Abstract
Objectives
The present study determined whether the number of medical conditions was associated with increased occurrence of anxiety and whether triads of medical conditions were associated with anxiety in a nationally representative sample of older Americans. We determined whether multimorbidity findings were unique to anxiety as compared with depressive symptoms.
Methods
4,219 participants (65 or older) completed anxiety and depression measures in the Health and Retirement Study 2006 wave. The logistic regression models’ outcome was elevated anxiety (≥12 on 5-item Beck Anxiety Inventory) or depressive symptoms (≥ on 8-item Center for Epidemiological Studies Depression Scale). The predictor variable was a tally of 7 self-report of doctor-diagnosed conditions: arthritis, cancer, diabetes, heart conditions, high blood pressure, lung disease, and stroke. Analyses were adjusted for age, gender, and depressive or anxiety symptoms. Associations among elevated anxiety or depressive symptoms and 35 triads of medical conditions were examined using Bonferroni corrected chi-square analyses.
Results
Three or more medical conditions conferred a 2.30-fold increase in elevated anxiety (95% CI: 1.44-4.01). Twenty triads were associated with elevated anxiety as compared with 13 associated with depressive symptoms. Six of 7 medical conditions, with the exception being stroke, were present in the majority of triads.
Conclusion
Number of medical conditions and specific conditions are associated with increased occurrence of elevated anxiety. Compared with elevated depressive symptoms, anxiety is associated with greater multimorbidity. Since anxiety and depression cause significant morbidity, it may be beneficial to consider these mental health symptoms when evaluating older adults with multimorbidity.
Keywords: anxiety, comorbidity, chronic conditions, depression, multimorbidity, older adults
Introduction
Anxiety symptoms afflict as many as one in two older patients in clinical settings (Bryant et al., 2008) and are linked to declines in functioning (de Beurs et al., 1999), cognitive impairment (Beaudreau and O'Hara, 2009: Petkus et al., 2016), frailty (Mháolain et al., 2012), and the presence of chronic health conditions. Evidence of anxiety among patients with chronic conditions has been found for hypertension (e.g., Barger and Sydeman, 2005); congestive heart failure (Cully et al., 2009), diabetes (Grigsby et al., 2002), gastrointestinal complaints (e.g., Mussell et al., 2008), and Parkinson's disease (e.g., Starkstein et al., 2014). Moreover, the prevalence of anxiety surpassed that of depression in the case of two chronic conditions: arthritis (Murphy et al., 2012), and congestive obstructive pulmonary disease (Cully et al., 2006). Anxiety occurs both alongside and independent of depression in most aforementioned studies, but researchers have suggested that in presence of co-occurring medical conditions providers recognize depression more often than anxiety (Calleo et al., 2009). Most previous studies have examined the co-occurrence of anxiety with a single comorbid psychiatric or health condition, yet this approach does not reflect the complexity of multi-comorbidities so common among older adults. For instance, in the United States, two-thirds of Medicare beneficiaries, that is, 21.4 million adults, have two or more chronic conditions (Center for Medicare and Medicaid Services, 2012) and half have three or more chronic conditions (American Geriatrics Society (AGS) Expert Panel on the Care of Older Adults with Multimorbidity, 2012). The ubiquity of multiple chronic conditions likely compounds the risk of anxiety symptoms and complicates the treatment of anxiety and medical conditions in late life. Furthermore, whether anxiety symptoms are associated with clusters of chronic medical conditions is largely unknown.
The field of psychiatry describes comorbidity as the co-occurrence of one condition with an index condition (Feinstein, 1970). A specific approach to comorbidity, defined by Kraemer and colleagues (Kraemer, 1995; Kraemer, Wilson, and Hayward, 2006), defines different types of comorbidity that represent differences in underlying causes of the co-occurrence of disorders. Overlap may be due to chance (random comorbidity), shared familial risk factors (familial comorbidity), different presentations of the same underlying disorder (epidemiological comorbidity), or one disorder influencing the prognosis and treatment of the second disorder (clinical comorbidity) (O'Hara, Beaudreau, et al., in preparation). Multimorbidity, namely the presence of multiple chronic conditions in which there is no index condition, has been well-characterized in the field of geriatrics (AGS Expert Panel on the Care of Older Adults with Multimorbidity, 2012). Multimorbidity may be assessed with simple disease counts, or measures of disease severity or burden (e.g., Charlson Comorbidity Index; Charlson et al., 1987), or clinical complexity of combinations of conditions (Zulman et al., 2013). In contrast with geriatrics, the field of psychiatry studies mental health conditions (i.e., index conditions) and thus psychiatry examines questions related to comorbidity with mental health conditions as the index conditions rather than questions related to multimorbidity. Limiting research to pairs of co-occurring conditions may hinder geriatric psychiatry in particular, because many older patients have been reported to have at least three or more conditions (AGS Expert Panel on the Care of Older Adults with Multimorbidity, 2012). Multimorbidity is particularly costly given that individuals with three or more medical conditions account for 49% of Medicare spending in the U.S. (Anderson, 2010). It is imperative that geriatric mental health providers consider the implications of multimorbidity on mental health disorders (e.g., Rej et al., 2015). Thus, the concepts of both multimorbidity and comorbidity have substantial merit for examining the co-occurrence of chronic medical conditions with psychiatric disorders in late life.
In the present study, we blended the two approaches to examine the co-occurrence of conditions. We aimed to characterize the clusters of medical conditions that co-occur with elevated anxiety in a large nationally representative sample of older Americans. We first examined the association of multimorbid medical conditions with elevated anxiety symptoms using a disease count. We hypothesized that the presence of more medical conditions will be associated with increased occurrence of elevated anxiety symptoms. We then tested whether clusters of all possible combinations of any three of the documented medical conditions (i.e., triads) were associated with elevated anxiety symptoms. In light of previous research findings, we hypothesized that medical condition clusters including arthritis, diabetes, heart conditions, and lung disease would be associated with elevated anxiety. In follow up analyses, we conducted the same logistic regression analyses with elevated depressive symptoms and examined whether clusters of medical conditions were associated with elevated depressive symptoms. Since the focus of the paper is anxiety, we did not generate specific hypotheses for the analyses of depressive symptoms as they served as a comparison to anxiety. Examining clusters of medical conditions may help identify potential pathways through which anxiety and medical conditions co-occur and exacerbate one another (i.e., clinical comorbidity).
Methods
Participants
Participants were individuals aged 65 years or older who were randomly selected to complete the Psychosocial Questionnaire in the 2006 wave of the Health and Retirement Study. The 2006 wave of Health and Retirement Study (HRS) public use dataset, was produced and distributed by the University of Michigan with funding from the National Institute on Aging (NIA U01AG009740). The study was reviewed and approved by the University of Michigan Institutional Review Board. The Psychosocial Questionnaire first included anxiety assessment items in the 2006 wave. For the present study, we selected older HRS participants who completed and returned the Psychosocial Questionnaire by mail, which yielded the sample of 4,437 individuals. To be included in our analyses, participants must have completed all five anxiety items, which yielded a sample of 4,219 individuals. The use of HRS sample weights in analyses yielded in a sample of 4,184 individuals.
Measures
Demographic information
The HRS collected demographic information including age, gender, race, ethnicity, marital status, and years of school completed.
Medical Conditions
The HRS assesses the presence of medical conditions using participants’ responses to questions about whether a doctor has “...ever told you that you had [arthritis, cancer, diabetes, a heart condition(s), high blood pressure, lung disease, stroke]?” Affirmative responses were summed to create a variable that represented the total number of medical conditions (0 to 7). Additionally, we also examined all the potential triads that could be created from conditions. Using a mathematical formula we determined the total number of unique combinations of k elements (k = 3) from n conditions (n = 7):
We determined that 35 combinations (triads) are possible from the seven chronic medical conditions.
Depression symptoms
Symptoms of depression were quantified using eight items from the Center for Epidemiological Studies Depression Scale (CES-D; Radloff, 1977) modified to be yes/no questions, with two items reverse-scored. The eight-item CES-D used in the HRS has good internal consistency (α = 0.81 to 0.83; Steffick, 2000). However with the smaller sample used in the present analyses, the internal consistency was slightly diminished (α = 0.78). The cut-point of scores of ≥ 4 suggestive of elevated depressive symptoms was used in the present study (Steffick, 2000).
Anxiety symptoms
Anxiety was measured using five items from the Beck Anxiety Inventory (BAI, Beck and Steer, 1990) selected for the HRS Psychosocial Questionnaire (Clarke et al., 2008). Items assessed: “fear of the worst happening,” “nervous,” hands trembling,” “fear of dying,” “felt faint.” Participants rated each item on a scale ranging from 1 (never) to 4 (most of the time). We define elevated anxiety as scores greater than or equal to 12 on the 5-item BAI used in HRS (Gould et al., 2015). Scores ≥ 12 indicate that individuals experience either three symptoms some of the time or two symptoms most of the time, which indicates a moderate level of anxiety. The 5-item BAI had good internal consistency in the present analyses (α = 0.81).
Statistical Analysis
Analyses were conducted with IBM SPSS Statistics 21.0 (Chicago, IL) using the HRS Psychosocial Questionnaire sampling weight (Ofstedal et al., 2011). We calculated frequencies (unweighted), percentages, standard errors (SE), and descriptive statistics to describe the sample. We examined the association between the number of medical conditions with the presence of elevated anxiety using multiple logistic regression analysis. After fitting the unadjusted models, we fit models adjusted for depressive symptoms, age, and gender to examine the association between number of medical conditions and elevated anxiety in the presence of demographic covariates. We examined whether the number of medical conditions was associated with elevated depressive symptoms in a multivariable adjusted logistic regression model. In follow-up analyses, we examined whether there was a dose-response relationship between number of medical conditions and odds ratios for elevated anxiety symptoms. We also examined whether individual BAI or CES-D items were associated with number of medical conditions using Spearman correlation analyses. Alpha was set at .05 for the analyses.
We examined the association of elevated anxiety with 35 triads of chronic medical conditions using chi-square analyses. The Bonferroni corrected alpha for the chi-square analyses was set at .0015 (p < .05/35).
Results
In our analyses examining older (≥ 65 years) HRS respondents to the 2006 Psychosocial Questionnaire, participants were 74.82 (SE = 0.13) years old, with 12.42 (SE = 0.05) years of education, and mean CES-D scores of 1.40 (SE = 0.03). The mean 5-item BAI total score for the sample was 7.89 (SE = 0.05); 12.9% of the sample had elevated anxiety defined as BAI ≥ 12. Table 1 displays demographic characteristics for the total sample (N = 4184) and for the low anxiety (n = 3667) and elevated anxiety (n = 517) groups.
Table 1.
Participant Characteristics
| Characteristic | All Respondents N = 4184 | Low Anxiety n = 3667 | Elevated Anxiety n = 517 | χ 2 | p |
|---|---|---|---|---|---|
| Age | 9.59 | .03 | |||
| 65-74 years | 2427 (53.4%) | 2150 (54.3%) | 277 (47.3%) | ||
| 75-84 years | 1359 (35.1%) | 1173 (34.3%) | 186 (40.3%) | ||
| ≥ 85 years | 398 (11.5%) | 344 (11.3%) | 54 (12.4%) | ||
| Education | 96.52 | .000 | |||
| < 12 years | 972 (23.5%) | 779 (21.2%) | 193 (39.4%) | ||
| 12 years | 1565 (36.5%) | 1378 (36.9%) | 187 (34.3%) | ||
| ≥13 years | 1647 (40.0%) | 1510 (42.0%) | 137 (26.3%) | ||
| CESD total | 344.28 | .000 | |||
| < 4 | 3614 (87.2%) | 3302 (91.4%) | 312 (61.4%) | ||
| ≥ 4 | 531 (12.8%) | 335 (9.2%) | 196 (38.6%) | ||
| Gender | 9.82 | .005 | |||
| Male | 1831 (43.7%) | 1641 (44.6%) | 190 (37.4%) | ||
| Female | 2353 (56.3%) | 2026 (55.4%) | 327 (62.6%) | ||
| Race | 32.28 | .000 | |||
| White | 3660 (91.4%) | 3249 (92.2%) | 411 (86.0%) | ||
| Black | 459 (7.1%) | 359 (6.2%) | 100 (12.9%) | ||
| Other | 65 (1.5%) | 59 (1.6%) | 6 (1.1%) | ||
| Ethnicity | 9.22 | .003 | |||
| Not Hispanic | 3939 (95.3%) | 3468 (95.7%) | 471 (92.7%) | ||
| Hispanic | 245 (4.7%) | 199 (4.3%) | 46 (7.3%) | ||
| Marital Status | 42.40 | .000 | |||
| Married | 2632 (59.6%) | 2367 (61.4%) | 265 (47.0%) | ||
| Divorced | 388 (9.6%) | 328 (9.4%) | 60 (11.0%) | ||
| Widowed | 1093 (28.7%) | 910 (27.2%) | 183 (39.2%) | ||
| Never married | 71 (2.1%) | 62 (2.1%) | 9 (2.8%) | ||
| Med. Conditions | 87.06 | .000 | |||
| 0 conditions | 330 (7.9%) | 312 (8.5%) | 18 (3.7%) | ||
| 1 condition | 922 (22.2%) | 852 (23.5%) | 70 (12.8%) | ||
| 2 conditions | 1276 (30.4%) | 1144 (30.9%) | 132 (26.6%) | ||
| 3+ conditions | 1656 (39.6%) | 1359 (37.1%) | 297 (56.8%) | ||
| Arthritis | 32.80 | .000 | |||
| Yes | 2881 (70.3%) | 2469 (68.7%) | 412 (80.9%) | ||
| No | 1243 (29.7%) | 1145 (31.3%) | 98 (19.1%) | ||
| Cancer | 8.19 | .010 | |||
| Yes | 823 (20.2%) | 695 (19.5%) | 128 (24.8%) | ||
| No | 3352 (79.8%) | 2965 (80.5%) | 387 (75.2%) | ||
| Diabetes | 16.90 | .000 | |||
| Yes | 896 (21.2%) | 742 (20.2%) | 154 (27.9%) | ||
| No | 3264 (78.8%) | 2902 (79.8%) | 362 (72.1%) | ||
| Heart Condition | 48.09 | .000 | |||
| Yes | 1291 (31.9%) | 1072 (30.0%) | 219 (45.0%) | ||
| No | 2849 (68.1%) | 2559 (70.0%) | 290 (55.0%) | ||
| High BP | 16.42 | .000 | |||
| Yes | 2647 (63.5%) | 2281 (62.3%) | 366 (71.4%) | ||
| No | 1478 (36.5%) | 1337 (37.7%) | 141 (28.6%) | ||
| Lung Disease | 45.93 | .000 | |||
| Yes | 485 (11.9%) | 384 (10.6%) | 101 (20.7%) | ||
| No | 3664 (88.1%) | 3255 (89.4%) | 409 (79.3%) | ||
| Stroke | 4.51 | .060 | |||
| Yes | 293 (7.4%) | 245 (7.0%) | 48 (9.6%) | ||
| No | 3855 (92.6%) | 3395 (93.0%) | 460 (90.4%) |
Note. Displays unweighted counts and weighted percentages calculated using HRS Psychosocial Questionnaire sample weights. BP = blood pressure, Divorced includes both separated and divorced.
Number of Medical Conditions
In unadjusted and multivariable-adjusted logistic regression models, number of medical conditions emerged as a significant predictor of elevated anxiety symptoms (see Table 2). In the unadjusted model the presence of two conditions and three or more conditions yielded a 1.96-fold (95% CI: 1.13-3.41) and 3.49-fold (95% CI: 2.05-5.95) increased occurrence of elevated anxiety respectively, Wald F (3, 4181) = 22.46, p < .001. In the second model adjusted by age, gender, race, ethnicity, and education, number of medical conditions remained a significant predictor of elevated anxiety, Wald F (3, 4181) = 17.08, p < .001. Two conditions were associated with a 1.79-fold (95% CI: 1.02-3.12) increase and three or more conditions were associated with a 3.04-fold (95% CI: 1.77-5.21) increased occurrence of elevated anxiety. The addition of depression to the third model attenuated the association of number of medical conditions and elevated anxiety, but the number of medical conditions remained a significant predictor of elevated anxiety, Wald F (3, 4107) = 9.93, p < .001. Three or more medical conditions conferred a 2.30-fold increased occurrence of elevated anxiety (95% CI: 1.32-4.01).
Table 2.
Logistic Regression of the Association between Number of Chronic Conditions and Elevated Anxiety Symptoms
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Independent Variables | OR (95% CI) | OR (95% CI) | OR (95% CI) |
| Medical Conditions | |||
| 0 | (ref) | (ref) | (ref) |
| 1 | 1.24 (0.70, 2.21) | 1.21 (0.67, 2.16) | 1.11 (0.61, 2.01) |
| 2 | 1.96 (1.13, 3.41) | 1.79 (1.02, 3.12) | 1.44 (0.81, 2.54) |
| 3 or more | 3.49 (2.05, 5.95) | 3.04 (1.77, 5.21) | 2.30 (1.32, 4.01) |
| Age | |||
| 65-74 years | (ref) | (ref) | |
| 75-84 years | 1.15 (0.92, 1.44) | 1.22 (0.97, 1.55) | |
| ≥ 85 years | 1.08 (0.75, 1.53) | 0.93 (0.64, 1.37) | |
| Gender | |||
| Male (ref) | (ref) | (ref) | |
| Female | 1.34 (1.06, 1.65) | 1.14 (0.91, 1.42) | |
| Race | |||
| White | (ref) | (ref) | |
| Black | 1.73 (1.30, 2.31) | 1.61 (1.17, 2.22) | |
| Other | 0.63 (0.23, 1.70) | 0.65 (0.23, 1.82) | |
| Ethnicity | |||
| Non-Hispanic | (ref) | (ref) | |
| Hispanic | 1.52 (1.00, 2.31) | 1.35 (0.86, 2.13) | |
| Education | |||
| <12 years | (ref) | (ref) | |
| 12 years | 0.57 (0.44, 0.74) | 0.67 (0.52, 0.91) | |
| ≥ 13 years | 0.42 (0.32, 0.55) | 0.54 (0.40, 0.72) | |
| CESD total | |||
| < 4 | (ref) | ||
| ≥ 4 | 5.05 (3.94, 6.48) | ||
Note. OR = Odds Ratio, CI = Confidence interval. Bolded values indicate that 95% CI does not cross one.
We modeled the effects of medical conditions on elevated depressive symptoms in a multivariable-adjusted logistic regression model displayed in Table 3. Our findings mirrored those for the anxiety models. The number of medical conditions was a significant predictor of depressive symptoms, Wald F (3, 4107) = 10.46, p < .001. As displayed in Tables 2 and 3, the odds ratios for the association of depressive symptoms with anxiety and anxiety symptoms with depression were very similar in magnitude.
Table 3.
Logistic Regression of the Association between Number of Chronic Conditions and Elevated Depressive Symptoms
| Multivariable-Adjusted Model |
|
|---|---|
| Independent Variables | OR (95% CI) |
| Medical Conditions | |
| 0 | (ref) |
| 1 | 1.69 (0.92, 3.11) |
| 2 | 2.92 (1.64, 5.19) |
| 3 or more | 3.34 (l.90, 5.88) |
| Age | |
| 65-74 years | (ref) |
| 75-84 years | 0.88 (0.70, 1.12) |
| ≥ 85 years | 1.32 (0.92, 1.90) |
| Gender | |
| Male (ref) | (ref) |
| Female | 1.57 (1.25, 1.98) |
| Race | |
| White | (ref) |
| Black | 1.29 (0.94, 1.77) |
| Other | 1.01 (0.48, 2.13) |
| Ethnicity | |
| Non-Hispanic | (ref) |
| Hispanic | 1.71 (1.13, 2.58) |
| Education | |
| <12 years | (ref) |
| 12 years | 0.57 (0.44, 0.75) |
| ≥ 13 years | 0.44 (0.33, 0.59) |
| BAI total | |
| < 12 | (ref) |
| ≥ 12 | 5.10 (3.98, 6.54) |
Note. OR = Odds Ratio, CI = Confidence interval. Bolded values indicate that 95% CI does not cross one.
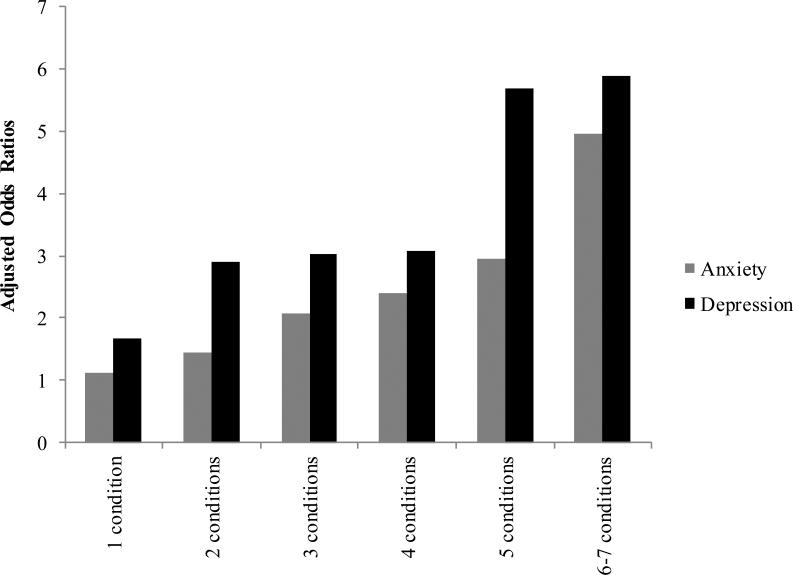
A follow-up dose-response analysis examined the variations in odds ratios for elevated anxiety from one to six medical conditions in a multivariable-adjusted model and the variations in odds ratios for depression in the multivariable-adjusted model. The findings, displayed in Figure 1, demonstrate a plateau effect between five and six conditions for the anxiety model and between four and five medical conditions for the depression model. This difference in plateaus suggests that the conferred risk of the number of medical conditions on anxiety and depression differs. Item level analyses of BAI or CES-D items with associated with number of medical conditions revealed small, statistically significant associations. For the BAI items, the Spearman correlation coefficients ranged from rs = .10, p < .001 for fear of the worst happening to rs =.17, p < .001 for feeling faint. For the CES-D items, the Spearman correlation coefficients ranged from rs = .09, p < .001 for feeling happy (reverse scored) to rs =.18, p < .001 for “could not get going”. Although these correlations were significant, they were substantially smaller than the inter-item correlation coefficients for the BAI items (rs = .38 to .62) or for the CES-D items (rs = .20 to .52).
Figure 1.
Dose-Response Analysis of Association of Elevated Anxiety or Depression with Number of Medical Conditions
Note: Zero conditions was the reference. Only three participants had seven medical conditions and were thus included with those with six conditions. All odds ratios are adjusted by age group, gender, ethnicity, race, education, and either elevated anxiety or depressive symptom status.
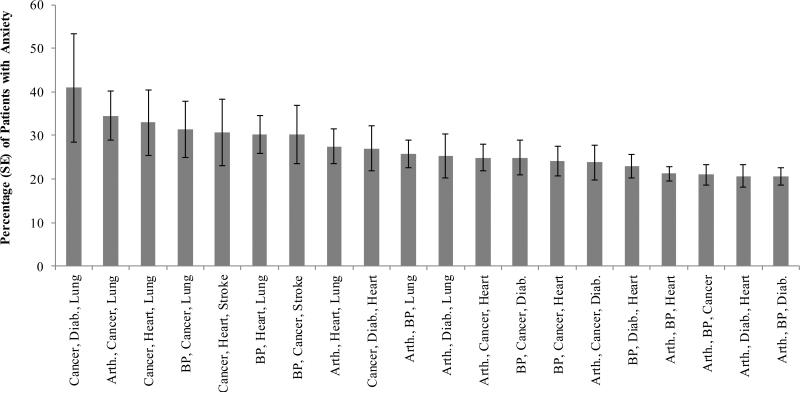
Clusters of Medical Conditions
The seven medical conditions examined yielded 35 unique triads or clusters of medical conditions. Chi-square analyses findings demonstrated that 20 clusters were associated with the increased occurrence of elevated anxiety (see Figure 1). The overall effect size was small for these associations (phi = .06 to .12). In general, six of the seven medical conditions occurred in the majority of clusters displayed in Figure 1. Specifically, of the 20 clusters, 12 clusters included cancer (60%); 10 included arthritis, high blood pressure or heart conditions (50%); eight clusters included lung disease or diabetes (40%); and two clusters included stroke (10%). The prevalence of elevated anxiety in the significant triads ranged from 20.6% (SE = 1.9%) to 40.9% (SE = 12.4%).
Chi-square analyses findings demonstrated that 13 clusters were associated with the increased risk of elevated depression. The overall effect size was small for these associations (phi = .07 to .12). In general, six of the seven medical conditions occurred in the majority of clusters displayed in Figure 1. Of the 13 clusters, eight clusters included arthritis (61.5%), heart conditions (61.5%), or lung disease (61.5%); six included high blood pressure (46.2%) or diabetes (46.2%); three clusters included cancer (23.1%) and no clusters included stroke. The prevalence of elevated depressive symptoms in the significant clusters ranged from 20.3% (SE = 1.9%) to 37.8% (SE = 6.8%). The clusters associated with elevated depression overlapped with those associated with elevated anxiety with the exception of two triads: diabetes, heart conditions, and lung disease; and high blood pressure, diabetes, and lung disease.
Discussion
The present study demonstrated that the majority of older adults with multimorbidity, defined as the presence of three or more conditions, have anxiety. Approximately 40% of participants had three or more medical conditions. Furthermore, the presence of three or more medical conditions confers a 2.3-fold increased likelihood of anxiety in our adjusted models. Yet this association may not be specific to anxiety, since previous work and our own secondary analyses here indicate that the presence of three or more medical conditions are associated with a 3.3-fold increased likelihood of depressive symptoms. The dose-response analysis revealed that the risk of anxiety symptoms substantially increases for older adults with six or more medical conditions, whereas for the risk for depressive symptoms increases for those with five or more conditions, a slightly lower threshold for the number of medical conditions.
Furthermore, over half of the clusters (57%) tested were associated with elevated anxiety. These findings are the first to demonstrate that late-life anxiety symptoms are associated with many different clusters of medical conditions (i.e., multimorbidity) in older Americans. Cancer, arthritis, high blood pressure, and heart conditions were found in more than half of the clusters and lung disease and diabetes were found in 40% of the clusters significantly associated with anxiety. Secondary analyses demonstrated that fewer clusters (37%) were associated with depression. However, the pattern of medical conditions included in the clusters associated with elevated depressive symptoms was similar to those conditions associated with anxiety. Arthritis, lung disease, heart conditions, blood pressure, and diabetes were found in 46% or more of the clusters significantly associated with depressive symptoms. The varied nature of the medical conditions that comprised the clusters associated with elevated anxiety or depression suggests that immunological, respiratory, cardiovascular, and metabolic system dysfunction that could be associated with geriatric mental health issues. Future research should examine trajectories of late-life mental health symptoms as they correspond to development and worsening of medical conditions. Longitudinal trajectories may illuminate the likely multifactorial mechanisms underlying the cross-sectional associations detected in the present study.
The findings from the analysis of triads of medical conditions suggest that a myriad of clusters of medical conditions co-occur with elevated anxiety, which highlights the diverse medical presentations that accompany late-life anxiety. All the medical conditions occurred frequently with the exception of stroke. The lack of an association of stroke with anxiety fits with previous research findings that found that depression commonly occurs alongside stroke (e.g., Pan et al., 2011), however, our follow analyses with depression unexpectedly revealed no association with stroke. This may point to the multiple mechanisms that may underlie late-life depression as put forth by Taylor and colleagues (2013). The authors propose multiple etiologies underlying the vascular depression hypothesis: hypoperfusion, inflammatory processes, and disrupted neural connections. Our finding that cardiovascular problems (e.g., high blood pressure, heart conditions), conditions that affect peripheral vascular functioning (e.g., diabetes), and conditions with inflammatory processes (e.g., rheumatoid arthritis) are associated with elevated depressive symptoms supports the vascular depression hypothesis.
The association of arthritis, diabetes, heart conditions, and lung disease with elevated anxiety fits with findings regarding elevated anxiety and specific medical conditions (e.g., Barger and Sydeman, 2005; Cully et al., 2006; Grigsby et al., 2002; Murphy et al., 2012). These findings also correspond with those of Wetherell and colleagues (2010) who found diabetes to be more prevalent among older adults with Generalized Anxiety Disorder compared with control participants. In summary, these findings highlight that anxiety symptoms are associated with the dysregulation of various systems not limited to respiratory, cardiovascular, metabolic, and inflammatory systems. Again, these findings are not specific to anxiety as demonstrated by our secondary analyses with depression. Future studies can explore mechanisms related to potential shared underlying pathophysiology for anxiety and depression and specific medical conditions. These findings also highlight the importance of including an expanded age range of older adults in geriatric mental health treatment studies as some findings support an upturn in mental health symptoms, specifically worry, among the adults aged 75 years and older (e.g., Neikrug, 2003).
The difference in association of multimorbidity with anxiety (OR = 2.3) and depression (OR = 3.3) could be a function of differences in the cut-points on the measures and how these cut-points were determined. Our follow-up item-level analyses suggest that no single anxiety or depressive symptom underlies the association with number of medical conditions. It is possible that the multitude of medical conditions is what underlies the associations between anxiety and multimorbidity, whereas, for depression, the threshold for multimorbidity is lower. Another possible explanation for the association is that patients who have elevated anxiety or depressive symptoms may receive more medical diagnoses if these symptoms result in patients visiting their doctors more often. Additionally, anxious patients may be more attentive of bodily symptoms compared with their less anxious counterparts, thus leading to more diagnoses. Prospective studies could help determine the direction of the relationship between anxiety, depression, and somatic symptoms.
Multimorbidity occurs among many older patients and is a challenge for primary care providers to manage. Primary care providers juggle many conflicting guidelines for managing these co-occurring medical conditions (Boyd et al., 2005), yet identifying mental health symptoms is paramount. Mental health symptoms reduce adherence to medical regimens (DiMatteo et al., 2000; Stein et al., 2006) and are associated with declines in functioning (e.g, de Beurs et al., 1999; Brenes et al., 2005). Depression is increasingly recognized by multiple disciplines within an interdisciplinary team, yet anxiety is often only recognized by the mental health providers (Karlin and Karel, 2014) if anxiety is recognized at all (Calleo et al., 2009). These findings point to the importance of improving the recognition and treatment of anxiety, in particular, among older patients with six or more medical conditions.
Limitations
The present findings should be interpreted in light of the following limitations. Medical conditions were self-reported of what a doctor told the individuals. Although we did not use biological measures to verify the presence of the medication conditions, a recent study did verify the self-reported diagnosis of diabetes with blood glucose levels in the HRS and found adequate sensitivity and specificity (76.4%; 86.5%) of self-reported diabetes (Ratcliff and Mezuk, 2015). Although Ratcliff and Mezuk performed a careful validation of the measurement of diabetes in the HRS, this validation has not been completed for the remaining six medical conditions examined in the present study. Nevertheless, the use of self-report of doctor-diagnosed medical conditions is a limitation in that self-report relies on the participants’ accurate memory of doctor diagnoses and these diagnoses cannot be cross-checked against prescribed medications. It is possible that there may be some underreporting of medical conditions such as stroke, because people may either not notice the symptoms or mistake them for other issues (Vermeer et al., 2007). The second limitation to the present study was that it did not assess all potential medical conditions and did omit one condition associated with anxiety in older adults, gastrointestinal symptoms (Wetherell et al., 2010). A third limitation is the use of the brief BAI instead of a diagnostic measure of anxiety to characterize late-life anxiety. Without a diagnostic measure and a clinical interview, it is difficult to ascertain the extent to which anxiety symptoms are affected by somatic symptoms of a medical illness or vice versa. Additionally, the brief BAI does not contain questions regarding worrying, a central anxiety symptom for many individuals.
Strengths of the study include the use of a nationally representative sample and innovative methods to identify and validate whether clusters of medical conditions were associated with anxiety. Our findings suggest that providers should evaluate older adults with multimorbidity for anxiety and depressive disorders if even minimal symptoms of anxiety or depression are detected or observed during clinic visits. Future studies need to examine the long-term effects of anxiety on functioning among patients with multimorbidity. Additionally, late-life anxiety treatment studies should begin to examine medical conditions as potential moderators of treatment rather than use covariates (Kraemer, 2015).
Conclusions
Based on our findings, we recommend that mental health and primary care providers consider the presence of anxiety symptoms in individuals with multimorbidity. Given our findings that multimorbidity in anxiety shares similarities with multimorbidity in depression, we recommend screening for both symptoms when multiple medical conditions are present in patients. First, providers must consider medical causes for anxiety and depression, which both include somatic symptoms that overlap considerably with medical disorders. Then, if no clear medical causes are found, providers can treat anxiety and depressive symptoms in patients with multimorbidity. This conclusion aligns with previous research findings of a reduction in somatic symptoms in older adults with Generalized Anxiety Disorder with pharmacological treatment (Lenze et al., 2005). Future research should examine the extent to which behavioral treatments may improve anxiety symptoms in the presence of multimorbidity.
Figure 2.
Percentage of Elevated Anxiety in Triads of Medical Condition
Acknowledgements
Dr. Gould is supported by the United States Department of Veterans Affairs (IK2 RX001478) and by Ellen Schapiro and Gerald Axelbaum through a 2014 NARSAD Young Investigator Grant from the Brain & Behavior Research Foundation. Views expressed in this article are those of the authors and not necessarily those of the Department of Veterans Affairs or the Federal Government.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to disclose.
The authors have no conflicts of interest to disclose related to the manuscript.
References
- American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity Patient-centered care for older adults with multiple chronic conditions: A stepwise approach from the American Geriatrics Society. J Am Geriatr Soc. 2012;60(10):1957–1968. doi: 10.1111/j.1532-5415.2012.04187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson G. Chronic care: Making the case for ongoing care. Robert Wood Johnson Foundation; Princeton, NJ: 2010. [Google Scholar]
- Barger SD, Sydeman SJ. Does generalized anxiety disorder predict coronary heart disease risk factors independently of major depressive disorder? J Affect Disorders. 2005;88(1):87–91. doi: 10.1016/j.jad.2005.05.012. [DOI] [PubMed] [Google Scholar]
- Beaudreau SA, O'Hara R. The association of anxiety and depressive symptoms with cognitive performance in community-dwelling older adults. Psychol Aging. 2009;24(2):507–512. doi: 10.1037/a0016035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Anxiety Inventory. Psychological Corporation; San Antonio, TX: 1990. [Google Scholar]
- Boyd CM, Darer H, Boult C, et al. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: Implications for pay for performance. JAMA. 2005;294(6):716–724. doi: 10.1001/jama.294.6.716. [DOI] [PubMed] [Google Scholar]
- Brenes GA, Guralnik JM, Williamson J, et al. Correlates of anxiety symptoms in physically disabled older women. Am J Geriat Psychiat. 2005;13(1):15–22. doi: 10.1176/appi.ajgp.13.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant C, Jackson H, Ames D. The prevalence of anxiety in older adults: methodological issues and a review of the literature. J Affect Disorders. 2008;109(3):233–250. doi: 10.1016/j.jad.2007.11.008. [DOI] [PubMed] [Google Scholar]
- Calleo J, Stanley MA, Greisinger A, et al. Generalized anxiety disorder in older medical patients: diagnostic recognition, mental health management and service utilization. J Clin Psychol Med S. 2009;16(2):178–185. doi: 10.1007/s10880-008-9144-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Medicare and Medicaid Services . Chronic Conditions among Medicare Beneficiaries, Chartbook. 2012 Edition Baltimore, MD: 2012. [Google Scholar]
- Charlson ME, Pompei T, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chron Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Clarke P, Fisher G, House J, et al. Guide to Content of the HRS Psychosocial Leave-Behind Participant Lifestyle Questionnaires: 2004 & 2006, Documentation Report Version 2.0. Institute for Social Research, University of Michigan; Ann Arbor, MI: 2008. [Google Scholar]
- Cully JA, Graham DP, Stanley MA, et al. Quality of life in patients with chronic obstructive pulmonary disease and comorbid anxiety or depression. Psychosomatics. 2006;47(4):312–319. doi: 10.1176/appi.psy.47.4.312. [DOI] [PubMed] [Google Scholar]
- Cully JA, Jimenez DE, Ledoux TA, et al. Recognition and treatment of depression and anxiety symptoms in heart failure. Primary Care Companion J Clin Psychiatry. 2009;11(3):103–109. doi: 10.4088/pcc.08m00700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Beurs E, Beekman ATF, Van Balkom AJLM, et al. Consequences of anxiety in older persons: its effect on disability, well-being and use of health services. Psychol Med. 1999;29(3):583–593. doi: 10.1017/s0033291799008351. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160(14):2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- Feinstein AR. The pre-therapeutic classification of co-morbidity in chronic disease. J Chron Dis. 1970;23(7):455–468. doi: 10.1016/0021-9681(70)90054-8. [DOI] [PubMed] [Google Scholar]
- Gould CE, Rideaux T, Spira A, et al. Anxiety and depression symptoms in male veterans and non-veterans: The Health and Retirement Study. Int J Geriatr Psychiatr. 2015;30(6):623–630. doi: 10.1002/gps.4193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grigsby AB, Anderson RJ, Freedland KE, et al. Prevalence of anxiety in adults with diabetes: a systematic review. J Psychosom Res. 2002;53(6):1053–1060. doi: 10.1016/s0022-3999(02)00417-8. [DOI] [PubMed] [Google Scholar]
- Karlin BE, Karel MJ. National integration of mental health providers in VA home-based primary care: an innovative model for mental health care delivery with older adults. Gerontologist. 2014;54(5):868–879. doi: 10.1093/geront/gnt142. [DOI] [PubMed] [Google Scholar]
- Kraemer HC. A source of false findings in published research studies adjusting for covariates. JAMA Psychiatry. 2015;72(10):961–962. doi: 10.1001/jamapsychiatry.2015.1178. [DOI] [PubMed] [Google Scholar]
- Kraemer HC. Statistical issues in assessing comorbidity. Statistics in Medicine. 1995;14(8):721–33. doi: 10.1002/sim.4780140803. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson KA, Hayward C. Lifetime prevalence and pseudocomorbidity in psychiatric research. Arch Gen Psych. 2006;63(6):604–608. doi: 10.1001/archpsyc.63.6.604. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Karp JF, Mulsant BH, et al. Somatic symptoms in late-life anxiety: treatment issues. Int J Geriatr Psychiatr. 2005;18(2):89–96. doi: 10.1177/0891988705276251. [DOI] [PubMed] [Google Scholar]
- Mhaoláin AM, Fan CW, Romero-Ortuno R, et al. Frailty, depression, and anxiety in later life. Int Psychogeriatr. 2012;24(8):1265–1274. doi: 10.1017/S1041610211002110. [DOI] [PubMed] [Google Scholar]
- Murphy LB, Sacks JJ, Brady TJ, et al. Anxiety and depression among US adults with arthritis: Prevalence and correlates. Arthrit Care Res. 2012;64(7):968–976. doi: 10.1002/acr.21685. [DOI] [PubMed] [Google Scholar]
- Mussell M, Kroenke K, Spitzer RL, et al. Gastrointestinal symptoms in primary care: Prevalence and association with depression and anxiety. J Psychosom Rese. 2008;64(6):605–612. doi: 10.1016/j.jpsychores.2008.02.019. [DOI] [PubMed] [Google Scholar]
- Neikrug SM. Worrying about a frightening old age. Aging & Mental Health. 2003;7(5):326–333. doi: 10.1080/1360786031000150702. [DOI] [PubMed] [Google Scholar]
- O'Hara R, Beaudreau SA, Gould CE, et al. In Preparation. Handling Clinical Comorbidity in Randomized Clinical Trials in Psychiatry. [DOI] [PubMed]
- Ofstedal MB, Weir DR, Chen KT, et al. Documentation of Updates to HRS Sample Weights in the Health and Retirement Study. Survey Research Center, University of Michigan; Ann Arbor, MI: 2011. [Google Scholar]
- Pan A, Sun Q, Okereke OI, et al. Depression and risk of stroke morbidity and mortality: a meta-analysis and systematic review. JAMA. 2011;306(11):1241–1249. doi: 10.1001/jama.2011.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petkus AJ, Reynolds CA, Wetherell JL, et al. Anxiety is associated with increased risk of dementia in older Swedish twins. Alzheimers Dement. 2016;12(4):399–406. doi: 10.1016/j.jalz.2015.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- Ratliff S, Mezuk B. Depressive Symptoms, Psychiatric Medication Use, and Risk of Type 2 Diabetes: Results from the Health and Retirement Study. Gen Hosp Psychiat. 2015;37(5):420–426. doi: 10.1016/j.genhosppsych.2015.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rej S, Yu C, Shulman K, et al. Medical comorbidity, acute medical care use in late-life bipolar disorder: a comparison of lithium, valproate, and other pharmacotherapies. Gen Hosp Psych. 2015;37(6):528–532. doi: 10.1016/j.genhosppsych.2015.07.001. [DOI] [PubMed] [Google Scholar]
- Starkstein SE, Dragovic M, Dujardin K, et al. Anxiety has specific syndromal profiles in Parkinson disease: a data-driven approach. Am J Geriat Psychiat. 2014;22(12):1410–1417. doi: 10.1016/j.jagp.2013.09.006. [DOI] [PubMed] [Google Scholar]
- Stein MB, Cantrell CR, Sokol MC, et al. Antidepressant adherence and medical resource use among managed care patients with anxiety disorders. Psychiatr Serv. 2006;57(5):673–680. doi: 10.1176/ps.2006.57.5.673. [DOI] [PubMed] [Google Scholar]
- Taylor WD, Aizenstein HJ, Alexopolous GS. The vascular depression hypothesis: mechanisms linking vascular disease with depression. Mol Psychiatry. 2013;18(9):963–974. doi: 10.1038/mp.2013.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [Feb. 22, 2013];The Health and Retirement Study: A Longitudinal Study of Health, Retirement, and Aging; Sponsored by the National Institute on Aging [on-line] Available at http://hrsonline.isr.umich.edu/
- Vermeer SE, Longstreth WT, Koudstaal PJ. Silent brain infarcts: a systematic review. The Lancet Neurol. 2007;6(7):611–619. doi: 10.1016/S1474-4422(07)70170-9. [DOI] [PubMed] [Google Scholar]
- Wetherell JL, Ayres CR, Nuevo R, et al. Medical conditions and depressive, anxiety, and somatic symptoms in older adults with and without generalized anxiety disorder. Aging Ment Health. 2010;14(6):764–768. doi: 10.1080/13607861003713240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zulman DM, Asch SM, Martins SB, et al. Quality of care for patients with multiple chronic conditions: the role of comorbidity interrelatedness. J Gen Intern Med. 2014;29(3):529–537. doi: 10.1007/s11606-013-2616-9. [DOI] [PMC free article] [PubMed] [Google Scholar]