Abstract
Exposure to protective factors, conditions that protect against the occurrence of an undesirable outcome or promote the occurrence of a desirable outcome within an adolescent’s environment, can foster healthy adolescent behaviors and reduce adult morbidity and mortality. Yet, little is known about the nature and effect of protective factors on the positive social and health outcomes among American Indian and Alaska Native (AIAN) adolescents. We conducted a review of the literature to identify the protective factors associated with positive health outcomes among AIAN adolescents. We consulted Elsevier Science Direct, ERIC EBSCOhost, PubMed, and the Web of Science databases. A total of 3,421 articles were encountered. Publications that did not focus on AIAN adolescents (n=3,341), did not identify protective factors (n=56), were not original research studies (n=8) or written in the English language were excluded. We identified nine categories of protective factors positively associated with health and social outcomes, including: current and/or future aspirations, personal wellness, positive self-image, self-efficacy, non-familial connectedness, family connectedness, positive opportunities, positive social norms, and cultural connectedness. Such factors positively influenced adolescent alcohol, tobacco, and substance use; delinquent and violent behavior; emotional health including depression, suicide attempt; resilience; and academic success. Protective factors spanned multiple domains of the socio-ecological model. Strengths-based health promotion efforts that leverage local, innate protective factors and work with AIANs to create environments rich in protective factors are key to improving the health and wellbeing of AIAN adolescents.
Keywords: American Indian, Alaska Native, Adolescent, Protective Factors, Asset-based
Introduction
Many of the leading causes of morbidity and mortality in American Indian and Alaska Native (AIAN) adults can be traced back to adolescent behaviors (CDC, 2015a; Lowe, Riggs, Henson, & Leihr, 2009), which indicates that adolescent behaviors are an important factor that should be a focus for improving AIAN health overall. Adolescent health behaviors are influenced by many co-occurring factors within the environment. Cummins et al. (1999) concluded that the negative environmental forces to which AIAN adolescents may be exposed to in their homes, schools, or community often predispose them to adverse health and social outcomes. However, not all AIAN adolescents engage in high-risk behaviors. The aim of this review of peer-reviewed literature is to identify the protective factors that are associated with healthy behaviors or positive health outcomes among AIAN adolescents. Understanding the determinants of health and identifying modifiable factors that support positive health choices during adolescence can inform interventions designed to improve AIAN adolescent health (Borowsky, Resnick, Ireland, & Blum, 1999; Whitesell et al., 2014).
Protective factors are conditions or variables capable of directly affecting adolescents and increasing the likelihood of positive health outcomes (Hawkins, Cummins, & Marlatt, 2004; Jessor, Turbin, & Costa et al., 1998). Multiple protective factors can foster healthy behaviors even when risk factors and adversity are present (Borowsky et al., 1999; Cummins et al., 1999; Hawkins et al., 2004; Jessor et al., 1998; LaFromboise, Hoyt, Oliver, & Whitbeck et al., 2006). Identifying protective factors at the individual, relationship, and community levels of the socio-ecological framework for prevention (CDC, 2015a), and recognizing ways to leverage these factors, are foundational to promoting AIAN adolescent and subsequent adult health (Cummins et al., 1999; LaFromboise et al., 2006; Mmari, Blum, & Teufel-Shone, 2010). We conducted a review of the literature to identify the protective factors associated with positive health outcomes among AIAN adolescents.
Methods
We conducted a search of the academic literature to identify factors within the socio-ecological domains of individual, relationship, and community levels associated with positive health outcomes among AIAN adolescents. We defined protective factors as any condition or variable that protects against the occurrence of an undesirable outcome (e.g., substance use), or promotes the occurrence a desirable outcome (e.g., academic success; Hawkins et al., 2004; Jessor et al., 1998). In our search we consulted Elsevier Science Direct, ERIC EBSCOhost, PubMed, and the Web of Science databases. Exact search terms used for each database included “American Indian,” “Alaska Native,” “adolescent,” “protective factors,” “protective mechanisms,” and “supportive factors.” We found that various age ranges were used to describe the adolescent life-stage as no standard age definition currently exists (AAP, 2003; APA, 2002; WHO 2015). Consequently, we defined adolescence as 10 to 21 years of age to be as inclusive as possible. Our search considered English-language articles published between January 1, 1970, and January 1, 2015.
A total of 16 quantitative and two qualitative studies are included in this review. Among the quantitative studies, we reviewed the protective factors identified by the study authors that were significantly associated with the outcome of interest. Among the qualitative studies, we reviewed the protective factors found to be salient to the study by the authors who conducted the analyses.
Results
We found a total of 3,421 articles (Figure 1). We excluded publications that did not focus on AIAN adolescents (n=3,341), did not identify protective factors (n=56), or were not original research studies (n=8). A total of 16 publications met the search criteria during the initial review; two of which (Allen et al., 2006; Mmari et al., 2010) were qualitative studies involving AIAN adolescents and adults. In the work done by Allen et al. (2006), Alaska Native (AN) adults were interviewed to retrospectively identify the protective factors they experienced as adolescents. In the study conducted by Mmari et al. (2010), focus groups were conducted with American Indian (AI) adolescents and adults to identify protective factors affecting AI adolescents. Upon detailed review of the selected articles, we found two additional publications meeting search criteria in one article’s bibliography (Cummins et al., 1999; Pu et al., 2013) and included them in this review. A total of 18 studies were reviewed. The selected research publications are predominately cross-sectional in design using self-administered close-ended survey methodology. Four studies (Barney, 2001; Borowsky et al., 1999; Cummins et al., 1999; Pharris, Resnick, & Blum, 1997) used data sets from the National American Indian Adolescent Health Survey from various years. Three studies (Bearinger et al., 2010, 2005; Pettingell et al., 2008) used data sets from the Urban Indian Health Survey for the years 1995–1998. Two publications by the same authors (Bearinger, Pettingell, Resnick, & Potthoff, 2010; Bearinger et al., 2005) were reviewed as one publication as both studies drew on the same study population assessing similar health outcomes (i.e., violence and weapon-carrying).
Figure 1.
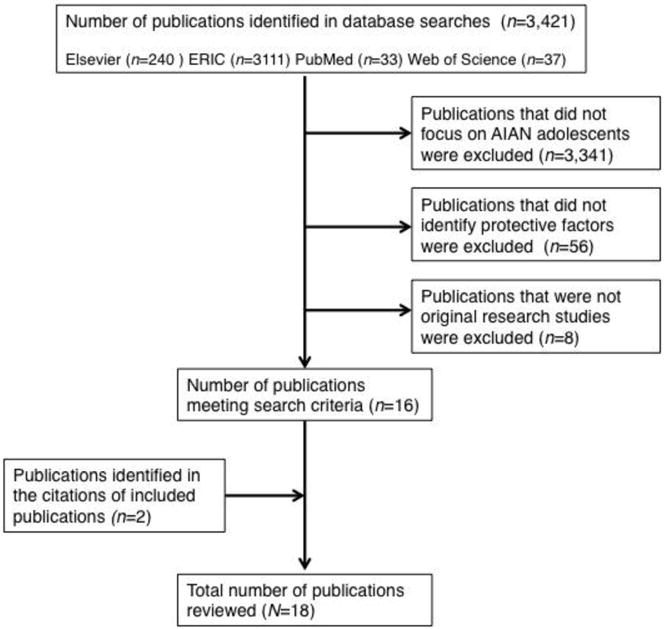
Number of Publications Identified and Selected
Table 1 provides an overview of the studies included in this review and lists the protective factors that are identified as either statistically significant (quantitative studies) or salient to study authors (qualitative studies) as identified in the Identified Protective Factors column. Table 1 is organized by the health and social outcome of interest for the particular study in order to display the identified protective factors from the literature that are found to have an association with that health/social outcome.
Table 1.
Protective Factors found to be significantly associated with positive health and social outcomes among AIAN adolescents aged 10–21 years (1997–2015)
| Health/Social Outcome | Publication | Study Population | Study Methodology | Instrument | Identified Protective Factors |
|---|---|---|---|---|---|
| Academic Success | Whitbeck et al. (2001) | 196 AI students, ages 10 to 15 (mean age=12.1–12.2) living on or near three reservations in the upper Midwest | Cross-sectional Adolescents completed structured, closed-ended surveys |
Self-esteem was assessed using the Tri-Ethnic Center’s self- esteem scale. Maternal warmth was measured using a scale adapted from the Iowa Youth and Families Project. Enculturation was measured using the AI cultural identification items (Oetting & Beauvais, 1991) and questions developed by the researchers and local advisory board. Other close-ended questions were developed by the researchers to measure participation in sports or clubs. | – Protective factors associated with school success were: high self-esteem, maternal warmth, enculturation, participation in sports or clubs after school |
| Alcohol Abuse | Allen et al. (2006) | 51 AN adults who had been lifetime abstainers, non- problem drinkers, or sober for the last five years, ages 19 to 83 (mean age = 49), from rural Alaska villages | Qualitative Researchers interviewed participants using a standard set of questions to identify retrospectively protective factors linked to their non-use or non-abuse of alcohol as adolescents |
Semi structured interviews using a standard set of questions developed by the researchers and community co- researchers | – Community characteristics associated with low alcohol abuse were: positive adult role models, rites of passage involving the opportunity to contribute to the community, limit setting on alcohol behavior, and the provision of safe places for children. – Family characteristics associated with low alcohol abuse were: close relationships with parents; parents acting as teachers/providing guidance; safe family environment where abusive alcoholic behavior was not tolerated; modeling of sobriety; expression of praise, affection, and specialness of the child; and transmission of cultural expectations and values. – Individual characteristics associated with low alcohol abuse were: wanting to be a role model, giving to others by contributing to the community, believing in one’s value and potential, awareness of consequences of one’s behavior, “interconnection” (a cultural term specific to the population), having awareness of life goals, and self- efficacy |
| Delinquent Behavior | Mmari et al. (2010) | 172 adolescent and adult AIs from an urban tribal community in the Southwest, a rural reservation in the Southwest, or a urban tribal community in the Midwest | Qualitative Focus groups identified protective factors linked to adolescents’ non-delinquent behavior |
Focus group guide developed by the researchers through key informant interviews at each site | – Community-level protective factors associated with low delinquent behavior were: tribal language, and adolescent involvement in ceremonies and pow wows. – School-level protective factors associated with low delinquent behavior were: mentors and role models in whom adolescents could confide. – Family-level protective factors associated with low delinquent behavior were: parental support. – Individual-level protective factors associated with low delinquent behavior were: religion or sense of spirituality, and motivation to succeed in life. |
| Depression | Barney (2001) | 2,034 AI students, 7th–12th grade, from reservation-based schools in 8 IHS service areas | Cross-sectional Self-administered, structured, close-ended survey |
National American Indian Adolescent Health Survey (1988) | – Protective factors associated with low number of depressive symptoms were: feeling cared about by family, feeling cared about by non-familial adults, and help- seeking behaviors (defined as an adolescent’s willingness to seek help from a parent or other adult). |
| Emotional Health | Cummins et al. (1999) | 13,454 AIAN students, 7th–12th grade, from reservation-based schools in 8 IHS service areas | Cross-sectional Self-administered, structured, close-ended survey |
National American Indian Adolescent Health Survey (1991–1992) | – Protective factors associated with emotional health in females were: perceived family caring, body pride, and religiosity. – Protective factors associated with emotional health in males were: perceived family caring, body pride, religiosity, and identification of a personal area of skill or competence |
| Resilience | LaFromboise et al. (2006) | 212 AI students, ages 10 to 15 (mean age=12.1–12.2) living on or near three reservations in the upper Midwest | Cross-sectional Adolescents self- administered structured, closed-ended surveys |
Enculturation was measured using the American Indian Cultural Identification Scale (Oetting & Beauvais, 1991) and additional questions developed through focus groups with local tribal members. Other close-ended questions were developed by the researchers and tribal community members to measure community support and maternal warmth. | – Protective factors associated with resilience were: enculturation, community support, and maternal warmth. |
| Substance Use | Moilanen et al. (2014) | 5,701 AIAN students, grades 8, 10 and 12, attending Arizona schools | Cross-sectional Self-administered, structured, close-ended survey |
Arizona Youth Survey (AYS) (2010) | – Protective factor associated with low substance use was: availability of extra curricular activities to adolescents. |
| Substance Use | Whitesell et al. (2014) | 381 AI students, 6th and 7th grade, attending seven different schools on a rural, northern Plains reservation | Cross-sectional Self-administered, structured, close-ended survey |
Close-ended questions developed by the researchers | – Protective factors associated with low substance use were: parent-child relationship, and pro-social peer influence. |
| Substance Use | Yu & Stiffman (2010) | 196 urban and 205 reservation-based youth, ages 13 to 19 (M= 15.4), living in a Southwestern state | Cross-sectional Face-to-face, structured, close-ended interviews |
Positive family relationships were measured using an adapted version of the Family Satisfaction Scale (Hudson, 1982). | – Protective factor associated with low substance abuse/dependence was: positive family relationships. |
| Suicide Attempt | Borowsky et al. (1999) | 11,666 AIAN students, 7th–12th grade, from reservation-based schools in 8 IHS service areas | Cross-sectional Self-administered, structured, close-ended survey |
National American Indian Adolescent Health Survey (1990) | – Protective factors associated with low suicide attempt were: discussing problems with friends or family members, good emotional health, and family connectedness. |
| Suicide Attempt | Mackin et al. (2012) | 503 AIAN students, ages 12 to 18 (mean age= 15), attending Oregon public schools | Cross-sectional Self-administered, structured, close-ended survey |
Oregon Healthy Teens Survey (2006) | – Protective factors associated with low suicide attempt were: ate breakfast seven out of seven days, very good or excellent physical health, and feeling able to handle problems (self-efficacy). |
| Suicide Attempt | Pettingell et al. (2008) | 569 AIs, ages 9 to 15 (mean age= 11.9), attending urban-based schools in Minneapolis, MN or attending an after-school program in Minneapolis, MN | Cross-sectional Self-administered, structured, close-ended survey |
Urban Indian Health Survey (1995–1998) | – Protective factor associated with low suicide attempt in females was: having a positive mood. – Protective factors associated with low suicide attempt in males were: having a positive mood, and parental pro-social behavior norms. |
| Suicide Attempt, Suicide Ideation, Hopelessness | Pharris et al. (1997) | 1,157 AIAN students, 7th–12th grade, from reservation-based schools in 8 IHS service areas, who self- reported past sexual abuse | Cross-sectional Self-administered, structured, close-ended survey |
National American Indian Adolescent Health Survey (1988–1990) | – Protective factors associated with the absence of suicide attempt in females were: attention from family, parental expectations, parent caring, and positive feelings about school. – Protective factors associated with the absence of suicide attempt in males were: positive feelings about school, family caring, involvement with traditional activities, and doing well in school. – Protective factors associated with the absence of suicide ideation in females were: family caring, parent caring, tribal leader caring, adult caring, attention from family, doing well in school, positive feelings about school, and parental expectations. – Protective factors associated with the absence of suicide ideation in males were: attention from family, adult caring, school officials caring, tribal leaders caring, and doing well in school. – Protective factors associated with the absence of hopelessness in females were: family caring, attention from family, tribal leaders caring, positive feelings about school, adult caring, and parental expectations. – No significant protective factors associated with the absence of hopelessness were identified for males. |
| Tobacco Use | LeMaster et al. (2002) | 2,390 AI students, ages 13 to 20 (mean age= 16.2), in 10 Western AI communities | Cross-sectional Self-administered, structured, close-ended survey |
Social support was measured using a social support scale (Zimet et al., 1998). Community mindedness was measured using an adapted version of a community mindedness scale (Sack et al., 1987). Other close-ended questions developed by the researchers to measure academic orientation and ethnic identity. | – Social support, community mindedness, academic orientation, and ethnic identity were not found to significantly contribute to tobacco use. |
| Tobacco Use | Osilla et al (2007) | 112 AIANs, ages 13 to 19 (mean age= 15), participating in a Seattle-based life-skills program | Cross-sectional Face-to-face, researcher administered structured, close-ended interviews |
Comprehensive Adolescent Severity Inventory (CASI) | – Protective factors associated with low tobacco use were: an adolescent possessing college aspirations, participation in a sports team, and participation in music. |
| Violent Behavior | Pu et al. (2013) | 630 AI students, 6th to 12th grade, from 5 Midwestern rural school (4 of 5 schools located on reservations) | Cross-sectional Self-administered, structured, close-ended survey |
Youth Intervention Project survey (1998) with an additional question developed by the researchers to measure adolescents’ interest in his or her tribe. | – Protective factors associated with low violent behavior were: perceived parental monitoring, self-efficacy in avoiding violence, and an interest in culture. |
| Violent Behavior & Weapon Carrying | Bearinger et al. (2005, 2010) | 577 AI adolescents, ages 9 to 15 (mean age= 11.9), attending various urban-based schools in Minneapolis, MN or attending an after-school program in Minneapolis, MN | Cross-sectional Self-administered, structured, close-ended survey |
Urban Indian Health Survey (1995–1998) | – Protective factors associated with low violent behavior were: school connectedness (defined as an adolescent feeling cared about by school staff and feeling school attendance was valued), peer pro-social behavior norms, and parent pro- social behavior norms. – Protective factors associated with low weapon-carrying were: school connectedness, and peer pro-social behavior norms. |
We used inductive content analysis to identify recurring themes among the identified protective factors, and then developed a thematic categorization system (Patton, 2002); in this case, themes identified in three or more publications are determined to be recurring. Based on these recurring themes and through a process of consensus (Guba, 1978), we developed a codebook to organize and define the thematic categories (Table 2). Thematic categories for protective factors included: current and future aspirations, personal wellness, positive self-image, self-efficacy, non-familial connectedness, family connectedness, positive opportunities, positive social norms, and cultural connectedness. Protective factors are categorized across the domains of individual, relationship, and community. Because cultural connectedness is identified as a protective factor in several socio-ecological domains, cultural connectedness is listed as a multi-level protective factor. Information regarding the study sample size and, in some cases, the definition of the study’s term(s), is included the first time a study appears in the results section.
Table 2.
Protective factors identified in the literature by protective factor thematic category
| Socio-Ecological Level | Protective Factor Thematic Category | Definition | Example Protective Factors Identified in the Literature |
|---|---|---|---|
| Individual Protective Factors | Current/Future Aspirations | An adolescent possessing goals and/or positive outlook regarding the present and/or future | College aspirations10; motivation to succeed in life8; wanting to be a role model1; having awareness of life goals1; positive feelings about school12; doing well in school12 |
| Personal Wellness | An adolescent possessing a high-level of personal health and wellness | (Eating) breakfast seven out of the last seven days7; very good or excellent physical health7; emotional health4; positive mood10 | |
| Positive Self-Image | An adolescent possessing a positive view of him or herself | Believing in one’s value and potential1; body pride5; identification of a skill5; high self-esteem14 | |
| Self-Efficacy | An adolescent possessing the feelings of being able to perform certain behaviors to accomplish goals | Feeling able to handle problems7; self-efficacy1,13 | |
| Relationship Protective Factors | Non-Familial Connectedness | Positive relationship and or interactions between an adolescent and members of his or her school or neighborhood that are not family members | Feeling cared about by adults2,12; community support6; discussing problems with friends4; mentors8; school connectedness3; prosocial peer influence15 |
| Family Connectedness | Positive relationship and/or interactions between an adolescent and members of his or her family | Close relationships with parents1; parents providing guidance1; expression of praise, affection, and specialness of the child1; discussion problems with family4; family connectedness4; family caring12; attentions from family12; parent caring12; feeling cared about by family2,5; maternal warmth6,14; parent-child relationships15; parental monitoring13; parental support8; positive family relationships16 | |
| Community Protective Factors | Positive Opportunities | Opportunities available to an adolescent within his or her school or community which provide the opportunity to engage in positive behaviors | Availability of extra curricular activities9; participation in sports10,14; participation in clubs14; participation in music10; opportunity to contribute to the community1 |
| Positive Social Norms | Individuals within an adolescent’s community who establish expectations of healthy behavior and/or serve as an example of healthy behavior | Parent prosocial behavior norms3,11; peer prosocial behavior norms3,15; positive adults role models1; modeling (of healthy behaviors)1 | |
| Multi-Level Protective Factors | Cultural Connectedness | Any aspect of an adolescent’s life that is uniquely influenced by his or her connection and/or engagement with his or her tribal culture | Enculturation6,14; interest in AIAN culture13; transmission of cultural expectations and values1; “interconnection”1; tribal language8; involvement in ceremonies and pow wows8; involvement with traditional activities12 |
Individual Protective Factors
Individual level protective factors include characteristics an adolescent personally possesses, including personal history and biological characteristics (CDC, 2015b). The protective factors identified on the individual level include current and/or future aspirations, personal wellness, positive self-image, and self-efficacy.
Current and/or Future Aspirations
Four studies identified possessing current or future aspirations as a protective factor. Osilla et al. (2007) found college aspirations to be the most influential protective factor against tobacco use in a sample of 112 AIAN adolescents. Through qualitative focus groups and interviews with 172 AIs, Mmari et al. (2010) identified motivation to succeed in life as a protective factor against delinquency and violent behavior. Allen et al. (2006) interviewed 51 AN adults who had been lifetime abstainers, non-problem drinkers, or sober for the last five years and found wanting to be a role model and having awareness of life goals to be protective against alcohol use and abuse. In a sample of 1,157 AIAN adolescents who had self-reported past sexual abuse, Pharris et al. (1997) identified positive feelings about school to be protective against suicide attempt in male and female adolescents, and protective against suicide ideation and hopelessness in female adolescents. Pharris et al. (1997) also identified doing well in school to be protective against suicide attempt in male adolescents and suicide ideation in both male and female adolescents.
Personal Wellness
Three studies identified adolescent personal wellness as a protective factor. From a sample of 503 AIAN adolescents, Mackin et al. (2012) identified [eating] breakfast seven out [of] past seven days and self-identifying as being in very good or excellent physical health as protective factors against suicide attempt. Borowsky et al. (1999) identified emotional health, defined as an adolescent’s emotional state (feelings of control, satisfaction, rest, emotional security, relaxation, and cheerfulness) in the last month as a protective factor against suicide attempt in a sample of 11,666 AIAN adolescents. Likewise, in a sample of 569 AI adolescents, Pettingell et al. (2008) identified positive mood as protective against suicide attempt.
Positive Self-Image
Three studies identified positive self-image as a protective factor for AIAN adolescents. Allen et al. (2006) identified believing in one’s value and potential as a protective factor against alcohol use and abuse. From a sample of 13,454 AIAN adolescents, Cummins et al. (1999) identified body pride in male and female adolescents and identification of personal area of skill in male adolescents as associated with emotional health. Whitbeck et al. (2001) found high self-esteem to be a contributing factor to school success in a sample of 196 AI adolescents.
Self-Efficacy
Three studies identified self-efficacy as a protective factor for AIAN adolescents. Mackin et al. (2012) identified feeling able to handle problems as a protective factor against suicide attempt. In a sample of 630 AI adolescents, Pu et al. (2013), found self-efficacy, defined as feeling able to avoid violence, to be protective against violent behavior. Lastly, Allen et al. (2006) found self-efficacy to be protective against alcohol use.
Relationship Protective Factors
Protective factors on the relationship level include the influential relationships an adolescent has with others including family members, peers, and non-familial adults (CDC, 2015b). The protective factors identified on the relationship level include non-familial connectedness and family connectedness.
Non-Familial Connectedness
Seven studies identified connectedness with others who are not family members to be a protective factor for AIAN adolescents. Pharris et al. (1997) found that [non-familial] adults caring, including school officials, religious leaders, and tribal leaders, were a protective factor against hopelessness in female adolescents and a protective factor against suicide ideation in male and female adolescents who self-reported past sexual abuse. Similarly, from a sample of 2,034 AI adolescents, Barney (2001) found feeling cared about by [non-familial] adults, including school staff, church leaders, and tribal leaders, to be protective against depression. From a sample of 212 AI adolescents, LaFromboise et al. (2006) identified community support as a factor contributing to adolescent ability to cope with adversity, or resilience, as defined by the study authors. LaFromboise et al. (2006) measured community support by asking adolescents to rate how concerned community members were about youth with regard to doing well in school, being good at sports, and learning their American Indian language and customs. Borowsky et al. (1999) identified discussing problems with friends as protective against suicide attempt. Mmari et al. (2010) found mentors within schools to be protective against adolescent delinquency. Likewise, from a sample of 577 AI adolescents, Bearinger et al. (2010, 2005) identified school connectedness, defined as an adolescent’s feeling cared about by school staff and that their school attendance was valued, to be protective against violent behavior and weapon carrying. In a sample of 381 AI adolescents, Whitesell et al. (2014) found prosocial peer influence, defined by researchers as the number of friends an adolescent possessed who volunteered, regularly attended sweats/ceremonies or church, thought schoolwork to be very important, and planned to go to college, to be protective against adolescent substance use.
Family Connectedness
Eleven studies identified family connectedness as being a protective factor for AIAN adolescents. Allen et al. (2006) found close relationships with parents, parents providing guidance, and parents’ expression of praise, affection and specialness of the child to be protective against adolescent alcohol use. Borowsky et al. (1999) identified discussing problems with family and family connectedness as protective against suicide attempt. Pharris et al. (1997) identified family caring to be protective against suicide attempt in male adolescents and against suicide ideation in female adolescents who self-reported past sexual abuse. Pharris et al. (1997) also identified attention from family as a protective factor against suicide attempt in female adolescents, suicide ideation in male and female adolescents, and feelings of hopelessness female adolescents who self-reported past sexual abuse, and identified parent caring as a protective factor against suicide attempts and suicide ideation in female adolescents who self-reported past sexual abuse. Similarly, Barney (2001) identified feeling cared about by family as protective against adolescent depression. LaFromboise et al. (2006) and Whitbeck (2001) explored the influence of maternal warmth, defined in both studies as the degree to which mother expresses caring and spends time with the adolescent. Maternal warmth fostered resilience (LaFromboise et al., 2006) and academic success (Whitbeck et al., 2001) in AI adolescents. Whitesell et al. (2014) found that parent-child relationships are a protective factor for substance use as assessed by the researchers through four measurements (maternal warmth, paternal warmth, parent-child communication, and shared activities). Pu et al. (2013) identified perceived parental monitoring to be a protective factor against adolescent violent behavior. Likewise, Mmari et al. (2010) found parental support protective against adolescent delinquency. Cummins et al. (1999) identified the most powerful protective factor associated with adolescent mental health to be perceived family caring. From a sample of 401 AIAN adolescents, Yu and Stiffman (2010) identified positive family relationships to be protective against adolescent substance abuse/dependence.
Community Protective Factors
Protective factors on the community level include the conditions and variables present in the settings an adolescent spends time including his or her school and neighborhood (CDC, 2015b). The protective factors identified on the community level include positive opportunities and positive social norms.
Positive Opportunities
Four studies identified the availability of positive opportunities as a protective factor for AIAN adolescents. From a sample of 5,701 AIAN adolescents, Moilanen et al. (2014) identified the availability of extra-curricular activities to be a protective factor against substance use. Whitbeck et al. (2001) found participation in a sports team and participation in clubs to be contributing factors for academic success, while Osilla et al. (2007) found participation in a sports team and participation in music to be protective against tobacco use. Allen et al. (2006) identified opportunities that allowed adolescents to contribute to the community as protective against alcohol use and abuse.
Positive Social Norms
Three studies identified the presence of positive role models as a protective factor for AIAN adolescents. Pettingell et al. (2008) found parent prosocial behavior norms, defined as an adolescents’ perception of their parents’ approval or disapproval of antisocial behavior, to be protective against suicide attempts. Allen et al. (2006) identified positive adult role models and modeling of sobriety to be protective against alcohol use and abuse. Bearinger et al. (2010, 2005) identified both peer prosocial behavior norms, defined as an adolescent’s perception of their peers’ approval or disapproval of antisocial behavior, and parent prosocial behavior norms, defined as an adolescent’s perception of their parents’ disapproval of antisocial behavior, to be protective against violent behavior and weapon carrying.
Multi-Level Protective Factors
Cultural connectedness appeared as a protective factor at the individual (LaFromboise et al., 2006, Pu et al., 2013; Whitbeck et al., 2001), relationship (Allen et al., 2006), and community levels (Mmari et al., 2010; Pharris el al., 1997).
Cultural Connectedness
Six studies identified cultural connectedness as a protective factor. LaFromboise et al. (2006) and Whitbeck et al. (2001) defined enculturation as composed of three components: involvement in traditional activities, identification with American Indian culture, and involvement and importance of traditional spirituality. On the individual level, LaFromboise et al. (2006) found enculturation to be the most influential protective factor in fostering resilience in AIAN adolescents. Similarly, Whitbeck et al. (2001) identified enculturation to be correlated with academic success. Pu et al. (2013) documented that those adolescents who had an interest in [their] tribe’s culture to be less likely to display violent behavior. On a relationship level, Allen et al. (2006) found the transmission of cultural expectations and values and the cultural concept of “interconnectedness” to be protective against adolescent alcohol abuse. On a community level, Mmari et al. (2010) identified both tribal language and an adolescent’s involvement in ceremonies and pow wows as protective against delinquent behaviors. Pharris et al. (1997) identified involvement with traditional activities to be protective against suicide attempt in male adolescents who reported past sexual abuse.
Discussion
We found a growing body of evidence demonstrating several protective factors associated with positive health and social outcomes of AIAN adolescents. We identified nine major categories of protective factors spanning individual, relationship, community, and multi-level domains. Given these findings, utilizing and enhancing protective factors at multiple levels could guide strength-based health promotion and prevention programing for adolescent AIANs. Interventions that enhance protective factors have the potential to be especially beneficial; when protective factors are strengthened, their positive health effects reach beyond the intervention’s target population to affect an entire community (Mackin et al., 2012). Additionally, the additive effects of multiple protective factors argue for leveraging several protective factors simultaneously (LaFromboise et al., 2006).
To our knowledge, this review of protective factors across multiple health outcomes among AIAN adolescents has not been conducted previously. Including both qualitative and quantitative studies is also unique and a strength of this review. We recommend the following for future health interventions with AIAN youth: 1) identify and utilize innate, local protective factors present within an AIAN community to promote adolescent health; and 2) focus on creating environments that are rich in protective factors across the domains of the social-ecological model.
Identify and leverage innate, local protective factors present within AIAN communities
A strengths-based approach to health promotion recognizes that a community possesses resources and capabilities as well as health concerns in need of attention (Jain & Cohen, 2013; Sabalauskas, Ortolani, & McCall, 2014). Providers in the child welfare and behavioral health fields have begun to utilize approaches that identify personal and community strengths and incorporate them as part of the process of improvement (Sabalauskas et al., 2014). Public health can utilize a strength-based approach by identifying the protective factors present within AIAN communities and integrating those factors into program design (Jain & Cohen, 2013). Table 3 displays examples from this literature review of protective factors and their observed positive effects across multiple health and social outcomes. A specific example of this practice in action can be seen in the The People Awakening Project (Allen, Mohatt, Fok, Henry, & People Awakening Team, 2009; Allen et al., 2006; Mohatt, Fok, Burket, Henry, & Allen, 2011). This project conducted qualitative interviews with 51 AN adults who had been lifetime abstainers, non-problem drinkers, or sober for the last five years in order to identify factors that led to their sobriety or recovery (Allen et al., 2009; Allen et al., 2006). These factors were then used to develop prevention programs for AN adolescents (Allen et al., 2009; Allen et al., 2006).
Table 3.
Protective factor categories and the health/social outcomes on which they have been identified as having a positive effect organized by theme and socio-ecological domain
| Protective Factor Thematic Category |
Health/Social Outcomes | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Academic Success |
Alcohol Abuse |
Delinquent Behavior |
Depression | Emotional Health |
Resilience | Substance Use |
Suicide | Tobacco Use | Violent Behavior |
|
| Individual-Level | ||||||||||
| Current/Future Aspirations | X1 | X8 | X12 | X10 | ||||||
| Personal Wellness | X4,7,11 | |||||||||
| Positive Self-Image | X14 | X1 | X5 | |||||||
| Self-Efficacy | X1 | X7 | X13 | |||||||
| Relationship-Level | ||||||||||
| Non-Familial Connectedness | X8 | X2 | X6 | X15 | X4,12 | X3 | ||||
| Family Connectedness | X14,16 | X1 | X8 | X2 | X5 | X6 | X15 | X4,12 | X13 | |
| Community-Level | ||||||||||
| Positive Opportunities | X14 | X1 | X9 | X10 | ||||||
| Positive Social Norms | X1 | X15 | X3 | |||||||
| Multi-Level | ||||||||||
| Cultural Connectedness | X14 | X1 | X8 | X6 | X12 | X13 | ||||
Focus on creating environments rich in protective factors across the domains of the social-ecological model
Our research is consistent with emerging literature that suggests “success, health, and prevention of problems often depend on the strengths that an individual possesses internally or can find in his or her family or environment” (Stiffman et al., 2007, p. 331). While health-promotion professionals can enhance existing interventions by locating protective factors within all areas of an adolescent’s life, a deeper understanding of the local definitions of complexities of social domains is required (Mackin et al., 2012). For example, family and extended family support is an important and powerful protective factor for AIAN adolescents (Allen et al., 2006; Barney, 2001; Borowsky et al., 1999; Cummins et al., 1999; LaFromboise et al., 2006; Mmari et al., 2010; Pharris et al., 1997; Pu et al., 2013; Whitbeck et al., 2001; Whitesell et al., 2014; Yu & Stiffman, 2010). In leveraging familial protective factors, intervention designs must recognize that AIAN definitions of family and kinship may differ from Euro-American definitions and family structures may look different from one AIAN community to the next (Whitbeck et al., 2001). Community-level protective factors, such as positive social norms and positive opportunities, also were found to improve the odds of health promoting behaviors among adolescents (Allen et al., 2006; Bearinger et al., 2010, 2005; Moilanen et al., 2014; Osilla et al., 2007; Pettingell et al., 2008; Pharris et al., 1997; Whitesell et al. 2014; Whitbeck et al., 2001). Public health practitioners and AIAN community members should partner to identify and enhance existing protective factors and create environments rich in protective factors. Through such collaborative partnerships in research and intervention design, local definitions of protective factors can be discovered and leveraged (Allen et al., 2009; Allen et al., 2006; Teufel-Shone et al., 2014). Additionally, given the importance of cultural protective factors to AIAN adolescent health (Allen et al., 2006; LaFromboise et al., 2006; Mmari et al., 2010; Pharris et al., 1997; Pu et al., 2013; Whitbeck et al., 2001), the need to support and invest in AIAN culture preservation and revitalization efforts are critical to ensure AIAN adolescents have access to uniquely tailored protective factors only their cultures can provide.
Study Limitations
This literature review focused only on the protective factors found to have a statistically significant association with the health and/or social outcome of interest or those that were discussed as protective within the two qualitative studies reviewed. Therefore, we may have under-represented the array of protective factors potentially associated with AIAN adolescent health. While we made efforts to thoroughly search the available literature regarding protective factors affecting AIAN adolescents, publications may have been missed. As suggested by Mackin et al. (2012), additional protective factors likely exist but have not been measured in the research studies reviewed here.
Additionally, not all the quantitative studies included in this review reported the statistical values of the results for the protective factors that are identified by the researchers to be statistically significant. In such cases, we included the protective factors as identified by the original study author in good faith.
Recommendations for Future Research
Protective factors influence positive health and social outcomes of AIAN adolescents. Even when exposed to trauma or high-risk environments, protective factors provide sources of support and motivation for adolescents (Allen et al., 2006; Borowsky et al., 1999; Cummins et al., 1999; LaFromboise et al., 2006). Continued research in this area is paramount, as is the creation of better tools for identifying and measuring cultural protective factors and incorporating AIANs’ views of their own assets, protective factors, and desirable health outcomes. Research should also address the rapid development and behavioral and cognitive differences across the continuum of adolescent age range (AAP, 2003; APA, 2002); considering the distinct social influences on younger and older adolescents would enhance future exploration of adolescent assets and protective factors.
Create tools to better identify and measure culturally centered protective factors
Cultural protective factors are identified across multiple domains of the social-ecological model. As Pavkov, Travis, Fox, and Bear King (2010) state, “traditional (AIAN) culture, when allowed to flower, provides an informal, flexible, strength-based, prevention oriented system with long-standing traditions” (p. 132). However, many researchers have noted the challenging nature of identifying and measuring culture and cultural protective factors (Allen et al., 2006; LaFromboise et al., 2006; Mohatt et al., 2011; Whitbeck et al., 2001; Whitesell et al., 2014). Culture is complex and difficult to measure using standard, one-dimensional measurement tools (Whitbeck et al., 2001). Currently, social science lacks culturally congruent measurement tools to identify and measure protective factors and positive outcomes within the AIAN population (LaFromboise et al., 2006; Whitbeck et al., 2001). As a result researchers may use tools to measure cultural factors that are not relevant to a particular AIAN population (LaFromboise et al., 2006; Whitbeck et al., 2001). Measuring cultural protective factors within the adolescent population can be particularly problematic as adolescents may be in the initial stages of forming a cultural identity (Whitesell et al., 2014).
Create opportunity for AIANs to identify protective factors and desirable health outcomes
Many of studies reviewed here are cross sectional and quantitative in design and used standardized questionnaires with predetermined variables or measurement scales. Qualitative research methods where participants identified any adolescent protective factors they felt were relevant and effective were only applied in two of the studies reviewed (Allen et al., 2006; Mmari et al., 2010). In only a few cases did the research team engage AIAN community members to adapt or create standardized instruments (LaFromboise et al., 2006; Whitbeck et al., 2001; Yu & Stiffman, 2010). Future research studies should engage AIANs in order for them to self-identify the protective factors for themselves and their communities (Allen et al., 2006; Stiffman et al., 2007). In using this approach, the protective factors identified will be contextually and culturally appropriate to the target population and better suited for guiding intervention efforts as compared to protective factors identified by academic researchers alone (Allen et al., 2006). Additionally, future intervention goals should align with local AIAN community definitions of wellness and health (Mohatt et al., 2011; Whitbeck et al., 2001).
Conclusion
Protective factors, located throughout the domains of the social-ecological model, are associated with a breadth of positive health and social outcomes in AIAN adolescents. Identifying and utilizing local, innate protective factors in health promotion ensures such efforts will be relevant and culturally congruent to the target population. Leveraging local protective factors also promotes an asset-based approach rather than focusing on deficits alone. Formative research with AIAN adults and adolescents is needed to identify protective factors that may exist but are not currently being measured with existing standardized instruments. AIANs should be integrally involved in identifying protective factors as a means towards reducing health disparities within the AIAN population.
Acknowledgments
Research reported in this publication was supported by the National Institute on Minority Health And Health Disparities of the National Institutes of Health under Award Number P20MD006872.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Special thanks to Beth Kaeding and to the Center for American Indian Resilience team.
Footnotes
Conflict of Interest
The authors have no conflicts of interest to report. This research did not involve human subjects or animals.
Contributor Information
Michele Henson, Center for American Indian Resilience, Department of Health Promotion Sciences, Zuckerman College of Public Health, University of Arizona College of Public Health, 1295 N Martin Ave, Tucson, AZ 85724, Phone: 406-381-1044, Fax: 520-626-3206.
Samantha Sabo, Assistant Professor, Department of Health Promotion Sciences, Zuckerman College of Public Health, University of Arizona College of Public Health, 1295 N Martin Ave, Tucson, AZ 85724.
Aurora Trujillo, Native Nations Institute, 803 E 1st Street Tucson, AZ 85719.
Nicolette Teufel-Shone, Professor, Center for American Indian Resilience, Department of Health Promotion Sciences, Zuckerman College of Public Health, University of Arizona College of Public Health, 1295 N Martin Ave, Tucson, AZ 85724.
References
*References include in the literature review.
- Allen J, Mohatt G, Fok C, Henry D, People Awakening Team Suicide prevention as a community development process: Understanding circumpolar youth suicide prevention through community level outcomes. International Journal of Circumpolar Health. 2009;68(3):274–291. doi: 10.3402/ijch.v68i3.18328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Allen J, Mohatt G, Rasmus M, Hazel K, Thomas L, Lindley S. The Tools to Understand: Community as co-researcher on culture-specific protective factors for Alaska Natives. Journal of Prevention & Intervention in the Community. 2006;32(1–2):41–59. doi: 10.1300/j005v32n01_04. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics (AAP) Caring For Your Teenager. American Academy of Pediatrics. 2003 Retrieved from http://www.healthychildren.org/English/ages-stages/teen/Pages/Stages-of-Adolescence.aspx.
- American Psychological Association (APA) United States Department of Health and Human Services. Washington, DC: 2002. A Reference for Professionals: Developing Adolescents; pp. 20002–4242. [Google Scholar]
- *.Barney D. Risk and protective factors for depression and health outcomes in American Indian and Alaska Native adolescents. Wicazo Sa Review. 2001;16(1):135–150. [Google Scholar]
- *.Bearinger L, Pettingell S, Resnick M, Potthoff S. Reducing weapon-carrying among urban American Indian young people. Journal of Adolescent Health. 2010;47(2010):43–50. doi: 10.1016/j.jadohealth.2009.12.033. [DOI] [PubMed] [Google Scholar]
- *.Bearinger L, Pettingell S, Resnick M, Skay C, Potthoff S, Eichhorn J. Violence perpetration among American Indian youth. Archives of Pediatrics and Adolescent Medicine. 2005;159:270–277. doi: 10.1001/archpedi.159.3.270. [DOI] [PubMed] [Google Scholar]
- *.Borowsky I, Resnick M, Ireland M, Blum R. Suicide attempts among American Indian and Alaska Native youth: Risk and protective factors. Archives of Pediatrics and Adolescent Medicine. 1999;153:573–580. doi: 10.1001/archpedi.153.6.573. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) The Social-Ecological Model: A framework for prevention. The Centers for Disease Control and Prevention. 2015b Retrieved from http://www.cdc.gov/violenceprevention/overview/social-ecologicalmodel.html.
- Centers for Disease Control and Prevention (CDC) Why schools? Schools: The right place for a healthy start. The Centers for Disease Control and Prevention. 2015a Retrieved from http://www.cdc.gov/healthyyouth/about/why_schools.htm.
- *.Cummins J, Ireland M, Resnick M, Blum R. Correlates of physical and emotional health among Native American adolescents. Journal of Adolescent Health. 1999;24(1):38–44. doi: 10.1016/s1054-139x(98)00063-9. [DOI] [PubMed] [Google Scholar]
- Goodkind J, LaNoue M, Lee C, Freeland L, Freund R. Feasibility, acceptability, and initial finding for a community-based cultural mental health intervention for American Indian youth and their families. Journal of Community Psychology. 2012;40(4):381–405. doi: 10.1002/jcop.20517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guba EG. Toward a methodology of naturalistic inquiry in educational evaluation. Los Angeles, CA: University of California Center for the Study of Evaluation; 1978. [Google Scholar]
- Hawkins E, Cummins L, Marlatt G. Preventing substance abuse in American Indian and Alaska Native youth: Promising strategies for healthier communities. Psychological Bulletin. 2004;130(2):304–323. doi: 10.1037/0033-2909.130.2.304. [DOI] [PubMed] [Google Scholar]
- Jain S, Cohen A. Fostering resilience among urban youth exposed to violence: A promising area for interdisciplinary research and practice. Health Education and Behaviors. 2013;40(6):651–662. doi: 10.1177/1090198113492761. [DOI] [PubMed] [Google Scholar]
- Jessor R, Turnbin M, Costa F. Risk and protection in successful outcomes among disadvantaged adolescents. Applied Developmental Science. 1998;2(4):194–208. [Google Scholar]
- *.LaFromboise T, Hoyt D, Oliver L, Whitbeck L. Family, community, and school influences on resilience among American Indian adolescents in the upper Midwest. Journal of Community Psychology. 2006;32(2):193–209. [Google Scholar]
- *.LeMaster P, Connel C, Mitchell C, Manson S. Tobacco use among American Indian adolescents: Protective and risk factors. Journal of Adolescent Health. 2002;30(6):426–432. doi: 10.1016/s1054-139x(01)00411-6. [DOI] [PubMed] [Google Scholar]
- Lowe J, Riggs C, Henson J, Leihr P. Cherokee self-reliance and word-use in stories of stress. Journal of Cultural Diversity. 2009;16(1):1–9. [PMC free article] [PubMed] [Google Scholar]
- *.Mackin J, Perkins T, Furrer C. The power of protection: A population-based comparison of Native and non-Native youth suicide attempts. American Indian & Alaska Native Mental Health Research. 2012;19(2):20–54. doi: 10.5820/aian.1902.2012.20. [DOI] [PubMed] [Google Scholar]
- Mohatt N, Fok C, Burket R, Henry D, Allen J. Assessment of awareness of connectedness as a culturally-based protective factor for Alaska Native youth. Cultural Diversity & Ethnic Minority Psychology. 2011;17(4):444–455. doi: 10.1037/a0025456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Mmari K, Blum R, Teufel-Shone N. What increases risk and protection for delinquent behaviors among American Indian youth? Findings from three tribal communities. Youth & Society. 2010;41(3):382–413. [Google Scholar]
- *.Moilanen K, Markstrom C, Jones E. Extracurricular activity availability and participation and substance use among American Indian adolescents. Journal of Youth and Adolescence. 2014;2014(23):454–469. doi: 10.1007/s10964-013-0088-1. [DOI] [PubMed] [Google Scholar]
- *.Osilla K, Lonczak H, Mail P, Larimer M, Marlatt G. Regular tobacco use among American Indian and Alaska Native adolescents: An examination of protective mechanisms. Journal of Ethnicity in Substance Use. 2007;6(3–4):143–153. doi: 10.1300/J233v06n03_06. [DOI] [PubMed] [Google Scholar]
- Patton MQ. Qualitative research & evaluation methods. Thousand Oaks, CA: Sage Publications, Inc; 2002. [Google Scholar]
- Pavkov T, Travis L, Fox K, Bear King C, Cross T. Tribal youth victimization and delinquency: Analysis of youth risk behavior surveillance survey data. Cultural Diversity and Ethnic Minority Psychology. 2010;16(2):123–134. doi: 10.1037/a0018664. [DOI] [PubMed] [Google Scholar]
- *.Pettingell S, Bearinger L, Skay C, Resnick M, Potthoff S, Eichhorn J. Protecting urban American Indian young people from suicide. American Journal of Health Behavior. 2008;32(5):465–476. doi: 10.5555/ajhb.2008.32.5.465. [DOI] [PubMed] [Google Scholar]
- *.Pharris M, Resnick M, Blum R. Protecting against hopelessness and suicidality in sexually abused American Indian adolescents. Journal of Adolescent Health. 1997;2:400–406. doi: 10.1016/S1054-139X(97)00166-3. [DOI] [PubMed] [Google Scholar]
- *.Pu J, Chewing B, St Clair I, Kokotailo P, Lacourt J, Wilson D. Protective factors in American Indian communities and adolescent violence. Journal of Maternal and Child Health. 2013;17:1199–1207. doi: 10.1007/s10995-012-1111-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabalauskas K, Ortolani C, McCall M. Moving from pathology to possibility: Integrating strengths-based interventions in child welfare provision. Child Care in Practice. 2014;20(1):120–134. [Google Scholar]
- Stiffman A, Brown E, Freedenthal S, House L, Ostmann E, Soo Yu M. American Indian youth: Personal, familial and environmental strengths. Journal of Child and Family Studies. 2007;16:331–346. [Google Scholar]
- Teufel-Shone N, Gamber M, Watahomigie H, Siyuja T, Crozier L, Irwin S. Using a participatory research approach in a school-based physical activity intervention to prevent diabetes in the Hualapai Indian community, Arizona, 2002–2006. Preventing Chronic Disease. 2014;11(E166):1–11. doi: 10.5888/pcd11.130397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Whitbeck L, Hoyt D, Stubben J, LaFromboise T. Traditional culture and academic success among American Indian children in the upper Midwest. Journal of America Indian Education. 2001;40(2):48–60. [Google Scholar]
- Whitbeck L, Walls M, Welch M. Substance abuse prevention in American Indian and Alaska Native communities. The American Journal of Drug and Alcohol Abuse. 2012;38(5):428–435. doi: 10.3109/00952990.2012.695416. [DOI] [PubMed] [Google Scholar]
- *.Whitesell N, Asdigian N, Kaufman C, Big Crow C, Shangreau C, Keane E, Mousseau A, Mitchell C. Trajectories of substance use among young American Indian adolescents: Patterns and predictors. Journal of Adolescent Health. 2014;43:437–453. doi: 10.1007/s10964-013-0026-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitesell N, Mitchell C, Spicer P, the Voices of Indian Teens Project Team A longitudinal study of self-esteem, cultural identity, and academic success among American Indian adolescents. Cultural Diversity and Ethnic Minority Psychology. 2009;15(1):38–50. doi: 10.1037/a0013456.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) Adolescent health. World Health Organization. 2015 Retrieved from www.who.int.topics/adolescent_health/en/
- *.Yu M, Stiffman A. Positive family relationships and religious affiliation as mediators between negative environment and illicit drug symptoms in American Indian Adolescents. Addictive Behaviors. 2010;35(2010):694–699. doi: 10.1016/j.addbeh.2010.03.005. [DOI] [PubMed] [Google Scholar]


