Abstract
Background
Screening, brief intervention, and referral to treatment (SBIRT) is an evidence-based practice that has been shown to reduce alcohol and drug use in healthcare, educational, and other settings, but research on the effectiveness of SBIRT with populations involved in the criminal justice system is limited. These populations have high rates of substance use but have limited access to interventions.
Methods
The study randomized 732 jail inmates from a large urban jail to the SBIRT intervention or to the control group. Using the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST), the intervention assessed the risk level for drug and alcohol misuse by inmates and provided those who were at low or medium risk with a brief intervention in jail and referred those at high risk to community treatment following release, including the opportunity to participate in a brief treatment (eight sessions) protocol. Using interview and records data from a 12-month follow-up, analyses compared the two groups with respect to the primary study outcomes of reductions in drug and alcohol use and the secondary outcomes of participation in treatment, rearrest, reduction in HIV risk behaviors, and quality of life. In addition, the costs of delivering the SBIRT intervention were calculated.
Results
When baseline differences were controlled, the groups did not differ at follow-up on any of the primary or secondary outcomes.
Conclusions
Future research should develop and evaluate SBIRT models that are specifically adapted to the characteristics and needs of the jail population. Until more favorable results emerge, attempts to use SBIRT with jail inmates should be implemented with caution, if at all.
Keywords: Screening, brief intervention, and referral to treatment (SBIRT), Jail, Substance use, Recidivism, HIV risk behaviors, Quality of life, Costs
1. Introduction
Nearly all people with a history of drug use enter the criminal justice system at some time in their drug use career, frequently on a recurring basis. Data from the Arrestee Drug Abuse Monitoring (ADAM II) program in 2013 indicated that between 63% and 83% of arrestees across five cities tested positive for at least one illicit drug at the time of arrest ([ONDCP, 2014). In a national representative survey in 2002 of jail inmates (James, 2004), 66% reported using alcohol regularly and 33% reported using alcohol at the time of the offense for which they were convicted. A re-analysis of this data (Binswanger, Merrill, Krueger, White, Booth, & Elmore, 2010) found that 52.7% of men and 59.3% of women met criteria for drug abuse or dependence; 47.9% of men and 36.9% of women met criteria for alcohol abuse or dependence.
Drug use is closely associated with crime, (MacCoun, Kilmer, & Reuter, 2003; Newcomb, Galaif, & Carmona, 2001; White & Gorman, 2000). A meta-analysis of the literature on drug use and crime (Bennett, Holloway, & Farrington, 2008) found that drug users were three to four times more likely to commit crime than non-drug users. Drug use, particularly when involving injection, also contributes to increased risk of HIV transmission (Taylor, 2009). For substance abusers who are incarcerated, relapse to drug or alcohol use tends to occur within the first few months of release (Belenko, Langley, Crimmins, & Chaple, 2004; Prendergast, Hall, & Wexler, 2003), highlighting the importance of providing intervention options at the pre-release or the reentry phase of the offender’s incarceration. Interventions for treating substance use disorders in the criminal justice system are important for improving public health and reducing criminal behavior (Chandler, Fletcher, & Volkow, 2009).
While many offenders use drugs at levels that do not necessarily require treatment, they are still at risk of progressing to abuse or dependence or of engaging in unhealthy behavior. Interventions for offenders at low or moderate risk are largely lacking within the criminal justice system. One strategy to address this would be to provide early intervention to offenders using approaches that are appropriate to level of risk. Such interventions would provide appropriate care earlier than would otherwise be the case, potentially curtailing progression to higher risk levels and reducing risky behaviors. Offenders who are serving a jail sentence, particularly on drug charges, may be at a “teachable moment” in which they are amenable to an intervention designed to reduce their risk of relapse and rearrest and improve other behaviors.
Screening, brief intervention, and referral to treatment (SBIRT) is a widely promoted intervention that provides universal low-cost screening to a target population using brief, valid, and reliable screening instruments. Based on results from the screening, counselors, health educators, or other staff can identify people at different risk levels and provide types and intensities of intervention in accordance with the level of risk, ranging from information or brief intervention for low-risk users to referral to formal treatment for high-risk users (Babor, McRee, Kassebaum, Grimaldi, Ahmed, & Bray, 2007). Through a combination of early intervention and formal treatment, SBIRT is a public health approach intended to have a positive impact on the drug- and alcohol-related behavior of a broad user population, rather than on the much smaller population of those diagnosed with abuse or dependence. Although the brief interventions that have been used in SBIRT are based on various theoretical orientations, differ in content, and vary in the number of sessions, typically brief interventions are based on motivational interviewing and consist of one to four sessions, with the length of a session varying from 10 minutes to 60 minutes (Jonas et al., 2012; Kaner, Brown, & Jackson, 2011). Studies in healthcare settings have reported that the costs of SBIRT for alcohol users are relatively low and that the benefit-cost ratio is favorable ($3–$4 for every dollar spent; Babor et al., 2007), although similar cost studies have not been conducted for illicit drugs or for SBIRT in nonmedical settings.
Less research has been conducted on SBIRT for illicit drug use than for alcohol use. Early randomized studies of brief intervention for drug use among adults found statistically significant effects for at least one of the primary outcomes (Baker et al., 2005; Bernstein et al., 2005; Copeland et al., 2001; Davis, Baer, Saxon, & Kivlahan, 2003; Humeniuk et al., 2012; McCambridge & Strang, 2004; Stephens, Roffman, & Curtin, 2000; Zahradnik et al., 2009), although some studies found no difference in outcomes (Marsden et al., 2006; Stein, Herman & Anderson, 2009; Woodruff et al., 2014). Also, published articles on SBIRT projects for drug use funded by the Substance Abuse and Mental Health Services Administration (SAMHSA) reported significant reductions in drug use and other problems from baseline to follow-up (Gryczynski et al., 2011; InSight Project Research Group, 2009; Madras et al., 2009; Woodruff, Eisenberg, McCabe, Clapp, & Hohman, 2013), although use of a single-group design in these projects precludes strong conclusions about the causal effect of SBIRT on drug use. The positive findings from this earlier body of research, however, have not been supported by two recent large randomized trials that found no significant effect on illicit drug use in primary healthcare settings (Roy-Byrne et al., 2014; Saitz et al., 2014).
Also, limited rigorous research bearing on the use of SBIRT with offenders is available, whether for alcohol use or illicit drug use (for a recent review of brief interventions for alcohol use disorders in the criminal justice system, see Newbury-Birch et al., 2016). Two randomized studies indicate that brief intervention did lead to positive change among probationers, either for alcohol (Wells-Parker & Williams, 2002) or for alcohol and drugs (Davis et al., 2003). A large (N = 525) randomized, multisite study of SBIRT for harmful alcohol use in probation settings in England found no statistically significant effect on alcohol use at 12 months, although those in the brief intervention group did have a lower reconviction rate than did those in the information-only group (Newbury-Birch et al., 2014). SBIRT for jail inmates has been even less studied than for probationers. One randomized study (Begun, Rose, & Lebel, 2011) of screening and brief intervention with women in jail found improved effects for drug and alcohol use at follow-up (2 months following release), but with no difference between groups for engagement in treatment; only 20.4% of the sample was interviewed for the follow-up. Another study (Stein, Caviness, Anderson, Hebert, & Clarke, 2010) that provided a brief intervention (two sessions) to incarcerated women designed to reduce hazardous drinking found increased abstinence for the treated group at the 3-month follow-up, but this positive effect disappeared at 6 months; in addition, those who did resume drinking tended to do so heavily.
In summary, although SBIRT has been found to be effective in healthcare and other settings, it remains an empirical question whether SBIRT is a feasible intervention for offenders and whether it encourages treatment participation, reduces substance use, and results in other benefits. Given the large proportion of offenders who use drugs and alcohol and who experience problems associated with such use, a relatively low-cost intervention such as SBIRT could have a significant positive impact on public health and safety, if it proves efficacious.
The aims of the SBIRT for Offenders study were to assess whether SBIRT is an effective intervention for jail inmates with respect to participation in interventions tailored to risk level; determine the effectiveness of SBIRT with jail inmates on public health and public safety outcomes at 12 months following study admission; and estimate the cost of providing SBIRT to jail inmates.
The purpose, setting, and design of the study of SBIRT with jail inmates make it a pragmatic trial, as defined by Zwarenstein et al. (2008, p. 2), namely, a study with design choices that “maximise applicability of the trial’s results to usual care settings, rely on unarguably important outcomes such as mortality and severe morbidity, and are tested in a wide range of participants.” The study contributes to the knowledge base on SBIRT in several ways. First, virtually all of the evaluation and dissemination work on SBIRT has occurred in healthcare settings, with little or no attention to the potential benefit of SBIRT for the large population of offenders, most of whom are at risk for drug and/or alcohol problems and for rearrest. This is one of the few experimental studies of the effectiveness of SBIRT with jail inmates. Second, whereas most previous research on SBIRT has focused on alcohol, this study expands the relatively limited evidence base on the effectiveness of SBIRT with persons who use drugs (or drugs and alcohol). Third, the study supplemented the brief intervention and the treatment referral components of SBIRT with a brief treatment protocol for offenders who are at moderate risk or for those who are not willing to commit to longer-term treatment. Fourth, unlike most studies of SBIRT, this study examined the effects of SBIRT on HIV risk behaviors. Finally, the study collected information on the costs associated with providing SBIRT to an offender population.
The primary hypotheses were that, over the 12-month follow-up period, participants in the SBIRT group would be more likely to reduce their level of drug and alcohol use compared with those in the control group. The secondary hypotheses were that participants in the SBIRT group, compared with those in the control group, would be more likely to participate in treatment, less likely to be arrested, less likely to engage in HIV-risk behaviors, and more likely to have a higher quality of life.
2. Methods
The full protocol for the study has previously been published (masked for review). The sections below summarize key features of the study design. The study procedures and informed consent forms were approved by the UCLA General Campus Institutional Review Board. Since this study involved prisoners, it was also reviewed by the federal Office for Human Research Protections.
2.1. Setting and participants
The intervention took place in two jails operated by the Los Angeles Sheriff’s Department (LASD): Men’s Central Jail houses male inmates; Twin Towers Detention Facility houses both male and female inmates. Eligible inmates were all adult (18+) males and females who were within 4 weeks of scheduled release and who were available during the times of recruitment, with the following exceptions: those who (1) did not speak English or Spanish, (2) were unwilling to provide locator information for follow-up, (3) planned to leave the Los Angeles area within 12 months, (4) already had a referral to treatment following release from jail, or (5) were unable to provide informed consent owing to cognitive impairment.
2.2. SBIRT intervention
SBIRT identifies, through a validated screening instrument, an individual’s level of risk and provides (or at least offers) an intervention that is appropriate to the assessed level of risk. The type and intensity of the intervention depend on the level of risk and the degree to which the individual is ready to make changes, as posited in the Stages of Change model (Pre-Contemplation, Contemplation, Preparation, Action, and Maintenance; Prochaska, DiClemente, & Norcross, 1992).
The screening tool used was the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST; Humeniuk et al., 2008). The ASSIST is an instrument developed by the World Health Organization (WHO) to screen for hazardous, harmful, and dependent use of tobacco, alcohol, and drugs (nonmedical use). The ASSIST has high internal consistency across drugs examined (0.77–0.94) and acceptable correlations between ASSIST scores and measures of risk factors for alcohol and drug use problems (0.48–0.76) (Humeniuk et al., 2008). We used a computer-based version of the ASSIST to reduce administration time and to make scoring automatic and immediate. The ASSIST can typically be administered in 5–10 minutes, although it may take longer depending on the number of drugs that the respondent has used during his/her lifetime. For each drug endorsed, the respondent is asked about the frequency of use in the previous 3 months (for this study, the 3 months prior to the current incarceration), problems related to use, dependence indicators, and injection drug use. Following ASSIST administration, separate risk scores for each drug are calculated, with scores falling within a low-, moderate-, or high-risk range. Table 1 shows the risk-level scores for alcohol and drugs and the indicated intervention for each risk level, as specified in the WHO brief intervention manual (Henry-Edwards, Humeniuk, Ali, Monterio, & Poznjak, 2003). The elements of the SBIRT intervention for inmates are described below.
Table 1.
ASSIST risk-level scores and type of intervention.
| ASSIST Alcohol Score | ASSIST Drug Score | Intervention | |
|---|---|---|---|
| Low risk | 0–10 | 0–3 | Feedback on ASSIST score, literature |
| Moderate risk | 11–26 | 4–26 | Feedback on ASSIST score, literature, brief intervention |
| High risk | 27+ | 27+ | Feedback on ASSIST score, literature, brief intervention, referral to treatment |
2.2.1. Low risk for drug and/or alcohol use
Study participants in the SBIRT group who scored at low risk (including no use)1 on the ASSIST received a minimal intervention; that is, they were notified by the health educator of their risk score and its meaning and were given literature on drug and alcohol use, HIV risk behaviors, and HIV testing. This literature was also provided to those who scored at medium or high risk. The health educator also provided participants with a list of treatment resources should they need treatment in the future or to share with family or friends. Although the ASSIST assesses tobacco risk, because of time constraints, the brief intervention did not address tobacco use; however, the literature provided did include advice on smoking cessation.
2.2.2. Moderate risk for drug and/or alcohol use
For those who scored at moderate risk on the ASSIST, the health educator explained the risk score and its meaning and then provided a brief intervention, which took about 15–20 minutes. The brief intervention used a motivational interviewing approach (Miller & Rollnick, 1992). The health educator reviewed the screening score and its meaning, assessed readiness to change, established goals with the client, and reviewed strategies for change. If requested by the client, the health educator provided a referral to treatment following release, including the opportunity to participate in a brief treatment intervention (described below).
Brief treatment (BT), which was available to SBIRT participants following release from jail, is an individual-based intervention that is intended for clients who score at moderate risk. It is designed mainly to help clients who have few complicating problems to learn and develop skills to change their behavior. It is also appropriate for those who score at high risk but who are unwilling to commit to longer-term treatment or for those who are on a waiting list for longer-term treatment. It was offered at no cost to participants assigned to the SBIRT condition. The manualized brief treatment (Beers, 2012) utilized elements of two evidence-based practices: motivational interviewing and cognitive behavioral therapy (Carroll, 1998; Miller & Rollnick, 1992; Substance Abuse and Mental Health Services Administration, 1999) and consisted of eight highly structured sessions delivered in person or by telephone.
2.2.3. High risk for drug and/or alcohol use
For clients who scored at high risk, the health educator provided feedback on the meaning of the screening score and then conducted a brief intervention to encourage the client to attend treatment following release (the “RT” component of SBIRT). The health educator provided printed referral information to one of 19 Community Assessment Services Center (CASC) offices located throughout Los Angeles County. The CASCs conduct assessments for substance use disorders and other problems and then refer clients to appropriate treatment programs. If the client preferred the brief treatment option, the health educator sent the client’s contact information to a counselor at the treatment agency offering the brief treatment, who attempted to contact the client after release from jail to schedule an in-person or telephone appointment. Note that clients had to visit a CASC on their own initiative, whereas health educators actively tried to engage clients who expressed an interest in brief treatment during the brief intervention in jail. Although the brief treatment was offered at no cost (paid for out of grant funds), clients who accessed treatment through the CASCs paid on a sliding scale.
2.3. Selection and training of SBIRT health educators
The health educators were employed by Homeless Health Care-Los Angeles (HHC-LA). All had experience working with offenders with substance use problems, and some had worked on a previous SBIRT study with offenders in Los Angeles (Lee, Rawson, & Beattie, 2012). They received a week-long training in study design, administration and scoring of the ASSIST, brief intervention, brief treatment, and procedures for referral to treatment. The developer of brief treatment participated in the training and subsequently provided refresher training.
2.4. Recruitment, randomization, and baseline interviews
Recruitment took place over 23 months (December 2012 through October 2014), during which 732 inmates agreed to participate in the study.2 The sampling strategy specified that at least 25% of the sample would be women. From a list of potentially eligible inmates provided by jail staff, interviewers called inmates to the interview location, explained the nature of the study, and reviewed the informed consent form, which the inmate signed upon agreeing to participate in the study. Using a set of randomly ordered opaque envelopes prepared at the research center, the interviewer assigned a participant to the SBIRT group (N = 369) or to the comparison group (N = 363). Of inmates who were approached to participate, 57 refused and 198 were ineligible (see Figure 1 for reasons for refusal and ineligibility). All participants who were assigned to the SBIRT group received the brief intervention; none of the control group participants received the brief intervention.
Fig. 1.
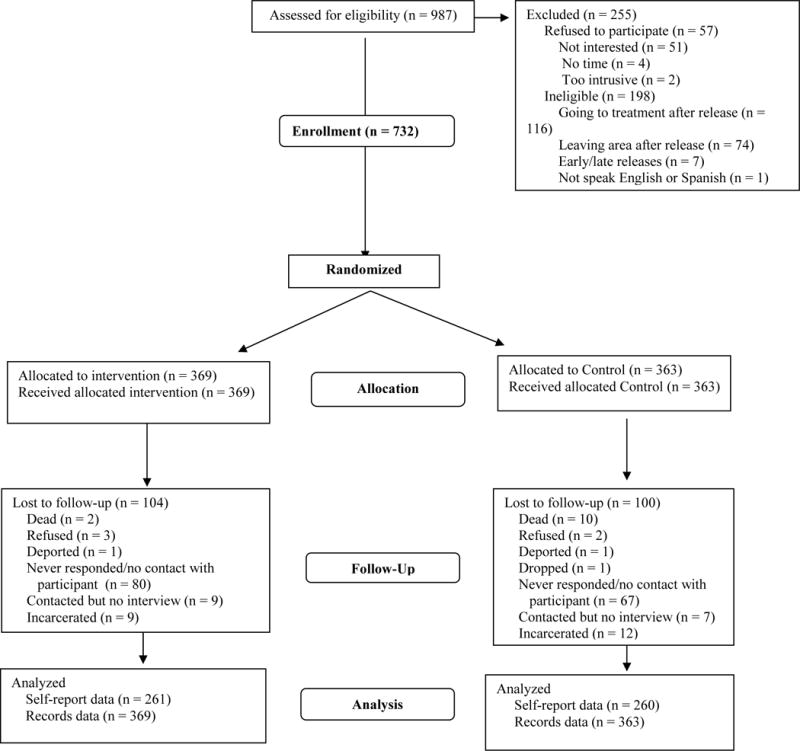
Enrollment and follow-up flow diagram for screening, brief intervention, and referral to treatment for jail inmates.
For participants randomized to the SBIRT group, the interviewer administered the baseline interview, collected locator information to contact participants for the follow-up interview, and then directed the person to meet with the health educator, who administered the ASSIST and conducted the appropriate intervention based on the ASSIST score. The SBIRT intervention occurred with little or no delay after the baseline interview in a private location within the jail.
For participants randomized to the control group, the interviewer administered the baseline interview, obtained locator information, and administered the ASSIST. The interviewer (rather than the health educator) administered the ASSIST to the control participants for two reasons: (1) it ensured that we had comparable data on risk levels for participants in both study groups, and (2) it ensured that control participants received the ASSIST in a research context rather than in a clinical context, in an effort to strengthen the intervention contrast between the two groups. The interviewer informed control participants of their ASSIST risk level and provided them with literature on reducing drug and alcohol use and HIV risk behaviors and with a list of treatment programs in Los Angeles County. Although control participants did not receive a brief intervention that included a referral to treatment, they could, of course, have decided to enroll in treatment on their own, which was determined in the follow-up interview and through agency records.
2.5. Data sources
2.5.1. Baseline interview
The domains covered in the baseline interview were demographic information, drug and alcohol use, treatment history, readiness for treatment, HIV risk behaviors, and crime and criminal justice history. Drug and alcohol history was collected from the ASSIST. Other items were drawn from the intake instrument of the Criminal Justice Drug Abuse Treatment Studies Cooperative (funded by the National Institute on Drug Abuse [NIDA]); the University of Rhode Island Change Assessment Scale (URICA; DiClemente, Schlundt, & Gemmell, 2004); and the HIV risk-behavior items used in the NIDA Clinical Trials Network.3
2.5.2. Follow-up interview
The 12-month follow-up interview included questions and scales on drug and alcohol use (using the ASSIST), participation in treatment, quality of life, HIV risk behaviors, crimes committed, and criminal justice system involvement.4 Quality of life was measured using the WHO Quality of Life–Brief Survey (World Health Organization, 1996; Bonomi, Patrick, Bushnell, & Martin, 2000).
2.5.3. Administrative records
Records on arrest were obtained from the California Department of Justice. Treatment admission information was provided by the Substance Abuse Prevention and Control office of the Los Angeles County Department of Public Health, which maintains data on publicly funded treatment programs.
2.5.4. Cost data
Data on the costs of the SBIRT intervention were collected using the Brief Drug Abuse Treatment Cost Analysis Program (www.datcap.com; French, 2003), which has been frequently used to conduct cost analyses of substance use treatment and related programs, including brief interventions (Kunz, French, & Bazargan-Hejazi, 2004). The analysis was framed from the perspective of the SBIRT provider (HHC-LA and the LASD). The DATCAP asks about costs associated with staff training and monitoring; staff time to conduct screening, brief intervention, and brief treatment5; time spent by sheriff’s department employees to facilitate and/or assist with screening or brief intervention of offenders while they were in jail, equipment and supplies, space costs, contracted services, and indirect/overhead costs. The cost analysis excluded research-related costs such as participant compensation and research staff time conducting baseline and follow-up interviews.
2.6. Interview procedures
The research staff received training in general research practices; a description of study aims, instruments, and interview procedures; confidentiality, informed consent, data integrity, and data security; issues and cautions in working with offenders; and how to recognize and respond to danger to self and others, child abuse, elder/dependent adult abuse, and domestic violence. The baseline interviews were conducted in private spaces at the jail facilities. Weekly project meetings enabled research and counseling staff to quickly identify and address problems in recruitment, data collection, and SBIRT procedures. Consent forms, instruments, and other materials were available in English and Spanish. All but one of the staff who administered the instruments were bilingual in English and Spanish.
Participants were paid $20 for the baseline interview and $60 for the follow-up interview. For interviews in the community, payment was in the form of a gift card provided immediately following the interview (or mailed if a telephone interview). For interviews conducted in jail, payment was either with a money order or cash (depending on institution policies) deposited to the inmate’s trust account.
The locator form completed at baseline contained detailed information to locate participants for follow-up interviews. Other tracking resources included VINELink, an online prisoner locator service; Lexis-Nexis public records database (with access limited to name, address, and phone number); and the California Department of Motor Vehicles.
For convenience and efficiency, follow-up interviews were conducted by telephone (51%). Interviews were also conducted in jails (45%). (We were unable to obtain permission to conduct interviews in state prisons or in most jails other than those in Los Angeles County.) The remainder were conducted in the research office or in the community. Follow-up interviews were conducted with 72% of the full sample. Not counting those who had died, who refused, were deported, or were in jail or prison, the follow-up rate was 76%. The mean time to the follow-up interview was 14.0 months (SD = 4.3), with a range of 10.4 to 35.0 months; time to follow-up did not differ by group (p = 0.64). All participants were included in the request for agency records data (arrest and treatment attendance).
2.7. Analyses
2.7.1. Variables
The independent variable for the outcome analyses is treatment status (i.e., assignment to either the SBIRT group or the comparison group). With respect to dependent variables, in accordance with Consolidated Standards of Reporting Trials (CONSORT) recommendations for randomized trials (Moher, Schulz, & Altman, 2001), we divided the dependent variables (outcomes) into primary and secondary. The two primary outcomes are reductions in the use of drugs and of alcohol (self-report). The secondary outcomes are post-release participation in treatment (self-report and records), rearrest (records), quality of life (self-report), and HIV risk behaviors (self-report). In addition, standard demographic and background baseline variables were examined.
Readiness for change at baseline was determined with the University of Rhode Island Change Assessment (URICA), which has been factored into four subscales reflecting the Stages of Change Model (Prochaska et al., 1992): Precontemplation, Contemplation, Action, and Maintenance. (Table 2 does not include Maintenance since all participants scored zero on that subscale.) A validation study of the URICA with male prisoners confirmed the factor structure of the URICA and indicated that internal consistency was acceptable (alphas 0.60–0.93 for the subscales) (Polascheka, Anstiss, & Wilson, 2010).
Table 2.
Sample characteristics from baseline interview, by group (Self-Report).
| Characteristics | Total | SBIRT | Control | P-value |
|---|---|---|---|---|
| (N = 732) | (n = 369) | (n = 363) | ||
| % M(SD) | % M(SD) | % M(SD) | ||
| Gender | 0.60 | |||
| Male | 72.68 | 71.82 | 73.55 | |
| Female | 27.32 | 28.18 | 26.45 | |
| Race/ethnicity | 0.87 | |||
| White | 25.68 | 25.75 | 25.62 | |
| Black | 30.33 | 30.62 | 30.03 | |
| Hispanic | 34.43 | 33.33 | 33.54 | |
| Multi-racial/Other a | 9.56 | 10.30 | 8.81 | |
| Age at admission | 37.60 (11.44) | 37.01 (11.12) | 38.20 (11.75) | 0.16 |
| Marital status | 0.54 | |||
| Never married | 68.03 | 69.92 | 66.12 | |
| Previously married | 20.08 | 18.97 | 21.21 | |
| Married/living together | 11.89 | 11.11 | 12.67 | |
| Highest level of education | 0.98 | |||
| Less than high school | 34.43 | 34.96 | 33.88 | |
| High school | 35.11 | 34.96 | 35.26 | |
| Trade/tech/some college | 25.27 | 25.20 | 25.34 | |
| 4+ years of college | 5.19 | 4.88 | 5.51 | |
| Employment status prior to incarceration | 0.15 | |||
| Full time | 19.95 | 17.62 | 22.31 | |
| Part time | 28.83 | 31.44 | 26.17 | |
| Unemployedb | 51.23 | 51.95 | 51.52 | |
| Illicit drug use past 3 months* | 0.02 | |||
| Daily/almost daily | 70.64 | 74.93 | 66.39 | |
| Sometimes | 18.98 | 17.27 | 20.66 | |
| No use | 10.39 | 7.80 | 12.95 | |
| Alcohol use past 3 months | 0.15 | |||
| Daily/almost daily | 24.52 | 27.86 | 21.21 | |
| Sometimes | 54.29 | 51.81 | 56.75 | |
| No use | 21.19 | 20.33 | 22.04 | |
| Alcohol risk level | 0.08 | |||
| High | 17.96 | 19.11 | 16.80 | |
| Moderate | 25.00 | 26.04 | 23.97 | |
| Low | 53.73 | 50.14 | 57.30 | |
| Never used | 3.31 | 4.71 | 1.93 | |
| Cannabis risk level** | 0.01 | |||
| High | 12.43 | 11.08 | 13.77 | |
| Moderate | 49.17 | 55.12 | 43.25 | |
| Low | 32.18 | 27.70 | 36.64 | |
| Never used | 6.22 | 6.09 | 6.34 | |
| Cocaine risk level | 0.32 | |||
| High | 12.98 | 13.57 | 12.40 | |
| Moderate | 21.55 | 24.10 | 19.01 | |
| Low | 36.88 | 34.90 | 38.84 | |
| Never used | 28.59 | 27.42 | 29.75 | |
| Amphetamine risk level*** | 0.0001 | |||
| High | 40.33 | 40.72 | 39.94 | |
| Moderate | 23.07 | 30.19 | 15.98 | |
| Low | 8.98 | 9.14 | 8.82 | |
| Never Used | 27.62 | 19.94 | 35.26 | |
| Opioid risk level*** | 0.0003 | |||
| High | 8.70 | 8.31 | 9.09 | |
| Moderate | 11.46 | 15.79 | 7.16 | |
| Low | 13.81 | 16.07 | 11.57 | |
| Never used | 66.02 | 59.83 | 72.18 | |
| Inpatient drug treatment (lifetime) | 1.57 (2.96) | 1.56 (2.75) | 1.57 (3.15) | 0.46 |
| Outpatient drug treatment (lifetime) | 1.00 (4.00) | 0.93 (2.20) | 1.07 (5.25) | 0.44 |
| Lifetime arrests* | 16.03 (20.33) | 17.56 (24.24) | 14.47 (15.24) | 0.04 |
| Times arrested past 3 months | 1.44 (0.93) | 1.46 (0.94) | 1.42 (0.92) | 0.36 |
| Condom use, past 30 days | 0.96 | |||
| Every time | 19.10 | 19.30 | 18.89 | |
| Often | 7.54 | 8.23 | 6.84 | |
| Sometimes | 13.64 | 13.92 | 13.36 | |
| Rarely | 10.27 | 9.81 | 10.75 | |
| Never | 49.44 | 48.73 | 50.16 | |
| Shared needles, past 30 days | 0.28 | |||
| Yes | 71.88 | 75.61 | 67.95 | |
| No | 28.13 | 24.39 | 32.05 | |
| Readiness for change (URICA) | 0.24 | |||
| Precontemplation | 16.53 | 14.36 | 18.73 | |
| Contemplation | 53.01 | 55.28 | 50.69 | |
| Preparation/Action | 30.46 | 30.35 | 30.58 | |
| Preferred assignment | 0.99 | |||
| SBIRT | 26.50 | 26.29 | 26.72 | |
| Control | 19.40 | 19.51 | 19.28 | |
| No preference | 54.10 | 54.20 | 53.99 |
Note: The time periods (e.g., past 3 months) refer to the time prior to the current incarceration. All drug and alcohol measures are based on the ASSIST.
Includes Asian, American Indian, Hawaiian
Includes looking for work, not looking for work, disabled, retired, home caretaker/stay at home parent, student
p ≤ .05;
p ≤ .01;
p ≤ .001
Drug and alcohol use
The effect of the SBIRT intervention on drug use and alcohol use was based on participant responses to the ASSIST. The groups were compared on three measures: (1) use at follow-up, (2) change in risk level from baseline to follow-up, and (3) length of time following release from jail to using drugs or alcohol. At follow-up, use of any illicit drug or alcohol over the past 3 months was categorized as daily/almost daily, sometimes, and no use.
The change in risk was based on the four ASSIST risk levels: never use, low risk, moderate risk, and high risk. Comparing baseline risk and follow-up risk, change in risk was broken into four categories: never used (at either time point), no change in risk (risk level the same at baseline and follow-up) improved risk (from high risk to medium risk or low risk, or from medium risk to low risk), or worse risk (from low risk to medium risk or high risk, or from medium risk to high risk). In addition to the change in risk level for alcohol use, the change in risk level was calculated for four drugs, using the ASSIST terminology: cannabis (marijuana, pot, grass, hash, etc.), cocaine (coke, crack, etc.), amphetamine (speed, diet pills, ecstasy, etc.), and opioids (heroin, morphine, methadone, codeine, etc.).
Because the ASSIST asks about alcohol or drug use behavior in the past 3 months, it does not capture use during the time shortly following release from jail. Two questions on the follow-up interview asked how many days after release did the respondent first use any illicit drug or alcohol.
Treatment participation
In order assess the “referral to treatment” component of SBIRT, treatment participation following release from jail was measured in two ways: self-report and records. Questions on the follow-up interview asked about attendance at outpatient and inpatient (residential) treatment during the 12 months prior to the follow-up interview.6 In addition, a request was submitted to the Substance Abuse Prevention and Control division of the Los Angeles County Department of Public Health, asking whether any study participants were admitted to a publicly funded treatment program in the county over the 12 months following study admission, along with the date of treatment admission. (Note that the time periods for self-report and records data do not correspond: the self-report data covers 12 months prior to the follow-up interview, whereas the records data covers 12 months following baseline.) For the analysis, we limited the time period to 3 months following study admission since, in the absence of knowing why someone went to treatment, it is likely that any admission by SBIRT participants shortly after leaving jail was due to the SBIRT intervention; the farther from release from jail, the more likely other pressures led to treatment admission. The brief intervention focused on participation in formal treatment, if indicated, but also encouraged participation in self-help groups. Thus, self-reported attendance at self-help groups is reported.
Rearrest
Comparison of groups on rearrest over the 12 months following baseline was based on arrest records from the California Department of Justice.
HIV-risk behaviors
HIV risk behavior was measured by two items from the HIV risk assessment questions: one asking about frequency of condom use in the past 30 days, the other asking whether the respondent had shared needles in the past 30 days.
Quality of life
Quality of life at follow-up was measured with the WHO Quality of Life assessment, brief version (WHOQOL-BREF; WHO, 1997). The assessment consists of 26 questions asking about “your life in the last two weeks,” with responses on a 5-point Likert scale, the anchors depending on the nature of the question. The scoring results in four domain scores: Physical, Psychological, Social, and Environment. The final score for each domain ranges from 0–100, with lower scores indicating a lower quality of life in that domain. The instrument has been found to have a high degree of internal consistency (0.82–0.95 across domains) and reproducibility (0.83–0.96) (Bonomi, Patrick, Bushnell, & Martin, 2000).
2.7.2. Outcome analyses
Comparison of the SBIRT group and the control group on background characteristics and outcome measures were tested either by t-test or chi-square. For comparisons where the distribution was excessively skewed, we used the Wilcoxon signed-ranks test. For outcomes on which the two groups differed significantly at baseline, we used a logistic regression model. The level of statistical significance for all comparisons was p ≤ .05.
2.7.3. Cost analysis
The cost analysis focused on estimating total intervention costs for the SBIRT, using data collected with the DATCAP (French, 2003). The analysis year was selected to be 2014, a period when the intervention was running at a steady state. Resources were categorized as counseling personnel, buildings/facilities, equipment, supplies and materials, miscellaneous, and Los Angeles Sheriff’s Department staff time. We calculated both the total annual cost of the SBIRT intervention and the average cost per participant, using the number of participants exposed to the intervention in 2014. To highlight the relative contribution of the cost components to the total operating costs of the intervention, we calculated the percentage of total annual cost accounted for by each cost category. Since control participants received screening by research staff but not the brief intervention while in jail, we did not estimate a cost for this condition.
3. Results
3.1. Baseline characteristics
Table 2 shows data comparing the SBIRT group and the comparison group on selected characteristics at baseline. For most of the characteristics, randomization resulted in balance between groups. There were no statistically significant differences between the groups for the demographic characteristics examined (gender, race/ethnicity, age, marital status, education, employment). Previous treatment participation was low (about once in participants’ lifetime) and did not differ between groups. With regard to HIV status, there were no differences in the frequency of condom use in the past 30 days or in the percentage who shared needles in the past 30 days. The groups did not differ with regard to readiness to change, with just over one-half of each group falling in the contemplation phase. Finally, to assess possible expectancy effects, we asked participants (prior to randomization) whether they would prefer to be in the SBIRT group or the control group, or had no preference. The groups did not differ in assignment preference, with about half of each group having no preference.
There was a significant difference between the groups at baseline for some measures of drug use and arrest history. For any drug use in the 3 months prior to incarceration across the three use categories (daily/almost daily, sometimes, no use), there was a statistically significant difference between the groups, with the percentage reporting daily/almost daily use being higher in the SBIRT group (74.9%) than in the control group (66.4%). There was no difference in level of alcohol use in the 3 months prior to incarceration. With regard to risk-level categories (high risk, moderate risk, low risk, never used), based on the ASSIST score, the groups did not differ in risk levels for alcohol and cocaine, but there were significant differences for cannabis, amphetamine, and opioids. For cannabis, the SBIRT group scored considerably higher in the moderate risk category than the control group (55.1% vs. 43.3%). For amphetamine and opioids, much lower percentages of SBIRT participants reported never having used the drugs than control participants (for amphetamine, 20.0% vs. 35.3%; for opioids, 59.8% vs. 72.2%). Given the similarity between the groups on demographics and other characteristics, these differences in measures of drug use risk are puzzling. A possible explanation is that some participants answered the ASSIST questions differently depending on whether the interviewer was a researcher (control group) or a health educator (SBIRT group).
Self-reported arrests over the 3 months prior to the current incarceration was virtually identical (SBIRT, 1.5; control, 1.4), but the number of lifetime arrests was significantly higher in the SBIRT group than in the control group (17.6 vs. 14.5).
3.2. Outcomes
The comparisons of the study groups on the various outcomes are shown in Table 3.
Table 3.
Comparison of treatment groups on primary and secondary outcomes.
| Characteristics | SBIRT (n = 261) %; M(SD) |
Control (n = 260) %; M(SD) |
P-value |
|---|---|---|---|
| Drug use past 3 monthsa | 0.19 | ||
| Daily/almost daily | 49.43 | 41.92 | |
| Sometimes | 25.67 | 27.31 | |
| No use | 24.90 | 30.77 | |
| Alcohol use past 3 months | 0.12 | ||
| Daily/almost daily | 16.86 | 11.92 | |
| Sometimes | 44.44 | 52.31 | |
| No use | 38.70 | 35.77 | |
| Days following release until drug useb | 32.62 (93.32) | 24.84 (70.49) | 0.11 |
| Days following release until alcohol useb | 27.64 (63.48) | 31.45 (63.24) | 0.16 |
| Change in cannabis risk | 0.95 | ||
| Never Used | 3.88 | 3.05 | |
| Improved Risk | 26.36 | 25.57 | |
| No Change is Risk | 60.08 | 61.45 | |
| Worse Risk | 9.69 | 9.92 | |
| Change in cocaine risk | 0.10 | ||
| Never Used | 19.38 | 21.37 | |
| Improved Risk | 21.71 | 14.50 | |
| No Change is Risk | 46.51 | 46.56 | |
| Worse Risk | 12.40 | 17.56 | |
| Change in amphetamine risk | 0.53 | ||
| Never Used | 18.99 | 22.90 | |
| Improved Risk | 29.07 | 25.57 | |
| No Change is Risk | 40.70 | 38.17 | |
| Worse Risk | 11.24 | 13.36 | |
| Change in opioid risk | 0.13 | ||
| Never Used | 58.14 | 61.07 | |
| Improved Risk | 6.98 | 5.34 | |
| No Change is Risk | 26.36 | 20.23 | |
| Worse Risk | 8.53 | 13.36 | |
| Change in alcohol risk | 0.08 | ||
| Never Used | 3.49 | 0.38 | |
| Improved Risk | 25.97 | 26.34 | |
| No Change is Risk | 61.24 | 63.36 | |
| Worse Risk | 9.30 | 9.92 | |
| Attended inpatient treatment past 12 months | 0.74 | ||
| Yes | 14.67 | 15.71 | |
| Attended outpatient treatment past 12 months | 0.49 | ||
| Yes | 9.27 | 11.11 | |
| Admitted to treatment within 3 months of study entrancec (Agency records) | 0.32 | ||
| Yes | 3.25 | 4.68 | |
| Attended self-help groups following release from jail | 0.74 | ||
| Yes | 28.79 | 27.00 | |
| Arrested within 12 months of follow-upc (Agency records) | 0.047d | ||
| Yes | 61.52 | 54.27 | |
| Condom use, past 30 days | 0.12 | ||
| Every time | 25.41 | 22.96 | |
| Often | 5.95 | 14.29 | |
| Sometimes | 7.57 | 6.12 | |
| Rarely | 6.49 | 6.12 | |
| Never | 54.59 | 50.51 | |
| Shared needles, past 30 days | 0.86 | ||
| Yes | 23.26 | 25.00 | |
| Quality of life (WHOQOL-BREF) | |||
| Physical | 70.04 (23.00) | 70.87 (23.16) | 0.68 |
| Psychological | 68.73 (20.46) | 69.29 (18.84) | 0.74 |
| Social | 62.34 (26.64) | 63.09 (25.92) | 0.74 |
| Environment | 55.85 (22.16) | 58.29 (21.83) | 0.20 |
Note: All data is from self-report, expect where “agency records” is indicated.
All drugs, excludes alcohol.
Wilcoxon signed-rank test due to non-normal distribution.
Includes all respondents enrolled at baseline.
Non-significant (p = 0.07) when controlling for a significant baseline difference in lifetime arrests.
p ≤ .05;
p ≤ .01;
p ≤ .001
Drug and alcohol use
At follow-up, drug use over the 3 months prior to the interview was reported by 75.1% of the SBIRT group and 69.2% of the control group, a nonsignificant difference (p = 0.19). Alcohol use over the past 3 months was also not significantly different between the two groups (p = 0.12): 61.1% for SBIRT and 64.2% for control. Time to complete the 12-month follow-up interviews were much longer than 12 months for some respondents (up to 34 months). As noted above, the groups did not differ by time to follow-up. But to account for any effect of differing time to follow up, this variable was controlled for in multinomial logistic regression models for the two primary outcomes of drug use and alcohol use 3 months prior to follow-up. No significant group differences were found for either drug use (p = 0.37) or alcohol use (p = 0.08), controlling for time to follow-up.
Change in risk level between baseline and follow-up for all drugs examined and for alcohol did not differ significantly between groups. Similarly, no difference was found for the third outcome related to drugs and alcohol—number of days until first use following release. For drugs, the mean days until first use was 32.6 (SD=93.4) for SBIRT and 24.8 (SD=70.5) for control; for alcohol, the mean number was 27.6 (SD=63.5) for the SBIRT group and 31.5 (SD=63.2) for the control group. The distribution was very skewed, with the median days until drug use being 2 for SBIRT and 1 for control; for alcohol use, the medium was 1 for SBIRT and 2 for control. Because of the skewness, we used the Wilcoxon sign-ranks test; neither difference was significant (p = 0.11 for drugs and p = 0.16 for alcohol).
Treatment participation
When asked about participation in treatment over the 12 months prior to the interview, similar percentages of SBIRT and control group participants reported attending inpatient treatment (14.7% vs. 15.1%) and outpatient treatment (9.3% vs. 11.1%). Neither of these differences was significant. A higher percentage of SBIRT participants may have entered treatment shortly after release from prison, encouraged by the discussion with the health educator about the importance of treatment. The records data on treatment participation can help to answer this question. Within 3 months of admission to the study, 3.3% of SBIRT participants and 4.7% of control participants were recorded in agency records as having been admitted to treatment, a nonsignificant difference. Records at HHC LA indicate that only five individuals in the SBIRT group participated in at least one brief treatment session. Reported attendance at a self-group after release from jail was similar for both groups (28.8% for SBIRT, 27.0% for control) and was not statistically significant.
Rearrest
According to records from the California Department of Justice, over half of the study participants were arrested at least once in the 12 months following release from jail; the percentage rearrested was significantly higher for SBIRT participants (61.5%) than for control participants (54.3%). Since the SBIRT group reported a significantly greater number of lifetime arrests at baseline compared with the control group, we controlled for this baseline difference in a logistic regression model of rearrest during the 12 months following study enrollment by the two groups. Once lifetime arrest at baseline was controlled for, the difference between the two groups disappeared (OR = 1.31; p = 0.07).
HIV risk behaviors
With regard to condom use in the past 30 days (for those who reported sexual activity in that period), there were no significant differences between the groups on the frequency categories (every time, often, sometimes, rarely, never). About half of the respondents reported never having used condoms. The second HIV risk behavior outcome was whether the respondent shared needles in the past 30 days (for those who reported drug use in that period). The difference in reporting having shared needles (23.3% SBIRT; 25.0% control) was not significant.
Quality of life
On the four domains of the WHO Quality of Life assessment (Physical, Psychological, Social, and Environment), the scores for the participants in the SBIRT and control groups were nearly the same, with none of the differences being statistically significant.
3.3. Cost outcomes
Results of the cost analysis of SBIRT are presented in Table 4. Six categories of resources are represented: personnel, buildings/facilities, equipment, supplies and materials, miscellaneous, and LA Sheriff’s Department staff time. Over a 12-month period, the total cost of SBIRT was $133,821. More than 80% of total intervention costs were attributable to personnel. Based on 236 participants receiving the intervention over the observation period, the average cost per person was $567.
Table 4.
Costs associated with provision of SBIRT for inmates.
| Resources | Annual Costs |
|---|---|
| Personnel | $107,437 |
| Buildings/Facilities | $4,488 |
| Equipment | $420 |
| Supplies and Materials | $900 |
| Miscellaneous Resources | $9,635 |
| LA Sheriff’s Department staff time | $10,941 |
| Total Annual SBIRT Cost | $133,821 |
| Average Cost per Participant | $567 |
Notes: Costs reported in 2014 dollars. Average cost per participant based on 236 offenders participating in the intervention during 2014.
4. Discussion
This study, one of the few randomized studies to assess the effectiveness of SBIRT with jail inmates, found that participants in the SBIRT group did not have statistically significant better outcomes than those in the control group for measures of drug use, treatment participation, HIV risk behaviors, or quality of life. Although the SBIRT group was more likely to be rearrested than the control group, the difference was not significant after controlling for the baseline difference in lifetime arrests. Previous research on the effectiveness of SBIRT for illicit drug use or with those in the criminal justice system has yielded mixed results, as noted in the Introduction. The results of this study lend support to those studies that have found SBIRT to have no significant impact on drug use in medical settings (Roy-Byrne et al., 2014; Saitz et al., 2014) or on alcohol among probationers (Newbury-Birch et al., 2014; Stein et al., 2010).
4.1. Screening
The screening instrument selected for this study—the ASSIST (Humeniuk, Dennington, & Ali, 2008)—is widely used in SBIRT applications that assess for illicit drug use as well as alcohol use. Because the ASSIST asks seven questions for each of 10 types of drugs, the time to administer the ASSIST can vary considerably depending on the number of drugs that the person endorses (i.e., used in their lifetime). For this study, we used a computer-based version of the ASSIST, which automatically calculated the risk score. The mean time to administer the ASSIST was 9.1 minutes (SD = 6.4). If a paper version of the ASSIST is used, manually calculating the scores for each drug adds to the time.
4.2. Brief intervention
The brief intervention provided to participants in jail was typical of SBIRT applications in that it followed a motivational interviewing model (Miller & Rollnick, 2012) that matched the content of the intervention to the client’s drug(s) of choice and risk level. The health educators had participated in an earlier SBIRT study conducted with inmates being processed through the police department (Lee et al., 2012). The content and procedures of the brief intervention was not explicitly adapted to clients with criminal backgrounds, other than to comply with jail regulations and space availability. Whether such adaptation would result in different outcomes would be worthy of further research.
The duration of brief interventions varies considerably. Some average 5–10 minutes; others last 60 minutes; still others may consist of up to four separate sessions (Jonas et al., 2012; Kaner, Brown, & Jackson, 2011). The brief intervention for this study varied from 5 minutes to 45 minutes, with an average of 23 minutes. Future research could evaluate a protocol that incorporated a longer planned duration to address the more extensive drug use and criminal histories of a jail population. Another possible approach, used in a recent study (Owens & McCrady, 2016), would be to incorporate advice on strengthening social networks into the brief intervention to help reduce substance use following release, whether or not the person participates treatment.
4.3. Referral to treatment
To provide the “referral to treatment” element of SBIRT, all study participants were provided with a list of treatment services in the community. In addition, for those in the SBIRT condition who scored at moderate or high risk, the health educator discussed two treatment options. The first was a list of Community Assessment Services Centers (CASCs) located throughout the county where the person could be assessed and referred to an appropriate treatment program; such a referral list is probably typical of SBIRT interventions that have been evaluated in diverse settings. The second was a specialized brief treatment option offered by a local treatment provider that consisted of an eight-session evidence-based intervention in person or by telephone.
A major difference between these two options was that the person had to take the initiative to call a CASC for services, whereas for the brief treatment, health educators made repeated efforts to contact participants, following their release from jail, who had expressed an interest in brief treatment and provided contact information (which was most of those in the SBIRT group) to ask them to set up an appointment to initiate treatment. In addition to multiple telephone calls and letters, the health educators offered incentives for an initial appointment in the form of bus passes and meal vouchers. These efforts were far greater (and more costly) than is typical in most SBIRT interventions. But the efforts did little to translate “referral to treatment” into actual treatment participation. Only five clients participated in at least one session; none completed more than two sessions. A few study participants (3.3% SBIRT; 4.7% control) did enter treatment at other programs in the county within 3 months of release from jail; for those in the SBIRT group, it is unknown how many did so because they had received the brief intervention in jail.
Limited participation in treatment following SBIRT is not unique to this study. A recent meta-analysis of participation in alcohol treatment services following brief alcohol interventions (Glass et al., 2015) found that across 13 randomized control trials, brief alcohol interventions in medical settings were not effective in increasing receipt of alcohol services following the brief intervention. It was unclear how much effort these studies devoted to promoting participation in treatment. Although models of SBIRT that place increased emphasis on treatment referral may prove effective, such interventions will increase the cost of SBIRT, which undercuts one of its attractions within the continuum of substance use disorder treatment services.
4.4. Costs of SBIRT for jail inmates
SBIRT is considered to be a low-cost approach to assessing need for substance use intervention and connecting individuals to more intensive forms of treatment if needed (Bray et al., 2014; Zarkin, Bray, Davis, Babor, & Higgins-Biddle, 2003). The cost analysis of SBIRT in jail found that the average annual cost per offender was $567 to conduct screening, brief intervention, and referral to brief treatment as needed. Costs were driven primarily by the cost of personnel to conduct the screening and brief intervention portions. Although some staff and administrative costs were expended as part of the brief treatment option, only two clients attended brief treatment sessions during the year chosen for the cost analysis; thus, most of the cost related to brief treatment was incurred in attempting to contact study participants to make an appointment for an initial session. Comparison groups only received screening by UCLA research staff. We did not estimate these screening costs directly, but according to recent studies of SBIRT, the average cost of screening ranges from $1.50 in an outpatient setting to $5.85 in an inpatient setting (Bray et al., 2014). Even at the higher end of this range, the additional components provided to the SBIRT group cost on average $560 more per year than the comparison group.
We were not able to break out personnel costs of the intervention by activity, although most of the resources went into the screening and brief intervention components. Staffing and other agency costs of providing brief treatment are also included here, although few offenders referred to treatment actually engaged in treatment, as discussed above. It is still important to include the opportunity cost of treatment resources because these resources would need to be in place regardless of how many patients take advantage of these services. Still, over time, the lack of engagement in brief treatment and other treatment services may result in an agency reallocating existing staff to support screening and brief intervention services specifically.
4.5. Limitations
The study findings need to be interpreted within the context of several limitations. First, the follow-up rate for interviews was 72%, although arrest and treatment participation records were obtained for virtually all participants. The interview follow-up rate was lower than is often considered standard in evidence-based medicine (generally 80%; Sackett et al., 1997) in order to limit bias in comparing outcomes. Criminal-justice involved persons are a particularly difficult population to track for follow-up given a reluctance to provide detailed tracking information, a transient life style, wariness of being contacted, and little or no contact with family members. The increasing use of mobile phones added to the difficulty of contacting participants for a follow-up interview. Even if an interview was scheduled, no-shows were not uncommon. Providing more than $60 for the follow-up interview might have led to higher participation. Higher payments for follow-up interviews do not appear to increase drug use or perceived coercion, but they do lead to higher follow-up rates (Festinger, Marlowe, Dugosh, Croft, & Arabia, 2008). But incentives can only be set at a level that an IRB would approve.
Second, most of the variables were based on self-report. Although there is often concern about the validity of self-report, prior research indicates that self-report interviews, when properly conducted, are generally reliable and valid in measuring drug and alcohol use (Buchan, Dennis, Tims, & Diamond, 2002; Darke, 1998) and criminal involvement (Thornberry & Krohn, 2000). Arrest and treatment participation following release from jail were based on records.
Third, several researchers (Bernstein et al., 2005; Clifford & Maisto, 2000; Jenkins, McAlaney, & McCambridge, 2009; Kaner et al., 2009) have noted that the treatment effects of a brief intervention may be difficult to disentangle from research effects—that is, research assessments in themselves may have a therapeutic effect for all study participants, thus diluting treatment effects. Although this study did not formally assess this possibility through manipulation, we attempted to reduce the impact of research effects by limiting the amount of data collected at baseline and by having the research interviewer (rather than the health educator) administer the ASSIST to participants in the control group. This procedure could still have resulted in a research effect on outcomes; however, this was unavoidable if we wished to collect self-report baseline data that could not be obtained from records.
Finally, the findings of this study are based on a sample of jail inmates in an urban area. Caution should be exercised in extending the findings beyond this population and setting. Applying the findings to “real world” settings is also limited by the fact that this was a research study. The participants were probably not typical of jail inmates who would be the intended population of SBIRT in routine practice. They were willing to participate in research activities, were compensated for their participation in research, and received an intervention from carefully trained and monitored counselors. These necessary research conditions would not be present in a typical setting that provided SBIRT to offenders, and thus, the effects found may be different in a “real world” setting.
5. Conclusion
Screening, brief intervention, and referral to treatment (SBIRT) provides a bridge between primary prevention and treatment by conducting early identification and intervention with people whose current use may be low but who are at risk for future alcohol and drug problems and by referring those with likely abuse or dependence to longer-term treatment. The public health assumption informing SBIRT is that individual reductions in alcohol and drug use, when aggregated over a large at-risk population, can have significant health, public health, and public safety effects (Anderson, Aromaa, & Rosenbloom, 2008).
For this study of SBIRT with jail inmates, participants in the treatment condition did not have better outcomes than those in the control condition. It may be that SBIRT needs to be more closely tailored to the characteristics and needs of people with extensive criminal and drug-use histories; or it may simply be that SBIRT is not effective with this population. SBIRT has become an increasingly popular element in the continuum of intervention for substance use disorders. This study suggests that, in the absence of further research on the use of SBIRT with a jail population, policy makers and treatment specialists should exercise caution in rolling out SBIRT interventions with this population.
Highlights.
This study tests the effectiveness of Screening, Brief Intervention, and Referral to Treatment with jail inmates in a randomized control trial design
The study collected 12-month follow-up data by interview and through records
The SBIRT group and the control group did not differ significantly on the primary outcomes of alcohol and drug use or on the secondary outcomes of treatment participation, rearrest, quality of life, and HIV risk behaviors.
Acknowledgments
This study was supported by National Institute on Drug Abuse grant R01DA031879. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or of the participating agencies. We are grateful for the willingness of the Los Angeles County Sheriff’s Department and Homeless Healthcare Los Angeles to participate in the study. At the latter, Mario Gonzalez, Yanira Lopez, Delia Mojarro, and Monica Quezada participated in brief treatment and brief intervention activities. The arrest data and the treatment participation data were provided by the California Department of Justice and the Substance Abuse Prevention and Control division of the Los Angeles County Department of Public Health, respectively. We acknowledge the contribution of Thomas Beers in preparing the Brief Treatment Manual and in providing training to the health educators. Expert research assistance was provided by Liliana Gregorio, Jason Grossman, Aida Santos, and Kory van Unen. Special appreciation is due to Jerry Cartier, who expertly served as project director until his retirement. Finally, the study could not have occurred without the willing participation of our study subjects.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Since this study regarded SBIRT as a universal intervention within a target setting, it (potentially) included inmates who (at least by self-report) had not used drugs or alcohol.
In the original protocol for this study, the sample size was 800. Because of problems encountered in recruiting participants, we reduced the sample size to 732. Doing so increased the detectable effect size from d = .20 to .22.
Seven baseline ASSIST interviews with SBIRT participants were lost, but other baseline data for them are available.
The original protocol included biological drug and alcohol tests at follow-up. Because it soon became clear that many of the interviews would be conducted by telephone or in jail, where samples could not be obtained, we decided to drop biological testing.
The cost data did not include efforts by the Community Assessment Services Centers to provide assessment and referral for those participants who showed up at one of the Centers for assessment.
The follow-up interview also asked about “brief treatment,” which was intended to refer specifically to the brief treatment provided by HHC-LA. But since participants in the control group would not have known what “brief treatment” referred to and since SBIRT participants may have forgotten the discussion of “brief treatment” during the brief intervention in jail, we decided not to include this variable in the analysis.
Trial registration number: NCT01683643
References
- Anderson P, Aromaa S, Rosenbloom D, Enos G. Screening and brief intervention: Making a public health difference. Boston, MA: Join Together, Boston University School of Public Health; 2008. [Google Scholar]
- Babor T, McRee B, Kassebaum P, Grimaldi P, Ahmed K, Bray J. Screening, brief intervention, and referral to treatment (SBIRT): Toward a public health approach to the management of substance abuse. Substance Abuse. 2007;28:7–30. doi: 10.1300/J465v28n03_03. [DOI] [PubMed] [Google Scholar]
- Baker A, Lee NK, Claire M, Lewin TJ, Grant T, Pohlman S, Carr VJ. Brief cognitive behavioural interventions for regular amphetamine users: A step in the right direction. Addiction. 2005;100:367–378. doi: 10.1111/j.1360-0443.2005.01002.x. [DOI] [PubMed] [Google Scholar]
- Beers T. Brief treatment manual. Los Angeles: Integrated Substance Abuse Programs; 2012. [Google Scholar]
- Begun AL, Rose SJ, LeBel TP. Intervening with women in jail around alcohol and substance abuse during preparation for community reentry. Alcoholism Treatment Quarterly. 2011;29(4):453–478. [Google Scholar]
- Belenko S, Langley S, Crimmins S, Chaple M. HIV risk behaviors, knowledge, and prevention among offenders under community supervision: A hidden risk group. AIDS Education and Prevention. 2004;16:367–385. doi: 10.1521/aeap.16.4.367.40394. [DOI] [PubMed] [Google Scholar]
- Bennett T, Holloway K, Farrington D. The statistical association between drug misuse and crime: A meta-analysis. Aggression and Violent Behavior. 2008;13(2):107–118. [Google Scholar]
- Bernstein E, Edwards E, Dorfman D, Heeren T, Bliss C, Bernstein J. Screening and brief intervention to reduce marijuana use among youth and young adults in a pediatric emergency department. Academic Emergency Medicine. 2009;16:1174–1185. doi: 10.1111/j.1553-2712.2009.00490.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein J, Bernstein E, Tassiopoulos K, Heeren T, Levenson S, Hingson R. Brief motivational intervention at a clinic visit reduces cocaine and heroin use. Drug and Alcohol Dependence. 2005;77:49–59. doi: 10.1016/j.drugalcdep.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Binswanger IA, Merrill JO, Krueger PM, White MC, Booth RE, Elmore JG. Gender differences in chronic medical, psychiatric, and substance-dependence disorders among jail inmates. American Journal of Public Health. 2010;100(3):476–482. doi: 10.2105/AJPH.2008.149591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonomi AE, Patrick DL, Bushnell DM, Martin M. Validation of the United States’ version of the World Health Organization Quality of Life (WHOQOL) instrument. Journal of Clinical Epidemiology. 2000;53(1):1–12. doi: 10.1016/s0895-4356(99)00123-7. [DOI] [PubMed] [Google Scholar]
- Bray JW, Mallonee E, Dowd W, Aldridge A, Cowell AJ, Vendetti J. Program-and service-level costs of seven screening, brief intervention, and referral to treatment programs. Substance Abuse and Rehabilitation. 2014;5:63–73. doi: 10.2147/SAR.S62127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchan BJ, Dennis ML, Tims FM, Diamond GS. Cannabis use: Consistency and validity of self-report, on-site urine testing, and laboratory testing. Addiction. 2002;97(Suppl 1):98–108. doi: 10.1046/j.1360-0443.97.s01.1.x. [DOI] [PubMed] [Google Scholar]
- Carroll KM. A cognitive-behavioral approach: Treating cocaine addiction. Rockville, MD: National Institute on Drug Abuse; 1998. (NIH Publication No. 98-44308). [Google Scholar]
- Chandler RK, Fletcher BW, Volkow ND. Treating drug abuse and addiction in the criminal justice system: Improving public health and safety. JAMA. 2009;301(2):183–190. doi: 10.1001/jama.2008.976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clifford PR, Maisto SA. Subject reactivity effects and alcohol treatment outcome research. Journal Studies of Alcohol. 2000;61:787–793. doi: 10.15288/jsa.2000.61.787. [DOI] [PubMed] [Google Scholar]
- Copeland J, Swift W, Roffman R, Stephens R. A randomized controlled trial of brief cognitive behavioral interventions for cannabis use disorder. Journal of Substance Abuse Treatment. 2001;21(1):55–64. doi: 10.1016/s0740-5472(01)00179-9. [DOI] [PubMed] [Google Scholar]
- Darke S. Self-report among injecting drug users: A review. Drug and Alcohol Dependence. 1998;51:253–263. doi: 10.1016/s0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- Davis TM, Baer JS, Saxon AJ, Kivlahan DR. Brief motivational feedback improves post-incarceration treatment contact among veterans with substance use disorders. Drug and Alcohol Dependence. 2003;69:97–203. doi: 10.1016/s0376-8716(02)00317-4. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Schlundt D, Gemmell L. Readiness and stages of change in addiction treatment. American Journal on Addictions. 2004;13:103–119. doi: 10.1080/10550490490435777. [DOI] [PubMed] [Google Scholar]
- Festinger DS, Marlowe DB, Dugosh KL, Croft JR, Arabia PL. Higher magnitude cash payments improve research follow-up rates without increasing drug use or perceived coercion. Drug and Alcohol Dependence. 2008;96(1):128–135. doi: 10.1016/j.drugalcdep.2008.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French MT. Drug Abuse Treatment Cost Analysis Program (DATCAP): Program version. 8th. Coral Gables, FL: University of Miami; 2003. [Google Scholar]
- French MT, Salomé HJ, Sindelar JL, McLellan AT. Benefit-cost analysis of addiction treatment: Methodological guidelines and application using the DATCAP and ASI. Health Services Research. 2003;37:433–455. doi: 10.1111/1475-6773.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass JE, Hamilton AM, Powell BJ, Perron BE, Brown RT, Ilgen MA. Specialty substance use disorder services following brief alcohol intervention: A meta-analysis of randomized controlled trials. Addiction. 2015;110(9):1404–1415. doi: 10.1111/add.12950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gryczynski J, Mitchell SG, Peterson TR, Gonzales A, Moseley A, Schwartz RP. The relationship between services delivered and substance use outcomes in New Mexico’s Screening, Brief Intervention, Referral and Treatment (SBIRT) Initiative. Drug and Alcohol Dependence. 2011;118:152–157. doi: 10.1016/j.drugalcdep.2011.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry-Edwards S, Humeniuk R, Ali R, Monterio M, Poznjak V. Brief intervention for substance use: A manual for use in primary care (Draft version 1.1 for field testing) Geneva: World Health Organization; 2003. [Google Scholar]
- Humeniuk R, Ali R, Babor T, Souza-Formigoni ML, de Lacerda RB, Ling W, Vendetti J. A randomized controlled trial of a brief intervention for illicit drugs linked to the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) in clients recruited from primary health-care settings in four countries. Addiction. 2012;107:957–966. doi: 10.1111/j.1360-0443.2011.03740.x. [DOI] [PubMed] [Google Scholar]
- Humeniuk RE, Ali RA, Babor TF, Farrell M, Formigoni ML, Jittiwutikarn J, Simon S. Validation of the Alcohol Smoking and Substance Involvement Screening Test (ASSIST) Addiction. 2008;103:1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- Humeniuk R, Dennington V, Ali R, on behalf of the WHO ASSIST Phase III Study Group . The effectiveness of a brief intervention for illicit drugs linked to the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) in primary health care settings: A technical report of Phase III findings of the WHO Assist randomized control trial. Geneva: World Health Organization; 2008. [Google Scholar]
- InSight Project Research Group. SBIRT outcomes in Houston: Final report on InSight, a hospital district-based program for patients at risk for alcohol or drug use problems. Alcoholism: Clinical and Experimental Research. 2009;33:1374–1381. doi: 10.1111/j.1530-0277.2009.00967.x. [DOI] [PubMed] [Google Scholar]
- James DJ. Profile of jail inmates, 2002 (NCJ 201932) Washington, DC: Bureau of Justice Statistics, U. S. Department of Justice; 2004. [Google Scholar]
- Jenkins RJ, McAlaney J, McCambridge J. Change over time in alcohol consumption in control groups in brief intervention studies: Systematic review and meta-regression study. Drug and Alcohol Dependence. 2009;100:107–114. doi: 10.1016/j.drugalcdep.2008.09.016. [DOI] [PubMed] [Google Scholar]
- Jonas DE, Garbutt JC, Amick HR, Brown JM, Brownley KA, Council CL, Harris RP. Behavioral counseling after screening for alcohol misuse in primary care: A systematic review and meta-analysis for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2012;157(9):645–654. doi: 10.7326/0003-4819-157-9-201211060-00544. [DOI] [PubMed] [Google Scholar]
- Kaner EFS, Brown N, Jackson K. A systematic review of the impact of brief interventions on substance use and co-morbid physical and mental conditions. Mental Health and Substance Use. 2011;4(1):38–61. [Google Scholar]
- Kaner EFS, Dickinson HO, Beyer F, Pienaar E, Schlesinger C, Campbell F, Heather N. The effectiveness of brief alcohol interventions in primary care settings: A systematic review. Drug and Alcohol Dependence. 2009;28:301–323. doi: 10.1111/j.1465-3362.2009.00071.x. [DOI] [PubMed] [Google Scholar]
- Kunz FM, French MT, Bazargan-Hejazi S. Cost-effectiveness analysis of a brief intervention delivered to problem drinkers presenting at an inner-city hospital emergency department. Journal on Studies of Alcohol. 2004;65:363–370. doi: 10.15288/jsa.2004.65.363. [DOI] [PubMed] [Google Scholar]
- Lee A, Rawson R, Beattie R. Supporting access to alcohol and other drug treatment: The Los Angeles County screening, brief intervention, and referral to treatment project for short-term jail detainees. Addiction Science and Clinical Practice. 2012;7(Suppl. 1):A57. [Google Scholar]
- MacCoun R, Kilmer B, Reuter P. Research on drugs-crime linkages: The next generation. In: Brownstein HH, Crossland C, editors. Toward a drugs and crime research agenda for the 21st century. Washington, DC: National Institute of Justice; 2003. pp. 65–95. [Google Scholar]
- Madras BK, Compton WM, Avula D, Stegbauer T, Stein JB, Clark HW. Screening, brief interventions, and referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: Comparison at intake and 6 months later. Drug and Alcohol Dependence. 2009;99:280–295. doi: 10.1016/j.drugalcdep.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsden J, Stillwell G, Barlow H, Boys A, Taylor C, Hunt N, Farrel M. An evaluation of a brief motivational intervention among young ecstasy and cocaine users: No effect on substance and alcohol use outcomes. Addiction. 2006;101:1014–1026. doi: 10.1111/j.1360-0443.2006.01290.x. [DOI] [PubMed] [Google Scholar]
- McCambridge J, Strang J. The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: Results from a multi-site cluster randomized trial. Addiction. 2004;99:39–52. doi: 10.1111/j.1360-0443.2004.00564.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. New York: Guilford; 1992. [Google Scholar]
- Moher D, Schulz K, Altman D. The CONSORT statement: Revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA. 2001;285:1987–1991. doi: 10.1001/jama.285.15.1987. [DOI] [PubMed] [Google Scholar]
- Newbury-Birch D, Coulton S, Bland M, Cassidy P, Dale V, Deluca P, Drummond C. Alcohol screening and brief interventions for offenders in the probation setting (SIPS trial): A pragmatic multicentre cluster randomized controlled trial. Alcohol and Alcoholism. 2014;49(5):540–548. doi: 10.1093/alcalc/agu046. [DOI] [PubMed] [Google Scholar]
- Newbury-Birch D, McGovern R, Birch J, O’Neill G, Kaner H, Sondhi A, Lynch K. A rapid systematic review of what we know about alcohol use disorders and brief interventions in the criminal justice system. International Journal of Prisoner Health. 2016;12(1):57–70. doi: 10.1108/IJPH-08-2015-0024. [DOI] [PubMed] [Google Scholar]
- Newcomb MD, Galaif ER, Carmona V. The drug-crime nexus in a community sample of adults. Psychology of Addictive Behaviors. 2001;15:185–193. doi: 10.1037//0893-164x.15.3.185. [DOI] [PubMed] [Google Scholar]
- ONDCP [Office of National Drug Control Policy] ADAM II: 2013 annual report. Washington, DC: Office of National Drug Control Policy, Executive Office of the President; 2014. [Google Scholar]
- Owens MD, McCrady BS. A pilot study of a brief motivational intervention for incarcerated drinkers. Journal of Substance Abuse Treatment. 2016;68:1–10. doi: 10.1016/j.jsat.2016.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polascheka DLL, Anstiss B, Wilson M. The assessment of offending-related stage of change in offenders: Psychometric validation of the URICA with male prisoners. Psychology, Crime & Law. 2010;16(4):305–325. [Google Scholar]
- Prendergast M, Hall E, Wexler H. Multiple measures of outcome in assessing a prison-based drug treatment program. Journal of Offender Rehabilitation. 2003;37:65–94. [Google Scholar]
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: Applications to addictive behaviors. American Psychologist. 1992;47:1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne P, Bumgardner K, Krupski A, Dunn C, Ries R, Donovan D, Zarkin GA. Brief intervention for problem drug use in safety-net primary care settings: A randomized clinical trial. JAMA. 2014;312(5):492–501. doi: 10.1001/jama.2014.7860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sackett DL, Richardson WS, Rosenberg W, Haynes R. Evidence-based medicine: How to practice and teach EBM. New York: Churchill Livingstone; 1997. [Google Scholar]
- Saitz R, Palfai TP, Cheng DM, Alford DP, Bernstein JA, Lloyd-Travaglini CA, Samet JH. Screening and brief intervention for drug use in primary care: The ASPIRE randomized clinical trial. JAMA. 2014;312(5):502–513. doi: 10.1001/jama.2014.7862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MD, Caviness CM, Anderson BJ, Hebert M, Clarke JG. A brief alcohol intervention for hazardously drinking incarcerated women. Addiction. 2010;105(3):466–475. doi: 10.1111/j.1360-0443.2009.02813.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MD, Herman DS, Anderson BJ. A motivational intervention trial to reduce cocaine use. Journal of Substance Abuse Treatment. 2009;36(1):118–125. doi: 10.1016/j.jsat.2008.05.003. [DOI] [PubMed] [Google Scholar]
- Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. Journal of Consulting and Clinical Psychology. 2000;68:898–908. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Brief intervention and brief therapies for substance abuse (Treatment Improvement Protocol 34) Rockville, MD: SAMHSA; 1999. [Google Scholar]
- Taylor M. Achieving better outcomes for adult probation. 2009 http://www.lao.ca.gov/2009/crim/Probation/probation_052909.pdf.
- Thornberry TP, Krohn MD. The self-report method for measuring delinquency and crime. In: Duffee D, Crutchfield RD, Mastrofski S, Mazerolle L, McDowall D, editors. Criminal justice 2000: Measurement and analysis of crime and justice. Vol. 4. Washington, DC: National Institute of Justice/Department of Justice; 2000. pp. 33–83. [Google Scholar]
- Wells-Parker E, Williams M. Enhancing the effectiveness of traditional interventions with drinking drivers by adding brief individual intervention components. Journal on Studies of Alcohol. 2002;63:655–664. doi: 10.15288/jsa.2002.63.655. [DOI] [PubMed] [Google Scholar]
- White HR, Gorman DM. Criminal justice 2000 (Vol. 1; pp. 51–218). The nature of crime: continuity and change. Washington, DC: US Department of Justice; 2000. Dynamics of the drug-crime relationship. [Google Scholar]
- WHO [World Health Organization] WHOQOL-BREF: Introduction, administration, scoring and generic version of the assessment. Geneva: World Health Organization; 1996. [Google Scholar]
- WHO [World Health Organization] WHOQOL: Measuring quality of life. Geneva: World Health Organization; 1997. [Google Scholar]
- Woodruff SI, Eisenberg K, McCabe C, Clapp JD, Hohman M. Evaluation of California’s alcohol and drug screening and brief intervention project for emergency department patients. Western Journal of Emergency Medicine. 2013;14:263–270. doi: 10.5811/westjem.2012.9.11551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodruff SI, Clapp JD, Eisenberg K, McCabe C, Hohman M, Shillington AM, Gareri J. Randomized clinical trial of the effects of screening and brief intervention for illicit drug use: The Life Shift/Shift Gears study. Addiction Science & Clinical Practice. 2014;9(8) doi: 10.1186/1940-0640-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahradnik A, Otto C, Brackau B, Löhrmann I, Bischof G, John U, Rumpf HJ. Randomized controlled trial of a brief intervention for problematic prescription drug use in non-treatment-seeking patients. Addiction. 2009;104:109–117. doi: 10.1111/j.1360-0443.2008.02421.x. [DOI] [PubMed] [Google Scholar]
- Zarkin GA, Bray JW, Davis KL, Babor TF, Higgins-Biddle JC. The costs of screening and brief intervention for risky alcohol use. Journal of Studies on Alcohol and Drugs. 2003;64(6):849–857. doi: 10.15288/jsa.2003.64.849. [DOI] [PubMed] [Google Scholar]
- Zwarenstein M, Treweek S, Gagnier JJ, Altman DG, Tunis S, Gent BHM, Moher D, for the CONSORT and Pragmatic Trials in Healthcare groups Improving the reporting of pragmatic trials: An extension of the CONSORT statement. BMJ. 2008;337:a2390. doi: 10.1136/bmj.a2390. [DOI] [PMC free article] [PubMed] [Google Scholar]


