Abstract
Objective
Although a transjugular intrahepatic portosystemic shunt (TIPS) is commonly placed to manage isolated gastric varices, balloon-occluded retrograde transvenous obliteration (BRTO) has also been used. We compare the long-term outcomes from these procedures based on our institutional experience.
Materials and Methods
We conducted a retrospective review of patients with isolated gastric varices who underwent either TIPS with a covered stent or BRTO between January 2000 and July 2013. We identified 52 consecutive patients, 27 who had received TIPS with a covered stent and 25 who had received BRTO. We compared procedural complications, re-bleeding rates, and clinical outcomes between the two groups.
Results
There were no significant differences in procedural complications between patients who underwent TIPS (7%) and those who underwent BRTO (12%) (p = 0.57). There were also no statistically significant differences in re-bleeding rates from gastric varices between the two groups (TIPS, 7% [2/27]; BRTO, 8% [2/25]; p = 0.94) or in developing new ascites following either procedure (TIPS, 4%; BRTO, 4%; p = 0.96); significantly more patients who underwent TIPS developed hepatic encephalopathy (22%) than did those who underwent BRTO (0%, p = 0.01). There was no statistically significant difference in mean survival between the two groups (TIPS, 30 months; BRTO, 24 months; p = 0.16); median survival for the patients who received TIPS was 16.6 months, and for those who underwent BRTO, it was 26.6 months.
Conclusion
BRTO is an effective method of treating isolated gastric varices with similar outcomes and complication rates to those of TIPS with a covered stent but with a lower rate of hepatic encephalopathy.
Keywords: Gastric varices, Portal hypertension, Transjugular intrahepatic portosystemic shunt, Balloon-occluded retrograde transvenous obliteration
INTRODUCTION
Variceal bleeding from either esophageal or gastric varices is a serious complication in patients with portal hypertension. Although they are less prevalent and less prone to bleeding than esophageal varices, gastric varices are notoriously difficult to treat, often requiring more transfusions; they are also associated with higher mortality, up to 55% (1). Currently, treatment options include medical, surgical, endoscopic, and endovascular approaches, with endoscopic variceal sclerotherapy the first line of treatment. However, due to the large size and location of isolated gastric varices, long-term success in managing them endoscopically is limited (2,3). Transjugular intrahepatic portosystemic shunt (TIPS) is also widely used in managing gastric varices, but high-level evidence of its benefits is lacking, and diverting portal blood flow can further compromise liver function and aggravate hepatic encephalopathy (4,5,6).
A number of studies have demonstrated balloon-occluded retrograde transvenous obliteration (BRTO) as an effective treatment method for isolated gastric varices, which are often associated with spontaneous gastrorenal shunts (7). By occluding portosystemic shunts, BRTO is thought to improve liver function by increasing portal venous blood flow; however, the increased portal pressure may increase the risk of esophageal variceal bleeding, worsening ascites and portal hypertensive gastropathy (8).
To date, only three studies directly compare the efficacy and outcomes of TIPS and BRTO (9,10,11), and only one study has evaluated the efficacy and outcomes of treating gastric varices using TIPS with a covered stent. TIPS created with bare metal stents are known to have lower patency rates compared with covered stents and likely account for the higher re-bleeding rates from TIPS procedures that were found in previous studies (9,10,12,11,14).
Therefore, we here present a retrospective study comparing the long-term outcomes of TIPS with covered stents and BRTO in managing isolated gastric varices at our institution.
MATERIALS AND METHODS
Patients
The Institutional Review Board approved this retrospective study, and informed consent was waived. We performed a retrospective cohort comparison of 52 consecutive patients from our institution with bleeding gastric varices who were treated with either TIPS using a covered stent or with BRTO. Specifically, isolated gastric varices (Type 1 and 2) were treated based on the Sarin classification (15). We searched the Radiology Information Systems database for patients who had undergone either TIPS or BRTO during the period of January 2000 through July 2013. Before 2009, TIPS was performed to manage isolated gastric varices. Since we began using BRTO in 2009, the choice of TIPS vs. BRTO has been based on the operator's preference.
We reviewed electronic medical records for patient demographics, pre-procedural clinical data, intra-procedural information, and post-procedural data including immediate and delayed complications and clinical, endoscopic and imaging follow-up.
During the period of January 2000 through July 2013, a total of 253 patients received TIPS for bleeding from gastric, esophageal and/or rectal varices, of whom 27 patients with isolated gastric varices were treated with TIPS using covered stents. Of these 27 patients, 26 had active bleeding or recent history of gastric variceal bleeding, and one had been treated with TIPS preoperatively prior to rectal surgery. Supplemental embolization of gastric varices with multiple coils had been performed in 10 of 27 patients (37%) when there was persistent filling of gastric varices after TIPS placement.
Beginning in November 2009 and through July 2013, 25 patients with isolated gastric varices underwent BRTO. Of these 25 patients, 20 had active bleeding or recent history of gastric variceal bleeding, and five had been treated for prophylaxis. Sixteen of the 25 patients (57%) had had supplemental collateral veins treated with procedures such as inferior phrenic vein embolization.
The baseline characteristics of both groups of patients are summarized in Table 1. There was no difference in age between the TIPS and BRTO patients in regards to age; the average age of the TIPS patients was 58 (range: 34–81 years), and that of the BRTO patients was 59 (range: 26–86 years). However, more women (16) had received BRTO than TIPS (8; p < 0.05). There were no differences in the etiologies of the gastric varices, the pre-treatment Model for End-Stage Liver Disease (MELD) scores, or portal hypertension complications, namely, hepatic encephalopathy and ascites (p > 0.05).
Table 1. Baseline Characteristics for Patients Who Underwent TIPS vs. BRTO for Isolated Gastric Varices.
| TIPS (n = 27) | BRTO (n = 25) | P | |
|---|---|---|---|
| Demographics | |||
| Male | 19 | 9 | < 0.05 |
| Mean age (years)† | 58 (13) | 59 (2.5) | |
| Gastric varices etiology‡ | |||
| Alcohol | 14 | 6 | |
| Viral hepatitis (B and/or C) | 10 | 9 | |
| NASH | 4 | 2 | |
| Cryptogenic | 2 | 4 | |
| Portal vein/splenic vein thrombosis | 1 | 1 | |
| Primary biliary cirrhosis | 0 | 1 | |
| Autoimmune hepatitis | 0 | 1 | |
| Medication related cirrhosis* | 0 | 1 | |
| Pre-procedure† | |||
| Ascites | 5 | 7 | 0.27 |
| Hepatic encephalopathy | 1 | 1 | 0.27 |
| Total bilirubin (mg/dL) | 2.2 (1.4) | 3.5 (7.2) | 0.19 |
| INR | 1.5 (0.3) | 1.4 (0.3) | 0.95 |
| Creatinine (mg/dL) | 0.8 (0.3) | 0.9 (0.3) | 0.55 |
| MELD score | 13 (3.6) | 14 (4.9) | 0.21 |
*Patient with hepatic C status post liver transplant and was thought to have drug related cirrhosis of allograft, †Numbers in parentheses represent standard deviation, ‡Some patients had multiple etiologies (i.e., hepatitis C + alcohol). BRTO = balloon-occluded retrograde transvenous obliteration, INR = international normalized ratio, MELD = Model for End-Stage Liver Disease, NASH = nonalcoholic steatohepatitis, TIPS = transjugular intrahepatic portosystemic shunts
TIPS
The TIPS procedure had been performed under moderate sedation or general anesthesia according to the patient's condition, and prophylactic antibiotics were administered to all patients. The hepatic vein was accessed from a right internal jugular approach, and wedged hepatic venography was performed to localize the portal vein. The portal vein was then accessed using a Colapinto needle (Cook Inc., Bloomington, IN, USA) passed from the right or middle hepatic vein. Pressures were measured in the right atrium and the portal vein to determine a pre-TIPS portosystemic gradient, and portal venograms were obtained. The parenchymal tract was then pre-dilated and then dilated using an 8–10 mm angioplasty balloon, and a 10-mm covered stent (Viatorr [n = 24], W. L. Gore and Associates Inc., Flagstaff, AZ, USA; Flucency [n = 2], Bard Peripheral Vascular, Tempe, AZ, USA; Viabahn [n = 1], W. L. Gore and Associates Inc.) was placed. After the TIPS was created, portal venography was performed with the catheter positioned in the splenic vein to assess for filling of any gastric varices; the varices were embolized if persistent filling was noted. A final mean portosystemic gradient was measured and optimized to be < 12 mm Hg. Technical success for each TIPS procedure was defined per the Society of Interventional Radiology reporting standards as the creation of a patent TIPS between the hepatic vein and a branch of the portal vein (16).
BRTO Procedure
The BRTO procedure was performed under moderate sedation via the transfemoral or transjugular approach following placement of a 9–10 French sheath based on the size and anatomy of the gastrorenal shunt; this shunt was selected and catheterized via the left renal vein, with occlusion balloon catheters such as a 6 Fr wedge pressure catheter (Teleflex Medical, Arrow International Inc., Wayne, PA, USA) or a 6 Fr Berenstein occlusion balloon catheter (Boston Scientific, Natick, MA, USA) advanced to the shunt coaxially over the stiff guide wire. Balloon-occluded retrograde venography was performed to evaluate the anatomy of the shunt and varices. After embolization of any collateral veins including the inferior phrenic vein with a 2.7 Fr microcatheter (Progreat; Terumo Medical, Elkron, MD, USA) and 3–6 mm microcoils (Nester Coil; Cook Inc.). With the occlusion balloon inflated, the sclerosant was administered to fill the varices under fluoroscopic guidance. Ethanolamine oleate (16–20 cc) mixed with Lipiodol (Ethiodol; Savage Laboratories, Melville, NY, USA) was used as the sclerosant for the initial four patients, and 8–16 cc sodium tetradecol sulfate (Sotradecol; AngioDynamics, Queensbury, NY, USA) mixed with Lipiodol and air (2:1:3 ratio) was used as the sclerosant for the remaining patients. The occlusion balloon remained inflated post procedure for 4–20 hours (mean inflation time: 13 hours) according to the timing of the procedure and was removed after stagnation of the sclerosant was confirmed on follow-up abdominal radiography. Technical success for the BRTO procedure was defined as successful placement of the occlusion balloon in the gastrorenal shunt and administration of the sclerosant mixture into the varices.
Endoscopy and Imaging Follow-Up
The patients were followed with endoscopy every 3–6 months following the BRTO procedure. All patients who presented with re-bleeding underwent endoscopy to determine the source of the bleeding.
Doppler ultrasonography (US) was performed at 1, 3, 6, and 12 months following TIPS placement and every 6–12 months thereafter unless there was intervening clinical deterioration.
Computed tomography (CT) or magnetic resonance (MR) imaging was performed at 3–6 months following each BRTO procedure to confirm variceal obliteration.
Analysis
Early re-bleeding was defined as recurrent bleeding within seven days following the TIPS or BRTO procedure, and late re-bleeding was defined as recurrent bleeding after seven days following the procedure. Hepatic encephalopathy was defined and the degree characterized based on the West Haven Criteria for quantitative grading of mental state in hepatic encephalopathy (17).
We used the chi-squared test and Fisher's exact test to compare differences in baseline characteristics, the rates of complications, re-bleeding, new hepatic encephalopathy, new ascites, repeat intervention, and resolution of gastric varices on follow-up endoscopies, and a p value of < 0.05 was considered statistically significant. We calculated survival using the Kaplan-Meier estimator and performed all statistical analyses with MedCalc Software (Version 16.8, Ostend, Belgium).
RESULTS
Technical Success
Technical success was achieved in 100% of the patients who received a TIPS (27 of 27) and 88% of the patients who underwent BRTO (22 of 25); the BRTO failures were balloon ruptures (n = 2) and a right common femoral artery injury (n = 1). As noted before, ten of the 27 TIPS patients underwent supplemental gastric varices embolization with multiple coils. The mean portosystemic gradients pre-TIPS and post-TIPS measured 15 ± 5.4 mm Hg and 6 ± 3.3 mm Hg, respectively, with a mean decrease of 9 ± 5.7 mm Hg in the portosystemic gradient following TIPS.
Procedural Complications
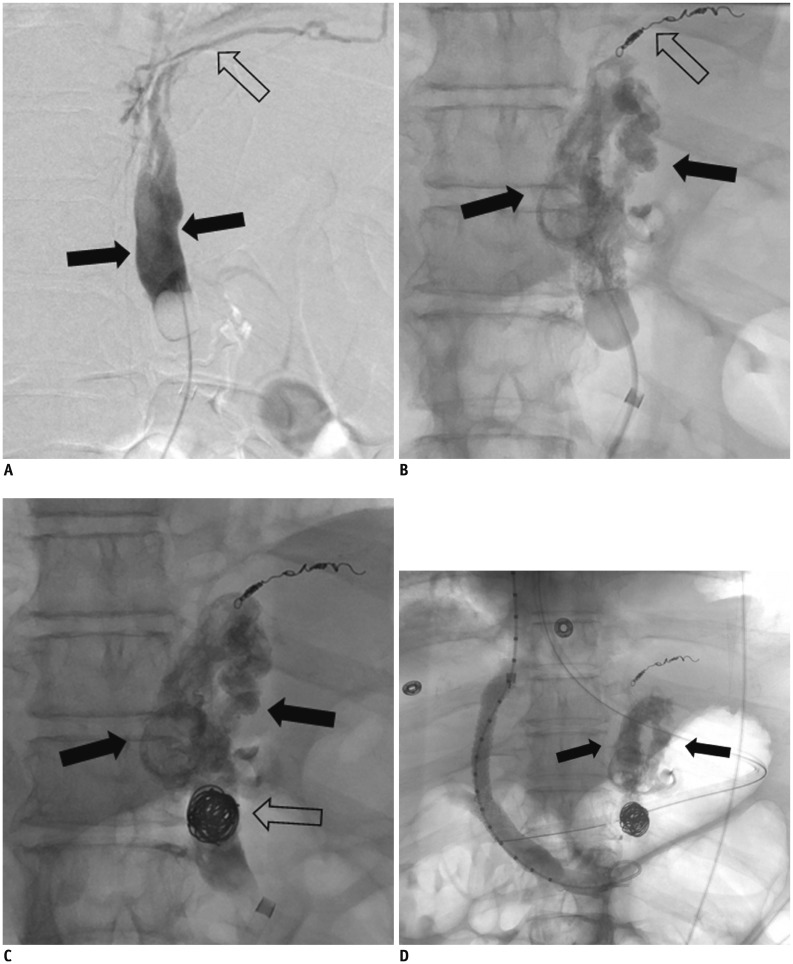
There were no statistically significant differences in procedural complications between the TIPS and BRTO groups (p = 0.57) (Table 2). Within the TIPS group, one patient had an episode of oxygen desaturation that required bag ventilation and administration of naloxone to return to baseline. Another patient had a 5 mm coil placed for variceal embolization that migrated to the left lower lobe pulmonary artery but remained asymptomatic. In the BRTO group, two patients experienced balloon rupture within six hours of inflation, and one of these patients underwent TIPS due to presumed gastric variceal bleeding one day later. Another patient sustained a common femoral artery injury during the process of acquiring femoral venous access, and this required an open arteriotomy repair. It was not possible to leave the occlusion balloon and sheath, and therefore, the gastrorenal shunt was embolized with coils to retain the sclerosant in the varix before the balloon was deflated and the sheath removed; this patient underwent TIPS due to presumed gastric variceal bleeding two days later (Fig. 1).
Table 2. Comparing Outcomes of TIPS vs. BRTO for Isolated Gastric Varices.
| TIPS (n = 27) | BRTO (n = 25) | P | |
|---|---|---|---|
| Procedural complications | |||
| Yes | 2 | 3 | 0.57 |
| Post procedure labs* | |||
| Mean # days after procedure | 64 (262) | 88 (117) | 0.68 |
| Total bilirubin (mg/dL) | 2.1 (1.4) | 3.7 (9.5) | 0.46 |
| INR | 1.5 (0.1) | 1.5 (0.4) | 0.98 |
| Serum creatinine (mg/dL) | 0.8 (0.3) | 1.0 (0.5) | 0.11 |
| MELD score | 13 (3.3) | 13 (6.4) | 0.97 |
| Change in MELD score | +1 (0.9) | 0 (3.6) | 0.21 |
| Clinical outcomes | |||
| New hepatic encephalopathy | 6 | 0 | 0.01 |
| New ascites | 1 | 1 | 0.96 |
| Rebleeding | 3 | 3 | 0.92 |
| Rebleeding from GV source | 2 | 2 | 0.94 |
| Mean follow-up (days)* | 917 (908) | 727 (533) | 0.03 |
*Numbers in parentheses represent standard deviation. BRTO = balloon-occluded retrograde transvenous obliteration, GV = gastric varices, INR = international normalized ratio, labs = laboratory examinations, MELD = Model for End-Stage Liver Disease, TIPS = transjugular intrahepatic portosystemic shunts
Fig. 1. 68-year-old woman with nonalcoholic steatohepatitis cirrhosis and recurrent gastric variceal bleeding.
A. Balloon-occluded venogram of gastro-renal shunt shows contrast filling of gastric varices (arrows) along with draining inferior phrenic collateral vein (open arrow). B. Inferior phrenic vein was embolized with microcoils (open arrow). This was followed by injection of sodium tetradecyl sulfate (Sotradecol; AngioDynamics) mixed with Lipiodol into gastric varices (arrows). C. It was not possible to leave occlusion balloon and sheath due to common femoral artery injury while obtaining femoral venous access. Therefore, gastrorenal shunt was embolized with multiple coils (open arrow) to retain sclerosant (arrows) in gastric varices before balloon was deflated and sheath was removed. D. Patient presented with hematemesis two days following procedure. TIPS was performed due to presumed gastric variceal bleeding. Venogram after TIPS placement showed no gastric varix filling from afferent veins and dense Lipiodol uptake (arrows) in gastric varices. Portosystemic gradient decreased from 15 mm Hg to 5 mm Hg. TIPS = transjugular intrahepatic portosystemic shunts
Outcomes
There were no differences in immediate post-procedure laboratory values (total bilirubin, INR, serum creatinine) and MELD scores during the follow-up period (TIPS: mean, 64 days vs. BRTO: mean, 88 days; p > 0.05) (Table 2).
There was a significantly higher rate of hepatic encephalopathy within the TIPS group (6 of 27 patients; 22%) than in the BRTO group (0 of 25 patients; 0%, p = 0.01) (Table 2). Among the six patients who were treated for hepatic encephalopathy in the TIPS group, five were documented as having trivial lack of awareness (grade 1), and one was noted to have mild disorientation to time and place (grade 2). All patients demonstrated improvement upon discharge.
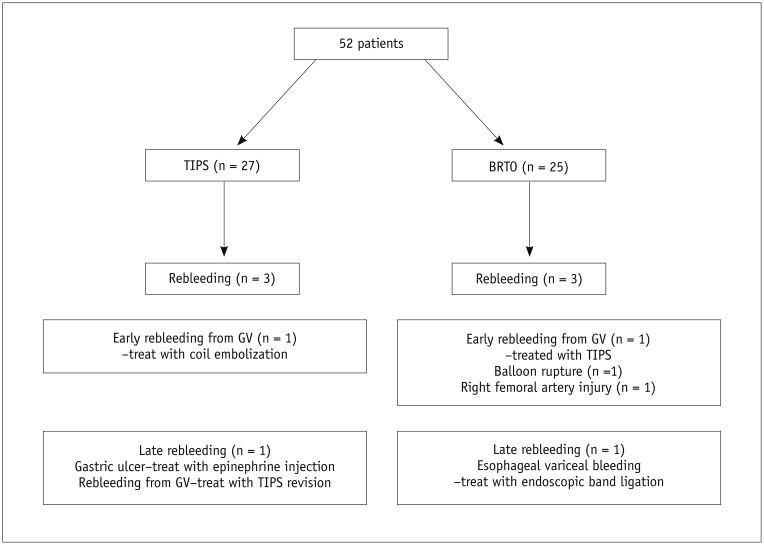
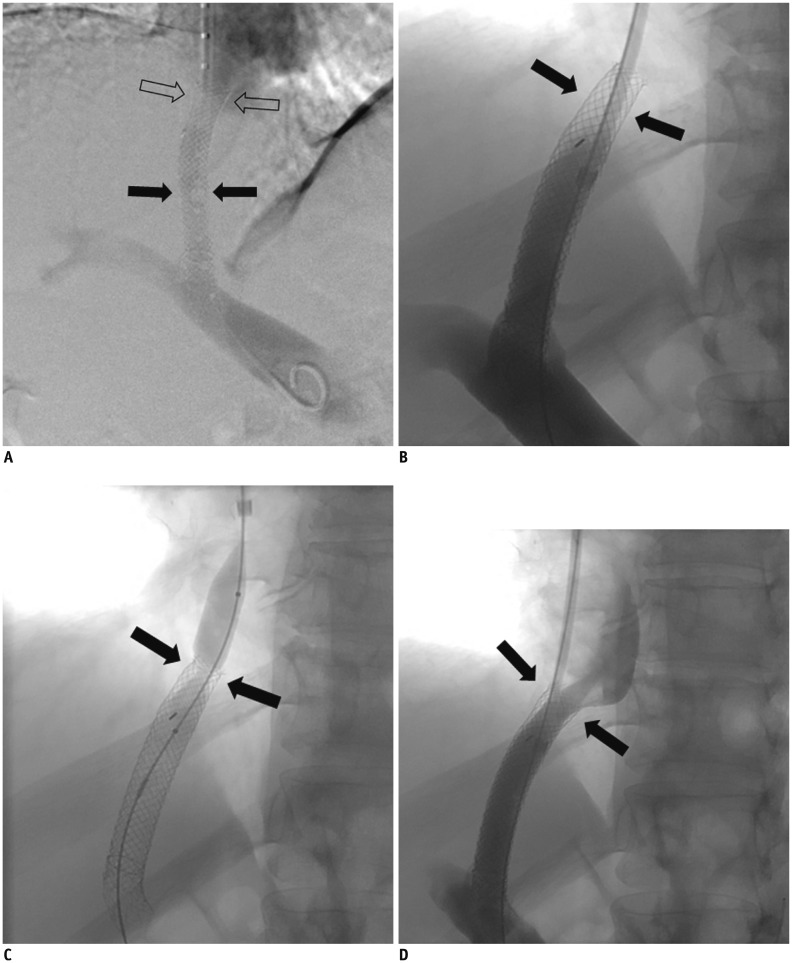
There was no statistically significant difference in development of new ascites following TIPS (4%) or BRTO (4%, p = 0.96) (Table 2). There was also no statistically significant difference in re-bleeding rates from gastric varices between the TIPS (2/27, 7%) and BRTO groups (2/25, 8%; p = 0.94) (Table 2). Figure 2 illustrates re-bleeding after TIPS or BRTO in 52 patients. Among the TIPS group, three patients (3/27, 11%) presented with early and late re-bleeding (gastric varices: n = 2; gastric ulcer: n = 1). One patient developed hematemesis two days following TIPS placement from gastric varices, which was successfully treated with coil embolization. Two additional patients presented with hematemesis: one case was 18 months following TIPS, from an oozing gastric ulcer–although no varices were seen–and was successfully treated with epinephrine injection, and the other, two years following TIPS, was re-bleeding from gastric varices that was treated with TIPS revision due to stenosis (Fig. 3).
Fig. 2. Flowchart summarizing re-bleeding after TIPS or BRTO in 52 patients.
BRTO = balloon-occluded retrograde transvenous obliteration, GV = gastric varices, TIPS = transjugular intrahepatic portosystemic shunts
Fig. 3. 47-year-old man with alcoholic liver cirrhosis with acute gastric variceal bleeding.
A. TIPS procedure was performed using 10 × 50 mm Viatorr stent (arrows) and 10 × 68 mm Wallstent (open arrows) extending to hepaticocaval junction. Portosystemic gradient decreased from 20 mm Hg to 8 mm Hg. Patient presented with recurrent gastric variceal bleeding two years later. B. TIPS venogram showed tight stenosis (arrows) at TIPS stent near hepaticocaval junction. C. Balloon angioplasty was performed at tight stenosis (arrows) near hepaticocaval junction. D. TIPS venogram after balloon angioplasty showed interval improvement of stenosis (arrows). Portosystemic gradient decreased from 15 mm Hg to 5 mm Hg. TIPS = transjugular intrahepatic portosystemic shunts
Among the BRTO group, three patients (12%) presented with early and late re-bleeding (gastric varices: n = 2; esophageal varices: n = 1). One patient who had a balloon rupture within six hours presented with hematemesis one day following the procedure from presumed gastric variceal bleeding and was treated with TIPS and coil embolization of the gastric varices. A second patient with right femoral artery injury presented with hematemesis from presumed gastric variceal bleeding two days following the procedure and was treated with TIPS (Fig. 1). One patient presented with hematemesis nine months later from esophageal variceal bleeding, which was subsequently treated with endoscopic band ligation.
The mean survival for the patients who received TIPS was 30 months, and for those who underwent BRTO, it was 24 months; there was no statistically significant difference between the two groups (p = 0.16). The median survival for the patients who received TIPS was 16.6 months, and for those who underwent BRTO, it was 26.6 months.
Endoscopy and Imaging Follow-Up
Significantly more patients who underwent BRTO received follow-up endoscopy, and of these, the gastric varices were resolved in 87% of the patients who underwent BRTO (13 of 15) and in 60% of those who received TIPS (3 of 5) (Table 2). However, these differences did not approach statistical significance. One TIPS patient demonstrated persistent gastric varices at three-month follow-up endoscopy; because of the increased risk of bleeding, the patient subsequently underwent TIPS revision. Among the BRTO group, one patient presented with persistent gastric varices, which decreased in size on nine-month follow-up endoscopy and remained asymptomatic and thus did not require any intervention. Another patient presented with recurrent gastric varices 3.5 years following the BRTO procedure with no bleeding episodes and thus did not require further intervention.
Two patients in the TIPS group underwent TIPS revision due to US Doppler findings suggesting shunt stenosis. Fifteen patients in the BRTO group underwent follow-up CT or MR imaging during follow-up that demonstrated complete obliteration of the gastric varices in all patients.
DISCUSSION
Variceal bleeding remains a serious complication of portal hypertension. Although treatment of esophageal varices is well established with endoscopic methods, the long-term success of gastric varices is limited in part due to the high flows through the varix and also the location of the varices in the cardia/gastric fundus (18). In addition, due to their size, sclerosis of the gastric varices often requires larger volumes of sclerosant and poses a higher risk of pulmonary system embolization (19). TIPS has been widely used for decades to manage gastric varices, and BRTO has emerged as an alternative treatment method, specifically among patients in the United States for whom TIPS is contraindicated (20).
Limited intra-institutional studies have compared the outcomes of TIPS and BRTO in managing gastric varices (9,10,11). In a study by Choi et al. (9), patients with active gastric variceal bleeding due to liver cirrhosis were treated with either TIPS (n = 13) or BRTO (n = 8), and no statistically significant differences were noted in either immediate hemostasis or re-bleeding (9). A larger study by Ninoi et al. (10) evaluated 104 patients, 27 of whom were treated with TIPS and 77 of whom were treated with transcatheter sclerotherapy. The cumulative gastric variceal bleeding rates at one year were significantly better in the BRTO group (TIPS: 20% vs. BRTO: 2%). Furthermore, survival rates at 1, 3, and 5 years following BRTO were better than those after TIPS. However, the improved survival was only statistically significant for patients classified as Child-Pugh class A (as opposed to class B or C) prior to treatment. It is important to note that the TIPS procedures in that study used bare metal stents, which are known to have lower patency than covered stents and which likely accounted for the higher re-bleeding rates (21). More recently, Sabri et al. (11) demonstrated equivalent short-term re-bleeding for isolated gastric varices managed by TIPS with covered stents (11%) and BRTO (0%, p = 0.25). Similar to the results reported by Sabri et al. (11), our study demonstrated no significant difference in gastric varix re-bleeding between the two groups (p = 0.94).
In the TIPS group, three patients (3/27, 11%) presented with early and late re-bleeding (gastric varices: n = 2; gastric ulcer: n = 1). The two patients who had re-bleeding from their gastric varices were subsequently treated with coil embolization of the varices and TIPS revision due to stenosis (Fig. 3).
In the BRTO group, three patients (12%) presented with early and late re-bleeding (gastric varices: n = 2; esophageal varix: n = 1). Two patients presented with presumed gastric variceal bleeding within two days following the procedure, and they were subsequently treated with TIPS placement. These early re-bleeding cases were mostly the result of inadequate sclerosis of the gastric varices. In one patient, there was balloon rupture within six hours, and in the other, the balloon was deflated after injection of sclerosant and coil embolization of gastrorenal shunts due to right common femoral artery injury (Fig. 1).
Because most fundal gastric varices drain into the left renal vein via a spontaneous gastrorenal shunt, obliterating the gastric varices excludes the shunt from portosystemic circulation (1,2,3), and occluding portosystemic shunts in BRTO leads to significant changes in portal hepatic hemodynamics (22). Although transient improvement in hepatic function has been reported with increased portal hepatic blood flow, symptoms associated with portal hypertension can be further exacerbated post treatment from blood flow diversion.
One of the most important reported complications associated with BRTO is aggravated esophageal varices (8,22); reported rates of worsening esophageal varices vary up to 63%, with 11–24% subsequent variceal bleeding (23,24). The wide range of reported rates is thought to be related to the variations in patient populations and the causes and severity of liver disease, as well as the different follow-up durations (8). In our present study, only one patient in the BRTO group presented, nine months following the procedure, with esophageal variceal bleeding, which was successfully treated with endoscopic band ligation. The rate of esophageal variceal bleeding in our study was relatively lower than that reported in the literature, which may in part have been due to the shorter follow-up duration.
A substantive risk from TIPS is that of severe encephalopathy, with incidence estimates as high as 20%. A potential benefit of BRTO is that it avoids this risk by diverting blood flow (25). In this study, none of the patients developed encephalopathy in the BRTO group, whereas six developed new encephalopathy following TIPS placement.
In our study, the mean pre-TIPS portosystemic gradient of 15 mm Hg was unusually low. In the study by Chao et al. (26), the mean hepatic venous pressure gradient was 11.2 mm Hg for gastric varices and 15.5 mm Hg for esophageal varices. Thus, diminished portal pressure (< 12 mm Hg) is more likely in patients with gastric varices.
It is difficult to compare the costs between the two groups including devices, procedure time, follow-up, etc. BRTO does require post-procedure dwell times for vascular sheaths in observation or intensive care units in our hospital; thus, it may be less cost-effective than TIPS unless the patient is already in intensive care.
This study has a number of limitations. First, it is retrospective nature and used a relatively small number of patients. Furthermore, the retrospective nature of the study limits the ability to evaluate for delayed complications such as hepatic encephalopathy and development of post-procedure ascites. Significantly more patients in the BRTO group (15 of 25; 60%) received follow-up endoscopies than in the TIPS group (5 of 27; 19%), although the mean follow-up for TIPS patients is significantly longer than that for BRTO patients. This is likely secondary to the fact that patients who undergo TIPS are more likely to be followed for signs of bleeding as opposed to routine endoscopy.
Second, there was selection bias in the choice of TIPS vs. BRTO with no selection criteria for the choice. Before 2009, TIPS was performed to manage isolated gastric varices, but since we began BRTO in 2009, the choice of management technique was based on operator preference.
In conclusion, BRTO is an effective method of treating isolated gastric varices with similar outcomes and complication rates as TIPS with a covered stent but lower rates of hepatic encephalopathy. Multi-center prospective randomized studies are needed to determine the long-term outcomes in order to develop tailored treatment strategies for individual patients who present with isolated gastric variceal bleeding.
Footnotes
This paper was presented as a scientific paper at the 2014 Annual Meeting of Society of Interventional Radiology in San Diego, CA, USA.
References
- 1.Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16:1343–1349. doi: 10.1002/hep.1840160607. [DOI] [PubMed] [Google Scholar]
- 2.Saad WE, Al-Osaimi AM, Caldwell S, Ray CE, Lorenz JM, Burke CT, et al. ACR appropriateness criteria: radiologic management of gastric varices. Expert Panel on Interventional Radiology, American College of Radiology 2012. Web site. [Accessed January 24, 2017]. https://acsearch.acr.org/docs/70911/Narrative/
- 3.Saad WE, Simon PO, Jr, Rose SC. Balloon-occluded retrograde transvenous obliteration of gastric varices. Cardiovasc Intervent Radiol. 2014;37:299–315. doi: 10.1007/s00270-013-0715-y. [DOI] [PubMed] [Google Scholar]
- 4.Kerlan RK, Jr, LaBerge JM, Baker EL, Wack JP, Marx M, Somberg KA, et al. Successful reversal of hepatic encephalopathy with intentional occlusion of transjugular intrahepatic portosystemic shunts. J Vasc Interv Radiol. 1995;6:917–921. doi: 10.1016/s1051-0443(95)71212-x. [DOI] [PubMed] [Google Scholar]
- 5.Brown RS, Jr, Lake JR. Transjugular intrahepatic portosystemic shunt as a form of treatment for portal hypertension: indications and contraindications. Adv Intern Med. 1997;42:485–504. [PubMed] [Google Scholar]
- 6.Sanyal AJ, Freedman AM, Luketic VA, Purdum PP, 3rd, Shiffman ML, DeMeo J, et al. The natural history of portal hypertension after transjugular intrahepatic portosystemic shunts. Gastroenterology. 1997;112:889–898. doi: 10.1053/gast.1997.v112.pm9041251. [DOI] [PubMed] [Google Scholar]
- 7.Katoh K, Sone M, Hirose A, Inoue Y, Fujino Y, Onodera M. Balloon-occluded retrograde transvenous obliteration for gastric varices: the relationship between the clinical outcome and gastrorenal shunt occlusion. BMC Med Imaging. 2010;10:2. doi: 10.1186/1471-2342-10-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elsamman MK, Fujiwara Y, Kameda N, Okazaki H, Tanigawa T, Shiba M, et al. Predictive factors of worsening of esophageal varices after balloon-occluded retrograde transvenous obliteration in patients with gastric varices. Am J Gastroenterol. 2009;104:2214–2221. doi: 10.1038/ajg.2008.140. [DOI] [PubMed] [Google Scholar]
- 9.Choi YH, Yoon CJ, Park JH, Chung JW, Kwon JW, Choi GM. Balloon-occluded retrograde transvenous obliteration for gastric variceal bleeding: its feasibility compared with transjugular intrahepatic portosystemic shunt. Korean J Radiol. 2003;4:109–116. doi: 10.3348/kjr.2003.4.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ninoi T, Nakamura K, Kaminou T, Nishida N, Sakai Y, Kitayama T, et al. TIPS versus transcatheter sclerotherapy for gastric varices. AJR Am J Roentgenol. 2004;183:369–376. doi: 10.2214/ajr.183.2.1830369. [DOI] [PubMed] [Google Scholar]
- 11.Sabri SS, Abi-Jaoudeh N, Swee W, Saad WE, Turba UC, Caldwell SH, et al. Short-term rebleeding rates for isolated gastric varices managed by transjugular intrahepatic portosystemic shunt versus balloon-occluded retrograde transvenous obliteration. J Vasc Interv Radiol. 2014;25:355–361. doi: 10.1016/j.jvir.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 12.Chau TN, Patch D, Chan YW, Nagral A, Dick R, Burroughs AK. “Salvage” transjugular intrahepatic portosystemic shunts: gastric fundal compared with esophageal variceal bleeding. Gastroenterology. 1998;114:981–987. doi: 10.1016/s0016-5085(98)00640-4. [DOI] [PubMed] [Google Scholar]
- 13.Barange K, Péron JM, Imani K, Otal P, Payen JL, Rousseau H, et al. Transjugular intrahepatic portosystemic shunt in the treatment of refractory bleeding from ruptured gastric varices. Hepatology. 1999;30:1139–1143. doi: 10.1002/hep.510300523. [DOI] [PubMed] [Google Scholar]
- 14.Rees CJ, Nylander DL, Thompson NP, Rose JD, Record CO, Hudson M. Do gastric and oesophageal varices bleed at different portal pressures and is TIPS an effective treatment? Liver. 2000;20:253–256. doi: 10.1034/j.1600-0676.2000.020003253.x. [DOI] [PubMed] [Google Scholar]
- 15.Sarin SK, Kumar A. Gastric varices: profile, classification, and management. Am J Gastroenterol. 1989;84:1244–1249. [PubMed] [Google Scholar]
- 16.Haskal ZJ, Rees CR, Ring EJ, Saxon R, Sacks D. Reporting standards for transjugular intrahepatic portosystemic shunts. Technology Assessment Committee of the SCVIR. J Vasc Interv Radiol. 1997;8:289–297. doi: 10.1016/s1051-0443(97)70558-x. [DOI] [PubMed] [Google Scholar]
- 17.Ferenci P, Lockwood A, Mullen K, Tarter R, Weissenborn K, Blei AT. Hepatic encephalopathy--definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th World Congresses of Gastroenterology, Vienna, 1998. Hepatology. 2002;35:716–721. doi: 10.1053/jhep.2002.31250. [DOI] [PubMed] [Google Scholar]
- 18.Saad WE, Kitanosono T, Koizumi J, Hirota S. The conventional balloon-occluded retrograde transvenous obliteration procedure: indications, contraindications, and technical applications. Tech Vasc Interv Radiol. 2013;16:101–151. doi: 10.1053/j.tvir.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 19.Patel A, Fischman AM, Saad WE. Balloon-occluded retrograde transvenous obliteration of gastric varices. AJR Am J Roentgenol. 2012;199:721–729. doi: 10.2214/AJR.12.9052. [DOI] [PubMed] [Google Scholar]
- 20.Borghei P, Kim SK, Zuckerman DA. Balloon occlusion retrograde transvenous obliteration of gastric varices in two non-cirrhotic patients with portal vein thrombosis. Korean J Radiol. 2014;15:108–113. doi: 10.3348/kjr.2014.15.1.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bureau C, Garcia-Pagan JC, Otal P, Pomier-Layrargues G, Chabbert V, Cortez C, et al. Improved clinical outcome using polytetrafluoroethylene-coated stents for TIPS: results of a randomized study. Gastroenterology. 2004;126:469–475. doi: 10.1053/j.gastro.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 22.Saad WE, Darcy MD. Transjugular intrahepatic portosystemic shunt (TIPS) versus balloon-occluded retrograde transvenous obliteration (BRTO) for the management of gastric varices. Semin Intervent Radiol. 2011;28:339–349. doi: 10.1055/s-0031-1284461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jang SY, Kim GH, Park SY, Cho CM, Tak WY, Kim JH, et al. Clinical outcomes of balloon-occluded retrograde transvenous obliteration for the treatment of gastric variceal hemorrhage in Korean patients with liver cirrhosis: a retrospective multicenter study. Clin Mol Hepatol. 2012;18:368–374. doi: 10.3350/cmh.2012.18.4.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Watanabe M, Shiozawa K, Ikehara T, Nakano S, Kougame M, Otsuka T, et al. Short-term effects and early complications of balloon-occluded retrograde transvenous obliteration for gastric varices. ISRN Gastroenterol. 2012;2012:919371. doi: 10.5402/2012/919371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fukuda T, Hirota S, Sugimura K. Long-term results of balloon-occluded retrograde transvenous obliteration for the treatment of gastric varices and hepatic encephalopathy. J Vasc Interv Radiol. 2001;12:327–336. doi: 10.1016/s1051-0443(07)61912-5. [DOI] [PubMed] [Google Scholar]
- 26.Chao Y, Lin HC, Lee FY, Wang SS, Tsai YT, Hsia HC, et al. Hepatic hemodynamic features in patients with esophageal or gastric varices. J Hepatol. 1993;19:85–89. doi: 10.1016/s0168-8278(05)80180-1. [DOI] [PubMed] [Google Scholar]