Abstract
Background and Purpose: Ureteropelvic junction obstruction is a common condition that can be treated with open pyeloplasty, minimally invasive pyeloplasty, and endopyelotomy. While all these treatments are effective, the extent to which they are used is unclear. We sought to examine the dissemination of these treatments.
Patients and Methods: Using the MarketScan® database, we identified adults 18 to 64 years old who underwent treatment for ureteropelvic junction obstruction between 2002 and 2010. Our primary outcome was ureteropelvic junction obstruction treatment (i.e., open pyeloplasty, minimally invasive pyeloplasty, endopyelotomy). We fit a multilevel multinomial logistic regression model accounting for patients nested within providers to examine several factors associated with treatment.
Results: Rates of minimally invasive pyeloplasty increased 10-fold, while rates of open pyeloplasty decreased by over 40%, and rates of endopyelotomy were relatively stable. Factors associated with receiving an open vs a minimally invasive pyeloplasty were largely similar. Compared with endopyelotomy, patients receiving minimally invasive pyeloplasty were less likely to be older (odds ratio [OR] 0.96; 95% confidence interval [CI], 0.95, 0.97) and live in the south (OR 0.52; 95% CI, 0.33, 0.81) and west regions (OR 0.57; 95% CI 0.33, 0.98) compared with the northeast and were more likely to live in metropolitan statistical areas (OR 1.52; 95% CI 1.08, 2.13).
Conclusions: Over this 9-year period, the landscape of ureteropelvic junction obstruction treatment has changed dramatically. Further research is needed to understand why geographic factors were associated with receiving a minimally invasive pyeloplasty or an endopyelotomy.
Keywords: : ureteropelvic junction obstruction, minimally invasive pyeloplasty, open pyeloplasty, endopyelotomy, MarketScan
Introduction
Ureteropelvic junction obstruction is a common condition that can be managed in several different ways.1 Traditionally, open pyeloplasty was the “gold standard” treatment, but more recently minimally invasive pyeloplasty has become an attractive alternative.2 Endopyelotomy is a third option that is less invasive than both the open and minimally invasive pyeloplasties.3
While all these treatments are effective,3–6 the extent to which they are used is unclear. Although recent studies have shown a rapid increase in the use of minimally invasive pyeloplasty, many of them only compare inpatient procedures (i.e., open and minimally invasive pyeloplasty) and exclude outpatient treatments (i.e., endopyelotomy).2,7 Other studies have shown a high rate of endopyelotomy in certain parts of the country but are not nationally representative and thus lack generalizability.8 As such, there remains a need to better understand the patterns of dissemination. In other urologic conditions, the diffusion of minimally invasive techniques, such as robotic prostatectomy, is associated with both clinical (e.g., age, comorbidity) and nonclinical (e.g., insurance status, region of residence) characteristics.9,10 The degree to which these factors are associated with the use of ureteropelvic junction obstruction treatments is unclear.
For these reasons, we sought to conduct a study that examines the dissemination of open pyeloplasty, minimally invasive pyeloplasty, and endopyelotomy for the treatment of ureteropelvic junction obstruction using a large employer-based data set. Understanding the trends in adoption and the clinical and nonclinical factors associated with use will inform patients, physicians, and policymakers about these three treatments of ureteropelvic junction obstruction, which is particularly important as comparative effectiveness research related to the adoption of robotic surgery continues to be a high priority.11
Patients and Methods
Data source and study population
For this study, we used the Truven Health Analytics MarketScan® Commercial Claims and Encounters Database, which contains data for ∼40 million employees and their dependents.12 Using this data set, we identified adults 18 to 64 years old who underwent treatment for ureteropelvic junction obstruction between 2002 and 2010. Specific treatments included open pyeloplasty (Healthcare Common Procedure Coding System [HCPCS] codes 50400, 50405), minimally invasive pyeloplasty (HCPCS code 50544), and endopyelotomy (HCPCS codes 50575, 52342, 52345, 52346). We only included patients with continuous enrollment in a benefits plan for 6 months before the treatment date to calculate patient comorbidity. Using these criteria, our study population consisted of 1127 open pyeloplasties, 1701 minimally invasive pyeloplasties, and 2238 endopyelotomies.
Outcomes
Our primary outcome was ureteropelvic junction obstruction treatment (i.e., open pyeloplasty, minimally invasive pyeloplasty, or endopyelotomy). We examined the association of several patient, regional, and provider characteristics with treatment. Patient characteristics included age, gender, comorbidity, benefit plan type, employment classification, and employment status. Patient race/ethnicity is not provided in the data set. Comorbidity was reported as a Charlson score, which was calculated using all claims in the 6-month period before treatment.13 Regional characteristics included metropolitan statistical area (MSA) and region of residence. Provider information included the provider MSA. We examined provider volume but did not include this in our model because the volume for the top 10% of providers ranged between two and four cases. This volume is likely inaccurate since it is only accounting for the volume of patients who have health plans providing data to MarketScan and, thus, does not reflect true provider volume.
Statistical analyses
Since MarketScan has HCPCS codes available for inpatient procedures, we performed a sensitivity analysis looking at the assignment of minimally invasive pyeloplasty using HCPCS codes vs an algorithm used previously using a combination of International classification of diseases, 9th revision (ICD-9) codes, and hospital length of stay.14 We calculated a kappa statistic (a standard way to assess the agreement between two categorical measurements) to measure the concordance of these two definitions of minimally invasive pyeloplasty. Our kappa value of 0.48 indicates that there is good agreement between these two definitions (0:40 ≤ κ < 0:75).
Next, we examined differences among patients receiving open pyeloplasty, minimally invasive pyeloplasty, and endopyelotomy using chi-square tests for categorical variables and analysis of variance for continuous variables. Then, we examined trends in treatment over the 9-year period using a chi-square test. Next, we fit a multilevel multinomial logistic regression model, adjusted for age, gender, comorbidity, benefit plan type, employment classification, employment status, region of residence, patient MSA, provider MSA, and treatment year.15 The model accounted for patients nested within providers. We performed a sensitivity analysis restricting the time period to 2002–2007 since more provider information was missing in the latter years (2008–2010). The estimates were largely the same, so we included the years 2002–2010 in our final model.
All analyses were performed using SAS v9.3 (Cary, NC). All tests were 2-tailed, and the probability of a type I error was set at 0.05. The Institutional Review Board of the RAND cooperation determined that the study design was exempt from review.
Results
Characteristics of the patients undergoing open pyeloplasty, minimally invasive pyeloplasty, and endopyelotomy are demonstrated in Table 1. Patients treated with endopyelotomy were older (47.8 years old) compared with minimally invasive pyeloplasty (39.9 years old) and open pyeloplasty (42.2 years old) (p < 0.001). Comorbidity was similar across treatments (p = 0.15). A slightly higher proportion of patients receiving minimally invasive pyeloplasty had preferred provider organization (PPO) insurance (p < 0.001), were salaried (p < 0.001), worked full-time (p = 0.01), and lived in MSAs (p < 0.001). Patients in north central regions were more likely to receive minimally invasive pyeloplasty, whereas those in the south were more likely to receive endopyelotomy (p < 0.001).
Table 1.
Patient Demographics According to Treatment
| Characteristics | Open pyeloplasty (n = 1127) | Minimally invasive pyeloplasty (n = 1701) | Endopyelotomy (n = 2238) | pa |
|---|---|---|---|---|
| Age, mean (SD) | 42.2 (14.9) | 39.9 (14.7) | 47.8 (12.8) | <0.001 |
| Gender, n (%) | ||||
| Female | 640 (57) | 973 (57) | 1285 (57) | 0.94 |
| Male | 487 (43) | 728 (43) | 953 (43) | |
| Comorbidity, n (%) | ||||
| 0 | 955 (85) | 1478 (87) | 1901 (85) | 0.15 |
| 1 or more | 172 (15) | 223 (13) | 337 (15) | |
| Benefit plan type, n (%) | ||||
| HMO | 155 (14) | 201 (12) | 286 (13) | |
| PPO | 698 (62) | 1163 (68) | 1438 (64) | <0.001 |
| Otherb | 274 (24) | 337 (20) | 514 (23) | |
| Employment classification, n (%) | ||||
| Nonsalaried | 300 (27) | 364 (21) | 602 (27) | |
| Salaried | 172 (15) | 331 (20) | 280 (13) | <0.001 |
| Unknown | 655 (58) | 1006 (59) | 1356 (61) | |
| Employment status, n (%) | ||||
| Nonfull-time | 708 (63) | 1032 (61) | 1461 (65) | 0.01 |
| Full-time | 419 (37) | 669 (39) | 777 (35) | |
| MSA status, n (%) | ||||
| Non-MSA | 210 (19) | 239 (14) | 444 (20) | <0.001 |
| MSA | 917 (81) | 1462 (86) | 1794 (80) | |
| Region of residence, n (%) | ||||
| Northeast | 142 (13) | 219 (13) | 261 (12) | |
| North Central | 282 (25) | 527 (31) | 450 (20) | |
| South | 497 (44) | 689 (41) | 1158 (52) | <0.001 |
| West | 187 (17) | 241 (14) | 342 (15) | |
| Unknown | 19 (2) | 25 (1) | 27 (1) | |
Chi-square for categorical variables and ANOVA for continuous variables.
Other includes comprehensive, exclusive provider organization, point of service, point of service with capitation, consumer directed health plan, and missing.
ANOVA = analysis of variance; HMO = health maintenance organization; MSA = metropolitan statistical area; PPO = preferred provider organization; SD = standard deviation.
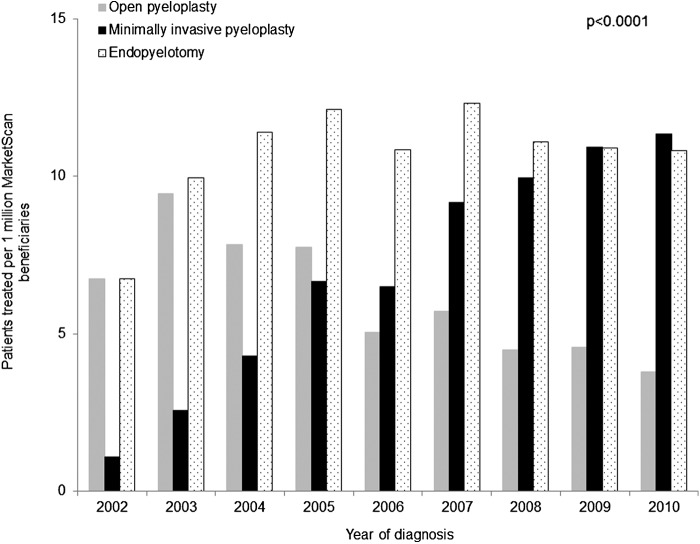
Trends in the use of these three treatments for ureteropelvic junction obstruction are shown in Figure 1. Rates of treatment increased dramatically for minimally invasive pyeloplasty with a concomitant decrease in the rates of open pyeloplasty. Specifically, rates of minimally invasive pyeloplasty increased 10-fold, from 1.1 per million MarketScan beneficiaries in 2002 to 11.3 per million beneficiaries in 2010. Conversely, open pyeloplasty rates decreased by over 40%, from 6.8 per million beneficiaries in 2002 to 3.8 per million beneficiaries in 2010. Rates of endopyelotomy increased from 2002 to 2005 and then tapered off in the latter years.
FIG. 1.
Trends in use of treatments for ureteropelvic junction obstruction. Rates of treatment increased dramatically for minimally invasive pyeloplasty with a concomitant decrease in the rates of open pyeloplasty. Rates of endopyelotomy increased from 2002 to 2005 and then tapered off in the latter years.
Results from our multilevel multinomial logistic regression model are shown in Table 2. Compared with open pyeloplasty, patients receiving minimally invasive pyeloplasty were less likely to be male (odds ratio [OR] 0.75; 95% confidence interval [CI], 0.56, 0.99) and more likely to be salaried as opposed to nonsalaried (OR 1.81; 95% CI, 1.08, 3.04). The likelihood of receiving a minimally invasive vs an open pyeloplasty was similar among the different geographic regions. The likelihood of receiving a minimally invasive pyeloplasty increased with treatment year (OR 1.38; 95% CI, 1.29, 1.49).
Table 2.
Predictors a of Minimally Invasive Pyeloplasty Use: Results of a Multilevel, Multinomial, Logistic Regression Analysis
| Characteristics | Minimally invasive pyeloplasty vs open pyeloplasty | Minimally invasive pyeloplasty vs endopyelotomy |
|---|---|---|
| Age | 0.99 (0.98–1.01) | 0.96 (0.95–0.97) |
| Gender | ||
| Female | 1 | 1 |
| Male | 0.75 (0.56–0.99) | 0.86 (0.68–1.10) |
| Comorbidity | ||
| 0 | 1 | 1 |
| 1 or more | 0.87 (0.59–1.29) | 1.22 (0.86–1.72) |
| Benefit plan typeb | ||
| HMO | 1 | 1 |
| PPO | 1.24 (0.82–1.88) | 1.38 (0.96–1.98) |
| Other | 0.90 (0.55–1.47) | 1.02 (0.67–1.55) |
| Employment classification | ||
| Nonsalaried | 1 | 1 |
| Salaried | 1.81 (1.08–3.04) | 1.56 (0.99–2.44) |
| Unknown | 1.30 (0.85–1.99) | 1.08 (0.75–1.57) |
| Employment status | ||
| Nonfull-time | 1 | 1 |
| Full-time | 1.27 (0.88–1.83) | 1.01 (0.74–1.38) |
| Region of residence | ||
| Northeast | 1 | 1 |
| North Central | 1.08 (0.64–1.84) | 0.96 (0.59–1.57) |
| South | 0.91 (0.55–1.48) | 0.52 (0.33–0.81) |
| West | 0.84 (0.46–1.54) | 0.57 (0.33–0.98) |
| Unknown | 0.62 (0.13–3.01) | 0.62 (0.11–3.37) |
| Patient MSA | 1.19 (0.80–1.76) | 1.52 (1.08–2.13) |
| Provider MSA | 1.59 (0.93–2.71) | 2.06 (1.29–3.30) |
| Treatment year | 1.38 (1.29–1.49) | 1.21 (1.13–1.29) |
The effect of each predictor was adjusted for all other predictors in the model.
Other includes comprehensive, exclusive provider organization, point of service, point of service with capitation, consumer directed health plan, and missing.
Significant values are denoted in bold.
Compared with endopyelotomy, patients receiving minimally invasive pyeloplasty were less likely to be older (OR 0.96; 95% CI, 0.95, 0.97) and less likely to live in the south (OR 0.52; 95% CI, 0.33, 0.81) and west regions (OR 0.57; 95% CI 0.33, 0.98) compared with the northeast. In addition, patients living in MSAs (as opposed to non-MSA) (OR 1.52; 95% CI 1.08, 2.13) and providers living in MSAs (OR 2.06; 95% CI 1.29, 3.30) were associated with a greater likelihood of receiving a minimally invasive pyeloplasty. The likelihood of receiving a minimally invasive pyeloplasty compared with endopyelotomy increased with treatment year (OR 1.21; 95% CI 1.13, 1.29).
The provider volumes were low in all three cases. Specifically, the mean (standard deviation) volume was 1.5 (1.8) for endopyelotomy, 1.8 (2.6) for open pyeloplasty, and 2.1 (2.7) for minimally invasive pyeloplasty. This corresponded to 994 endopyelotomy providers, 971 open pyeloplasty providers, and 563 minimally invasive pyeloplasty providers.
Discussion
From 2002 to 2010, the rate of minimally invasive pyeloplasty increased 10-fold, while the rate of open pyeloplasty decreased by over 40%. The rate of endopyelotomy, the most common treatment, increased early on in the study period and then stabilized. Other than gender, employment classification, and year of treatment, there were no differences in the likelihood of receiving a minimally invasive or an open pyeloplasty. Conversely, the likelihood of receiving a minimally invasive pyeloplasty vs an endopyelotomy was influenced by a patient's age, where they lived, and where their provider lived.
Not surprisingly, there was a shift from an open to a minimally invasive approach for pyeloplasties over this time period. This coincided with the introduction of the daVinci robotic platform (Intuitive Surgical, Sunnyvale, CA). The robotic platform provides advantages of a minimally invasive approach, such as smaller incisions, less pain, and less blood loss.16 Although a laparoscopic approach provides these same benefits,5 it is generally more cumbersome to suture laparoscopically and it is not ergonomic.17,18 Another reason for the adoption of the minimally invasive approach likely pertains to the transfer of skill obtained from using the robotic platform for other procedures. As an example, during this study period, the use of robotic prostatectomy rapidly increased; by 2013, 85% of prostatectomies were done robotically.19 At the same time, providers were becoming more comfortable performing robotic kidney surgery, which uses similar port placement and requires similar steps to expose the kidney and ureter.20
The patients who received open and minimally invasive pyeloplasties had many similarities. They did not differ in terms of age, number of comorbidities, type of health plan, or area of residence (in terms of region and urbanicity). This may reflect the general acceptance of the robotic approach among patients, providers, and payers, as well as the relative comfort of providers with this approach, which eliminates the need to selectively choose healthier patients (e.g., younger and fewer comorbidities). The minimally invasive approach was associated with female patients and those who were salaried, the reason of which is not entirely clear.
In this study, endopyelotomy was performed more commonly than either pyeloplasty approach. Endopyelotomy is a less invasive approach that is performed as an outpatient. This corresponds with the finding that older patients have a lower likelihood of receiving a minimally invasive pyeloplasty. However, failure rates with endopyelotomy are higher.21 Arguably, sicker patients may choose a procedure with a higher failure rate that was safer, but the endopyelotomy patients had a similar number of comorbidities compared with the other two groups. Some of the endopyelotomies may represent secondary treatments for failed primary pyeloplasties, yet with primary pyeloplasty success rates upwards of 90%, this would represent a small number of patients.21 In addition, some endopyelotomies may have been performed primarily for a ureteral stricture more so than for a true ureteropelvic junction obstruction, which can be challenging to differentiate in claims data.
Given the low volumes of procedures noted by surgeon, an alternative explanation is that many providers who perform endopyelotomies may not perform pyeloplasties. Pyeloplasties are a more technically challenging procedure that are more often performed at tertiary referral centers and not in community practice.17 Specialists tend to migrate to academic institutions and urban areas, which may explain in part why minimally invasive pyeloplasties were less likely to be performed in the south and central regions compared with the northeast and were more likely to be performed if patients and/or their providers lived in metropolitan areas.22 Toward the end of the study period (i.e., 2009–2010), the rate of minimally invasive pyeloplasties was higher than endopyelotomy, which may reflect a start of a change in this trend.
The changing landscape of the treatment of ureteropelvic junction obstruction has several implications. More robust outcomes data are needed to assess the comparative effectiveness of these three treatments. Insofar as the morbidity of the minimally invasive approach is low and the success rate is superior to that of endopyelotomy as some prior studies indicate,21,23 more research needs to examine the contexts for primary treatment with endopyelotomy. Perhaps many of these procedures are performed in a salvage setting or more for a ureteral stricture than a true ureteropelvic junction obstruction. However, if large numbers of providers are habitually treating patients with a primary endopyelotomy as the standard of care without considering clinical factors, such as patient age, comorbidities, or patient goals in a shared decision-making process, there may be some value in a policy goal of referral management to increase the number of pyeloplasties performed as a primary treatment.
In interpreting our findings, it is important to consider several limitations. First, this is an observational study using administrative claims data and, thus, is subject to biases related to unmeasured differences among groups. Certain information is not available in MarketScan (e.g., race/ethnicity, income, and body habitus), which may influence our findings. Nonetheless, we adjusted for several patient, regional, and provider characteristics to minimize confounding. Second, our findings may not be generalizable to the uninsured or older populations. MarketScan contains claims for working age adults and their dependents. However, this study focuses on the group of adults that is most likely to receive treatment for ureteropelvic junction obstruction.2 Third, we were unable to adjust for primary vs redo pyeloplasties. However, the primary success rates for both pyeloplasty approaches are high, so we would expect the proportion of redo pyeloplasties in both groups to be low. Fourth, the provider plays an important role in treatment choice, but we were unable to account for specific provider characteristics, such as fellowship training or years in practice. Nonetheless, we were able to fit a multilevel model to account for patients nested within providers, which will indirectly account for some of these factors.
Conclusions
Despite these limitations, this study merits consideration for two reasons. First, there was a congruent increase in the use of minimally invasive pyeloplasty, a decrease in the use of open pyeloplasty, and a relatively stable use of endopyelotomy (the most common treatment of the three) over the 9-year study period. Second, geographic factors (i.e., region of the country and population of where a patient or provider lived) were associated with the receipt of a minimally invasive pyeloplasty or an endopyelotomy. Further work is indicated to elucidate whether or not the treatment variation is warranted.
Abbreviations Used
- CI
confidence interval
- HCPCS
Healthcare Common Procedure Coding System
- HMO
health maintenance organization
- ICD-9
International Classification of Diseases, 9th edition
- MSA
metropolitan statistical area
- OR
odds ratio
- PPO
preferred provider organization
- SD
standard deviation
Contributor Information
Collaborators: for the Urologic Diseases in America Project
Acknowledgments
B.L.J. is supported in part by the National Institutes of Health Institutional KL2 award (KL2TR001856), the GEMSSTAR award (R03AG048091), the Jahnigen career development award, and the Tippins Foundation Scholar Award. B.K.H. is supported in part by the National Institutes on Aging (R01 AG04871).
Author Disclosure Statement
B.L.J. is a consultant for ViaOncology. B.K.H. is an Associate Editor of Urology. For all other authors, no competing financial interests exist.
References
- 1.Schulam PG. Utereropelvic junction obstruction. In: Litwin MS, Saigal CS, eds. Urologic Diseases in America US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases NIH Publication No. 07-5512. Washington, DC: US Government Printing Office, 2007, pp. 323–332 [Google Scholar]
- 2.Sukumar S, Sun M, Karakiewicz PI, et al. . National trends and disparities in the use of minimally invasive adult pyeloplasty. J Urol 2012;188:913–918 [DOI] [PubMed] [Google Scholar]
- 3.Brooks JD, Kavoussi LR, Preminger GM, et al. . Comparison of open and endourologic approaches to the obstructed ureteropelvic junction. Urology 1995;46:791–795 [DOI] [PubMed] [Google Scholar]
- 4.Gogus C, Karamursel T, Tokatli Z, et al. . Long-term results of Anderson-Hynes pyeloplasty in 180 adults in the era of endourologic procedures. Urol Int 2004;73:11–14 [DOI] [PubMed] [Google Scholar]
- 5.Bansal P, Gupta A, Mongha R, et al. . Laparoscopic versus open pyeloplasty: Comparison of two surgical approaches—A single centre experience of three years. J Minim Access Surg 2008;4:76–79 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 6.Feng CC, Dong G, Hang Z, et al. . Ho:YAG Laser endopyelotomy is effective for primary and secondary UPJOs. Minerva Urol Nefrol 2015. [Epub ahead of print] [PubMed] [Google Scholar]
- 7.Monn MF, Bahler CD, Schneider EB, et al. . Emerging trends in robotic pyeloplasty for the management of ureteropelvic junction obstruction in adults. J Urol 2013;189:1352–1357 [DOI] [PubMed] [Google Scholar]
- 8.Jacobs BL, Kaufman SR, Morgenstern H, et al. . Trends in the treatment of adults with ureteropelvic junction obstruction. J Endourol 2013;27:355–360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trinh QD, Sammon J, Sun M, et al. . Perioperative outcomes of robot-assisted radical prostatectomy compared with open radical prostatectomy: Results from the nationwide inpatient sample. Eur Urol 2012;61:679–685 [DOI] [PubMed] [Google Scholar]
- 10.Kowalczyk KJ, Levy JM, Caplan CF, et al. . Temporal national trends of minimally invasive and retropubic radical prostatectomy outcomes from 2003 to 2007: Results from the 100% Medicare sample. Eur Urol 2012;61:803–809 [DOI] [PubMed] [Google Scholar]
- 11.100 Initial Priority Topics for Comparative Effectiveness Research, Institute of Medicine, 2009. Available from: www.nationalacademies.org/hmd/∼/media/Files/Report%20Files/2009/ComparativeEffectivenessResearchPriorities/Stand%20Alone%20List%20of%20100%20CER%20Priorities%20-%20for%20web.ashx Accessed July29, 2016
- 12.Hansen LG, Chang S: Health research data for the real world: The MarketScan databases. Available from: http://truvenhealth.com/portals/0/assets/PH_11238_0612_TEMP_MarketScan_WP_FINAL.pdf Accessed June11, 2015
- 13.Klabunde CN, Potosky AL, Legler JM, et al. . Development of a comorbidity index using physician claims data. J Clin Epidemiol 2000;53:1258–1267 [DOI] [PubMed] [Google Scholar]
- 14.Jacobs BL, Kaufman SR, Morgenstern H, et al. . Trends in the treatment of adults with ureteropelvic junction obstruction. J Endourol 2013;27:355–360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Allison PD. Logistic Regression Using SAS: Theory and Application. Cary, NC: SAS Institute Inc., 1999 [Google Scholar]
- 16.Babbar P, Hemal AK. Robot-assisted urologic surgery in 2010—Advancements and future outlook. Urol Ann 2011;3:1–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marcovich R, Jacobson AI, Aldana JP, et al. . Practice trends in contemporary management of adult ureteropelvic junction obstruction. Urology 2003;62:22–25; discussion 25–26. [DOI] [PubMed] [Google Scholar]
- 18.Moreno-Sierra J, Castillon-Vela I, Ortiz-Oshiro E, et al. . Robotic Anderson-Hynes dismembered pyeloplasty: Initial experience. Int J Med Robot 2013;9:127–133 [DOI] [PubMed] [Google Scholar]
- 19.Leow JJ, Chang SL, Meyer CP, et al. . Robot-assisted versus open radical prostatectomy: A contemporary analysis of an all-payer discharge database. Eur Urol 2016;70:837–845 [DOI] [PubMed] [Google Scholar]
- 20.Sivarajan G, Taksler GB, Walter D, et al. . The effect of the diffusion of the surgical robot on the hospital-level utilization of partial nephrectomy. Med Care 2015;53:71–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yanke BV, Lallas CD, Pagnani C, et al. . The minimally invasive treatment of ureteropelvic junction obstruction: A review of our experience during the last decade. J Urol 2008;180:1397–1402 [DOI] [PubMed] [Google Scholar]
- 22.Pruthi RS, Neuwahl S, Nielsen ME, et al. . Recent trends in the urology workforce in the United States. Urology 2013;82:987–993 [DOI] [PubMed] [Google Scholar]
- 23.Khan F, Ahmed K, Lee N, et al. . Management of ureteropelvic junction obstruction in adults. Nat Rev Urol 2014;11:629–638 [DOI] [PubMed] [Google Scholar]