Abstract
Purpose
Parathyroid adenoma detection with dual-phase 99mTc-sestamibi (MIBI) scintigraphy depends on differential MIBI washout from thyroid. However, autoimmune thyroid disease (AITD) may cause MIBI to be retained in the thyroid gland and reduce parathyroid detection. We evaluated the impact of AITD on MIBI thyroid retention and additional benefit of SPECT/CT in these patients.
Methods
Dual phase planar MIBI and SPECT/CT was performed on 82 patients. SPECT/CT was performed immediately after delayed planar scan. Thyroid density (Hounsfield unit, CT-HU) and size were measured on CT component of SPECT/CT. MIBI uptake in early scans and retention in delayed scans were visually graded and correlated with clinical factors and CT findings. Finally, planar and SPECT/CT findings were compared for parathyroid lesion visualization according to thyroid MIBI retention.
Results
In early scan, multivariate analysis showed only thyroid size predicted early uptake. In delayed scan, multivariate analysis showed higher visual grade in early scan, lower CT-HU or AITD were significant predictors for delayed thyroid parenchymal retention. Overall, ten more parathyroid lesions were visualized on SPECT/CT compared to planar scans (57 vs. 47, p = 0.002). SPECT/CT was especially more useful in patients with thyroidal MIBI retention, as eight out of the ten additional lesions detected were found in patients with thyroid MIBI retention.
Conclusion
AITD is an important factor for MIBI thyroid parenchymal retention on delayed scans, and may impede parathyroid lesion detection. Patients with MIBI retention in the thyroid parenchyma on delayed scans are likely to benefit from an additional SPECT/CT.
Keywords: Autoimmune thyroid disease, 99mTc-sestamibi scintigraphy, SPECT/CT, Parathyroid
Introduction
Accurate preoperative localization of parathyroid adenomas or hyperplasia has gained in importance as more patients opt for minimally invasive parathyroid surgery. Compared to other conventional imaging modalities such as ultrasonogram (US), computed tomography (CT), and magnetic resonance (MR), 99mTc-2-methoxy-2-methylpropyl isonitrile (99mTc-sestamibi, MIBI) parathyroid scintigraphy has been shown to have higher sensitivity in detecting parathyroid adenomas [1, 2]. In addition, the anatomical information provided by single positron emission computed tomography/computed tomography (SPECT/CT) has improved the detection and localization of parathyroid lesions compared to planar scans alone [3, 4].
Parathyroid visualization using dual phase parathyroid scintigraphy protocol relies on differential washout of MIBI from the thyroid parenchyma with parathyroid lesion retention on delayed planar images [5]. However, previous studies have shown that MIBI is not equally washed out from the thyroid gland for all patients on delayed images; focal thyroid disease or amiodarone induced thyrotoxicosis has been reported to be a factor for MIBI retention in the thyroid gland [6, 7]. Few studies have attempted to evaluate factors of MIBI retention in the thyroid gland, and its impact on parathyroid lesion detection. We underwent this study to evaluate the usefulness of SPECT/CT in evaluating parathyroid lesion detection in patients with thyroid parenchymal diseases.
The thyroid gland has the unique characteristic of high attenuation in non-contrast CT scan due to its high iodine content [8, 9]. Previous reports have shown that iodine content decreases in autoimmune thyroid diseases (AITD), such as Graves’ disease or Hashimoto thyroiditis, which can be reliably detected with non-contrast CT [10–12]. The purpose of this study was to correlate clinical and imaging findings with MIBI retention in the thyroid gland, and to evaluate the additional benefit of SPECT/CT in parathyroid lesion detection in patients with thyroidal MIBI retention.
Materials and Methods
Patients
We retrospectively reviewed hospital records of 86 patients who were referred for dual phase MIBI parathyroid scintigraphy with SPECT/CT from November 2012 to May 2014 for elevated parathyroid hormone (PTH) and/or serum calcium levels. We excluded four patients who previously underwent previous thyroidectomy before MIBI scan. Finally, 82 patients were included in this study. Of these, 40 patients had undergone surgical exploration. All initial PTH levels were obtained within 1 month of MIBI scintigraphy. All patients underwent ultrasonogram for evaluation of parathyroid lesions, and ultrasonogram scans was retrospectively reviewed by an experienced radiologist specialized in thyroid, and radiologic findings of diffuse thyroid parenchymal disease were recorded. AITD was considered when patients had ultrasonogram findings of diffuse thyroid parenchymal disease and positive serum antithyroid autoantibodies or thyroid hormones levels indicative of primary hyper/hypothyroidism [13]. The institutional review board approved this study and informed consent was waived for this retrospective study.
Imaging Protocol
All patients were injected intravenously with 740 MBq ± 20 MBq of MIBI. Early and planar delayed images were acquired at 10 min and 2 h after radiotracer injection, and multiple planar images were obtained: anterior, 20° right anterior oblique, and 20° left anterior oblique using a Symbia TruePoint SPECT/CT (Siemens Healthcare, Knoxville, TN, USA). Immediately after delayed planar imaged scan, we obtained SPECT and CT images, and CT images were obtained at 5 mm slice thickness, voltage of 110 kV, and current of 42 mA, with 512 × 512 matrix using standard filter. SPECT images of the neck were acquired into 1.78× zoom, 128 × 128 matrix with step and shoot scan mode (32 frameset, 25 s per frame, and 5.5° angles). SPECT image reconstruction was performed with CT based attenuation correction and a Hanning 3-dimensional post-filter (cut-off frequency, 0.85 cycles/cm), with a 3D Flash iterative reconstruction (eight subsets and eight iterations). The SPECT acquisition took approximately 14 min, whereas the CT acquisition took approximately 10–20 s.
Imaging Analysis
All planar images were retrospectively reviewed on dedicated Syngo workstation (Siemens, VA60A software) by two experienced nuclear medicine physicians separately, and differences in opinion were resolved by consensus. In planar image analysis, thyroid gland uptake in early planar images were visually graded into three groups (E1: MIBI uptake lower than the salivary gland, E2: MIBI uptake similar to the salivary gland, and E3: higher uptake than the salivary gland) (Fig. 1a–c). The delayed planar images were visually categorized into two groups (D0: thyroid washout group, no thyroid parenchyma visualization, and D1: thyroid retention group, thyroid parenchymal visualization) (Fig. 1d–e). Patients were grouped according to early uptake and delayed washout patterns.
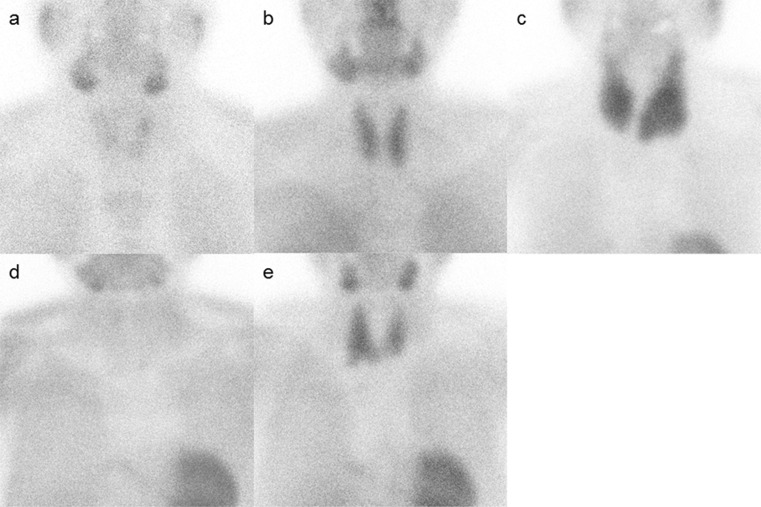
Fig. 1.
Representative cases of MIBI uptake and retention patterns of the thyroid in early and delayed planar images. Early scans were graded into three grades (a = E1, low; b = E2, moderate; c = E3, high) and delayed scans were graded in two grades (d = D0, thyroid washout; e = D1, thyroid retention)
In CT scan image analysis, the Hounsfield units values of the thyroid glands was measured by drawing three circular region of interests (ROI) and recording the average of the mean value of each Hounsfield unit (CT-HU). Thyroid gland size (CT size) were calculated by semiautomatically drawing an ROI manually around the thyroid parenchyma on each axial CT scan image and automatically calculated thyroid size using AW workstation (AW 4.4, GE Healthcare, Milwaukee, WI, USA).
Finally, SPECT/CT scans were reviewed for parathyroid visualization. SPECT/CT scans were reviewed by the same two nuclear medicine physicians who were blinded to the planar findings and other clinical factors. Positive parathyroid lesion visualization was defined as nodular uptake higher than thyroid parenchyma in the parathyroid lesion seen on CT component of SPECT/CT. Differences in opinion were resolved by consensus.
Statistical Analysis
Chi-square test was performed to evaluate correlation between early uptake with retention in delayed images. Univariate linear regression analysis was performed to evaluate the relationship between visual grade (E1, E2, and E3) from clinical factors (age, sex, AITD, PTH, and serum calcium level) and CT factors (CT-HU, and CT size). Multivariate analysis was performed on the statistically significant factors in univariate analysis. For delayed images, univariate logistic regression analysis of the same clinical and CT factors as well as early scan MIBI uptake (E1, E2, and E3) was used to predict MIBI retention at 2 h delayed images (D1, and D2). Receiver operating characteristic (ROC) curve analysis was performed to determine the CT-HU cut-off values with the highest sensitivity in predicting MIBI retention at delayed images. Multivariate analysis was performed on the statistically significant factors in univariate analysis. McNemar’s test was performed to compared parathyroid lesion detection for planar and SPECT/CT according to thyroid MIBI retention. Furthermore, subgroup analysis was performed in patients who underwent surgical exploration to compared pathologically confirmed parathyroid lesions detection according to thyroid MIBI retention using McNemar’s test. Software used to perform these analyses was SPSS 20.0 (IBM Corp., Armonk, NY, USA). Statistical significance was defined by a p value <0.05 for all statistical analysis.
Results
Patient Characteristics
A total of 82 patients (58 female; overall mean age 53.0 ± 13.4 years old, range 23–81) were included in this study. All patients had elevated PTH levels (414.6 ± 612.4 pg/ml, normal range 15–65 pg/ml). Serum calcium levels were elevated in 35 patients (10.5 ± 1.5 mg/dl, range 7.9-17.2 mg/dl, normal range 8.5-10.5 mg/dl). Ultrasonogram findings of diffuse thyroid parenchymal disease were seen in 36 patients (43.9 %) and 42 patients (51.2 %) showed positive serum antithyroid autoantibodies or primary hyper/hypothyroidism. A total of 21 (25.6 %) patients were positive in both studies, and considered to have AITD. Table 1 shows demographics of study population.
Table 1.
Patient demographics and MIBI thyroid parenchyma retention patterns
| Early scan | Delayed scan | ||||
|---|---|---|---|---|---|
| Low (E1) | Moderate (E2) | High (E3) | Washout (D0) | Retention (D1) | |
| E1 washout n (%) | 20 | 16 (80.0 %) | 4 (20.0 %) | ||
| E2 washout n (%) | 50 | 27 (54.0 %) | 23 (46.0 %) | ||
| E3 washout n (%) | 12 | 0 (0 %) | 12 (100 %) | ||
| Mean HU† | 107.3 ± 24.6 | 100.0 ± 20.7 | 91.3 ± 20.5 | 110.2 ± 19.6 | 89.8 ± 19.4 |
| CT size (cm3) | 14.3 ± 6.5 | 18.1 ± 10.5 | 33.2 ± 24.6 | 14.6 ± 5.9 | 24.6 ± 18.0 |
| Age (years) | 50.3 ± 14.5 | 53.0 ± 13.1 | 57.8 ± 12.3 | 50.6 ± 14.1 | 55.7 ± 12.1 |
| PTH (ng/ml) | 448.3 ± 499.6 | 446.5 ± 711.3 | 225.3 ± 174.8 | 485.0 ± 716.8 | 336.8 ± 468.7 |
| Serum calcium (mg/dl) | 10.2 ± 1.4 | 10.5 ± 1.5 | 10.9 ± 1.5 | 10.3 ± 1.2 | 10.6 ± 1.7 |
| AITD‡ (yes:no) | 5:15 | 10:40 | 6:6 | 5:38 | 16:23 |
| Sex (female:male) | 15:5 | 33:17 | 10:2 | 31:12 | 27:12 |
HU† = Hounsfield unit; AITD‡ = autoimmune thyroid disease
Continuous values are in mean value ± SD
Factors for MIBI Uptake in Early Scans and Retention in Delayed Scan
Visual analysis of thyroid uptake and retention showed that higher MIBI uptake on early planar images was correlated with increased retention on delayed planar images (p < 0.001, chi-squared test for trend) (Table 1). Most patients with low early thyroid uptake (E1, n = 20) predominately showed no retention on delayed scans (D0 = 16 patients, 80.0 %; D1 = 4 patient, 20.0 %). Patients that showed moderate early thyroid uptake (E2, n = 50) showed similar proportion of washout or retention pattern on delayed scans (D0 = 27 patients, 54.0 %; D1 = 23 patients, 46.0 %). All patients with high early thyroid uptake (E3, n = 12) showed retention on delayed images (D1 = 12, 100 %).
Univariate linear regression analysis for clinical factors (age, sex, AITD, PTH, and serum calcium level) and CT factors (CT size, and CT-HU) contributing to higher uptake during early scan showed that larger CT size (p < 0.001), and lower CT-HU (p = 0.044) were significant predictors of higher uptake at early scan. Clinical factors such as age, sex, AITD, PTH, and serum calcium level were not significantly correlated with uptake in early scans (p = 0.134, p = 0.799, p = 0.195, p = 0.392, and p = 0.247, respectively). Multivariate analysis showed that only CT size was significant for higher uptake in early scans (p = 0.001) (Table 2).
Table 2.
Univariate and multivariate analysis in the prediction of MIBI thyroid parenchyma retention on early and delayed scans
| Early scan | ||||||
| Factors | Univariate | Multivariate | ||||
| B (95 % CI†) | p-value | B (95 % CI) | p-value | |||
| CT size | 0.017 (0.008–0.026) | <0.001* | 0.016 (0.006–0.025) | 0.001* | ||
| CT-HU | −0.006 (−0.012–−0.001) | 0.044* | −0.004 (−0.010–0.001) | 0.134 | ||
| Age | 0.008 (−0.002–0.018) | 0.134 | ||||
| Sex (male reference) | 0.039 (−0.264–0.340) | 0.799 | ||||
| AITD‡ | 0.216 (−0.116–0.507) | 0.195 | ||||
| PTH | 0.000 (0.000–0.000) | 0.392 | ||||
| Serum calcium | 0.054 (−0.038–0.147) | 0.247 | ||||
| Delayed scan | ||||||
| Factors | Univariate | Multivariate model 1 | Multivariate model 2 | |||
| OR§ (95 % CI) | p-value | OR (95 % CI) | p-value | OR (95 % CI) | p-value | |
| Early scan | 7.122 (2.473–20.515) | <0.001* | 11.365 (2.727–47.375) | 0.001* | 7.130 (2.092–24.300) | 0.002* |
| CT size | 1.089 (1.032–1.150) | 0.002* | 1.064 (0.984–1.151) | 0.119 | 1.066 (0.998–1.139) | 0.057 |
| CT-HUcat║ | 9.867 (3.360–28.971) | <0.001* | 20.102 (4.339–93.122) | <0.001* | ||
| Age | 1.030 (0.996–1.066) | 0.085 | ||||
| Sex (male reference) | 0.871 (0.336–2.257) | 0.776 | ||||
| AITD | 5.287 (1.708–16.364) | 0.004* | 6.076 (1.432–25.787) | 0.014* | ||
| PTH | 1.000 (0.999–1.000) | 0.285 | ||||
| Serum calcium | 1.177 (0.866–1.600) | 0.297 | ||||
CI† = confidence interval; AITD‡ = autoimmune thyroid disease; OR§ = odds ratio; CT-HUcat║ = CT-HU categorized by 92.6 Hounsfield unit (HU) cut-off
*statistically significant
ROC analysis for CT-HU showed a cut–off of 92.6 as highly specific (86.1 %) in detecting retention on delayed images (area under the curve: 0.782, 95 % confidence interval 0.677–0.866, p < 0.001). Univariate analysis of factors contributing to MIBI retention in delayed scan showed that larger CT size, lower CT-HU, AITD, and higher intensity in early scans were significant predictors for increased retention on delayed scans (p = 0.002, p < 0.001, p = 0.004, and p < 0.001, respectively). Age, sex, PTH, and serum calcium level were not significant for retention on delayed scans (p = 0.085, p = 0.776, p = 0.285, and p = 0.297, respectively). Two models for logistic multivariate analysis were done to evaluate for MIBI retention on delayed scans due to the multi-collinearity between CT-HU and AITD. Model 1 showed that patients with low CT-HU (odds ratio (OR) = 20.102, CI = 4.339–93.122, p < 0.001) and higher retention on early scans (OR = 11.365, CI = 2.727–47.375, p = 0.001) significantly predicted retention of delayed scans, but CT size did not (p = 0.119). Model 2 showed that both early uptake on early scans (OR = 7.130, CI = 2.092–24.300, p = 0.002) and AITD (OR = 6.076, CI = 1.432–25.787, p = 0.014) significantly predicted retention on delayed scans (Table 2).
Comparison of SPECT/CT and Planar Scans in Parathyroid Pathology Detection According to Thyroid MIBI Retention
To determine the effect of MIBI retention in the thyroid gland in visualizing parathyroid lesions at the thyroid bed, delayed scans and SPECT/CT scans were reviewed and parathyroid lesion visibility was analyzed. SPECT/CT significantly detected more parathyroid lesions compared to planar scans (McNemar test, p = 0.002). Overall, 57 lesions were seen on delayed planar scans, which were all seen on SPECT/CT. Additionally, ten more lesions were seen on SPECT/CT. Twenty-five patients had no parathyroid lesions seen on both planar and SPECT/CT scans.
Finally, comparison between planar and SPECT/CT in parathyroid lesion detection according to thyroid MIBI retention was performed. In patients with thyroid MIBI washout (D0 group, 43/82, 52.4 %), there was no significant difference between SPECT/CT and planar scans in parathyroid lesion detection (McNemar test p = 0.500, Table 3). Planar scans detected 35 patients, whereas SPECT/CT detected 37 patients. Both scans did not detect parathyroid lesions in six patients.
Table 3.
Comparison between delayed planar scan and SPECT/CT in parathyroid visibility according to MIBI thyroid parenchymal retention
| Thyroid retention | Parathyroid pathology visualization | ||||
|---|---|---|---|---|---|
| D0 (thyroid washout, n = 43) | SPECT/CT | p-value* | |||
| Delayed planar scan | Not visualized | Visualized | 0.500 | ||
| Not visualized | 6 | 2 | |||
| Visualized | 0 | 35 | |||
| D1 (thyroid retention, n = 39) | SPECT/CT | p-value* | |||
| Delayed planar scan | Not visualized | Visualized | 0.008 | ||
| Not visualized | 19 | 8 | |||
| Visualized | 0 | 12 | |||
*McNemar test
In the thyroid MIBI retention patients (D1 group, 39/82, 47.6 %), SPECT/CT detected significantly more parathyroid lesions compared to planar scans (McNemar test p = 0.008, Table 3). Planar scans detected only 12 parathyroid patients, whereas SPECT/CT detected 20 parathyroid patients. Overall, eight more patients were detected using SPECT/CT compared to planar scans in the D1 group. Figure 2 shows representative cases where thyroid parenchymal MIBI retention can lower the sensitivity of parathyroid adenoma visibility. Note the mild MIBI uptake in the parathyroid hyperplasia in Fig. 2b, which is not much higher than the MIBI retention in the thyroid seen in Fig. 2g.
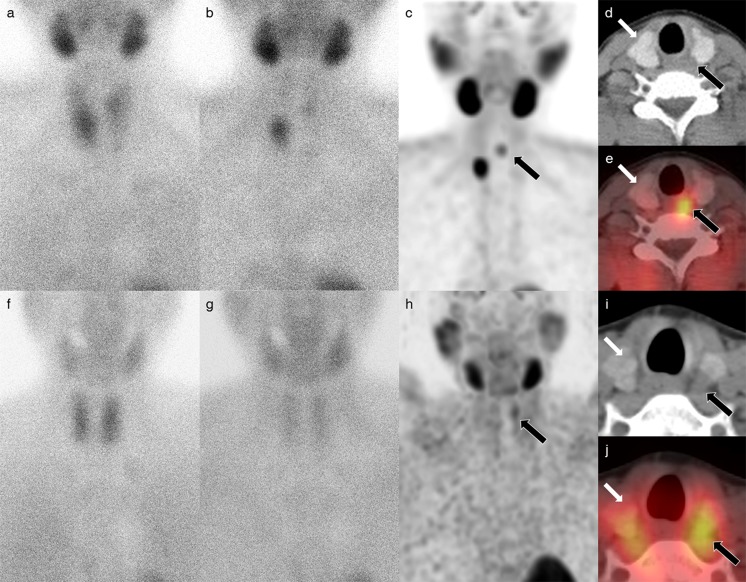
Fig. 2.
Representative cases of parathyroid visualization according to MIBI retention in thyroid parenchyma. a–e A 26-year-old female patient with parathyroid lesion visualization on delayed scans after washout from thyroid parenchyma (a). Early scan showed mild thyroid uptake (E1) (b). Delayed scan shows thyroid washout (D0), resulting in two nodular lesions corresponding to parathyroid lesions (c–e). No additional benefit in lesion detection on SPECT/CT. Black arrow indicates parathyroid lesion, and white arrow indicates minimal MIBI retention in the normal thyroid parenchyma (HU = 145.9). Final pathology was parathyroid hyperplasia in both parathyroid lesions. f–j A 53-year-old female patient with thyroid MIBI retention, resulting in parathyroid lesion visualization only on SPECT/CT (f). Early scan showed high uptake (E3) (g). Delayed scan shows thyroid retention (D1). No parathyroid lesion was detected on planar scans (h–j). Detection of parathyroid lesion on SPECT/CT only. Black arrow shows parathyroid adenoma clearly seen on MIP and SPECT/CT fusion images. White arrow depicts MIBI retention in the thyroid gland (HU = 96.3). Final pathology was parathyroid adenoma
Subgroup analysis was performed for 18 patients in thyroid washout group (D0) and 22 patients in thyroid retention group (D1) who underwent surgical exploration. A total of 40 lesions were pathologically confirmed in D0 group, and 45 lesions in D1 group. In patients with thyroid MIBI washout group, planar scans detected 28 lesions (sensitivity per lesion, 70.0 %) and SPECT/CT scan detected 34 lesions (sensitivity per lesion, 85.0 %) (McNemar test, p = 0.031, Table 4). In the thyroid MIBI retention groups, planar scans detect 26 lesions (sensitivity per lesion, 57.8 %), whereas SPECT/CT detected 36 lesions (sensitivity per lesion, 80.0 %) (McNemar test, p = 0.002, Table 4).
Table 4.
Comparison between delayed planar scan and SPECT/CT in parathyroid visibility according to MIBI thyroid parenchymal retention for pathologically confirmed parathyroid lesions
| Thyroid retention | Pathologically confirmed parathyroid pathology visualization | ||||
|---|---|---|---|---|---|
| D0 (thyroid washout, 18 patients, 40 lesions) | SPECT/CT | p-value* | |||
| Delayed planar scan | Not visualized | Visualized | 0.031 | ||
| Not visualized | 6 | 6 | |||
| Visualized | 0 | 28 | |||
| D1 (thyroid retention, 22 patients, 45 lesions) | SPECT/CT | p-value* | |||
| Delayed planar scan | Not visualized | Visualized | 0.002 | ||
| Not visualized | 9 | 10 | |||
| Visualized | 0 | 26 | |||
*McNemar test
Discussion
We have shown in our study that MIBI is retained in AITD patients compared to patients without AITD. We have also shown that the non-contrast CT component of SPECT/CT is useful in predicting MIBI retention. Due to the high iodine content of the thyroid parenchyma, the thyroid gland can be well visualized on non-contrast CT (average HU of 107.0 ± 18.3), whereas AITD such as Graves’ disease and Hashimoto’s thyroiditis has lower iodine concentrations on pathology, which is reflected as lower iodine content on non-contrast CT (average HU of 81.6 ± 21.0) [9, 11, 12]. Taillefer et al. initially introduced the dual phase, single isotope method using MIBI to detect parathyroid adenomas. This method relied on the more rapid washout of MIBI in the thyroid than in pathologic parathyroid tissues [5]. Herein, we have shown that MIBI washout is not the same in all patients and that AITD is a significant factor for MIBI retention. This finding is indirectly seen in previous studies that showed MIBI retention in AITD patients on 30 min post-injection images [14, 15].
Theoretically, retention of MIBI in the thyroid gland on delayed images may be an important factor of reduced visibility of small parathyroid adenomas and, especially, parathyroid hyperplasia; it may also be a significant contributing factor of false negative results. In the present study, we have shown that MIBI retention is an important factor of reduced sensitivity in parathyroid detection in planar scans. In patients without thyroid MIBI retention, planar scans and SPECT/CT scans were nearly totally concordant (35/37, 94.6 %). In patients with MIBI retention, significantly more lesions were detected on SPECT/CT compared to planar scans (20 vs. 12). This suggests that SPECT/CT may be especially useful in reducing false negative results on planar scans in patients with AITD or thyroid MIBI retention.
Previous studies have shown a clear benefit of SPECT/CT, with an increased sensitivity and accuracy over ultrasonogram or planar scans alone, and especially in patients with concomitant nodular goiter [16, 17]. However, only one study has specifically evaluated the effect of AITD on parathyroid lesion detection. Our results are comparable to a recent study by Boi et al. [13], who evaluated MIBI and ultrasonogram detection rates of parathyroid lesions in patients with and without AITD. They found that in patients with AITD, MIBI had a very low sensitivity and specificity of 36 % and 42 %, respectively, compared to 100 % accuracy in patients without clinical or imaging evidence of AITD. Boi concluded that PTH level analysis from fine needle aspiration of cytologic fluid will be helpful in these patients. We suggest that an immediate SPECT/CT may be a more efficient, and less stressful method to evaluated for parathyroid lesion detection in patients with known AITD or in patients with thyroid parenchymal retention on delated scans.
We showed in our study a significant contribution of SPECT/CT over planar scans in detection of parathyroid lesions in patients with thyroid MIBI retention on planar scans. One potential reason for increased detection of parathyroid lesions in these patients is the differences in reconstruction algorithms between planar and SPECT images. Planar scans show the summation of all radiotracer activity in the thyroid and parathyroid, and parathyroid lesions will not be detected when focal MIBI uptake is not higher than the summation of thyroid parenchymal MIBI retention. Whereas in axial SPECT images, the focal MIBI uptake in the parathyroid lesion compared to the diffuse uptake in the thyroid parenchyma may provide higher contrast for parathyroid visualization. The CT component was also beneficial in that HU of parathyroid adenomas are lower than thyroid parenchyma, which helps in localization. Via our analyses, we discerned that higher MIBI uptake during early scans significantly predicts MIBI retention on delayed scans, suggesting that these patients are more likely to benefit from delayed SPECT/CT during delayed imaging. Clinically determined AITD also significantly predicted MIBI retention on delayed scans, suggesting that the presence of AITD may also be of use in pre-selecting patients who will benefit from SPECT/CT. We can also infer from our results that SPECT/CT will be especially useful compared to dual isotope parathyroid scintigraphy in patients with subacute thyroiditis or chronic phase of Hashimoto’s thyroiditis. These patients will have minimal 99mTc-pertechnetate uptake in the thyroid gland, which also reduces the effectiveness of 99mTc-pertechnetate in subtracting 99mTc-sestamibi thyroid parenchymal uptake.
Previous studies on thyroid pathology focused on thyroid nodules retaining MIBI on delayed scans, resulting in false positive results. This may be due to the high incidence of concomitant multinodular goiters in patients with primary hyperparathyroidism [18], especially in post-menopausal women [19]. Considering that some parathyroid lesions do not retain MIBI, whereas some thyroid gland nodules do retain MIBI [20], selection of patients that will benefit from other imaging modalities, such as SPECT/CT or dual isotope methods, may be beneficial in reducing medical costs.
The limitations of this study were parathyroid lesions were not all resected or biopsied, therefore, false positive and false negative analysis was not possible. Further prospective studies are warranted to evaluate the additional value of SPECT/CT in patients with diffuse thyroid diseases.
Conclusion
AITD is an important factor for thyroid parenchymal retention of MIBI on delayed scans, which results in reduced visibility of parathyroid lesions. In patients with increased retention on delayed scans, SPECT/CT was shown to have additional benefit in parathyroid lesion detection, compared to planar scans.
Compliance with Ethical Standards
Conflict of Interest
Sang Hyun Hwang, Yumie Rhee, Mijin Yun, Jung Hyun Yoon, Jeong Won Lee, and Arthur Cho declare that they have no conflict of interest.
Ethical Statement
This study was approved by the institutional review board (IRB) of our institution. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was waived because of the retrospective design of this study. We declare that this paper is solely submitted to Nuclear Medicine and Molecular Image. The content has not been published or submitted for publication elsewhere. Final approval of the version to be published was done by all authors.
Informed Consent
The institutional review board of our institute approved this retrospective study, and the requirement to obtain informed consent was waived.
References
- 1.Ishibashi M, Nishida H, Hiromatsu Y, Kojima K, Tabuchi E, Hayabuchi N. Comparison of technetium-99m-MIBI, technetium-99m-tetrofosmin, ultrasound and MRI for localization of abnormal parathyroid glands. J Nucl Med. 1998;39:320–4. [PubMed] [Google Scholar]
- 2.Geatti O, Shapiro B, Orsolon PG, Proto G, Guerra UP, Antonucci F, et al. Localization of parathyroid enlargement: experience with technetium-99m methoxyisobutylisonitrile and thallium-201 scintigraphy, ultrasonography and computed tomography. Eur J Nucl Med. 1994;21:17–22. doi: 10.1007/BF00182301. [DOI] [PubMed] [Google Scholar]
- 3.Kim YI, Jung YH, Hwang KT, Lee HY. Efficacy of (99m)Tc-sestamibi SPECT/CT for minimally invasive parathyroidectomy: comparative study with (99m)Tc-sestamibi scintigraphy, SPECT, US and CT. Ann Nucl Med. 2012;26:804–10. doi: 10.1007/s12149-012-0641-0. [DOI] [PubMed] [Google Scholar]
- 4.Lavely WC, Goetze S, Friedman KP, Leal JP, Zhang Z, Garret-Mayer E, et al. Comparison of SPECT/CT, SPECT, and planar imaging with single- and dual-phase (99m)Tc-sestamibi parathyroid scintigraphy. J Nucl Med. 2007;48:1084–9. doi: 10.2967/jnumed.107.040428. [DOI] [PubMed] [Google Scholar]
- 5.Taillefer R, Boucher Y, Potvin C, Lambert R. Detection and localization of parathyroid adenomas in patients with hyperparathyroidism using a single radionuclide imaging procedure with technetium-99m-sestamibi (double-phase study) J Nucl Med. 1992;33:1801–7. [PubMed] [Google Scholar]
- 6.Piga M, Cocco MC, Serra A, Boi F, Loy M, Mariotti S. The usefulness of 99mTc-sestaMIBI thyroid scan in the differential diagnosis and management of amiodarone-induced thyrotoxicosis. Eur J Endocrinol. 2008;159:423–9. doi: 10.1530/EJE-08-0348. [DOI] [PubMed] [Google Scholar]
- 7.Eskes SA, Wiersinga WM. Amiodarone and thyroid. Best Pract Res Clin Endocrinol Metab. 2009;23:735–51. doi: 10.1016/j.beem.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 8.Iida Y, Konishi J, Harioka T, Misaki T, Endo K, Torizuka K. Thyroid CT number and its relationship to iodine concentration. Radiology. 1983;147:793–5. doi: 10.1148/radiology.147.3.6844615. [DOI] [PubMed] [Google Scholar]
- 9.Imanishi Y, Ehara N, Mori J, Shimokawa M, Sakuyama K, Ishikawa T, et al. Measurement of thyroid iodine by CT. J Comput Assist Tomogr. 1991;15:287–90. doi: 10.1097/00004728-199103000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Silverman PM, Newman GE, Korobkin M, Workman JB, Moore AV, Coleman RE. Computed tomography in the evaluation of thyroid disease. AJR Am J Roentgenol. 1984;142:897–902. doi: 10.2214/ajr.142.5.897. [DOI] [PubMed] [Google Scholar]
- 11.Imanishi Y, Ehara N, Shinagawa T, Tsujino D, Endoh I, Baba K, et al. Correlation of CT values, iodine concentration, and histological changes in the thyroid. J Comput Assist Tomogr. 2000;24:322–6. doi: 10.1097/00004728-200003000-00026. [DOI] [PubMed] [Google Scholar]
- 12.Kaneko T, Matsumoto M, Fukui K, Hori T, Katayama K. Clinical evaluation of thyroid CT values in various thyroid conditions. J Comput Tomogr. 1979;3:1–4. doi: 10.1016/0149-936X(79)90054-7. [DOI] [PubMed] [Google Scholar]
- 13.Boi F, Lombardo C, Cocco MC, Piga M, Serra A, Lai ML, et al. Thyroid diseases cause mismatch between MIBI scan and neck ultrasound in the diagnosis of hyperfunctioning parathyroids: usefulness of FNA-PTH assay. Eur J Endocrinol. 2013;168:49–58. doi: 10.1530/EJE-12-0742. [DOI] [PubMed] [Google Scholar]
- 14.Kao CH, Wang SJ, Liao SQ, Lin WY, Hsu CY. Quick diagnosis of hyperthyroidism with semiquantitative 30-minute technetium-99m-methoxy-isobutyl-isonitrile thyroid uptake. J Nucl Med. 1993;34:71–4. [PubMed] [Google Scholar]
- 15.Kao CH, Lin WY, Wang SJ, Yeh SH. Visualization of suppressed thyroid tissue by Tc-99m MIBI. Clin Nucl Med. 1991;16:812–4. doi: 10.1097/00003072-199111000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Patel CN, Salahudeen HM, Lansdown M, Scarsbrook AF. Clinical utility of ultrasound and 99mTc sestamibi SPECT/CT for preoperative localization of parathyroid adenoma in patients with primary hyperparathyroidism. Clin Radiol. 2010;65:278–87. doi: 10.1016/j.crad.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 17.Shafiei B, Hoseinzadeh S, Fotouhi F, Malek H, Azizi F, Jahed A, et al. Preoperative (99m)Tc-sestamibi scintigraphy in patients with primary hyperparathyroidism and concomitant nodular goiter: comparison of SPECT-CT, SPECT, and planar imaging. Nucl Med Commun. 2012;33:1070–6. doi: 10.1097/MNM.0b013e32835710b6. [DOI] [PubMed] [Google Scholar]
- 18.Klingler PJ, Strolz S, Profanter C, Klingler A, Kendler D, Lhotta K, et al. Management of hyperparathyroidism in an endemic goiter area. World J Surg. 1998;22:301–7. doi: 10.1007/s002689900386. [DOI] [PubMed] [Google Scholar]
- 19.Regal M, Paramo C, Luna Cano R, Perez Mendez LF, Sierra JM, Rodriguez I, et al. Coexistence of primary hyperparathyroidism and thyroid disease. J Endocrinol Investig. 1999;22:191–7. doi: 10.1007/BF03343540. [DOI] [PubMed] [Google Scholar]
- 20.Palestro CJ, Tomas MB, Tronco GG. Radionuclide imaging of the parathyroid glands. Semin Nucl Med. 2005;35:266–76. doi: 10.1053/j.semnuclmed.2005.06.001. [DOI] [PubMed] [Google Scholar]