Abstract
Background:
Effective methods for postoperative pain relief are an important concern in outpatient surgery. For arthroscopies we combine a single-shot peripheral nerve block using low-volume, low-concentration ropivacaine with general anesthesia. We hypothesized that the patients would have less postoperative pain and be more rapidly home ready than after general anesthesia alone.
Methods:
Patients (American Society of Anesthesiologists I–III, 18–80 years old) scheduled for outpatient arthroscopy on the upper or lower extremity were randomized to have either a combination of peripheral nerve block and general anesthesia (NB + GA, study group) or general anesthesia alone (GA, control group). The relevant nerve was localized by ultrasound and 10 mL ropivacaine 0.2% was injected. General anesthesia was with propofol and remifentanil. Numeric rating scales were used to assess pain and patient satisfaction in the recovery room, on the evening of surgery, and on the following 2 days.
Results:
A total of 120 patients participated in the study (NB + GA: 61; GA: 59). The percentage of patients reporting relevant pain in the recovery room were 0% versus 44% (P < 0.001), on the evening after surgery 3% versus 80% (P < 0.001), and on days 1 and 2 postsurgery 12% versus 73% and 12% versus 64% (NB + GA vs GA, respectively). Median time to home discharge was NB + GA 34.5 min (range 15–90) versus GA 55 min (20–115) (P < 0.001).
Conclusions:
The combination of a peripheral nerve block with low-dose ropivacaine and general anesthesia reduced postoperative pain compared with general anesthesia alone for several days after outpatient arthroscopy. It also shortened the time to home discharge.
Keywords: ambulatory anesthesia, general anesthesia, low-dose local anesthetic, peripheral nerve block
1. Introduction
Outpatient surgery is becoming more popular for reasons of economy and patient satisfaction.[1,2] Rapid discharge from the facility increases the cost-effective use of resources and also accommodates patients’ expectations. Rapid recovery and a low incidence of postoperative adverse events are prime factors in the choice of the suitable anesthetic regimen.
Postoperative pain is one of the most common reasons for delayed home discharge or unscheduled hospital admission in outpatient surgery.[1,3] Effective pain control should therefore be a central element in the management of surgical outpatients. Studies have indicated that regional nerve blocks can reduce postoperative pain compared with general anesthesia without delaying home discharge while also increasing patient satisfaction.[4,5] But general anesthesia alone is still the most commonly used anesthetic technique for outpatient surgery.[5] Wennervirta et al[6] showed that combining an interscalene plexus block with general anesthesia for surgery of the upper limb gave a more stable course of anesthesia, lowered anesthetic requirements and reduced intraoperative stress. One might also expect that a preoperatively established nerve block can prevent or reduce postoperative pain for several days.[7]
In this study, we investigated the effects of the combination of a general anesthetic with a single-shot peripheral nerve block using low-volume, low-concentration ropivacaine for outpatient orthopedic surgery. We documented the incidence and intensity of postoperative pain, postoperative adverse events, the time to home discharge, and patient satisfaction and compared them to those after general anesthesia alone. The aim of this study was to test whether a combination of general anesthesia and peripheral nerve block with low-dose ropivacaine reduces postoperative pain after outpatient arthroscopy.
2. Methods
This prospective randomized trial was conducted between June 15, 2012 and August 25, 2012 in an orthopedic outpatient clinic (Baunatal, Germany) after approval by the institutional review board of the University Medical Center Göttingen (No. 9/8/11). It was registered with the German Clinical Trials Register under the clinical trial number DRKS00004537 on May 2012.
American Society of Anesthesiologists (ASA) class I to III patients scheduled for outpatient knee, ankle, or shoulder arthroscopy with less invasive interventions (e.g., subacromial decompression, partial meniscus resection, meniscal suturing, cartilage debridement) and with no contraindications for a peripheral nerve block were consecutively recruited for the study. Their preoperative pain at rest and at motion was assessed and recorded by the attending orthopedic surgeon. After having given their informed consent they were randomized according to the calendar day to have either general anesthesia with a peripheral nerve block (NB + GA, study group) or general anesthesia alone (GA, control group). Two anesthetists (IB and BB) performed all anesthetics in approximately equal shares.
All patients were given ibuprofen (600 mg p.o.) 15 min before beginning with the anesthesia preparations. A peripheral vein was cannulated and patient monitoring was established (noninvasive blood pressure, pulse oximetry, continuous electrocardiography, bispectral index [BIS, Covidien, Medtronic, Minneapolis, MN]). Midazolam was given intravenously as premedication in a dose titrated to render the patient relaxed but still cooperative (1–3 mg). The nerve block was performed in a separate room before induction of general anesthesia in the operating room.
2.1. Single-shot peripheral nerve block
An interscalene block of the brachial plexus was used in shoulder arthroscopy. For knee arthroscopy the femoral nerve was blocked 2 to 3 cm distal to the inguinal ligament, and the sciatic nerve was blocked 5 to 10 cm proximal to the popliteal fossa for ankle arthroscopy. The patients were placed in the appropriate positions for the blocks, and the targeted nerve was located by ultrasound (12 MHz transducer, M-Turbo, FUJIFILM SonoSite, Bothell, WA). The puncture site was disinfected, draped, and anesthetized with mepivacaine 1%. A 19G stimulating cannula (55 mm, B. Braun Melsungen AG, Melsungen, Germany) was advanced to the nerve under ultrasound guidance. After identifying the correct position of the needle tip by ultrasound, 10 mL of ropivacaine 0.2% were injected until the entire circumference of the nerve could be seen surrounded by the local anesthetic. Immediately afterward general anesthesia was induced.
2.2. General anesthesia
General anesthesia was a total intravenous technique with remifentanil and propofol. Anesthesia was induced with a bolus injection of remifentanil (1 μg/kg body weight [BW]) followed by a bolus injection of propofol (2 mg/kg BW given over 2 min). Anesthesia was maintained with infusions of remifentanil (initial rates: NB + GA 0.05 μg/kg BW per min; GA 0.3 μg/kg BW per min) and propofol (initial rate: 4 mg/kg BW per h). A laryngeal mask airway (LMA Supreme, Teleflex, Pennsylvania, PA) was inserted when a sufficiently deep plane of anesthesia was established (loss of lid reflex, apnea, BIS < 60). The lungs were ventilated with 40% oxygen with a tidal volume of 7 mL/kg BW and a frequency of 15 per min. This was adjusted to keep end-tidal CO2 between 35 and 45 mm Hg. The propofol infusion rate was adjusted to keep BIS between 40 and 60, and the remifentanil infusion rate was adjusted to maintain mean arterial blood pressure between 60 and 100 mm Hg and the heart rate between 50 and 100 bpm. The laryngeal mask airway was removed when the patients had regained adequate control over their airways and had a respiratory rate >10 breaths/min. This was usually before the dressing was applied.
2.3. Discharge from the recovery room
In the recovery room, patients with pain intensity >3 on a numeric rating scale (NRS, 0 = no pain to 10 = worst pain imaginable) were given 1 g metamizole (dipyrone) p.o. up to 2 times. In the study group, loss of sensation was tested. The criteria for home discharge were stable vital signs, no nausea or active vomiting, the ability to sit and walk without dizziness, ability to tolerate oral fluids. and tolerable pain treatable with minor analgesics (NRS ≤ 3). In addition, the effect of the peripheral nerve block had to be wearing off, and the strength of the affected muscles had to have returned to grade 5 on the Medical Research Council (MRC) scale (5 = normal strength, 4 = still able to move against resistance, 3 = only able to move against gravity, 2 = only able to move with gravity eliminated, 1 = flicker or trace contraction, 0 = no movement).[8] The patients were given a prescription for ibuprofen (600 mg p.o., t.i.d.). Metamizole (1 g p.o., up to 4 times daily) was prescribed if further analgesia was necessary.
2.4. Data assessment
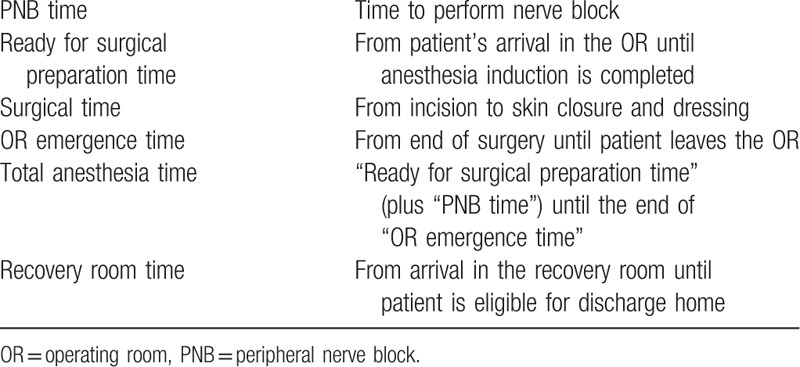
BIS was recorded during general anesthesia and vital parameters were documented continuously until the patients were discharged home. The process times defined in Table 1 were documented. A study nurse who was blinded to the group allocation gathered and recorded the data regarding pain intensity (NRS 0–10), undesired postoperative events (e.g., nausea, vomiting, paresthesias or other neurological symptoms, dysphagia), consumption of analgesic drugs at home, and patient satisfaction with anesthetic management (on a scale of 1 = very satisfied to 6 = very unsatisfied). These data were obtained with a standardized protocol in the recovery room, and by telephone on the evening of surgery and on the 2 following days.
Table 1.
Definitions of perioperative process times.
2.5. Statistical analysis
The primary outcome factors were incidence and severity of postoperative pain and time spent in recovery room. Secondary outcomes were total anesthesia time and postoperative complications. Most patients with general anesthesia experience pain on the day of surgery and the day after.[9] Thirty-four patients per group would be required to detect a 30% decrease in this incidence at a significance level of 5% and a power of 90%. We enrolled more patients in each group in order to detect an even smaller effect (see the “Results” section). The data were analyzed with the statistics program STATISTICA (Version 12, StatSoft, Dell Inc, Round Rock, TX). Continuous data were tested for normal distribution with the Kolmogorov–Smirnov test. Normally distributed data were described with mean and standard deviation, other with median and range. Categorical data were given as percentages. Normally distributed data were compared with the Student t test, non-normal data with Mann–Whitney U test. Categorical data were compared with Fisher exact test. A P value <0.05 was defined as statistically significant.
3. Results
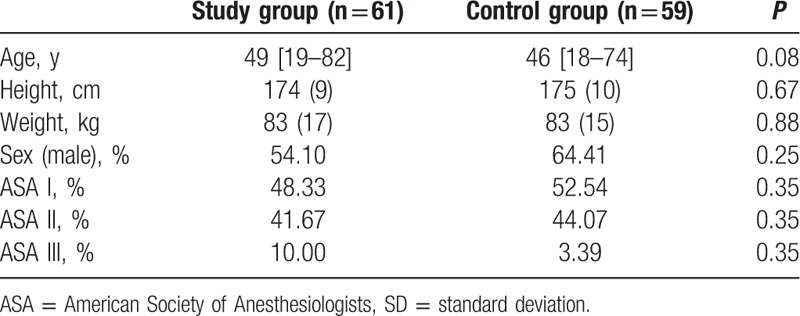
A total of 121 patients were recruited for the study. One patient in the study group was excluded from the analysis because of an incomplete dataset resulting in 61 patients in the study group and 59 in the control group. The groups did not differ significantly with regard to age, gender distribution, height, weight, or ASA classification (Table 2). The distribution of surgical site between upper and lower extremity was the same in both groups.
Table 2.
Characteristics of patients (median [range], means (± SD)).
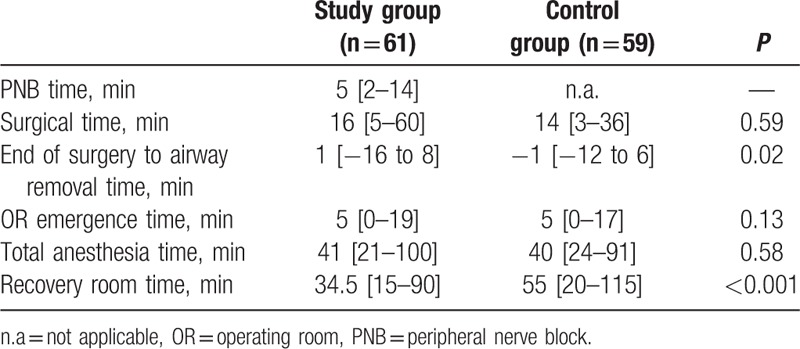
The median time required to perform the single-shot peripheral nerve block was 5 min (range 2–15). All peripheral nerve blocks were successful. Heart rate and blood pressure were within normal limits in both groups during general anesthesia. The total dose of propofol (induction dose plus infused amount) required to maintain the BIS within the defined limits was significantly greater in the control group (GA + NB: 6.0 ± 1.4 mg/kg BW per h; GA: 6.8 ± 1.4 mg/kg BW per h, P < 0.001).
Median total anesthesia time and surgical time did not differ between the groups (Table 3). The laryngeal mask airway was removed at the end of surgery when adequate spontaneous respiration had returned. The airway device was removed earlier in the study group (Table 3). The median time until the patients were transferred to the recovery room was the same in both groups.
Table 3.
Process times (median [range]).
A similar number of patients in both groups reported preoperative pain in the extremity scheduled for surgery, and the reported intensity was also similar (Table 4). Only patients in the control group (44%) reported relevant pain (NRS > 3) arising already in the recovery room and they were given 1 g metamizole (dipyrone). More patients in the control group than in the study group had pain at least until the 2nd postsurgical day (Table 4). Prescribed analgesic medication was taken by 63% of the study patients and 79% of the controls (P = 0.07). Neither the patients of the study group nor of the control group took rescue analgesic at home.
Table 4.
Perioperative pain in operated extremity and patient satisfaction.
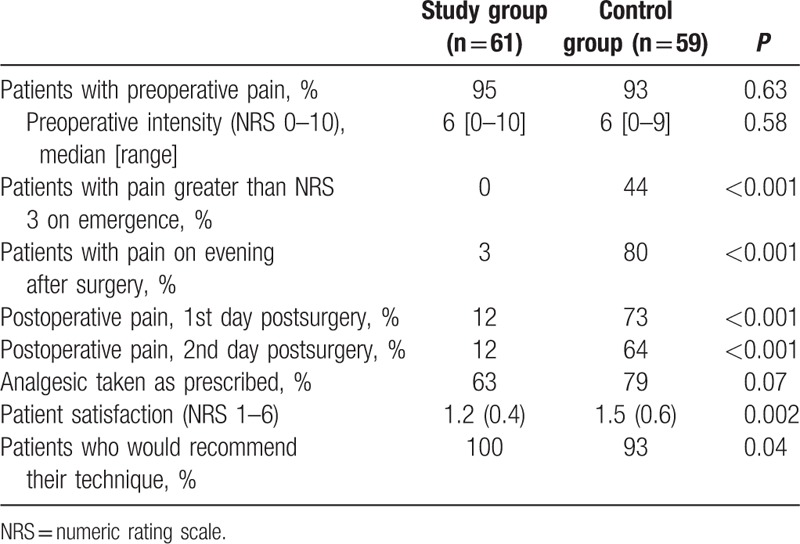
The patients in the study group were eligible for home discharge after a recovery room stay of 34.5 min (range 15–90) compared with 55 min (20–115) in the control group (P < 0.001). Muscle strength in the extremity with the nerve block had recovered fully (MRC 5) after a median time of 5 min (0–75) after emergence. Paresthesias in the extremity undergoing surgery were reported on the day after surgery by 35% of the study patients and 14% of the controls (P < 0.001).
The groups did not differ in the incidences of nausea and vomiting, shivering, airway morbidity, or severity of dysphagia. The combination of peripheral nerve block with general anesthesia was given a better overall rating than general anesthesia alone. More patients with the anesthetic combination would recommend their technique than those with general anesthesia alone (Table 4).
4. Discussion
In this study, we investigated whether the combination of general anesthesia with a single-shot peripheral nerve block using a small volume of ropivacaine in a low concentration would have an effect on recovery and postoperative pain compared with general anesthesia alone. Our results showed that patients with the combination were eligible for home discharge earlier and had less postoperative pain than those with general anesthesia alone.
Continuous regional block, either alone or in combination with general anesthesia, has been shown to reduce the severity of postoperative pain and speed postoperative recovery, and regional blocks have been recommended for outpatient surgery.[1,4,5,10] However, it has not been clearly established how a single-shot nerve block using a low-volume, low-concentration local anesthetic and combining with general anesthesia would affect late postoperative pain.
In the present study, patients who had a single-shot peripheral nerve block had lower incidence of pain and less severe pain at least until the 2nd day after surgery. This persisting analgesia covers the core time of postoperative pain,[9] but cannot be explained by a direct residual effect of the local anesthetic, since the effects of ropivacaine wear off after 10 h. Espelund et al[11] could not show any benefit for an adductor canal block at all compared to a basic analgesic regimen of paracetamol and ibuprofen conducted after completing the surgical procedure of arthroscopic anterior cruciate ligament reconstruction. We suggest, however, that by blocking nociceptive input to spinal and supraspinal centers before beginning the surgical trauma, the nerve block acted in a manner that prevented central sensitization during surgery and hence postoperative hyperalgesia.[12] Opioids produce analgesia but are unable to block central nociceptive input or prevent sensitization.[13] Opioid-induced hyperalgesia resulting from the use of remifentanil may have been present and possibly increased the intensity of early postoperative pain in the control patients. The duration of this hyperalgesia, which may last for several hours,[14] may have coincided with the duration of the nerve block in the study patients and thus have not been noticeable. It is unlikely that the extent of the opioid-induced hyperalgesia would have been different in the 2 groups, and it is therefore unlikely that it contributed to the observed difference between the 2 groups with regard to the incidence of pain.
While regional anesthesia can reduce postoperative pain, it is infrequently used in the outpatient setting.[5] This is probably based on the assumption that the associated muscle block tends to prolong the stay in the recovery room. In order to avoid this problem, we used a small volume of the local anesthetic in a low concentration to induce a differential block, that is, analgesia with little effect on muscle strength.[15] This is possible with 0.2% ropivacaine. As expected, patients in the study group showed fast recovery from the motor block. In a volunteer study, low volume 0.2% ropivacaine gave sufficient nerve block to be used as the sole anesthetic in up to 90% of the cases.[16] Combining this with a general anesthetic removes the risk of inadequate analgesia.
The risk of nerve damage is frequently given as the reason not to choose peripheral nerve blocks.[17] But Sites and co-workers[18] recently documented that ultrasound-guided peripheral nerve blocks are a very safe technique. A considerable number of patients with a peripheral nerve block reported paresthesias in the extremity that had undergone surgery, but this had resolved after 1 day at the latest. It is interesting to note that 14% of the patients who had not been given a nerve block also reported paresthesias probably due to the intraoperatively used tourniquet or the surgical trauma.
As also shown in several other studies,[4,5,19] total anesthesia time was not prolonged by the establishment the peripheral nerve block. This result was largely due to an optimally organized workflow with a separate room in which the nerve block was performed parallel to ongoing surgery, and to the use of ultrasound-guided techniques to localize the nerves.
Patients with general anesthesia alone recovered control of their airways a clinically irrelevant 2 min earlier than patients in the study group. In numerous patients, the airway device could be removed before the final stitches had been laid and the dressing applied. Transfer to the recovery room was not delayed in any way in either group.
The groups did differ significantly and to a clinically relevant extent with regard to the time until the patients were eligible for discharge home. Any concerns regarding persisting motor block preventing discharge home were unfounded as is also shown in other studies.[4,5,19] The motor block had resolved within a median interval of 5 min after arrival in the recovery room. With the combination of low-dose peripheral nerve block and general anesthesia, the recovery room times in our patients were shorter than those published for brachial plexus block alone where a larger volume of a more highly concentrated local anesthetic was required to provide adequate analgesia.[19] The patients in the study group had also received a significantly lower total dose of propofol and were thus less impaired by its residual effects. The onset of pain requiring treatment also prolongs recovery room stay.
There are some limitations to our study. At the moment we cannot exclude a placebo-effect triggered by nerve blockade procedure in the study group; to exclude such an effect, perineural injection could be done with saline solution in the control group. Furthermore, according to the fact that the measured postoperative pain scores were low per se due to the less invasive operations, nerve blockade procedures may not be superior to the same extent in more invasive surgical procedures. Using scheduled working days could have been lead to cluster effects.
The combination of general anesthesia with a low-volume, low-concentration, and single-shot peripheral nerve block for arthroscopies reduces postoperative pain for at least 2 days after surgery compared with general anesthesia alone. It also speeds recovery, allows earlier discharge home, and meets with a higher degree of patient satisfaction.
Footnotes
Abbreviations: ASA = American Society of Anesthesiologists, BIS = bispectral index, BW = body weight, GA = control group, MRC = Medical Research Council, NB + GA = study group, NRS = numeric rating scale.
BB: conception and design of the study, patient recruitment, acquisition of data, data analysis and interpretation, writing the first draft of the paper, final approval of the submitted manuscript. AM: patient recruitment, acquisition of data, final approval of the submitted manuscript. JH: design of the study, data analysis and interpretation, final approval of the submitted manuscript. JE: data analysis and interpretation, final approval of the submitted manuscript. MB: design of the study, data analysis and interpretation, final approval of the submitted manuscript. IB: conception and design of the study, acquisition of data, patient recruitment, data analysis and interpretation, and finalization the first draft of the paper.
All authors had full access to all of the data and can take responsibility for the integrity of the data and the accuracy of the data analysis.
The authors declare that the co-author AM, Associate Professor, is an Academic Editor of Medicine (Section Anesthesiology). This does not alter the authors’ adherence to all the Medicine policies.
BB and AM have equally contributed to this work.
This work was supported only by departmental funding sources.
The authors have no conflicts of interest to disclose.
References
- [1].White PF, Eng M. Fast-track anesthetic techniques for ambulatory surgery. Curr Opin Anaesthesiol 2007;20:545–57. [DOI] [PubMed] [Google Scholar]
- [2].Fosnot CD, Fleisher LA, Keogh J. Providing value in ambulatory anesthesia. Curr Opin Anaesthesiol 2015;28:617–22. [DOI] [PubMed] [Google Scholar]
- [3].Schug SA, Chong C. Pain management after ambulatory surgery. Curr Opin Anaesthesiol 2009;22:738–43. [DOI] [PubMed] [Google Scholar]
- [4].Liu SS, Strodtbeck WM, Richman JM, et al. A comparison of regional versus general anesthesia: a meta-analysis of randomized controlled trials. Anesth Analg 2005;101:1634–42. [DOI] [PubMed] [Google Scholar]
- [5].Kopp SL, Horlocker TT. Regional anaesthesia in day-stay and short-stay surgery. Anaesthesia 2010;65(suppl 1):84–96. [DOI] [PubMed] [Google Scholar]
- [6].Wennervirta J, Hynynen M, Koivusalo AM, et al. Surgical stress index as a measure of nociception/antinociception balance during general anesthesia. Acta Anaesthesiol Scand 2008;52:1038–45. [DOI] [PubMed] [Google Scholar]
- [7].Barreveld A, Witte J, Chahal H, et al. Preventive analgesia by local anesthetics: the reduction of postoperative pain by peripheral nerve blocks and intravenous drugs. Anesth Analg 2013;116:1141–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Medical Research Council. Aids to Examination of the Peripheral Nervous System. Memorandum no. 45. London: Her Majesty's Stationery Office; 1976. [Google Scholar]
- [9].Gerbershagen HJ, Aduckathil S, van Wijck AJ, et al. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology 2013;118:934–44. [DOI] [PubMed] [Google Scholar]
- [10].Boezaart AP, Davis G, Le-Wendling L. Recovery after orthopedic surgery: techniques to increase duration of pain control. Curr Opin Anaesthesiol 2012;25:665–72. [DOI] [PubMed] [Google Scholar]
- [11].Espelund M, Fomsgaard JS, Haraszuk J, et al. Analgesic efficacy of ultrasound-guided adductor canal blockade after arthroscopic anterior cruciate ligament reconstruction: a randomised controlled trial. Eur J Anaesthesiol 2013;30:422–8. [DOI] [PubMed] [Google Scholar]
- [12].Rivat C, Bollag L, Richebé P. Mechanisms of regional anaesthesia protection against hyperalgesia and pain chronicization. Curr Opin Anaesthesiol 2013;26:621–5. [DOI] [PubMed] [Google Scholar]
- [13].Katz J, Clarke H, Seltzer Z. Review article: Preventive analgesia: quo vadismus? Anesth Analg 2011;113:1242–53. [DOI] [PubMed] [Google Scholar]
- [14].Fletcher D, Martinez V. Opioid-induced hyperalgesia in patients after surgery: a systematic review and a meta-analysis. Br J Anaesth 2014;112:991–1004. [DOI] [PubMed] [Google Scholar]
- [15].Kii N, Yamauchi M, Takahashi K, et al. Differential axillary nerve block for hand or forearm soft-tissue surgery. J Anesth 2014;28:549–53. [DOI] [PubMed] [Google Scholar]
- [16].Marhofer P, Eichenberger U, Stöckli S, et al. Ultrasonographic guided axillary plexus blocks with low volumes of local anaesthetics: a crossover volunteer study. Anaesthesia 2010;65:266–71. [DOI] [PubMed] [Google Scholar]
- [17].Matthey PW, Finegan BA, Finucane BT. The public's fears about and perceptions of regional anesthesia. Reg Anesth Pain Med 2004;29:96–101. [DOI] [PubMed] [Google Scholar]
- [18].Sites BD, Taenzer AH, Herrick MD, et al. Incidence of local anesthetic systemic toxicity and postoperative neurologic symptoms associated with 12,668 ultrasound-guided nerve blocks: an analysis from a prospective clinical registry. Reg Anesth Pain Med 2012;37:478–82. [DOI] [PubMed] [Google Scholar]
- [19].Gonano C, Kettner SC, Ernstbrunner M, et al. Comparison of economical aspects of interscalene brachial plexus blockade and general anaesthesia for arthroscopic shoulder surgery. Br J Anaesth 2009;103:428–33. [DOI] [PubMed] [Google Scholar]


