated with nitrosative stress while it is independent of lipid peroxidation.
In our study, we focused on HIF-1α regulation and signaling as it has been previously shown that it can mediate atherosclerosis progression [20] and HIF-1α is linked to enzymes which play important roles in NO (iNOS) and CO (HO-1) production and in nitro-oxidative stress regulation (NOX-4). Decreasing HIF-1α activity in macrophages prevents the progression of vascular remodeling, therefore HIF-1α might be a therapeutic target for vascular diseases [37]. Herein, we showed that HIF-1α is upregulated in patients with unstable plaques versus patients with stable lesions indicating that HIF-1α is positively associated with plaque instability. Subsequently, we determined the expression of three key enzymes which are downstream of HIF-1α. NOX-4 contributes to increased intracellular oxidative stress, through production of H2O2 and VSMC apoptosis therefore, is involved in the genesis and the progression of atherosclerotic disease [38], [39]. Additionally NOX-4 is significantly increased in human coronary artery disease (CAD) and correlates with signs of plaque instability [39]. We showed herein that NOX-4 expression is increased in unstable plaques versus stable ones, indicating that the production of ROS in the plaque is associated with instability of the atheroma. HO-1 expression defines the progression and stability of vulnerable atherosclerotic plaque through suppression of iNOS/NO production, inflammation, and apoptosis in lesions [28]. However, another study demonstrated that HO-1 was upregulated in vulnerable unstable plaques versus stable lesions, proposing that HO-1 is upregulated as an antioxidant response against atherosclerosis progression [40]. Moreover, there is evidence that decreased NO production by eNOS leads to a parallel increase in HO-1 expression which balances the concomitant iNOS upregulation [41]. Our results revealed that the expression of HO-1 is significantly increased in patients with unstable versus stable plaques. Based on the observations for increased NT levels and the increased expression of NOX-4 in unstable plaques we propose that HO-1 is expressed as an antioxidant defense enzyme.
Distortion of NO homeostasis through iNOS upregulation and production of ONOO- is a leading cause of vascular dysfunctions and can be a contributing factor in atheroma formation and rupture [42]. On the other hand the restoration of the balance between eNOS activation/expression and iNOS expression would afford vascular protection [32]. Herein we showed that eNOS is phosphorylated on its activation site S1177 and its expression is increased in patients with stable plaques; decreased expression of iNOS was observed in the same group. Therefore, we can propose that restoration of NO homeostasis is a key event in plaque stability. Additionally, our findings deduce that the balance between HIF-1α (along with its downstream targets) and eNOS is restored, and this might be a potent mechanism through which plaque stabilization is induced. Soluble guanylyl cyclase (sGC) is a key enzyme of the NO pathway which mediates vasoprotective actions [35]; therefore, we can propose that the upregulation of sGC along with the restoration of eNOS/iNOS ratio contributes to the overall improvement of vascular health in asymptomatic patients with stable plaques.
H2S exerts a multitude of beneficial effects in the cardiovascular system including reduction of blood pressure and vascular tone, inhibition of LDL oxidation and foam cell formation [43]. On the other hand, it is well established that H2S induces angiogenesis [44], an effect that can aggravate the progression of the plaque, since neovascularization of the plaque can be a detrimental factor in atheroma stability [45]. Even though, it is well established that endothelial H2S generation can be anti-atherosclerotic [46], the contribution of intraplaque formation of H2S to plaque stability is still unknown. We observed herein that the expression of both CBS and CSE is decreased in patients with stable plaques versus those with unstable ones. We must mention that H2S is an antioxidant molecule that has been previously shown to protect various cell types, including endothelial cells, from oxidative injury [47]. H2S impacts on cellular redox state as it inhibits ROS production and up regulates the expression of anti-oxidant genes. Therefore we speculate that the increased expression of CSE in unstable plaques, in which elevated oxidative stress was confirmed in our experiments, might occur to offset the increased levels of ROS, acting as an antioxidant defense system. However since endogenous H2S has been related to increased angiogenesis, our results indicate that increased expression of CBS and CSE in atherosclerotic plaques may be a potential risk factor for plaque vulnerability. However, we should mention that given the low endogenous tissue concentration of free H2S, it is unlikely that H2S acts as a direct scavenger of peroxynitrite or other oxidants in vivo [48]. Instead, we believe that H2S exerts its action through indirect effects by activating redox-sensitive transcription factors such as Nrf-2 [49].
We next investigated the molecular changes associated with the use of a widely used agent for the pharmacotherapy of hyperlipidemia, simvastatin. Statins exert a variety of beneficial effects on the cardiovascular system, including improved endothelial function, reduced oxidative stress, and reduction of atheroma instability [13]. It should, however be kept in mind that not all HMGCoA reductase inhibitors exert identical responses, as lipophilicity of each compound in this class influences its pharmacological profile [50].
Statin administration triggers antioxidant responses in the cardiovascular system [51]. Moreover, simvastatin was shown to reduce the expression of HIF-1α in abdominal vessels in an in vivo model of atherosclerosis and acute myocardial infarction and this correlated with its beneficial effects [52]. On the contrary, statins up-regulated the expression of HO-1 and HIF-1α in monocytes derived from patients with CAD. However in the latter scientific work the treatment of the patients was not well defined and included the administration of a wide range of pharmacological factors such as adrenergic receptor blockers, angiotensin-converting enzyme inhibitors or statins [53]. Nevertheless, the actual role of intraplaque HIF-1α regulation by statins, as far as plaque stability is concerned is yet to be elucidated in humans. We, herein, showed that the aforementioned protein is associated with simvastatin-induced plaque stability as it is further reduced in patients with stable plaques under statin therapy versus untreated group.
Statins can reduce NOX-4 expression and activity in heart and vessels [54], [55]. However, to the best of our knowledge, there are no experimental or clinical data accessing the effect of simvastatin on intraplaque NOX-4 regulation. We observed that although NOX-4 is associated with plaque stability and is increased in patients with unstable lesions, it is independent of simvastatin administration. In parallel, we showed that MDA levels did not differ among patients receiving simvastatin or not. As far as iNOS is concerned, it has been reported that simvastatin downregulates iNOS expression in atherosclerosis [56]. We observed that in addition to HIF-1α, simvastatin also decreased iNOS levels in patients with stable plaques protecting against atheroma vulnerability/rupture with a parallel decrease in nitrotyrosine levels. Additionally, simvastatin is known to upregulate HO-1 in in vitro and in vivo experimental models of oxidative stress, such as ischemia reperfusion injury [57], [58]. We have found that the expression of HO-1 is decreased in patients with stable plaques under simvastatin therapy versus untreated ones; data which indicate that simvastatin may uses the HIF-1α/HO-1 axis to exert its additional vasoprotective effects.
In line with the findings that statins improve NO bioavailability through eNOS upregulation and activation [59] we found that eNOS activation (S1177) and expression was enhanced in patients under simvastatin therapy, with a concomitant decrease in iNOS expression. The latter results support the hypothesis that the simvastatin-induced plaque stabilization is mediated through restoration of the eNOS/iNOS balance. Interestingly, both sGC and Akt, enzymes that operate downstream and upstream of NO respectively, were found to be unchanged in stable plaques after simvastatin treatment. It has been reported, that statins upregulate H2S production [60] in in vivo animal models; however this effect is not uniform among statins as induction of H2S generation is proportional to statin lipophilicity [61]. We observed that only CSE expression was decreased by simvastatin in patients with stable plaques, while CBS remained unchanged. Targeting CSE by simvastatin might be a novel mechanism against atheromatosis as it is recently proven to be expressed in atherosclerotic lesions and to be highly associated with plaque instability due to its pro-angiogenic properties [62]. The above findings reinforce the notion that simvastatin might improve plaque intergrity through restoration of eNOS/iNOS balance with a parallel decrease of the excess H2S production. However, this is largely supposition and additional studies are necessary to establish a cost and effect link between changes in enzyme level expression and simvastatin plaque stabilization.
5. Study limitations
A limitation of the study is that patients received previous therapies that might influence disease progression. Carotid intima-media thickness (IMT) progression has been shown to be blunted by long-term antihypertensive treatment such as ACE-inhibitors, and beta-blockers [63]. Combination treatment with ACE inhibitors and antiplatelets, such as aspirin, reduced the expression of inflammatory markers in human carotid artery plaques [64]. Additionally the various drugs might also influence vascular reactivity and probably levels or synthesis of CO, NO and H2S. It is well established that angiotensin II plays a key role in the pathophysiology of endothelial dysfunction by reducing NO bioavailability [65]. The ACE inhibitor, S-zofenopril, has been shown to improve vascular function by potentiating the H2S pathway in a model of spontaneous hypertension [66]. Another ACE inhibitor, ramipril increased aorta endothelium HO-1 expression in a type 2 diabetes animal model [67]. However, we must mention that there were no statistically significant differences between the two groups of patients (simvastatin and non simvastatin therapy) considering the various medications that the patients received.
Another limitation of the study is that we have determined only the expression of NO H2S and CO generating enzymes. Although the expression of protein levels could change, the overall activity of the above mentioned enzymes has not been determined. Since there are reports shown that CSE knockout animals are prone to atherosclerosis [46], and the triply NOS−/− mice exhibits an atherosclerotic phenotype [68], the activity of the enzymes that generate H2S and NO in human atheroma should be evaluated in further studies, particularly because a cross talk between the H2S, CO and NO pathway signal transduction systems may exist. Additionally, despite that the time of carotid artery lesion development and the total atherosclerotic burden are rather impossible to be precisely defined it would be interesting to correlate the expression of gasotransmitters generating enzymes or a switch of their enzymes activity with the severity of atheroma.
6. Conclusion
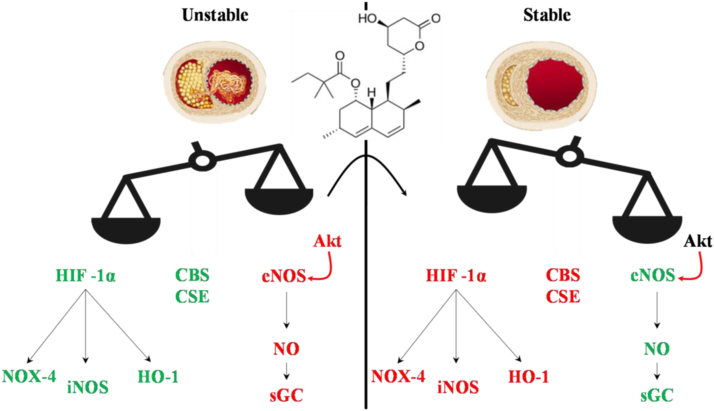
Taken together our data suggest that stable carotid plaques are characterized by a decrease in the expression of HIF-α and a concomitant downregulation of its downstream targets NOX-4, HO-1 and iNOS resulting in reduced levels of nitrotyrosine. Additionally, stable plaques are characterized by restored NO bioavailability through eNOS upregulation and decreased expression of H2S generating enzymes. By assessing the effect of simvastatin on plaque stability, we concluded that besides its known effect on eNOS upregulation, simvastatin also reduces the expression of HIF-1α and its downstream targets, iNOS and HO-1. Finally CSE reduced expression seems to be an additional mechanism of simvastatin induced plaque stability. The proposed mechanism of plaque stability and the effect of simvastatin are illustrated in Fig. 9 [69].
Fig. 9.
Reciprocal regulation of eNOS vs H2S in atherosclerotic plaques. eNOS-derived NO increases bioavailability of NO in stable plaques, which would be expected to occur due to eNOS upregulation and phosphorylation (due to Akt activation); concomitantly iNOS and NOX-4 are downregulated presumably due to reduced HIF-1α. Moreover CBS and CSE positively correlate with plaque vulnerability. Simvastatin administration decreases HIF-1α expression and its downstream targets, iNOS and HO-1, whereas it increases the phosphorylation and expression of eNOS. Reduced CSE expression is associated with simvastatin administration and enhanced plaque stability (Modified by [69]). Red color indicates signaling molecules that decreased, whereas green color indicates signaling molecules that are upregulated.
Ten years ago, the only established criterion for predicting stroke was the degree of carotid stenosis. Since then, the complicated carotid plaque has received considerable attention because of its correlation with the clinical manifestations of carotid occlusive disease. Plaque instability is considered an essential determinant of clinical manifestation of symptomatic carotid occlusive disease. The recognition of novel targets for plaque stabilization and a better understanding of the underlying mechanisms utilized by statins to promote plaque stabilization are of paramount clinical importance, since it would allow further pharmacologic innovations in managing this crucial topic of atherosclerotic disease which will be implicated in all beds of arterial atherosclerotic disease.
Conflict of interest/disclosures
None.
References
- 1.Den Hartog A.G., Achterberg S., Molletal F.L. Asymptomatic carotid artery stenosis and the risk of ischemic stroke according to subtype in patients with clinical manifest arterial disease. Stroke. 2013;44:1002–1007. doi: 10.1161/STROKEAHA.111.669267. [DOI] [PubMed] [Google Scholar]
- 2.Inzitari D., Eliasziw M., Gates P., Sharpe B.L., Chan R.K., Meldrum H.E., Barnett H.J. The causes and risk of stroke in patients with asymptomatic internal-carotid-artery stenosis. North American symptomatic Carotid Endarterectomy trial Collaborators. New Engl. J. Med. 2000;342:1693–1700. doi: 10.1056/NEJM200006083422302. [DOI] [PubMed] [Google Scholar]
- 3.Petty G.W., Jr, Brown R.D., Whisnant J.P., Sicks J.D., O’Fallon W.M., Wiebers D.O. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke. 1999;30:2513–2516. doi: 10.1161/01.str.30.12.2513. [DOI] [PubMed] [Google Scholar]
- 4.Bentzon J.F., Otsuka F., Virmani R., Falk E. Mechanisms of plaque formation and rupture. Circ. Res. 2014;114:1852–1866. doi: 10.1161/CIRCRESAHA.114.302721. [DOI] [PubMed] [Google Scholar]
- 5.Hopkins P.N. Molecular biology of atherosclerosis. Physiol. Rev. 2013;93:1317–1542. doi: 10.1152/physrev.00004.2012. [DOI] [PubMed] [Google Scholar]
- 6.Andreadou I., Iliodromitis E.K., Rassaf T., Schulz R., Papapetropoulos A., Ferdinandy P. The role of gasotransmitters NO, H2S and CO in myocardial ischaemia/reperfusion injury and cardioprotection by preconditioning, postconditioning and remote conditioning. Br. J. Pharm. 2015;172:1587–1606. doi: 10.1111/bph.12811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Szabo C. Gasotransmitters in cancer: from pathophysiology to experimental therapy. Nat. Rev. Drug Disco. 2016;15:185–203. doi: 10.1038/nrd.2015.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kabil O., Banerjee R. Enzymology of H(2)S biogenesis, decay and signaling. Antiox. Redox Signal. 2014;20:770–782. doi: 10.1089/ars.2013.5339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kimura H. Production and physiological effects of hydrogen sulfide. Antiox. Redox Signal. 2014;20:783–793. doi: 10.1089/ars.2013.5309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang R., Szabo C., Ichinose F., Ahmed A., Whiteman M., Papapetropoulos A. The role of H2S bioavailability in endothelial dysfunction. Trends Pharmacol. Sci. 2015;36:568–578. doi: 10.1016/j.tips.2015.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kockx M.M., Herman A.G. Apoptosis in atherosclerosis: beneficial or detrimental? Cardiovasc. Res. 2000;45:736–746. doi: 10.1016/s0008-6363(99)00235-7. [DOI] [PubMed] [Google Scholar]
- 12.Mihaylova B., Emberson J., Blackwell L., Keech A., Simes J., Barnes E.H., Voysey M., Gray A., Collins R., Baigent C. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380:581–590. doi: 10.1016/S0140-6736(12)60367-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ludman A., Venugopal V., Yellon D.M., Hausenloy D.J. Statins and cardioprotection--more than just lipid lowering? Pharmacol. Ther. 2009;122:30–43. doi: 10.1016/j.pharmthera.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 14.Lahera V., Goicoechea M., de Vinuesa S.G., Miana M., de las Heras N., Cachofeiro V., Luno J. Endothelial dysfunction, oxidative stress and inflammation in atherosclerosis: beneficial effects of statins. Curr. Med. Chem. 2007;14:243–248. doi: 10.2174/092986707779313381. [DOI] [PubMed] [Google Scholar]
- 15.North American Symptomatic Carotid Endarterectomy Trial Collaborators Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N. Engl. J. Med. 1991;325:445–453. doi: 10.1056/NEJM199108153250701. [DOI] [PubMed] [Google Scholar]
- 16.Stary H.C., Chandler A.B., Dinsmore R.E., Fuster V., Glagov S., Insull W., Jr., Rosenfeld M.E., Schwartz C.J., Wagner W.D., Wissler R.W. A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis. A report from the Committee on vascular Lesions of the Council on Arteriosclerosis. Am. Heart Assoc. Circ. 1995;92:1355–1374. doi: 10.1161/01.cir.92.5.1355. [DOI] [PubMed] [Google Scholar]
- 17.Papalambros E., Sigala F., Georgopoulos S., Panou N., Kavantzas N., Agapitos M., Bastounis E. Vascular endothelial growth factor and matrix Metalloproteinase-9 expression in human carotid atherosclerotic plaques: relationship with plaque destabilization via neovascularization. Cerebrovasc. Dis. 2004;18:160–165. doi: 10.1159/000079736. [DOI] [PubMed] [Google Scholar]
- 18.Bibli S.I., Andreadou I., Chatzianastasiou A., Tzimas C., Sanoudou D., Kranias E., Brouckaert P., Coletta C., Szabo C., Kremastinos D.T., Iliodromitis E.K., Papapetropoulos A. Cardioprotection by H2S engages a cGMP-dependent protein kinase G/phospholamban pathway. Cardiovasc. Res. 2015;106:432–442. doi: 10.1093/cvr/cvv129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sigala F., Kotsinas A., Savari P., Filis K., Markantonis S., Iliodromitis E.K., Gorgoulis V.G., Andreadou I. Oxidized LDL in human carotid plaques is related to symptomatic carotid disease and lesion instability. J. Vasc. Surg. 2010;52:704–713. doi: 10.1016/j.jvs.2010.03.047. [DOI] [PubMed] [Google Scholar]
- 20.Liu D., Lei L., Desir M., Huang Y., Cleman J., Jiang W., Fernandez-Hernando C., Di Lorenzo A., Sessa W.C., Giordano F.J. Smooth muscle hypoxia-inducible factor 1α links intravascular pressure and atherosclerosis—Brief Report. Arterioscler. Thromb. Vasc. Biol. 2016;36:442–445. doi: 10.1161/ATVBAHA.115.306861. [DOI] [PubMed] [Google Scholar]
- 21.Akhtar S., Hartmann P., Karshovska E., Rinderknecht F.A., Subramanian P., Gremse F., Grommes J., Jacobs M., Kiessling F., Weber C., Steffens S., Schober A. Endothelial hypoxia-inducible factor-1α promotes atherosclerosis and monocyte recruitment by upregulating MicroRNA-19a. Hypertension. 2015;66:1220–1226. doi: 10.1161/HYPERTENSIONAHA.115.05886. [DOI] [PubMed] [Google Scholar]
- 22.Tawakol A., Singh P., Mojena M., Pimentel-Santillana M., Emami H., MacNabb M., Rudd J.H., Narula J., Enriquez J.A., Través P.G., Fernández-Velasco M., Bartrons R., Martín-Sanz P., Fayad Z.A., Tejedor A., Boscá L. HIF-1α and PFKFB3 mediate a tight Relationship Between proinflammatory activation and anaerobic metabolism in atherosclerotic macrophages. Arterioscler. Thromb. Vasc. Biol. 2015;35:1463–1471. doi: 10.1161/ATVBAHA.115.305551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhao R., Feng J., He G. Hypoxia increases Nrf2-induced HO-1 expression via the PI3K/Akt pathway. Front. Biosci. (Landmark Ed.) 2016;21:385–396. doi: 10.2741/4395. [DOI] [PubMed] [Google Scholar]
- 24.Diebold I., Petry A., Hess J., Görlach A. The NADPH oxidase subunit NOX4 is a new target gene of the hypoxia-inducible factor-1. Mol. Biol. Cell. 2010;21:2087–2096. doi: 10.1091/mbc.E09-12-1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Idelman G., Smith D.L., Zucker S.D. Bilirubin inhibits the up-regulation of inducible nitric oxide synthase by scavenging reactive oxygen species generated by the toll-like receptor 4-dependent activation of NADPH oxidase. Redox Biol. 2015;5:398–408. doi: 10.1016/j.redox.2015.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Szocs K., Lassegue B., Sorescu D., Hilenski L.L., Valppu L., Couse T.L., Wilcox J.N., Quinn M.T., Lambeth J.D., Griendling K.K. Upregulation of Nox-based NAD(P)H oxidases in restenosis after carotid injury. Arterioscler. Thromb. Vasc. Biol. 2002;22:21–27. doi: 10.1161/hq0102.102189. [DOI] [PubMed] [Google Scholar]
- 27.Bedard K., Krause K.-H. The NOX family of ROS-generating NADPH oxidases: physiology and pathophysiology. Physiol. Rev. 2007;87:245–313. doi: 10.1152/physrev.00044.2005. [DOI] [PubMed] [Google Scholar]
- 28.Li T., Tian H., Zhao Y., An F., Zhang L., Zhang J., Peng J., Zhang Y., Guo Y. Heme oxygenase-1 inhibits progression and destabilization of vulnerable plaques in a rabbit model of atherosclerosis. Eur. J. Pharm. 2011;672:143–152. doi: 10.1016/j.ejphar.2011.09.188. [DOI] [PubMed] [Google Scholar]
- 29.Espinola-Klein C., Blankenberg S., Münzel T. Is heme oxygenase-1 a causal player for plaque stability? Stroke. 2005;36 (1901-193) [PubMed] [Google Scholar]
- 30.Yet S.-F., Layne M.D., Liu X., Chen Y.-H., Ith B., Sibinga E.S., Perrella M.A. Absence of heme oxygenase-1 exacerbates atherosclerotic lesion formation and vascular remodeling. FASEB J. 2003;17:1759–1761. doi: 10.1096/fj.03-0187fje. [DOI] [PubMed] [Google Scholar]
- 31.Huang H., Koelle P., Fendler M., Schröttle A., Czihal M., Hoffmann U., Conrad M., Kuhlencordt P.J. Induction of inducible nitric oxide synthase (iNOS) expression by oxLDL inhibits macrophage derived foam cell migration. Atherosclerosis. 2014;235:213–222. doi: 10.1016/j.atherosclerosis.2014.04.020. [DOI] [PubMed] [Google Scholar]
- 32.Badimon L., Vilahur G. Thrombosis formation on atherosclerotic lesions and plaque rupture. J. Int. Med. 2014;276:618–632. doi: 10.1111/joim.12296. [DOI] [PubMed] [Google Scholar]
- 33.Fulton D., Gratton J.P., McCabe T.J., Fontana J., Fujio Y., Walsh K., Franke T.F., Papapetropoulos A., Sessa W.C. Regulation of endothelium derived nitric oxide production by the protein kinase Akt. Nature. 1999;399:597–601. doi: 10.1038/21218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fernández-Hernando C., József L., Jenkins D., Di Lorenzo A., Sessa W.C. Absence of Akt1 reduces vascular smooth muscle cell migration and survival and induces features of plaque vulnerability and cardiac dysfunction during atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2009;29:2033–2040. doi: 10.1161/ATVBAHA.109.196394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Francois M., Kojda G. Effect of hypercholesterolemia and of oxidative stress on the nitric oxide-cGMP pathway. Neurochem. Int. 2004;45:955–961. doi: 10.1016/j.neuint.2004.03.026. [DOI] [PubMed] [Google Scholar]
- 36.Katsouda A., Bibli S.-I., Pyriochou A., Szabo C., Papapetropoulos A. Regulation and role of endogenously produced hydrogen sulfide in angiogenesis. Pharmacol. Res. 2016;113:175–185. doi: 10.1016/j.phrs.2016.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nakayama T., Kurobe H., Sugasawa N., Kinoshita H., Higashida M., Matsuoka Y., Yoshida Y., Hirata Y., Sakata M., Maxfield M.W., Shimabukuro M., Takahama Y., Sata M., Tamaki T., Kitagawa T., Tomita S. Role of macrophage-derived hypoxia-inducible factor (HIF)−1α as a mediator of vascular remodelling. Cardiovasc. Res. 2013;99:705–715. doi: 10.1093/cvr/cvt146. [DOI] [PubMed] [Google Scholar]
- 38.Pedruzzi E., Guichard C., Ollivier V., Driss F., Fay M., Prunet C., Marie J.C., Pouzet C., Samadi M., Elbim C., O'Dowd Y., Bens M., Vandewalle A., Gougerot-Pocidalo M.A., Lizard G., Ogier-Denis E. NAD(P)H oxidase Nox-4 mediates 7-ketocholesterol-induced endoplasmic reticulum stress and apoptosis in human aortic smooth muscle cells. Mol. Cell. Biol. 2004;24:10703–10717. doi: 10.1128/MCB.24.24.10703-10717.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sorescu D., Weiss D., Lassegue B., Clempus R.E., Szocs K., Sorescu G.P., Valppu L., Quinn M.T., Lambeth J.D., Vega J.D., Taylor W.R., Griendling K.K. Superoxide production and expression of nox family proteins in human atherosclerosis. Circulation. 2002;105:1429–1435. doi: 10.1161/01.cir.0000012917.74432.66. [DOI] [PubMed] [Google Scholar]
- 40.Cheng C., Noordeloos A.M., Jeney V., Soares M.P., Moll F., Pasterkamp G., Serruys P.W., Duckers H.J. Heme oxygenase 1 determines atherosclerotic lesion progression into a vulnerable plaque. Circulation. 2009;119:3017–3027. doi: 10.1161/CIRCULATIONAHA.108.808618. [DOI] [PubMed] [Google Scholar]
- 41.Siow R.C., Sato H., Mann G.E. Heme oxygenase-carbon monoxide signalling pathway in atherosclerosis: anti-atherogenic actions of bilirubin and carbon monoxide? Cardiovasc. Res. 1999;41:385–394. doi: 10.1016/s0008-6363(98)00278-8. [DOI] [PubMed] [Google Scholar]
- 42.Cau S.B., Carneiro F.S., Tostes R.C. Differential modulation of nitric oxide synthases in aging: therapeutic opportunities. Fron. Physiol. 2012;3:218. doi: 10.3389/fphys.2012.00218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mani S., Untereiner A., Wu L., Wang R. Hydrogen sulfide and the pathogenesis of atherosclerosis. Antiox. Redox Sign. 2014;20:805–817. doi: 10.1089/ars.2013.5324. [DOI] [PubMed] [Google Scholar]
- 44.Coletta C., Papapetropoulos A., Erdelyi K., Olah G., Modis K., Panopoulos P., Asimakopoulou A., Gero D., Sharina I., Martin E., Szabo C. Hydrogen sulfide and nitric oxide are mutually dependent in the regulation of angiogenesis and endothelium-dependent vasorelaxation. Proc. Nat. Acad. Sci. USA. 2012;109:9161–9166. doi: 10.1073/pnas.1202916109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Michel J.B., Martin-Ventura J.L., Nicoletti A., Ho-Tin-Noe B. Pathology of human plaque vulnerability: mechanisms and consequences of intraplaque haemorrhages. Atherosclerosis. 2014;234:311–319. doi: 10.1016/j.atherosclerosis.2014.03.020. [DOI] [PubMed] [Google Scholar]
- 46.Mani S., Li H., Untereiner A., Wu L., Yang G., Austin R.C., Dickhout J.G., Lhoták Š., Meng Q.H., Wang R. Decreased endogenous production of hydrogen sulfide accelerates atherosclerosis. Circulation. 2013;127:2523–2534. doi: 10.1161/CIRCULATIONAHA.113.002208. [DOI] [PubMed] [Google Scholar]
- 47.Suzuki K., Olah G., Modis K., Coletta C., Kulp G., Gerö D., Szoleczky P., Chang T., Zhou Z., Wu L., Wang R., Papapetropoulos A., Szabo C. Hydrogen sulfide replacement therapy protects the vascular endothelium in hyperglycemia by preserving mitochondrial function. Proc. Natl. Acad. Sci. USA. 2011;108:13829–13834. doi: 10.1073/pnas.1105121108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carballal S., Trujillo M., Cuevasanta E., Bartesaghi S., Möller M.N., Folkes L.K., García-Bereguiaín M.A., Gutiérrez-Merino C., Wardman P., Denicola A., Radi R., Alvarez B. Reactivity of hydrogen sulfide with peroxynitrite and other oxidants of biological interest. Free Radic. Biol. Med. 2011;50:196–205. doi: 10.1016/j.freeradbiomed.2010.10.705. [DOI] [PubMed] [Google Scholar]
- 49.Xie L., Gu Y., Wen M., Zhao S., Wang W., Ma Y., Meng G., Han Y., Wang Y., Liu G., Moore P.K., Wang X., Wang H., Zhang Z., Yu Y., Ferro A., Huang Z., Ji Y. Hydrogen Sulfide induces keap1 S-sulfhydration and suppresses Diabetes-Accelerated Atherosclerosis via Nrf2 activation. Diabetes. 2016;65:3171–3184. doi: 10.2337/db16-0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stuart S.A., Robertson J.D., Marrion N.V., Robinson E.S. Chronic pravastatin but not atorvastatin treatment impairs cognitive function in two rodent models of learning and memory. PloS One. 2013;8:e75467. doi: 10.1371/journal.pone.0075467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ceriello A., Taboga C., Tonutti L., Quagliaro L., Piconi L., Bais B., Da Ros R., Motz E. Evidence for an independent and cumulative effect of postprandial hypertriglyceridemia and hyperglycemia on endothelial dysfunction and oxidative stress generation: effects of short- and long-term simvastatin treatment. Circulation. 2002;106:1211–1218. doi: 10.1161/01.cir.0000027569.76671.a8. [DOI] [PubMed] [Google Scholar]
- 52.Shen W., Shi H.M., Fan W.H., Luo X.P., Jin B., Li Y. The effects of simvastatin on angiogenesis: studied by an original model of atherosclerosis and acute myocardial infarction in rabbit. Mol. Biol. Rep. 2011;38:3821–3828. doi: 10.1007/s11033-010-0497-0. [DOI] [PubMed] [Google Scholar]
- 53.Chen S.M., Li Y.G., Wang D.M., Zhang G.H., Tan C.J. Expression of heme oxygenase-1, hypoxia inducible factor-1alpha, and ubiquitin in peripheral inflammatory cells from patients with coronary heart disease. Clin. Chem. Lab. Med. 2009;47:327–333. doi: 10.1515/CCLM.2009.073. [DOI] [PubMed] [Google Scholar]
- 54.Sarath T.S., Waghe P., Gupta P., Choudhury S., Kannan K., Pillai A.H., Harikumar S.K., Mishra S.K., Sarkar S.N. Atorvastatin ameliorates arsenic-induced hypertension and enhancement of vascular redox signaling in rats. Toxicol. Appl. Pharm. 2014;280:443–454. doi: 10.1016/j.taap.2014.08.032. [DOI] [PubMed] [Google Scholar]
- 55.Li J., Wang J.J., Yu Q., Chen K., Mahadev K., Zhang S.X. Inhibition of reactive oxygen species by Lovastatin downregulates vascular endothelial growth factor expression and ameliorates blood-retinal barrier breakdown in db/db mice: role of NADPH oxidase 4. Diabetes. 2010;59:1528–1538. doi: 10.2337/db09-1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nachtigal P., Kopecky M., Solichova D., Zdansky P., Semecky V. The changes in the endothelial expression of cell adhesion molecules and iNOS in the vessel wall after the short-term administration of simvastatin in rabbit model of atherosclerosis. J. Pharm. Pharm. 2005;57:197–203. doi: 10.1211/0022357055353. [DOI] [PubMed] [Google Scholar]
- 57.Mrad M.F., Mouawad C.A., Al-Hariri M., Eid A.A., Alam J., Habib A. Statins modulate transcriptional activity of heme-oxygenase-1 promoter in NIH 3T3 Cells. J. Cell. Biochem. 2012;113:3466–3475. doi: 10.1002/jcb.24223. [DOI] [PubMed] [Google Scholar]
- 58.Tu Y.P., Chuang S.J., Chen S.C., Liu Y.H., Chen C.F.T.C. Simvastatin induces the expression of hemeoxygenase-1 against ischemia-reperfusion injury on the testes in rats. Toxicol. Lett. 2011;207:242–250. doi: 10.1016/j.toxlet.2011.09.016. [DOI] [PubMed] [Google Scholar]
- 59.Balakumar P., Kathuria S., Taneja G., Kalra S., Mahadevan N. Is targeting eNOS a key mechanistic insight of cardiovascular defensive potentials of statins? J. Mol. Cell. Cardiol. 2012;52:83–92. doi: 10.1016/j.yjmcc.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 60.Xu Y., Du H.P., Li J., Xu R., Wang Y.L., You S.J., Liu H., Wang F., Cao Y.J., Liu C.F., Hu L.F. Statins upregulate cystathionine gamma-lyase transcription and H2S generation via activating Akt signaling in macrophage. Pharmacol. Res. 2014;87:18–25. doi: 10.1016/j.phrs.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 61.Wojcicka G., Jamroz-Wisniewska A., Atanasova P., Chaldakov G.N., Chylinska-Kula B., Beltowski J. Differential effects of statins on endogenous H2S formation in perivascular adipose tissue. Pharmacol. Res. 2011;63:68–76. doi: 10.1016/j.phrs.2010.10.011. [DOI] [PubMed] [Google Scholar]
- 62.van den Born J.C., Mencke R., Conroy S., Zeebregts C.J., van Goor H., Hillebrands J.L. Cystathionine γ-lyase is expressed in human atherosclerotic plaque microvessels and is involved in micro-angiogenesis. Sci. Rep. 2016;6:34608. doi: 10.1038/srep34608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cuspidi C., Negri F., Giudici V., Capra A., Sala C. Effects of antihypertensive drugs on carotid intima-media thickness: focus on angiotensin II receptor blockers. A review of randomized, controlled trials. Integr. Blood Press. Control. 2009;2:1–8. doi: 10.2147/ibpc.s5174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sattler K.J., Woodrum J.E., Galili O., Olson M., Samee S., Meyer F.B., Zhu X.Y., Lerman L.O., Lerman A. Concurrent treatment with renin-angiotensin system blockers and acetylsalicylic acid reduces nuclear factor kappaB activation and C-reactive protein expression in human carotid artery plaques. Stroke. 2005;36:14–20. doi: 10.1161/01.STR.0000150643.08420.78. [DOI] [PubMed] [Google Scholar]
- 65.Savoia C., Schiffrin E.L. Inhibition of the renin angiotensin system: implications for the endothelium. Curr. Diab. Rep. 2006;6:274–278. doi: 10.1007/s11892-006-0060-5. [DOI] [PubMed] [Google Scholar]
- 66.Bucci M., Vellecco V., Cantalupo A., Brancaleone V., Zhou Z., Evangelista S., Calderone V., Papapetropoulos A., Cirino G. Hydrogen sulfide accounts for the peripheral vascular effects of zofenopril independently of ACE inhibition. Cardiovasc. Res. 2014;102:138–147. doi: 10.1093/cvr/cvu026. [DOI] [PubMed] [Google Scholar]
- 67.Tian S., Ge X., Wu K., Yang H., Liu Y. Ramipril protects the endothelium from high glucose-induced dysfunction through CaMKKβ/AMPK and heme oxygenase-1 activation. J. Pharmacol. Exp. Ther. 2014;350:5–13. doi: 10.1124/jpet.114.212928. [DOI] [PubMed] [Google Scholar]
- 68.Tsutsui M., Shimokawa H., Otsuji Y., Yanagihara N. Pathophysiological relevance of NO signaling in the cardiovascular system: novel insight from mice lacking all NO synthases. Pharm., Ther. 2010;128:499–508. doi: 10.1016/j.pharmthera.2010.08.010. [DOI] [PubMed] [Google Scholar]
- 69.Libby P. Inflammation in atherosclerosis. Nature. 2002;202:420 868. doi: 10.1038/nature01323. [DOI] [PubMed] [Google Scholar]