Abstract
Pregnancy-related osteoporosis is a very rare condition characterized by the occurrence of fracture during pregnancy or the puerperium. Despite its relative rarity, it can be a dangerous condition that causes severe back pain, height loss and disability. Normal physiologic changes during pregnancy, genetic or racial difference, obstetrical history and obstetrical disease, such as preterm labor or pregnancy-induced hypertension, are presumed risk factors of pregnancy-related osteooporosis. However, exact etiology and pathogenesis are uncertain. The management and natural history are still poorly defined. Traditional medications for osteoporosis are calcium/vitamin D and bisphosphonate. Concerns with bisphosphonate include accumulation in bone and fetal exposure in subsequent pregnancies. The newly developed medication, teriparatide, has shown good results. We report six cases of pregnancy-related osteoporosis and spinal fracture with literature review.
Keywords: Fractures, compression, Osteoporosis, Pregnancy
Introduction
Osteoporosis is the most common bone disease in humans. It is characterized by low bone mass, deterioration of bone tissue and disruption of bone architecture, compromised bone strength and an increase in the risk of fracture [1]. The prevalence of osteoporosis is less than 2% in women younger than 50 years and only 1.2% between the ages of 20 and 40 years [2].
At the last period of pregnancy, calcium mobilization and bone resorption are increased and lactation imposes a further increase [3]. These changes could lead to osteoporosis and fracture in young women. Pregnancy-related osteoporosis is a very rare condition. Its exact prevalence, etiology and pathogenesis are unknown, and risk factors have not been identified, although heparin usage, thyrotoxicosis and genetic background have been suspected [4].
In this paper, we present six cases of pregnancy-related osteoporosis with a review of the relevant literature.
Case report
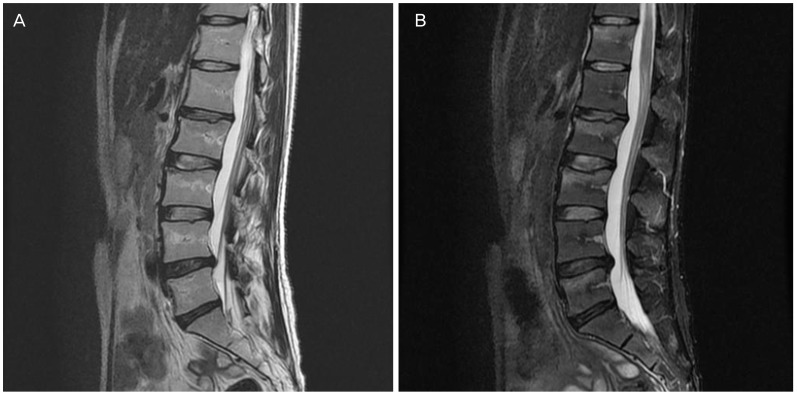
Six cases of pregnancy-related osteoporosis from January 2011 through December 2015 were identified in a medical record search at Pusan National University Hospital. Mean age of the patients was 33 years. All were women diagnosed as osteoporosis after their first delivery. The interval of delivery and hospital visit was 1 to 3 months. All patients showed vertebral fractures diagnosed mainly by magnetic resonance imaging (MRI) (Fig. 1).
Fig. 1. (A,B) Vertebral compression fractures in magnetic resonance imaging in case 3.
1. Case 1
A 31-year-old primiparous woman visited because of back pain. Three months earlier, she underwent vaginal delivery. She had breast-fed her baby after delivery. Her height was 162 cm and her weight was 57 kg. She had no past surgical or family histories, or trauma. On physical examination, she had diffuse back pain. Lumbar spine anteroposterior and lateral MRI revealed recent compression fractures of T12. Bone mineral density (BMD) using dual energy X-ray absorptiometry revealed markedly low T-scores for the lumbar vertebrae L1–L4, femoral neck and femoral total (Table 1). She was given calcium 500 mg daily and cholecalciferol 1,000 IU.
Table 1. Treatment and BMD changes.
| Pretreatment BMD Z-score |
Posttreatment BMD Z-score |
Z-score change | Pretreatment BMD T-score |
Posttreatment BMD T-score |
T-score change | Treatment modality and duration of treatment | ||
|---|---|---|---|---|---|---|---|---|
| Case 1 | L1–L4 | −2.6 | −2.4 | +0.2 | −2.5 | −2.4 | +0.1 | Calcium/vitamin D, 8 months |
| femur | −1.9 | −1.8 | +0.1 | −1.9 | −1.8 | +0.1 | ||
| Case 2 | L1–L4 | −1.9 | −1.0 | +0.9 | −1.3 | −1.0 | +0.3 | Teriparatide, 6 months |
| femur | 0 | −0.8 | −0.8 | −0.8 | −0.8 | 0 | ||
| Case 3 | L1–L4 | −2.6 | −2.4 | +0.2 | −2.9 | −2.4 | +0.5 | Calcium/vitamin D, 7 months |
| femur | −1.5 | −1.2 | +0.3 | −1.7 | −1.2 | +0.5 | ||
| Case 4 | L1–L4 | −2.5 | −1.8 | +0.7 | −1.5 | −1.8 | −0.3 | Calcium/vitamin D, 8 months |
| femur | −2.1 | −2.0 | +0.1 | −1.7 | −2.0 | −0.3 | ||
| Case 5 | L1–L4 | −2.7 | −1.0 | +1.7 | −2.5 | −1.0 | +1.5 | Teriparatide, 9 months |
| femur | −1.6 | −1.2 | +0.4 | −1.2 | −1.2 | 0 | ||
| Case 6 | L1–L4 | −1.9 | −1.8 | +0.1 | −1.7 | −1.8 | −0.1 | Calcium/vitamin D, 8 months |
| femur | −1.6 | −1.6 | 0 | −1.4 | −1.6 | −0.2 |
BMD, bone mineral density; femur, femur neck.
2. Case 2
A 33-year-old primiparous woman visited because of back and hip pain that had started 3 months previously ago, beginning 1 month after a vaginal delivery. She had breast-fed her baby after delivery. Her height was 169 cm and her weight was 62 kg. She had no past surgical or family histories. Lumbar spine MRI revealed recent compression fractures of T11. She was given teriparatide. After the second injection, she reported nausea, dizziness and myalgia. Injections were withheld for 2 weeks and restarted. No further side effects developed.
3. Case 3
A 31-year-old primiparous woman visited because of back pain that had started 2 days following a vaginal delivery. She had breast-fed her baby since delivery. Her height was 164 cm and her weight was 61 kg. She had a history of back pain treatment at 22-years-of-age that was treated with pain killer. Lumbar spine MRI revealed compression fractures of T12, L2, L4, and L5. She was given calcium 500 mg daily and cholecalciferol 1,000 IU.
4. Case 4
A 35-year-old primiparous woman visited because of back and chest pain that started 3 month ago immediately after vaginal delivery. Her height was 165 cm and her weight was 63 kg. The spine MRI revealed recent compression fractures of T4, T5, T7, T8, T10-T12 and L2. She was given calcium 500 mg daily and cholecalciferol 1,000 IU with use of a chest brace. After 16 months of osteoporosis diagnosis, she became pregnant. The BMD Z-scores before the second pregnancy were -2.1 at L1–L4 and -2.0 at femur total. Scores after delivery were -1.2 at L1–L4 and -2.4 at femur total.
5. Case 5
A 36-year-old primiparous woman visited because of back and right paraspinal area pain that began one month previously immediately after vaginal delivery. Her height was 160 cm and her weight was 45 kg. She had no past surgical or family histories, or trauma. A bone scan (Tc-99m dicarboxypropane diphosphonate) revealed compression fractures of T7, T9–L5. She was given calcium 500 mg daily and cholecalciferol 1,000 IU with use of a chest brace. After one month of calcium/vitamin D medication, teriparatide injcetion was started. After 9 months of teriparatide injection, she was diagnosed as papillary thyroid cancer and underwent total thyroidectomy. BMD score after teriparatide injection showed an improved state of osteoporosis.
6. Case 6
A 28-year-old primiparous woman visited because of back pain. She had delivered 3 months previously and back pain had started 3 weeks before the hospital visit. Her height was 161 cm and her weight was 52 kg. She had no past surgical or family histories. Lumbar spine MRI revealed recent compression fractures of T6–T9, T12, L2, and L5. She was given calcium 500 mg daily and cholecalciferol 1,000 IU for 8 months.
Pretreatment BMD Z-score determined by dual energy X-ray absorptiometry in all patients was -2.5±0.3 at L1–L4 and -1.5±0.7 at femur (Table 1). The post-treatment mean BMD Z-score was -1.7±0.6 at L1–L4 and -1.4±0.4 at femur. The mean BMD Z-score change was 0.8±0.6 at L1–L4, 0.1±0.4 at femur in all patients, 0.5±0.4 at L1–L4, 0.2±0.1 at femur in calcium/vitamin D supplementation group and 1.3±0.6 at L1–L4 and -0.2±0.81 in those treated with teriparatide.
Discussion
The incidence of pregnancy-related osteoporosis is unknown. The mechanisms of pregnancy-related osteoporosis is also unclear. Several possible mechanisms had been suggested. First, calcium deficiency and hypoestrogenemia can give rise to bone mineral loss [5] in pregnant or lactating women. Calcium is needed for fetal growth and lactation. To meet the increased demands for calcium during fetal development, especially the third trimester of pregnancy, the maternal intestinal absorption of calcium doubles. Even with calcium homeostasis during pregnancy, loss of BMD in the spine and hip can occur [6]. Lactating women experience a transient 3% to 9% decrease in bone density [4], as bone calcium is scavenged. More et al. [7] found that all markers of bone turnover increased during normal pregnancy and failed to reach baseline level by 12 months postpartum. Also, during lactation, ovarian follicular development is inhibited and postpartum amenorrhea continues. So, women can become hypoestrogenic and BMD can decrease continuously.
Second, women experience endocrine changes during pregnancy that can cause ligament laxity [8]. Multiple sex hormones including such as progesterone, estrogen and relaxin affect ligament laxity. Pregnant women with pregnancy-induced hypertension (PIH) or preterm labor need specific treatment, such as magnesium sulfate injection or prolonged bed-rest. These can lead to stress or fatigue fractures during delivery [8]. However, in our case series, there was no case of PIH or preterm labor.
The relationship of obstetrical history and postpartum osteoporosis is controversial. Previous lactation period and obstetrical history might be risk factors for postpartum osteoporosis. Ghannam et al. [9] reported that the number of pregnancies and total duration of lactation negatively correlated with BMD Z-score at the spine and that Saudi women displayed significantly lower BMD levels than their United States counterparts. On the contrary, in another study BMD measured on postpartum day 2 was not correlated with parity and previous history of prolonged lactation [3]. Prolonged breast-feeding showed a negative long-term effect on BMD only in postmenopausal women in another [6]. Presently, five of the patients were primiparous and there was no history of PIH or preterm labor. The relationship of obstetrical history and pregnancy-related osteoporosis needs more research with greater numbers of patients.
We considered that another risk factor might be important in Korean women. Dunne et al. [10] reported that the higher prevalence of fractures in the mothers of postpartum osteoporosis patients compared to controls. This raises the possibility association of genetic factor in the etiology of this condition [10]. Undoubtedly, lower BMD before pregnancy can also cause postpartum osteoporosis. However, generally BMD is not checked before pregnancy. Evaluation of BMD before pregnancy could be beneficial for women with a family history of osteoporotic fracture.
The most common symptom is severe back pain [11]; all six of the present cases complained of severe back pain. Postpartum women, especially those who breast-feeding, suffer back pain and osteoporosis, and osteoporotic fracture must be suspected and evaluated carefully.
There is no clinical guideline for the treatment of pregnancy-related osteoporosis. Traditional management of postpartum osteoporosis includes calcium and vitamin D supplementation and weaning [2]. But, calcium and vitamin D deficiency is not a universal finding [12]. Bisphosphonates are effective [12], but there are some concerns that they accumulate in bone and may be exposed to fetus in subsequent pregnancies and have adverse effects on the fetal roden skeleton [4]. The optimal duration of bisphosphonate in pregnancy-related osteoporosis also remains unsolved. However, treatment for up to 5 years seems a reasonable approach [13]. Recently, teriparatide, the human recombinant parathyroid hormone, was introduced for management of osteoporotic fracture. It has been shown to increase BMD and reduce the risk of fractures [11]. Teriparatide is not retained in the skeleton and is not likely to affect a fetus conceived after its discontinuation [4]. In one report, the effect of teriparatide for 18 months in three women with pregnancy or lactation-related osteoporosis was analyzed [14]. BMD increased by 14.5% to 25.0% at the lumbar spine and by 9.5% to 16.7% at the femoral neck after treatment. In another report, BMD increased by 24.4% at the lumbar spine, 9.9% and 4.6% at the left and the right total hip, respectively, and 12.6% and 7.8% at the left and right femur neck, respectively, after 13 months of treatment [15]. Presently, two cases were treated with teriparatide and the effect on BMD restoration was greatest compared with the other treatments. Another report described successful 1-34 PTH treatment after failure of bisphosphonate therapy. Therefore teriparatide is implicated as an optimal medical therapy in severe cases of pregnancy-related osteoporosis [4].
Another important issue is recurrence of pregnancy-related osteoporosis in subsequent pregnancy. Previous reports have indicated variable rates of fracture recurrence, as high as 33%. Therefore, women with pregnancy-related osteoporosis should be warned that subsequent pregnancy carries a modest risk of further fracture [12].
Although postpartum osteoporosis is relatively rare problem, we should recognize the potential risk factors and main symptoms of postpartum osteoporosis to prevent osteoporotic fractures and further sequelae.
Acknowledgments
This work was supported by clinical research grant from Pusan National University Hospital in 2015.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, et al. Clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25:2359–2381. doi: 10.1007/s00198-014-2794-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim TH, Lee HH, Jeon DS, Byun DW. Compression fracture in postpartum osteoporosis. J Bone Metab. 2013;20:115–118. doi: 10.11005/jbm.2013.20.2.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lebel E, Mishukov Y, Babchenko L, Samueloff A, Zimran A, Elstein D. Bone mineral density in gravida: effect of pregnancies and breast-feeding in women of differing ages and parity. J Osteoporos. 2014;2014:897182. doi: 10.1155/2014/897182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Polat SB, Evranos B, Aydin C, Cuhaci N, Ersoy R, Cakir B. Effective treatment of severe pregnancy and lactation-related osteoporosis with teriparatide: case report and review of the literature. Gynecol Endocrinol. 2015;31:522–525. doi: 10.3109/09513590.2015.1014787. [DOI] [PubMed] [Google Scholar]
- 5.Holmberg-Marttila D, Sievanen H, Tuimala R. Changes in bone mineral density during pregnancy and postpartum: prospective data on five women. Osteoporos Int. 1999;10:41–46. doi: 10.1007/s001980050192. [DOI] [PubMed] [Google Scholar]
- 6.Tsvetov G, Levy S, Benbassat C, Shraga-Slutzky I, Hirsch D. Influence of number of deliveries and total breast-feeding time on bone mineral density in premenopausal and young postmenopausal women. Maturitas. 2014;77:249–254. doi: 10.1016/j.maturitas.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 7.More C, Bhattoa HP, Bettembuk P, Balogh A. The effects of pregnancy and lactation on hormonal status and biochemical markers of bone turnover. Eur J Obstet Gynecol Reprod Biol. 2003;106:209–213. doi: 10.1016/s0301-2115(02)00237-3. [DOI] [PubMed] [Google Scholar]
- 8.Clemetson IA, Popp A, Lippuner K, Ballmer F, Anderson SE. Postpartum osteoporosis associated with proximal tibial stress fracture. Skeletal Radiol. 2004;33:96–98. doi: 10.1007/s00256-003-0721-2. [DOI] [PubMed] [Google Scholar]
- 9.Ghannam NN, Hammami MM, Bakheet SM, Khan BA. Bone mineral density of the spine and femur in healthy Saudi females: relation to vitamin D status, pregnancy, and lactation. Calcif Tissue Int. 1999;65:23–28. doi: 10.1007/s002239900652. [DOI] [PubMed] [Google Scholar]
- 10.Dunne F, Walters B, Marshall T, Heath DA. Pregnancy associated osteoporosis. Clin Endocrinol (Oxf) 1993;39:487–490. doi: 10.1111/j.1365-2265.1993.tb02398.x. [DOI] [PubMed] [Google Scholar]
- 11.Ofluoglu O, Ofluoglu D. A case report: pregnancy-induced severe osteoporosis with eight vertebral fractures. Rheumatol Int. 2008;29:197–201. doi: 10.1007/s00296-008-0641-5. [DOI] [PubMed] [Google Scholar]
- 12.O'Sullivan SM, Grey AB, Singh R, Reid IR. Bisphosphonates in pregnancy and lactation-associated osteoporosis. Osteoporos Int. 2006;17:1008–1012. doi: 10.1007/s00198-006-0112-3. [DOI] [PubMed] [Google Scholar]
- 13.Ott SM. Long-term safety of bisphosphonates. J Clin Endocrinol Metab. 2005;90:1897–1899. doi: 10.1210/jc.2005-0057. [DOI] [PubMed] [Google Scholar]
- 14.Choe EY, Song JE, Park KH, Seok H, Lee EJ, Lim SK, et al. Effect of teriparatide on pregnancy and lactation-associated osteoporosis with multiple vertebral fractures. J Bone Miner Metab. 2012;30:596–601. doi: 10.1007/s00774-011-0334-0. [DOI] [PubMed] [Google Scholar]
- 15.Lampropoulou-Adamidou K, Trovas G, Stathopoulos IP, Papaioannou NA. Case report: teriparatide treatment in a case of severe pregnancy -and lactation-associated osteoporosis. Hormones (Athens) 2012;11:495–500. doi: 10.14310/horm.2002.1383. [DOI] [PubMed] [Google Scholar]