Abstract
AIM
To determine whether cemented, cementless, or hybrid implant was superior to the other in terms of survival rate.
METHODS
Systematic searches across MEDLINE, CINAHL, and Cochrane that compared cemented, cementless and hybrid total hip replacement (THR) were performed. Two independent reviewers evaluated the risk ratios of revision due to any cause, aseptic loosening, infection, and dislocation rate of each implants with a pre-determined form. The risk ratios were pooled separately for clinical trials, cohorts and registers before pooled altogether using fixed-effect model. Meta-regressions were performed to identify the source of heterogeneity. Funnel plots were analyzed.
RESULTS
Twenty-seven studies comprising 5 clinical trials, 9 cohorts, and 13 registers fulfilled the research criteria and analyzed. Compared to cementless THR, cemented THR have pooled RR of 0.47 (95%CI: 0.45-0.48), 0.9 (0.84-0.95), 1.29 (1.06-1.57) and 0.69 (0.6-0.79) for revision due to any reason, revision due to aseptic loosening, revision due to infection, and dislocation respectively. Compared to hybrid THR, the pooled RRs of cemented THR were 0.82 (0.76-0.89), 2.65 (1.14-6.17), 0.98 (0.7-1.38), and 0.67 (0.57-0.79) respectively. Compared to hybrid THR, cementless THR had RRs of 0.7 (0.65-0.75), 0.85 (0.49-1.5), 1.47 (0.93-2.34) and 1.13 (0.98-1.3).
CONCLUSION
Despite the limitations in this study, there was some tendency that cemented fixation was still superior than other types of fixation in terms of implant survival.
Keywords: Total hip replacement, Implant survival, Cemented, Cementless, Hybrid, Meta-analysis
Core tip: To determine whether cemented, cementless, or hybrid implant was superior to the other in terms of survival rate, a meta-analysis of 27 studies, comprising 5 clinical trials, 9 cohorts, and 13 registers, were performed to evaluate the risk ratios of revision due to any cause, aseptic loosening, infection, and dislocation rate. The risk ratios were pooled separately for clinical trials, cohorts and registers before pooled altogether using fixed-effect model. Meta-regressions were performed to identify the source of heterogeneity. Despite the limitations in this study, there was some tendency that cemented fixation was still superior than other types of fixation in terms of implant survival.
INTRODUCTION
Rationale
Currently, total hip replacement is one of the most performed orthopaedic surgeries. In Sweden, the number of THR performed increased by 20% from 1986-1997 and up to 68% in Netherland during the same period of observation[1]. In Organisation for Economic Cooperation and Development countries, the rate of THR increase from 50-130/100000 inhabitants to 60-200/100000 inhabitants in the late 1990s[2]. In United States, more than 200000 THR are conducted annually[3].
Superiority of either cemented or cementless implants has been a longstanding debate. Wroblewski et al[4] in 1993 reported the superiority of either implants could not be determined on a scientific basis. Rorabeck et al[5,6] reported similar clinical outcome by any of those implants. Zimmerman et al[7] agreed that no significant differences in clinical and functional outcome between the implants and reported non-cemented prosthesis to be more costly. Emerson et al[8] found cementless titanium stems offered better resistance to osteolysis and mechanical failure.
Morshed et al[9] conducted a meta-analysis in 2007 and found no difference in survival between those two groups. Since then, many larger studies with longer duration of follow-up had been conducted and resulted in different results thus resuming the controversy.
Objective
We conducted a meta-analysis of articles published after January 2000 comparing the cemented, cementless and hybrid THR implants to evaluate the superiority of each in terms of risk of revision due to any reason, revision due to infection, revision due to aseptic loosening, and dislocation.
MATERIALS AND METHODS
The structure of this study was written in accordance with the PRISMA checklist for systematic review and meta-analysis[10].
Selection criteria
All studies including randomized clinical trials and cohorts reporting direct comparison between cementless, hybrid and cemented implant in primary THR were included. Recent reports from national registry were also included in this study. The inclusion criteria was pre-determined: (1) all patients over 18 years of age; (2) primary total hip replacement; and (3) revision due to any reason as the primary endpoint. Studies about inverse hybrid arthroplasty were excluded from the analysis. These studies were restricted according to these characteristics: (1) published after January 2000; (2) English language; (3) available abstract; and (4) original research.
Information source and search strategy
In June 2012, literature search was conducted across MEDLINE, CINAHL, and The Cochrane Library using strategies listed in appendices 1. Manual search was also conducted to identify studies that were not included by the initial MeSH keyword search. All identified articles were retrieved from previously mentioned databases.
Study selection
Two reviewers independently performed the study selection in accordance with the aforementioned selection criteria by screening the titles and abstracts. Studies were excluded if they don’t meet the selection criteria. If the information required determining eligibility was not found in the abstract, a full-text search was run after data extraction. The studies included were determined from the discussion of two reviewers in accordance with the selection criteria. Reviewers were not blinded to any study characteristic such as journal, author or institution. Algorithm in selecting studies included in this meta-analysis is shown in Figure 1.
Figure 1.
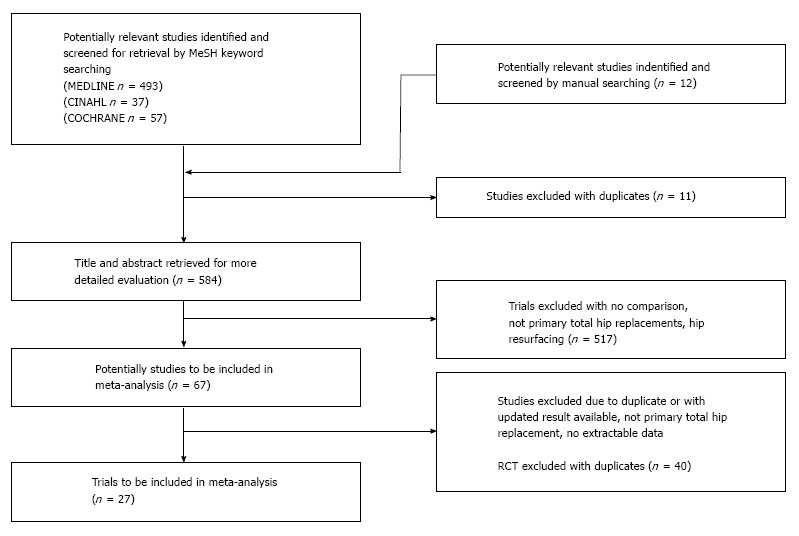
Study selection algorithm.
Data collection process and data items
All results were checked for consistency between the two reviewers independently. Any discrepancies were be judged by a third independent reviewer. Data extraction was performed using a predetermined standardized form as shown in Tables 1 and 2. Study quality was first assessed using sample size, study design, duration of follow up and variability of result. Overall level of evidence was also assessed.
Table 1.
Characteristics of the included studies
| Ref. | Age (years old) | Length of follow-up (years) | Diagnosis | Cementing technique (generation) | Comparison | Approach | Comments | |
| Bjørgul et al[11] | 65 to 66 | 14 | Osteoarthritis (most) | 3rd | Cemented (n = 120) | Hybrid (n = 120) | direct lateral | |
| Chandran et al[12] | 64.5 to 65.5 | 14 | primary Osteoarthritis | 2nd | Cemented (n = 97) | Cementless (n = 105) | anterolateral | |
| Corten et al[13] | 64 (mean) | 19.5 | primary Osteoarthritis | 2nd | Cemented (n = 124) | Cementless (n = 126) | direct lateral | |
| Kim et al[14] | 43.4 to 46.8 | 18.4 | Avascular necrosis (most) | 3rd | Hybrid (n = 109) | Cementless (n = 110) | ND | May overlap with Kim et al[15] |
| McCombe et al[16] | 67.3 | 6.5 to 8 | Primary OA (most) | 2nd | Cemented (n = 84) | Hybric (n = 78) | posterolateral | |
| Berend et al[17] | 67.1 | 6.8 | Osteoarthritis (most) | ND | Cemented (n = 1908) | Cementless (n = 623) | anterolateral and posterior | |
| Clohisy et al[18] | 61 to 62 | 10 to 11 | Osteoarthritis | 2nd | Cemented (n = 45) | Hybrid (n = 45) | posterolateral | |
| Emerson et al[8] | 55 to 70 | 6.7 to 7.2 | Osteoarthritis (most) | 3rd | Hybrid (n = 113) | Cementless (n = 88) | anterolateral | |
| Hartofilakidis et al[19] | 39.6 to 45.4 | 12.4 to 15.4 | Osteoarthrosis secondary to congenital hip disease (most) | 2nd | Cemented (n = 59) | Hybric (n = 58) | lateral transtrochanteric | |
| Kim et al[15] | 64.6 | 17.3 | Avascular necrosis | 3rd | Hybrid (n = 50) | Cementless (n = 98) | ND | May overlap with et al[14] |
| Pospula et al[20] | 46.7 to 53.7 | 3 to 5 | Avascular necrosis (most) | ND | Cemented (n = 87) | Cementless (n = 95) | cemented posterolateral cementless transgluteal | |
| Van Stralen et al[21] | 69.5 | 2.5 | Primary OA (most) | Cemented (n = 746) | Cementless (n = 138) | posterior | ||
| Thomason et al[22] | 54 | 7.4 | Rheumatoid arthritis | ND | Hybrid (n = 47) | Cementless (n = 51) | posterior | |
| Zimmerman et al[7] | 74.9 | 1 | Osteoarthritis | ND | Hybrid (n = 85) | Cementless (n = 174) | anterolateral, posterior | |
| Conroy et al[23] | Any | 5 | Osteoarthritis | ND | Cemented (n = 8945); hybrid (n = 20445); | ND | ||
| Cementless (n = 28582) | ||||||||
| Dale et al[24] | Any | 0 to 20 | Osteoarthritis (most) | ND | Cemented (n = 82996) | Cementless (n = 14348) | ND | May overlap with study of et al[16] |
| Engesaeter et al[25] | Any | 0 to 16 | Primary Osteoarthritis | ND | Cemented (n = 51016) | Cementless (n = 5259) | ND | May overlap with et al[15] |
| Eskelinen et al[26] | < 55 | 0 to 24 | Rheumatoid arthritis | ND | Cemented (n = 821) | Cementless (n = 724) | ND | |
| Hailer et al[27] | Any | 15 | Osteoarthritis (most) | ND | Cemented (n = 161460) | Cementless (n = 8593) | ND | |
| Hooper et al[28] | Any | 7 | ND | ND | Cemented (n = 16005); hybrid (n = 15189) | ND | ||
| Cementless (n = 10898) | ||||||||
| Lucht et al[29] | Any | 4 | ND | Cemented (n = 11671); hybric (n = 4491) | ND | |||
| Cementless (n = 2030) | ||||||||
| Mäkelä et al[30] | > 55 | 15 | Osteoarthritis | ND | Cemented (n = 9549) | Cementless (n = 10310) | ND | |
| Mäkelä et al[31] | 63 to 69 (> 55) | 15 | Rheumatoid arthritis | ND | Cemented (n = 3440) | Cementless (n = 579) | ND | |
| Mäkelä et al[32] | < 55 | 15 | Osteoarthritis | ND | Cemented (n = 2342) | Cementless (n = 1326) | ND | |
| Malchau et al[33] | All | 8 | Osteoarthritis (most) | ND | Cemented (n = 178762) | Cementless (n = 6102) | ND | |
| Pedersen et al[34] | Any | 0 to 14 | Osteoarthritis (most) | ND | Cemented (n = 34656); cementless (n = 25571) | ND | ||
| Hybrid (n = 20539) | ||||||||
| Roberts et al[35] | All | ND | ND | ND | Cemented (n = 92928) | Cementless (n = 69882) | ND | |
Table 2.
Summary of finding comparing cemented and cementless total hip replacement
|
Illustrative comparative risks7 (95%CI) |
Relative effect | No of participants | Quality of the evidence | Comments | ||
| Assumed risk | Corresponding risk | (95%CI) | (studies) | (GRADE) | ||
| Cementless | Cemented | |||||
| Revision of any component due to any reason - RCT Follow-up: 14 to 19.5 yr | Study population | RR 1.43 (1 to 2.04) | 452 (2 studies) | ++-- low1,2 | ||
| 165 per 1000 | 235 per 1000 (165 to 336) | |||||
| Moderate | ||||||
| 156 per 1000 | 223 per 1000 (156 to 318) | |||||
| Revision of any component due to any reason - Register or Cohort of register Follow-up: 0 to 24 yr | Study population | RR 0.46 (0.45 to 0.47) | 518774 (10 studies) | +--- very low2,3,4 | ||
| 99 per 1000 | 46 per 1000 (45 to 47) | |||||
| Moderate | ||||||
| 122 per 1000 | 56 per 1000 (55 to 57) | |||||
| Revision of any component due to any reason - All types of study Follow-up: 0 to 24 yr | Study population | RR 0.47 (0.45 to 0.48) | 521757 (13 studies) | +--- very low2,3,5 | ||
| 99 per 1000 | 46 per 1000 (44 to 47) | |||||
| Moderate | ||||||
| 106 per 1000 | 50 per 1000 (48 to 51) | |||||
| Revision of any component due to aseptic loosening - RCT Follow-up: 14 to 19.5 yr | Study population | RR 2 (1.29 to 3.1) | 452 (2 studies) | +++- moderate2 | ||
| 104 per 1000 | 208 per 1000 (134 to 322) | |||||
| Moderate | ||||||
| 97 per 1000 | 194 per 1000 (125 to 301) | |||||
| Revision of any component due to aseptic loosening - Register or Cohort of register Follow-up: 0 to 24 yr | Study population | RR 0.88 (0.83 to 0.94) | 255779 (6 studies) | +--- very low2,3,4 | ||
| 47 per 1000 | 41 per 1000 (39 to 44) | |||||
| Moderate | ||||||
| 48 per 1000 | 42 per 1000 (40 to 45) | |||||
| Revision of any component due to aseptic loosening - All types of study Follow-up: 0 to 24 yr | Study population | RR 0.9 (0.84 to 0.95) | 256231 (8 studies) | +--- very low2,3,5,6 | ||
| 47 per 1000 | 43 per 1000 (40 to 45) | |||||
| Moderate | ||||||
| 48 per 1000 | 43 per 1000 (40 to 46) | |||||
| Revision of any component due to infection - Register or Cohort of register Follow-up: 0 to 20 yr | Study population | RR 1.27 (1.04 to 1.55) | 382433 (6 studies) | +--- very low2,4 | ||
| 5 per 1000 | 6 per 1000 (5 to 7) | |||||
| Moderate | ||||||
| 4 per 1000 | 5 per 1000 (4 to 6) | |||||
| Revision of any component due to infection - All types of study Follow-up: 0 to 20 yr | Study population | RR 1.29 (1.06 to 1.57) | 382683 (7 studies) | +--- very low2,5 | ||
| 5 per 1000 | 6 per 1000 (5 to 7) | |||||
| Moderate | ||||||
| 4 per 1000 | 5 per 1000 (4 to 6) | |||||
| Dislocation of any component - Cohort Follow-up: 2.5 to 5 yr | Study population | RR 0.69 (0.29 to 1.67) | 1066 (2 studies) | +--- very low1,2,3 | ||
| 30 per 1000 | 21 per 1000 (9 to 50) | |||||
| Moderate | ||||||
| 30 per 1000 | 21 per 1000 (9 to 50) | |||||
| Dislocation of any component - Register or Cohort of register Follow-up: 5 to 15 yr | Study population | RR 0.69 (0.59 to 0.8) | 254786 (6 studies) | +--- very low3,4 | ||
| 6 per 1000 | 4 per 1000 (4 to 5) | |||||
| Moderate | ||||||
| 13 per 1000 | 9 per 1000 (8 to 10) | |||||
| Dislocation of any component - All types of study Follow-up: 2.5 to 15 yr | Study population | RR 0.69 (0.6 to 0.79) | 255852 (8 studies) | +--- very low2,5 | ||
| 6 per 1000 | 4 per 1000 (4 to 5) | |||||
| Moderate | ||||||
| 14 per 1000 | 10 per 1000 Ta(8 to 11) | |||||
CI: Confidence interval; RR: Risk ratio; GRADE Working Group grades of evidence; High quality: Further research is very unlikely to change our confidence in the estimate of effect; moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate; low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate; very low quality: We are very uncertain about the estimate.
95% confidence interval around the pooled or best estimate of effect includes both (1) no effect and (2) appreciable benefit or appreciable harm (> 25%);
No explanation was provided;
Unexplained heterogeneity;
Indirect studies from registers;
Overall result from all types of study;
High heterogeneity, explained by meta-regression;
The basis for the assumed risk (e.g., the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95%CI).
Synthesis of results
Risk ratios were calculated to determine risk of revision due to any cause, revision due to aseptic loosening, revision due to infection, and dislocation between each implants. Data were analysed separately for clinical trials, cohorts and registers before pooled altogether. Fixed-effect model was used in the determination of the risk ratio. In comparison with high heterogeneity, we preformed meta-regression to evaluate to identify the source of heterogeneity. Funnel plots for all included trials was constructed to assess the degree of publication bias. The results of the study were graded according to grading system advocated by Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working Group. Statistical test was performed using the meta-analysis software of Review Manager 5, Meta-regression was conducted using STATA 10, and grading of the results was performed using GRADEprofiler 3.6.
RESULTS
Following algorithm for study selection, 27 studies were left for final analysis[8,11-36]. Characteristics of the included studies were outlined in Table 1.
Cemented vs cementless THR
Revision of any component due to any reason: Two RCTs, one cohort, and ten registers addressed revision of any component due to any reason. The RCTs found no differences between cemented and cementless THR. Analysis of registers supported cemented to be superior to cementless THR (Figure 2) Pooled all studies together, the RR was 0.47 (95%CI: 0.45-0.48) with a heterogeneity of 98%. Meta-regression using age group, diagnosis, length of follow-up, starting year, publication type, and type of funding failed to correct the heterogeneity.
Figure 2.
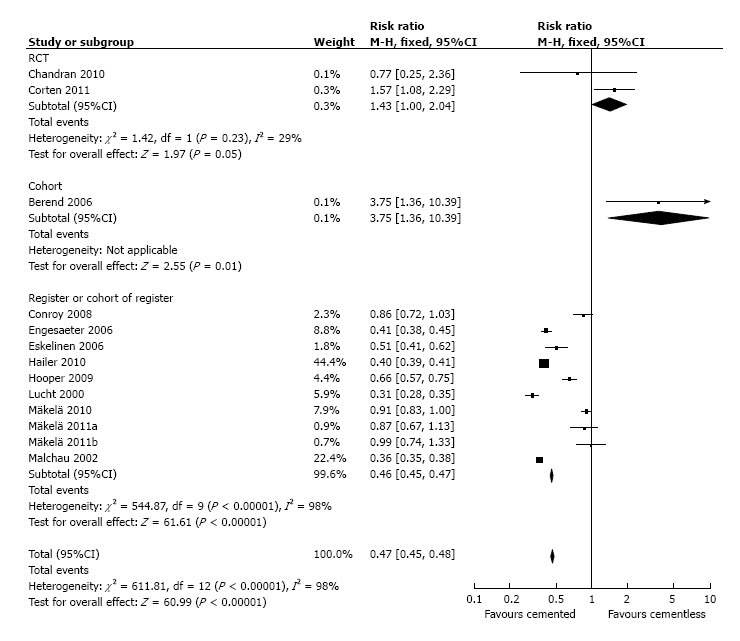
Forest plot of comparison: Cemented vs cementless: Revision of any component due to any reason.
Revision of any component due to aseptic loosening: Data regarding revision of any component due to aseptic loosening were available in two RCTs and six registers (Figure 3). Controversy existed between result of analysis of RCTs and registers (RR = 2; 95%CI: 1.2-3.1 and RR = 0.88; 95%CI: 0.83-0.94 respectively). Pooled together, the RR was 0.90 (95%CI: 0.84-0.95) with a heterogeneity of 98%. Meta-regression by age group, diagnosis, length of follow-up, starting year, publication type and funding corrected the heterogeneity into 0%, although none of the factors showed significant influence.
Figure 3.
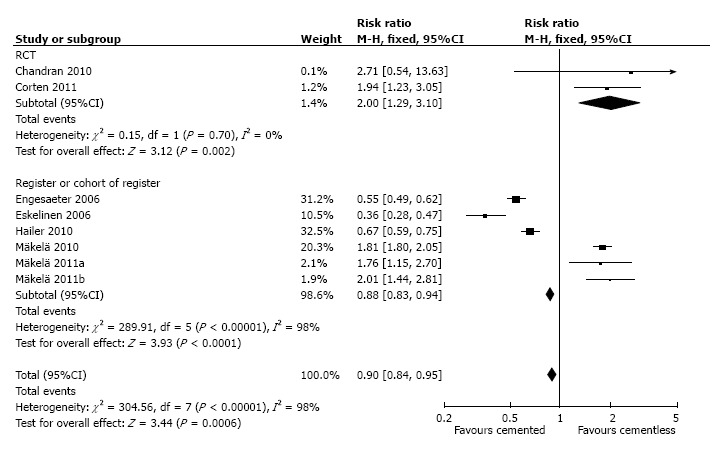
Forest plot of comparison: Cemented vs cementless: Revision of any component due to aseptic loosening.
Revision of any component due to infection: One RCT and six registers provided sufficient data for determination of revision of any component due to infection (Figure 4). Analysis of registers favored cementless implant in term of revision of any component due to infection (RR = 1.25; 95%CI: 1.10-1.42). Pooled together, the RR was 1.26 (95%CI: 1.11-1.42) with heterogeneity of 57%.
Figure 4.
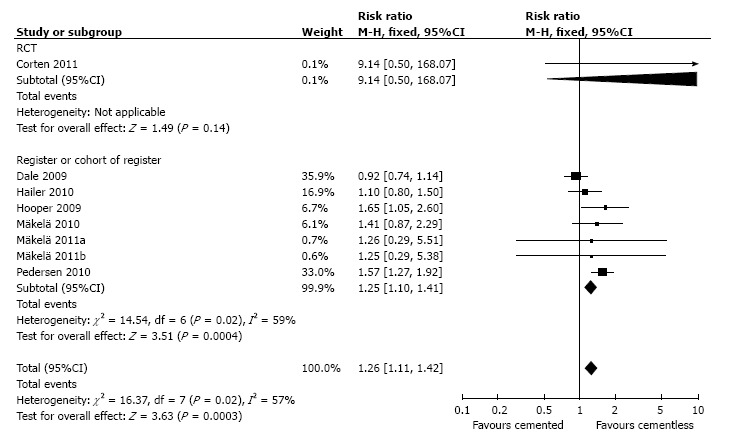
Forest plot of comparison: Cemented vs cementless: Revision of any component due to infection.
Dislocation of any component: Data from two cohorts and five registers were available to determine dislocation of any component (Figure 5). Analysis of cohorts found no difference in dislocation of any component between any types of THR while analysis of registers favors cemented THR (RR = 0.69; 95%CI: 0.29-1.67 and RR = 0.72; 95%CI: 0.64-0.80 respectively). Pooled RR was 0.72 (95%CI: 0.64-0.80) with heterogeneity of 38%.
Figure 5.
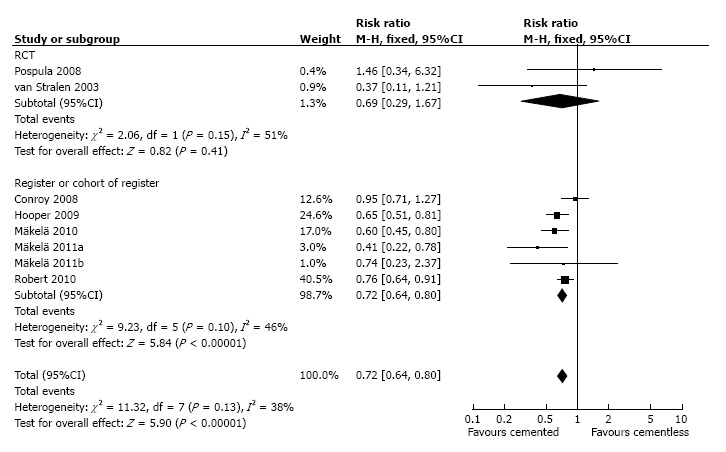
Forest plot of comparison: Cemented vs cementless: Dislocation of any component.
Cemented vs hybrid THR
Revision of any component due to any reason: Revision of any component due to any reason was addressed by two RCTs, one cohort, and three registers (Figure 6). Analysis of RCTs showed similar risk of revision of any component due to any reason while analysis of registers favored cemented fixation (RR = 0.73; 95%CI: 0.47-1.13 and RR = 0.82; 95%CI: 0.76-0.89 respectively). Pooled all studies together, the RR was 0.82 (95%CI: 0.76-0.89) with a heterogeneity of 41%.
Figure 6.
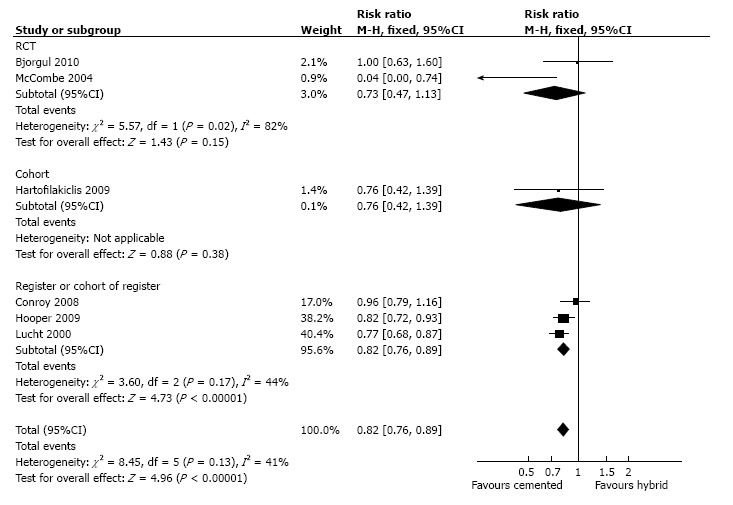
Forest plot of comparison: Cemented vs hybrid: Revision of any component due to any reason.
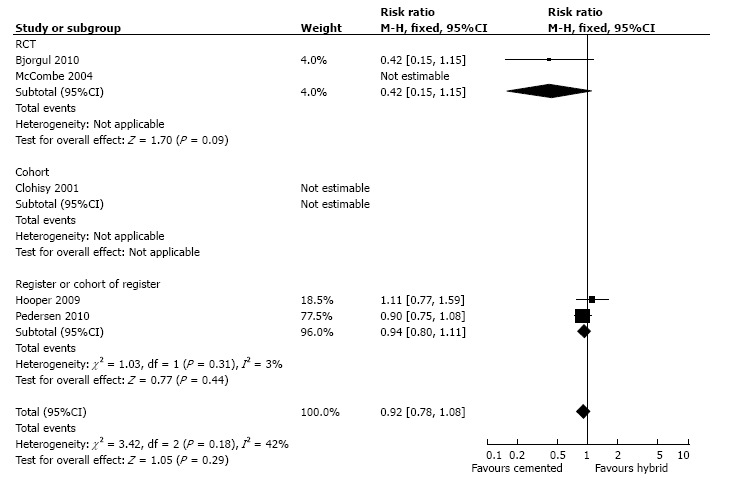
Revision of any component due to aseptic loosening: Only one RCT and one cohort provided information for evaluation of revision of any component due to aseptic loosening (Figure 7). When both studies were pooled, the RR was 2.65 (95%CI: 1.14-6.17) and the heterogeneity was 0%.
Figure 7.
Forest plot of comparison: Cemented vs hybrid: Revision of any component due to aseptic loosening.
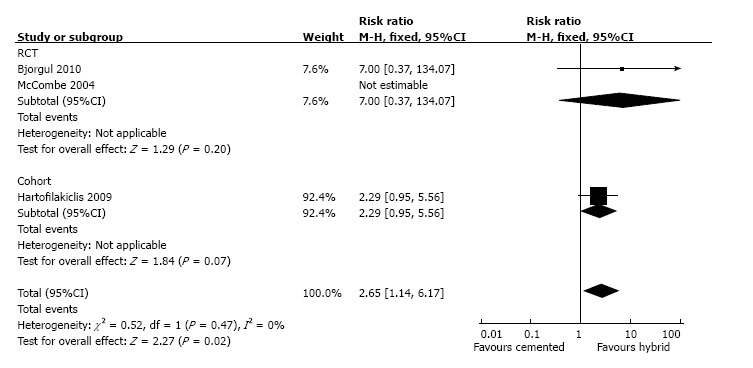
Revision of any component due to infection: Two RCTs and one cohort and two registers reported revision of any component due to infection (Figure 8). However, one RCT and the cohort encountered zero-event in both arms, so only meta-analysis of registers could be conducted, resulting in RR of 0.94 (95%CI: 0.80-1.11). If all types of study were pooled together, the RR was 0.92 (95%CI: 0.78-1.08) with heterogeneity of 42%.
Figure 8.
Forest plot of comparison: Cemented vs hybrid: Revision of any component due to infection.
Dislocation of any component: One RCT and two registers addressed dislocation of any component (Figure 9). Analysis of registers found that risk of dislocation of any component in cemented THR was lower than hybrid THR (RR = 0.11; 95%CI: 0.77-1.59). Pooled together, the RR was 0.67 (95%CI: 0.57-0.79) with heterogeneity of 0%.
Figure 9.
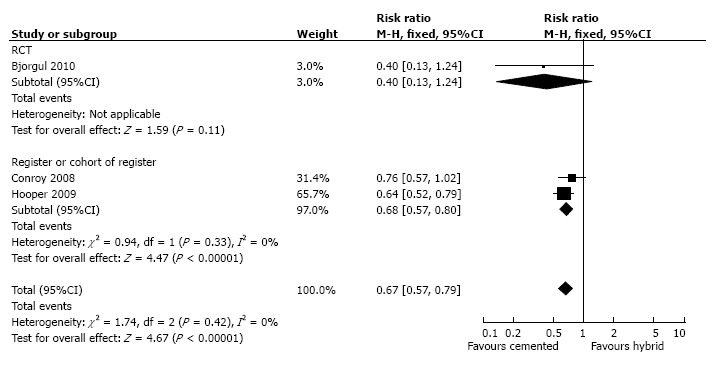
Forest plot of comparison: Cemented vs hybrid: Dislocation of any component.
Cementless vs hybrid THR
Revision of any component due to any reason: One RCT, four cohorts, and three registers investigated revision of any component due to any reason. Analysis of cohorts found similar risk while analysis of registers favored hybrid THR (Figure 10). Meta-regression reduced the heterogeneity into 23.7% but none of the factors analyzed (age group, diagnosis, length of follow-up, starting year, publication type, and funding) showed significant influence.
Figure 10.
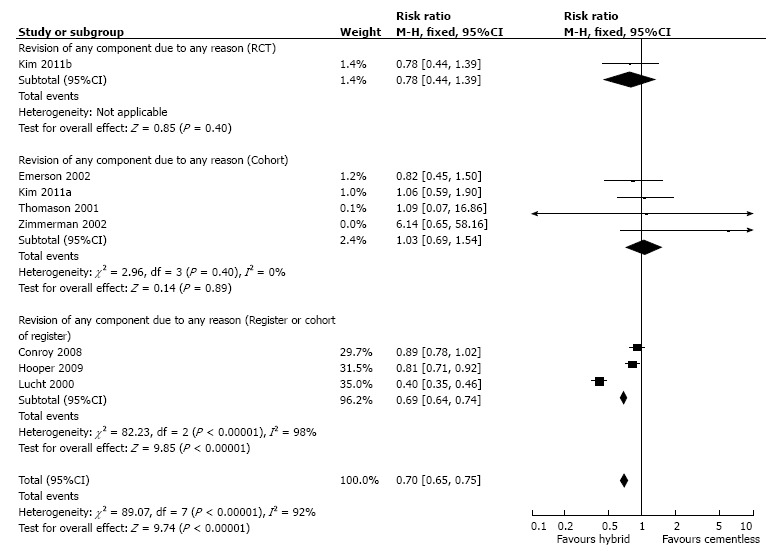
Forest plot of comparison: Cementless vs hybrid: Revision of any component due to any reason.
Revision of any component due to aseptic loosening: One RCT and three cohorts addressed risk of revision of any component due to aseptic loosening (Figure 11). However, one cohorts encountered zero-events in both arms so only two cohorts were eligible for further analysis, which revealed no difference (RR = 0.84; 95%CI: 0.47-1.51). Pooled all study types together; the RR was 0.85 (95%CI: 0.49-1.50) with heterogeneity of 0%.
Figure 11.
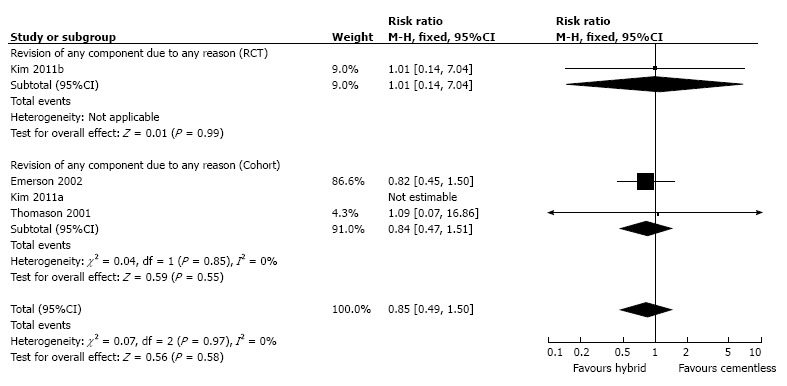
Forest plot of comparison: Cementless vs hybrid: Revision of any component due to infection.
Revision of any component due to infection: One RCT, three cohorts, and two registers addressed revision of any component due to infection (Figure 12). However, two cohorts encountered zero events in both arm of studies so insufficient cohort was left for further analysis. Analysis of registers revealed RR of 1.69 (95%CI: 1.38-2.07). If all available studies were put together, the RR was 1.69 (95%CI: 1.38-2.06) and the heterogeneity was 0%.
Figure 12.
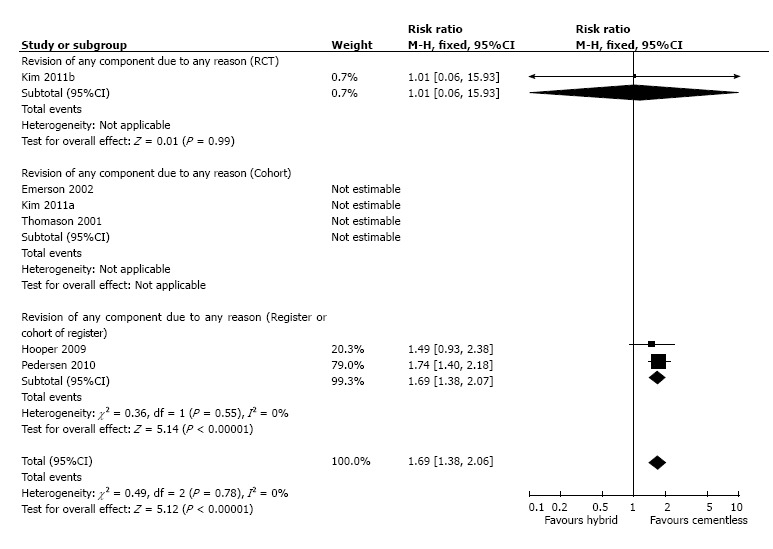
Forest plot of comparison: Cementless vs hybrid: Revision of any component due to infection.
Dislocation of any component: One RCT and two cohorts evaluated risk of dislocation (Figure 13). Analysis of the registers resulted in insignificant difference between any types of THR (RR = 1.12; 95%CI: 0.97-1.30). Pooled all study types together; the RR was 1.13 (95%CI: 0.98-1.30).
Figure 13.
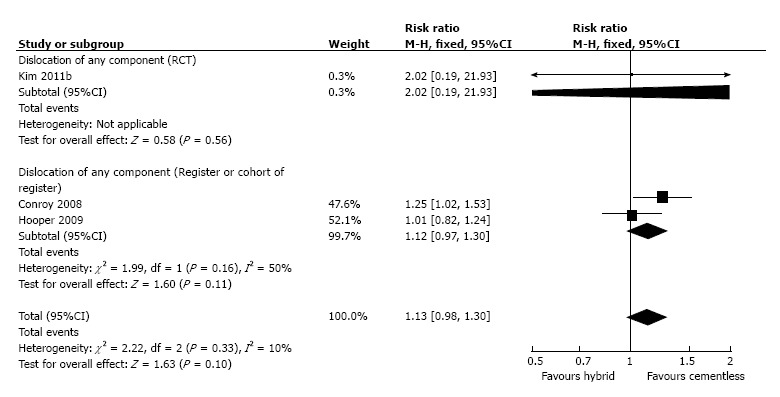
Forest plot of comparison: Cementless vs hybrid: Dislocation of any component.
Analysis of publication bias: Figure 14 showed funnel plots based on risk of revision of any component due to any reason between cemented and cementless (a), cemented and hybrid (b), and cementless and hybrid THR (c). Asymmetries were found in these plots suggesting the existence of bias.
Figure 14.
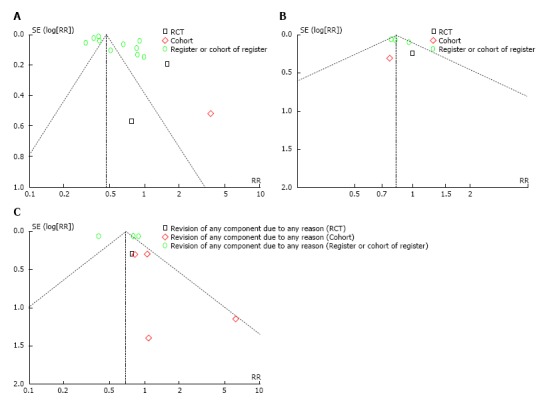
Funnel plot of comparison of revision of any component (A) cementless vs cementless; (B) cemented vs hybrid; (C) cementless vs hybrid.
Grading of the evidence: Most of the results were of low to very low level of evidence. The summaries of the grading were shown in Table 2, Table 3, Table 4.
Table 3.
Summary of finding table comparing cemented to hybrid total hip replacement
| Outcomes |
Illustrative comparative risks6 (95%CI) |
Relative effect (95%CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Hybrid | Cemented | |||||
| Revision of any component due to any reason - RCT Follow-up: 6.5 to 14 yr | Study population | RR 0.73 (0.47 to 1.13) | 402 (2 studies) | +--- very low1,2,3 | ||
| 187 per 1000 | 136 per 1000 (88 to 211) | |||||
| Moderate | ||||||
| 177 per 1000 | 129 per 1000 (83 to 200) | |||||
| Revision of any component due to any reason - Register or Cohort of register Follow-up: 4 to 7 yr | Study population | RR 0.82 (0.76 to 0.89) | 76746 (3 studies) | +--- very low3,4 | ||
| 30 per 1000 | 24 per 1000 (23 to 26) | |||||
| Moderate | ||||||
| 31 per 1000 | 25 per 1000 (24 to 28) | |||||
| Revision of any component due to any reason - All types of study Follow-up: 4 to 15.4 yr | Study population | RR 0.82 (0.76 to 0.89) | 77265 (6 studies) | +--- very low3,5 | ||
| 31 per 1000 | 25 per 1000 (23 to 27) | |||||
| Moderate | ||||||
| 104 per 1000 | 85 per 1000 (79 to 93) | |||||
| Revision of any component due to aseptic loosening - All types of study Follow-up: 6.5 to 15.4 yr | Study population | RR 2.65 (1.14 to 6.17) | 519 (3 studies) | +--- very low3,5 | ||
| 23 per 1000 | 62 per 1000 (27 to 145) | |||||
| Moderate | ||||||
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Revision of any component due to infection - Register or Cohort of register Follow-up: 0 to 14 yr | Study population | Not estimable | 86389 (2 studies) | +--- very low3,4 | ||
| 7 per 1000 | 0 per 1000 (0 to 0) | |||||
| Moderate | ||||||
| Revision of any component due to infection - All types of study Follow-up: 0 to 14 yr | Study population | RR 0.98 | 86881 | +--- | ||
| 7 per 1000 | 7 per 1000 (5 to 10) | (0.7 to 1.38) | (5 studies) | very low1,2,3,5 | ||
| Moderate | ||||||
| 2 per 1000 | 2 per 1000 (1 to 3) | |||||
| Dislocation of any component - Register of Cohort of register Follow-up: 5 to 7 yr | Study population | RR 0.68 (0.57 to 0.8) | 60584 (2 studies) | +--- very low3,4 | ||
| 11 per 1000 | 7 per 1000 (6 to 9) | |||||
| Moderate | ||||||
| 11 per 1000 | 7 per 1000 (6 to 9) | |||||
| Dislocation of any component - All types of study Follow-up: 5 to 14 yr | Study population | RR 0.67 (0.57 to 0.79) | 60824 (3 studies) | +--- very low3,5 | ||
| 11 per 1000 | 7 per 1000 (6 to 9) | |||||
| Moderate | ||||||
| 14 per 1000 | 9 per 1000 (8 to 11) | |||||
CI: Confidence interval; RR: Risk ratio; GRADE Working Group grades of evidence; High quality: Further research is very unlikely to change our confidence in the estimate of effect; moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate; low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate; very low quality: We are very uncertain about the estimate.
95% confidence interval around the pooled or best estimate of effect includes both (1) no effect and (2) appreciable benefit or appreciable harm (> 25%);
No explanation was provided;
Unexplained heterogeneity;
Indirect studies from registers;
Overall result from all types of study;
The basis for the assumed risk (e.g., the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95%CI).
Table 4.
Summary of finding table comparing hybrid and cementless total hip replacement
| Outcomes |
Illustrative comparative risks7 (95%CI) |
Relative effect (95%CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Cementless | Hybrid | |||||
| Revision of any component due to any reason - Cohort Follow-up: 1 to 17.3 yr | Study population | RR 1.03 (0.69 to 1.54) | 706 (4 studies) | +--- very low1,2 | ||
| 105 per 1000 | 108 per 1000 (72 to 161) | |||||
| Moderate | ||||||
| 106 per 1000 | 109 per 1000 (73 to 163) | |||||
| Revision of any component due to any reason - Register or Cohort of register Follow-up: 4 to 7 yr | Study population | RR 0.69 (0.64 to 0.74) | 81635 (3 studies) | +--- very low2,3,4 | ||
| 33 per 1000 | 23 per 1000 (21 to 25) | |||||
| Moderate | ||||||
| 39 per 1000 | 27 per 1000 (25 to 29) | |||||
| Revision of any component due to any reason - All types of study Follow-up: 1 to 18.4 yr | Study population | RR 0.7 (0.65 to 0.75) | 82560 (8 studies) | +--- very low2,5,6 | ||
| 34 per 1000 | 24 per 1000 (22 to 26) | |||||
| Moderate | ||||||
| 116 per 1000 | 81 per 1000 (75 to 87) | |||||
| Revision of any component due to aseptic loosening - Cohort Follow-up: 6.7 to 17.3 yr | Study population | RR 0.84 (0.47 to 1.51) | 447 (3 studies) | +--- very low1,2 | ||
| 76 per 1000 | 64 per 1000 (36 to 115) | |||||
| Moderate | ||||||
| 20 per 1000 | 17 per 1000 (9 to 30) | |||||
| Revision of any component due to aseptic loosening - All types of study Follow-up: 6.7 to 17.3 yr | Study population | RR 0.85 (0.49 to 1.5) | 666 (4 studies) | +--- very low1,2,6 | ||
| 58 per 1000 | 49 per 1000 (28 to 86) | |||||
| Moderate | ||||||
| 19 per 1000 | 16 per 1000 (9 to 28) | |||||
| Revision of any component due to infection - Register or Cohort of register Follow-up: 0 to 14 yr | Study population | Not estimable | 72197 (2 studies) | +--- very low2,4 | ||
| 4 per 1000 | 0 per 1000 (0 to 0) | |||||
| Moderate | ||||||
| Revision of any component due to infection - All types of study Follow-up: 0 to 18.4 yr | Study population | RR 1.47 (0.93 to 2.34) | 72863 (5 studies) | +--- very low1,2,6 | ||
| 4 per 1000 | 6 per 1000 (4 to 10) | |||||
| Moderate | ||||||
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Dislocation of any component - Register or Cohort of register Follow-up: 5 to 7 yr | Study population | RR 1.12 (0.97 to 1.3) | 75114 (2 studies) | +--- very low1,2,4 | ||
| 9 per 1000 | 10 per 1000 (9 to 11) | |||||
| Moderate | ||||||
| 10 per 1000 | 11 per 1000 (10 to 13) | |||||
| Dislocation of any component - All types of study Follow-up: 5 to 18.4 yr | Study population | RR 1.13 (0.98 to 1.3) | 75333 (3 studies) | +--- very low1,2,6 | ||
| 9 per 1000 | 10 per 1000 (9 to 11) | |||||
| Moderate | ||||||
| 9 per 1000 | 10 per 1000 (9 to 12) | |||||
CI: Confidence interval; RR: Risk ratio; GRADE Working Group grades of evidence; High quality: Further research is very unlikely to change our confidence in the estimate of effect; moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate; low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate; very low quality: We are very uncertain about the estimate.
95% confidence interval around the pooled or best estimate of effect includes both (1) no effect and (2) appreciable benefit or appreciable harm (> 25%);
No explanation was provided;
Unexplained heterogeneity;
Indirect studies from registers;
Overall result from all types of study;
High heterogeneity, explained by meta-regression;
The basis for the assumed risk (e.g., the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95%CI).
DISCUSSION
We summarized the evidence from 5 randomized clinical trials, 9 cohorts, and 13 registers or cohorts of register about total hip replacement and found that that cemented THR was superior to cementless THR and hybrid THR in terms of risk of revision due to any reason. Moreover, cemented THR was also more superior compared with cementless THR if revision due to aseptic loosening and revision due to dislocation were used as the endpoint but inferior if revision due to infection was used. Cemented THR was superior to hybrid THR in the risk of revision due to any reason and dislocation. Meanwhile cementless THR was most inferior compared to the others in risk of revision due to any reason.
In our knowledge, Morshed et al[9] performed the first metaanalysis reviewing the survival and outcome of cemented and uncemented fixation in total hip replacement in 2007. Although cemented fixation seemed to outperform cementless fixation in large subsets of study population, there was no significant advantages were found for either type of fixation in terms of survival. There was an association between difference in survival and year of publication, with cementless fixation showing relative superiority over time. However, our recent analysis still suggested that cemented fixation continued to outperform uncemented fixation especially in large study populations (registers)[24,26-33].
Recent metaanalysis by Abdulkarim et al[37] reviewed 9 RCTs that primarily comparing implants survival between cemented and cementless THR. In their study, no significant differences were found in implant survival especially as measured by the revision rate. By using RCT, which is the gold standard of clinical research, the quality of evidence in GRADE approach should be moderate or even high. However, the average follow up duration were only 4.3 years (2-8 years), which was relatively short to evaluate the implant survival.
In our study, an analysis of 2 RCTs comparing the survival of cemented and cementless implant was performed. As the duration of follow up ranged from 14-19 years, these RCTs would give a better evaluation in terms of implant survival. In this analysis, the relative risk of revision due to any revision was higher in cemented group with RR = 1.43 (1-2.04), which also meant that the cementless implant was superior. But it were pooled together with the cohort studies and registers, the results would be contradictive as it favored the cemented implant with RR = 0.47 (0.46-0.48).
Despite the tendencies of most registers towards cemented implant, there are some studies and even some registries[29,30,33] noted that uncemented implant survived better in the group of younger patients. Malchau et al[33] in their Swedish arthroplasty register, found that uncemented implants had better survival in patients with less than 55 years of age. Similar findings were reported by the Lucht et al[29] when they evaluated the Danish arthroplasty register. Eskelinen et al[26] in the Finnish arthroplasty register, reported that in age group under 55-years had higher revision rates for aseptic loosening in cemented group compared with proximally coated cementless femoral components. Further analysis of Finnish arthroplasty register in patients aged 55-year and older showed that uncemented femoral stem has better survival in the 55 to 74-year age group while there was no significant difference in 75-year and older patients[30].
This series of studies might explain the reason why contradictive result occurred in our analysis. In their inclusion criteria, both RCTs used 75 years as the upper age limit without any lower age limit, and the average age in both RCTs was around 64 years[12,13]. It was seemed that this fact might play a role in our result.
Hybrid THR was first introduced to address the results of cemented THR in younger patients in whom acetabular failure was the main reason for revision. However, recent studies reported that hybrid THR was the most common THR types to be revised due to dislocation in the first 90 d and even after 90 d after the primary surgery[28]. In their prospective multicenter study about primary total hip arthroplasty revision due to dislocation, Girard et al[38] described that, from their revision series, cementless acetabular fixation and cemented femoral stem fixation were involved in a higher number of dislocation which are 63.8% and 53% respectively. However it was not mentioned about the reason why cementless acetabular fixation has a higher chance of dislocation compared to the cemented one. Although there are no supporting data, there was a hypothesis that positioning of acetabular component may be more accurate in cemented components[23]. Although Parrate and Argenson[39] didn’t include cemented acetabular cup in their study, they showed that 57% cementless cup that inserted in conventional way and 20% navigated were outside of the defined safe zone (outliers). While cementing the acetabular component, few adjustments can be made during insertion and while waiting for the cement polymerization. On the other hand, cementless cup has less adjustability and may change their orientation from the most desired position during the final seating of the component. Despite all, from the economic perspective, hybrid prostheses lead to grater gain in mean postoperative quality of life and the most cost effective alternative for most patients according to cost effectiveness analysis model by Pennington et al[40].
Clinical trials, cohorts, and register-based studies were included into our meta-analysis. Inclusion of register based studies had certain benefits and limitations[30,36]. Register provided large number of samples for analysis and the population data corresponded to the actual population[36]. Moreover, a poor result in a single center would not have major effect on the result of the study[30]. Despite RCTs is considered the gold standard design for clinical research, one of its disadvantages is that strict inclusion and exclusion criteria might not reflect the condition of real population, as it often narrowed the samples to a highly selected group of patients that is operated by only a few surgeons. However, the desired outcome was not the main purpose of the registry. Accuracy of the data might be limited due to inconsistencies or errors in data collection inputted to the register[41]. Data available in clinical trials and cohorts might also have been included in the register and therefore were used twice in the analysis.
Various implant designs, surgical approaches and techniques (such as cementing technique), rehabilitation protocols, and activity levels were included in our study. Lack of data prevented us to analyze them separately in subgroup analysis or in meta-regression. Therefore, it was understandable that high heterogeneity existed in our study. We explored the heterogeneity to the greatest degree possible, in to a meta-regression, yet very high heterogeneity remained in some comparison.
Very high heterogeneity indicated that effect size of each study varied greatly[42]. Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working group recommended to lower the quality assessment in study with unexplained heterogeneity[41]. Even though the result was obtain by a meta-analysis, interpreting the result must be careful.
In conclusion, despite some limitations in the selected studies especially the low quality assessment and heterogeneity, there was some tendency that cemented fixation was still superior than other types of fixation in terms of implant survival. Future high quality randomized clinical trials, preferably multicenter, to obtain larger sample size, considering all factors that may influent results, are required to give definite recommendations regarding the best type of total hip replacement.
COMMENTS
Background
Controversies still persisted on the optimal method of fixation for primary total hip replacement (THR). Previous meta-analysis found no difference between cemented and cementless implant, but since then, many larger studies with longer duration of follow-up had been conducted. In this meta-analysis, more recent studies were enrolled to determine whether cemented, cementless, or hybrid implant was superior to the other.
Research frontiers
Implant survival analysis in different type of THR fixation is still a controversial debate. Worldwide researches are still focused on which type of implant that suits best on patients to provide better care to the patients.
Innovations and breakthroughs
Despite some limitations in the selected studies especially the low quality assessment and heterogeneity, their study presented a metaanalysis of studies with a long duration of follow up, which would give a better perspective in terms of implant survival. There was some tendency that cemented fixation was still superior than other types of fixation.
Applications
There was some tendency that cemented fixation was still superior to other types of fixation.
Peer-review
It is well presented, well-structured and extensively build up and therefore useful for the readers.
Footnotes
Conflict-of-interest statement: The authors declare no conflicts of interest regarding this manuscript.
Data sharing statement: No data were created no data are available.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Indonesia
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
Peer-review started: September 7, 2016
First decision: September 29, 2016
Article in press: December 9, 2016
P- Reviewer: Antoniadis A, Drosos GI, Li XM S- Editor: Qiu S L- Editor: A E- Editor: Lu YJ
References
- 1.Ostendorf M, Johnell O, Malchau H, Dhert WJ, Schrijvers AJ, Verbout AJ. The epidemiology of total hip replacement in The Netherlands and Sweden: present status and future needs. Acta Orthop Scand. 2002;73:282–286. doi: 10.1080/000164702320155257. [DOI] [PubMed] [Google Scholar]
- 2.Merx H, Dreinhöfer K, Schräder P, Stürmer T, Puhl W, Günther KP, Brenner H. International variation in hip replacement rates. Ann Rheum Dis. 2003;62:222–226. doi: 10.1136/ard.62.3.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Felson DT, Zhang Y. An update on the epidemiology of knee and hip osteoarthritis with a view to prevention. Arthritis Rheum. 1998;41:1343–1355. doi: 10.1002/1529-0131(199808)41:8<1343::AID-ART3>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 4.Wroblewski BM. Cementless versus cemented total hip arthroplasty. A scientific controversy? Orthop Clin North Am. 1993;24:591–597. [PubMed] [Google Scholar]
- 5.Rorabeck CH, Bourne RB, Laupacis A, Feeny D, Wong C, Tugwell P, Leslie K, Bullas R. A double-blind study of 250 cases comparing cemented with cementless total hip arthroplasty. Cost-effectiveness and its impact on health-related quality of life. Clin Orthop Relat Res. 1994;(298):156–164. [PubMed] [Google Scholar]
- 6.Rorabeck CH, Bourne RB, Mulliken BD, Nayak N, Laupacis A, Tugwell P, Feeney D. The Nicolas Andry award: comparative results of cemented and cementless total hip arthroplasty. Clin Orthop Relat Res. 1996;(325):330–344. [PubMed] [Google Scholar]
- 7.Zimmerma S, Hawkes WG, Hudson JI, Magaziner J, Hebel JR, Towheed T, Gardner J, Provenzano G, Kenzora JE. Outcomes of surgical management of total HIP replacement in patients aged 65 years and older: cemented versus cementless femoral components and lateral or anterolateral versus posterior anatomical approach. J Orthop Res. 2002;20:182–191. doi: 10.1016/S0736-0266(01)00090-0. [DOI] [PubMed] [Google Scholar]
- 8.Emerson RH, Head WC, Emerson CB, Rosenfeldt W, Higgins LL. A comparison of cemented and cementless titanium femoral components used for primary total hip arthroplasty: a radiographic and survivorship study. J Arthroplasty. 2002;17:584–591. doi: 10.1054/arth.2002.32696. [DOI] [PubMed] [Google Scholar]
- 9.Morshed S, Bozic KJ, Ries MD, Malchau H, Colford JM. Comparison of cemented and uncemented fixation in total hip replacement: a meta-analysis. Acta Orthop. 2007;78:315–326. doi: 10.1080/17453670710013861. [DOI] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Bjørgul K, Novicoff WM, Andersen ST, Brevig K, Thu F, Wiig M, Ahlund O. No differences in outcomes between cemented and uncemented acetabular components after 12-14 years: results from a randomized controlled trial comparing Duraloc with Charnley cups. J Orthop Traumatol. 2010;11:37–45. doi: 10.1007/s10195-010-0082-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chandran P, Azzabi M, Miles J, Andrews M, Bradley J. Furlong hydroxyapatite-coated hip prosthesis vs the Charnley cemented hip prosthesis. J Arthroplasty. 2010;25:52–57. doi: 10.1016/j.arth.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Corten K, Bourne RB, Charron KD, Au K, Rorabeck CH. Comparison of total hip arthroplasty performed with and without cement: a randomized trial. A concise follow-up, at twenty years, of previous reports. J Bone Joint Surg Am. 2011;93:1335–1338. doi: 10.2106/JBJS.J.00448. [DOI] [PubMed] [Google Scholar]
- 14.Kim YH, Kim JS, Park JW, Joo JH. Comparison of total hip replacement with and without cement in patients younger than 50 years of age: the results at 18 years. J Bone Joint Surg Br. 2011;93:449–455. doi: 10.1302/0301-620X.93B4.26149. [DOI] [PubMed] [Google Scholar]
- 15.Kim YH, Kim JS, Park JW, Joo JH. Contemporary total hip arthroplasty with and without cement in patients with osteonecrosis of the femoral head: a concise follow-up, at an average of seventeen years, of a previous report. J Bone Joint Surg Am. 2011;93:1806–1810. doi: 10.2106/JBJS.J.01312. [DOI] [PubMed] [Google Scholar]
- 16.McCombe P, Williams SA. A comparison of polyethylene wear rates between cemented and cementless cups. A prospective, randomised trial. J Bone Joint Surg Br. 2004;86:344–349. doi: 10.1302/0301-620x.86b3.14567. [DOI] [PubMed] [Google Scholar]
- 17.Berend ME, Smith A, Meding JB, Ritter MA, Lynch T, Davis K. Long-term outcome and risk factors of proximal femoral fracture in uncemented and cemented total hip arthroplasty in 2551 hips. J Arthroplasty. 2006;21:53–59. doi: 10.1016/j.arth.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 18.Clohisy JC, Harris WH. Matched-pair analysis of cemented and cementless acetabular reconstruction in primary total hip arthroplasty. J Arthroplasty. 2001;16:697–705. doi: 10.1054/arth.2001.24447. [DOI] [PubMed] [Google Scholar]
- 19.Hartofilakidis G, Georgiades G, Babis GC. A comparison of the outcome of cemented all-polyethylene and cementless metal-backed acetabular sockets in primary total hip arthroplasty. J Arthroplasty. 2009;24:217–225. doi: 10.1016/j.arth.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 20.Pospula W, Abu Noor T, Roshdy T, Al Mukaimi A. Cemented and cementless total hip replacement. Critical analysis and comparison of clinical and radiological results of 182 cases operated in Al Razi Hospital, Kuwait. Med Princ Pract. 2008;17:239–243. doi: 10.1159/000117799. [DOI] [PubMed] [Google Scholar]
- 21.van Stralen GM, Struben PJ, van Loon CJ. The incidence of dislocation after primary total hip arthroplasty using posterior approach with posterior soft-tissue repair. Arch Orthop Trauma Surg. 2003;123:219–222. doi: 10.1007/s00402-003-0482-3. [DOI] [PubMed] [Google Scholar]
- 22.Thomason HC, Lachiewicz PF. The influence of technique on fixation of primary total hip arthroplasty in patients with rheumatoid arthritis. J Arthroplasty. 2001;16:628–634. doi: 10.1054/arth.2001.23720. [DOI] [PubMed] [Google Scholar]
- 23.Conroy JL, Whitehouse SL, Graves SE, Pratt NL, Ryan P, Crawford RW. Risk factors for revision for early dislocation in total hip arthroplasty. J Arthroplasty. 2008;23:867–872. doi: 10.1016/j.arth.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 24.Dale H, Hallan G, Hallan G, Espehaug B, Havelin LI, Engesaeter LB. Increasing risk of revision due to deep infection after hip arthroplasty. Acta Orthop. 2009;80:639–645. doi: 10.3109/17453670903506658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Engesaeter LB, Espehaug B, Lie SA, Furnes O, Havelin LI. Does cement increase the risk of infection in primary total hip arthroplasty? Revision rates in 56,275 cemented and uncemented primary THAs followed for 0-16 years in the Norwegian Arthroplasty Register. Acta Orthop. 2006;77:351–358. doi: 10.1080/17453670610046253. [DOI] [PubMed] [Google Scholar]
- 26.Eskelinen A, Paavolainen P, Helenius I, Pulkkinen P, Remes V. Total hip arthroplasty for rheumatoid arthritis in younger patients: 2,557 replacements in the Finnish Arthroplasty Register followed for 0-24 years. Acta Orthop. 2006;77:853–865. doi: 10.1080/17453670610013132. [DOI] [PubMed] [Google Scholar]
- 27.Hailer NP, Garellick G, Kärrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthop. 2010;81:34–41. doi: 10.3109/17453671003685400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hooper GJ, Rothwell AG, Stringer M, Frampton C. Revision following cemented and uncemented primary total hip replacement: a seven-year analysis from the New Zealand Joint Registry. J Bone Joint Surg Br. 2009;91:451–458. doi: 10.1302/0301-620X.91B4.21363. [DOI] [PubMed] [Google Scholar]
- 29.Lucht U. The Danish Hip Arthroplasty Register. Acta Orthop Scand. 2000;71:433–439. doi: 10.1080/000164700317381081. [DOI] [PubMed] [Google Scholar]
- 30.Mäkelä KT, Eskelinen A, Paavolainen P, Pulkkinen P, Remes V. Cementless total hip arthroplasty for primary osteoarthritis in patients aged 55 years and older. Acta Orthop. 2010;81:42–52. doi: 10.3109/17453671003635900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mäkelä KT, Eskelinen A, Pulkkinen P, Virolainen P, Paavolainen P, Remes V. Cemented versus cementless total hip replacements in patients fifty-five years of age or older with rheumatoid arthritis. J Bone Joint Surg Am. 2011;93:178–186. doi: 10.2106/JBJS.I.01283. [DOI] [PubMed] [Google Scholar]
- 32.Mäkelä KT, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. Results of 3,668 primary total hip replacements for primary osteoarthritis in patients under the age of 55 years. Acta Orthop. 2011;82:521–529. doi: 10.3109/17453674.2011.618908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Malchau H, Herberts P, Eisler T, Garellick G, Söderman P. The Swedish Total Hip Replacement Register. J Bone Joint Surg Am. 2002;84-A Suppl 2:2–20. doi: 10.2106/00004623-200200002-00002. [DOI] [PubMed] [Google Scholar]
- 34.Pedersen AB, Svendsson JE, Johnsen SP, Riis A, Overgaard S. Risk factors for revision due to infection after primary total hip arthroplasty. A population-based study of 80,756 primary procedures in the Danish Hip Arthroplasty Registry. Acta Orthop. 2010;81:542–547. doi: 10.3109/17453674.2010.519908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Roberts DJS, Garlick NI. Increased rate of dislocation of total hip arthroplasty with cementless implants: accuracy of acetabular inclination. Internet J Orthop Surg. 2010;17:1. [Google Scholar]
- 36.Skyttä ET, Jarkko L, Antti E, Huhtala H, Ville R. Increasing incidence of hip arthroplasty for primary osteoarthritis in 30- to 59-year-old patients. Acta Orthop. 2011;82:1–5. doi: 10.3109/17453674.2010.548029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Abdulkarim A, Ellanti P, Motterlini N, Fahey T, O’Byrne JM. Cemented versus uncemented fixation in total hip replacement: a systematic review and meta-analysis of randomized controlled trials. Orthop Rev (Pavia) 2013;5:e8. doi: 10.4081/or.2013.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Girard J, Kern G, Migaud H, Delaunay C, Ramdane N, Hamadouche M. Primary total hip arthroplasty revision due to dislocation: prospective French multicenter study. Orthop Traumatol Surg Res. 2013;99:549–553. doi: 10.1016/j.otsr.2013.03.026. [DOI] [PubMed] [Google Scholar]
- 39.Parratte S, Argenson JN. Validation and usefulness of a computer-assisted cup-positioning system in total hip arthroplasty. A prospective, randomized, controlled study. J Bone Joint Surg Am. 2007;89:494–499. doi: 10.2106/JBJS.F.00529. [DOI] [PubMed] [Google Scholar]
- 40.Pennington M, Grieve R, Sekhon JS, Gregg P, Black N, van der Meulen JH. Cemented, cementless, and hybrid prostheses for total hip replacement: cost effectiveness analysis. BMJ. 2013;346:f1026. doi: 10.1136/bmj.f1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ. What is “quality of evidence” and why is it important to clinicians? BMJ. 2008;336:995–998. doi: 10.1136/bmj.39490.551019.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thompson SG, Higgins JP. How should meta-regression analyses be undertaken and interpreted? Stat Med. 2002;21:1559–1573. doi: 10.1002/sim.1187. [DOI] [PubMed] [Google Scholar]


