Abstract
Objective
Presently, little is known about what factors predict adolescent psychiatric rehospitalization. Thus, the present study tested whether a battery of demographic and clinical characteristics predicted readmission within 6 months of discharge.
Methods
Participants were 165 adolescents (112 females) aged 13–19 years (mean = 15.61, SD = 1.48) admitted to an acute residential treatment program between November 25, 2013, and November 18, 2014. Patients met diagnostic criteria (DSM-IV-TR) for current major depressive disorder or dysthymia. At admission, participants completed a battery of clinical interviews and questionnaires assessing demographics, early life stress, comorbid diagnoses, psychiatric symptoms, suicidality, self-injury, and risky behavior engagement. At discharge, psychiatric symptoms were reassessed. Readmission to the same residential service was monitored over a 6-month period following discharge.
Results
Overall, 12.1% of adolescents were rehospitalized. We conducted a series of Cox regression survival analyses to test demographic and clinical predictors of patients’ time to readmission. More frequent self-injurious behaviors in the month prior to hospitalization was significantly associated with a more rapid time to rehospitalization (β = 0.05, SE = .02, Wald1 = 4.35, P = .037, OR = 1.05, 95% CI = 1.003–1.10).
Conclusions
It is critical to more effectively manage self-injury during the treatment of depressed adolescents, as this is the strongest predictor of later rehospitalization.
Major depressive disorder (MDD) is a debilitating mental illness that affects approximately 11% of adolescents.1 Although the majority of adolescents treated for depression receive outpatient interventions,2 short-term acute residential treatment services are an intensive option for adolescents with particularly severe symptoms. Adolescents admitted to residential treatment services are characterized by diagnostic comorbidity, elevated rates of nonsuicidal self-injury (NSSI), and escalating suicidal thoughts and behaviors.3,4 Short-term residential programs involve brief (approximately 15 days) lengths of stay during which patients are provided 24-hour supervision and targeted psychosocial and pharmacologic interventions.5 Despite the severity of the patient population and time-limited nature of the interventions, outcome studies indicate that short-term residential programs significantly improve youth’s symptoms and functioning.6
Although short-term residential programs are effective, approximately a third of patients are rehospitalized within a year of discharge, with most readmissions occurring within 3 months.7–9 These rehospitalizations are associated with a substantial economic burden10 and have a pronounced psychosocial toll on adolescents and their families.11,12 For patients, repeated hospitalizations may disrupt social support and result in greater stigmatization.10,13 Nonetheless, there is a dearth of studies that have investigated potential predictors of rehospitalization among adolescent psychiatric samples.14 To address this empirical gap, the present study recruited a sample of depressed adolescents admitted to a short-term residential unit and tested whether key demographic and clinical characteristics were associated with rehospitalization within 6 months of discharge.
The extant literature on predictors of rehospitalization among adolescents is largely dependent on inpatient cohorts, and these results are mixed. In terms of demographic correlates, some studies show that rehospitalization is associated with younger age8,9,15 and male sex,7 while others do not find these effects.8,9,12,15 Research on ethnicity has focused exclusively on the effect of identifying as white or nonwhite, and no significant effects were found.8,9,16 Although low socioeconomic status is considered a risk factor for rehospitalization,8,17 this has yet to be confirmed. Studies also have explored the role that early life stress plays in predicting rehospitalization. Child abuse was a predictor in some,8,15 but not all,7 studies. Despite the overrepresentation of adopted adolescents in psychiatric settings,18 there is no documented association between adoption status and rehospitalization among child inpatients.19 Taken together, these studies underscore the need for more systematic study.
Surprisingly, few studies have investigated clinical characteristics of adolescent patients that predict rehospitalization, particularly as it may relate to the role of psychiatric diagnoses, symptom severity, and improvement in acute care. First, with respect to diagnosable mental disorders, a unipolar mood disorder is a strong predictor of rehospitalization16,20; however, other studies12,15 found no effect of any specific psychiatric diagnosis. Despite the high prevalence of comorbidity among adolescent psychiatric patients,3 it remains unclear whether such comorbidity predicts rehospitalization. Second, with respect to symptom severity, higher levels of depressive symptoms are a well-established predictor of poor treatment response among adolescents in outpatient settings.21 Yet, it is unknown whether depression severity and related symptoms are implicated in rehospitalization for acute care. Last, although short-term residential psychiatric care is effective for most adolescents, it seems plausible that modest treatment gains and residual symptoms may predict rehospitalization. Among outpatients with MDD, residual symptoms are among the strongest predictors of future episodes.22,23 Nevertheless, no study has tested the association between symptom change during residential treatment and later rehospitalization among adolescent patients.
Clinical Points.
Rehospitalization following acute psychiatric treatment is common and costly among adolescent patients. However, reliable predictors of readmission have not been identified.
Nonsuicidal self-injury in the month prior to hospitalization was the strongest predictor of rehospitalization among depressed adolescents.
Clinicians should implement clinical interventions targeting self-injury during hospitalization and should consider these behaviors in risk assessments and discharge decisions.
In addition to these clinical factors, suicidality, NSSI, and other risky behaviors may lead to rehospitalization. The only study8 to include any of these factors found that recent suicidal ideation or attempts prior to hospitalization predicted readmissions. However, no research has examined the impact of NSSI or risky behavior engagement. Both behaviors tend to be relatively stable and persist among depressed adolescents24,25 and may be less likely to change in the context of short-term treatment. Further, as NSSI and risky behavior engagement tend to be more overt, these behaviors may act as early warning signs for families and outpatient clinicians to increase the level of care needed for adolescents.
In sum, the literature on predictors of rehospitalization among adolescent patients is limited. The present study investigates a broad set of potential predictors in a sample of depressed adolescents admitted to short-term residential treatment. On the basis of existing research, our analyses first tested 5 clusters of potential predictors: (1) demographic characteristics (age, sex, ethnicity, and parental education), (2) early life stress (childhood abuse, adoption status, peer victimization), (3) diagnoses at admission and general comorbidity, (4) symptom severity at admission (depression, anhedonia, hopelessness, and anxiety) and change in these symptoms, and (5) suicidality, NSSI, and risky behaviors. Significant predictors from each of these broad clusters were then tested simultaneously in a distilled model.
METHODS
Participants
Participants (n = 165, 112 females) were adolescents satisfying Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR)26 criteria for current MDD or dysthymia upon admission to a short-term adolescent residential treatment program between November 25, 2013, and November 18, 2014. Diagnoses were confirmed with the Mini-International Neuropsychiatric Interview for Children and Adolescents (MINI-KID).27 Participants were 13–19 years old (mean = 15.61, SD = 1.48), and their racial/ethnic distribution included 83.3% white, 10.5% multicultural (ie, endorsed more than 1 race), 3.7% Asian, 1.2% black, and 1.2% Native American. The majority of participants’ parents received continued education beyond high school (eg, community college, university): 84.9% of mothers (n = 129, 13 cases had missing data) and 83.7% of fathers (n = 123, 18 cases had missing data).
The program to which participants were admitted provides short-term residential care for adolescents with emotional and behavioral difficulties. While living in the unit, adolescents received a combination of individual and group psychotherapy (eg, cognitive-behavioral therapy, dialectical behavior therapy), family therapy, pharmacotherapy, and case management geared toward stabilization and rapid symptom reduction. Length of treatment ranged from 3 to 32 days (mean = 13.21, SD = 4.04).*
Measures
Demographic characteristics
Participants provided information regarding sex, age, race/ethnicity, maternal and paternal education level, and adoption status.
MINI-KID
The MINI-KID27 is a structured diagnostic interview that assesses current and past DSM-IV Axis I diagnoses in youth. Research has shown that it is a reliable tool for diagnosing psychopathology in outpatient27 and inpatient3 adolescents. All interviews were conducted by bachelor’s-level research assistants or graduate students after they received 25 hours of training.
Self-Injurious Thoughts and Behaviors Interview (SITBI)
The SITBI28 is a brief structured interview assessing NSSI and suicidal thoughts and behaviors. NSSI thoughts/behaviors and suicide ideation/attempts in the past month were used as predictors for rehospitalization.
Childhood Trauma Questionnaire (CTQ)
The CTQ29 is a 25-item self-report questionnaire that assesses the presence and severity of childhood maltreatment and abuse. We used the three 5-item subscales that assess emotional, physical, and sexual abuse and summed these to create a total abuse score. Responses to individual items ranged from 1 (never true) to 5 (very often true), with higher scores reflecting more severe abuse. The internal consistency of the 15-item total abuse scale was strong (α = .89).
Revised Peer Experiences Questionnaire (RPEQ)
The RPEQ30 is a questionnaire assessing adolescent aggression and peer victimization. This study employed a 9-item subscale that captures total victimization, including direct (eg, teasing, hitting) and indirect (eg, excluding, spreading rumors) experiences. Each item ranges from 1 (never) to 5 (a few times a week). The 9-item total victimization scale had good internal consistency (α = .89).
Center for Epidemiologic Studies Depression scale (CES-D)
The CES-D31 is a 20-item self-report measure assessing the presence and severity of depressive symptoms in the past week. Items are rated from 0 (rarely or none of the time) to 3 (most or all of the time), and higher scores indicate greater depressive symptoms. The CES-D had excellent internal consistency (α values = .93–.96).
Multidimensional Anxiety Scale for Children (MASC)
The MASC32 is a 39-item self-report questionnaire wherein each item is rated from 0 (never true about me) to 3 (often true about me); higher scores indicate more severe anxiety symptoms. The internal consistency of MASC was excellent across administrations (α values = .91–.92).
Snaith-Hamilton Pleasure Scale (SHAPS)
The SHAPS33 is a 14-item self-report inventory that assesses one’s ability to experience pleasure on a scale ranging from 1 (strongly agree) to 4 (strongly disagree). Scores range from 14 to 56, with higher scores reflecting more severe anhedonia. In adolescent samples, the SHAPS demonstrates construct convergent and discriminant validity.34 The SHAPS had excellent internal consistency across administrations (α values = .90–.91).
Beck Hopelessness Scale (BHS)
The BHS35 is a 20-item self-report measuring hopelessness in the past week. Each item is rated as “true” or “false,” and total scores range from 0 to 20, with higher scores indicating greater hopelessness. The BHS had excellent internal consistency (α values = .91–.92).
Risky Behavior Questionnaire for Adolescents (RBQ-A)
The RBQ-A36 is a 20-item questionnaire that assesses the presence and frequency of risky behaviors (ie, sexual precociousness, aggression, rule-breaking, dangerous/illegal behaviors, self-injurious behaviors, and substance use) over the past month. Respondents rate each item from 0 (never) to 4 (always: 4 or more times per week) and higher scores indicate greater risky behavior engagement. Item 14 (ie, “Have you made attempts to cut or burn yourself?”) was removed as this information was assessed with the SITBI. Total scores ranged from 0 to 76. The 19 included items had good internal consistency (α = .76).
Procedures
The internal review board provided ethical approval for this study, and data were collected in the context of a larger quality assurance program. Parents and adolescents aged 18 years or older provided consent, and youth aged 13–17 provided assent. Within 48 hours of admission, participants completed the baseline clinical interviews and self-report all participants were readministered self-report measures of psychiatric symptom severity. Rehospitalization was defined as reentry into the same short-term residential program, and this was cross-referenced with participants’ medical records. The study included any readmission that occurred within 6 months of discharge.
Data Analysis
Preliminary analyses revealed univariate outliers (ie, scores greater than 3 standard deviations from the mean) in the following variables: NSSI thoughts, NSSI behaviors, suicidal ideation, and suicide attempts. Thus, these variables were winsorized prior to primary analyses. Our primary analyses were conducted in 2 stages. First, we ran a series of 5 preliminary Cox regression survival analyses predicting time to rehospitalization. These initial models were used to identify the strongest predictors within theoretically meaningful sets of variables. In these models, time was defined as the difference between the date of discharge and the date of readmission for each participant; participants who were not readmitted were assigned a time of 183 days (ie, 6 months). In step 1 of each model, covariates of age, sex, and baseline depressive symptoms were included.* For step 2, the following variables were entered in separate models: (1) demographics (ethnicity and parental education), (2) early life stress (adoption status, child abuse, peer victimization), (3) clinical diagnoses and comorbidity, (4) baseline symptom severity (depression, anhedonia, hopelessness, anxiety), and (5) suicidality, NSSI, and risky behaviors. In model 4, participants’ depression, anhedonia, hopelessness, and anxiety scores at discharge (ie, posttreatment) were entered on step 3, which, consistent with the recommendations of Cohen et al37 allowed us to measure the effects of change in these symptoms during treatment on the time to rehospitalization. In the second phase of our analyses, significant predictors of rehospitalization from the preliminary models were included together in a final Cox regression model. Again, step 1 of the model included age, sex, and baseline depressive symptoms as covariates, and the previously identified predictors were entered in step 2. With this approach, only predictors that were significant beyond the concurrent effects of other potential predictors within the same domain were considered in the final model.
RESULTS
Preliminary Analyses
Twenty adolescents (12.1%) were readmitted within 6 months of discharge from their initial hospitalization; the average time from discharge to rehospitalization was approximately 3 months (mean = 92.65 days, SD = 56.11). There were no significant differences between adolescents who were rehospitalized and those that were not in terms of sex, ethnicity, maternal education, paternal education, or adoption status (all P values > .09). However, rehospitalized adolescents were significantly younger (mean = 14.95 years, SD = 1.32) than those who were not (mean = 15.70 years, SD = 1.48) (t163= 2.14, P= .034, Hedges’ g= 0.51). The clinical characteristics of the sample, stratified by readmission status, are presented in Table 1.
Table 1.
Clinical Characteristics of the Sample, Stratified by Rehospitalization Status
| Characteristic | Admission Status
|
χ2/ta | Pa | Hedges’ ga | |
|---|---|---|---|---|---|
| Single Admission (n = 145) | Rehospitalized (n = 20) | ||||
| Length of stay, mean (SD) | 13.19 (4.03) | 13.30 (4.24) | −0.11 | .912 | −0.03 |
| No. of diagnoses, mean (SD) | 3.29 (1.69) | 3.90 (2.15) | −1.46 | .146 | −0.34 |
| Comorbidity, n (%) | |||||
| Separation anxiety | 6 (4.10) | 2 (10.00) | 1.31 | .253 | |
| Social anxiety | 48 (33.10) | 8 (40.00) | 0.37 | .541 | |
| Specific phobia | 8 (5.50) | 1 (5.00) | 0.01 | .924 | |
| Panic | 44 (30.30) | 7 (35.00) | 0.18 | .673 | |
| GAD | 68 (46.90) | 14 (70.00) | 3.75 | .053 | |
| OCD | 15 (10.30) | 1 (5.00) | 0.57 | .449 | |
| PTSD | 33 (22.80) | 5 (25.00) | 0.05 | .823 | |
| ADHD | 41 (28.30) | 6 (30.00) | 0.03 | .873 | |
| Substance useb | 11 (7.60) | 0 (0.00) | 1.63 | .202 | |
| Eating disordersc | 7 (4.80) | 3 (15.00) | 3.19 | .074 | |
| Conduct disorder and/or oppositional defiant disorder | 4 (2.80) | 0 (0.00) | 0.57 | .452 | |
| NSSI, n (%) | |||||
| NSSI thoughts | 101 (71.10) | 20 (100.00) | 7.73 | .005 | |
| NSSI behaviors | 83 (58.50) | 19 (95.00) | 10.04 | .002 | |
| Suicidality, n (%) | |||||
| Suicidal ideation | 111 (78.20) | 18 (90.00) | 1.51 | .219 | |
| Suicide attempts | 32 (22.50) | 3 (15.00) | 0.45 | .503 | |
| CTQ score (childhood abuse), mean (SD) | 25.46 (10.27) | 22.30 (6.78) | 1.82 | .079 | 0.32 |
| RPEQ score (peer victimization), mean (SD) | 20.72 (8.16) | 19.20 (7.08) | 0.79 | .429 | 0.19 |
| CES-D score (depression symptoms), mean (SD) | |||||
| Baseline | 34.90 (13.62) | 41.23 (10.31) | −2.00 | .048 | −0.47 |
| Discharge | 21.75 (14.19) | 25.67 (16.20) | −1.02 | .309 | −0.27 |
| SHAPS score (anhedonia symptoms), mean (SD) | |||||
| Baseline | 30.69 (7.80) | 32.31 (6.74) | −0.89 | .377 | −0.21 |
| Discharge | 26.60 (6.59) | 27.88 (7.41) | −0.72 | .476 | −0.19 |
| MASC score (anxiety symptoms), mean (SD) | |||||
| Baseline | 60.78 (18.60) | 67.75 (18.90) | −1.57 | .119 | −0.37 |
| Discharge | 57.35 (17.67) | 64.44 (18.15) | −1.50 | .135 | −0.40 |
| BHS score (hopelessness symptoms), mean (SD) | |||||
| Baseline | 10.58 (6.06) | 13.72 (4.03) | −2.98 | .006 | −0.53 |
| Discharge | 6.64 (5.31) | 5.60 (4.68) | 0.72 | .471 | 0.20 |
| RBQ-A score (risky behavior), mean (SD) | 8.47 (6.98) | 7.83 (5.16) | 0.40 | .691 | 0.10 |
Boldface values indicate statistical significance.
Alcohol and/or substance abuse or dependence.
Anorexia or bulimia nervosa.
Abbreviations: ADHD = attention-deficit/hyperactivity disorder, BHS = Beck Hopelessness Scale, CES-D = Center for Epidemiologic Studies Depression scale, CTQ = Childhood Trauma Questionnaire, GAD = generalized anxiety disorder, MASC = Multidimensional Anxiety Scale for Children, NSSI = nonsuicidal self-injury, OCD = obsessive-compulsive disorder, PTSD = posttraumatic stress disorder, RBQ-A = Risky Behavior Questionnaire for Adolescents, RPEQ = Revised Peer Experiences Questionnaire, SHAPS = Snaith-Hamilton Pleasure Scale.
Predicting Rehospitalization
Demographics
Step 1 including age, sex, and baseline depressive symptom severity was significant (n = 143, Δχ23= 12.35, P = .006). Within this step, younger age uniquely predicted a faster time to rehospitalization (β = −0.44, SE = .20, Wald1= 5.02, OR = 0.64, 95% CI = 0.44–0.95, P = .025). The addition of race and maternal/paternal education in step 2 was nonsignificant (n = 143, Δχ28= 5.89, P = .660), and none were unique predictors of rehospitalization (P values > .31).
Early life stress
Step 1 significantly improved upon the null model (n = 159, Δχ23= 9.41, P = .024), but none of the covariates uniquely predicted rehospitalization (P values > .06). Entering adoption status, total childhood abuse, and peer victimization on step 2 significantly improved the model (n = 159, Δχ23= 8.27, P= .041). However, none of the early life-stress variables uniquely predicted rehospitalization (P values > 24); only baseline depression was significant in step 2 (β = 0.05, SE = .03, Wald1= 4.07, OR = 1.05, 95% CI = 1.001–1.10, P = .044).
Diagnoses and comorbidity
Step 1 was significant (n = 165, Δχ23= 8.69, P = .034), but no covariate uniquely predicted rehospitalization (P values > .07). Step 2 including individual diagnoses and overall comorbidity was nonsignificant (n = 165, Δχ29= 9.65, P= .646), and neither the individual diagnoses nor the number of diagnoses was significant unique predictors in this step (P values > .16).
Baseline symptoms and change during treatment
Step 1 was nonsignificant (n = 133, Δχ23= 4.39, P= .222), and none of the covariates uniquely predicted rehospitalization. (P values > .15). Step 2 including baseline anhedonia, hopelessness, and anxiety was also nonsignificant (n = 133, Δχ23= 0.93, P = .819), and none of the variables uniquely predicted rehospitalization (P values > .54). Step 3 captured the change in symptoms; thus, depression, anhedonia, hopelessness, and anxiety measured at discharge were entered. The overall step was nonsignificant (n = 133, Δχ24= 7.71, P= .103), but discharge hopelessness was a significant, unique predictor of rehospitalization. Less change in hopelessness during treatment predicted a more rapid time to rehospitalization (Table 2).
Table 2.
Results of Cox Regression Survival Analysis Predicting Time to Rehospitalization From Baseline Psychiatric Symptoms and Change in Symptoms During Treatmenta
| Measure | β (SE) | Waldb | P | OR | 95% CI |
|---|---|---|---|---|---|
| Step 1 | |||||
| Age | −0.15 (0.19) | 0.64 | .423 | 0.86 | 0.59–1.24 |
| Sexc | 0.47 (0.67) | 0.49 | .486 | 1.59 | 0.43–5.89 |
| Baseline depression symptomsd | 0.04 (0.02) | 2.05 | .152 | 1.04 | 0.99–1.09 |
| Step 2 | |||||
| Age | −0.13 (0.19) | 0.43 | .512 | 0.88 | 0.60–1.29 |
| Sexc | 0.40 (0.69) | 0.33 | .563 | 1.49 | 0.39–5.76 |
| Baseline depression symptomsd | 0.02 (0.03) | 0.38 | .537 | 1.02 | 0.96–1.08 |
| Baseline anhedonia symptomse | −0.01 (0.04) | 0.02 | .889 | 0.99 | 0.91–1.08 |
| Baseline hopelessness symptomsf | 0.04 (0.06) | 0.34 | .558 | 1.04 | 0.92–1.17 |
| Baseline anxiety symptomsg | 0.01 (0.02) | 0.37 | .541 | 1.01 | 0.97–1.05 |
| Step 3 | |||||
| Age | −0.20 (0.21) | 0.94 | .331 | 0.82 | 0.55–1.23 |
| Sexc | 0.19 (0.72) | 0.07 | .796 | 1.20 | 0.29–4.95 |
| Baseline depression symptomsd | 0.01 (0.03) | 0.08 | .776 | 1.01 | 0.95–1.08 |
| Baseline anhedonia symptomse | −0.06 (0.07) | 0.82 | .365 | 0.94 | 0.82–1.08 |
| Baseline hopelessness symptomsf | 0.14 (0.08) | 3.48 | .062 | 1.15 | 0.99–1.34 |
| Baseline anxiety symptomsg | −0.01 (0.03) | 0.20 | .651 | 0.99 | 0.93–1.05 |
| Discharge depression symptomsd | 0.02 (0.03) | 0.61 | .434 | 1.02 | 0.97–1.07 |
| Discharge anhedonia symptomse | 0.08 (0.07) | 1.07 | .300 | 1.08 | 0.94–1.24 |
| Discharge hopelessness symptomsf | −0.21 (0.08) | 6.64 | .010 | 0.81 | 0.69–0.95 |
| Discharge anxiety symptomsg | 0.03 (0.03) | 0.90 | .343 | 1.03 | 0.97–1.09 |
n = 133 (15 rehospitalizations).
Boldface values indicate statistical significance.
df = 1.
Reference category = male.
Center for Epidemiologic Studies Depression scale.
Snaith-Hamilton Pleasure Scale, during treatment.
Beck Hopelessness Scale.
Multidimensional Anxiety Scale for Children Abbreviation: OR = odds ratio.
Risky behaviors, NSSI, and suicidality
Step 1 was significant (n = 144, Δχ23= 8.55, P = .036), but no covariate was uniquely associated with rehospitalization (P values > .06). The addition of suicidality, NSSI, and risky behavior engagement in step 2 significantly improved the model (n = 144, χ25= 24.93, P< .001) (Table 3). Nonsuicidal self-injury behaviors in the month prior to admission were significantly associated with a more rapid time to rehospitalization after discharge. In contrast, suicide attempts in the same time period were associated with a longer time to rehospitalization.
Table 3.
Results of Cox Regression Survival Analysis Predicting Time to Rehospitalization From Suicidality, Self-Injury, and Risky Behavior Engagementa
| Measure | β (SE) | Waldb | P | OR | 95% CI |
|---|---|---|---|---|---|
| Step 1 | |||||
| Age | −0.27 (0.18) | 2.27 | .132 | 0.77 | 0.54–1.08 |
| Sexc | 0.30 (0.59) | 0.26 | .609 | 1.35 | 0.43–4.28 |
| Baseline depression symptomsd | 0.04 (0.02) | 3.39 | .065 | 1.04 | 1.00–1.09 |
| Step 2 | |||||
| Age | −0.14 (0.21) | 0.47 | .492 | 0.87 | 0.58–1.30 |
| Sexc | −0.07 (0.70) | 0.01 | .918 | 0.93 | 0.23–3.70 |
| Baseline depression symptomsd | 0.04 (0.03) | 1.52 | .217 | 1.04 | 0.98–1.10 |
| Risky behaviorse | −0.07 (0.04) | 2.65 | .103 | 0.93 | 0.86–1.02 |
| NSSI thoughtsf | 0.02 (0.03) | 0.25 | .615 | 1.02 | 0.96–1.08 |
| NSSI behaviorsf | 0.13 (0.03) | 17.08 | < .001 | 1.14 | 1.07–1.21 |
| Suicidal ideationf | −0.06 (0.03) | 3.42 | .064 | 0.95 | 0.89–1.003 |
| Suicide attemptsf | −1.04 (0.52) | 4.02 | .045 | 0.35 | 0.13–0.98 |
n = 144 (19 rehospitalizations).
Boldface values indicate statistical significance.
df = 1.
Reference category = male.
Center for Epidemiologic Studies Depression scale.
Risky Behavior Questionnaire for Adolescents.
Self-Injurious Thoughts and Behaviors Interview.
Abbreviations: NSSI = nonsuicidal self-injury, OR = odds ratio.
Final model
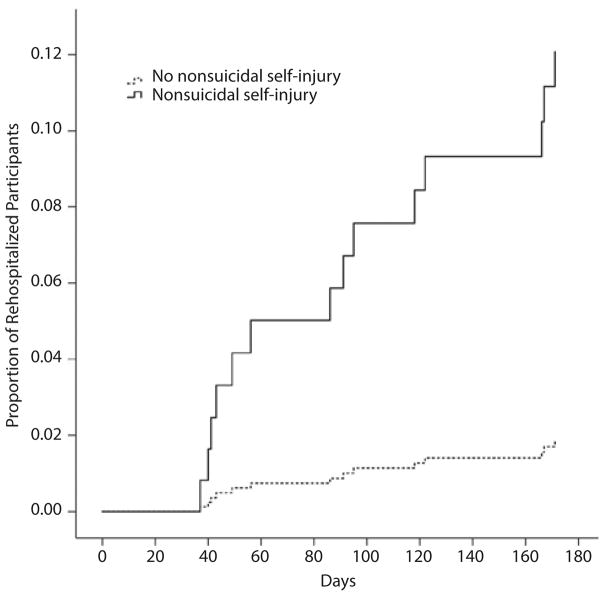
Step 1 included age, sex, and baseline depression, as well as baseline hopelessness, and was nonsignificant (n = 127, Δχ24= 4.36, P = .359), and no covariate was a significant unique predictor (P values > .31). The addition of discharge hopelessness, NSSI behaviors, and suicide attempts in step 2 was significant (n = 127, Δχ23= 8.09, P = .044) (Table 4). Only greater engagement in NSSI behavior in the month prior to hospitalization significantly predicted more rapid time to rehospitalization following discharge (Table 4); Figure 1 provides a visual depiction of this effect.
Table 4.
Results of Cox Regression Survival Analysis Predicting Time to Rehospitalization From Self-Injurious Behaviors, Risky Behavior Engagement, and Change in Hopelessness During Treatmenta
| Measure | β (SE) | Waldb | P | OR | 95% CI |
|---|---|---|---|---|---|
| Step 1 | |||||
| Age | −0.12 (0.19) | 0.36 | .548 | 0.89 | 0.61–1.30 |
| Sexc | 0.51 (0.67) | 0.57 | .452 | 1.66 | 0.45–6.17 |
| Baseline depression symptomsd | 0.03 (0.03) | 0.92 | .338 | 1.03 | 0.97–1.09 |
| Baseline hopelessness symptomse | 0.03 (0.06) | 0.34 | .559 | 1.04 | 0.92–1.16 |
| Step 2 | |||||
| Age | −0.26 (0.22) | 1.44 | .230 | 0.77 | 0.51–1.18 |
| Sexc | −0.01 (0.73) | < 0.001 | .995 | 1.00 | 0.24–4.17 |
| Baseline depression symptomsd | 0.02 (0.03) | 0.32 | .574 | 1.02 | 0.96–1.08 |
| Baseline hopelessness symptomse | 0.06 (0.07) | 0.87 | .351 | 1.07 | 0.93–1.22 |
| Discharge hopelessness symptomse | −0.09 (0.07) | 1.99 | .159 | 0.91 | 0.80–1.04 |
| NSSI behaviorsf | 0.05 (0.02) | 4.35 | .037 | 1.05 | 1.003–1.10 |
| Suicide attemptsf | −1.06 (0.95) | 1.26 | .261 | 0.35 | 0.05–2.21 |
n = 127 (14 rehospitalizations).
Boldface values indicate statistical significance.
df = 1.
Reference category = male.
Center for Epidemiologic Studies Depression scale.
Beck Hopelessness Scale.
Self-Injurious Thoughts and Behaviors Interview.
Abbreviations: NSSI = nonsuicidal self-injury, OR = odds ratio.
Figure 1.
Proportion of Adolescent Patients Who Were Rehospitalized 6 Months After Discharge, Stratified by Whether They Reported Nonsuicidal Self-Injury in the Month Prior to Admission
DISCUSSION
In view of the alarming prevalence7–9 and costs of repeated hospitilizations,14 the current study aimed to identify predictors of rehospitalization in depressed adolescents admitted to a short-term residential treatment service. Over 12% of our sample were readmitted to the same residential service within 6 months of discharge, a rate that is similar to that in previous studies.16 Across the broad range of predictors, only NSSI frequency prior to admission was significantly associated with rehospitalization.
This study is the first to report on the role of NSSI in the rehospitalization of depressed youth, and there are several important implications. First, residential care aims to stabilize symptoms and reduce suicide risk.38 At the same time, NSSI behaviors may persist after discharge,39 especially when adolescents transition to environments without 24-hour clinical care. Second, NSSI is robustly associated with suicidal thoughts and behaviors40,41; therefore, adolescents reporting more frequent baseline NSSI may be more likely to experience increased suicidality (eg, suicide plans, gestures) after discharge. Last, compared with internalizing symptoms, NSSI tends to present with more overt consequences (eg, cuts, burns), which signal distress, ultimately leading to readmission.42 In light of these results, more specialized clinical attention to NSSI behaviors in short-term treatment may be warranted.
The findings from our preliminary models should be considered exploratory and require replication in future studies. We found that less improvement in hopelessness, but not depression, anhedonia, or anxiety, during treatment predicted rehospitalization, which is consistent with previous research. Specifically, studies have shown that hopelessness is a strong marker of therapeutic nonresponse among depressed adolescent outpatients,43 and pretreatment hopelessness predicts elevated patterns of suicidality following discharge for adolescent patients and higher rates of rehospitalization.44 In preliminary analyses, but not in the final model, we found that more frequent suicide attempts in the month prior to hospitalization was associated with a longer time to rehospitalization. This counterintuitive effect may have been due to adolescents’ with recent suicide attempts receiving more intensive posthospitalization treatment, reducing risk of rehospitalization. Surprisingly, we found that neither a history of childhood abuse nor suicidal ideation was associated with time to rehospitalization, which is inconsistent with previous studies.8,15 These contradictory findings may be due to our recruitment of a homogeneous sample of depressed adolescents, and these factors should be further examined in a more heterogeneous sample of adolescent inpatients.
Results should be considered in light of the following limitations. First, we only assessed readmissions to the same short-term residential service to which participants were originally admitted. Therefore, the study may underestimate the rate of total rehospitalization. Second, we did not measure NSSI or suicidality at discharge and therefore could not test their effects on rehospitalization. Relatedly, we did not assess the longitudinal course of symptoms, and some research has indicated that a stable, elevated rate of suicidal ideation following hospitalization predicts rehospitalization among adolescent patients.44 Third, our sample had a relatively high level of parental education, which reflects the demographic of the greater Boston area. Future studies should examine the generalizability of our findings. Fourth, we did not record the data on the treatment participants may have received during the follow-up period, which may have also impacted the likelihood of rehospitalization. Last, our measures relied on clinical interviews and self-report instruments. This introduces the possibility of response biases.
In sum, our findings highlight the importance of more effectively managing self-injury during treatment and in discharge planning, as this is strongly associated with later rehospitalization. An improved understanding of factors that predict readmission will help clinicians identify adolescents at highest risk, which may guide effective treatment.
Acknowledgments
Funding/support: This study was partially supported through funding from National Institute of Mental Health (K23MH097786), the Klingenstein Third Generation Foundation Adolescent Depression Fellowship, the Tommy Fuss Fund, and the Simches Fund.
Role of the sponsor: The funding organizations had no role in the design or conduct of the study.
Footnotes
Including length of treatment as a covariate in our Cox regression analyses did not alter the pattern of our results, and length of treatment was a nonsignificant predictor in all models.
Although some of our models included identical step 1 predictors of the same outcome variable (time to rehospitalization), results nonetheless differed across models due to different patterns of missing data in the primary predictor variables.
Potential conflicts of interest: The authors declare no competing interests.
References
- 1.Avenevoli S, Swendsen J, He J-P, et al. Major depression in the national comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry. 2015;54(1):37–44. e2. doi: 10.1016/j.jaac.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Essau CA. Frequency and patterns of mental health services utilization among adolescents with anxiety and depressive disorders. Depress Anxiety. 2005;22(3):130–137. doi: 10.1002/da.20115. [DOI] [PubMed] [Google Scholar]
- 3.Auerbach RP, Kim JC, Chango JM, et al. Adolescent nonsuicidal self-injury: examining the role of child abuse, comorbidity, and disinhibition. Psychiatry Res. 2014;220(1–2):579–584. doi: 10.1016/j.psychres.2014.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Auerbach RP, Millner AJ, Stewart JG, et al. Identifying differences between depressed adolescent suicide ideators and attempters. J Affect Disord. 2015;186:127–133. doi: 10.1016/j.jad.2015.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balkin RS. A reexamination of trends in acute care psychiatric hospitalization for adolescents: Ethnicity, payment, and length of stay. J Professional Counseling: Pract, Theory, Res. 2006;34(1–2):49–59. [Google Scholar]
- 6.Bettmann JE, Jasperson RA. Adolescents in residential and inpatient treatment: A review of the outcome literature. Child Youth Care Forum. 2009;38(4):161–183. [Google Scholar]
- 7.Barker D, Jairam R, Rocca A, et al. Why do adolescents return to an acute psychiatric unit? Australas Psychiatry. 2010;18(6):551–555. doi: 10.3109/10398562.2010.501380. [DOI] [PubMed] [Google Scholar]
- 8.Fontanella CA. The influence of clinical, treatment, and healthcare system characteristics on psychiatric readmission of adolescents. Am J Orthopsychiatry. 2008;78(2):187–198. doi: 10.1037/a0012557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.James S, Charlemagne SJ, Gilman AB, et al. Post-discharge services and psychiatric rehospitalization among children and youth. Adm Policy Ment Health. 2010;37(5):433–445. doi: 10.1007/s10488-009-0263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bardach NS, Coker TR, Zima BT, et al. Common and costly hospitalizations for pediatric mental health disorders. Pediatrics. 2014;133(4):602–609. doi: 10.1542/peds.2013-3165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moses T. Adolescents’ perspectives about brief psychiatric hospitalization: what is helpful and what is not? Psychiatr Q. 2011;82(2):121–137. doi: 10.1007/s11126-010-9151-1. [DOI] [PubMed] [Google Scholar]
- 12.Romansky JB, Lyons JS, Lehner RK, et al. Factors related to psychiatric hospital readmission among children and adolescents in state custody. Psychiatr Serv. 2003;54(3):356–362. doi: 10.1176/appi.ps.54.3.356. [DOI] [PubMed] [Google Scholar]
- 13.Noyola N, Sorgi K, Alday CS, et al. Clinical judgment at work: predicting rehospitalization in an adolescent inpatient unit. Brown Univ Child Adolesc Behav Lett. 2014;30(6):1–6. [Google Scholar]
- 14.Chung W, Edgar-Smith S, Palmer RB, et al. Psychiatric rehospitalization of children and adolescents: implications for social work intervention. Child Adolesc Social Work J. 2008;25(6):483–496. [Google Scholar]
- 15.Bobier C, Warwick M. Factors associated with readmission to adolescent psychiatric care. Aust N Z J Psychiatry. 2005;39(7):600–606. doi: 10.1080/j.1440-1614.2005.01632.x. [DOI] [PubMed] [Google Scholar]
- 16.Arnold EM, Goldston DB, Ruggiero A, et al. Rates and predictors of rehospitalization among formerly hospitalized adolescents. Psychiatr Serv. 2003;54(7):994–998. doi: 10.1176/appi.ps.54.7.994. [DOI] [PubMed] [Google Scholar]
- 17.Fontanella CA, Zuravin SJ, Burry CL. The effect of a Medicaid managed care program on patterns of psychiatric readmission among adolescents: evidence from Maryland. J Behav Health Serv Res. 2006;33(1):39–52. doi: 10.1007/s11414-005-9004-0. [DOI] [PubMed] [Google Scholar]
- 18.Miller BC, Fan X, Grotevant HD, et al. Adopted adolescents’ overrepresentation in mental health counseling: adoptees’ problems or parents’ lower threshold for referral? J Am Acad Child Adolesc Psychiatry. 2000;39(12):1504–1511. doi: 10.1097/00004583-200012000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Blader JC. Symptom, family, and service predictors of children’s psychiatric rehospitalization within one year of discharge. J Am Acad Child Adolesc Psychiatry. 2004;43(4):440–451. doi: 10.1097/00004583-200404000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Consoli A, Cohen D, Bodeau N, et al. Risk and protective factors for suicidality at 6-month follow-up in adolescent inpatients who attempted suicide: an exploratory model. Can J Psychiatry. 2015;60(suppl 1):S27–S36. [PMC free article] [PubMed] [Google Scholar]
- 21.Nilsen TS, Eisemann M, Kvernmo S. Predictors and moderators of outcome in child and adolescent anxiety and depression: a systematic review of psychological treatment studies. Eur Child Adolesc Psychiatry. 2013;22(2):69–87. doi: 10.1007/s00787-012-0316-3. [DOI] [PubMed] [Google Scholar]
- 22.ten Doesschate MC, Bockting CL, Koeter MW, et al. DELTA Study Group. Prediction of recurrence in recurrent depression: a 5.5-year prospective study. J Clin Psychiatry. 2010;71(8):984–991. doi: 10.4088/JCP.08m04858blu. [DOI] [PubMed] [Google Scholar]
- 23.Paykel ES. Partial remission, residual symptoms, and relapse in depression. Dialogues Clin Neurosci. 2008;10(4):431–437. doi: 10.31887/DCNS.2008.10.4/espaykel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Auerbach RP, Tsai B, Abela JR. Temporal relationships among depressive symptoms, risky behavior engagement, perceived control, and gender in a sample of adolescents. J Res Adolesc. 2010;20(3):726–747. [Google Scholar]
- 25.Barrocas AL, Giletta M, Hankin BL, et al. Nonsuicidal self-injury in adolescence: longitudinal course, trajectories, and intrapersonal predictors. J Abnorm Child Psychol. 2015;43(2):369–380. doi: 10.1007/s10802-014-9895-4. [DOI] [PubMed] [Google Scholar]
- 26.American Psychiatric Association. Diagnostic and Statistical Manual for Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- 27.Sheehan DV, Sheehan KH, Shytle RD, et al. Reliability and validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID) J Clin Psychiatry. 2010;71(3):313–326. doi: 10.4088/JCP.09m05305whi. [DOI] [PubMed] [Google Scholar]
- 28.Nock MK, Holmberg EB, Photos VI, et al. Self-Injurious Thoughts and Behaviors Interview: development, reliability, and validity in an adolescent sample. Psychol Assess. 2007;19(3):309–317. doi: 10.1037/1040-3590.19.3.309. [DOI] [PubMed] [Google Scholar]
- 29.Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 30.Prinstein MJ, Boergers J, Vernberg EM. Overt and relational aggression in adolescents: social-psychological adjustment of aggressors and victims. J Clin Child Psychol. 2001;30(4):479–491. doi: 10.1207/S15374424JCCP3004_05. [DOI] [PubMed] [Google Scholar]
- 31.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 32.March JS, Parker JD, Sullivan K, et al. The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry. 1997;36(4):554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- 33.Snaith RP, Hamilton M, Morley S, et al. A scale for the assessment of hedonic tone the Snaith-Hamilton Pleasure Scale. Br J Psychiatry. 1995;167(1):99–103. doi: 10.1192/bjp.167.1.99. [DOI] [PubMed] [Google Scholar]
- 34.Leventhal AM, Unger JB, Audrain-McGovern J, et al. Measuring anhedonia in adolescents: a psychometric analysis. J Pers Assess. 2015;97(5):506–514. doi: 10.1080/00223891.2015.1029072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beck AT, Weissman A, Lester D, et al. The measurement of pessimism: the Hopelessness Scale. J Consult Clin Psychol. 1974;42(6):861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- 36.Auerbach RP, Gardiner CK. Moving beyond the trait conceptualization of self-esteem: the prospective effect of impulsiveness, coping, and risky behavior engagement. Behav Res Ther. 2012;50(10):596–603. doi: 10.1016/j.brat.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 37.Cohen J, Cohen P, West SG, et al. Applied Multiple Correlation/Regression Analysis for the Behavioral Sciences. 3. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 2003. [Google Scholar]
- 38.Balkin RS, Roland CB. Reconceptualizing stabilization for counseling adolescents in brief psychiatric hospitalization: a new model. J Couns Dev. 2007;85(1):64–72. [Google Scholar]
- 39.Asarnow JR, Porta G, Spirito A, et al. Suicide attempts and nonsuicidal self-injury in the treatment of resistant depression in adolescents: findings from the TORDIA study. J Am Acad Child Adolesc Psychiatry. 2011;50(8):772–781. doi: 10.1016/j.jaac.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Giletta M, Prinstein MJ, Abela JR, et al. Trajectories of suicide ideation and nonsuicidal self-injury among adolescents in mainland China: peer predictors, joint development, and risk for suicide attempts. J Consult Clin Psychol. 2015;83(2):265–279. doi: 10.1037/a0038652. [DOI] [PubMed] [Google Scholar]
- 41.Hamza CA, Stewart SL, Willoughby T. Examining the link between nonsuicidal self-injury and suicidal behavior: a review of the literature and an integrated model. Clin Psychol Rev. 2012;32(6):482–495. doi: 10.1016/j.cpr.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 42.Nock MK, Prinstein MJ. A functional approach to the assessment of self-mutilative behavior. J Consult Clin Psychol. 2004;72(5):885–890. doi: 10.1037/0022-006X.72.5.885. [DOI] [PubMed] [Google Scholar]
- 43.Birmaher B, Brent DA, Kolko D, et al. Clinical outcome after short-term psychotherapy for adolescents with major depressive disorder. Arch Gen Psychiatry. 2000;57(1):29–36. doi: 10.1001/archpsyc.57.1.29. [DOI] [PubMed] [Google Scholar]
- 44.Czyz EK, King CA. Longitudinal trajectories of suicidal ideation and subsequent suicide attempts among adolescent inpatients. J Clin Child Adolesc Psychol. 2015;44(1):181–193. doi: 10.1080/15374416.2013.836454. [DOI] [PMC free article] [PubMed] [Google Scholar]