Abstract
Elbow arthroscopy is a technical challenging surgical procedure because of close proximity of neurovascular structures and the limited articular working space. With the rising number of elbow arthroscopies being performed nowadays due to an increasing number of surgeons performing this procedure and a broader range of indications, a rise in complications is foreseen. With this editorial we hope to create awareness of possible complications of elbow arthroscopy, particularly nerve injuries, and provide a guideline to avoid complications during elbow arthroscopy.
Keywords: Elbow, Arthroscopy, Complications, Nerve injury, Education, Preventive strategies
Core tip: Elbow arthroscopy is a technical challenging surgical procedure because of close proximity of neurovascular structures and the limited articular working space. With the rising number of elbow arthroscopies being performed nowadays due to an increasing number of surgeons performing this procedure and a broader range of indications, a rise in complications is foreseen. With this editorial we hope to create awareness of possible complications of elbow arthroscopy, particularly nerve injuries, and provide a guideline to avoid complications during elbow arthroscopy.
INTRODUCTION
A small working space and close by neurovascular structures are the main reasons elbow arthroscopy is a technical challenging surgical procedure[1-12]. Advantages over open surgery may be less scar tissue, decreased risk of infection, less postoperative pain, fast return to work and sports and better visualization of intra-articular pathology[13-17]. Nowadays arthroscopy of the elbow is performed more frequently for an increasing range of indications; loose bodies, primary degenerative and rheumatoid arthritis, posttraumatic contractures, lateral/medial epicondylitis, osteochondral defects, posteromedial impingement, synovial disorders, fractures of the radial head, capitellum and coronoid, and debridement of osteophytes[2,18-22]. With the rising number of elbow arthroscopies being performed nowadays due to an increasing number of surgeons performing this procedure and a broader range of indications, a rise in complications is foreseen.
A range of complications has been described after elbow arthroscopy, such as: Transient neuropraxia[3,6,13,23-45], permanent nerve injury[28,41,46-55], complex regional pain syndrome[31], delayed wound healing[31], superficial wound infection[28,32,37,42,43,56-58], deep wound infection[32], limited range of motion[28,44,59], synovial fistula[28,37], ganglion cyst at portal site[32], granuloma of portal scar[39], heterotopic ossifications[23,32,43] and triceps tendon ossification[32]. One of the most devastating complications is nerve injury[19,60] of which the majority is fortunately transient[13,32].
Recently Desai et al[60] conducted a survey among the member of the American Society for Surgery of the Hand to determine which nerves and what kind of nerve injuries were treated after elbow arthroscopy over a five-year period; 222 nerve injuries were identified, an estimated 1.2% occurrence rate. In half of the patients additional surgical intervention was needed; 77%-80% had either partial or no recovery. This seems contradictory with the only 13 cases on permanent nerve injury after elbow arthroscopy published in current literature[28,41,46-55]. Desai et al[60] stated that in view of the high number of elbow arthroscopies performed these days permanent nerve injury is probably under-reported. In current literature the ulnar nerve seems most susceptible for nerve injury during elbow arthroscopy[60-62].
The goal of this current concepts review is to raise awareness of possible complications of elbow arthroscopy, in particular nerve injuries, and provide a practical guideline that can help to avoid nerve complications during elbow arthroscopy.
HOW TO AVOID NERVE COMPLICATIONS IN ELBOW ARTHROSCOPY?
A general necessity is thorough knowledge of the anatomy of the elbow in order to comprehend the spatial relation among neurovascular structures and portals and be able to safely perform elbow arthroscopy (Figure 1, Figure 2 and Figure 3).
Figure 1.
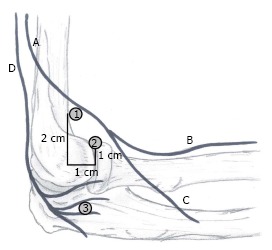
Proximity of nerves and portals: Lateral side view. A: Radial nerve; B: Superficial branch; C: Deep branch; D: Posterior antebrachial cutaneous nerve; 1: Proximal lateral portal; 2: Anterolateral portal; 3: Midlateral portal.
Figure 2.
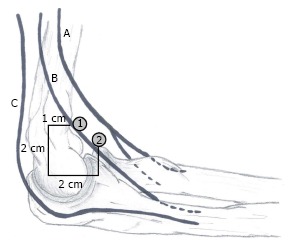
Proximity of nerves and portals: Medial side view. A: Median nerve; B: Medial antebrachial cutaneous nerve; C: Ulnar nerve; 1: Proximal medial portal; 2: Anteromedial portal.
Figure 3.
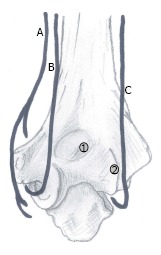
Proximity of nerves and portals: Posterior side view. A: Medial antebrachial cutaneous nerve; B: Ulnar nerve; C: Posterior antebrachial cutaneous nerve; 1: Transtricipital portal; 2: Posterolateral portal.
Work up
Avoiding peri-operative complications starts with a proper work-up. Firstly, there has to be a valid indication for surgery, which starts with patient complaints, history taking and physical examination. Setting a valid indication prevents unnecessary surgery and subsequently prevents neurological complications. A history of trauma, previous elbow surgery or rheumatoid arthritis, or burns, skingrafts, a subluxing ulnar nerve or congenital deformity of the elbow on physical examination can be complicating factors for surgery due to alteration of the anatomy; for example nerves can be adhered to the capsule[63], the capsule may have less distension capacity and scar tissue may make identifying nerves and vessels difficult. Additional imaging studies (CT, MRI or ultrasound) might be needed to confirm the diagnosis or for careful planning of surgery when expecting changed or difficult anatomy (Figure 4)[25]. For example, a subluxing or previously transposed ulnar nerve. The incidence of a subluxing ulnar nerve is reported to be 11%-21%[64,65] and not recognizing its presence preoperatively may lead to iatrogenic ulnar nerve injury. Dodson et al[19] suggested that arthroscopic surgery should be avoided if the patient had undergone previous ulnar nerve transposition. In order to prevent missing a not physiological ulnar nerve course it is recommended to routinely report if patients had a ulnar nerve transposition or are diagnosed with a subluxing ulnar nerve during physical examination in the outpatient setting.
Figure 4.
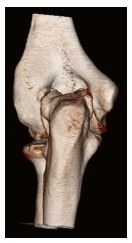
Osteophytes can cause changed anatomy, for example posteromedial osteophytes could push the ulnar nerve out of its groove.
Preoperative preventive measures
Prior to incision and distension of the joint, preoperative examination under anesthesia, marking of anatomic landmarks and portal sites, and palpation of the course of the ulnar nerve are of great importance to obtain good orientation and avoid complications[3,18,28,66] (Figures 5 and 6). In cases with changed ulnar nerve anatomy a possible safe anteromedial approach depending on with what certainty the course of the ulnar nerve can be determined is described by Sahajpal et al[66]. If the course is unequivocal a safe anteromedial approach is possible by placing the portal 1cm from the nerve, if the course is equivocal portal placement should be 1 cm from the nerve by mini-incision, or by open approach via an incision of 2- to 4-cm in order to identify the nerve and subsequently place the portal if localization of the nerve is impossible. However, in the opinion of the authors the safest approach of an elbow with a subluxing or transposed ulnar nerve is an immediate open approach and starting elbow arthroscopy after identifying the ulnar nerve. Whenever establishing or re-entering the portal the ulnar nerve should be fixated posteriorly of the medial epicondyle.
Figure 5.

Marking of anatomical structures and portals: Lateral side view. A: Lateral epicondyle; B: Anterolateral portal; C: Radial head.
Figure 6.
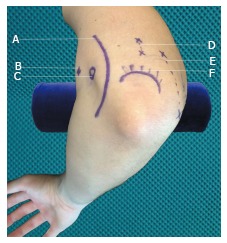
Marking of anatomical structures and portals: Medial side view. A: Ulnar nerve; B: Proximal medial portal; C: Medial epicondyle; D: Transtricipetal portals; E: Posterolateral portals; F: Olecranon.
Anesthesia
Most surgeons prefer general anesthesia with total muscle relaxation because of patient comfort and the disabling of unexpected patient movement, and it allows for supine positioning[2,18]. Some surgeons prefer to add regional anesthesia, for optimal reduction of postoperative pain. However, in a randomized controlled trial performed by Wada et al[67] no additional pain relief was observed using a supplemental axillary nerve block over general anesthesia alone. In addition, regional anesthesia has a small risk for nerve injury with an incidence of 3:10000 based on two large prospective studies[68-70].
Patient positioning
Several alternatives are available in positioning of the patient: The most common are the lateral decubitus position and the supine-suspended position with the use of a limb positioner (Figure 7). An advantage of the lateral decubitus position over the supine-suspended position is that gravity assists in displacing the neurovascular structures away from the anterior capsule and from the anterior working field. Furthermore, the lateral decubitus position facilitates easy access to all compartments. A stable and comfortable patient position can be achieved by use of vacuum beanbag immobilizer.
Figure 7.
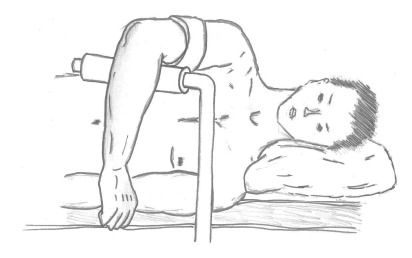
Lateral decubitus position.
Joint distension
When proper orientation of the surgical landmarks and patient positioning has been acquired, the next step is fluid distension (20-30 mL) of the joint via the midlateral soft spot or via a posterior approach. The latter approach is preferred by the authors because of the absence of cartilage in addition to the absence of nerves. Fluid distension of the elbow joint space moves the neurovascular structures away from the surgical field by expanding the joint capsule[3-5,10,45,71-75] (Figures 8 and 9). It is very important to realize that the nerve-to-capsule distance does not increase with joint distension, but only nerve-to-portal distance and the nerve to osseous structures distance[3,5,75,76]. Therefore, joint distension probably reduces the chance of nerve injury during joint entry via the portals and during intra-articular surgical procedures, but not during performance of capsular procedures. Since the capsule may rupture at pressures below 50 mmHg, it is advised to use gravitational force only, and avoid pressurized infusion, to keep the joint distended. Higher pressures occurring in fluid pumps cause fluid to flow extra-articular decreasing joint visibility[76,77]. Saline-infusion of 5 mL or less indicates a decreased displacement of neurovascular structures and less working space, for example in elbow contractures, making surgery more complicated[1]. Successful joint insufflation of the elbow with fluid will cause an extension movement.
Figure 8.
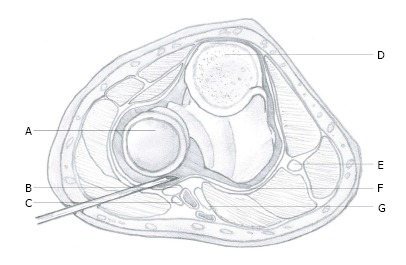
Non-distended joint. A: Head of radius; B: Radial nerve; C: Lateral antebrachial nerve; D: Cross-section of olecranon; E: Ulnar nerve; F: Capsule; G: Median nerve.
Figure 9.
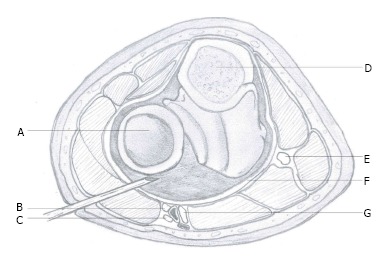
Distended joint joint. A: Head of radius; B: Radial nerve; C: Lateral antebrachial nerve; D: Cross-section of olecranon; E: Ulnar nerve; F: Capsule; G: Median nerve.
Elbow positioning
It is advised to flex the elbow to 90 degrees as it displaces the brachial artery and the anterior nerves anteriorly[4,9], maximizing the distance between the joint capsule and the brachial artery, and the nerve-to-capsule distance[3,73]. The distance between the portals and the medial and radial nerves is doubled solely by elbow flexion, in combination with the aforementioned joint distension this distance even triples[72]. Furthermore, capsular capacity is maximized by flexion, increasing arthroscopic working space and minimizing the chance of neurovascular complications[1,3-5,73,78]. Disorders as rheumatoid arthritis, stiff and posttraumatic elbows may compromise the distension capacity of the capsule, thus raising the risk of neurovascular complications[1,3,5,13,38,52]. For maximal range of flexion, compression of the flexion crease due to supportive arm holders should be avoided.
Portal placement
Portal placing can cause nerve injury[13,18,46,62]. The above-mentioned preventive measures are meant to minimize the risk of neurovascular injury during the placing of portals. Mini-incision of the skin, avoiding incision of subcutaneous tissue, and the use of a blunt trocar or clamp are the first two preventive measures to avoid injury to the antebrachial nerves[9,75]. Furthermore, recognize that portals placed proximally of the joint have the tendency of being safer[9,79]. Pronation (in addition to flexion) of the elbow protects the posterior interosseous nerve when placing lateral portals. The elbow should be in midpronation at least. This way the nerve is brought more anteromedial and the portal-to-nerve distance has increased[4,78,80]. When assessing the anterior compartment of the elbow it is advised to start with an anteromedial portal subsequently placing a lateral portal using the camera because this possibly reduces the risk of radial nerve, i.e., posterior interosseous nerve (PIN), injury[7,9,10,12]. The proximal medial portal might even be a superior alternative compared to the anteromedial portal due to greater distance to the medial antebrachial nerve and no difference in arthroscopic view[9,81]. When placing the proximal medial portal stay anterior of the medial intermuscular septum to keep the ulnar nerve posterior of the portal and avoid ulnar nerve injury[9,82]. A method to reduce neurovascular injury when placing the proximal medial portal is by using a blunt hemostat or clamp after the usual mini-incision of the skin and place it on the anterior aspect of the humerus and aim it at the coronoid. By sliding downward over the humerus the capsule will be reached with small chance of injuring the median nerve, medial antebrachial nerve or brachial artery[81]. When assessing the posterior compartment of the elbow avoid using the posteromedial portal as it brings risk for ulnar nerve injury; posterolateral and midposterior portal are good alternatives[81].
Use of instruments
Once safe entry to the joint has been established it is important to always keep your instrument tips within sight even under hard conditions and keep clear of using suction when working in the proximity of a nerve or the capsule to prevent within-out- injury[75]. Never use suction while shaving. Another way of preventing within-out injury is using a retractor, via a separate portal, to keep the capsule away from a debriding instrument[75]. This particularly applies to the posteromedial and the anterolateral compartment because of limited distance to the ulnar nerve and radial nerve respectively. Other advantages of using a retractor, aside from preventing within-out injury, are better visualization and exposure of the elbow joint. Lastly, to prevent a burr from getting entangled in the surrounding soft tissues and causing damage to an adjacent nerve hooded burrs are advised. Availability of different sizes of shavers during surgery is obligatory, so you can adjust the shaver size to the specific circumstances and avoid within-out-injury due to usage of a too large shaver.
All aforementioned recommendations are summarized in Table 1.
Table 1.
Recommendations in short
| Step | Phase | Recommendations |
| 1 | Work-up | Determine a valid indication. Identify possible complicating factors. If needed obtain additional imaging studies for careful planning of surgery Routinely report a subluxing or previously transposed ulnar nerve for all patients in the outpatient clinic setting previous of elbow arthroscopy Critical assessment of CT-studies to determine if osteophytes compress or mobilize the nerves (Figure 4) |
| 2 | Preoperative preventive measures | Examination under anesthesia (ROM) Marking of anatomic landmarks and portal sites (Figures 5 and 6) Palpation of the ulnar nerve course |
| 3 | Anesthesia | General anesthesia is recommended because of patient comfort and disabling unexpected patient movement |
| 4 | Patient positioning | Lateral decubitus position is recommended because of additional gravitational displacement of nerves away from the anterior capsule and easy access to all compartments (Figure 7) Use a bean bag for stable patient positioning |
| 5 | Joint insufflation | Increases nerve-to-portal distance by expanding the joint space en pushing the neurovascular structures away from the surgical field. Recognize that joint insufflation does not increase nerve-to-capsule distance (Figures 8 and 9) |
| 6 | Elbow positioning | Elbow flexion increases distension capacity of the joint and increases nerve-to-portal distance Supportive arm holders should not compress the flexion crease |
| 7 | Portal placement | Portals proximal to the joint tend to be safer Mini-incision of the skin only and the use of a blunt trocar or clamp prevents injury to the antebrachial nerves Pronation and flexion of the elbow protects the posterior interosseous nerve when placing lateral portals Avoid use of the posteromedial portal as the posterolateral and midposterior portals are good alternatives when inspecting the posterior compartment |
| 8 | Use of instruments | Always visualize the tip of the instrument Avoid suction when in the vicinity of a nerve or against the capsule Use a retractor to lift the capsule away from the debriding instrument, particularly in compartments at risk The use of hooded burrs instead of unhooded burrs is recommended as it help prevent the burr tangling up in the soft tissues No suction while shaving Availability of different shaver sizes during surgery |
DISCUSSION
Thorough knowledge of the anatomy of the elbow in health and various diseases, handling of arthroscopic instruments and number of performed elbow arthroscopies are of influence on one’s arthroscopic expertise[13,20,31,83,84]. There still is no consensus on the minimal number of elbow arthroscopies that has to be performed to become an experienced arthroscopist. However it is apparent that elbow arthroscopy has a long(er) learning curve. Savoie[20] states that a minimal number of 100 performed elbow arthroscopies is necessary to become an experienced elbow arthroscopist. After the first 15 arthroscopies Kim et al[84] observed a significant decrease in surgical time in elbow arthroscopy.
It is common sense that with more experience comes a decreased complication rate. This seems to be confirmed when comparing the study of Claessen et al[83] with the studies of Marti et al[31] and Elfeddali et al[28]. Claessen et al[83], observed a 30% complication rate in portal placement by novice surgeons whom were trained by a single didactic lecture and a single cadaveric training and found the complication rate significantly higher when compared to studies in current literature by experienced elbow arthroscopists. Marti et al[31] found 6 minor complications (5%) in a series of 100 elbow arthroscopies done by 1 fellowship trained surgeon with only previous cadaveric experience, however no correlation could be found between the complication rate and the learning curve. Elfeddali et al[28], found a 7.5% complication rate in 200 elbow arthroscopies over 8 years all performed by a single surgeon; due to the sample size it was not possible to detect any significant learning effect.
Following out of the aforementioned studies is that inexperienced surgeons are more likely to cause iatrogenic complications during elbow arthroscopy. A ”young” surgeon should undergo extensive training with as much hands-on exposure as possible, comprehending guidance by an experienced elbow arthroscopist, computer-simulated hands-on courses, pre-clinical hands-on cadaveric courses preferably yearly and in line with the current opinion of arthroscopy experts and Claessen et al[83] fellowship training.
In current literature the prevalence of neurologic injury after elbow arthroscopy, transient and permanent, is reported to range between 0% and 14%[8,13,14,32,34,42,45,63,85-88]. As stated by Desai et al[60] the reported prevalence is probably underreported. Possible causes of nerve injury underreporting after elbow arthroscopy are; the lack of a national registration for nerve injuries like there is for orthopedic implants, loss-to-follow-up due to the diagnosis and treatment of nerve injury by another specialty, and the possible reluctance or fear of the consequences when reporting iatrogenic nerve injury.
The goal of this editorial is to make one aware of the complications that can occur when performing elbow arthroscopy and more importantly stress the difficulty of performing elbow arthroscopy. The abovementioned instructions are to be a general guideline in order to help avoid complications during elbow arthroscopy. We believe a proper and thorough work-up and awareness of the possible severe complications throughout all steps of the procedure is the key for a successful elbow arthroscopy.
No matter the experience of an elbow arthroscopist, for every indication a surgeon should assess if he is capable to perform the procedure as a surgeon’s experience is directly related to the incidence of complications[20].
Footnotes
Conflict-of-interest statement: Hilgersom NFJ, Oh LS and Flipsen M have no conflicts of interest or financial ties to disclose. Eygendaal D has received travel expenses from the ESSKA board and fees for serving as a consultant for Lima Elbow System and as a speaker for the AO foundation. van den Bekerom MPJ has received an enabling grant from Smith and Nephew for research in rotator cuff surgery and research funding from Tornier.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: The Netherlands
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Peer-review started: September 18, 2016
First decision: October 21, 2016
Article in press: November 29, 2016
P- Reviewer: Ertem K, Guerado E, Ohishi T S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
References
- 1.Gallay SH, Richards RR, O’Driscoll SW. Intraarticular capacity and compliance of stiff and normal elbows. Arthroscopy. 1993;9:9–13. doi: 10.1016/s0749-8063(05)80336-6. [DOI] [PubMed] [Google Scholar]
- 2.Abboud JA, Ricchetti ET, Tjoumakaris F, Ramsey ML. Elbow arthroscopy: basic setup and portal placement. J Am Acad Orthop Surg. 2006;14:312–318. doi: 10.5435/00124635-200605000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Lynch GJ, Meyers JF, Whipple TL, Caspari RB. Neurovascular anatomy and elbow arthroscopy: inherent risks. Arthroscopy. 1986;2:190–197. doi: 10.1016/s0749-8063(86)80067-6. [DOI] [PubMed] [Google Scholar]
- 4.Marshall PD, Fairclough JA, Johnson SR, Evans EJ. Avoiding nerve damage during elbow arthroscopy. J Bone Joint Surg Br. 1993;75:129–131. doi: 10.1302/0301-620X.75B1.8421009. [DOI] [PubMed] [Google Scholar]
- 5.Miller CD, Jobe CM, Wright MH. Neuroanatomy in elbow arthroscopy. J Shoulder Elbow Surg. 1995;4:168–174. doi: 10.1016/s1058-2746(05)80047-3. [DOI] [PubMed] [Google Scholar]
- 6.Morrey BF. Arthroscopy of the elbow. Instr Course Lect. 1986;35:102–107. [PubMed] [Google Scholar]
- 7.Omid R, Hamid N, Keener JD, Galatz LM, Yamaguchi K. Relation of the radial nerve to the anterior capsule of the elbow: anatomy with correlation to arthroscopy. Arthroscopy. 2012;28:1800–1804. doi: 10.1016/j.arthro.2012.05.890. [DOI] [PubMed] [Google Scholar]
- 8.Small NC. Complications in arthroscopic surgery performed by experienced arthroscopists. Arthroscopy. 1988;4:215–221. doi: 10.1016/s0749-8063(88)80030-6. [DOI] [PubMed] [Google Scholar]
- 9.Stothers K, Day B, Regan WR. Arthroscopy of the elbow: anatomy, portal sites, and a description of the proximal lateral portal. Arthroscopy. 1995;11:449–457. doi: 10.1016/0749-8063(95)90200-7. [DOI] [PubMed] [Google Scholar]
- 10.Verhaar J, van Mameren H, Brandsma A. Risks of neurovascular injury in elbow arthroscopy: starting anteromedially or anterolaterally? Arthroscopy. 1991;7:287–290. doi: 10.1016/0749-8063(91)90129-l. [DOI] [PubMed] [Google Scholar]
- 11.Field LD, Altchek DW, Warren RF, O’Brien SJ, Skyhar MJ, Wickiewicz TL. Arthroscopic anatomy of the lateral elbow: a comparison of three portals. Arthroscopy. 1994;10:602–607. doi: 10.1016/s0749-8063(05)80055-6. [DOI] [PubMed] [Google Scholar]
- 12.Lindenfeld TN. Medial approach in elbow arthroscopy. Am J Sports Med. 1990;18:413–417. doi: 10.1177/036354659001800414. [DOI] [PubMed] [Google Scholar]
- 13.Kelly EW, Morrey BF, O’Driscoll SW. Complications of elbow arthroscopy. J Bone Joint Surg Am. 2001;83-A:25–34. doi: 10.2106/00004623-200101000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Kim SJ, Kim HK, Lee JW. Arthroscopy for limitation of motion of the elbow. Arthroscopy. 1995;11:680–683. doi: 10.1016/0749-8063(95)90109-4. [DOI] [PubMed] [Google Scholar]
- 15.Savoie FH, Nunley PD, Field LD. Arthroscopic management of the arthritic elbow: indications, technique, and results. J Shoulder Elbow Surg. 1999;8:214–219. doi: 10.1016/s1058-2746(99)90131-3. [DOI] [PubMed] [Google Scholar]
- 16.Kim SJ, Shin SJ. Arthroscopic treatment for limitation of motion of the elbow. Clin Orthop Relat Res. 2000;(375):140–148. doi: 10.1097/00003086-200006000-00017. [DOI] [PubMed] [Google Scholar]
- 17.Andrews JR, St Pierre RK, Carson WG. Arthroscopy of the elbow. Clin Sports Med. 1986;5:653–662. [PubMed] [Google Scholar]
- 18.Baker CL, Jones GL. Arthroscopy of the elbow. Am J Sports Med. 1999;27:251–264. doi: 10.1177/03635465990270022401. [DOI] [PubMed] [Google Scholar]
- 19.Dodson CC, Nho SJ, Williams RJ, Altchek DW. Elbow arthroscopy. J Am Acad Orthop Surg. 2008;16:574–585. doi: 10.5435/00124635-200810000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Savoie FH. Guidelines to becoming an expert elbow arthroscopist. Arthroscopy. 2007;23:1237–1240. doi: 10.1016/j.arthro.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 21.Adams JE, King GJ, Steinmann SP, Cohen MS. Elbow arthroscopy: indications, techniques, outcomes, and complications. Instr Course Lect. 2015;64:215–224. [PubMed] [Google Scholar]
- 22.Yeoh KM, King GJ, Faber KJ, Glazebrook MA, Athwal GS. Evidence-based indications for elbow arthroscopy. Arthroscopy. 2012;28:272–282. doi: 10.1016/j.arthro.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 23.Adams JE, Wolff LH, Merten SM, Steinmann SP. Osteoarthritis of the elbow: results of arthroscopic osteophyte resection and capsulectomy. J Shoulder Elbow Surg. 2008;17:126–131. doi: 10.1016/j.jse.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 24.Blonna D, Lee GC, O’Driscoll SW. Arthroscopic restoration of terminal elbow extension in high-level athletes. Am J Sports Med. 2010;38:2509–2515. doi: 10.1177/0363546510376727. [DOI] [PubMed] [Google Scholar]
- 25.Blonna D, Wolf JM, Fitzsimmons JS, O’Driscoll SW. Prevention of nerve injury during arthroscopic capsulectomy of the elbow utilizing a safety-driven strategy. J Bone Joint Surg Am. 2013;95:1373–1381. doi: 10.2106/JBJS.K.00972. [DOI] [PubMed] [Google Scholar]
- 26.Dolderer JH, Prandl EC, Kehrer A, Beham A, Schaller HE, Briggs C, Kelly JL. Solitary paralysis of the flexor pollicis longus muscle after minimally invasive elbow procedures: anatomical and clinical study of the anterior interosseous nerve. Plast Reconstr Surg. 2011;127:1229–1236. doi: 10.1097/PRS.0b013e3182043ac0. [DOI] [PubMed] [Google Scholar]
- 27.El Hajj F, Hoteit M, Ouaknine M. Elbow arthroscopy: An alternative to anteromedial portals. Orthop Traumatol Surg Res. 2015;101:411–414. doi: 10.1016/j.otsr.2015.03.011. [DOI] [PubMed] [Google Scholar]
- 28.Elfeddali R, Schreuder MH, Eygendaal D. Arthroscopic elbow surgery, is it safe? J Shoulder Elbow Surg. 2013;22:647–652. doi: 10.1016/j.jse.2013.01.032. [DOI] [PubMed] [Google Scholar]
- 29.Lattermann C, Romeo AA, Anbari A, Meininger AK, McCarty LP, Cole BJ, Cohen MS. Arthroscopic debridement of the extensor carpi radialis brevis for recalcitrant lateral epicondylitis. J Shoulder Elbow Surg. 2010;19:651–656. doi: 10.1016/j.jse.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 30.Lee BP, Morrey BF. Arthroscopic synovectomy of the elbow for rheumatoid arthritis. A prospective study. J Bone Joint Surg Br. 1997;79:770–772. doi: 10.1302/0301-620x.79b5.7466. [DOI] [PubMed] [Google Scholar]
- 31.Marti D, Spross C, Jost B. The first 100 elbow arthroscopies of one surgeon: analysis of complications. J Shoulder Elbow Surg. 2013;22:567–573. doi: 10.1016/j.jse.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 32.Nelson GN, Wu T, Galatz LM, Yamaguchi K, Keener JD. Elbow arthroscopy: early complications and associated risk factors. J Shoulder Elbow Surg. 2014;23:273–278. doi: 10.1016/j.jse.2013.09.026. [DOI] [PubMed] [Google Scholar]
- 33.Nguyen D, Proper SI, MacDermid JC, King GJ, Faber KJ. Functional outcomes of arthroscopic capsular release of the elbow. Arthroscopy. 2006;22:842–849. doi: 10.1016/j.arthro.2006.04.100. [DOI] [PubMed] [Google Scholar]
- 34.O'Driscoll SW, Morrey BF. Arthroscopy of the elbow. Diagnostic and therapeutic benefits and hazards. J Bone Joint Surg Am. 1992;74:84–94. [PubMed] [Google Scholar]
- 35.Papilion JD, Neff RS, Shall LM. Compression neuropathy of the radial nerve as a complication of elbow arthroscopy: a case report and review of the literature. Arthroscopy. 1988;4:284–286. doi: 10.1016/s0749-8063(88)80046-x. [DOI] [PubMed] [Google Scholar]
- 36.Park JY, Cho CH, Choi JH, Lee ST, Kang CH. Radial nerve palsy after arthroscopic anterior capsular release for degenerative elbow contracture. Arthroscopy. 2007;23:1360.e1–1360.e3. doi: 10.1016/j.arthro.2006.11.021. [DOI] [PubMed] [Google Scholar]
- 37.Pederzini LA, Nicoletta F, Tosi M, Prandini M, Tripoli E, Cossio A. Elbow arthroscopy in stiff elbow. Knee Surg Sports Traumatol Arthrosc. 2014;22:467–473. doi: 10.1007/s00167-013-2424-0. [DOI] [PubMed] [Google Scholar]
- 38.Rosenberg BM, Loebenberg MI. Elbow arthroscopy. Bull NYU Hosp Jt Dis. 2007;65:43–50. [PubMed] [Google Scholar]
- 39.Schubert T, Dubuc JE, Barbier O. A review of 24 cases of elbow arthroscopy using the DASH questionnaire. Acta Orthop Belg. 2007;73:700–703. [PubMed] [Google Scholar]
- 40.Tanaka N, Sakahashi H, Hirose K, Ishima T, Ishii S. Arthroscopic and open synovectomy of the elbow in rheumatoid arthritis. J Bone Joint Surg Am. 2006;88:521–525. doi: 10.2106/JBJS.E.00472. [DOI] [PubMed] [Google Scholar]
- 41.Thomas MA, Fast A, Shapiro D. Radial nerve damage as a complication of elbow arthroscopy. Clin Orthop Relat Res. 1987:130–131. [PubMed] [Google Scholar]
- 42.Vavken P, Müller AM, Camathias C. First 50 Pediatric and Adolescent Elbow Arthroscopies: Analysis of Indications and Complications. J Pediatr Orthop. 2016;36:400–404. doi: 10.1097/BPO.0000000000000461. [DOI] [PubMed] [Google Scholar]
- 43.Wu X, Wang H, Meng C, Yang S, Duan D, Xu W, Liu X, Tang M, Zhao J. Outcomes of arthroscopic arthrolysis for the post-traumatic elbow stiffness. Knee Surg Sports Traumatol Arthrosc. 2015;23:2715–2720. doi: 10.1007/s00167-014-3032-3. [DOI] [PubMed] [Google Scholar]
- 44.Somanchi BV, Funk L. Evaluation of functional outcome and patient satisfaction after arthroscopic elbow arthrolysis. Acta Orthop Belg. 2008;74:17–23. [PubMed] [Google Scholar]
- 45.Andrews JR, Carson WG. Arthroscopy of the elbow. Arthroscopy. 1985;1:97–107. doi: 10.1016/s0749-8063(85)80038-4. [DOI] [PubMed] [Google Scholar]
- 46.Carofino BC, Bishop AT, Spinner RJ, Shin AY. Nerve injuries resulting from arthroscopic treatment of lateral epicondylitis: report of 2 cases. J Hand Surg Am. 2012;37:1208–1210. doi: 10.1016/j.jhsa.2012.01.038. [DOI] [PubMed] [Google Scholar]
- 47.Murphy RK, Ray WZ, Mackinnon SE. Repair of a median nerve transection injury using multiple nerve transfers, with long-term functional recovery. J Neurosurg. 2012;117:886–889. doi: 10.3171/2012.8.JNS111356. [DOI] [PubMed] [Google Scholar]
- 48.Gay DM, Raphael BS, Weiland AJ. Revision arthroscopic contracture release in the elbow resulting in an ulnar nerve transection: a case report. J Bone Joint Surg Am. 2010;92:1246–1249. doi: 10.2106/JBJS.I.00555. [DOI] [PubMed] [Google Scholar]
- 49.Dumonski ML, Arciero RA, Mazzocca AD. Ulnar nerve palsy after elbow arthroscopy. Arthroscopy. 2006;22:577.e1–577.e3. doi: 10.1016/j.arthro.2005.12.049. [DOI] [PubMed] [Google Scholar]
- 50.Gupta A, Sunil Tm Tm. Complete division of the posterior interosseous nerve after elbow arthroscopy: a case report. J Shoulder Elbow Surg. 2004;13:566–567. doi: 10.1016/j.jse.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 51.Reddy AS, Kvitne RS, Yocum LA, Elattrache NS, Glousman RE, Jobe FW. Arthroscopy of the elbow: a long-term clinical review. Arthroscopy. 2000;16:588–594. doi: 10.1053/jars.2000.8953. [DOI] [PubMed] [Google Scholar]
- 52.Haapaniemi T, Berggren M, Adolfsson L. Complete transection of the median and radial nerves during arthroscopic release of post-traumatic elbow contracture. Arthroscopy. 1999;15:784–787. doi: 10.1016/s0749-8063(99)70015-0. [DOI] [PubMed] [Google Scholar]
- 53.Hahn M, Grossman JA. Ulnar nerve laceration as a result of elbow arthroscopy. J Hand Surg Br. 1998;23:109. doi: 10.1016/s0266-7681(98)80236-2. [DOI] [PubMed] [Google Scholar]
- 54.Ruch DS, Poehling GG. Anterior interosseus nerve injury following elbow arthroscopy. Arthroscopy. 1997;13:756–758. doi: 10.1016/s0749-8063(97)90014-1. [DOI] [PubMed] [Google Scholar]
- 55.Jones GS, Savoie FH. Arthroscopic capsular release of flexion contractures (arthrofibrosis) of the elbow. Arthroscopy. 1993;9:277–283. doi: 10.1016/s0749-8063(05)80422-0. [DOI] [PubMed] [Google Scholar]
- 56.Cefo I, Eygendaal D. Arthroscopic arthrolysis for posttraumatic elbow stiffness. J Shoulder Elbow Surg. 2011;20:434–439. doi: 10.1016/j.jse.2010.11.018. [DOI] [PubMed] [Google Scholar]
- 57.Grewal R, MacDermid JC, Shah P, King GJ. Functional outcome of arthroscopic extensor carpi radialis brevis tendon release in chronic lateral epicondylitis. J Hand Surg Am. 2009;34:849–857. doi: 10.1016/j.jhsa.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 58.Krishnan SG, Harkins DC, Pennington SD, Harrison DK, Burkhead WZ. Arthroscopic ulnohumeral arthroplasty for degenerative arthritis of the elbow in patients under fifty years of age. J Shoulder Elbow Surg. 2007;16:443–448. doi: 10.1016/j.jse.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 59.McLaughlin RE, Savoie FH, Field LD, Ramsey JR. Arthroscopic treatment of the arthritic elbow due to primary radiocapitellar arthritis. Arthroscopy. 2006;22:63–69. doi: 10.1016/j.arthro.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 60.Desai MJ, Mithani SK, Lodha SJ, Richard MJ, Leversedge FJ, Ruch DS. Major Peripheral Nerve Injuries After Elbow Arthroscopy. Arthroscopy. 2016;32:999–1002.e8. doi: 10.1016/j.arthro.2015.11.023. [DOI] [PubMed] [Google Scholar]
- 61.Blonna D, Bellato E, Marini E, Scelsi M, Castoldi F. Arthroscopic treatment of stiff elbow. ISRN Surg. 2011;2011:378135. doi: 10.5402/2011/378135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dwyer T, Henry PD, Cholvisudhi P, Chan VW, Theodoropoulos JS, Brull R. Neurological Complications Related to Elective Orthopedic Surgery: Part 1: Common Shoulder and Elbow Procedures. Reg Anesth Pain Med. 2015;40:431–442. doi: 10.1097/AAP.0000000000000178. [DOI] [PubMed] [Google Scholar]
- 63.Schneider T, Hoffstetter I, Fink B, Jerosch J. Long-term results of elbow arthroscopy in 67 patients. Acta Orthop Belg. 1994;60:378–383. [PubMed] [Google Scholar]
- 64.Childress HM. Recurrent ulnar-nerve dislocation at the elbow. Clin Orthop Relat Res. 1975;(108):168–173. doi: 10.1097/00003086-197505000-00027. [DOI] [PubMed] [Google Scholar]
- 65.Van Den Berg PJ, Pompe SM, Beekman R, Visser LH. Sonographic incidence of ulnar nerve (sub)luxation and its associated clinical and electrodiagnostic characteristics. Muscle Nerve. 2013;47:849–855. doi: 10.1002/mus.23715. [DOI] [PubMed] [Google Scholar]
- 66.Sahajpal DT, Blonna D, O’Driscoll SW. Anteromedial elbow arthroscopy portals in patients with prior ulnar nerve transposition or subluxation. Arthroscopy. 2010;26:1045–1052. doi: 10.1016/j.arthro.2009.12.029. [DOI] [PubMed] [Google Scholar]
- 67.Wada T, Yamauchi M, Oki G, Sonoda T, Yamakage M, Yamashita T. Efficacy of axillary nerve block in elbow arthroscopic surgery: a randomized trial. J Shoulder Elbow Surg. 2014;23:291–296. doi: 10.1016/j.jse.2013.11.022. [DOI] [PubMed] [Google Scholar]
- 68.Auroy Y, Benhamou D, Bargues L, Ecoffey C, Falissard B, Mercier FJ, Bouaziz H, Samii K. Major complications of regional anesthesia in France: The SOS Regional Anesthesia Hotline Service. Anesthesiology. 2002;97:1274–1280. doi: 10.1097/00000542-200211000-00034. [DOI] [PubMed] [Google Scholar]
- 69.Auroy Y, Narchi P, Messiah A, Litt L, Rouvier B, Samii K. Serious complications related to regional anesthesia: results of a prospective survey in France. Anesthesiology. 1997;87:479–486. doi: 10.1097/00000542-199709000-00005. [DOI] [PubMed] [Google Scholar]
- 70.Brull R, McCartney CJ, Chan VW, El-Beheiry H. Neurological complications after regional anesthesia: contemporary estimates of risk. Anesth Analg. 2007;104:965–974. doi: 10.1213/01.ane.0000258740.17193.ec. [DOI] [PubMed] [Google Scholar]
- 71.Adams JE, Steinmann SP. Nerve injuries about the elbow. J Hand Surg Am. 2006;31:303–313. doi: 10.1016/j.jhsa.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 72.Hackl M, Lappen S, Burkhart KJ, Leschinger T, Scaal M, Müller LP, Wegmann K. Elbow Positioning and Joint Insufflation Substantially Influence Median and Radial Nerve Locations. Clin Orthop Relat Res. 2015;473:3627–3634. doi: 10.1007/s11999-015-4442-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Adolfsson L. Arthroscopy of the elbow joint: A cadaveric study of portal placement. J Shoulder Elbow Surg. 1994;3:53–61. doi: 10.1016/S1058-2746(09)80110-9. [DOI] [PubMed] [Google Scholar]
- 74.Baker CL, Brooks AA. Arthroscopy of the elbow. Clin Sports Med. 1996;15:261–281. [PubMed] [Google Scholar]
- 75.Morrey BF. Complications of elbow arthroscopy. Instr Course Lect. 2000;49:255–258. [PubMed] [Google Scholar]
- 76.O'Driscoll SW, Morrey BF, An KN. Intraarticular pressure and capacity of the elbow. Arthroscopy. 1990;6:100–103. doi: 10.1016/0749-8063(90)90007-z. [DOI] [PubMed] [Google Scholar]
- 77.Ogilvie-Harris DJ, Weisleder L. Fluid pump systems for arthroscopy: a comparison of pressure control versus pressure and flow control. Arthroscopy. 1995;11:591–595. doi: 10.1016/0749-8063(95)90137-x. [DOI] [PubMed] [Google Scholar]
- 78.Unlu MC, Kesmezacar H, Akgun I, Ogut T, Uzun I. Anatomic relationship between elbow arthroscopy portals and neurovascular structures in different elbow and forearm positions. J Shoulder Elbow Surg. 2006;15:457–462. doi: 10.1016/j.jse.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 79.Nowicki KD, Shall LM. Arthroscopic release of a posttraumatic flexion contracture in the elbow: a case report and review of the literature. Arthroscopy. 1992;8:544–547. doi: 10.1016/0749-8063(92)90024-6. [DOI] [PubMed] [Google Scholar]
- 80.Diliberti T, Botte MJ, Abrams RA. Anatomical considerations regarding the posterior interosseous nerve during posterolateral approaches to the proximal part of the radius. J Bone Joint Surg Am. 2000;82:809–813. doi: 10.2106/00004623-200006000-00007. [DOI] [PubMed] [Google Scholar]
- 81.Raphael BS, Weiland AJ, Altchek DW, Gay DM. Revision arthroscopic contracture release in the elbow resulting in an ulnar nerve transection: surgical technique. J Bone Joint Surg Am. 2011;93 Suppl 1:100–108. doi: 10.2106/JBJS.J.01272. [DOI] [PubMed] [Google Scholar]
- 82.O'Holleran JD, Altchek DW. The thrower’s elbow: arthroscopic treatment of valgus extension overload syndrome. HSS J. 2006;2:83–93. doi: 10.1007/s11420-005-5124-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Claessen FM, Kachooei AR, Kolovich GP, Buijze GA, Oh LS, van den Bekerom MP, Doornberg JN. Portal placement in elbow arthroscopy by novice surgeons: cadaver study. Knee Surg Sports Traumatol Arthrosc. 2016 doi: 10.1007/s00167-016-4186-y. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 84.Kim SJ, Moon HK, Chun YM, Chang JH. Arthroscopic treatment for limitation of motion of the elbow: the learning curve. Knee Surg Sports Traumatol Arthrosc. 2011;19:1013–1018. doi: 10.1007/s00167-010-1334-7. [DOI] [PubMed] [Google Scholar]
- 85.Guhl JF. Arthroscopy and arthroscopic surgery of the elbow. Orthopedics. 1985;8:1290–1296. doi: 10.3928/0147-7447-19851001-17. [DOI] [PubMed] [Google Scholar]
- 86.Rodeo SA, Forster RA, Weiland AJ. Neurological complications due to arthroscopy. J Bone Joint Surg Am. 1993;75:917–926. doi: 10.2106/00004623-199306000-00015. [DOI] [PubMed] [Google Scholar]
- 87.Savoie FH, 3rd . New York: Churchill Livingstone; 1996. Complications. Arthroscopy of the elbow; pp. 151–156. [Google Scholar]
- 88.Ward WG, Anderson TE. Elbow arthroscopy in a mostly athletic population. J Hand Surg Am. 1993;18:220–224. doi: 10.1016/0363-5023(93)90350-C. [DOI] [PubMed] [Google Scholar]


