Abstract
Tibial plateau fractures are common injuries that occur in a bimodal age distribution. While there are various treatment options for displaced tibial plateau fractures, the standard of care is open reduction and internal fixation (ORIF). In physiologically young patients with higher demand and better bone quality, ORIF is the preferred method of treating these fractures. However, future total knee arthroplasty (TKA) is a consideration in these patients as post-traumatic osteoarthritis is a common long-term complication of tibial plateau fractures. In older, lower demand patients, ORIF is potentially less favorable for a variety of reasons, namely fixation failure and the need for delayed weight bearing. In some of these patients, TKA can be considered as primary mode of treatment. This paper will review the literature surrounding TKA as both primary treatment and as a salvage measure in patients with fractures of the tibial plateau. The outcomes, complications, techniques and surgical challenges are also discussed.
Keywords: Arthroplasty, Knee, Tibia, Intra-articular fractures, Fracture fixation
Core tip: It is well known that patients undergoing open reduction and internal fixation (ORIF) following tibial plateau fracture have a high rate of post-traumatic arthritis (PTOA) requiring total knee arthroplasty (TKA) in the future. Currently, ORIF is the standard of care for all patients requiring operative management. Small groups of select patients have shown good results with TKA as primary treatment of tibial plateau fracture. This group includes elderly patients with poor bone stock who are shown to have high rates of post-traumatic arthritis and fixation failure. In younger and more active patients, the options for salvage TKA in the case of PTOA is discussed, as this procedure is more complex than primary TKA.
INTRODUCTION
Tibial plateau fracture is a common injury of the lower extremity that is seen in the population with a bimodal age distribution. These injuries are often categorized using the Schatzker classification, which can be been used to classify the fracture pattern and oftentimes dictate treatment. Type I, II and III fractures involve the lateral plateau. Type IV fractures involve the medial plateau, while type V describes bicondylar involvement. In type VI fractures, there is complete metadiaphyseal dissociation. In younger patients with more robust bone stock, tibial plateau fractures are generally the result of high energy mechanisms, whereas low energy mechanisms are usually observed in the elderly, osteoporotic population. Due to the mechanical axis of the lower extremity, with the lateral plateau higher and in 3 degrees of varus, the medial tibial plateau receives 60% of the load placed on the knee, creating stronger subchondral bone. As a result, lower energy injuries more commonly injure the lateral plateau. Therefore, medial injuries are not simply the counterpart to lateral injuries, but rather represent a much higher energy impact, and therefore associated injuries (i.e., ACL and MCL) are more common with this pattern[1]. Approach to the patient should commence with evaluation of the soft-tissue envelope and neurovascular exam. In Schatzker IV-VI fractures, clinicians should be especially sensitive to the possibility of vascular injuries and compartment syndrome[1]. Computed tomography imaging in addition to standard radiographs are important in both fracture classification and operative planning.
Options for the management of these fractures range from conservative methods including bracing and limited weight bearing to surgical management, most commonly open reduction and internal fixation. The decision to pursue surgery is based upon the characteristics of the fracture. Regardless of patient age and bone quality, fractures with significant displacement or fragment depression require surgical management for a successful outcome. Instability and fracture displacement usually require an operative approach to restore joint surface congruity. A major factor when considering surgical management in the acute period following the injury is concomitant damage to the soft tissue structures surrounding the knee. If there is significant soft tissue damage or swelling precluding acute open reduction and internal fixation (ORIF), external fixation using a spanning frame with delayed surgical management of 2-3 wk is usually pursued. Goals of articular fracture management include restoration of the articular surface, normalization of the mechanical axis, stable fixation, early range of motion and delayed weight bearing in most cases. Lansinger et al[2] determined that long-term outcomes correlate better with restoration of joint axis in the sagittal and coronal planes than exact articular reduction. Achieving these goals gives patients the best chance of restoring their pre-injury level of function and avoiding the complications associated with these types of injuries[1,3].
Complications of tibial plateau fractures may require arthroplasty as a salvage procedure. Complications of operative management of tibial plateau fractures include infection, knee stiffness, non-union, fixation failure, and most relevant to this discussion, post-traumatic osteoarthritis (PTOA). Infections may be a frequent complication of ORIF of tibial plateau fractures with rates ranging from 2%-11%[4]. With optimal handling of the soft tissue envelope and appropriate decision-making by the surgeon, rates of infectious complication can be kept to a minimum. Infection should be avoided at all costs because patients who suffer infection following ORIF incur on average an additional five surgeries[5]. Factors associated with infection after tibial plateau fracture include smoking, compartment syndrome requiring fasciotomy and fractures requiring dual incisions with dual plating[6]. Knee stiffness is thought to be the result of post-operative immobilization. Patients with higher-energy fracture patterns are noted to be more likely to experience unsatisfactory knee motion following ORIF of the tibial plateau. This is also the case in patients with longer periods of immobilization. Three to four weeks of immobilization vs immediate ROM is associated with higher rates of stiffness and flexion contracture[4]. Fixation failure can be loosely defined as loss of reduction resulting in either step off of > 3 mm or malalignment of the extremity of greater than 5 degrees, loosening or breaking of implants. The rates of fixation failure range from between 1%-31%[7].
PTOA is caused mainly by articular incongruity and joint instability, although direct damage to the articular surface at the time of injury may play a role. PTOA is seen in 23%-44% of patients following tibial plateau fracture, even in those with stable knees. In one study, the rate of secondary OA was seen in 44% of patients who suffered PTOA and were followed up at an average of 7.6 years. An important point was that after 7 years, the rate of OA development did not increase significantly[8,9]. Weigel et al[10]’s 20-year follow-up of patients with high energy tibial plateau fractures found that after 2-4 years of follow-up, there was not a significant change in the rate or grade of arthrosis. There is a higher rate of PTOA in patients who undergo meniscectomy during fracture repair, and therefore preservation of menisci should be a priority during surgical management of these patients. Ligamentous injury also correlates with the development of secondary arthritis, as does residual tilt of the tibial plateau. Seventy-five percent of patients with ligamentous injury at the time of surgery developed secondary osteoarthritis vs 27% of those with no evidence of ligamentous injury or instability at the time of repair[8]. Not surprisingly, age is also a predictor of development of PTOA, with older patients being more likely to suffer secondary OA following trauma. Risk of degenerative change increases significantly with greater age at time of injury[4,9,10]. It should be noted that there does not seem to be a difference in the rate of PTOA between those managed operatively vs non-operatively[8].
For patients who develop post-traumatic arthrosis of the knee, total knee arthroplasty (TKA) is a widely accepted treatment option, just as prosthetic replacement is considered for patients who develop primary osteoarthritis of the knee. In fact, the risk of TKA in patients with previous fracture of the tibial plateau is 5-times higher than matched controls from the general population, at 7.3% in the 10-year period following injury[11]. Age of the patient, activity level and the status of bone mineralization are some of the major factors that are involved in treatment of PTOA. Non arthroplasty options for physiologically younger patients generally include osteotomy and arthrodesis, however in most patients, especially older patients, TKA should be considered the optimal treatment for end stage PTOA[12].
In contrast to TKA for salvage in patients who suffered complications of tibial plateau fractures, TKA is potentially a primary treatment option for elderly patients with lower demands along with fracture patterns and bone quality that make ORIF a less desirable option. Elderly, osteopenic patients present several unique issues in the management of tibial plateau fractures. Fractures in this patient population are generally lower-energy injuries than seen in younger patients. Due to poor bone quality, fracture patterns are often complex with significant displacement and damage to the articular surface. As such, there is an association between patient age and failure of fracture fixation. Patients older than 60 have an increased risk of fixation failure and radiographic evidence of osteoporosis is a major predictor of failed fixation. One study reported a 79% rate of radiographic fixation failure in elderly patients vs 7% in the younger group of patients[7]. Second, fracture fixation in elderly patients will often times prevent early weight-bearing following surgical intervention. Delayed weight bearing in elderly patients is associated with higher morbidity and mortality than in younger populations. The earlier you can get an elderly patient mobile following surgery, the better the outcome and more likely the return to preoperative functional status, which should be the ultimate goal in management of these injuries. Therefore, investigators selecting patients to undergo TKA acutely following tibial plateau fracture used evidence of osteopenia or osteoarthritis as indications for TKA. This allows the identification of patients who are at risk for either failed fixation or later requirement of TKA. Some groups specified an age range, for instance, Vermeire et al[13] limited participants to over 70 years of age with evidence of poor bone stock or over 55 with severe, debilitating pre injury osteoarthritis.
Finally, as some studies have indicated, delayed TKA presents a greater challenge both in the operating room and during recovery than primary TKA, and complications can often be more dramatic in elderly patients. Considering these ideas, several papers are presented here that have examined groups of patients with tibial plateau fractures treated primarily with TKA and examined the outcomes and complications experienced by these patients.
APPROACH TO TKA IN TIBIAL PLATEAU FRACTURES
Total knee arthroplasty for PTOA
Arthroplasty in patients with prior fixation about the knee can present major challenges. It is more technically demanding and is associated with higher rates of complication than arthroplasties performed in patients with primary OA[14]. When planning TKA for patients with prior fixation of tibial plateau fracture, surgeons must consider several factors. First of all, patients should undergo a standard and thorough preoperative evaluation. This includes a medical evaluation, full length alignment radiographs along with an infectious and nutrition workup. Next the surgeon should take into consideration the previous repair and hardware present in the knee. Prior hardware may be removed intraoperatively or the removal can be staged it if will require extensive incisions or dissection, which can predispose to infection if performed simultaneously with TKA[15]. Additionally, not all hardware requires removal. Some authors suggest removing only the hardware that is going to directly interfere with the prosthesis[12].
In addition to challenges posed by the fracture, alterations to the soft tissue environment imposed by previous surgeries can complicate wound healing. Prior incisions should be approached carefully by using the most lateral incision and taking care not to create acute angles across prior transverse incisions. Careful attention should be taken to preserve the medial skin flap, as this is where the perforators arise. Other issues that can be encountered in this population is surgically constructed flaps and grafts which have a tenuous blood supply of their own. Surgeons should have a low threshold for consulting a plastic surgeon for management of the soft tissues in patients with prior soft tissue reconstruction. Careful consideration in this regard is necessary to preventing skin necrosis and wound healing complications.
Exposure of the knee can be difficult, as PTOA patients often have stiff knees. Certain maneuvers can be employed in different scenarios to provide excellent exposure as well as to manage injury to extensor mechanism and collateral ligaments. These include quadriceps, snip, VY turndown, tibial tubercle osteotomy and lateral retinacular release. Weiss et al[16] performed lateral release in 28% of their patients to facilitate their approach while Saleh et al[17] performed the same maneuver in 33% of their patients. Civinini et al[18] performed quadriceps snip and tibial tubercle osteotomy to facilitate exposure in 12% and 16% of their patients, respectively. It must be pointed out that these maneuvers are not without morbidity. Lateral release is generally benign and doesn’t require any additional post-operative rehabilitation. Tubercle osteotomy can be more problematic, and mechanical complications relation to the procedure include disruption of the extensor mechanism or resultant fracture, with rates around 15%[19]. Quadriceps snip and VY turndown are soft tissue techniques that evolved as an alternative to tibial tubercle osteotomy, however they also pose a minor threat to the extensor function[20]. One study identified factors in their patient population that predicted patellar tendon rupture and these includes diabetes mellitus, steroids, trauma and patella baja[17]. Managing bony loss in these patients involves techniques similar to those for revision TKA including cement filling, morselized bone grafting and metal wedge augmentation, among others[12] (Figure 1).
Figure 1.
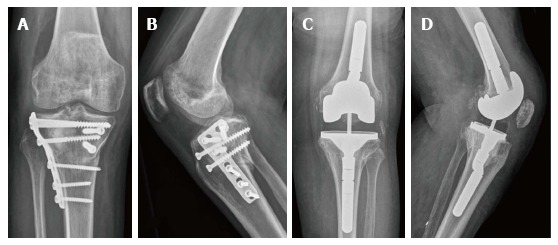
Total knee arthroplasty following open reduction and internal fixation of the tibial plateau. A and B: Radiographs of a 61-year-old woman made 3 years after ORIF for tibial plateau fracture; C and D: Radiographs at 7-year follow-up after constrained PS prosthesis with offset and stem in both components. ORIF: Open reduction and internal fixation.
Device selection should take into account ligament integrity and bone quality. A general rule is to use the least amount of prosthesis constraint necessary while allowing symmetric and balanced flexion and extension of the knee[12]. The high rate of constrained implant use in these patients makes this procedure more similar to revision TKA than primary standard TKA. The choice of implant should take into account the stability of the knee and existing bony defects. The most common implants types were varus/valgus constrained, hinged and PCL-retaining prostheses. Most but not all groups performed patellar resurfacing and required long-stems in certain patients to bypass fracture areas.
There is a well-known benefit to using computer assistance (CAS) in total knee arthroplasty. Kini et al[21] examined the use of CAS in acute TKA for a group of elderly patients with proximal tibial fractures, 6 of which were Schatzker type II. Mean time to walking was 2 d and all patients returned to preoperative functional status. There were no major complications or revisions. Successful TKA relies on restoration of mechanical axis, which is improved with CAS. All patients in this sample had mechanical axis restored to within 3 degrees, which prevents off-axis loading and can lead to greater implant survivability. This study, while small, suggests that navigation systems for TKA can play a role in delivering acceptable outcomes to patients undergoing primary TKA for tibial plateau fracture. While CAS is an option for TKA in tibial plateau fractures, it is certainly not the standard of care[21].
TKA AS PRIMARY TREATMENT
Most authors evaluating this approach comment on the technical aspects of arthroplasty as the primary treatment for tibial plateau fracture. Preoperative planning as always is the first major step in ensuring an optimal outcome. Implant type and level of constraint should be determined based on pre-operative radiographs, assessing whether or not the fracture line likely compromises the medial or lateral collateral ligaments. In this case, a rotating hinge prosthesis should be selected. In terms of timing of surgery, all authors discussed the immediate post-injury period as ideal for surgery, as the primary goal of arthroplasty was early mobilization to prevent the sequelae of prolonged non-weightbearing. One study reported a mean surgical delay of 7.5 d, while another reported 4 d of mean surgical delay[22]. While it makes sense to allow a modest period of time for soft-tissue healing to prevent infection, we recommend allowing no more than three weeks before definitive repair. In most cases, unless prevented by the fracture site, medial parapatellar approach to the joint was used. Some authors utilized tibial tubercle osteotomies in all patients as a protocol[13], while other authors managed to avoid it entirely. For the bony cuts, the distal femoral cut should be 2.5 cm distal to the epicondyles and the tibial cut should allow joint line positioning 1 cm above the fibular head[19]. In terms of selecting prostheses, the choice between a hinged system and posterior-stabilized is made based on the integrity of the ligaments. In the studies evaluated, constrained, PS, rotating hinge and super stabilized prostheses were all used. If the fracture line is compromising the stability of the medial or lateral collateral ligaments, a rotating hinge prosthesis is best option[22]. Vermeire et al[13] has noted equally satisfactory results in using PS modular prostheses and cemented rotating hinge implants. This group also used stemmed cemented components, which allowed early weight bearing in these elderly patients. In series published on this topic, more attention should be paid in the future to discussing the reasoning behind implant selection. As most studies were retrospective in nature, surgeon preference was often cited as the reasoning behind surgical decisions. Patellar resurfacing was variable between studies, with some groups performing this step systemically in all patients, others in select patients, and other groups not at all. In terms of managing bony loss, usually in osteoporotic or comminuted fractures most authors made use of wedges, augments and bone grafts to deal with osseous defects in these patients. One paper expanded on this and recommended wedges or cone shaped metallic augments or the patient’s own bone for fixing defects[22]. Fracture reduction and joint alignment to determine pre-injury joint congruity and rotation, making use of diaphyseal landmarks is one approach used by Boureau et al[23]. If this cannot be performed accurately, surgeons should elect to approach the case as a revision TKA with major bone loss[22]. Simultaneous bony stabilization was used by all authors in this review (Figure 2).
Figure 2.
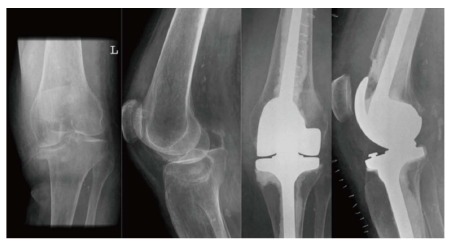
Primary total knee arthroplasty following tibial plateau fracture. Proximal tibial fracture with poor bone stock and post-operative radiograph showing rotating hinge prosthesis.
RESEARCH RESULTS
TKA for ptoa following tibial plateau fracture
A number of studies exist in the literature that identified patients who underwent TKA following tibial plateau fractures that were managed operatively and nonoperatively Most of these series have looked at outcomes in terms of function and pain scores, patient satisfaction as well as stability, survivability of prosthesis, and incidence of common complications of TKA, such as infection, component loosening or periprosthetic fracture. Weiss et al[16] found improvements in KSS for pain and function in a group of 62 patients, with excellent or good results in 48 of those patients. Optimal component positioning had a positive impact on outcome. Civinini et al[18] had a good result in 18 of 25 patients undergoing TKA for this indication. Alternatively, poor outcome was related to complications in this group of patients. Range of motion and stability was significantly improved in this group. Saleh et al[17] reported HSS knee scores that improved from 51 pre-operatively to 80 post-operatively. Twelve/fifteen outcomes were considered good or excellent in their paper. Scott et al[14] matched the patients undergoing TKA for prior tibial plateau fracture with controls undergoing TKA for primary OA. Absolute OKS scores did not differ significantly between the two groups at five years. This is in sharp contrast to other studies of this nature which highlight poorer knee outcomes based on KSS and HSS knee scores. The authors here suggest that OKS is a more-patient centered scale that is based on the experience of the patient, while the HSS and KSS scales may be reporting more physician-centered data that might ignore the fact that patients are actually satisfied with their implants despite clinically discouraging measures such as range of motion, contracture and instability[14]. Lizaur-Utrilla et al[15] performed a similar comparison. The authors of this study challenged the notion that the outcomes between TKA for PTOA and routine TKA are significantly different. This study had a homogenous surgical and postoperative protocol not seen in most of its contemporaries. Functional outcomes including WOMAC pain score, KSS knee and function scores, ROM, SF12 physical and mental scores did not differ significantly between the two groups. The authors posited that a protocolized surgical scheme, which involved separate removal of hardware and standardized exposure strategy, can improve outcomes for patients undergoing TKA for PTOA secondary to tibial plateau fracture[15]. Abdel et al[24] followed 46 patients over 15 years and found that KSS and ROM both improved significantly from pre-operative values.
TKA as primary treatment
More recently in the literature is a group of studies analyzing the success of TKA as a primary treatment of tibial plateau fractures in elderly patients. Considering that TKA for PTOA is a more established concept than primary TKA for tibial plateau fracture, the series presented in this section are also smaller. The first small series performed primary TKA on four elderly patients with tibial plateau fractures. Excellent results were obtained in three cases and a fair result in one. No reoperations were required, and radiographic follow up showed optimal alignment with no evidence of loosening[25]. Vermeire et al[13] selected 12 patients who underwent primary TKA within 3 wk of tibial plateau fracture. Seven patients had outcomes rated as excellent and median final knee score was 78 and function score was 58. The authors concluded that primary TKA for tibial plateau fracture is an acceptable alternative to fracture fixation in patients with difficult fractures or poor bone quality who would likely end up requiring a TKA[22]. Malviya et al[26] studied a group of elderly patients who underwent primary TKA for either tibial plateau or distal femoral fractures. Eighty-one percent of elderly patients with fractures about the knee returned to preoperative functional status. Patient satisfaction was similarly excellent although KSS were not overall excellent (90.2 knee and 35.5 for function). The authors remind us to consider that this patient population likely did not have excellent knee function to begin with[26]. Haufe et al[27] limited their series to only patients with fractures of the tibial plateau. They found improved mean knee scores for patients undergoing the procedure. Their paper contended that in the elderly population, tibial plateau fractures represent a great technical challenge in primary repair and primary TKA can avoid this challenge while presenting the patient an opportunity for full weight-bearing in the early postoperative period, which is likely to reduce some of the morbidity associated with delayed weight-bearing following ORIF. An interesting finding in this paper was that the subgroup of patients treated in the later part of the series (2013-2014) showed better functional results than the overall group, potentially indicating that we can expect improved results for this procedure as experience and technology progress[27]. Another group examining the outcomes of TKA as primary treatment of periarticular fractures about the knee in elderly patients did not find evidence to support the idea that primary TKA in these patients preserves patient autonomy as widely suggested. Patient autonomy was measured using the Parker Score of mobility, and found a significant decline following surgery (7.2 pre op to 4.6 post op). Moreover, autonomy decline was evidenced by only 7/15 patients returning to pre-operative level of independence and only 11/15 patients returning home following surgery. While this group did stratify proximal tibial from distal femoral fractures, the knee scores did not differ significantly between the groups, allowing us to generalize these results to our specific discussion of tibial plateau fractures[23]. Parratte et al[22] highlighted 16 cases of tibial plateau fractures treated primarily with TKA in a multicenter retrospective trial in France from 1990-2010. While functional results of the knee were considered good, there was a significant loss of autonomy in this group of patients, as seen in other studies of its nature[22].
COMPLICATIONS
TKA for PTOA
Despite an acceptable functional outcome, Weiss et al[16] showed a great deal of complications. Twenty-six percent of patients encountered post-operative complications, most commonly stiffness and wound breakdown. Of note, there were 5 intraoperative patellar tendon ruptures in this sample, all of which were repaired successfully during surgery. For Civinini et al[18] 8 of 25 knees encountered complication, including patellar tendon rupture and two implant failures. Saleh et al[17] also reported a high rate of postoperative complications, 11/15 patients experienced some sort of complication. There were two early patellar tendon ruptures and three patients requiring treatment for early wound complications with prolonged drainage and oral antibiotics. For the controlled trial conducted by Scott et al[14], rates of intraoperative complication were higher in in the PTOA cohort although the incidence of early and late complications failed to differ significantly. In the trial conducted by Lizaur-Utrilla et al[15], the PTOA group did have significantly more complications than the primary patients, including patellar tendon rupture and wound infection, however they weren’t serious enough to affect the functional outcomes. Shearer et al[28] determined that in patients with soft tissue graft coverage, more common in this population, outcomes were poorer.
In all series reviewed, a number of patients experienced post-operative stiffness, some requiring manipulation under anesthesia. In the papers reviewed, the rates of manipulation under anesthesia for persistent stiffness ranged from 3.44%-20%[14-18]. Several papers reported repeat manipulations. Stiffness is therefore a major complication associated with arthroplasty following previous ORIF of the tibial plateau. Another common complication experienced throughout the literature is intra-operative avulsion of the patellar tendon and/or the MCL, owing to exposure difficulty in knees with significant scar tissue from previous surgery.
Overall, the type of complications encountered were similar and reflected the complex nature in performing TKA in knees with prior injury. Methods to avoid patellar tendon rupture and to preserve the delicate soft tissue are recommended to avoiding some of the common problems encountered by these authors. In Abdel et al[24]’s 15-year follow-up, they found that from the 5 to 15 year follow-up, there were only 2 additional complications (periprosthetic fracture and periprosthetic infection), leading the authors to conclude that if the early complications of TKA can be avoided, long-term survivorship free from aseptic loosening and revision (96% and 82%, respectively) can be achieved in pts undergoing TKA for this indication[24].
Primary TKA
The overall complication rate for primary TKA following tibial plateau fracture is higher than that for primary TKA in the general population but lower than that for TKA following operative repair of the tibial plateau by ORIF[23]. Overall complication rates of the studies included ranged from 9.5%-33%. The most commonly reported complications were infectious and wound complications, stiffness and flexion contracture, as well as periprosthetic fracture. All authors reported at least one case of wound complications, with many patients requiring re-operation for debridement or revision. Parratte et al[22] and Boureau et al[23] both reported problems with knee stiffness with 8% and 19% requiring closed manipulation under anesthesia, respectively. Component loosening was seen radiographically in one patient who required reoperation. Vermeire et al[13] discussed the case of a patient with a periprosthetic fracture which was repaired using plates and screws. Other less common complications, which were not unique to this procedure, included hematoma formation and DVT/PE, reported in several papers. In the 12-patient analysis by Vermeire et al[13], three developed spontaneously resolving hematomas and one developed a lower extremity DVT treated with low-molecular weight heparin.
DISCUSSION
The discussion of TKA in patients with fractures of the tibial plateau is two-fold. First, patients who develop complications of fracture management, most commonly post-traumatic osteoarthritis of the knee, can be managed with arthroplasty. It is most commonly considered in older patients with less demand, as arthroplasty is usually not preferred in younger patients who may require several revisions throughout their lifetime. Our review shows that while good results may be achieved, complication rates are high and the procedure requires thoughtful decision making and careful attention to avoid complications. Avoiding the early complications can result in acceptable function and survivability. The body of literature regarding this topic is well-rounded, and will benefit in future years from longer-term data on patients and evolving technology in total joint replacement. While recognizing that there is no argument to be made for primary TKA replacing ORIF for primary treatment of tibial plateau fractures, there is a certain group of patients for whom a primary TKA may be indicated. It has been demonstrated in this literature review that fixation failure is more common in elderly patients with poor bone stock. In patients with low demand, poor bone stock in whom we can predict a high rate of TKA, primary arthroplasty should be considered as a primary treatment for fractures of the tibial plateau.
With that in mind, the second discussion is that of TKA as primary treatment for tibial plateau fractures, which is usually carried out in these older, osteoporotic patients. Most series on this topic are small in number and carried out in Europe. While theoretically well-understood to avoid complications of delayed weight-bearing and poor outcomes of fracture fixation, the overall body of literature for this indication is lacking. Currently, the literature which has discussed the use of acute TKA for this injury has been limited to series of elderly patients with poor bone quality. Perhaps expanding the indications for primary TKA in tibial plateau fracture to outside of the group with obviously poor bone may prove to be beneficial for a wider group of patients. However, at this time there is no reason to consider expanding in the indications for primary TKA following a fracture to the tibial plateau. At the same time, it should also be recognized that a high percentage of patients who undergo successful ORIF will need prosthetic knee replacement down the road. This is well established and accepted in the world of orthopaedic trauma. Refining the indications and technique for performing a primary TKA after tibial plateau fracture is an important task. Future effort should be placed in identifying patients with high risk of poor outcome (either failed fixation or PTOA) and evaluating TKA as an alternative to fixation in this group. Our paper shows clearly that for the elderly patients selected, primary TKA is a potentially valuable option to address their injury. Slowly expanding the indications with future series will possibly show that younger patients with healthier bone can benefit as well. For now, ORIF remains the standard of care for these patients. Large cohort, multi-center data, as well as head-to head comparison of the two methods is going to be required to determine the true benefit of primary TKA for patients with fractures of the tibial plateau.
Footnotes
Conflict-of-interest statement: No potential conflicts of interest. No financial support.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Peer-review started: September 10, 2016
First decision: October 20, 2016
Article in press: January 4, 2017
P- Reviewer: Anand A, Guerado E, Vulcano E S- Editor: Gong XM L- Editor: A E- Editor: Lu YJ
References
- 1.Berkson EM, Virkus WW. High-energy tibial plateau fractures. J Am Acad Orthop Surg. 2006;14:20–31. doi: 10.5435/00124635-200601000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Lansinger O, Bergman B, Körner L, Andersson GB. Tibial condylar fractures. A twenty-year follow-up. J Bone Joint Surg Am. 1986;68:13–19. [PubMed] [Google Scholar]
- 3.Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience 1968--1975. Clin Orthop Relat Res. 1979;(138):94–104. [PubMed] [Google Scholar]
- 4.Papagelopoulos PJ, Partsinevelos AA, Themistocleous GS, Mavrogenis AF, Korres DS, Soucacos PN. Complications after tibia plateau fracture surgery. Injury. 2006;37:475–484. doi: 10.1016/j.injury.2005.06.035. [DOI] [PubMed] [Google Scholar]
- 5.Young MJ, Barrack RL. Complications of internal fixation of tibial plateau fractures. Orthop Rev. 1994;23:149–154. [PubMed] [Google Scholar]
- 6.Morris BJ, Unger RZ, Archer KR, Mathis SL, Perdue AM, Obremskey WT. Risk factors of infection after ORIF of bicondylar tibial plateau fractures. J Orthop Trauma. 2013;27:e196–e200. doi: 10.1097/BOT.0b013e318284704e. [DOI] [PubMed] [Google Scholar]
- 7.Ali AM, El-Shafie M, Willett KM. Failure of fixation of tibial plateau fractures. J Orthop Trauma. 2002;16:323–329. doi: 10.1097/00005131-200205000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Honkonen SE. Degenerative arthritis after tibial plateau fractures. J Orthop Trauma. 1995;9:273–277. doi: 10.1097/00005131-199509040-00001. [DOI] [PubMed] [Google Scholar]
- 9.Volpin G, Dowd GS, Stein H, Bentley G. Degenerative arthritis after intra-articular fractures of the knee. Long-term results. J Bone Joint Surg Br. 1990;72:634–638. doi: 10.1302/0301-620X.72B4.2380219. [DOI] [PubMed] [Google Scholar]
- 10.Weigel DP, Marsh JL. High-energy fractures of the tibial plateau. Knee function after longer follow-up. J Bone Joint Surg Am. 2002;84-A:1541–1551. doi: 10.2106/00004623-200209000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Wasserstein D, Henry P, Paterson JM, Kreder HJ, Jenkinson R. Risk of total knee arthroplasty after operatively treated tibial plateau fracture: a matched-population-based cohort study. J Bone Joint Surg Am. 2014;96:144–150. doi: 10.2106/JBJS.L.01691. [DOI] [PubMed] [Google Scholar]
- 12.Bedi A, Haidukewych GJ. Management of the posttraumatic arthritic knee. J Am Acad Orthop Surg. 2009;17:88–101. doi: 10.5435/00124635-200902000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Vermeire J, Scheerlinck T. Early primary total knee replacement for complex proximal tibia fractures in elderly and osteoarthritic patients. Acta Orthop Belg. 2010;76:785–793. [PubMed] [Google Scholar]
- 14.Scott CE, Davidson E, MacDonald DJ, White TO, Keating JF. Total knee arthroplasty following tibial plateau fracture: a matched cohort study. Bone Joint J. 2015;97-B:532–538. doi: 10.1302/0301-620X.97B4.34789. [DOI] [PubMed] [Google Scholar]
- 15.Lizaur-Utrilla A, Collados-Maestre I, Miralles-Muñoz FA, Lopez-Prats FA. Total Knee Arthroplasty for Osteoarthritis Secondary to Fracture of the Tibial Plateau. A Prospective Matched Cohort Study. J Arthroplasty. 2015;30:1328–1332. doi: 10.1016/j.arth.2015.02.032. [DOI] [PubMed] [Google Scholar]
- 16.Weiss NG, Parvizi J, Trousdale RT, Bryce RD, Lewallen DG. Total knee arthroplasty in patients with a prior fracture of the tibial plateau. J Bone Joint Surg Am. 2003;85-A:218–221. doi: 10.2106/00004623-200302000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Saleh KJ, Sherman P, Katkin P, Windsor R, Haas S, Laskin R, Sculco T. Total knee arthroplasty after open reduction and internal fixation of fractures of the tibial plateau: a minimum five-year follow-up study. J Bone Joint Surg Am. 2001;83-A:1144–1148. doi: 10.2106/00004623-200108000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Civinini R, Carulli C, Matassi F, Villano M, Innocenti M. Total knee arthroplasty after complex tibial plateau fractures. Chir Organi Mov. 2009;93:143–147. doi: 10.1007/s12306-009-0033-3. [DOI] [PubMed] [Google Scholar]
- 19.Wolff AM, Hungerford DS, Krackow KA, Jacobs MA. Osteotomy of the tibial tubercle during total knee replacement. A report of twenty-six cases. J Bone Joint Surg Am. 1989;71:848–852. [PubMed] [Google Scholar]
- 20.Garvin KL, Scuderi G, Insall JN. Evolution of the quadriceps snip. Clin Orthop Relat Res. 1995;(321):131–137. [PubMed] [Google Scholar]
- 21.Kini SG, Sathappan SS. Role of navigated total knee arthroplasty for acute tibial fractures in the elderly. Arch Orthop Trauma Surg. 2013;133:1149–1154. doi: 10.1007/s00402-013-1792-8. [DOI] [PubMed] [Google Scholar]
- 22.Parratte S, Bonnevialle P, Pietu G, Saragaglia D, Cherrier B, Lafosse JM. Primary total knee arthroplasty in the management of epiphyseal fracture around the knee. Orthop Traumatol Surg Res. 2011;97:S87–S94. doi: 10.1016/j.otsr.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 23.Boureau F, Benad K, Putman S, Dereudre G, Kern G, Chantelot C. Does primary total knee arthroplasty for acute knee joint fracture maintain autonomy in the elderly? A retrospective study of 21 cases. Orthop Traumatol Surg Res. 2015;101:947–951. doi: 10.1016/j.otsr.2015.09.021. [DOI] [PubMed] [Google Scholar]
- 24.Abdel MP, von Roth P, Cross WW, Berry DJ, Trousdale RT, Lewallen DG. Total Knee Arthroplasty in Patients With a Prior Tibial Plateau Fracture: A Long-Term Report at 15 Years. J Arthroplasty. 2015;30:2170–2172. doi: 10.1016/j.arth.2015.06.032. [DOI] [PubMed] [Google Scholar]
- 25.Nourissat G, Hoffman E, Hémon C, Rillardon L, Guigui P, Sautet A. [Total knee arthroplasty for recent severe fracture of the proximal tibial epiphysis in the elderly subject] Rev Chir Orthop Reparatrice Appar Mot. 2006;92:242–247. doi: 10.1016/s0035-1040(06)75731-2. [DOI] [PubMed] [Google Scholar]
- 26.Malviya A, Reed MR, Partington PF. Acute primary total knee arthroplasty for peri-articular knee fractures in patients over 65 years of age. Injury. 2011;42:1368–1371. doi: 10.1016/j.injury.2011.06.198. [DOI] [PubMed] [Google Scholar]
- 27.Haufe T, Förch S, Müller P, Plath J, Mayr E. The Role of a Primary Arthroplasty in the Treatment of Proximal Tibia Fractures in Orthogeriatric Patients. Biomed Res Int. 2016;2016:6047876. doi: 10.1155/2016/6047876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shearer DW, Chow V, Bozic KJ, Liu J, Ries MD. The predictors of outcome in total knee arthroplasty for post-traumatic arthritis. Knee. 2013;20:432–436. doi: 10.1016/j.knee.2012.12.010. [DOI] [PubMed] [Google Scholar]


