Abstract
The cervix is a cylindrical structure that is proximally connected to the uterus and distally to the vaginal cavity. The Bishop score has been used to evaluate the cervix during pregnancy. However, alternatives have been evaluated because the Bishop score is uncomfortable for patients, relies on a subjective examination, and lacks internal os data. Elastography has been used to assess the cervix, as it can estimate tissue stiffness. Recent articles on elastography for cervical assessment during pregnancy have focused on its usefulness for prediction of preterm birth and successful labor induction. There is a clinical need for cervical elastography, as an evaluation of biomechanical factors, because cervical length only assesses morphological changes. However, until now, cervical elastography has been studied in the limited field, and not shown a uniformed methodological technique. In this review, the current status, limitations, and future possibility of cervical elastography were discussed. Future studies should focus on overcoming the limitations of cervical elastography. Although the cervical elastography is presently an incompletely defined technique, it needs to be improved and evaluated as a method for use in combination with cervical length.
Keywords: Cervix uteri, Elastography, Labor induction, Premature birth
Introduction
The cervix is a cylindrical structure that is proximally connected to the uterus and distally to the vaginal cavity. The cervix is composed of fibrous connective tissue and the uterus is composed mainly of smooth muscle, and they are therefore distinct organs [1]. The cervix can change significantly over a short time period. It is a closed, firm structure during early pregnancy, and undergoes softening later in pregnancy. Cervical effacement and dilatation are active, dynamic processes, and adequate effacement allows passage of the fetus and enables successful delivery [2]. Cervical integrity is essential in pregnancy. Preterm cervical dilatation may predict preterm delivery. On the other hand, a cervix that remains firm after term may increase induction or cesarean section rates [3].
Traditionally, the Bishop score has been used to evaluate the cervix during pregnancy. It assesses cervical status based on dilatation, effacement, consistency, fetal head station, and position [4]. However, alternatives have been evaluated because the Bishop score is uncomfortable for patients, relies on a subjective examination, and lacks internal os data. Cervical elastography is one of the alternatives. Elastography was first introduced about 20 years ago as an adjunct to routine sonography [5]. Since then, elastography has been used for the diagnosis and characterization of various tumors or cancers in the breast, prostate, and thyroid gland [6,7]. Recently, elastography has been used to assess the cervix, as it can estimate tissue stiffness. This article reviews the use of elastography to assess the cervix during pregnancy, in order to clarify its current status, limitations, and need for further research.
Elastography
Initially described more than 20 years ago, elastography has emerged as an important adjunct to sonography [5]. Elastography is able to image firm lesions in the prostate and other organs as dark areas against a green background of movable tissue [8,9]. Elastography is a noninvasive method in which images of soft tissue stiffness are used to detect or classify masses. It is reportedly useful for the diagnosis and characterization of breast cancer, prostate cancer, and thyroid nodules, which are usually stiffer than normal tissues [7].
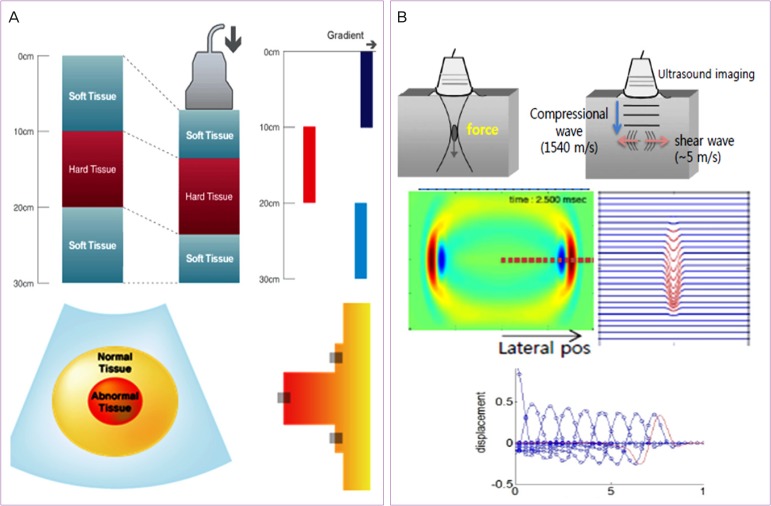
The technique is classified according to the principles of strain elastography and shear wave elastography, depending on whether the impulse source is generated by external pressure or by internal artificial force (Fig. 1) [10,11]. Strain elastography provides images that describe the extent of tissue deformation under external impulse pressure. An external impulse is generated by manual compression using a sonography probe, or by patient respirations or arterial pulsations. Strain elastography measures tissue displacement in a very short time interval. A large displacement is characteristic of soft tissue, and small displacement characterizes hard tissue. The result is visualized in color. However, strain elastography is unable to determine the absolute value of tissue stiffness. In many studies, the target value obtained in a specific tissue and the ratio of the target value to normal tissue were quantified. In contrast, shear wave elastography uses an ultrasonic wave to generate an impulse. This artificial impulse propagates a transverse wave (shear wave) through the tissue. When this wave passes through the tissue, the velocity of the wave varies with tissue stiffness, which enables measurement of tissue stiffness. Although shear wave elastography can acquire data regardless of examiner experience, there is no standardized technique for clinical use.
Fig. 1. Principles of (A) strain elastography and (B) shear wave elastography. (A) The displacement of a hard area is less than that of a soft area. Gradient values of the displacement of hard areas are also less than those for soft areas. Strain elastography shows the gradient values of displacement on a color map. Reproduced from Samsung Medison. ElastoScan enables the imaging of malignant tumors and other diseases that would normally be undetectable through conventional studies [Internet]. Seoul: Samsung Medison; c2011. Available from: http://www.samsungmedison.com/technology/elastoscan.jsp, with permission from Samsung Medison [10]. (B) If the intensity of the wave created by ultrasound energy is high enough, and the duration of the pulse long enough, the impulse pressure on the tissue will be large enough to cause a small local displacement of the tissue. This transverse displacement is a shear wave. Since the shear wave speed in soft tissue travels a thousand times faster than in hard tissue, ultrasound imaging can be used to monitor the propagation of the shear wave and measure its speed. Reproduced from Shin DK. Principles of ultrasound elastography. In: Korean Society of Ultrasound in Obstetrics and Gynecology. Korean Society of Ultrasound in Obstetrics and Gynecology workshop; 2015 Oct 24; Seoul, Korea. Seoul: Korean Society of Ultrasound in Obstetrics and Gynecology, with permission from Samsung Medison [11]. pos, position.
Current use of cervical elastography
The uterine cervix has no reference tissue, i.e., the cervix is its own reference tissue. Thus, strain elastography is limited, because it evaluates stiffness without use of a reference tissue. Shear wave elastography is affected by how firmly the probe pushes against the cervix, by where the impulse should be generated, and by whether it is safe for a pregnant women and the fetus. Until now, strain elastography has been primarily used to assess the pregnant cervix. Some studies evaluated shear wave elastography [12,13]. Most elastography studies have focused on the prediction of successful labor induction and preterm birth using data measured in mid-pregnancy.
1. Strain elastography for prediction of successful induction of labor
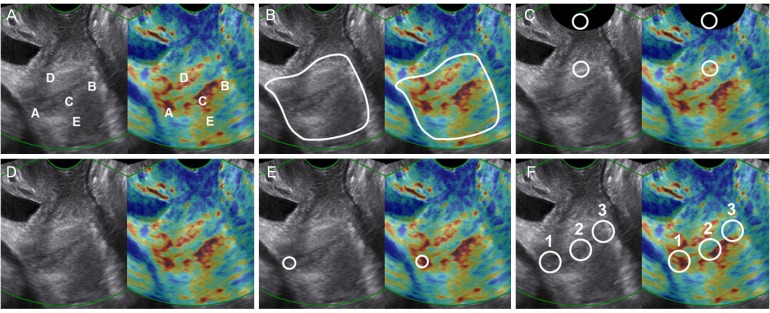
Labor induction is performed in 15% to 20% of pregnant women. There are many reasons for labor induction: prolonged pregnancy, hypertensive disorders, large for gestational age, and oligohydramnios. Clinicians who want to predict the result of labor induction can use the digital pelvic examination or cervical length. However, this information is unsatisfactory for prediction of successful labor induction. Six articles published in 2011 to 2015 assessed the uterine cervix with strain elastography to predict successful labor induction (Table 1) [14,15,16,17,18,19]. These articles had relatively small patient numbers, and the region of interest (ROI) was varied widely (Fig. 2). Numerous objective methods have been used to evaluate stiffness. Hee et al. [16] used a reference cap to overcome the shortcomings of strain elastography, but this method only analyzes a small ROI.
Table 1. Characteristics of studies using strain elastography to evaluate the uterine cervix prior to labor induction.
| Author (year) | Patients no. | Nulli-parous | Gestational age at scan | Method of labor induction | Success of labor induction | ROI | Scoring system | Compression of cervix | Reference materials | Software |
|---|---|---|---|---|---|---|---|---|---|---|
| Swiatkowska-Freund et al. (2011)a) [14] | 29 | 0 (0–1) 0 (0–3) |
40 (33–42) 38 (36–41) |
Oxytocin | Uterine contraction and labor progress within 9 hours | No | Subjective color scoring for 5 cervical points | No | No | ElastoScan (Samsumg Medison, Korea) |
| Hwang et al. (2013) [15] | 145 | 100% | 41 (37–42) | Oxytocin, amniotomy | Onset of active labor within 9 hours or delivery within 24 hours after labor induction | Single area (whole uterine cervix) | Objective imaging analysis for entire cervix | No | No | ElastoScan (Samsung Medison, Korea) |
| Hee et al. (2014) [16] | 48 | 54% | 40 (1.3) | Oral misoprostol, amniotomy | The cervical dilation time from 4 to 10 cm | 2 Circles (4–6 mm) | Objective strain ratio for 2 circles | Compression and decompression | Cap (silicone:oil = 45:55) | Volusion E8 (GE, Austria) |
| Muscatello et al. (2014) [17] | 53 | 62% | 32 (21–44) | Prostaglandin | Vaginal delivery | No | Subjective color scoring for entire cervix | No | No | ElastoScan (Samsung Medison, Korea) |
| Pereira et al. (2014)a) [18] | 99 | 93.9% 62.1% |
41 (39–42) 41 (39–42) |
Dinoprostone, amniotomy, oxytocin | Vaginal delivery | Small single circle (internal os at sagittal plain) | Subjective color scoring for internal os | No | No | ElastoScan (Samsung Medison, Korea) |
| Wozniak et al. (2015) [19] | 39 | 61.50% | 40 (36–42) | Foley catheter (18F) | Regular uterine contractions ( ≥ 3 in 10 min) within 24 hours | 3 Circles (internal os, middle, external os) | Subjective color scoring for 3 circles | No | No | ElastoScan (Samsung Medison, Korea) |
Data are presented as median (minimum–maximum) unless otherwise indicated.
ROI, region of interest.
a)Upper data: failed labor induction group, lower data: successful labor induction group.
Fig. 2. Color map strain elastography and variable region of interest (ROI) in studies of prediction of successful induction of labor. Dual images of the uterine cervix on gray scale sonography and color map elastography showing different ROIs: (A) five-point ROI, (B) whole cervix ROI, (C) small, circular ROI with reference area, (D) subjective scoring without ROI, (E) small, single ROI of internal os, and (F) three small ROIs for the cervical canal.
2. Strain elastography for prediction of preterm delivery
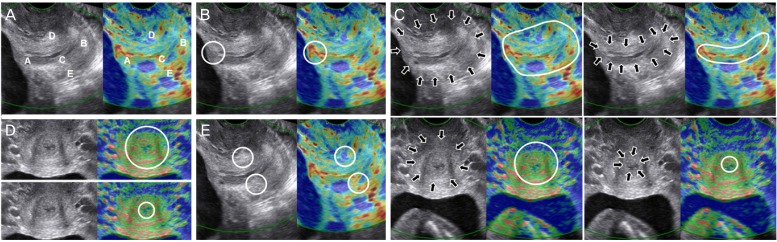
Prediction of spontaneous preterm birth remains difficult. Preterm labor, preterm premature rupture of membranes, or an incompetent internal cervical os can cause spontaneous preterm birth. The predictive value of digital pelvic examination in mid-pregnancy or sonographic cervical length is low. Not only to predict preterm birth, but also to decide when to give progesterone to women at risk for preterm birth, a more precise predictive model is needed. Several studies have investigated the predictability of preterm birth using cervical elastography in mid-pregnancy. Table 2 summarizes 5 recent articles that assessed the use of strain elastography of the cervix to predict spontaneous preterm birth [20,21,22,23,24]. These studies evaluated a larger area than that used in labor induction, by analyzing several ROIs (Fig. 3). However, they used different methods with or without compression of the cervix, the number of patients was small, and data were obtained for low-risk pregnant women.
Table 2. Characteristics of studies using strain elastography of the uterine cervix to predict risk of spontaneous preterm birth.
| Author (year) | Patients number | Nulli-parous | Gestational age at scan | Preterm birth | Enrolled patients' inclusion criteria | ROI | Scoring system | Compression of cervix | Software |
|---|---|---|---|---|---|---|---|---|---|
| Swiatkowska-Freund et al. (2014) [20] | 44 | 61.40% | 22 to 36 | 21 (47.7) | Women admitted to the hospital with threatened preterm labor | 5 Circles (5 mm) | Subjective color scoring for 5 circles | No | ElastoScan (Samsung Medison, Korea |
| Wozniak et al. (2014) [21] | 337 | NA | 18+0 to 22+6 | 35 (10.4) | Low risk, singleton, cervical length ≥ 25 mm | Small single circle (internal os at sagittal plain) | Subjective color scoring for internal os | No | ElastoScan (Samsung Medison, Korea |
| Hernandez-Andrade et al. (2014) [22] | 189 | 42% | 16 to 24 | 21 (11.1) | Low risk, singleton | 4 Areas (2 midsagittal and 2 cross-sectional) | Mean strain percentage of displacement or deformation | Oscillatory pressure | Hitachi, HI Vision 900 (Hitachi, Japan) |
| Hernandez-Andrade et al. (2015) [23] | 545 | 39% | 11 to 28 | 45 (8.2) | Singleton regardless of short cervix or previous preterm birth | Single area (internal os at cross-sectional plain) | Mean strain quartiles | Oscillatory pressure | Hitachi, HI Vision 900 (Hitachi, Japan) |
| Sabiani et al. (2015) [24] | 72 | 36.10% | First, second, third trimester | 9 (12.5) | Low risk, singleton | 2 Circles (middle anterior and posterior lip) | Subjective color scoring for 2 circles, and its ratio | No | Hitachi, HI Vision (Hitachi, Gerrmany) |
Data are presented as gestational age at scan (weeks) or number (%) unless otherwise indicated.
ROI, region of interest; NA, not available.
Fig. 3. Color map strain elastography and variable region of interest (ROI) in studies of prediction of preterm delivery. Dual images of the uterine cervix on gray scale sonography and color map elastography showing different ROIs: (A) five-point ROI, (B) small, single ROI of internal os, (C) four ROIs with two midsagittal and two cross-sectional areas, (D) single ROI of internal os in cross-sectional plain, and (E) two circular ROIs on middle anterior and posterior cervical lips.
Limitations and challenges in cervical elastography
Thus far, cervical strain elastography alone has been studied in pregnancy. Various ROIs, scoring systems, and compression methods reveal the limitations of cervical elastography studies, but also hint at ways to overcome these limitations.
1. Limitations of cervical elastography
The limitations of cervical elastography in the studies presented are as follows. First, unlike other organs, there is no distinction between a reference tissue and the target tissue in the uterine cervix. A strain ratio for normal and target tissue cannot be acquired. Second, there are multiple pressure sources. Because the elastographic image is made by an external pressure, the uniformed pressure is needed for the stable elastographic image. However, the uterine cervix of pregnant women is affected by several pressure sources, such as patient's respirations, arterial pulsations, fetal movements, and shaking hands of the operator. When there are several vibration sources, it is difficult to determine which images represent cervical stiffness. Shear wave elastography values are also affected by the impulse target.
2. Region of interest and image calculation
Existing studies have shown the difficulty of determining the ROI in elastographic color images. If the ROI is too wide, the color in the inner region varies, which make it difficult to establish a representative color. Conversely, if the ROI is too narrow, although it is easier to establish a representative color value, the smaller ROI does not represent the entire cervix (Fig. 2E, F). When the ROI is set as the circle of the internal os, which is clinically and empirically important, the endocervical canal at the internal os is relatively soft, and should be excluded in determining cervix stiffness. This is methodologically difficult. It is reasonable to include the entire cervix as the ROI, rather than using a small ROI to assess uterine cervical stiffness. Several methods to assess the stiffness of the ROI have been proposed. One uses a scoring system with the ROI as a color map (Fig. 2A, C, E, F). Another uses an image analysis system to evaluate pixel colors in ROI images of various shapes. The third uses a strain data analysis system that directly analyzes raw data from the ROI (Fig. 2C, D).
The shape of the uterine cervix varies in pregnancy. A cervix greater than 3 to 4 cm is relatively long, and may have a straight, anteverted, or sometimes retroverted endocervical canal. It is difficult to assess cervical stiffness with present methods if the uterine cervix is short. To assess various cervical shapes and sizes, various ROIs should be used. Moreover, to develop a scoring system that can provide consistent stiffness data for various ROIs, it is important to use strain data for the cervix itself in the analysis.
3. Cervical length and cervical elastography
Because the positive predictive value for preterm birth using the routine cervical length examination is low, clinical guidelines do not recommend checking cervical length in low-risk pregnant women during the mid-trimester. Researches on the usefulness of universal cervical length examination for prevention of preterm birth in low-risk pregnant women have recently been published [25,26]. Past studies have reported the use of cervical elastography alone in the prediction of preterm birth. Because of the characteristics of the cervix, combining the two methods of cervical elastography and determination of cervical length might be more effective in predicting preterm birth than the use of either method alone.
Conclusion
Elastography has been used in various fields as an adjunct to 2-dimensional gray scale ultrasonography, and has been extensively studied. Elastography has been increasingly used in the assessment of liver and breast disease. Guidelines for elastography from the Japanese Society of Ultrasound in Medicine [27,28], the European Federation of Societies for Ultrasound in Medicine and Biology [29], and the World Federation for Ultrasound in Medicine and Biology have been published [30]. However, guidelines for cervical elastography are currently not available.
The clinical importance of assessing the uterine cervix during pregnancy is obvious. It is well known that the cervix undergoes biochemical changes in advance of morphological change during pregnancy. Thus, there is clearly a clinical need for cervical elastography in the evaluation of biochemical factors in combination with cervical length, which only assesses morphological changes. Future studies should focus on overcoming the limitations of cervical elastography. Although cervical elastography has some limitations, improved technique and the combination with measurement of cervical length will make it possible to assess the uterine cervix of pregnant women more precisely.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Danforth DN. The morphology of the human cervix. Clin Obstet Gynecol. 1983;26:7–13. doi: 10.1097/00003081-198303000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Timmons B, Akins M, Mahendroo M. Cervical remodeling during pregnancy and parturition. Trends Endocrinol Metab. 2010;21:353–361. doi: 10.1016/j.tem.2010.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.House M, Kaplan DL, Socrate S. Relationships between mechanical properties and extracellular matrix constituents of the cervical stroma during pregnancy. Semin Perinatol. 2009;33:300–307. doi: 10.1053/j.semperi.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crane JM. Factors predicting labor induction success: a critical analysis. Clin Obstet Gynecol. 2006;49:573–584. doi: 10.1097/00003081-200609000-00017. [DOI] [PubMed] [Google Scholar]
- 5.Wilson LS, Robinson DE. Ultrasonic measurement of small displacements and deformations of tissue. Ultrason Imaging. 1982;4:71–82. doi: 10.1177/016173468200400105. [DOI] [PubMed] [Google Scholar]
- 6.Ginat DT, Destounis SV, Barr RG, Castaneda B, Strang JG, Rubens DJ. US elastography of breast and prostate lesions. Radiographics. 2009;29:2007–2016. doi: 10.1148/rg.297095058. [DOI] [PubMed] [Google Scholar]
- 7.Lim DJ, Luo S, Kim MH, Ko SH, Kim Y. Interobserver agreement and intraobserver reproducibility in thyroid ultrasound elastography. AJR Am J Roentgenol. 2012;198:896–901. doi: 10.2214/AJR.11.7009. [DOI] [PubMed] [Google Scholar]
- 8.Lerner RM, Parker KJ, Holen J, Gramiak R, Waag RC. Sono-elasticity: medical elasticity images derived from ultrasound signals in mechanically vibrated targets. Acoust Imaging. 1988;16:317–327. [Google Scholar]
- 9.Parker KJ, Huang SR, Musulin RA, Lerner RM. Tissue response to mechanical vibrations for “sonoelasticity imaging”. Ultrasound Med Biol. 1990;16:241–246. doi: 10.1016/0301-5629(90)90003-u. [DOI] [PubMed] [Google Scholar]
- 10.Samsung Medison. ElastoScan enables the imaging of malignant tumors and other diseases that would normally be undetectable through conventional studies [Internet] Seoul: Samsung Medison; c2011. [cited 2016 Dec 1]. Available from: http://www.samsungmedison.com/technology/elastoscan.jsp. [Google Scholar]
- 11.Shin DK. Principles of ultrasound elastography; Korean Society of Ultrasound in Obstetrics and Gynecology. Korean Society of Ultrasound in Obstetrics and Gynecology workshop; 2015 Oct 24; Seoul, Korea. Seoul: Korean Society of Ultrasound in Obstetrics and Gynecology; [Google Scholar]
- 12.Hernandez-Andrade E, Aurioles-Garibay A, Garcia M, Korzeniewski SJ, Schwartz AG, Ahn H, et al. Effect of depth on shear-wave elastography estimated in the internal and external cervical os during pregnancy. J Perinat Med. 2014;42:549–557. doi: 10.1515/jpm-2014-0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Muller M, Ait-Belkacem D, Hessabi M, Gennisson JL, Grange G, Goffinet F, et al. Assessment of the cervix in pregnant women using shear wave elastography: a feasibility study. Ultrasound Med Biol. 2015;41:2789–2797. doi: 10.1016/j.ultrasmedbio.2015.06.020. [DOI] [PubMed] [Google Scholar]
- 14.Swiatkowska-Freund M, Preis K. Elastography of the uterine cervix: implications for success of induction of labor. Ultrasound Obstet Gynecol. 2011;38:52–56. doi: 10.1002/uog.9021. [DOI] [PubMed] [Google Scholar]
- 15.Hwang HS, Sohn IS, Kwon HS. Imaging analysis of cervical elastography for prediction of successful induction of labor at term. J Ultrasound Med. 2013;32:937–946. doi: 10.7863/ultra.32.6.937. [DOI] [PubMed] [Google Scholar]
- 16.Hee L, Rasmussen CK, Schlutter JM, Sandager P, Uldbjerg N. Quantitative sonoelastography of the uterine cervix prior to induction of labor as a predictor of cervical dilation time. Acta Obstet Gynecol Scand. 2014;93:684–690. doi: 10.1111/aogs.12389. [DOI] [PubMed] [Google Scholar]
- 17.Muscatello A, Di Nicola M, Accurti V, Mastrocola N, Franchi V, Colagrande I, et al. Sonoelastography as method for preliminary evaluation of uterine cervix to predict success of induction of labor. Fetal Diagn Ther. 2014;35:57–61. doi: 10.1159/000355084. [DOI] [PubMed] [Google Scholar]
- 18.Pereira S, Frick AP, Poon LC, Zamprakou A, Nicolaides KH. Successful induction of labor: prediction by preinduction cervical length, angle of progression and cervical elastography. Ultrasound Obstet Gynecol. 2014;44:468–475. doi: 10.1002/uog.13411. [DOI] [PubMed] [Google Scholar]
- 19.Wozniak S, Czuczwar P, Szkodziak P, Paszkowski T. Usefulness of elastography in predicting the outcome of Foley catheter labour induction. Aust N Z J Obstet Gynaecol. 2015;55:245–250. doi: 10.1111/ajo.12331. [DOI] [PubMed] [Google Scholar]
- 20.Swiatkowska-Freund M, Traczyk-Los A, Preis K, Lukaszuk M, Zielinska K. Prognostic value of elastography in predicting premature delivery. Ginekol Pol. 2014;85:204–207. doi: 10.17772/gp/1714. [DOI] [PubMed] [Google Scholar]
- 21.Wozniak S, Czuczwar P, Szkodziak P, Milart P, Wozniakowska E, Paszkowski T. Elastography in predicting preterm delivery in asymptomatic, low-risk women: a prospective observational study. BMC Pregnancy Childbirth. 2014;14:238. doi: 10.1186/1471-2393-14-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hernandez-Andrade E, Romero R, Korzeniewski SJ, Ahn H, Aurioles-Garibay A, Garcia M, et al. Cervical strain determined by ultrasound elastography and its association with spontaneous preterm delivery. J Perinat Med. 2014;42:159–169. doi: 10.1515/jpm-2013-0277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hernandez-Andrade E, Garcia M, Ahn H, Korzeniewski SJ, Saker H, Yeo L, et al. Strain at the internal cervical os assessed with quasi-static elastography is associated with the risk of spontaneous preterm delivery at ≤34 weeks of gestation. J Perinat Med. 2015;43:657–666. doi: 10.1515/jpm-2014-0382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sabiani L, Haumonte JB, Loundou A, Caro AS, Brunet J, Cocallemen JF, et al. Cervical HI-RTE elastography and pregnancy outcome: a prospective study. Eur J Obstet Gynecol Reprod Biol. 2015;186:80–84. doi: 10.1016/j.ejogrb.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 25.Son M, Grobman WA, Ayala NK, Miller ES. A universal mid-trimester transvaginal cervical length screening program and its associated reduced preterm birth rate. Am J Obstet Gynecol. 2016;214:365.e1–365.e5. doi: 10.1016/j.ajog.2015.12.020. [DOI] [PubMed] [Google Scholar]
- 26.Orzechowski KM, Boelig RC, Baxter JK, Berghella V. A universal transvaginal cervical length screening program for preterm birth prevention. Obstet Gynecol. 2014;124:520–525. doi: 10.1097/AOG.0000000000000428. [DOI] [PubMed] [Google Scholar]
- 27.Nakashima K, Shiina T, Sakurai M, Enokido K, Endo T, Tsunoda H, et al. JSUM ultrasound elastography practice guidelines: breast. J Med Ultrason. 2013;40:359–391. doi: 10.1007/s10396-013-0457-0. [DOI] [PubMed] [Google Scholar]
- 28.Kudo M, Shiina T, Moriyasu F, Iijima H, Tateishi R, Yada N, et al. JSUM ultrasound elastography practice guidelines: liver. J Med Ultrason. 2013;40:325–357. doi: 10.1007/s10396-013-0460-5. [DOI] [PubMed] [Google Scholar]
- 29.Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, et al. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: Clinical applications. Ultraschall Med. 2013;34:238–253. doi: 10.1055/s-0033-1335375. [DOI] [PubMed] [Google Scholar]
- 30.Barr RG, Nakashima K, Amy D, Cosgrove D, Farrokh A, Schafer F, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 2: breast. Ultrasound Med Biol. 2015;41:1148–1160. doi: 10.1016/j.ultrasmedbio.2015.03.008. [DOI] [PubMed] [Google Scholar]