Abstract
Background and Purpose: Ureteropelvic junction obstruction is a common urologic condition that accounts for approximately $12 million in inpatient spending annually. Few studies have assessed the costs related to treatment. We sought to examine the cost of care for patients treated for ureteropelvic junction obstruction.
Patients and Methods: We used the MarketScan® database to identify adults from 18 to 64 years old treated with minimally invasive pyeloplasty, open pyeloplasty, and endopyelotomy for ureteropelvic junction obstruction between 2002 and 2010. Our primary outcome was total expenditures related to the surgical episode, defined as the period from 30 days prior until 30 days after the index surgery. We fit a multinomial linear regression model to evaluate cost of the surgical episode, adjusting for age, gender, comorbidity, benefit plan type, and region of residence.
Results: We identified 1251 endopyelotomies, 717 open pyeloplasties, and 1048 minimally invasive pyeloplasties. The adjusted mean costs were $16,379 for endopyelotomy, $22,421 for open pyeloplasty, and $22,843 for minimally invasive pyeloplasty (p < 0.0001, ANCOVA). Both open and minimally invasive pyeloplasties were more costly than endopyelotomy (both p < 0.0001, comparison between groups). However, the cost of open and minimally invasive pyeloplasties was similar (p = 0.57, comparison between groups).
Conclusions: Among the three treatments, endopyelotomy was the least expensive in the immediate perioperative period. Open and minimally invasive pyeloplasties were similar in cost, but both more expensive than endopyelotomies. The similar cost between the two pyeloplasty approaches provides additional evidence that minimally invasive pyeloplasty should be considered the standard treatment for ureteropelvic junction obstruction.
Keywords: : cost, ureteropelvic junction obstruction, minimally invasive pyeloplasty, open pyeloplasty, endopyelotomy
Introduction
Ureteropelvic junction obstruction is a common urologic condition that accounts for ∼1000 adult hospitalizations and $12 million in inpatient spending annually.1 There are three primary treatments for this condition: minimally invasive pyeloplasty, open pyeloplasty, and endopyelotomy. These treatments have varying success rates and associated morbidities, but they are all generally considered effective.2,3
Although prior work has examined factors associated with their use4 as well as their outcomes,3,5 few studies have assessed the costs related to these procedures. On the one hand, minimally invasive pyeloplasties (i.e., laparoscopic or robotic approaches) may reduce costs due to decreased hospital length of stay, quicker convalescence, and increased productivity.3,6 On the other hand, capital expenditures and lack of competition among suppliers (e.g., for robotic equipment) may increase costs.7 Only a few studies have specifically examined the cost of endopyelotomy, with somewhat conflicting findings in terms of its cost-effectiveness.2,8 Regardless, with annual healthcare costs reaching $3 trillion or nearly 18% of our country's gross domestic product,9 understanding the cost of these different treatments for ureteropelvic junction obstruction is warranted.
For these reasons, we sought to examine the cost of care for patients treated with minimally invasive pyeloplasty, open pyeloplasty, and endopyelotomy for ureteropelvic junction obstruction. We focused on the costs of perioperative care since this represents a surgical episode that could potentially be incorporated into a bundled payment—an alternative payment model to traditional fee-for-service. The Centers for Medicare and Medicaid Services recently implemented bundled payments for hip and knee replacements10 and plans to launch them for the treatment of heart attacks and cardiac bypass surgery in July 2017.11 This payment model will likely expand to other conditions in the near future. The Medicare Access and Children's Health Insurance Program Reauthorization Act of 2015 aspires to have 50% of Medicare payments tied to quality or value through alternative payment models by the end of 2018.12 Findings from this study will help inform the debate surrounding bundled payments for surgical episodes.
Materials and Methods
Data source and study population
We used the Truven Health Analytics MarketScan® Commercial Claims and Encounters Database to identify adults from 18 to 64 years old who were treated for ureteropelvic junction obstruction between 2002 and 2010. The MarketScan database provides the largest convenience sample available in proprietary databases and, with data on ∼40 million employees and their dependents, allows for the creation of a nationally representative sample of Americans with employer-provided health insurance.13 Using Healthcare Common Procedure Coding System (HCPCS) codes, we assigned patients to one of three treatments: endopyelotomy (HCPCS codes 50575, 52342, 52345, 52346), open pyeloplasty (HCPCS codes 50400, 50405), and minimally invasive pyeloplasty (HCPCS code 50544).
We required continuous enrollment in a benefits plan for 6 months before the treatment date to calculate patient comorbidity. We also required continuous enrollment for 30 days after treatment to facilitate the calculation of total expenditures for the surgical episode. We excluded 199 patients with negative total expenditure costs. Using these criteria, our study population consisted of 1251 endopyelotomies, 717 open pyeloplasties, and 1048 minimally invasive pyeloplasties.
Outcomes
Our primary outcome was total expenditures related to the surgical episode for endopyelotomies, open pyeloplasties, and minimally invasive pyeloplasties. We defined a surgical episode as the period from 30 days prior until 30 days after the index surgery. All costs were standardized to 2011 dollars using the gross domestic product index.14 We investigated expanding the surgical episode from 60 days prior until 60 days after the index surgery and found the relationship among the costs of the three treatments to be the same. Thus, we report the total expenditure costs for the shorter time period to minimize the risk of attributing costs to treatments that were associated with unrelated conditions.
We examined the association of several patient and regional characteristics with cost. Patient race/ethnicity is not reported in the data set. Comorbidity was represented as a Charlson index, which was calculated using all claims in the 6-month period before treatment.15
Statistical analysis
We examined differences among patients receiving minimally invasive pyeloplasty, open pyeloplasty, and endopyelotomy using chi-square tests. Next, we fit a multinomial linear regression model to evaluate the cost of the surgical episode, adjusting for age, gender, comorbidity, benefit plan type, and region of residence.16 We compared the adjusted mean costs among the three treatments (ANCOVA test) as well as differences between each pair of treatments (comparison between groups). We then fit a cost model that was log transformed. The decision to use a log-transformed model was informed by a Box–Cox transformation of the costs. In this model, each predictor was adjusted for all other predictors in the model. Next, we performed a sensitivity analysis where we examined the influence of high-cost observations (i.e., outliers) by excluding the most costly 5% of patients, and the main results were similar. Thus, our final model was based on the full sample.
All analyses were performed using SAS v9.3 (Cary, NC). All tests were two tailed and the probability of a type I error was set at 0.05. The Institutional Review Board of the RAND cooperation determined that the study design was exempt from review.
Results
The patient demographics of our study population are shown in Table 1. On average, patients treated with endopyelotomy were older compared with those treated with open pyeloplasty and minimally invasive pyeloplasty (p < 0.0001). There were no differences in gender (p = 0.43) or comorbidity (p = 0.54) among the three treatments. Patients undergoing endopyelotomy were less likely to have salaried employment or live in a metropolitan statistical area, and were more likely to live in the south (all p < 0.0001).
Table 1.
Patient Demographics According to Treatment
| Characteristics | Endopyelotomy (n = 1251) | Open pyeloplasty (n = 717) | Minimally invasive pyeloplasty (n = 1048) | pa |
|---|---|---|---|---|
| Age, years (%) | <0.0001 | |||
| 18–34 | 208 (17) | 217 (30) | 411 (39) | |
| 35–44 | 212 (17) | 133 (19) | 179 (17) | |
| 45–54 | 316 (25) | 167 (23) | 205 (20) | |
| 55–64 | 515 (41) | 200 (28) | 253 (24) | |
| Gender (%) | 0.43 | |||
| Female | 756 (60) | 412 (57) | 619 (59) | |
| Male | 495 (40) | 305 (43) | 429 (41) | |
| Comorbidity (%) | 0.54 | |||
| 0 | 1066 (85) | 612 (85) | 909 (87) | |
| 1 or more | 185 (15) | 105 (15) | 139 (13) | |
| Benefit plan type (%) | 0.03 | |||
| HMO | 145 (12) | 84 (12) | 105 (10) | |
| PPO | 809 (65) | 451 (63) | 732 (70) | |
| Otherb | 297 (24) | 182 (25) | 211 (20) | |
| Employment classification (%) | <0.0001 | |||
| Nonsalaried | 352 (28) | 179 (25) | 245 (23) | |
| Salaried | 167 (13) | 131 (18) | 215 (21) | |
| Unknown | 732 (59) | 407 (57) | 588 (56) | |
| Employment status (%) | 0.85 | |||
| Non-full time | 714 (57) | 402 (56) | 587 (56) | |
| Full time | 537 (43) | 315 (44) | 461 (44) | |
| MSA status (%) | <0.0001 | |||
| MSA | 977 (78) | 567 (79) | 895 (85) | |
| Non-MSA | 274 (22) | 150 (21) | 153 (15) | |
| Region of residence (%) | <0.0001 | |||
| Northeast | 137 (11) | 81 (11) | 140 (13) | |
| North Central | 257 (21) | 198 (28) | 324 (31) | |
| South | 645 (52) | 329 (46) | 433 (41) | |
| West | 195 (16) | 99 (14) | 139 (13) | |
| Unknown | 17 (1) | 10 (1) | 12 (1) |
Percentages may not add to 100 due to rounding.
p-values generated from chi-square tests.
Other includes comprehensive, exclusive provider organization, point of service, point of service with capitation, consumer-directed health plan, and missing.
HMO = health maintenance organization; MSA = metropolitan statistical area; PPO = preferred provider organization; SD = standard deviation.
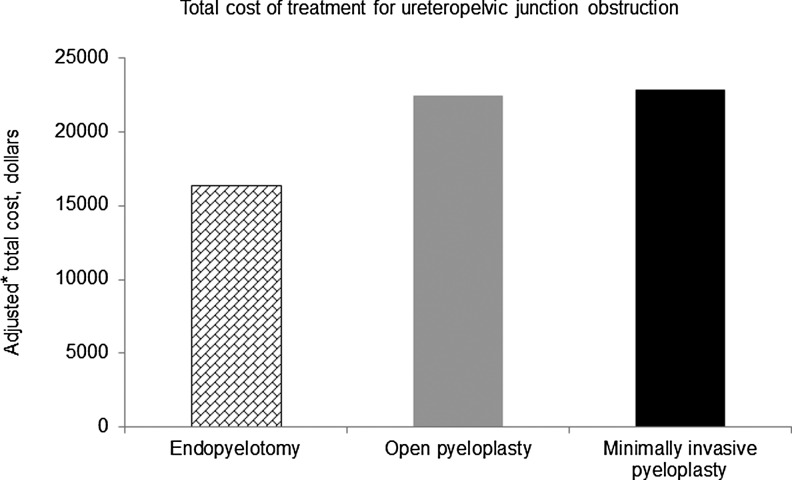
The surgical episode costs for each treatment are shown in Figure 1. The adjusted mean costs were $16,379 for endopyelotomy, $22,421 for open pyeloplasty, and $22,843 for minimally invasive pyeloplasty (p < 0.0001, ANCOVA). Specifically, both open and minimally invasive pyeloplasties were more costly than endopyelotomy (both p < 0.0001, comparison between groups). However, the cost of open and minimally invasive pyeloplasties was similar (p = 0.57, comparison between groups).
FIG. 1.
Total cost of treatment for ureteropelvic junction obstruction. *Adjusted for age, gender, comorbidity, plan type, and region. The cost of the three treatments differed (p < 0.0001, ANCOVA). Specifically, both open and minimally invasive pyeloplasties were more costly than endopyelotomy (both p < 0.0001, comparison between groups). However, open and minimally invasive pyeloplasties did not differ significantly in cost (p = 0.57, comparison between groups).
The results from our log-cost model evaluating predictors of treatment cost are shown in Table 2. A patient's age was not associated with cost (p > 0.05 for all age categories). Men had higher treatment costs than women (p = 0.003) and patients with comorbidities cost more than those without (p = 0.0001). Compared with health maintenance organizations (HMOs), patients with preferred provider organization (PPO) or other health insurance had higher costs (p < 0.0001 and p = 0.0002, respectively). There were no cost differences based on geographic region, except in the south, where costs were lower (p = 0.002).
Table 2.
Results of Log-Cost Model Examining Predictors of Treatment Cost
| Characteristic | Parameter estimate | Standard error | p |
|---|---|---|---|
| Intercept | 9.19 | 0.05 | <0.0001 |
| Treatment | |||
| Endopyelotomy | 1 | — | — |
| Open pyeloplasty | 0.46 | 0.03 | <0.0001 |
| Minimally invasive pyeloplasty | 0.49 | 0.03 | <0.0001 |
| Age, years | |||
| 18–34 | 1 | — | — |
| 35–44 | 0.02 | 0.04 | 0.58 |
| 45–54 | 0.05 | 0.03 | 0.13 |
| 55–64 | −0.003 | 0.03 | 0.93 |
| Gender | |||
| Female | 1 | — | — |
| Male | 0.07 | 0.02 | 0.003 |
| Comorbidity | |||
| 0 | 1 | — | — |
| 1 or more | 0.13 | 0.03 | 0.0001 |
| Benefit plan type | |||
| HMO | 1 | — | — |
| PPO | 0.18 | 0.04 | <0.0001 |
| Othera | 0.15 | 0.04 | 0.0002 |
| Region of residence | |||
| Northeast | 1 | — | — |
| North Central | −0.03 | 0.04 | 0.42 |
| South | −0.12 | 0.04 | 0.002 |
| West | −0.002 | 0.04 | 0.96 |
| Unknown | −0.12 | 0.10 | 0.24 |
The effect of each predictor was adjusted for all other predictors in the model.
Other includes comprehensive, exclusive provider organization, point of service, point of service with capitation, consumer-directed health plan, and missing.
Discussion
The cost of treatment of ureteropelvic junction obstruction around the time of surgery was less for endopyelotomy ($16,379) compared with open pyeloplasty ($22,421) and minimally invasive pyeloplasty ($22,843). Minimally invasive pyeloplasty was the costliest treatment, but there were only marginal cost differences between the two pyeloplasty approaches.
There are at least two potential reasons why endopyelotomies are less expensive than open and minimally invasive pyeloplasties. First, the operative time for an endopyelotomy is considerably shorter.3 Operating times for an endopyelotomy with a standard retrograde approach range from 30 to 90 minutes, whereas times for pyeloplasties range from 165 to 510 minutes.3,17 In analyzing expenditures, it is well described that operating time is a large contributor to cost.18,19 In one study, operating time cost $772 per hour.18 Second, endopyelotomies are typically performed as an outpatient procedure.3 Hospital stays increase the perioperative cost of care18 and both open and minimally invasive pyeloplasties generally necessitate a hospital admission. Even in uncomplicated cases, both open and minimally invasive pyeloplasties require a 1- to 4-day stay in the hospital.3,17,20
However, the lower cost of care with endopyelotomies should be taken with some caution. We looked at a 60-day window around the time of the procedure because this captured the costs most likely related to the treatment episode. Although this information may be the most relevant for policymakers, there are potentially additional costs with endopyelotomies that do not manifest until a later time. For example, treatment failures occur more frequently with endopyelotomies, but may not manifest until several months or even years after the procedure.21 This can lead to readmissions and secondary procedures that may increase the cost of endopyelotomies relative to pyeloplasties in the long term. Thus, in considering an episode of care for a bundled payment, it may make sense to incorporate a longer time period.
There was no difference in cost between open and minimally invasive pyeloplasties. Even with the increased use of robotic pyeloplasty over the study period, the cost of the minimally invasive approach was similar. One potential explanation for this finding is that the increasing costs associated with performing robot-assisted surgery were offset by quicker convalescence and decreased hospital length of stay.5 Although these treatment costs only pertain to a 60-day window around the time of the procedure, we expect that the two approaches would continue to have similar long-term costs since they have comparable success and complication rates.3,22 In calculating costs associated with treatments, we did not account for the up-front cost of the robotic platform (∼$1.5 million) or the annual maintenance fees (∼$150,000).18 How these additional costs affect the cost per treatment directly relates to the volume of cases and number of robotic platforms at each institution: as the number of cases per robotic platform increases, the amount that these costs contribute to each case decreases. As the number of robotic pyeloplasties continues to increase, it will be important to monitor its relative cost compared with the open approach.
The similar cost between the open and minimally invasive approaches is in contrast to findings with other urologic conditions. In prostate cancer, robotic prostatectomy is the most expensive approach, followed by laparoscopic prostatectomy and then open prostatectomy.19 Both robotic and laparoscopic prostatectomies are more expensive than open prostatectomy due to their increased surgical supply costs and increased operative times.19 In kidney cancer, the robotic approach is also the costliest for partial nephrectomies due to the higher cost of surgical equipment and of purchasing and maintaining the robot.18 Interestingly, the laparoscopic approach was the least expensive due to similar operating times, a shorter length of stay, and lower equipment costs.18 As the cost of robotic equipment decreases with the eventual entry of competitive suppliers and operative times become shorter, the robotic approach will become more cost-effective.
Regardless of the type of ureteropelvic junction obstruction treatment, patients with an HMO benefit plan received less expensive care. The HMOs often cap payments, review the use of services, and restrict patient choices to reduce costs.23,24 Indeed, patients with HMO use expensive technologies (e.g., MRI and intensity-modulated radiotherapy) less frequently.25,26 In our study, patients who were part of an HMO received less expensive care, even after accounting for potential confounders such as the type of treatment, patient comorbidities, and region of residence. In many ways, HMOs have evolved into the modern day accountable care organizations.27 As these organizations gain traction, it will be important to examine how they affect the cost of treating ureteropelvic junction obstruction.
The findings of lower costs with endopyelotomy and similar costs between open and minimally invasive pyeloplasty have two policy implications. First, if bundled payments extend to ureteropelvic junction obstruction, providers will need to balance the lower cost of endopyelotomy in the short term with its higher failure rates (and potentially higher costs) in the long term. This issue may become a reality in the near future since the transition from traditional fee-for-service to alternative payment models appears imminent.10 In implementing bundled payments, the duration of the episode of care will become important as some treatments may be less expensive in the short term but more expensive in the long term. Second, given that the two pyeloplasty approaches have similar costs and have been previously shown to have similar outcomes,3,22 perhaps the minimally invasive approach should be considered the standard approach. Critics point out that robot-assisted approaches are more costly,18,19 but this was not the case in this study. Future studies examining other factors contributing to treatment costs, including up-front equipment costs and indirect costs (e.g., time off work, travel costs), are warranted.
In interpreting our findings, it is important to consider several limitations. We incorporated all healthcare expenditures into our cost analysis, which potentially included expenditures not related to treatment. For this reason, we based our analysis on a 30-day window pre- and post-treatment rather than on a longer time period. Since this patient population is generally young and healthy (at least 85% of patients in each treatment group had no comorbidities), this concern should be mitigated in this study. A similar limitation is that we did not exclude patients who had a failed procedure, so costs associated with failed procedures within 30 days would be included in the analysis. However, failed procedures will not typically manifest until after the postoperative stent is removed, which is generally near the end or after this 30-day period.28 Another limitation is that we did not incorporate indirect costs, such as work absenteeism and travel time, into our analysis.29,30 These are important factors that are not captured in our data set. However, if anything, our findings underestimate the cost differences among treatments since work absenteeism is likely less in patients undergoing endopyelotomy. Finally, this study does not factor in success rates for the different procedures. The up-front costs of pyeloplasties may be more cost-effective in the long term if their success rates are higher, thus avoiding the inherent costs of treating failed procedures. Nonetheless, understanding the short-term costs associated with surgical treatments has important implications as policymakers begin to implement episode-based bundled payments in payment models.10
Conclusions
Among the three treatments for ureteropelvic junction obstruction, endopyelotomy was the least expensive in the perioperative period. Open and minimally invasive pyeloplasties were more expensive than endopyelotomies, but had similar costs to each other. The similar cost between the two pyeloplasty approaches provides additional evidence that minimally invasive pyeloplasty should be considered the standard treatment for ureteropelvic junction obstruction.
Abbreviations Used
- HCPCS
Healthcare Common Procedure Coding System
- HMO
health maintenance organization
- MRI
magnetic resonance imaging
- MSA
metropolitan statistical area
- PPO
preferred provider organization
- SD
standard deviation
Contributor Information
Collaborators: for the Urologic Diseases in America Project
Acknowledgments
B.J. is supported, in part, by the National Institutes of Health Institutional KL2 award (KL2TR000146-08), the GEMSSTAR award (R03AG048091), the Jahnigen Career Development Award, and the Tippins Foundation Scholar Award. B.H. is supported, in part, by the National Institutes on Aging (R01 AG04871).
Author Disclosure Statement
B.J. is a consultant for ViaOncology. B.H. is an Associate Editor of Urology. For all other authors, no competing financial interests exist.
References
- 1.Schulam PG. Utereropelvic junction obstruction. In: Litwin MS, and Saigal CS, eds. Urologic Diseases in America US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases NIH Publication No 07-5512. Washington, DC: US Government Printing Office, 2007, pp. 323–332 [Google Scholar]
- 2.Baldwin DD, Dunbar JA, Wells N, et al. Single-center comparison of laparoscopic pyeloplasty, Acucise endopyelotomy, and open pyeloplasty. J Endourol 2003;17:155–160 [DOI] [PubMed] [Google Scholar]
- 3.Brooks JD, Kavoussi LR, Preminger GM, et al. Comparison of open and endourologic approaches to the obstructed ureteropelvic junction. Urology 1995;46:791–795 [DOI] [PubMed] [Google Scholar]
- 4.Jacobs BL, Kaufman SR, Morgenstern H, et al. Trends in the treatment of adults with ureteropelvic junction obstruction. J Endourol 2013;27:355–360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oberlin DT, McGuire BB, Pilecki M, et al. Contemporary national surgical outcomes in the treatment of ureteropelvic junction obstruction. Urology 2015;85:363–367 [DOI] [PubMed] [Google Scholar]
- 6.Bansal P, Gupta A, Mongha R, et al. Laparoscopic versus open pyeloplasty: Comparison of two surgical approaches- a single centre experience of three years. J Minim Access Surg 2008;4:76–79 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 7.Yu HY, Hevelone ND, Lipsitz SR, et al. Use, costs and comparative effectiveness of robotic assisted, laparoscopic and open urological surgery. J Urol 2012;187:1392–1399 [DOI] [PubMed] [Google Scholar]
- 8.Chandhoke PS, DeAntoni E. Cost-effectiveness analysis: Application to endourology. J Endourol 1998;12:485–491 [DOI] [PubMed] [Google Scholar]
- 9.Centers for Medicare and Medicaid Services. National health expenditure data. Available from: www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountshistorical.html, Accessed August12, 2016
- 10.Centers for Medicare and Medicaid Services. The Comprehensive Care for Joint Replacement model. Available from: https://innovation.cms.gov/initiatives/CJR, Accessed August12, 2016
- 11.CMS wants to expand mandatory bundled payments—to cardiology. Here's what you need to know. Available from: www.advisory.com/daily-briefing/2016/07/26/cms-mandatory-bundled-payments, Accessed August12, 2016
- 12.Centers for Medicare & Medicaid Services. CMS Quality Measure Development Plan: Supporting the Transition to the Merit-based Incentive Payment System (MIPS) and Alternative Payment Models (APMs) (DRAFT). Available from: www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html, Accessed June16, 2016
- 13.Hansen LG, Chang S. Health research data for the real world: The MarketScan databases. Available from: http://truvenhealth.com/portals/0/assets/PH_11238_0612_TEMP_MarketScan_WP_FINAL.pdf, Accessed June11, 2015
- 14.U.S. Department of Commerce, Bureau of Economic Analysis. Available from: www.bea.gov/National/index.html, Accessed June10, 2015
- 15.Klabunde CN, Potosky AL, Legler JM, et al. Development of a comorbidity index using physician claims data. J Clin Epidemiol 2000;53:1258–1267 [DOI] [PubMed] [Google Scholar]
- 16.Allison PD. Logistic Regression Using SAS: Theory and Application. Cary, NC: SAS Institute, Inc., 1999 [Google Scholar]
- 17.Hopf HL, Bahler CD, Sundaram CP. Long-term outcomes of robot-assisted laparoscopic pyeloplasty for ureteropelvic junction bstruction. Urology 2016;90:106–111 [DOI] [PubMed] [Google Scholar]
- 18.Mir SA, Cadeddu JA, Sleeper JP, et al. Cost comparison of robotic, laparoscopic, and open partial nephrectomy. J Endourol 2011;25:447–453 [DOI] [PubMed] [Google Scholar]
- 19.Bolenz C, Gupta A, Hotze T, et al. Cost comparison of robotic, laparoscopic, and open radical prostatectomy for prostate cancer. Eur Urol 2010; 57:453–458 [DOI] [PubMed] [Google Scholar]
- 20.Mufarrij PW, Woods M, Shah OD, et al. Robotic dismembered pyeloplasty: A 6-year, multi-institutional experience. J Urol 2008;180:1391–1396 [DOI] [PubMed] [Google Scholar]
- 21.Yanke BV, Lallas CD, Pagnani C, et al. The minimally invasive treatment of ureteropelvic junction obstruction: A review of our experience during the last decade. J Urol 2008;180:1397–1402 [DOI] [PubMed] [Google Scholar]
- 22.Klingler HC, Remzi M, Janetschek G, et al. Comparison of open versus laparoscopic pyeloplasty techniques in treatment of uretero-pelvic junction obstruction. Eur Urol 2003;44:340–345 [DOI] [PubMed] [Google Scholar]
- 23.Baker LC. Managed care and technology adoption in health care: Evidence from magnetic resonance imaging. J Health Econ 2001;20:395–421 [DOI] [PubMed] [Google Scholar]
- 24.Simon CJ, Dranove D, White WD: The effect of managed care on the incomes of primary care and specialty physicians. Health Serv Res 1998;33:549–569 [PMC free article] [PubMed] [Google Scholar]
- 25.Baker LC, Wheeler SK. Managed care and technology diffusion: The case of MRI. Health Aff (Millwood) 1998;17:195–207 [DOI] [PubMed] [Google Scholar]
- 26.Jacobs BL, Zhang Y, Skolarus TA, et al. Managed care and the diffusion of intensity-modulated radiotherapy for prostate cancer. Urology 2012;80:1236–1242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weil TP. Accountable care organizations: HMOs by another name? J Fam Pract 2012;61:10. [PubMed] [Google Scholar]
- 28.Desai MM, Desai MR, Gill IS. Endopyeloplasty versus endopyelotomy versus laparoscopic pyeloplasty for primary ureteropelvic junction obstruction. Urology 2004;64:16–21; discussion 21 [DOI] [PubMed] [Google Scholar]
- 29.Hohwu L, Akre O, Pedersen KV, et al. Open retropubic prostatectomy versus robot-assisted laparoscopic prostatectomy: A comparison of length of sick leave. Scand J Urol Nephrol 2009;43:259–264 [DOI] [PubMed] [Google Scholar]
- 30.Penson DF. Editorial comment. J Urol 2012;187:1398. [DOI] [PubMed] [Google Scholar]