Abstract
Background
Compared with men, women are at higher risk of rehospitalization in the first month after discharge for AMI. However, it is unknown if this risk extends to the full year, and if this varies by age. Explanatory factors potentially mediating the relationship between sex and rehospitalization remain unexplored and are needed to reduce readmissions. The aim of this study was to assess sex differences and factors associated with 1 year rehospitalization rates after acute myocardial infarction (AMI).
Methods
We recruited 3,536 patients (33% women) hospitalized with AMI aged ≥18 years from twenty-four U.S. centers into the Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status (TRIUMPH) study. Data were obtained by medical record abstraction and patient interviews, and a physician panel adjudicated hospitalizations within the first year after AMI. We compared sex differences in rehospitalization using a Cox proportional hazards model, following sequential adjustment for covariates and testing for an age-sex interaction.
Results
One-year crude all-cause rehospitalization rates for women were significantly higher than men following AMI (HR=1.29 for women, 95% CI 1.12, 1.48). Following adjustment for demographics and clinical factors, women had a persistent 26% higher risk of rehospitalization (HR=1.26, 95% CI 1.08, 1.47). However, following adjustment for health status and psychosocial factors (HR=1.14, 95% CI 0.96, 1.34), the association was attenuated. There was no significant age-sex interaction for 1 year rehospitalization, suggesting that the increased risk applied to both older and younger women.
Conclusion
Women, regardless of age, have a higher risk of rehospitalization compared with men over the first year after AMI. While the increased risk persisted following adjustment for clinical factors, the poorer health and psychosocial state of women attenuated the difference.
Keywords: Acute myocardial infarction, Readmission, Sex differences, Women
INTRODUCTION
Based on data predominately from the elderly Medicare population, it is known that patients aged 65 years and older have a high rehospitalization rate up to 1 year following acute myocardial infarction (AMI), approaching or exceeding 50%.1 For example, women are at higher risk of rehospitalization than men,2–6 particularly during the first month after discharge.7 However, much about these associations is unexamined as prior studies predominately used shorter-term outcomes and administrative claims data, limiting the ability to consider clinical, patient-centered data in understanding the increased risks in women.
To better understand potential disparities in rehospitalization rates of women and men, we used data from the multi-center Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status (TRIUMPH) study.8 TRIUMPH provides data on adjudicated rehospitalizations and a depth of patient, clinical and treatment factors that might be associated with rehospitalization after AMI. Our objectives were to: (a) examine sex differences in the incidence of all-cause rehospitalization 1 year after AMI; (b) assess the independent association of sex with 1 year rehospitalization by sequential adjustment for socio-demographics, risk factors, disease severity and psychosocial factors and whether there was an interaction between age and sex to determine whether sex differences in rehospitalization are prevalent for both younger (≤55 years) and older patients (>55 years), given that younger women have been shown to have poorer outcomes and worse recovery 1 year after AMI.9–11 Our hypothesis was that women, particularly younger women, have a higher risk of rehospitalization up to 1 year following AMI, which would be explained by differences in clinical characteristics, health status, and psychosocial factors.
METHODS
Participants and Study Design
Between April 2005 and December 2008, 4340 patients hospitalized with AMI were enrolled into the TRIUMPH study, a prospective, 24-center United States study designed to investigate disparities in health outcomes following AMI.8 The methodology of TRIUMPH has been previously described.8 In brief, patients were eligible if they were ≥18 years of age, had an elevated troponin or creatinine kinase-MB blood test during the initial 24 hours of admission and presented with other evidence supporting the diagnosis of AMI (e.g., 20 minutes of ischemic symptoms or electrocardiographic ST-changes). Patients who did not present to the enrolling institution were eligible only if they were transferred within the first 24 hours of presentation. Patients who developed elevated cardiac enzymes as a complication of elective coronary revascularization were excluded. The institutional review board at each institution approved the study and participants gave informed consent.
For our study, we further excluded patients who were discharged against medical advice (N=10), transferred to another facility during their hospitalization (N=86), died in-hospital (N=24) or were missing rehospitalization data (N=684), resulting in a final cohort of 3,536 patients (2,366 men and 1,170 women).
Data Collection and Study Definitions
Baseline hospitalization data were collected by medical chart abstraction and standardized in-person interviews administered by trained personnel within the first 72 hours of the index AMI admission. Detailed information on socio-demographic/socio-economic factors (SES), medical history and presentation characteristics were collected by interview and chart abstraction (Table 1).
Table 1.
Baseline characteristics of all patients stratified by sex.
| Total Sample (N=3,536) |
Men (N=2,366) |
Women (N=1,170) |
P-Value | |
|---|---|---|---|---|
| Socio-Demographics (%) | ||||
| Age (Mean±SD) | 59.2 ± 12.0 | 58.0 ± 11.4 | 61.4 ± 12.7 | < 0.001 |
| Race | ||||
| White | 2475 (70.2%) | 1766 (74.9%) | 709 (60.8%) | |
| Black | 822 (23.3%) | 433 (18.4%) | 389 (33.3%) | < 0.001 |
| Other | 229 (6.5%) | 160 (6.8%) | 69 (5.9%) | |
| No health insurance | 738 (21.2%) | 505 (21.7%) | 233 (20.3%) | 0.346 |
| Married | 1891 (53.5%) | 1461 (61.7%) | 430 (36.8%) | < 0.001 |
| High school education | 2830 (80.4%) | 1928 (81.8%) | 902 (77.6%) | 0.003 |
| Employment status | ||||
| Not working | 1737 (49.5%) | 991 (42.2%) | 746 (64.3%) | |
| Working full time | 1430 (40.8%) | 1134 (48.3%) | 296 (25.5%) | < 0.001 |
| Working part time | 341 (9.7%) | 222 (9.5%) | 119 (10.2%) | |
| Difficulty getting care | ||||
| Extremely difficult | 237 (6.8%) | 140 (6.0%) | 97 (8.3%) | |
| Moderately difficult | 215 (6.1%) | 134 (5.7%) | 81 (7.0%) | |
| Somewhat difficult | 348 (9.9%) | 225 (9.6%) | 123 (10.6%) | 0.021 |
| Not very difficult | 415 (11.8%) | 285 (12.2%) | 130 (11.2%) | |
| No problem at all | 2292 (65.4%) | 1561 (66.6%) | 731 (62.9%) | |
| Medical History (%) | ||||
| Hypertension | 2315 (65.5%) | 1454 (61.5%) | 861 (73.6%) | < 0.001 |
| Diabetes | 1040 (29.4%) | 615 (26.0%) | 425 (36.3%) | < 0.001 |
| Current Smoking | 2095 (59.2%) | 1487 (62.8%) | 608 (52.0%) | < 0.001 |
| Chronic Heart Failure | 258 (7.3%) | 160 (6.8%) | 98 (8.4%) | 0.082 |
| Chronic Lung Disease | 245 (6.9%) | 123 (5.2%) | 122 (10.4%) | < 0.001 |
| Chronic Kidney Disease | 231 (6.5%) | 152 (6.4%) | 79 (6.8%) | 0.710 |
| Peripheral Vascular Disease | 167 (4.7%) | 98 (4.1%) | 69 (5.9%) | 0.020 |
| Atrial Fibrillation | 159 (4.5%) | 108 (4.6%) | 51 (4.4%) | 0.781 |
| Dyslipidemia | 1737 (49.1%) | 1151 (48.6%) | 586 (50.1%) | 0.420 |
| Prior Angina | 520 (14.7%) | 357 (15.1%) | 163 (13.9%) | 0.360 |
| Prior CAD | 1114 (31.5%) | 769 (32.5%) | 345 (29.5%) | 0.069 |
| Prior Stroke/TIA | 230 (6.5%) | 139 (5.9%) | 91 (7.8%) | 0.031 |
| Alcohol Abuse | 343 (9.7%) | 281 (11.9%) | 62 (5.3%) | < 0.001 |
| Cancer | 256 (7.2%) | 154 (6.5%) | 102 (8.7%) | 0.017 |
| Depression | 265 (7.5%) | 132 (5.6%) | 133 (11.4%) | < 0.001 |
| Sleep Apnea | 102 (2.9%) | 88 (3.7%) | 14 (1.2%) | < 0.001 |
| Obesity (BMI ≥30kg/m2) | 1411 (39.9%) | 891 (37.7%) | 520 (44.4%) | < 0.001 |
| Clinical Characteristics (%) | ||||
| GRACE Score >100 | 1678 (47.5%) | 1039 (43.9%) | 639 (54.6%) | < 0.001 |
| Ejection Fraction <40% | 587 (19.4%) | 419 (20.6%) | 168 (16.9%) | 0.014 |
| STEMI | 1583 (44.8%) | 1131 (47.8%) | 452 (38.6%) | < 0.001 |
| NSTEMI | 1953 (55.2%) | 1235 (52.2%) | 718 (61.4%) | |
| Diseased vessels | ||||
| 0 | 281 (8.5%) | 126 (5.6%) | 155 (14.5%) | |
| 1 | 1410 (42.6%) | 945 (42.1%) | 465 (43.5%) | < 0.001 |
| 2 | 875 (26.4%) | 636 (28.3%) | 239 (22.4%) | |
| 3 | 747 (22.5%) | 538 (24.0%) | 209 (19.6%) | |
| Initial heart rate (BPM) (Mean±SD) | 81.7 ± 21.9 | 80.8 ± 21.9 | 83.6 ± 21.6 | < 0.001 |
| Initial Systolic Blood pressure (Mean±SD) | 143.4 ± 30.3 | 142.7 ± 29.5 | 144.8 ± 31.8 | 0.055 |
| Peak Troponin (I/T) (Mean±SD) | 29.6 ± 76.1 | 33.2 ± 78.7 | 22.3 ± 69.9 | < 0.001 |
| Initial Creatinine (Mean±SD) | 1.2 ± 1.0 | 1.3 ± 1.0 | 1.1 ± 0.9 | < 0.001 |
| Peak CK (Mean±SD) | 1018.8 ± 1435.8 | 1145.5 ± 1556.8 | 755.4 ± 1099.2 | < 0.001 |
| F/U Appt w/Cardiologist | 2914 (82.4%) | 1962 (82.9%) | 952 (81.4%) | 0.252 |
|
In-Hospital Revascularization Procedures /complications |
||||
| None | 837 (23.7%) | 468 (19.8%) | 369 (31.5%) | |
| PCI | 2366 (66.9%) | 1652 (69.8%) | 714 (61.0%) | < 0.001 |
| CABG | 333 (9.4%) | 246 (10.4%) | 87 (7.4%) | |
| In-Hospital Bleeding | 359 (10.2%) | 249 (10.5%) | 110 (9.4%) | 0.298 |
| In-Hospital Transfusion | 384 (10.9%) | 221 (9.3%) | 163 (13.9%) | < 0.001 |
| In-Hospital Cardiac Arrest | 79 (2.2%) | 62 (2.6%) | 17 (1.5%) | 0.027 |
| In-Hospital Cardiogenic Shock | 99 (2.8%) | 66 (2.8%) | 33 (2.8%) | 0.958 |
| In-Hospital AMI | 15 (0.4%) | 10 (0.4%) | 5 (0.4%) | 1.000 |
Abbreviations: CAD= coronary artery disease, TIA=transient ischemic attack, BMI=body mass index, GRACE score=global registry of acute coronary events, STEMI=ST-elevation myocardial infarction, NSTEMI=non-ST-elevation myocardial infarction, BPM=beats per minute, CK=creatinine kinase, F/U=follow up, PCI=percutaneous coronary intervention, CABG=coronary artery bypass grafting, AMI= acute myocardial infarction.
Health status domains were measured using the Short Form-12 (SF-12),12 and the Seattle Angina Questionnaire (SAQ).13 The SF-12 is a valid and reliable instrument and is the most widely used generic health status instrument to quantify patients’ mental and physical functional status.12, 14 Both the SF-12 physical (PCS) and mental (MCS) component summary scores were calculated for this study and range from 0–100, with higher scores indicating greater functioning. A score of 50 represents the US population average, with a standard deviation of 10 points.15, 16 The SAQ is a 19-item disease-specific health-related quality of life measure for patients with coronary artery disease (CAD).13, 17–19 For the purpose of our study the physical limitation, angina frequency, treatment satisfaction, quality of life domains and the Summary Score were used, which range from 0 to 100 points, with higher scores being better.13
Depression was assessed using the Patient Health Questionnaire-9 (PHQ-9),20 a standardized and validated instrument in cardiac populations.21–23 The PHQ quantifies the frequency of depressive symptoms experienced in the past 2 weeks based on the 9 Diagnostic and Statistical Manual of Mental Disorders (4th edition) criteria for a major depressive disorder.24 A PHQ-9 score ≥10 has 88% sensitivity and specificity to detect major depression.25 Perceived social support was measured using the ENRICHD Social Support Instrument (ESSI),26 a reliable and valid assessment of social support in cardiac populations26, 27 and after AMI.28–30 Lastly, perceived stress was measured using the 4-item perceived stress scale (PSS-4),31 a reliable and valid measure of patients’ sense of control or confidence in handling circumstances over the prior month, with higher scores (range: 0–16) indicating greater perceived stress.
Rehospitalization Data Adjudication
Patients enrolled in the TRIUMPH study were interviewed at 1, 6 and 12-months after their AMI, and were asked to report all hospitalizations since their last contact, including the hospital name, date and reason. After obtaining consent from the patient and each hospital, all hospitalization records within the first year after the patient's index AMI were requested and adjudicated by a physician panel. The first unplanned rehospitalization due to any cause, within 1 year of the index admission, was identified as a rehospitalization. Two cardiologists reviewed the hospital records and independently classified the reason for hospitalization. If there was disagreement, the record was adjudicated by a third senior cardiologist and, if disagreement persisted, up to 5 cardiologists independently reviewed the charts until consensus was obtained. The TRIUMPH study also collected data on the principal diagnoses associated with rehospitalization, with particular attention to cardiac vs. non-cardiac diagnoses (Supplemental Table 1). Survival through 1 year was also assessed.
Statistical Analysis
Frequencies, means and standard deviations, and medians with interquartile ranges were calculated for categorical and continuous variables. Statistical differences for the overall sample and between sexes were determined using chi-squared tests, t-tests, and Wilcoxon Rank Sum tests, where appropriate.
Kaplan Meier curves were used to compare rehospitalization outcomes at 1 year for women and men using the Log-rank test. To examine for potential biases due to attrition from mortality, we considered death as a competing event (i.e. if a death and rehospitalization occurred on the same day, the death would be counted, and the censoring for rehospitalization would cease) to compare the cumulative incidence rates with the Kaplan-Meier (KM) estimated rate of 1 year rehospitalization.
We selected several patient and hospital level variables, a priori, that might be associated with sex differences in the risk of all-cause rehospitalization at 1 year. Bivariate analyses were first performed to examine the association of potential predictors with all-cause rehospitalization at 1 year.32 A Cox proportional hazards model, using sequential adjustment for potential confounders, was used to determine the independent effect of sex on 1 year rehospitalization for women versus men, which was represented by risk-adjusted hazard ratios and 95% confidence intervals. The first model included only sex (Model 1). The second model included Model 1 and socio-demographics/SES (age, race, marital/partner status, education, employment status, insurance status, access to care) (Model 2). The third model included Model 2 and medical history (hypertension, diabetes, smoking status, chronic heart failure, chronic lung disease, chronic kidney disease, peripheral artery disease, and prior CAD (prior AMI/percutaneous coronary intervention [PCI] or coronary artery bypass grafting [CABG] (Model 3). The fourth model included Model 3 and presentation and treatment characteristics (GRACE score, in-hospital revascularization procedure [PCI, CABG, none], in-hospital complications/events [i.e. bleeding, transfusion, cardiac arrest, shock], coronary angiographic findings [un-revascularized lesion >70% after all in-hospital procedures], and follow up appointment scheduled) (Model 4). The fifth model included Model 4 and health status ([SAQ Summary score], SF-12 MCS/PCS (Model 5). The sixth model included psychosocial factors comprised of depression (PhQ-9), social support (ESSI) and perceived stress (PSS-4) (Model 6). In the final model we tested the interaction between age and sex to explicitly examine whether rehospitalization was modified by age (using age ≤ or >55, based on previous studies).10, 11 The multivariable model accounted for clustering of patients within site of care, using a hierarchical model with site as a random effect.33
Approximately 20% of patients were missing rehospitalization data due to lost to follow up. Because of this, we conducted a sensitivity analysis using inverse probably weighting on the probability of being observed.34 The final results were similar to the complete case analysis. Characteristics of those included in the final cohort and those missing rehospitalization data are presented in Supplemental Table 2. In brief, there were similar rates of missingness by sex (observed: 33% women vs. 67% men; not observed: 34% women vs. 66% men, P=0.69), the key exposure variable for this analysis. In general, patients missing rehospitalization data were younger, were more likely to be black, to be not married, to be uninsured and not working. Patients also missing rehospitalization data had higher rates of hypertension, diabetes, heart failure, and alcohol abuse. In terms of psychosocial factors, patients missing rehospitalization data had significantly poorer physical and mental generic health status; worse disease-specific physical limitations, more angina frequency, and worse quality of life; and reduced levels of social support, versus patients included in the final cohort.
Missing covariate data were assumed to be non-informatively missing. For covariates considered in each model, missing values were rare (<5% in the study cohort), and given the available observed data, were imputed using multiple imputation to allow incorporation of all patients and to correctly account for uncertainly due to missingness. More specifically, missing covariate data were imputed using a sequential regression imputation that contained all independent and dependent variables from the full multivariable model (IVEware; Institute for Social Research, Ann Arbor, MI). The missing covariate data for baseline clinical, health status, and psychosocial factors are presented in Supplemental Table 3. For all statistical analyses, the significance level was 2-sided with a p value <0.05. All analyses were conducted using SAS 9.2 (SAS Institute Inc., Cary NC).
RESULTS
Baseline Characteristics
Baseline characteristics for the overall sample (N=3,536) and stratified by sex (N=1,170; 33% women) are presented in Table 1. Women were significantly older than men and were more likely to be black, non-married, to have a lower education, were less likely to be working and had more difficulty in receiving medical care as compared with men. In addition, women were more likely to have hypertension, diabetes, chronic lung disease, peripheral vascular disease, prior stroke/TIA, cancer, depression and obesity, but they were less likely to smoke, to have alcohol abuse or sleep apnea.
On arrival, women had a higher GRACE risk score and were more likely to present with NSTEMI, to have smaller infarcts (as suggested by lower creatine kinase/troponin levels), to have a higher initial heart rate and to have less diseased vessels, than similarly aged men; they were also less likely to receive PCI or CABG.
Women reported significantly poorer physical and mental generic health status than men, and worse disease-specific physical limitations, more angina frequency, and worse quality of life. Finally, women reported higher levels of depression and perceived stress, but had similar levels of social support to men (Table 2).
Table 2.
Baseline Psychosocial factors of all patients stratified by sex.
| Total Sample (N=3,536) |
Men (N=2,366) |
Women (N=1,170) |
P Value | |
|---|---|---|---|---|
| General Health (SF-12) (Mean±SD) | ||||
| SF-12 PCS | 42.9 ± 12.2 | 44.3 ± 11.8 | 40.0 ± 12.5 | < 0.001 |
| SF-12 MCS | 50.0 ± 11.4 | 51.0 ± 10.7 | 48.0 ± 12.4 | < 0.001 |
| CVD Functional Status (SAQ) (Mean±SD) | ||||
| SAQ Physical Limitation Score | 86.5 ± 21.5 | 89.3 ± 19.0 | 80.1 ± 25.2 | < 0.001 |
| SAQ Angina Frequency Score | 86.5 ± 20.3 | 87.0 ± 19.9 | 85.3 ± 21.1 | 0.016 |
| SAQ Treatment Satisfaction Score | 94.2 ± 10.0 | 94.4 ± 10.0 | 93.8 ± 10.1 | 0.107 |
| SAQ Quality of Life Score | 63.8 ± 23.4 | 65.3 ± 22.9 | 60.9 ± 23.9 | < 0.001 |
| PHQ-9 Depression Score (Mean±SD) | 5.1 ± 5.3 | 4.6 ± 5.0 | 6.3 ± 5.8 | < 0.001 |
| ENRICHD Social Support Score (Mean±SD) | 22.0 ± 4.4 | 22.0 ± 4.4 | 21.8 ± 4.4 | 0.217 |
| Stress at Home (%) | ||||
| Never Experience Stress | 360 (30.7%) | 286 (34.7%) | 74 (21.3%) | |
| Some Period of Stress | 541 (46.2%) | 375 (45.5%) | 166 (47.7%) | < 0.001 |
| Several Periods of Stress | 192 (16.4%) | 124 (15.0%) | 68 (19.5%) | |
| Permanent Stress | 79 (6.7%) | 39 (4.7%) | 40 (11.5%) |
Abbreviations: SF-12=Short-form 12, CVD=cardiovascular disease, SAQ=Seattle angina questionnaire, PHQ-9= patient health questionnaire
One Year Crude Rehospitalization Rates
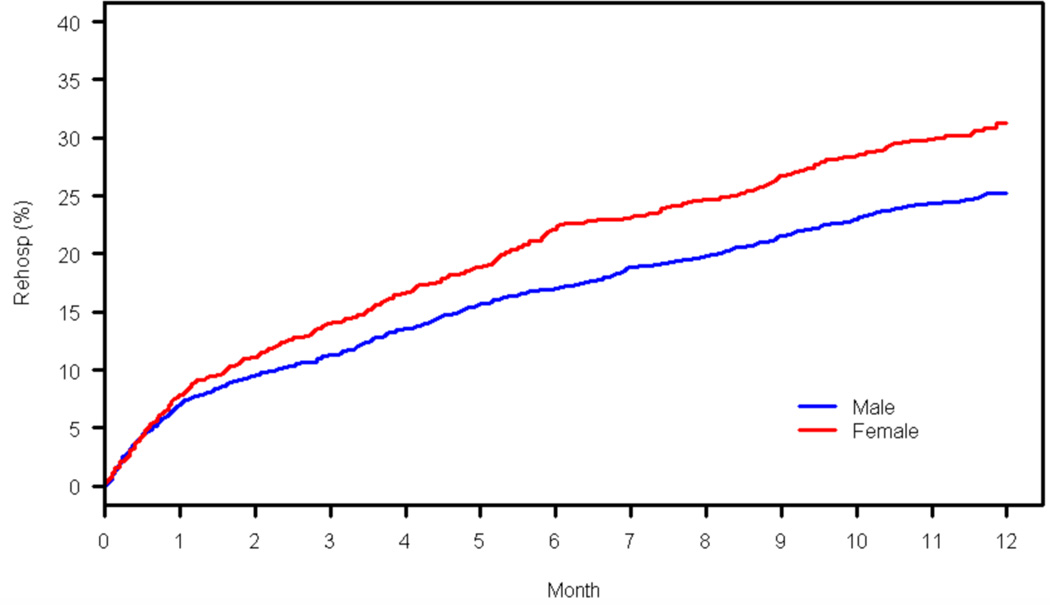
The unadjusted rehospitalization curves for the overall population are presented in Figure 1. Results stratified by age (≤55 and >55 years) are presented in Figure 2. In total there were 865 (24.5%) all-cause rehospitalizations at 1 year, including 537 (22.7%) rehospitalizations for men and 328 (28.0%) for women within the first year of an AMI. The crude 1 year rehospitalization rate (KM estimated) for women was significantly higher than that for men (31.3% vs. 25.2%, P<0.001), with the curves for rehospitalization diverging within 1 month after discharge.
Figure 1.
Unadjusted Kaplan Meier curve for the overall population for 1 year rehospitalization (men=blue, women=red).
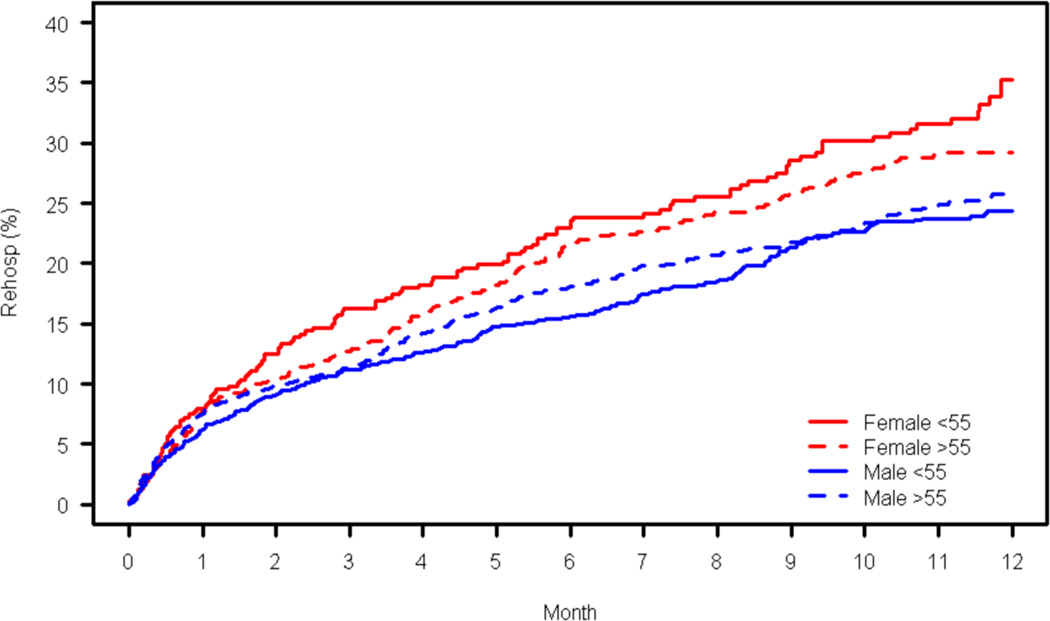
Figure 2.
Unadjusted Kaplan Meier curve for ≤55 and >55 year age groups for 1 year rehospitalization (young men= solid blue, young women=solid red; old men=broken blue, old women=broken red).
The 1 year mortality rates for women and men were 3.6% and 2.9%, respectively (P=0.034). Even after accounting for the competing risk of mortality, there were still statistically significant differences between the sexes in readmission rates. The crude readmission (KM Estimated) rate for women at 1 year was 26.0%, compared with 21.6% for men (P=<.001) (Figure 1).
Principal Discharge Rehospitalization Diagnoses at 1 year
The principal rehospitalization diagnoses at 1 year for women and men are presented in Supplemental Table 1. There were few significant differences between cardiac and non-cardiac diagnoses between women and men. Women and men had similar rates of cardiac causes (35.2% vs. 34.3%, P=0.83).
Association of Sex with 1 year Rehospitalization
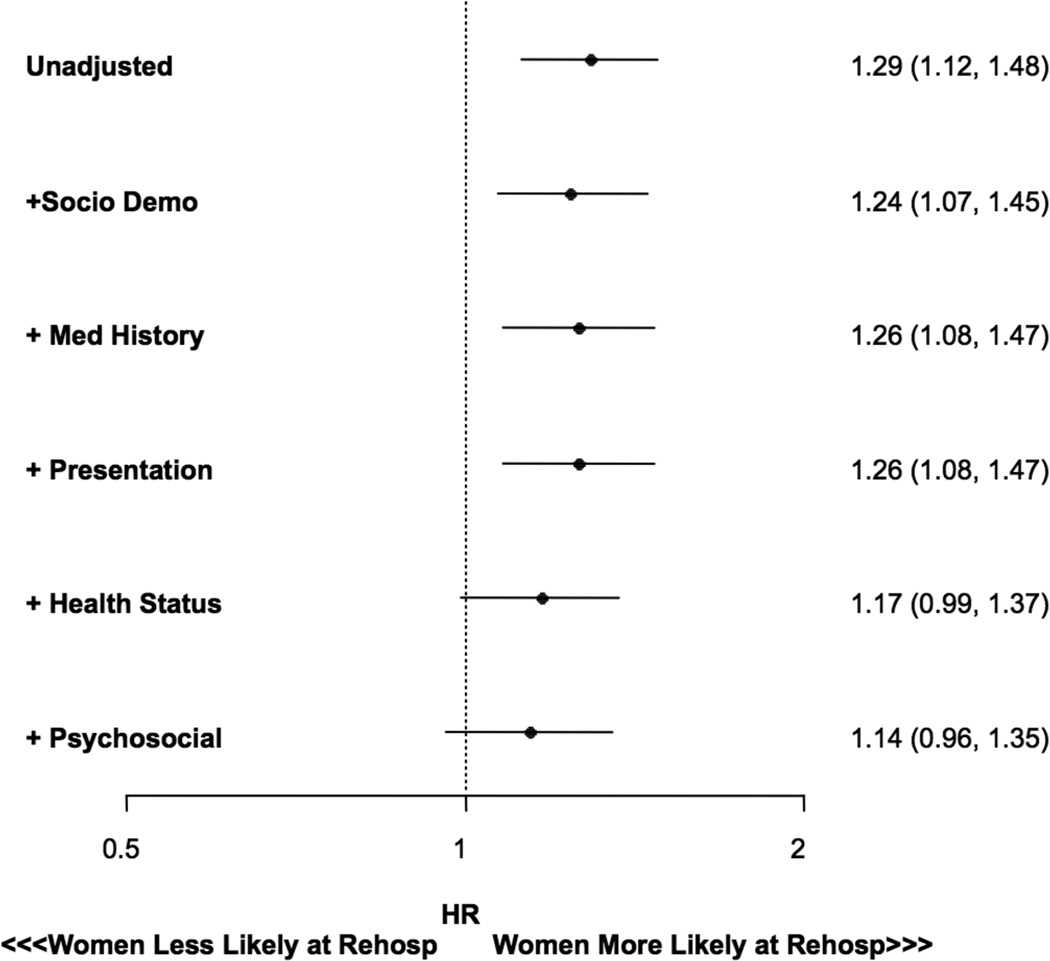
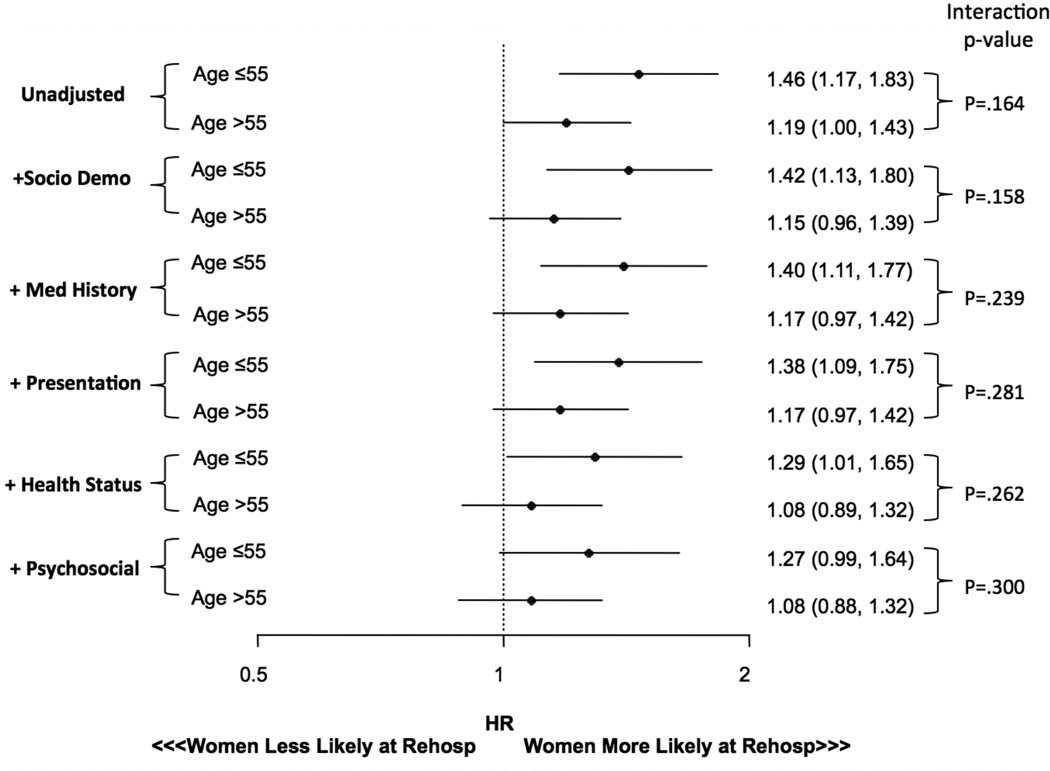
Figure 3 shows the association of sex with 1 year rehospitalization for the overall population, following sequential adjustment for potential confounders. Results stratified by age (≤55 and >55 years) are presented in Figure 4. Women had a 29% higher hazard of being hospitalized within 1 year (HR=1.29, 95% CI 1.12, 1.48). Following adjustment for socio-demographics/SES, medical history and presentation characteristics, women had a persistent, significant 26% higher risk of rehospitalization (HR=1.26, 95% CI 1.08, 1.47). However, following adjustment for health status (HR=1.17, 95% CI =0.99, 1.37) and psychosocial factors (HR=1.14, 95% CI 0.96, 1.34), the association was attenuated. When assessing the interaction between age and sex on rehospitalization in the final step, there was no significant difference, suggesting that the association of sex with rehospitalization was not significantly modified by age (P=0.30). To assess the increment in readmission risk from 1-month to 1-year post AMI, we performed a landmark analysis. Results indicate that the hazard ratio between men and women in the fully adjusted model was not statistically significant, both from day 0 – 1 month (HR 1.0; 95% CI 0.75,1.34, P=.99) and from 1 –12 months (HR=1.20, 95% CI 0.99,1.46, p=.059), however there was a trend towards significance for the second time period. In addition, Our sensitivity analysis, conducted due to the concern of missing rehospitalization data, confirmed that there were no systematic sex differences in those who had rehospitalization data and those who did not, as our primary results were unchanged [women vs. men, HR=1.13, 95% CI (.97, 1.31) P=0.11].
Figure 3.
Forest plot showing unadjusted/adjusted HR and 95% CI for 1 year rehospitalization in women versus men for the overall population.
Figure 4.
Forest plot showing unadjusted/adjusted HR and 95% CI for 1 year rehospitalization by age.
DISCUSSION
This study demonstrates that women of all age groups have a higher crude risk of rehospitalization, as compared with men, over the first year after AMI. There was no set of diagnoses that caused the difference. While the increased risk of rehospitalization persisted after adjustment for standard clinical variables, the worse baseline health status and psychosocial state of women attenuated the difference, reducing its magnitude and making it non-significant.
Our study extends the literature in several important ways. First, this is the largest study to characterize sex differences in the incidence of and association of sex with 1 year rehospitalization following AMI. Prior studies have indicated that older women (≥65 years) have up to a 60% greater risk for rehospitalization up to 1 year following hospitalization for an acute coronary syndrome, versus similarly aged men.2–6 Although these studies provided important insight, they did not explicitly focus on understanding sex differences in their primary objectives (as per the current study) and simply reported the incidence of readmission. We also extend our prior work, which focused on examining the 30-day period, whereby we demonstrated that women are more susceptible than men to rehospitalization at 30-days following AMI.7 Even after adjustment for a range of potentially explanatory variables between sexes, women still had a 22% higher risk of readmission than similarly-aged men.7 In the current study, while we show discrepancies in 30-day readmission rates in comparison to our prior work (as indicated by our landmark analysis), we provide supportive evidence that the risk of rehospitalization persists in an elevated state beyond the initial month after hospital discharge,1 as the crude rate of rehospitalization at 1 year in TRIUMPH was 28% in women versus 23% in men.
Second, women of all age groups appear to be at increased risk for rehospitalization within 1 year after AMI as compared with similarly aged men. The association between sex and rehospitalization in our study persisted after adjustment for clinical factors, however the poorer health status and psychosocial state of women appeared to have attenuated the difference. This finding is supported by prior research. For example, Parashar et al and colleagues demonstrated that following adjustment for depressive symptoms, the relationship between sex and rehospitalization was further attenuated, indicating that depression may be an explanatory factor in the risk of rehospitalization in women.5 Our study extends these findings by accounting for other important patient outcomes that may explain patients’ increased risk of rehospitalization such as health status, stress and social support. In addition, our study incorporates physician-adjudicated readmission data versus patient self-report, which has been shown to be unreliable in longitudinal clinical research studies.35
Third, few studies have deeply investigated the effect of patient-level SES, presentation characteristics and psychosocial factors as potential determinants of rehospitalization after AMI, mainly due to the utilization of administrative datasets and subsequent lack of validated multidimensional instruments among population health studies,32, 36 and no prior research has explicitly focused on understanding sex differences. Using an observational dataset with detailed information on patient reported outcomes, clinical and treatment characteristics, we were able to validate whether the risk of rehospitalization following AMI in women extended to 1 year, and identified factors which may help explain the relationship between sex and rehospitalization. Further research is needed to see whether some of the most important characteristics, such as baseline health and psychosocial status, can be targeted to improve outcomes for women and men and to decrease the sex differences in readmission risk.
Fourth, young women represent a vulnerable population with an excess risk of morbidity and mortality, compared with similar aged men.10, 11 Although we did not observe a significant sex-age interaction, it appears that clinically, young women are at greatest risk for rehospitalization as evidenced by the large unadjusted difference. For example, at 1 year we showed that younger women (≤55 years) had a 32% crude rate of rehospitalization compared with only 23% in younger men and a 29% increased risk in older women (>55 years). Furthermore, although not significant in the final adjusted model, younger women had a 27% higher risk of rehospitalization at 1 year compared with only 8% in older women. This information on sex differences in rehospitalization risk up to 1 year following AMI, particularly in regards to patient-reported characteristics that are most attenuating this difference (i.e. health status), may help inform patients of their long term recovery, and provide worthwhile targets for hospitals to consider addressing in future interventions.
In our study we also observed interesting patterns in regards to the timing and principal diagnoses of readmission. The separation of the curves for rehospitalization in both sexes occurred around the 30-day time period and was more pronounced for women versus men over the first year post AMI. Furthermore, we observed important differences by age. It appears that visually, younger patients (≤55 years) are more likely to present earlier than older patients (>55 years) after an AMI. These findings are important as they suggest that women and men (particularly younger women) have a higher risk of rehospitalization in the initial stages following AMI and continue to experience a greater risk over the course of 1 year, irrespective of mortality.7 Reducing rehospitalizations during this time period may necessitate in-hospital interventions and better discharge planning, including incorporating early ambulatory interventions.
With regard to principal diagnoses of rehospitalization at 1 year, we observed few significant differences by sex. For example, we showed that 25% of patients were readmitted within 1 year and that there is heterogeneity in the causes of readmission. These data suggest that the period of generalized vulnerability following hospitalization for many conditions,37 termed the post-hospital syndrome, is equally important for both sexes. These results are consistent with findings from the elderly Medicare population and in younger patients enrolled from administrative claims data.1, 38
Study Implications
We have provided confirmatory evidence that a sex disparity exists for 1 year rehospitalization, whereby women of all age groups are at higher risk compared with similarly aged men. This period of vulnerability is long lasting and continues to increase from the first month after hospital discharge up to 1 year following AMI. In addition, our study highlights that the increased risk observed in women may be explained by a complex interplay of multiple factors, such as health status and depression, as adjustment for these factors attenuated the magnitude of the effect. The contribution of these factors on readmission is worthy of future investigation. Moving forward, there may be an opportunity to design sex-based interventions to improve post discharge care for patients over the first year following AMI, including interventions in women that aim to improve health status and psychosocial well being.39–41
Limitations
This study should be interpreted in the context of several potential limitations. First, 20% of patients were missing rehospitalization data at 1 year follow up, due to patients being lost to follow up. However, this limitation is unlikely to bias results, as patients with missing data were similar to those without missing data, as confirmed by our sensitivity analysis. Second, there may also be a potential selection bias, as not all women and men with AMI at study hospitals were included in this study. However, we found few differences in participation rates by sex.8 In general, our TRIUMPH study sample is directly comparable to similarly aged AMI patients observed in other large observational studies, supporting the generalizability of our study findings.42 Third, although our data are derived from 2005–2008, we do not believe the age of the data could impact and/or bias the specific question addressed in these analyses as medical practice has not changed over the last decade. Lastly, our landmark analysis revealed differences in 30-day readmission rates post AMI in the current dataset versus our prior work. This may be due to differences in study populations, as administrative datasets include all patients versus observational prospective datasets such as TRIUMPH that include enrolled patients - and the later tend to represent a healthier population. Additionally, lost to follow up rates may be higher in prospective studies such as TRIUMPH versus administrative datasets. Overall, we do not believe the differences observed between datasets affect the overall validity of our study findings.
CONCLUSION
Women of all ages have a persistently higher risk of rehospitalization compared with men over the first year after AMI. We observed that the spectrum of diagnoses appears to be similar, indicating a general elevation of risk, but not for a particular diagnosis. Psychosocial factors attenuate the risk of rehospitalization, suggesting a potential role in the underlying difference between sexes. Moving forward, healthcare providers should be made aware that women constitute a specific population at greater risk of readmission after AMI and to consider their psychological state as an opportunity to minimize the risks for readmission.
Supplementary Material
CLINICAL PERSPECTIVE.
What is new?
This is the largest study to date that characterizes sex differences in the incidence of and association of sex with 1 year rehospitalization following AMI.
We also provide information on whether sex differences in rehospitalization vary by age, given that younger women have been shown to have poorer outcomes and worse recovery 1 year after AMI.
In addition, we advance the field by providing potential explanatory factors that may mediate the relationship between sex and rehospitalization, which are needed to reduce readmissions.
What are the clinical implications?
This study provides confirmatory support that a sex disparity exists for 1 year rehospitalization, whereby women of all age groups are at higher risk compared with similarly aged men.
We also show that the increased risk for readmission in women may be explained by a complex interplay of factors including health status and depression.
There may be an opportunity to design sex-based interventions to improve post discharge care for patients over the first year following AMI (i.e. that aim to improve health status/psychosocial well being).
Acknowledgments
None.
Sourcs of Funding: The TRIUMPH study was supported in part by grant funding from the National Heart, Lung and Blood Institute (P50 HL077113). RPD is supported by an Early Career Fellowship funded by the National Health and Medical Research Council of Australia.
KD is supported by grant K23AG048331 from the National Institute on Aging and the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program. He is also supported by grant P30AG021342 via the Yale Claude D. Pepper Older Americans Independence Center. HMK is supported by grant U01 HL105270-05 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Health and Medical Research Council of Australia, the American Federation for Aging Research, or the National Institutes of Health.
KD and HMK work under contract with the Centers for Medicare & Medicaid Services to develop and maintain performance measures. KD is a consultant for Clover Health and is a member of the scientific advisory board for Clover Health. HMK is chair of a cardiac scientific advisory board for UnitedHealth and is the recipient of research grants from Medtronic, Inc. and Johnson and Johnson through Yale University. In addition, JAS is supported by grants from Gilead, Genentech, Lilly, Amorcyte, and EvaHeart, and has a patent Seattle Angina Questionnaire with royalties paid.
Footnotes
Author Disclosures: No other relevant disclosers are reported. RPD, KFK, PGJ, VV, KM, SVN, KGS, DMB, and JAS report no financial disclosures that contributed to the production of this manuscript.
REFERENCES
- 1.Dharmarajan K, Hsieh AF, Kulkarni VT, Lin Z, Ross JS, Horwitz LI, Kim N, Suter LG, Lin H, Normand SL, Krumholz HM. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: Retrospective cohort study. BMJ. 2015;350:h411. doi: 10.1136/bmj.h411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anand SS, Xie CC, Mehta S, Franzosi MG, Joyner C, Chrolavicius S, Fox KA, Yusuf S. Differences in the management and prognosis of women and men who suffer from acute coronary syndromes. J Am Coll Cardiol. 2005;46:1845–1851. doi: 10.1016/j.jacc.2005.05.091. [DOI] [PubMed] [Google Scholar]
- 3.Dey S, Flather MD, Devlin G, Brieger D, Gurfinkel EP, Steg PG, Fitzgerald G, Jackson EA, Eagle KA. Sex-related differences in the presentation, treatment and outcomes among patients with acute coronary syndromes: The global registry of acute coronary events. Heart. 2009;95:20–26. doi: 10.1136/hrt.2007.138537. [DOI] [PubMed] [Google Scholar]
- 4.Humphries KH, Pu A, Gao M, Carere RG, Pilote L. Angina with "normal" coronary arteries: Sex differences in outcomes. Am Heart J. 2008;155:375–381. doi: 10.1016/j.ahj.2007.10.019. [DOI] [PubMed] [Google Scholar]
- 5.Parashar S, Rumsfeld JS, Reid KJ, Buchanan D, Dawood N, Khizer S, Lichtman J, Vaccarino V. Impact of depression on sex differences in outcome after myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2:33–40. doi: 10.1161/CIRCOUTCOMES.108.818500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen HY, Tisminetzky M, Lapane KL, Yarzebski J, Person SD, Kiefe CI, Gore JM, Goldberg RJ. Decade-long trends in 30-day rehospitalization rates after acute myocardial infarction. J Am Heart Assoc. 2015;4:e002291. doi: 10.1161/JAHA.115.002291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dreyer RP, Ranasinghe I, Wang Y, Dharmarajan K, Murugiah K, Nuti SV, Hsieh AF, Spertus JA, Krumholz HM. Sex differences in the rate, timing and principal diagnoses of 30-day readmissions in younger patients with acute myocardial infarction. Circulation. 2015;132:158–166. doi: 10.1161/CIRCULATIONAHA.114.014776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arnold SV, Chan PS, Jones PG, Decker C, Buchanan DM, Krumholz HM, Ho PM, Spertus JA. Translational research investigating underlying disparities in acute myocardial infarction patients' health status (triumph): Design and rationale of a prospective multicenter registry. Circ Cardiovasc Qual Outcomes. 2011;4:467–476. doi: 10.1161/CIRCOUTCOMES.110.960468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dreyer RP, Wang Y, Strait KM, Lorenze NP, D'Onofrio G, Bueno H, Lichtman JH, Spertus JA, Krumholz HM. Gender differences in the trajectory of recovery in health status among young patients with acute myocardial infarction: Results from the variation in recovery: Role of gender on outcomes of young ami patients (virgo) study. Circulation. 2015;131:1971–1980. doi: 10.1161/CIRCULATIONAHA.114.014503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM. Sex-based differences in early mortality after myocardial infarction. National registry of myocardial infarction 2 participants. N Engl J Med. 1999;341:217–225. doi: 10.1056/NEJM199907223410401. [DOI] [PubMed] [Google Scholar]
- 11.Vaccarino V, Krumholz HM, Yarzebski J, Gore JM, Goldberg RJ. Sex differences in 2-year mortality after hospital discharge for myocardial infarction. Ann Intern Med. 2001;134:173–181. doi: 10.7326/0003-4819-134-3-200102060-00007. [DOI] [PubMed] [Google Scholar]
- 12.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McDonell M, Fihn SD. Development and evaluation of the seattle angina questionnaire: A new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25:333–341. doi: 10.1016/0735-1097(94)00397-9. [DOI] [PubMed] [Google Scholar]
- 14.Muller-Nordhorn J, Roll S, Willich SN. Comparison of the short form (sf)-12 health status instrument with the sf-36 in patients with coronary heart disease. Heart. 2004;90:523–527. doi: 10.1136/hrt.2003.013995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wyrwich KW, Bullinger M, Aaronson N, Hays RD, Patrick DL, Symonds T. Estimating clinically significant differences in quality of life outcomes. Qual Life Res. 2005;14:285–295. doi: 10.1007/s11136-004-0705-2. [DOI] [PubMed] [Google Scholar]
- 16.Ware JE, Kosinski M, Keller SD, Lincoln RI. Sf-12: How to score the sf-12 physical and mental health summary scales. 4th. Boston, MA: Lincoln, RI, QualityMetric Incorporated; 2002. [Google Scholar]
- 17.Spertus JA, Dawson J, Masoudi FA, Krumholz HM, Reid KJ, Peterson ED, Rumsfeld JS. Prevalence and predictors of angina pectoris one month after myocardial infarction. Am J Cardiol. 2006;98:282–288. doi: 10.1016/j.amjcard.2006.01.099. [DOI] [PubMed] [Google Scholar]
- 18.Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Fihn SD. Monitoring the quality of life in patients with coronary artery disease. Am J Cardiol. 1994;74:1240–1244. doi: 10.1016/0002-9149(94)90555-x. [DOI] [PubMed] [Google Scholar]
- 19.Spertus J, Safley D, Garg M, Jones P, Peterson ED. The influence of race on health status outcomes one year after an acute coronary syndrome. J Am Coll Cardiol. 2005;46:1838–1844. doi: 10.1016/j.jacc.2005.05.092. [DOI] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JB. The phq-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mallik S, Spertus JA, Reid KJ, Krumholz HM, Rumsfeld JS, Weintraub WS, Agarwal P, Santra M, Bidyasar S, Lichtman JH, Wenger NK, Vaccarino V. Depressive symptoms after acute myocardial infarction: Evidence for highest rates in younger women. Arch Intern Med. 2006;166:876–883. doi: 10.1001/archinte.166.8.876. [DOI] [PubMed] [Google Scholar]
- 22.Ruo B, Rumsfeld JS, Hlatky MA, Liu H, Browner WS, Whooley MA. Depressive symptoms and health-related quality of life: The heart and soul study. JAMA. 2003;290:215–221. doi: 10.1001/jama.290.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Whooley MA, de Jonge P, Vittinghoff E, Otte C, Moos R, Carney RM, Ali S, Dowray S, Na B, Feldman MD, Schiller NB, Browner WS. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300:2379–2388. doi: 10.1001/jama.2008.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) 4th. Washington, DC: American Psychiatric Publishing; 1994. [Google Scholar]
- 25.Kroenke K, Spitzer RL. The phq-9: A new depression diagnostic and severity measure. Psychiatr Ann. 2002;32:509–521. [Google Scholar]
- 26.The ENRICHD Investigators. Enhancing recovery in coronary heart disease patients (enrichd): Study design and methods. Am Heart J. 2000;139:1–9. doi: 10.1016/s0002-8703(00)90301-6. [DOI] [PubMed] [Google Scholar]
- 27.Vaglio J, Jr, Conard M, Poston WS, O'Keefe J, Haddock CK, House J, Spertus JA. Testing the performance of the enrichd social support instrument in cardiac patients. Health Qual Life Outcomes. 2004;2:24. doi: 10.1186/1477-7525-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lett HS, Blumenthal JA, Babyak MA, Strauman TJ, Robins C, Sherwood A. Social support and coronary heart disease: Epidemiologic evidence and implications for treatment. Psychosom Med. 2005;67:869–878. doi: 10.1097/01.psy.0000188393.73571.0a. [DOI] [PubMed] [Google Scholar]
- 29.Burg MM, Barefoot J, Berkman L, Catellier DJ, Czajkowski S, Saab P, Huber M, DeLillo V, Mitchell P, Skala J, Taylor CB Investigators E. Low perceived social support and post-myocardial infarction prognosis in the enhancing recovery in coronary heart disease clinical trial: The effects of treatment. Psychosom Med. 2005;67:879–888. doi: 10.1097/01.psy.0000188480.61949.8c. [DOI] [PubMed] [Google Scholar]
- 30.Leifheit-Limson EC, Reid KJ, Kasl SV, Lin H, Jones PG, Buchanan DM, Parashar S, Peterson PN, Spertus JA, Lichtman JH. The role of social support in health status and depressive symptoms after acute myocardial infarction: Evidence for a stronger relationship among women. Circ Cardiovasc Qual Outcomes. 2010;3:143–150. doi: 10.1161/CIRCOUTCOMES.109.899815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 32.Desai MM, Stauffer BD, Feringa HH, Schreiner GC. Statistical models and patient predictors of readmission for acute myocardial infarction: A systematic review. Circ Cardiovasc Qual Outcomes. 2009;2:500–507. doi: 10.1161/CIRCOUTCOMES.108.832949. [DOI] [PubMed] [Google Scholar]
- 33.Sullivan LM, Dukes KA, Losina E. Tutorial in biostatistics. An introduction to hierarchical linear modelling. Stat Med. 1999;18:855–888. doi: 10.1002/(sici)1097-0258(19990415)18:7<855::aid-sim117>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 34.Seaman SR, White IR. Review of inverse probability weighting for dealing with missing data. Stat Methods Med Res. 2013;22:278–295. doi: 10.1177/0962280210395740. [DOI] [PubMed] [Google Scholar]
- 35.Krishnamoorthy A, Peterson ED, Knight JD, Anstrom KJ, Effron MB, Zettler ME, Davidson-Ray L, Baker BA, McCollam PL, Mark DB, Wang TY. How reliable are patient-reported rehospitalizations? Implications for the design of future practical clinical studies. J Am Heart Assoc. 2016;5:e002695. doi: 10.1161/JAHA.115.002695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Spertus J. Barriers to the use of patient-reported outcomes in clinical care. Circ Cardiovasc Qual Outcomes. 2014;7:2–4. doi: 10.1161/CIRCOUTCOMES.113.000829. [DOI] [PubMed] [Google Scholar]
- 37.Krumholz HM. Post-hospital syndrome--an acquired, transient condition of generalized risk. N Engl J Med. 2013;368:100–102. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ranasinghe I, Wang Y, Dharmarajan K, Hsieh AF, Bernheim SM, Krumholz HM. Readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia among young and middle-aged adults: A retrospective observational cohort study. PLoS Med. 2014;11:e1001737. doi: 10.1371/journal.pmed.1001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Orth-Gomer K, Schneiderman N, Wang HX, Walldin C, Blom M, Jernberg T. Stress reduction prolongs life in women with coronary disease: The stockholm women's intervention trial for coronary heart disease (switchd) Circ Cardiovasc Qual Outcomes. 2009;2:25–32. doi: 10.1161/CIRCOUTCOMES.108.812859. [DOI] [PubMed] [Google Scholar]
- 40.Rollman BL, Belnap BH, LeMenager MS, Mazumdar S, Houck PR, Counihan PJ, Kapoor WN, Schulberg HC, Reynolds CF., 3rd Telephone-delivered collaborative care for treating post-cabg depression: A randomized controlled trial. JAMA. 2009;302:2095–2103. doi: 10.1001/jama.2009.1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Davidson KW, Bigger JT, Burg MM, Carney RM, Chaplin WF, Czajkowski S, Dornelas E, Duer-Hefele J, Frasure-Smith N, Freedland KE, Haas DC, Jaffe AS, Ladapo JA, Lesperance F, Medina V, Newman JD, Osorio GA, Parsons F, Schwartz JE, Shaffer JA, Shapiro PA, Sheps DS, Vaccarino V, Whang W, Ye S. Centralized, stepped, patient preference-based treatment for patients with post-acute coronary syndrome depression: Codiacs vanguard randomized controlled trial. JAMA Intern Med. 2013;173:997–1004. doi: 10.1001/jamainternmed.2013.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Spertus JA, Peterson E, Rumsfeld JS, Jones PG, Decker C, Krumholz H. The prospective registry evaluating myocardial infarction: Events and recovery (premier)--evaluating the impact of myocardial infarction on patient outcomes. Am Heart J. 2006;151:589–597. doi: 10.1016/j.ahj.2005.05.026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.