Abstract
Objective
Concurrent low brain and high liver uptake are sometimes observed on fluorine-18-labeled fluoro-2-deoxy-D-glucose (FDG) positron emission tomography (PET). We investigated the potential clinical significance of this uptake pattern related to metabolic syndrome (MS).
Materials and Methods
We retrospectively reviewed data from 264 consecutive males who had undergone general health check-ups, including FDG PET/CT scans. After an overnight fast, the men had their peripheral blood drawn and the levels of various laboratory parameters measured; an FDG PET/CT scan was performed on the same day. We measured the maximum standardized uptake values of the brain and liver from regions of interest manually placed over the frontal cortex at the level of the centrum semiovale and the right lobe of the liver parenchyma, respectively.
Results
Fasting blood glucose (FBG; odds ratio [OR] = 1.063, p < 0.001) and glycated hemoglobin (HbA1c; OR = 3.634, p = 0.010) were the strongest predictive factors for low brain FDG uptake, whereas waist circumference (OR = 1.200, p < 0.001) and γ-glutamyl transpeptidase (OR = 1.012, p = 0.001) were the strongest predictive factors for high liver uptake. Eleven subjects (4.2%) showed concurrent low brain and high liver FDG uptake, and all but one of these subjects (90.9%) had MS. Systolic blood pressure, waist circumference, FBG, triglyceride, alanine aminotransferase, insulin resistance (measured by homeostasis model assessment), insulin, HbA1c, and body mass index were higher in subjects with this FDG uptake pattern than in those without (all, p < 0.001).
Conclusion
Concurrent low brain and high liver FDG uptake were closely associated with MS. Moreover, subjects with this pattern had higher values for various cardiovascular risk factors than did those without.
Keywords: Brain, Liver, FDG, PET, Cardiovascular risk factor
INTRODUCTION
Positron emission tomography (PET) using fluorine-18-401labeled fluoro-2-deoxy-D-glucose (FDG) has been widely accepted as a useful, noninvasive imaging modality for evaluating a variety of neoplastic and brain diseases (1).
The brain and liver are useful organs for evaluating FDG uptake because they are relatively large in human bodies and can be shown with certainty on FDG-PET images. In general, the brain demonstrates the highest physiologic FDG uptake in the human body because of its high glucose metabolism, and this high FDG uptake complicates differentiating lesions from normal tissue in clinical situations. FDG uptake by the brain is sometimes abnormally low, even in the absence of brain disease. The most well known cause of reduced brain FDG uptake is a hyperglycemic state at the time of the FDG PET/CT study (2). In addition, a number of studies have revealed other factors associated with reduced brain FDG uptake (3,4,5,6,7,8,9). In contrast, the liver generally shows low FDG uptake that is only slightly higher than that of the mediastinal blood pool. Because the liver can show increased uptake even in the absence of malignant disease, true hepatic lesions with mildly increased uptake can be overlooked. It has been reported that liver FDG uptake is also affected by various clinical factors (10,11,12,13,14,15).
Concurrent low brain and high liver uptake are sometimes observed on FDG PET; however, no studies have yet investigated the clinical significance of this pattern. We intended to investigate potential associations between degree of brain FDG uptake, degree of liver FDG uptake, and various physical and hematological factors, with the ultimate aim of defining determinants of low brain uptake and high liver uptake on FDG PET. Because we included all components of metabolic syndrome (MS) in the present study, we also investigated the potential clinical significance of concurrent low brain and high liver FDG uptake related to MS.
MATERIALS AND METHODS
Subjects
The Institutional Review Board approved our study design and all informed consent exemptions, and we retrospectively reviewed data from 264 consecutive males who had undergone general health check-ups, including FDG PET/CT scans to screen for malignancies. None of the enrolled subjects had a known malignant disease, hepatitis B or C, cardiac symptoms, previous coronary artery disease, neurodegenerative disorders, psychiatric diseases, or previous cerebral vascular accidents, nor did they use neuropsychological medications. We measured their height, weight, and waist circumference and calculated body mass index (BMI, kg/m2) as an index of obesity. After at least five minutes of rest, we measured systolic and diastolic blood pressures (SBP and DBP, mm Hg). After an overnight fast, we drew peripheral blood and measured the levels of fasting blood glucose (FBG, mg/dL), glycated hemoglobin (HbA1c, %), total cholesterol (mg/dL), high-density lipoprotein cholesterol (HDLc, mg/dL), low-density lipoprotein cholesterol (LDLc, mg/dL), triglyceride (TG, mg/dL), aspartate aminotransferase (AST, IU/L), alanine aminotransferase (ALT, IU/L), γ-glutamyl transpeptidase (γ-orgGT, IU/L), alkaline phosphatase (IU/L), total bilirubin (mg/dL), total protein (g/dL), blood urea nitrogen (mg/dL), creatinine (mg/dL), erythrocyte sedimentation rate (mm/hr), high-sensitivity C-reactive protein (mg/L), insulin (µIU/mL), and thyroid-stimulating hormone (TSH, µIU/mL).
A radiologist determined the presence of fatty liver using abdominal ultrasonography interpretation, and we obtained the Framingham Risk Score (FRS) from the medical records. We estimated insulin resistance using the homeostasis model assessment of insulin resistance (HOMA-IR) equation from the FBG and insulin concentrations as follows: HOMA-IR = (FBG × insulin) / 405. We conducted all measurements on the same day as the FDG PET/CT scan. We defined diabetes mellitus (DM) as serum FBG level ≥ 126 mg/dL or the use of any hypoglycemic drug and hypertension (HTN) as SBP ≥ 140 or DBP ≥ 90 mm Hg or the use of any anti-hypertensive drug.
Patients were diagnosed with MS based on criteria established by the American Heart Association and National Heart, Lung, and Blood Institute using waist circumferences adjusted for Asians, specifically, when three or more of the following criteria were met: 1) waist circumference ≥ 90.0 cm; 2) fasting TG ≥ 150 mg/dL; 3) HDLc < 40 mg/dL; 4) SBP ≥ 130 mm Hg, DBP ≥ 85 mm Hg, or use of HTN medication; and 5) FBG ≥ 100 mg/dL or use of DM medication (16).
FDG PET/CT Protocol
All subjects were examined using a dedicated PET/CT scanner (Discovery 710; GE Healthcare, Waukesha, WI, USA). FDG PET/CT imaging was performed 60 min after injection of FDG at a dose of 3.7 MBq/kg (0.1 mCi/kg) body weight. Before FDG administration, subjects were asked to fast for at least 6 hours. Blood glucose level at the time of FDG injection was less than 180 mg/dL in all subjects. No additional glucose control drugs were used in subjects with high blood glucose levels (17). Sixty minutes after the administration of FDG, low-dose CT covering the area from the vertex of the skull to the proximal thigh was performed for attenuation correction and precise anatomical localization. Thereafter, an emission scan was conducted in the three-dimensional mode. Emission scan time per bed position was 1.5 minutes, and nine or 10 bed positions were acquired. PET data were obtained using a high-resolution whole-body scanner with an axial view field of 15.7 cm. The average axial resolution varied between 5.6 mm (full width at half maximum) at 1 cm and 6.3 mm at 10 cm. The average total PET/CT examination time was 15 minutes. The CT scan was obtained with tube voltage of 120 kVp and tube current of 30–180 mAs. The PET data were iteratively reconstructed with attenuation correction and then reoriented in axial, sagittal, and coronal slices.
Image Analysis
We reviewed the images using an Advantage Workstation 4.6 (GE Healthcare), using round regions of interest (ROIs) to measure the standardized uptake values (SUVs) of the brain and liver of each subject. We calculated SUV as the tissue activity of the ROI (MBq/g)/(injected dose [MBq]/body weight [g]) on PET images and measured the maximum SUVs (SUVmax) of the brain and liver from ROIs (2 cm and 5 cm diameters, respectively) manually placed over the frontal cortex at the level of the centrum semiovale (3,18) and the right lobe of the liver parenchyma, respectively. Because SUVmax is most conveniently measured by the surrounding target region and is less observer-dependent and more reproducible than SUVmean in spite of its vulnerability to image noise (19), we used SUVmax as a representative value for glucose metabolism in the brain and liver.
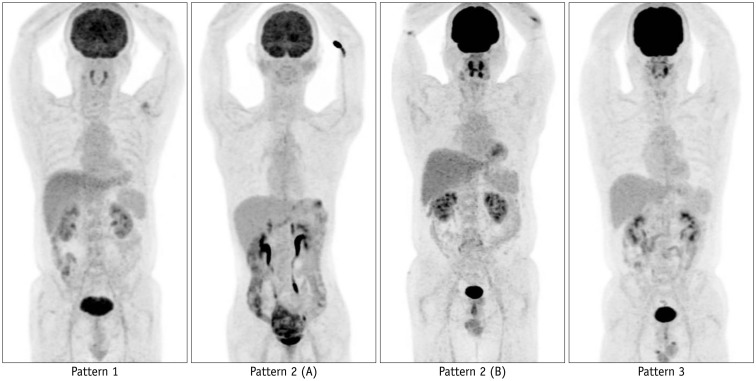
We classified all subjects whose brain SUVmax was below the 25th percentile of the entire study population as having low brain uptake and all subjects whose liver SUVmax was above the 75th percentile as having high liver uptake. According to the combination of brain and liver FDG uptake, we classified all subjects into one of three patterns as follows: pattern 1, concurrent low brain and high liver uptake; pattern 2, either (A) low brain uptake alone or (B) high liver uptake alone; pattern 3, neither (Fig. 1).
Fig. 1. FDG PET maximum intensity projection images of representative subjects according to brain and liver uptake patterns.
Pattern 1, concurrent low brain and high liver FDG uptake; pattern 2 (A), low brain uptake alone or pattern 2 (B), high liver uptake alone; pattern 3, neither. FDG = fluorine-18-labeled fluoro-2-deoxy-D-glucose, PET = Positron emission tomography
Statistical Analysis
Values are expressed as the mean ± standard deviation or number (%). To compare between-group differences, we used the Student's t test or the Mann-Whitney U test, as appropriate, for the continuous variables. We also used the chi-square test or Fisher's exact test for the categorical variables. We compared the three patterns classified by the combination of brain and liver FDG uptake using one-way ANOVA analysis followed by post hoc testing with the Student-Newman-Keuls comparison test, and we used multiple logistic stepwise regression analysis to identify predictive factors for low brain uptake and high liver uptake. We evaluated the correlations between variables using Spearman rho rank correlation analysis. We performed all statistical analyses using MedCalc (ver. 14.12.0, MedCalc Software bvba, Ostend, Belgium) and defined statistical significance as p < 0.05 (two-tailed test).
RESULTS
Subject Characteristics According to the Intensity of FDG Uptake in the Brain and Liver
We classified a total of 264 male subjects (mean 46.1 years; range 38–65 years) according to their brain and liver FDG uptake; the subjects' clinical characteristics are compared in Table 1. The mean SUVmax values for the brain and liver in all subjects were 13.47 ± 2.16 and 3.80 ± 0.50, respectively. Of the 264 subjects, 50 (18.2%) had MS. Compared with subjects without MS, the subjects with MS had lower brain FDG uptake (12.30 ± 2.44 vs. 13.75 ± 2.00, p < 0.001) and higher liver FDG uptake (4.14 ± 0.49 vs. 3.72 ± 0.47, p < 0.001).
Table 1. Subject Characteristics According to Intensity of FDG Uptake in Brain and Liver.
| Variable | Brain Uptake | P | Liver Uptake | P | ||
|---|---|---|---|---|---|---|
| Low (n = 67) | Normal (n = 197) | High (n = 66) | Normal (n = 198) | |||
| SUVmax range | 6.98–12.08 | 12.08–20.74 | 4.155–5.07 | 2.44–4.155 | ||
| Age (years) | 47.6 ± 4.9 | 45.6 ± 4.6 | 0.003* | 45.7 ± 4.7 | 46.2 ± 4.8 | 0.480 |
| SBP (mm Hg) | 127.9 ± 18.9 | 124.9 ± 15.2 | 0.193 | 132.2 ± 16.2 | 123.5 ± 15.7 | < 0.001* |
| DBP (mm Hg) | 78.5 ± 12.5 | 76.7 ± 11.0 | 0.277 | 80.8 ± 9.8 | 75.9 ± 11.7 | 0.003* |
| Waist (cm) | 83.9 ± 7.8 | 85.7 ± 7.8 | 0.086 | 92.0 ± 7.2 | 83.0 ± 6.6 | < 0.001* |
| FBG (mg/dL) | 107.0 ± 20.6 | 91.3 ± 9.3 | < 0.001* | 99.2 ± 20.1 | 94.0 ± 12.3 | 0.182 |
| HDLc (mg/dL) | 55.7 ± 16.6 | 55.8 ± 14.6 | 0.566 | 52.8 ± 12.0 | 56.8 ± 15.9 | 0.088 |
| TG (mg/dL) | 143.5 ± 83.2 | 131.6 ± 79.2 | 0.276 | 165.9 ± 82.2 | 124.2 ± 77.0 | < 0.001* |
| Total cholesterol (mg/dL) | 202.9 ± 36.2 | 201.9 ± 35.0 | 0.837 | 213.6 ± 35.4 | 198.3 ± 34.5 | 0.002* |
| LDLc (mg/dL) | 134.3 ± 34.3 | 133.1 ± 32.5 | 0.798 | 144.4 ± 33.0 | 129.8 ± 32.2 | 0.002* |
| AST (IU/L) | 26.2 ± 11.6 | 23.7 ± 7.0 | 0.426 | 26.9 ± 9.3 | 23.5 ± 8.0 | 0.003* |
| ALT (IU/L) | 27.4 ± 15.9 | 26.1 ± 14.0 | 0.945 | 33.7 ± 16.6 | 24.0 ± 12.9 | < 0.001* |
| γ-GT (IU/L) | 48.5 ± 45.7 | 44.0 ± 44.7 | 0.082 | 69.2 ± 58.8 | 37.1 ± 36.0 | < 0.001* |
| ALP (IU/L) | 76.0 ± 20.3 | 76.2 ± 17.8 | 0.651 | 75.6 ± 18.7 | 76.4 ± 18.4 | 0.745 |
| Total bilirubin (mg/dL) | 0.86 ± 0.30 | 0.91 ± 0.40 | 0.660 | 0.91 ± 0.41 | 0.90 ± 0.37 | 0.814 |
| Total protein (g/dL) | 7.36 ± 0.40 | 7.75 ± 4.55 | 0.318 | 7.50 ± 0.34 | 7.70 ± 4.54 | 0.053 |
| BUN (mg/dL) | 13.8 ± 3.1 | 13.8 ± 2.8 | 0.981 | 13.9 ± 2.6 | 13.8 ± 3.0 | 0.846 |
| Creatinine (mg/dL) | 0.96 ± 0.12 | 1.00 ± 0.11 | 0.063 | 1.00 ± 0.12 | 0.98 ± 0.12 | 0.169 |
| ESR (mm/hr) | 4.50 ± 4.17 | 5.13 ± 4.82 | 0.400 | 5.91 ± 4.17 | 4.65 ± 4.79 | 0.001 |
| hsCRP (mg/L) | 1.44 ± 2.83 | 1.32 ± 4.66 | 0.828 | 1.46 ± 2.10 | 1.32 ± 4.77 | 0.028 |
| HOMA-IR | 1.37 ± 1.01 | 1.15 ± 0.77 | 0.207 | 1.65 ± 1.08 | 1.06 ± 0.69 | < 0.001* |
| Insulin (µIU/mL) | 5.46 ± 3.22 | 5.58 ± 3.60 | 0.922 | 7.35 ± 4.57 | 4.96 ± 2.85 | < 0.001* |
| TSH (µIU/mL) | 1.89 ± 1.24 | 1.84 ± 1.02 | 0.795 | 2.07 ± 0.99 | 1.78 ± 1.10 | 0.006* |
| BMI (kg/m2) | 24.3 ± 2.8 | 24.7 ± 3.0 | 0.286 | 27.0 ± 2.9 | 23.8 ± 2.5 | < 0.001* |
| HbA1c (%) | 5.96 ± 0.87 | 5.38 ± 0.33 | < 0.001* | 5.69 ± 0.65 | 5.47 ± 0.54 | 0.001* |
| Presence of MS | 24 (35.8) | 26 (13.2) | < 0.001* | 26 (39.4) | 24 (12.1) | < 0.001* |
| No. of MS components | 1.81 ± 1.42 | 1.17 ± 1.18 | < 0.001* | 2.17 ± 1.34 | 1.06 ± 1.12 | < 0.001* |
| DM | 16 (23.9) | 4 (2.0) | < 0.001* | 8 (12.1) | 12 (6.1) | 0.179 |
| DM medication | 11 (16.4) | 9 (4.6) | 0.004* | 6 (9.1) | 14 (7.1) | 0.788 |
| HTN | 28 (41.8) | 48 (24.4) | 0.010* | 26 (39.4) | 50 (25.3) | 0.041* |
| HTN medication | 12 (17.9) | 3 (1.5) | < 0.001* | 5 (7.6) | 10 (5.1) | 0.645 |
| Statin medication | 2 (3.0) | 3 (1.5) | 0.604 | 3 (4.5) | 2 (1.0) | 0.101 |
| Current smoking | 37 (55.2) | 92 (46.7) | 0.287 | 30 (45.5) | 99 (50.0) | 0.619 |
| FRS (%) | 7.45 ± 5.57 | 5.73 ± 4.71 | 0.014* | 6.98 ± 5.48 | 5.89 ± 4.80 | 0.128 |
| Fatty liver | 33 (49.3) | 68 (34.5) | 0.042* | 43 (65.2) | 58 (29.3) | < 0.001* |
| Brain SUVmax | 10.80 ± 1.16 | 14.38 ± 1.59 | < 0.001* | 14.00 ± 2.51 | 13.30 ± 2.01 | 0.005* |
| Liver SUVmax | 3.68 ± 0.48 | 3.84 ± 0.50 | 0.021* | 4.42 ± 0.23 | 3.59 ± 0.37 | < 0.001* |
Data are presented as mean ± SD or number (%). *p < 0.05. ALP = alkaline phosphatase, ALT = alanine aminotransferase, AST = aspartate aminotransferase, BMI = body mass index, BUN = blood urea nitrogen, DBP = diastolic blood pressure, DM = diabetes mellitus, ESR = erythrocyte sedimentation rate, FBG = fasting blood glucose, FRS = Framingham risk score, HbA1c = glycated hemoglobin, HDLc = high-density lipoprotein cholesterol, HOMA-IR = homeostasis model assessment of insulin resistance, hsCRP = high-sensitivity C-reactive protein, HTN = hypertension, LDLc = low-density lipoprotein cholesterol, MS = metabolic syndrome, SBP = systolic blood pressure, SUVmax = maximum standardized uptake value, TG = triglyceride, TSH = thyroid–stimulating hormone, γ-GT = γ-glutamyl transpeptidase
Age (p = 0.003), FBG (p < 0.001), AST (p = 0.037), HbA1c (p < 0.001), the number of MS components (p < 0.001), FRS (p = 0.017), and fatty liver (p = 0.037) were associated with brain FDG uptake. SBP (p < 0.001), DBP (p = 0.003), waist circumference (p < 0.001), FBG (p = 0.018), TG (p = 0.001), total cholesterol (p = 0.003), LDLc (p = 0.002), AST (p = 0.007), ALT (p < 0.001), γ-GT (p < 0.001), HOMA-IR (p < 0.001), insulin (p < 0.001), BMI (p < 0.001), HbA1c (p = 0.012), the number of MS components (p < 0.001), and fatty liver (p < 0.001) were associated with liver FDG uptake. We conducted multiple logistic stepwise regression analysis including these factors, and the results revealed that FBG and HbA1c were the strongest predictive factors for low brain FDG uptake and waist circumference and γ-GT were the strongest predictors for high liver FDG uptake (Table 2).
Table 2. Multiple Logistic Stepwise Regression Analysis of Low Brain (A) and High Liver FDG Uptake (B).
| Variable | Odds Ratio | 95% Confidence Interval | P |
|---|---|---|---|
| (A) Brain | |||
| HbA1c (%) | 3.634 | 1.369–9.641 | 0.010 |
| FBG (mg/dL) | 1.063 | 1.026–1.101 | < 0.001 |
| (B) Liver | |||
| Waist (cm) | 1.200 | 1.133–1.270 | < 0.001 |
| γ-GT (IU/L) | 1.012 | 1.005–1.020 | 0.001 |
FBG = fasting blood glucose, HbA1c = glycated hemoglobin, γ-GT = γ-glutamyl transpeptidase
Comparison of MS Components According to FDG Uptake by the Brain and Liver in Subjects with and without MS
Regardless of the presence of MS, subjects with low brain FDG uptake had significantly higher FBG levels than did those with high FDG uptake (with MS; 122.7 ± 23.6 mg/dL vs. 96.9 ± 9.5 mg/dL, p < 0.001, without MS; 98.2 ± 11.9 mg/dL vs. 90.5 ± 9.0 mg/dL, p < 0.001). Moreover, subjects with high liver FDG uptake had significantly larger waist circumferences than those of the men with low FDG uptake (with MS; 95.2 ± 5.9 cm vs. 89.1 ± 7.1 cm, p = 0.002, without MS; 90.0 ± 7.3 cm vs. 82.2 ± 6.1 cm, p < 0.001) (Table 3).
Table 3. Comparison of MS Components According to FDG Uptake by Brain (A) and Liver (B) in Subjects with and without MS.
| Variable | With MS | P | Without MS | P | ||
|---|---|---|---|---|---|---|
| Low (n = 24) | Normal (n = 26) | Low (n = 43) | Normal (n = 171) | |||
| (A) Brain | ||||||
| SBP (mm Hg) | 140.3 ± 19.5 | 141.5 ± 14.2 | 0.802 | 121.0 ± 14.7 | 122.4 ± 13.8 | 0.561 |
| DBP (mm Hg) | 84.8 ± 11.4 | 87.1 ± 10.8 | 0.471 | 74.9 ± 11.7 | 75.1 ± 10.2 | 0.912 |
| Waist (cm) | 90.4 ± 6.8 | 94.0 ± 7.1 | 0.073 | 80.2 ± 5.6 | 84.5 ± 7.1 | < 0.001* |
| FBG (mg/dL) | 122.7 ± 23.6 | 96.9 ± 9.5 | < 0.001* | 98.2 ± 11.9 | 90.5 ± 9.0 | < 0.001* |
| HDLc (mg/dL) | 45.1 ± 7.1 | 46.7 ± 12.0 | 0.572 | 61.6 ± 17.4 | 57.2 ± 14.5 | 0.139 |
| TG (mg/dL) | 216.0 ± 85.9 | 229.8 ± 75.7 | 0.549 | 103.1 ± 46.5 | 116.6 ± 68.5 | 0.220 |
Data are presented as mean ± SD. *p < 0.05. DBP = diastolic blood pressure, FBG = fasting blood glucose, HDLc = high-density lipoprotein cholesterol, MS = metabolic syndrome, SBP = systolic blood pressure, TG = triglyceride
Comparison of Clinical Variables among Three Patterns Classified by Combination of Brain and Liver FDG Uptake
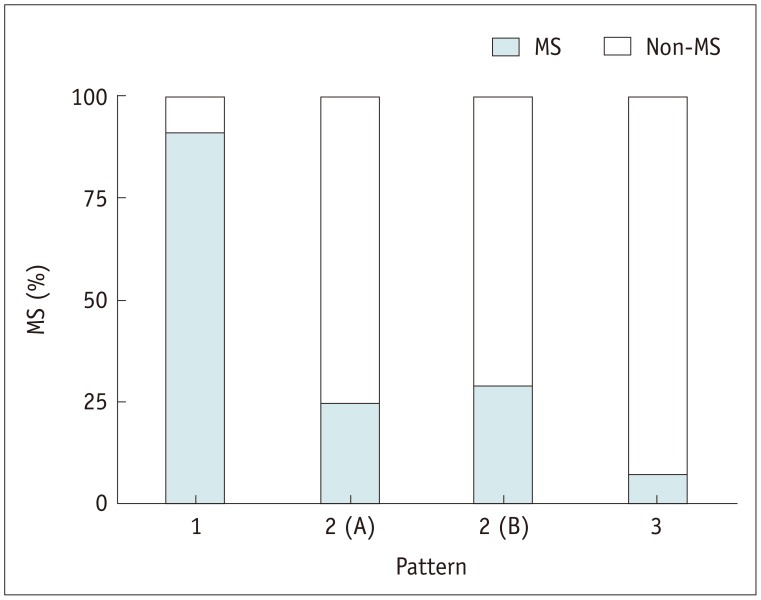
Eleven subjects (4.2%) showed concurrent low brain and high liver FDG uptake, and all but one of these subjects (90.9%) had MS. Of the 142 subjects with pattern 3, 132 (93.0%) did not have MS (Fig. 2), and the proportion of MS in subjects with pattern 2 was 27.0% (30/111). Subjects with pattern 1 had higher values for SBP, waist circumference, FBG, TG, ALT, HOMA-IR, insulin, HbA1c, and BMI than did those with patterns 2 or 3 (Table 4). Subjects with pattern 2 had higher values for SBP, DBP, waist circumference, FBG, TG, total cholesterol, LDL, AST, ALT, γ-GT, HOMA-IR, HbA1c, BMI, and FRS than did those with pattern 3. FRS was correlated with brain (r = -0.183, p = 0.003) and liver (r = 0.122, p = 0.047) FDG uptake.
Fig. 2. Presence of metabolic syndrome (MS) according to brain and liver FDG uptake patterns.
Proportions of MS were 90.9% in subjects with pattern 1, 25.0% in subjects with pattern 2 (A), 29.1% in subjects with pattern 2 (B), and 7.0% in subjects with pattern 3. Pattern 1, concurrent low brain and high liver FDG uptake; pattern 2 (A), low brain uptake alone or pattern 2 (B), high liver uptake alone; pattern 3, neither (normal uptake pattern). FDG = fluorine-18-labeled fluoro-2-deoxy-D-glucose
Table 4. Comparison of Clinical Variables among Patterns Classified by Combination of Low Brain and High Liver FDG Uptake.
| Variable | Pattern 1 (n = 11) | Pattern 2 (n = 111) | Pattern 3 (n = 142) | P |
|---|---|---|---|---|
| Age (years) | 47.0 ± 4.5 | 46.6 ± 5.0 | 45.6 ± 4.6 | 0.241 |
| Brain SUVmax | 9.84 ± 1.62 a | 12.89 ± 2.36 b | 14.21 ± 1.52 c | < 0.001* |
| Liver SUVmax | 4.46 ± 0.23 a | 3.97 ± 0.54 b | 3.61 ± 0.38 c | < 0.001* |
| SBP (mm Hg) | 144.1 ± 18.5 a | 127.2 ± 16.3 b | 123.0 ± 15.0 c | < 0.001* |
| DBP (mm Hg) | 84.5 ± 11.3 a | 78.7 ± 11.1 a | 75.4 ± 11.3 b | 0.007* |
| Waist (cm) | 92.9 ± 5.3 a | 86.9 ± 8.7 b | 83.4 ± 6.5 c | < 0.001* |
| FBG (mg/dL) | 132.5 ± 26.8 a | 97.3 ± 13.2 b | 90.8 ± 9.4 c | < 0.001* |
| HDLc (mg/dL) | 45.2 ± 4.2 | 56.0 ± 15.1 | 56.4 ± 15.4 | 0.057 |
| TG (mg/dL) | 197.1 ± 84.0 a | 146.2 ± 81.1 b | 120.7 ± 76.0 c | < 0.001* |
| Total cholesterol (mg/dL) | 202.8 ± 31.4 | 209.3 ± 37.1 a | 196.5 ± 33.2 b | 0.016* |
| LDLc (mg/dL) | 134.1 ± 30.4 | 140.4 ± 34.7 a | 128.0 ± 30.8 b | 0.012* |
| AST (IU/L) | 26.8 ± 12.4 a | 26.5 ± 10.2 a | 22.4 ± 5.7 b | < 0.001* |
| ALT (IU/L) | 38.2 ± 21.7 a | 29.0 ± 15.0 b | 23.6 ± 12.6 c | < 0.001* |
| ALP (IU/L) | 73.6 ± 20.2 | 76.3 ± 19.4 | 76.3 ± 17.6 | 0.896 |
| γ-GT (IU/L) | 58.1 ± 41.7 a | 58.9 ± 55.8 a | 33.4 ± 30.2 b | < 0.001* |
| Total protein (g/dL) | 7.45 ± 0.42 | 7.42 ± 0.37 | 7.84 ± 5.35 | 0.695 |
| Total bilirubin (mg/dL) | 0.80 ± 0.36 | 0.90 ± 0.36 | 0.90 ± 0.39 | 0.694 |
| BUN (mg/dL) | 15.5 ± 2.3 | 13.5 ± 2.9 | 13.9 ± 2.9 | 0.073 |
| Creatinine (mg/dL) | 0.98 ± 0.13 | 0.98 ± 0.12 | 0.99 ± 0.11 | 0.922 |
| ESR (mm/hr) | 4.00 ± 2.93 | 5.43 ± 4.40 | 4.68 ± 4.95 | 0.346 |
| hsCRP (mg/L) | 1.72 ± 1.67 | 1.40 ± 2.63 | 1.29 ± 5.32 | 0.943 |
| HOMA-IR | 2.63 ± 1.03 a | 1.28 ± 0.91 b | 1.03 ± 0.64 c | < 0.001* |
| Insulin (µIU/mL) | 9.15 ± 3.75 a | 5.84 ± 3.90 b | 5.05 ± 2.96 b | < 0.001* |
| HbA1c (%) | 6.75 ± 0.84 a | 5.64 ± 0.63 b | 5.33 ± 0.32 c | < 0.001* |
| TSH (µIU/mL) | 2.21 ± 1.24 | 1.93 ± 1.11 | 1.76 ± 1.05 | 0.229 |
| BMI (kg/m2) | 27.3 ± 2.2 a | 25.3 ± 3.2 b | 23.9 ± 2.5 c | < 0.001* |
| FRS (%) | 8.55 ± 6.85 a | 6.96 ± 5.24 a | 5.36 ± 4.49 b | 0.011* |
| Fatty liver | 10 (90.9) | 56 (50.5) | 35 (24.6) | < 0.001* |
| Current smoking | 5 (45.5) | 57 (51.4) | 67 (47.2) | 0.784 |
| Presence of MS | 10 (90.9) | 30 (27.0) | 10 (7.0) | < 0.001* |
| DM | 7 (63.6) | 10 (9.0) | 3 (2.1) | < 0.001* |
| HTN | 8 (72.7) | 38 (26.8) | 30 (21.1) | < 0.001* |
Data are presented as mean ± SD or number (%). Pattern 1, concurrent low brain and high liver FDG uptake; pattern 2, either low brain or high liver FDG uptake; pattern 3, without either. a–c, same letter indicates nonsignificant difference between groups based on Student-Newman-Kuels multiple comparison test. *p < 0.05. ALP = alkaline phosphatase, ALT = alanine aminotransferase, AST = aspartate aminotransferase, BMI = body mass index, BUN = blood urea nitrogen, DBP = diastolic blood pressure, DM = diabetes mellitus, ESR = erythrocyte sedimentation rate, FBG = fasting blood glucose, FRS = Framingham risk score, HbA1c = glycated hemoglobin, HDLc = high-density lipoprotein cholesterol, HOMA-IR = homeostasis model assessment of insulin resistance, hsCRP = high-sensitivity C-reactive protein, HTN = hypertension, LDLc = low-density lipoprotein cholesterol, MS = metabolic syndrome, SBP = systolic blood pressure, SUVmax = maximum standardized uptake value, TG = triglyceride, TSH = thyroid–stimulating hormone, γ-GT = γ-glutamyl transpeptidase
DISCUSSION
The present study demonstrated that various clinical and hematological factors are associated with metabolic activity in the brain and liver, as measured by FDG PET, and subjects with concurrent low brain and high liver FDG uptake had a higher prevalence of MS. MS is a potent predictor of future cardiovascular disease and its prevalence (20,21). Thus, we evaluated the relationship between this FDG uptake pattern and cardiovascular risk. The results revealed that subjects with this FDG uptake pattern had higher values for the various factors that are closely associated with cardiovascular risk than subjects without this pattern.
In this study, FBG and HbA1c were the strongest determinants of brain FDG uptake; brain SUVmax was significantly lower in subjects with high FBG, regardless of the presence of MS. Glucose is a major substrate for brain energy metabolism, and in the hyperglycemic state, excess unlabeled glucose and the action of insulin can alter FDG accumulation in the body as follows. First, glucose transporters (GLUTs) become saturated in the presence of excess unlabeled glucose (22,23). Second, plasma insulin levels increase, resulting in translocation of GLUT-4 from an intracellular pool to the plasma membrane (24,25). Whereas saturation with unlabeled glucose is likely to reduce FDG uptake in insulin-insensitive organs such as the brain, insulin is likely to increase FDG uptake in insulin-sensitive tissues such as the myocardium and muscles. This implies that the saturation effect of unlabeled serum glucose is more evident in tissues with high glucose metabolism than in organs with lower glucose demands. One study also demonstrated that blood glucose only exerts a significant impact on FDG uptake in the brain, where there is a high level of glucose metabolism, whereas a nonsignificant effect was observed in organs that consume less glucose such as the liver and spleen (2). Because HbA1c reflects average plasma glucose over the previous eight to 12 weeks (26), this finding implies that chronically uncontrolled hyperglycemia also has a significant influence on brain FDG uptake as well as acute hyperglycemia. However, serum glucose levels (< 180 mg/dL) were sufficiently low in the present study that they may not have saturated the GLUTs, and therefore, other mechanisms should be considered. Insulin resistance, which is broadly defined as reduced tissue responsiveness to the action of insulin, is one possible explanation. Insulin increase and subsequent GLUT activation is a normal response to hyperglycemia, whereas it appears that dysglycemia is the main cause of low FDG uptake in the brain; in dysglycemia, high serum glucose is not the cause but the result of peripheral insulin resistance. Peripheral insulin resistance strongly corresponds to brain insulin resistance owing to reduced insulin transport into the brain or potentially similar changes in receptor sensitivity and activation (27,28), and insulin resistance leads to decreased GLUT1 and GLUT3 expression and consequent glucose uptake in the brain (29). This may be why our enrolled subjects showed different brain FDG uptake despite exhibiting similar insulin levels (p = 0.922).
In contrast to brain FDG uptake, FBG did not influence liver FDG uptake. Moreover, we observed no differences in the serum FBG levels of subjects with high versus normal liver uptake regardless of the presence of MS. The strongest determinants of liver FDG uptake were waist circumference and γ-GT, which supports the findings of a previous study that found that BMI was the strongest determinant (13). Both waist circumference and BMI are regarded as obesity-related factors, and obesity is associated with increased plasma levels of inflammatory cytokines such as tumor necrosis factor-α (TNF-α) and interleukin-6 (IL-6). Altered long-term expression of liver metabolic enzymes mediated by TNF-α and IL-6 may be critical in the transition to a chronic inflammatory state (30). Because the sites of FDG accumulation in infectious lesions are located in migratory inflammatory cells such as macrophages (31), high liver uptake may be induced by the inflammatory state of the liver in obese subjects. One previous study reported that inflammation is a primary cause of hyperlipidemia (32). Liver inflammation and fibrosis have both been associated with the presence and severity of MS (33), and therefore, high FDG uptake by the liver indicates more severe MS. Elevated serum γ-GT has been suggested to be a marker of excess fat deposition in the liver. Serum γ-GT is closely related to obesity and visceral fat deposition, and is involved in inflammatory response (34,35,36). However, considering that the chronic, low-active, systemic inflammation related to obesity has been observed primarily in adipose tissue, the speculation that increased liver uptake is caused by inflammation needs to be supported by evidence that inflammation is more active in the liver than in adipose or other tissues in the body. An even distribution of inflammatory activity does not lead to observed differences in regional uptake. In addition, FDG uptake in fat is very low (37). The FDG uptake of non-fatty tissues may be influenced by the distribution and volume of fatty tissue in obese subjects. Given the zero-sum nature of FDG uptake in the body (38), increased non-FDG-avid fatty tissue may result in increased liver FDG uptake, and this may explain the significant correlations between liver FDG uptake and obesity.
Interestingly, waist circumference exhibited a positive, albeit weak, association with brain FDG uptake (Spearman rho rank correlation coefficient = 0.199, p = 0.001) and was also greater in subjects who exhibited normal uptake than in those who had low uptake in the brain regardless of the presence of MS. These results differ from our expectations that the brain would show lower FDG uptake in obese than in non-obese subjects due to insulin resistance; a previous study of 28 obese patients (2) did not detect any differences in brain FDG uptake between obese and non-obese patients (12.6 ± 4.5 vs. 11.6 ± 3.9, p = 0.308). Taken together, it is unlikely that increased waist circumference leads to decreased brain activity, although the extent of correlation between these two factors remains unclear. More studies are needed to clarify this relationship.
In the current study, subjects with pattern 1 had higher values for SBP, waist circumference, FBG, TG, ALT, HbA1c, insulin, HOMA-IR, and BMI, which are all closely associated with cardiovascular risk. Subjects with pattern 1 had high FRS compared with those with pattern 3, although there was no significant difference compared with the values in the pattern 2 subjects. In addition, FRS was negatively correlated with brain (r = -0.183, p = 0.003) FDG uptake and positively correlated with liver (r = 0.122, p = 0.047) FDG uptake. In addition, because subjects with pattern 2 had higher values for various cardiovascular risk factors compared with those with pattern 3, subjects with either low brain or high liver uptake should also be evaluated for cardiovascular disease.
This study had some limitations. First, the study was cross-sectional and retrospective in design and thus could not clarify the causal relationships between brain uptake, liver uptake, and cardiovascular risk factors. Second, only males were included in the study because very few females had undergone general health check-ups at our institution. In addition, the number of subjects 55 years or older (n = 19, 7.2%) was relatively small, which may weaken the findings of this study. Studies with females and more subjects older than 55 years are needed to validate the findings of the present study. Third, the present study only included clinical and laboratory data that were available from general health check-ups at our institution; thus, other factors that could affect glucose metabolism in the brain or liver could have been missed. Despite these limitations, the present study is the first to demonstrate that incidentally concurrent low brain and high liver FDG uptake are associated with various cardiovascular risk factors.
In conclusion, concurrent low brain and high liver FDG uptake were closely associated with MS, and therefore, when this pattern is incidentally found on FDG PET, subjects should be further evaluated for MS. Moreover, subjects with this pattern had higher values for various cardiovascular risk factors compared with those without it, and a longitudinal study is needed to verify whether this FDG uptake pattern is directly related to cardiovascular events.
References
- 1.Strauss LG, Conti PS. The applications of PET in clinical oncology. J Nucl Med. 1991;32:623–648. discussion 649-650. [PubMed] [Google Scholar]
- 2.Büsing KA, Schönberg SO, Brade J, Wasser K. Impact of blood glucose, diabetes, insulin, and obesity on standardized uptake values in tumors and healthy organs on 18F-FDG PET/CT. Nucl Med Biol. 2013;40:206–213. doi: 10.1016/j.nucmedbio.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 3.Minamimoto R, Takahashi N, Inoue T. FDG-PET of patients with suspected renal failure: standardized uptake values in normal tissues. Ann Nucl Med. 2007;21:217–222. doi: 10.1007/s12149-007-0012-4. [DOI] [PubMed] [Google Scholar]
- 4.Langbaum JB, Chen K, Launer LJ, Fleisher AS, Lee W, Liu X, et al. Blood pressure is associated with higher brain amyloid burden and lower glucose metabolism in healthy late middle-age persons. Neurobiol Aging. 2012;33:827.e11–827.e19. doi: 10.1016/j.neurobiolaging.2011.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reiman EM, Chen K, Langbaum JB, Lee W, Reschke C, Bandy D, et al. Higher serum total cholesterol levels in late middle age are associated with glucose hypometabolism in brain regions affected by Alzheimer's disease and normal aging. Neuroimage. 2010;49:169–176. doi: 10.1016/j.neuroimage.2009.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miao Q, Zhang S, Guan YH, Ye HY, Zhang ZY, Zhang QY, et al. Reversible changes in brain glucose metabolism following thyroid function normalization in hyperthyroidism. AJNR Am J Neuroradiol. 2011;32:1034–1042. doi: 10.3174/ajnr.A2449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loessner A, Alavi A, Lewandrowski KU, Mozley D, Souder E, Gur RE. Regional cerebral function determined by FDG-PET in healthy volunteers: normal patterns and changes with age. J Nucl Med. 1995;36:1141–1149. [PubMed] [Google Scholar]
- 8.Petit-Taboué MC, Landeau B, Desson JF, Desgranges B, Baron JC. Effects of healthy aging on the regional cerebral metabolic rate of glucose assessed with statistical parametric mapping. Neuroimage. 1998;7:176–184. doi: 10.1006/nimg.1997.0318. [DOI] [PubMed] [Google Scholar]
- 9.Ivançevic’ V, Alavi A, Souder E, Mozley PD, Gur RE, Bénard F, et al. Regional cerebral glucose metabolism in healthy volunteers determined by fluordeoxyglucose positron emission tomography: appearance and variance in the transaxial, coronal, and sagittal planes. Clin Nucl Med. 2000;25:596–602. doi: 10.1097/00003072-200008000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Liu G, Li Y, Hu P, Cheng D, Shi H. The combined effects of serum lipids, BMI, and fatty liver on 18F-FDG uptake in the liver in a large population from China: an 18F-FDG-PET/CT study. Nucl Med Commun. 2015;36:709–716. doi: 10.1097/MNM.0000000000000301. [DOI] [PubMed] [Google Scholar]
- 11.Kuruva M, Mittal BR, Abrar ML, Kashyap R, Bhattacharya A. Multivariate analysis of various factors affecting background liver and mediastinal standardized uptake values. Indian J Nucl Med. 2012;27:20–23. doi: 10.4103/0972-3919.108835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kubota K, Watanabe H, Murata Y, Yukihiro M, Ito K, Morooka M, et al. Effects of blood glucose level on FDG uptake by liver: a FDG-PET/CT study. Nucl Med Biol. 2011;38:347–351. doi: 10.1016/j.nucmedbio.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 13.Kamimura K, Nagamachi S, Wakamatsu H, Higashi R, Ogita M, Ueno S, et al. Associations between liver (18)F fluoro-2-deoxy-D-glucose accumulation and various clinical parameters in a Japanese population: influence of the metabolic syndrome. Ann Nucl Med. 2010;24:157–161. doi: 10.1007/s12149-009-0338-1. [DOI] [PubMed] [Google Scholar]
- 14.Lin CY, Ding HJ, Lin T, Lin CC, Kuo TH, Kao CH. Positive correlation between serum liver enzyme levels and standard uptake values of liver on FDG-PET. Clin Imaging. 2010;34:109–112. doi: 10.1016/j.clinimag.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 15.Lin CY, Ding HJ, Lin CC, Chen CC, Sun SS, Kao CH. Impact of age on FDG uptake in the liver on PET scan. Clin Imaging. 2010;34:348–350. doi: 10.1016/j.clinimag.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 17.Roy FN, Beaulieu S, Boucher L, Bourdeau I, Cohade C. Impact of intravenous insulin on 18F-FDG PET in diabetic cancer patients. J Nucl Med. 2009;50:178–183. doi: 10.2967/jnumed.108.056283. [DOI] [PubMed] [Google Scholar]
- 18.Delbeke D, Meyerowitz C, Lapidus RL, Maciunas RJ, Jennings MT, Moots PL, et al. Optimal cutoff levels of F-18 fluorodeoxyglucose uptake in the differentiation of low-grade from high-grade brain tumors with PET. Radiology. 1995;195:47–52. doi: 10.1148/radiology.195.1.7892494. [DOI] [PubMed] [Google Scholar]
- 19.Adams MC, Turkington TG, Wilson JM, Wong TZ. A systematic review of the factors affecting accuracy of SUV measurements. AJR Am J Roentgenol. 2010;195:310–320. doi: 10.2214/AJR.10.4923. [DOI] [PubMed] [Google Scholar]
- 20.Dekker JM, Girman C, Rhodes T, Nijpels G, Stehouwer CD, Bouter LM, et al. Metabolic syndrome and 10-year cardiovascular disease risk in the Hoorn study. Circulation. 2005;112:666–673. doi: 10.1161/CIRCULATIONAHA.104.516948. [DOI] [PubMed] [Google Scholar]
- 21.Ford ES, Li C, Zhao G. Prevalence and correlates of metabolic syndrome based on a harmonious definition among adults in the US. J Diabetes. 2010;2:180–193. doi: 10.1111/j.1753-0407.2010.00078.x. [DOI] [PubMed] [Google Scholar]
- 22.Crippa F, Gavazzi C, Bozzetti F, Chiesa C, Pascali C, Bogni A, et al. The influence of blood glucose levels on [18F]fluorodeoxyglucose (FDG) uptake in cancer: a PET study in liver metastases from colorectal carcinomas. Tumori. 1997;83:748–752. doi: 10.1177/030089169708300407. [DOI] [PubMed] [Google Scholar]
- 23.Lindholm P, Minn H, Leskinen-Kallio S, Bergman J, Ruotsalainen U, Joensuu H. Influence of the blood glucose concentration on FDG uptake in cancer--a PET study. J Nucl Med. 1993;34:1–6. [PubMed] [Google Scholar]
- 24.Cheung JY, Conover C, Regen DM, Whitfield CF, Morgan HE. Effect of insulin on kinetics of sugar transport in heart muscle. Am J Physiol. 1978;234:E70–E78. doi: 10.1152/ajpendo.1978.234.1.E70. [DOI] [PubMed] [Google Scholar]
- 25.Sun D, Nguyen N, DeGrado TR, Schwaiger M, Brosius FC., 3rd Ischemia induces translocation of the insulin-responsive glucose transporter GLUT4 to the plasma membrane of cardiac myocytes. Circulation. 1994;89:793–798. doi: 10.1161/01.cir.89.2.793. [DOI] [PubMed] [Google Scholar]
- 26.Nathan DM, Turgeon H, Regan S. Relationship between glycated haemoglobin levels and mean glucose levels over time. Diabetologia. 2007;50:2239–2244. doi: 10.1007/s00125-007-0803-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Talbot K, Wang HY, Kazi H, Han LY, Bakshi KP, Stucky A, et al. Demonstrated brain insulin resistance in Alzheimer's disease patients is associated with IGF-1 resistance, IRS-1 dysregulation, and cognitive decline. J Clin Invest. 2012;122:1316–1338. doi: 10.1172/JCI59903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Messier C, Teutenberg K. The role of insulin, insulin growth factor, and insulin-degrading enzyme in brain aging and Alzheimer's disease. Neural Plast. 2005;12:311–328. doi: 10.1155/NP.2005.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deng Y, Li B, Liu Y, Iqbal K, Grundke-Iqbal I, Gong CX. Dysregulation of insulin signaling, glucose transporters, O-GlcNAcylation, and phosphorylation of tau and neurofilaments in the brain: implication for Alzheimer's disease. Am J Pathol. 2009;175:2089–2098. doi: 10.2353/ajpath.2009.090157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith SR, Ravussin E. Emerging paradigms for understanding fatness and diabetes risk. Curr Diab Rep. 2002;2:223–230. doi: 10.1007/s11892-002-0087-1. [DOI] [PubMed] [Google Scholar]
- 31.Kubota R, Yamada S, Kubota K, Ishiwata K, Tamahashi N, Ido T. Intratumoral distribution of fluorine-18-fluorodeoxyglucose in vivo: high accumulation in macrophages and granulation tissues studied by microautoradiography. J Nucl Med. 1992;33:1972–1980. [PubMed] [Google Scholar]
- 32.Wellen KE, Hotamisligil GS. Inflammation, stress, and diabetes. J Clin Invest. 2005;115:1111–1119. doi: 10.1172/JCI25102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rector RS, Thyfault JP, Wei Y, Ibdah JA. Non-alcoholic fatty liver disease and the metabolic syndrome: an update. World J Gastroenterol. 2008;14:185–192. doi: 10.3748/wjg.14.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marchesini G, Brizi M, Bianchi G, Tomassetti S, Bugianesi E, Lenzi M, et al. Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes. 2001;50:1844–1850. doi: 10.2337/diabetes.50.8.1844. [DOI] [PubMed] [Google Scholar]
- 35.Lee DH, Jacobs DR., Jr Association between serum gamma-glutamyltransferase and C-reactive protein. Atherosclerosis. 2005;178:327–330. doi: 10.1016/j.atherosclerosis.2004.08.027. [DOI] [PubMed] [Google Scholar]
- 36.Kang YH, Min HK, Son SM, Kim IJ, Kim YK. The association of serum gamma glutamyltransferase with components of the metabolic syndrome in the Korean adults. Diabetes Res Clin Pract. 2007;77:306–313. doi: 10.1016/j.diabres.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 37.Zasadny KR, Wahl RL. Standardized uptake values of normal tissues at PET with 2-[fluorine-18]-fluoro-2-deoxy-D-glucose: variations with body weight and a method for correction. Radiology. 1993;189:847–850. doi: 10.1148/radiology.189.3.8234714. [DOI] [PubMed] [Google Scholar]
- 38.Lindholm H, Johansson O, Jonsson C, Jacobsson H. The distribution of FDG at PET examinations constitutes a relative mechanism: significant effects at activity quantification in patients with a high muscular uptake. Eur J Nucl Med Mol Imaging. 2012;39:1685–1690. doi: 10.1007/s00259-012-2202-0. [DOI] [PubMed] [Google Scholar]