Abstract
Objective
To examine the association of the use of hospice care on patient experience and outcomes of care. Promoting high-value, safe, and effective care is an international healthcare imperative. However, the extent to which hospice care may improve the value of care is not well characterized.
Methods
A secondary analysis of variations in care was conducted using the Dartmouth Atlas Report, matched to the American Hospital Association Annual Survey Database to abstract organizational characteristics for 236 US hospitals to examine the relationship between hospice utilization and a number of variables that represent care value including hospital care intensity index, hospital deaths, ICU deaths, patient satisfaction, and a number of patient quality indicators. Structural equation modeling was used to demonstrate the effect of hospice use on patient experience of care variables, clinical outcomes of care variables, and efficiency of care variables.
Results
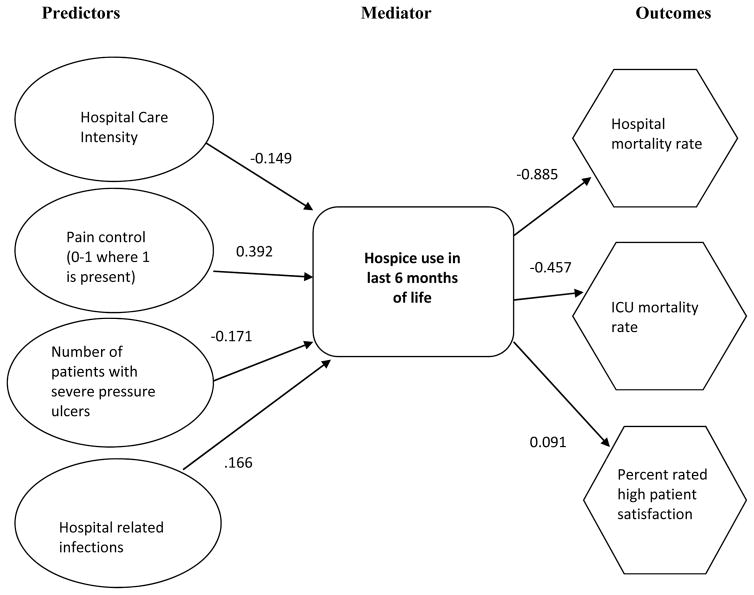
Hospice admissions in the last 6 months of life were correlated with a number of variables including increases in patient satisfaction ratings (r=0.448, p=0.01) and better pain control (r=0.491, p=0.01), and reductions in hospital days (r=−0.517, p=0.01), fewer deaths in the hospital (r=−0.842, p=0.01), and fewer deaths occurring with an ICU admission during hospitalization (r=−0.358, p=0.01). The structural equation model identified use of hospice care was inversely related to both hospital mortality (−.885) and ICU mortality rate (−.457).
Conclusions
The results of this investigation demonstrate that greater utilization of hospice care during the last 6-months of life is associated with improved patient experience of care including satisfaction and pain control, as well as clinical outcomes of care including decreased ICU and hospital mortality.
Keywords: hospice care, palliative care, end-of-life, clinical decisions, hospital care
INTRODUCTION
The concept of regional variations in healthcare has been repeatedly demonstrated by several Dartmouth Atlas of Health Care Reports.1 The Dartmouth Atlas Project focuses on describing how medical resources are distributed and used in the U.S.2 The project has demonstrated significant variations in how health care is delivered across the United States, including a recent report that informs current and prospective medical students with information about the patterns of care provided by 236 major teaching hospitals.3 Wide variation was found in the use of physicians, hospital beds, and hospice. In addition, there was variability among measures of quality, safety, and patient experience ratings.3
As the focus of hospital reimbursement moves towards a value based system, hospitals are searching for ways to reduce unnecessary health care utilization and improve quality, safety, and patient experience. This focus has sharpened following enactment of Value-Based Purchasing (VBP), authorized by the Affordable Care Act and now part of the Centers for Medicare & Medicaid Services (CMS). VBP is an effort to link payment for inpatient acute care services to a value-based system to improve healthcare quality, improve patient satisfaction, and reduce cost.4
Palliative care and hospice services have been proposed a potential means to improve outcomes of care as well as the efficiency and satisfaction with care.5 For example, hospice use has been demonstrated to improve the quality of care for patients and their families near the end of life. Studies have demonstrated that hospice use is associated with reductions in symptom distress, improved outcomes for caregivers, patient and family satisfaction, and reduced use of hospital based resources including emergency room visits and intensive care unit (ICU) treatment.6–9 Hospice use has also been shown to result in decreased costs and reduced hospital length of stay.10 Yet, wide variability in hospice use prior to death exists, with utilization rates ranging from 10% to 45% during the last six months of life.11–15
We hypothesized that increasing hospice utilization would be associated with improvements in the various VBP domains. Specifically, we hypothesized that hospice utilization would be associated with 1) Improved patient experience (as measured by patient satisfaction and percent recommending the hospital), and 2) Improved clinical outcomes of care (as measured by ICU and hospital mortality). The relationship of hospice care to these specific outcomes has not been extensively explored, yet plausible associations may exist in light of palliative care focus on a patient-centered approach to care.
METHODS
Study Design / Inclusion / Exclusion Criteria
We performed a retrospective cross sectional analysis. We included academic medical centers that were included in the Dartmouth Atlas 2012 report and responded to the American Hospital Association (AHA) annual hospital survey from the same year.
Data Sources
The Dartmouth Atlas provides healthcare utilization data from the last six months of life among Medicare beneficiaries. We utilized data from the Dartmouth Atlas report released in 2012 that examined variations in medical care for Medicare beneficiaries among 236 academic medical centers rated by U.S. News and World Report as the best hospitals for clinical excellence in 2012–13. This cohort was selected because of the availability of hospital level patient experience, outcomes, and care efficiency data.
The study population included fee-for service Medicare beneficiaries who died in 2010 and who were hospitalized for a chronic illness at least once during their last two years of life. The cohort was restricted to patients with at least one of nine chronic illnesses associated with high mortality rates: malignant cancer/leukemia, chronic pulmonary disease, coronary artery disease, congestive heart failure, peripheral vascular disease, severe chronic liver disease, diabetes with end organ damage, chronic renal failure, and dementia. Patients were assigned to the hospital they used most frequently during their last two years of life. The hospital care intensity (HCI) index, a summary measure of inpatient care intensity, was used to reflect regional use of acute care resources in managing chronic illness over the last two years of life.16 The HCI index reflects both the amount of time spent in the hospital and the intensity of physician intervention during hospitalization as it is based on both the number of days spent in the hospital and the number of inpatient physician visits patients experienced.15 Regional prediction was based on the 306 Dartmouth Atlas hospital referral regions (HRRs) and 3,436 geographically distinct hospital service areas.
The AHA Annual Survey Database™ was used from the most recently available survey (2012). The AHA Annual Survey Database™ is a comprehensive hospital census of U.S. hospitals based on the AHA Annual Survey of Hospitals, conducted by the American Hospital Association since 1946. The Database of over 6,400 hospitals includes up to 1,000 fields of information in several categories including organizational structure, facility and service lines, inpatient and outpatient utilization and geographic indicators, among other hospital-level characteristics that may influence patient experience, clinical, and efficiency outcomes.
Ethics
Institutional Review Board approval was submitted and received from Rush University Medical Center, Chicago Illinois and was deemed exempt as no identifiable information was used in the study and results are reported in aggregate.
Patient Experience Outcomes
Patient satisfaction was measured using the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). The primary outcome of interest was patient ratings of the overall hospital stay. Secondary patient experience outcomes included recommendations of the hospital, pain control, explanations of medications, and information about post-discharge care.
Clinical Outcomes
The primary clinical outcome of interest was mortality. Hospital mortality outcomes were reflected as the percent of patients with an ICU admission who died. Secondary clinical outcomes included number of patients with severe pressure ulcers, falls and injuries, central-line associated blood stream infections (CLABSI), and catheter associated urinary catheter infections (CAUTI).
Efficiency Outcomes
Efficiency of care outcomes included the number of days hospitalized in the last 6 months of life, and the number of physician visits in the last 6 months of life.
Predictors
Hospital-level, and regional-level predictors (including patient safety outcomes) were assessed using both the Dartmouth Atlas and AHA databases. The primary predictor of interest was hospice utilization as measured by the percentage of patients utilizing hospice in the last 6 months of life which was hypothesized to be associated with increased patient satisfaction and, reduced hospital and ICU mortality. We additionally examined how this predictor would be associated with the secondary outcomes of interest.
Covariates
Covariates for correlational and structural analyses included hospital specific services and characteristics which were obtained from the AHA database. These included total beds, total facility admissions, total facility inpatient days, hospital unit admissions, hospital unit inpatient days, hospital Medicare discharges, average daily census, number of ICU beds, number of intensivists, registered nurse vacancies, registered nurse full-time equivalents, teaching status, staffing ratios; predictors which were used to examine the relationship of hospital related characteristics and hospice utilization.
Statistical Analysis
SPSS 19.0 and AMOS 4.0 (Analysis of Moment Structures) were used to conduct the statistical analysis. Hospitals were matched based on their names, as presented in the two databases. There were 236 observations in the Dartmouth database, and 6317 in the AHA database, creating a merged database of 236 facilities representing over 163,122 patients. Correlational analysis (Pearson product-moment correlation coefficient) was first used to assess for associations among the variables of interest. An analysis plan was constructed using patient satisfaction (percent who rated high patient satisfaction), and hospital mortality (percent deaths in the hospital), as the main dependent variables and the percentage of patients using hospice in the last six months of life as the proximal independent variable, taking into account hospital and structural characteristics, quality indicators and patient characteristics (hospital care intensity index) as described above.
Statistical Modeling
Additional analyses using structural equation modeling were used to estimate the effects of six potential exogenous predictors (hospice use last six months of life, use of pain control, pressure sores, HCI index, full-time RNs, region) on three endogenous outcomes (high patient satisfaction, overall mortality, and mortality for patients who had an ICU admission). Hospital was used as unit of analysis in these models. The models were developed a priori based on clinical experience and medical literature, and then were further refined using modification indices to arrive at a model that fit the empirical data.
RESULTS
Descriptive statistics for the final sample are displayed in Table 1. There was a significant relationship between hospice use in the last 6 months of life and several of the primary outcomes including higher patient satisfaction ratings (r=0.448, p=0.01), hospital days (r=−0.517, p=0.01), fewer deaths in the hospital (r=−0.842, p=0.01), fewer deaths occurring with an ICU admission during hospitalization, (r=−0.358, p=0.01), and fewer hospital days (r=−0.517, p=0.01) (Table 2). There were additional significant relationships noted among the secondary outcomes. For example, greater use of hospice was associated with greater patient reports that medications were explained before they were administered (p=0.01), and greater patient reports that information was given about postdischarge care (p=0.01).
Table 1.
Descriptive Statistics of Study Variables
| Study Variables | Number of Hospitals | Mean | Std. Deviation |
|---|---|---|---|
| Percent patients in hospice last six months | 236 | 46.84% | 10.85% |
| Region (0=north, 1=south) | 236 | 0.31 | 0.46 |
| Hospital Care Intensity index | 236 | 1.06 | 0.31 |
| Patient Experience of Care Variables | |||
| Percent who rated high patient satisfaction | 236 | 68.22% | 6.97% |
| Percent who recommended hospital | 236 | 73.24% | 7.41% |
| Percent who reported pain control | 236 | 67.57% | 4.03% |
| Medicine explained before given | 236 | 59.58% | 4.22% |
| Given information about post discharge care | 236 | 83.19% | 3.94% |
| Clinical Outcomes of Care Variables | |||
| Percent of deaths in the hospital | 236 | 31.05% | 7.05% |
| Percent of deaths in the ICU | 236 | 21.90% | 5.61% |
| Number of patients with severe pressure ulcers per 1000 patients discharged | 236 | 0.21 | 0.24 |
| Falls and injuries per 1000 patients discharged | 230 | 0.46 | 0.22 |
| Blood infection from large vein catheter | 230 | 0.56 | 0.45 |
| Infection from urinary catheter | 230 | 0.47 | 0.57 |
| Signs of un-controlled blood sugar | 230 | 0.09 | 0.11 |
| Efficiency of Care Variables | |||
| Number of days hospitalized the last 6 months of life | 236 | 13.35 | 3.27 |
| Number of MD visits last 6 months of life | 236 | 34.40 | 11.82 |
| Number of full-time RNs | 236 | 1338.64 | 836.59 |
Table 2.
Associations Among Study Variables and Percent of Hospice use in the Last Six Months of Life
| Study Variables | Correlations with percent of patients in hospice last six months |
|---|---|
| Patient Experience Outcomes | |
| Percent who rated high patient satisfaction | 0.448** |
| Percent who recommend hospital | 0.367** |
| Percent who indicate pain controlled | 0.491** |
| Medicine explained before given | 0.414** |
| Given information about post-discharge care | 0.349** |
| Clinical Outcomes of Care | |
| Percent of deaths in the hospital | −0.842** |
| Percent of deaths in the ICU | −0.358** |
| Number of patients with severe pressure ulcers per 1000 patients discharged | −0.252** |
| Falls and injuries per 1000 patients discharged | 0.042 |
| Blood infection from large vein catheter | 0.061 |
| Infection from urinary catheter | 0.102 |
| Efficiency Outcomes | |
| Number of days hospitalized the last six months of life | −0.517** |
| MD visits in last 6 months of life | −0.156* |
Correlation is significant at the 0.01 level (2-tailed).
Correlation is significant at the 0.05 level (2-tailed).
Structural Equation Modeling
Structural equation modeling was used to demonstrate the effect of hospice use on patient experience of care variables (as measured by patient satisfaction and percent recommending the hospital) and outcomes of care variables (as measured by ICU and hospital mortality). The final three-stage model identified that the use of hospice care mediated the relationship between the exogenous predictors described above and overall hospital mortality (SEM coefficient = −0.885), and hospital mortality among those with an ICU admission (SEM coefficient = −0.457). In addition, hospitals that use hospice care had higher patient reports of satisfaction (SEM coefficient= 0.0091) (Figure 1).
Figure 1.
Final structural model for predicting mortality and patient satisfaction
DISCUSSION
The results of this study demonstrate that use of hospice was associated with improvements in the domains of VBP including improvements in patient experience, clinical outcomes and efficiency. Hospice admissions in the last 6 months of life was a significant mediator and was correlated with improved patient satisfaction ratings (r=0.448, p=0.01), lower deaths in the hospital (r=−0.842, p=0.01), and reductions in health care intensity. This was demonstrated both using simple bivariate relationships, as well as by examining the structural equation model that controlled for a number of possible confounders.
In a retrospective cohort study of Medicare claims data, Wennberg et al.14 evaluated healthcare use in the last six months of life for 115,089 patients - 98,415 (85%) of whom were chronically ill - from 77 hospitals rated by US News and World Report as “best hospitals”. Substantial variability was found in the intensity of care measures including the number of days spent in the hospital (<10 to > 27), number of days in the ICU (1.6 to 9.5 days per person), ICU mortality (<9 to >36), and the percent of patients receiving hospice care (< 11% to > 43%). However, the relationship between hospice use and patient satisfaction and clinical outcomes was not described. The results of the current study are similar to prior research which has shown a relationship between hospice use and decreased hospital inpatient mortality rates. Chang and Steinberg17 demonstrated that high hospice enrollment was associated with lower Medicare inpatient mortality in a state level analysis. The study identified that an increase in hospice population by 100 individuals was associated with a reduction of 28 inpatient deaths.
Of interest, in the current study, the percent of hospice admissions in the last 6 months of life was found to be a strong overall indicator of value based outcomes, including clinical outcomes and patient satisfaction. With regard to clinical outcomes, hospice use was negatively correlated to a number of crude end-of-life measures (mortality in general and for patients with an ICU admission during hospitalization; and physician visits and hospital days the last six months of life). However, it was positively correlated to five measures of patient satisfaction, patient recommendations of the hospital, patient reports on whether medications and post discharge care were explained to them, and pain control. These correlations ranged from .35 to .49 and all were statistically significant (see Table 2).
Overall, the results of this secondary data analysis highlight that opportunities exist for greater expansion of hospice use to reduce deaths in the hospital setting and improve the quality of care for chronically ill patients. Limitations of the study include the use of cross sectional data, focus on academic medical centers, and limit of analyses to Medicare patient outcomes; and the potential impact of unmeasured confounding variables.
While the results are associative and not causal, this exploratory analysis can help hospitals and researchers begin to understand factors that will help drive value in today’s healthcare environment. CMS highlights the importance of high quality care for patients in designating the patient care experience as measures of performance and reimbursement as part of VBP, with 30% of incentive payments derived from patient ratings of their care.4 As hospital VBP and the focus on patient experience of care now impact reimbursement rates, optimal hospital care goals should promote quality of care outcomes in addition to promoting quality end-of-life care. As highlighted by the Institute for Healthcare Improvement, the drivers of achieving an exceptional patient and family experience of inpatient hospital care (defined as care that is patient centered, safe, effective, timely, efficient, and equitable), are focused on providing respectful, reliable care, which is also evidence based.18 Targeting hospital care that promotes best outcomes for patients while simultaneously achieving a positive patient and family experience is now an expectation of healthcare. As highlighted in the recently released Institute of Medicine report on improving end-of-life care, providing high-quality care for people who are nearing the end of life is a professional commitment and responsibility.19 Additional research is needed which further focuses on strategies for achieving goals of care in conjunction with focusing on the patient and family experience of care. Dissemination of successful hospital based initiatives is also needed to promote replication and further testing of successful models of care.
CONCLUSIONS
The results of this secondary data analysis from a recent Dartmouth Atlas Report which explored variations in medical care for Medicare beneficiaries among 236 academic medical centers, demonstrate that greater use of hospice care for hospitalized patients results in improved patient satisfaction ratings along with lower mortality rates, both in the hospital as well as for those patients with an ICU admission during hospitalization. Consistent with other studies demonstrating benefit, the use of hospice care is associated with better quality of care outcomes, including patient-centered care metrics. Recent research has demonstrated the feasibility and economic impact of dedicated hospice inpatient units for terminally ill ICU patients.20–21 As the risk trajectory for death after hospital discharge can range from 25% to 35%,22 and as nationally, 10–20% of patients admitted to the ICU will die in the ICU,23 providing quality end-of-life care including integration of hospice care become important goals for targeting healthcare that is focused on high value, as well as patient and family centered care.
Acknowledgments
Dr. Vasilevskis was supported by the National Institute on Aging of the National Institutes of Health under Award Number K23AG040157 and the Veterans Affairs Clinical Research Center of Excellence, and the Geriatric Research, Education and Clinical Center (GRECC). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Department of Veterans’ Affairs
Footnotes
Conflict of Interest Disclosures: None
Contributorship Statement
All authors actively contributed to the conception, design, interpretation of study results, and manuscript preparation. Ruth Kleinpell, Louis Fogg, E Wesley Ely and Eduard Vasilevkis planned the study; Louis Fogg conducted the statistical analysis work; and all authors actively contributed to the reporting of the work as described in the manuscript.
References
- 1.Dartmouth Atlas of Healthcare Reports. [Accessed June 24, 2015];Patient experience and quality at 236 teaching hospitals. 2013 http://www.dartmouthatlas.org/pages/quality_236_hospitals.
- 2. [Accessed June 24, 2015];Dartmouth Atlas of Healthcare Reports. http://www.dartmouthatlas.org/publications/reports.aspx.
- 3.Arora A, True A. The Dartmouth Atlas. The Dartmouth Institute for Health Policy and Clinical Practice; 2012. What Kind of Physician Will You Be? Variation in Health Care and Its Importance for Residency Training. [PubMed] [Google Scholar]
- 4.Center for Medicaid Services. [Accessed June 24, 2015];Hospital Value Based Purchasing. http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/hospital-value-based-purchasing/index.html?redirect=/Hospital-Value-Based-Purchasing/
- 5.Frist WH, Presley MK. Training the Next Generation of Doctors in Palliative Care Is the Key to the New Era of Value-Based Care. Academic Medicine. 2015;90(3):268–271. doi: 10.1097/ACM.0000000000000625. [DOI] [PubMed] [Google Scholar]
- 6.Meier DE. Increased access to palliative care and hospice services: Opportunities to improve value in health care. The Milbank Quarterly. 2011;89:343–380. doi: 10.1111/j.1468-0009.2011.00632.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Teno JM, Shu JE, Casarett D, Spence C, Rhodes R, Connor S. Timing of referral to hospice and quality of care. J Pain Symptom Manage. 2007;34(2):120–5. doi: 10.1016/j.jpainsymman.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 8.Teno JM, Clarridge BR, Casey V, Welch LC, Wetle T, Shield R, Mor V. Family Perspectives on End-of-Life Care at the Last Place of Care. JAMA. 2004;291:88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 9.Wright AA, Keating NL, Balboni TA, Matulonis UA, Block SD, Prigerson HG. Place of death: correlations with quality of life of patients with cancer and predictors of bereaved caregivers’ mental health. J Clin Oncol. 2010;28(29):4457–64. doi: 10.1200/JCO.2009.26.3863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carlson M, Herrin J, Du Q, Epstein A, Barry C, Morrison R, Back A, Bradley E. Impact of Hospice Disenrollment on Health Care Use and Medicare Expenditures for Patients with Cancer. J Clinical Oncol. 2010;28:4371–75. doi: 10.1200/JCO.2009.26.1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Connor NR, Hu R, Harris PS, Ache K, Casarett DJ. Hospice admissions for cancer in the final days of life: independent predictors and implications for quality measures. J Cancer Oncol. 2014;32:3184–3189. doi: 10.1200/JCO.2014.55.8817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nicholas LH, Langa KM, Iwashyna TJ, Weir DR. Regional variation in the association between advanced directives and end-of-life medicare expenditures. JAMA. 2011;306:1447–1453. doi: 10.1001/jama.2011.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keating NL, Herrinton LJ, Zaslavsky AM, Liu L, Avanian JZ. Variations in hospice use among cancer patients. Variations in hospice use among cancer patients. J Nat Cancer Inst. 2006;98:1053–9. doi: 10.1093/jnci/djj298. [DOI] [PubMed] [Google Scholar]
- 14.Wennberg JE, Fisher ES, Stukel TA, Skinner JS, et al. Use of hospitals, physician visits, and hospice care during last six months of life among cohorts loyal to highly respected hospitals in the United States. BMJ. 2004;328:607. doi: 10.1136/bmj.328.7440.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Virnig BA, Kind S, McBean M, Fisher E. Geographic variation in hospice use prior to death. JAGS. 2000;48:1117–1125. doi: 10.1111/j.1532-5415.2000.tb04789.x. [DOI] [PubMed] [Google Scholar]
- 16.Wennberg JE, Bronner K, Skinner JS, Fisher ES, Goodman DC. Inpatient Care Intensity And Patients’ Ratings Of Their Hospital Experiences: What could explain the fact that Americans with chronic illnesses who receive less hospital care report better hospital experiences? Health Affairs. 2009;28:103–112. doi: 10.1377/hlthaff.28.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang CF, Steinberg SC. Influence of hospice use on hospital inpatient mortality: a state-level analysis. Hospital Topics. 2006;84:2–10. doi: 10.3200/HTPS.84.2.2-10. [DOI] [PubMed] [Google Scholar]
- 18.Balik B, Conway J, Zipperer L, Watson J. IHI Innovation Series white paper. Cambridge, Massachusetts: Institute for Healthcare Improvement; 2011. Achieving an Exceptional Patient and Family Experience of Inpatient Hospital Care. (Available on www.IHI.org) [Google Scholar]
- 19.Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Washington DC: National Academies Press; 2014. [PubMed] [Google Scholar]
- 20.Binney ZO, Quest TE, Feingold PL, Buchman T, Majesko AA. Feasibility and economic impact of dedicated hospice inpatient units for terminally ill ICU patients. Crit Care Med. 2014;42:1074–1080. doi: 10.1097/CCM.0000000000000120. [DOI] [PubMed] [Google Scholar]
- 21.Kelley AS, Deb P, Du Q, Aldridge MD, Morrison SR. Hospice Enrollment Saves Money For Medicare And Improves Care Quality Across A number of different lengths-of-stay. Health Affairs. 2013;32:552–561. doi: 10.1377/hlthaff.2012.0851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dharmarajan K, Hsieh AF, Kulkarni VT, Lin Z, Ross JS, et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: retrospective cohort study. BMJ. 2015;350:h411. doi: 10.1136/bmj.h411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goodman DC, Esty AR, Fisher ES, et al. Trends and variations in end-of-life care for medicare beneficiaries with severe chronic illness. Hanover, NH: Dartmouth Atlas Project; 2011. [PubMed] [Google Scholar]