Abstract
Measurement of wrist range of motion (ROM) is often considered to be an essential component of wrist physical examination. The measurement can be carried out through various instruments such as goniometers and inclinometers. Recent smartphones have been equipped with accelerometers and magnetometers, which, through specific software applications (apps) can be used for goniometric functions. This study, for the first time, aimed to evaluate the reliability and concurrent validity of a new smartphone goniometric app (Goniometer Pro©) for measuring active wrist ROM. In all, 120 wrists of 70 asymptomatic adults (38 men and 32 women; aged 18–40 years) were assessed in a physiotherapy clinic located at the School of Rehabilitation Sciences, Iran University of Medical Science and Health Services, Tehran, Iran. Following the recruitment process, active wrist ROM was measured using a universal goniometer and iPhone® 5 app. Two blinded examiners each utilized the universal goniometer and iPhone® to measure active wrist ROM using a volar/dorsal alignment technique in the following sequences: flexion, extension, radial deviation, and ulnar deviation. The second (2 h later) and third (48 h later) sessions were carried out in the same manner as the first session. All the measurements were conducted three times and the mean value of three repetitions for each measurement was used for analysis. Intraclass correlation coefficient (ICC) models (3, k) and (2, k) were used to determine the intra‐rater and inter‐rater reliability, respectively. The Pearson correlation coefficients were used to establish concurrent validity of the iPhone® app. Good to excellent intra‐rater and inter‐rater reliability was demonstrated for the goniometer with ICC values of ≥ 0.82 and ≥ 0.73 and the iPhone® app with ICC values of ≥ 0.83 and ≥ 0.79, respectively. Minimum detectable change at the 95% confidence level (MDC 95) was computed as 1.96 × standard error of measurement × √2. The MDC 95 ranged from 1.66° to 5.35° for the intra‐rater analysis and from 1.97° to 6.15° for the inter‐rater analysis. The concurrent validity between the two instruments was high, with r values of ≥ 0.80. From the results of this cross‐sectional study, it can be concluded that the iPhone® app possesses good to excellent intra‐rater and inter‐rater reliability and concurrent validity. It seems that this app can be used for the measurement of wrist ROM. However, further research is needed to evaluate symptomatic subjects using this app.
Keywords: arthrometry, articular; range of motion, articular; smartphone; wrist joint
Introduction
Normal wrist range of motion (ROM) is always required for daily activities and many sports activities. The hand and wrist are the most active part of the upper extremity; thus, they are susceptible to injury, which can lead to ROM limitations and great functional problems (Magee, 2014). In addition, various pathologies such as autoimmune diseases, neurological diseases, soft tissue diseases, and degenerative joint disease (DJD) can greatly impede normal wrist ROM (Horger, 1990; Cauraugh et al. 2000; Dziedzic & Hammond, 2010; Squeri et al. 2014; Tonga et al. 2015; Bain et al. 2016). Therefore, measurement of wrist ROM with a valid and reliable instrument can help clinicians determine the amount of limitation, monitor the effectiveness of the rehabilitation process, and improve effective communication between them (Carter et al. 2009). The method or instrument a clinician uses to measure wrist ROM may vary and is dependent upon biomedical criteria such as accessibility of the instrument, easy administration, cost, familiarity, insusceptibility or insensitivity to external influences, safety, and educational background (Chaffin et al. 2006; Kolber et al. 2013).
The goniometers are widely used in clinical practice and goniometric measurement can be considered a reference standard (Ellis et al. 1997; Norkin & White, 2009; McVeigh et al. 2016; Pourahmadi et al. 2016a). It has been shown that goniometry is the most objective reliable method available for clinicians to assess a joint ROM (Ellis & Bruton, 1998; Fess, 1998; Bruton et al. 1999). To date, several studies have looked at the reliability of goniometric measurement of wrist ROM. These studies reported high overall intra‐rater and inter‐rater reliability for measuring wrist joint ROM (Bovens et al. 1990; Horger, 1990; LaStayo & Wheeler, 1994). According to the American Society of Hand Therapists (ASHT), five variables can directly affect the reliability of goniometric ROM measurements: the size and design of goniometer, goniometer placement, the amount of force applied by the clinician, method of documentation, and the type of ROM being measured (Adams et al. 1992).
The number of smartphone users has increased markedly in recent years, and it has been estimated that this number will rise to 2.5 billion people by 2017 (Faurholt‐Jepsen et al. 2016). More and more people spend time using smartphone and numerous software programs/applications (apps) have been developed for a variety of purposes in orthopaedic medicine. Nowadays, smartphones are equipped with a set of cheap but powerful embedded sensors, such as accelerometers, magnetometers, and gyroscopes that make the phone capable of detecting joint position and measuring joint ROM (Otter et al. 2015). A wide range of clinical measurement apps can be downloaded freely or for little cost from the internet (Shin et al. 2012; Kolber et al. 2013; Milanese et al. 2014; Salamh & Kolber, 2014; Pourahmadi et al. 2016b). The purpose of these apps is to provide easy, quick and simple ROM measurement.
The use of smartphone apps for clinical assessment is gaining popularity and many studies have evaluated the reliability and validity of smartphone apps for the measurements of the ROM of many joints (Shin et al. 2012; Kolber et al. 2013; Milanese et al. 2014; Quek et al. 2014; Salamh & Kolber, 2014; Werner et al. 2014; Charlton et al. 2015; Otter et al. 2015; Vohralik et al. 2015; Behnoush et al. 2016; Cuesta‐Vargas & Roldán‐Jiménez, 2016; Guidetti et al. 2016; Pourahmadi et al. 2016b). Generally, good to excellent intra‐rater and inter‐rater reliability have been reported in the previous studies. Although overall reliability of the apps has been shown to be good to excellent, the reliability varies according to the joint and the ROM being measured. As far as the authors know, in only one study has wrist ROM been measured using a smartphone app (Gyroscope) and a universal goniometer (Kim et al. 2014). The result of that study indicated that there was no statistically significant difference between the mean values of the iPhone® and universal goniometer (Kim et al. 2014). However, to the best of the present authors’ knowledge, no study has investigated the reliability and validity of smartphone apps for the measurements of wrist ROM. This study, for the first time, evaluated the reliability and validity of a new iPhone® app (G‐pro©) for measuring wrist ROM. The main purposes of the study were as follows:
To determine the reproducibility [between‐day (intra‐rater) and within‐day (intra‐rater and inter‐rate)] reliability] of a new iPhone® app [Goniometer Pro© (G‐pro©)] and universal goniometer for measuring active wrist ROM.
To determine the concurrent validity of the G‐pro©, using the universal goniometer as the reference standard.
We hypothesised that there would be agreement between repeated measures of wrist ROM when using the universal goniometer and G‐pro©, and that the inter‐rater and intra‐rater reliability of these two instruments would be high. In addition, we hypothesised that the G‐pro© is a valid and reliable app to measure wrist ROM.
Materials and methods
Study design
This cross‐sectional observational study was carried out between October 2015 and April 2016 (~ 28 weeks) in Tehran, Iran. The le\vel of evidence of this investigation was level IIb. Approval for the study was obtained from the Ethics Committee at Iran University of Medical Science and Health Services (Tehran‐Iran).
Subjects
In all, 120 wrist joints were measured in a sample of 70 healthy (asymptomatic) adult subjects (male = 38, female = 32). The subjects ranged in age from 18 to 40 years, with a mean of 27.50 years. Both wrists were assessed, except in subjects in which one of the two wrists was impaired. Inclusion criteria of the study were: (i) age ≥ 18 years, (ii) no history of wrist, forearm, elbow fracture, (iii) no surgical implants in the upper extremity, (iv) no obvious deformity of the upper extremity, (v) no pathologies affecting wrist, elbow, or shoulder joints (e.g. carpal tunnel syndrome, rheumatoid arthritis (RA), neurological diseases, soft tissue diseases, tendon tears, diabetes, and DJD), (vi) no pain during data acquisition time, (vii) no pregnancy, and (viii) ability to provide written informed consent. All the subjects were identified and recruited by posters, emails and word of mouth from the university and the surrounding community. A written informed consent was obtained from all subjects before participation. Subjects’ baseline demographic characteristics are presented in Table 1.
Table 1.
Subjects’ baseline demographic characteristics
| Asymptomatic subjects | n | Age (years) | Body mass (kg) | Height (cm) | BMI (kg m−2) |
|---|---|---|---|---|---|
| Male | 38 (54%) | 26.65 ± 5.44 | 74.44 ± 9.18 | 173.56 ± 8.63 | 21.91 ± 3.37 |
| Female | 32 (46%) | 28.62 ± 5.87 | 62.36 ± 7.65 | 166.21 ± 5.82 | 23.04 ± 2.28 |
| Total | 70 (100%) | 27.50 ± 6.89 | 68.40 ± 10.64 | 169.89 ± 8.17 | 25.20 ± 2.03 |
BMI, body mass index.
All values are presented as mean ± standard deviation.
Examiners
All goniometric measurements were performed by two independent blinded examiners (M.R.P. and M.B.) and wrist ROM was read directly from the instruments by a third person (M.T.). The examiners of the study were two PhD candidates in physiotherapy (M.R.P. and M.T.) and a bachelor of physiotherapy (M.B.). The clinical experience of the three examiners ranged from 4 to 12 years, with a mean of 8 years. Furthermore, all the three examiners had experience in the use of universal goniometer for measuring ROM. However, none of the examiners had any experience using the G‐pro© app.
Instrumentation
Active wrist ROM was measured using a plastic universal two‐arm goniometer with 360° goniometer face, and 35 cm (about 13.78 inch) movable arms. The universal goniometer used in the current study was accurate to within 1° (Fig. 1). In addition, an iPhone® model 5 (iPhone® is a trademark of Apple Inc., Cupertino, CA, USA) with the G‐pro© app (free version; downloaded from Apple's App Store; https://itunes.apple.com/us/app/goniometer-pro/id646925503?mt=8) was used to measure wrist ROM. The G‐pro© is a new app developed for smartphones and iPad/computer tablets. It works like a digital gravity‐based inclinometer and calculates the angle between two adjacent segments. The current app utilizes the iPhone's built‐in accelerometer sensor and a digital display to show the measured angle (Fig. 2). The precision of the G‐pro© app has been reported between 0.2° and 0.3° [Goniometer Pro (Internet), 2015]. Prior to the measurements, all covers were removed from the iPhone® 5.
Figure 1.
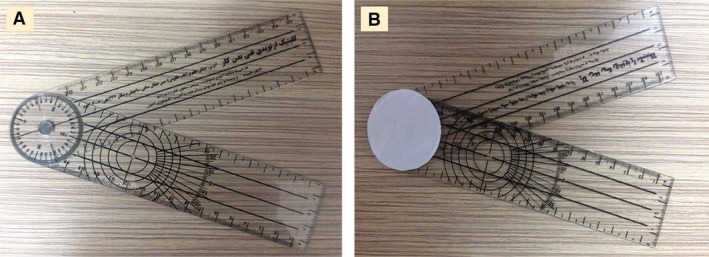
(A) Testing universal goniometer. (B) One surface of the universal goniometer face was blinded to the examiners and the numerical side was visible to the recorder.
Figure 2.

(A) iPhone® model 5 with screen showing the G‐pro© app. (B) Definition of each item on the app (from https://itunes.apple.com/us/app/goniometer-pro/id646925503?mt=8).
Procedure
Following the recruitment process, the subjects were brought to a physiotherapy clinic at the School of Rehabilitation Sciences (Iran University of Medical Sciences and Health Services). The subjects were asked to sit in their usual posture on a metal stool and their shoulders were positioned in 90° abduction and neutral rotation, the elbows in 90° flexion, and the forearms were placed on a supporting surface next to the subjects and were positioned in 0° supination‐pronation (Fig. 3). The wrist joints were positioned in neutral (0°) flexion–extension and radial–ulnar deviation. To ensure that the wrist joints were in neutral, the long axes of the third metacarpal and the radius were checked visually to fall in a straight line. This testing position was maintained in all experimental sessions. According to LaStayo & Wheeler (1994), the volar/dorsal alignment technique is the best goniometric technique for measuring wrist flexion and extension ROM. Hence, the volar/dorsal alignment technique was used in this study. First, the physiotherapist (examiner A: M.R.P.) palpated the wrist to find the joint line and placed the axis of the universal goniometer over the joint line on the dorsal side of the wrist. Then, the proximal arm (stationary arm) of the universal goniometer was placed on the dorsal midline of the forearm and the distal arm (movable arm) was positioned on the dorsal midline of the third metacarpal bone. One surface of the universal goniometer face was covered with a white sheet of paper so that the figures could not be seen from the examiner side. After goniometric placement, the physiotherapist asked the subject to perform maximum wrist flexion. Verbal cues (feedbacks) were also provided by the physiotherapist to encourage the subjects to make their maximum effort in order to reach the end of the available range. The same method was repeated for measuring wrist extension ROM; however, the universal goniometer was placed on the volar side of the wrist. The physiotherapist placed the stationary arm of the universal goniometer on the volar midline of the forearm and the movable arm was positioned on the volar midline of the third metacarpal bone. To evaluate wrist radial and ulnar deviation, the method of placement was the same as that described for measuring wrist flexion ROM (dorsal alignment technique). The physiotherapist then asked the subject to move the hand in the direction of the thumb (for radial deviation) and little finger (for ulnar deviation), as far as possible (Fig. 4). All the measured angles were documented by a third person (recorder: M.T.). The movements were measured in the following sequences: flexion, extension, radial deviation, and ulnar deviation. Randomization in measurements was not used because the purpose of the study was to investigate reproducibility, which requires a consistent physiological status (Kolber et al. 2013; Salamh & Kolber, 2014). All the universal goniometer measurements were repeated by the second physiotherapist (examiner B: M.B.).
Figure 3.

Testing position of subjects.
Figure 4.
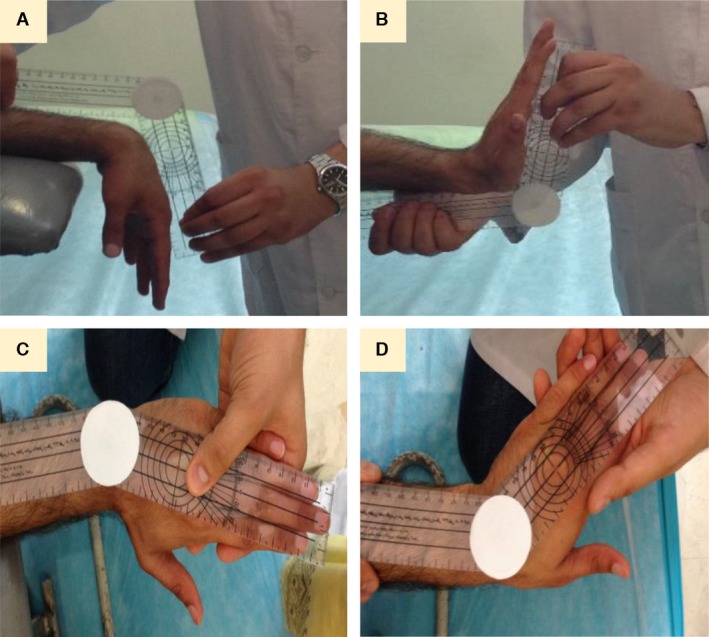
Measurement of active wrist ROM by use of the universal goniometer. (A) Wrist flexion, (B) wrist extension, (C) wrist radial deviation, (D) wrist ulnar deviation.
The ROM of the wrist joint was also evaluated using the G‐pro© app on the iPhone® 5. The examiners activated the G‐pro© app and pressed the ‘device axis’ button to adjust the axis according to the test condition. The back of the iPhone® 5 was fixated with an elastic band on the dorsal side of the hand and one bottom corner of the iPhone® 5 was placed on the centre of the extensor pollicis longus border of anatomical snuff box. The elastic band also covered the digital display to prevent the examiners from viewing the angles measured (Fig. 5). This method of placement was used for measuring wrist flexion and radial/ulnar deviation ROM. To measure wrist extension ROM, the back of the iPhone® 5 was placed on the volar side of the hand near the wrist joint line. The examiners asked the subject to move the wrist to the maximum available ROM. When the examiner was satisfied that measurement was complete, they tapped on the iPhone® screen to record and store the angles. The recorder then documented the measured angles from the device screen, before clearing them from the iPhone®. The sequence of wrist ROM measurement using the G‐pro© app was the same as that listed for the universal goniometer and no randomization was performed.
Figure 5.

Measurement of active wrist ROM using the G‐pro© app. (A) Wrist flexion, (B) wrist extension, (C) wrist radial deviation, (D) wrist ulnar deviation.
The procedure was repeated in the same manner after 2 and 48 h. All the measurements were carried out three times by the two examiners and the mean value of three repetitions from each measurement was used for statistical analysis.
Statistical analysis
All statistical analyses were performed on a personal laptop using Statistical Package for the Social Sciences (SPSS for Windows, Release version 21.0, SPSS Inc., Chicago, IL, USA). Prior to the statistical analyses, the Kolmogorov–Smirnov (K–S) test was used to check for normality of data. All probability values (P‐values) were set at significance levels of 0.05. Descriptive data are reported as mean angles ± standard deviations (SD) calculated for each series of measurements (Table 2). The reliability of all measurements was tested using the ICC model (3, k) for the intra‐rater analysis and the ICC model (2, k) for the inter‐rater analysis. For the intra‐rater reliability and concurrent validity, examiner A (M.R.P.) was the only rater of interest. Model (2, k) was used to assess whether the instrument of choice (universal goniometer, iPhone® app) can be utilized with reliability and confidence by experienced clinicians (Kolber et al. 2013; Salamh & Kolber, 2014). Using SPSS software, the ICC model (2, k) was computed by selecting the options 2‐way random, average measure, and absolute agreement, and the ICC model (3, k) the options 2‐way mixed and average measure.
Table 2.
Descriptive statistics for universal goniometer and iPhone® app values
| Instrument | Rater | Mean flexion ROM ± SD (minimum angle, maximum angle) | Mean extension ROM ± SD (minimum angle, maximum angle) | Mean radial deviation ROM ± SD (minimum angle, maximum angle) | Mean ulnar deviation ROM ± SD (minimum angle, maximum angle) |
|---|---|---|---|---|---|
| Universal goniometer | Rater A | 73.57° ± 4.53° (63.53°–82.33°) | 67.98° ± 4.25° (60.39°–75.68°) | 18.56° ± 1.66° (14.82°–22.54°) | 31.29° ± 3.28° (25.91°–38.64°) |
| Rater B | 72.57° ± 3.91° (59.21°–78.52°) | 65.36° ± 3.83° (61.19°–73.41°) | 17.67° ± 1.50° (13.98°–21.53°) | 29.90° ± 3.32° (23.66°–37.78°) | |
| iPhone® app | Rater A | 74.51° ± 4.68° (62.56°–84.20°) | 68.56° ± 3.27° (63.25°–78.32°) | 19.11° ± 2.56° (13.55°–24.09°) | 32.27° ± 3.72° (27.40°–39.33°) |
| Rater B | 77.12° ± 5.01° (56.19°–83.98°) | 64.33° ± 4.39° (57.53°–80.49°) | 16.91° ± 2.21° (11.79°–22.48°) | 32.19° ± 4.12° (25.72°–41.64°) |
ROM, range of motion; SD, standard deviation.
The scale from Bland & Altman (1999) was used in the classification of the reliability values (≤ 0.20 poor, 0.21–0.40 fair, 0.41–0.60 moderate, 0.61–0.80 good, and 0.81–1.00 excellent). Standard error of measurement (SEM) was employed to examine the precision of the instruments and was calculated as follows: . One SEM and 2 SEMs were calculated from the ICC models (2, k) and (3, k) used in this study. One SEM shows that the clinician may be 68% certain that the true measurement value lies within ± 1 SEM of measurement from the clinical measurement, and 2 SEMs provide the clinician with a value with 95% confidence (McKenna et al. 2004). Furthermore, minimum detectable change at the 95% confidence level (MDC95) was computed as √2 × 1.96 × SEM, which represents the magnitude of change necessary to provide confidence that a change is not be the result of random variation or measurement error (Haley & Fragala‐Pinkham, 2006).
The concurrent validity which determines the instrument performance was assessed between the universal goniometer and iPhone® app using the Pearson correlation coefficient (r). The Pearson correlation coefficient can vary between −1 and +1. A value of 0 indicates that there is no linear correlation between the two continuous variables. A value > 0 indicates a positive correlation; that is, as one variable increases, the other variable also increases (direct relationship). A value < 0 indicates a negative correlation; that is, as one variable increases, the other variable decreases (inverse relationship) (Ling et al. 2009). The values of the correlation coefficient were classified according to Hopkins’ extension of Cohen's guidelines (0.00–0.09 nonexistent, 0.10–0.29 small, 0.30–0.49 medium, 0.50–0.69 large, 0.70–0.89 very large, 0.90–0.99 nearly perfect, and 1.00 perfect) (Cohen, 1992, Hopkins, 2008).
The 95% limits of agreement were also calculated as mean difference ± 1.96 × SD (Bland & Altman, 1999). After statistically analysing the data, the results were rounded to 2 decimal places.
Results
The mean ± SD, minimum and maximum values of all goniometric measurements (universal goniometer and iPhone® app) for both examiners are presented in Table 2. Measurement data from the intra‐rater (within‐day and between‐day) and inter‐rater (within‐day) reliability analysis including the ICC with 95% confidence interval (CI), SEM, 2 SEMs, and MDC95 are reported in Tables 3 and 4. Excellent intra‐rater reliability was found with both the universal goniometer and iPhone® app for wrist ROM ranging from 0.82 to 0.93 (Table 3). Furthermore, the results of the current study showed that the inter‐rater reliability was good to excellent, ranging from 0.73 to 0.82 (Table 4). Concurrent validity analysis showed very large to nearly perfect correlations among the universal goniometer and iPhone® app with r values of 0.84, 0.80, 0.85, and 0.92 for flexion, extension, radial deviation, and ulnar deviation, respectively (high direct relationship) (Fig. 6).
Table 3.
Intra‐rater reliability of universal goniometer and iPhone® app
| Measurements | Intra‐rater reliability | Universal goniometer | iPhone® app | ||
|---|---|---|---|---|---|
| Within‐day (2 h) | Between‐day (48 h) | Within‐day (2 h) | Between‐day (48 h) | ||
| Flexion ROM | ICC (95% CI) | 0.91 (0.83–0.94) | 0.85 (0.74–0.90) | 0.89 (0.75–0.93) | 0.83 (0.69–0.92) |
| SEM | 1.36° | 1.75° | 1.55° | 1.93° | |
| 2 SEMs | 2.72° | 3.5° | 3.1° | 3.86° | |
| MDC95 | 3.77° | 4.85° | 4.30° | 5.35° | |
| Extension ROM | ICC (95% CI) | 0.93 (0.85–0.97) | 0.87 (0.76–0.93) | 0.90 (0.83–0.94) | 0.85 (0.74–0.89) |
| SEM | 1.12° | 1.53° | 1.03° | 1.27° | |
| 2 SEMs | 2.24° | 3.06° | 2.06° | 2.54° | |
| MDC95 | 3.10° | 4.24° | 2.85° | 3.52° | |
| Radial deviation ROM | ICC (95% CI) | 0.87 (0.73–0.91) | 0.82 (0.71–0.88) | 0.87 (0.70–0.92) | 0.83 (0.74–0.94) |
| SEM | 0.60° | 0.70° | 0.92° | 1.05° | |
| 2 SEMs | 1.20° | 1.40° | 1.84° | 2.10° | |
| MDC95 | 1.66° | 1.94° | 2.55° | 2.91° | |
| Ulnar deviation ROM | ICC (95% CI) | 0.89 (0.77–0.95) | 0.86 (0.72–0.94) | 0.91 (0.80–0.96) | 0.86 (0.73–0.93) |
| SEM | 1.09° | 1.23° | 1.12° | 1.39° | |
| 2 SEMs | 2.18° | 2.46° | 2.24° | 2.78° | |
| MDC95 | 3.02° | 3.41° | 3.10° | 3.85° | |
CI, confidence interval; ICC, intraclass correlation coefficient; MDC95, minimum detectable change at the 95% confidence level; ROM, range of motion; SEM, standard error of measurement; 2 SEMs, two standard errors of measurement.
Table 4.
Inter‐rater reliability of universal goniometer and iPhone® app
| Inter‐rater reliability | Universal goniometer | iPhone® app | ||||||
|---|---|---|---|---|---|---|---|---|
| Flexion ROM | Extension ROM | Radial deviation ROM | Ulnar deviation ROM | Flexion ROM | Extension ROM | Radial deviation ROM | Ulnar deviation ROM | |
| ICC (95% CI) | 0.78 (0.72–0.85) | 0.81 (0.74–0.87) | 0.80 (0.72–0.88) | 0.73 (0.67–0.81) | 0.79 (0.67–0.89) | 0.81 (0.75–0.90) | 0.80 (0.72–0.87) | 0.82 (0.75–0.88) |
| SEM | 1.98° | 1.76° | 0.71° | 1.71° | 2.22° | 1.67° | 1.06° | 1.62° |
| 2 SEMs | 3.96° | 3.52° | 1.42° | 3.42° | 4.44° | 3.34° | 2.12° | 3.24° |
| MDC95 | 5.49° | 4.88° | 1.97° | 4.74° | 6.15° | 4.63° | 2.94° | 4.49° |
CI, confidence interval; ICC, intraclass correlation coefficient; MDC95, minimum detectable change at the 95% confidence level; SEM, standard error of measurement; 2 SEMs, two standard errors of measurement; ROM, range of motion.
Figure 6.
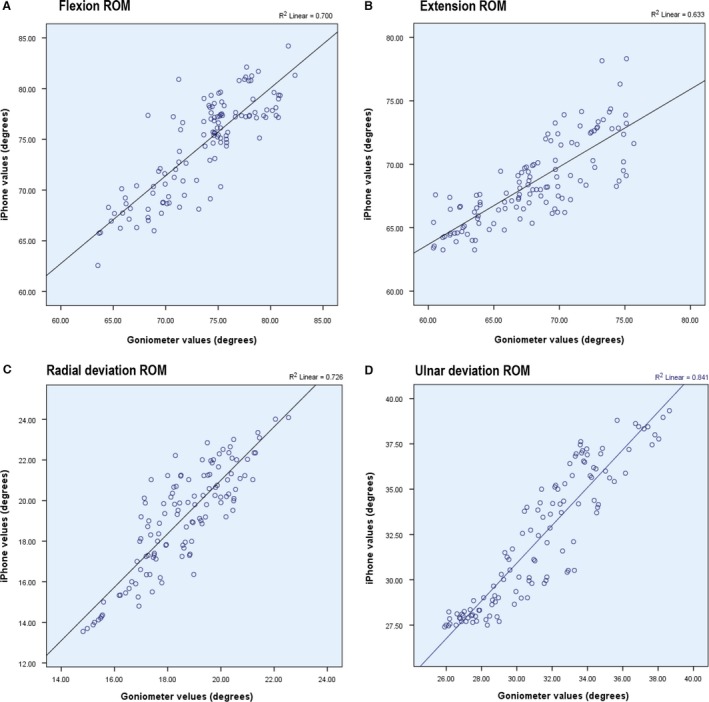
Scatterplots showing relationship between the iPhone® app and universal goniometer for maximum active wrist (A) flexion, (B) extension, (C) radial deviation, and (D) ulnar deviation.
The 95% limits of agreement (Bland–Altman plots; Fig. 7) indicate that there are no differences between the values measured using the two instruments as the zero point lies within the range of differences between universal goniometer and iPhone® values; however, individual differences may cause variations in the measured angle by iPhone® or universal goniometer. According to the results, in active wrist flexion, differences (95% limits of agreement) may range from the iPhone® measurements being 6.08° greater to 4.22° less than those with the universal goniometer. Differences between the iPhone® and universal goniometer for wrist extension, radial deviation, and ulnar deviation are depicted by Bland–Altman plots in Fig. 7.
Figure 7.
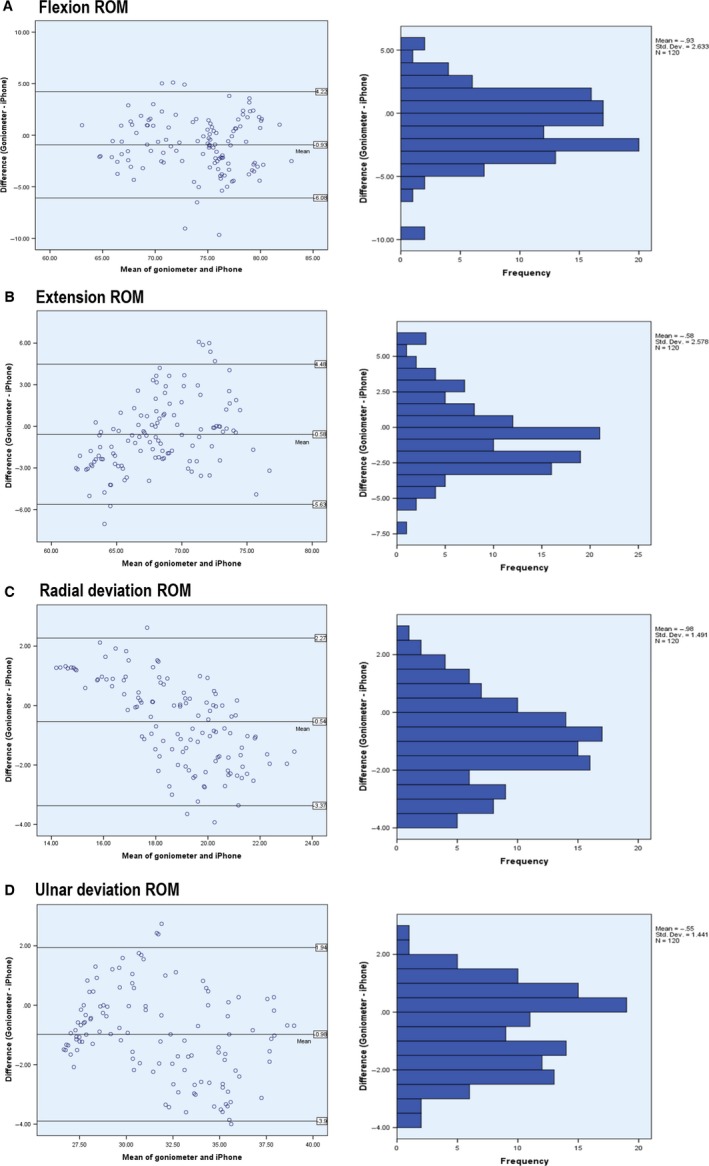
Bland–Altman plots (left column) representing mean differences and 95% limits of agreement between the universal goniometer and iPhone® measurements of maximum active wrist (A) flexion, (B) extension, (C) radial deviation, and (D) ulnar deviation (degrees). Histograms (right column) are also included to represent the distribution of measurement error.
Discussion
To the best of the authors’ knowledge, this is the first study to investigate the intra‐rater and inter‐rater reliability, MDC95, and concurrent validity of a new accelerometer‐based smartphone goniometric app (G‐pro©) for measuring wrist ROM in asymptomatic subjects.
The wrist joint is a unique and complicated structure that moves in all three cardinal planes and provides a stable platform for the function of the hand in all positions in space (Bain et al. 2016; Shin & Lee, 2016). Stresses from the activities of daily living, trauma (micro and macro), and also many pathologies can affect wrist mechanics and function. Measurement of wrist ROM with valid and reliable instruments can help clinicians provide more accurate clinical assessment in patients with wrist injuries. A universal goniometer is an instrument used for measuring wrist ROM (Horger, 1990; LaStayo & Wheeler, 1994). The reliability of the universal goniometer in the present study is consistent with previous studies, which have reported good to excellent ICC values (Horger, 1990; LaStayo & Wheeler, 1994). In the Horger (1990) study, the intra‐rater and inter‐rater reliability of the measurement of active wrist ROM ranged from 0.90 to 0.96 and from 0.78 to 0.90, respectively. LaStayo & Wheeler (1994) reported a mean of intra‐rater reliability ranging from 0.80 to 0.92 for passive wrist ROM measurement using three different techniques. The mean of inter‐rater reliability ranged between 0.80 and 0.93 (LaStayo & Wheeler, 1994). In our investigation, the ICC values for the intra‐rater reliability of measuring active wrist ROM using a universal goniometer were between 0.82 and 0.93, and the ICC values for the inter‐rater reliability ranged from 0.73 to 0.81. Good to excellent reliability in this study is likely due to accurate and firm placement of the universal goniometer and controlling its slippage on subjects’ skin during movement, three repetitions of each measurement, the simplicity of the instrument being used, and increased familiarity of subjects with the testing procedures. No published study has evaluated the within‐day intra‐rater reliability of the universal goniometer and the iPhone® app for measuring active wrist ROM; therefore, the results of this study provide the groundwork for further research in this area. The reliability of the iPhone® app was good to excellent, with ICC ranging from 0.79 to 0.82. All above‐mentioned reasons could also explain the high reliability in measuring active wrist ROM using the iPhone®. Due to the lack of research in using smartphones for measuring wrist ROM, a comparison between the reliability results of our study and previous research cannot be made.
The mean descriptive measurement values of the two instruments were similar, although both raters found the mean values of the universal goniometer were slightly lower when compared with the iPhone® mean values. This slight difference may have been caused by differences between the shapes of the two instruments. A point worth mentioning is that the difference was not statistically significant and therefore did not have a negative influence or cause concerns to clinicians about the measurement of wrist ROM using the iPhone® app. Kim et al. (2014) measured the ROM of the wrist using a universal goniometer and the iPhone® 4 Gyroscope app. The mean flexion–extension values of the universal goniometer were about 1° higher than the values obtained with the iPhone® app. Differences in the placement techniques used between the two instruments for the measurement of wrist flexion–extension ROM may have been responsible for this. In that study, the ulnar alignment technique was utilized for the measurement with the universal goniometer and the dorsal alignment technique was utilized for the measurement with the iPhone® app (Kim et al. 2014). However, Kim et al. (2014) indicated that there are no statistically differences between the mean values of the universal goniometer and iPhone® app. In the current study in order to generate homogeneity in the measurement methods, the placement technique was the same for both instruments. This may allow a better comparison between the results of the universal goniometer and iPhone® app.
Previous studies have evaluated wrist ROM using universal goniometers and reported that on average, the wrist flexes from 0° to about 70° to 85° and extends from 0° to about 60° to 75° (Horger, 1990; LaStayo & Wheeler, 1994; Neumann, 2010; Kim et al. 2014). Neumann (2010) stated that total wrist flexion ROM normally exceeds wrist extension ROM by about 10° to 15°. In addition, ulnar deviation occurs from 0° to about 35° to 40° and radial deviation from 0° to about 15° to 20° (Horger, 1990; LaStayo & Wheeler, 1994; Neumann, 2010; Kim et al. 2014). The results of our study indicated that all goniometer ROM measurements were in the range described by other studies for normal wrists. Active ROM values measured by the iPhone® app (G‐pro©) were similar to the findings of Kim et al. (2014). The iPhone® placement technique used in the current study was based on the Kim et al. (2014) study. Therefore, the similarity of the results may be due to the similar method of measurement employed in both studies. However, further investigation is needed to evaluate the ROM of the wrist using smartphone apps because the research in this area is limited and the publications on the measurement of wrist ROM using smartphone apps are very recent.
Concurrent validity is a type of criterion‐related validity examining how well a new specific instrument (iPhone® app: G‐pro©) correlates with a previously validated measure (Kerlinger & Lee, 2000). According to Sullivan (2011), measurement instruments must be valid for study results to be credible. Concurrent validity analysis of the current study reported very large to nearly perfect correlations between the two instruments with r values of ≥ 0.80. The hypothesis of the current study that the G‐pro© app is a valid app for measuring wrist ROM was confirmed.
One advantage of using the iPhone® app over the universal goniometer is that the app is available anytime, anywhere, and can be downloaded for free from the Apple App Store. Moreover, the trial version of this app is also available for free for Android smartphones on Google Play (https://play.google.com/store/apps/details?id=com.FiveFufFive.GoniometerProPreviewAndroid&hl=en). However, it is important to consider limitations related to smartphone use. Clinicians may be reluctant to use their personal smartphone for assessment because there would be a direct contact between the smartphone and the patient's skin (Kolber et al. 2013; Salamh & Kolber, 2014). In addition, smartphones sometimes freeze or stop unexpectedly and would therefore obstruct or interfere with the measurement (Pourahmadi et al. 2016b). The smartphone battery charge level is another important factor that should be considered during the assessment. Insufficient battery charge level results in the smartphone turning off, and the collected data being lost.
As the number of smartphone users has been increasing in the last decade, utilizing a valid and reliable app instead of traditional instruments can enable clinicians to measure wrist ROM in a simpler and faster manner (Kim et al. 2014). In addition, the app can be used alongside a self‐assessment questionnaire such as the Munich wrist questionnaire (MWQ; Beirer et al. 2016) or the patient‐rated wrist evaluation outcome questionnaire (PRWE; MacDermid, 1996; MacDermid et al. 1998, 2000) to evaluate the functional status of the wrist joint in various pathologies. Using the app and a self‐assessment score can help clinicians determine the amount of functional limitation of the wrist joint and enable them to monitor the effectiveness of rehabilitation process in patient‐centred follow‐up studies. Combination of subjective assessments and objective measurements of the wrist joint may facilitate the comparisons of treatment results in wrist disorders.
Study limitation and future research recommendations
There are some limitations in the present study. We did not perform a power analysis to determine the needed sample size. However, we attempted to assess a large number of wrist joints.
The subjects of the present study were asymptomatic, therefore, the generalizability of these findings is limited and the data obtained from the healthy (asymptomatic) subjects is not representative of the population with wrist pathologies. Hence, further research is required to evaluate symptomatic subjects. In addition, future studies can investigate the reliability and validity of this app for measuring the ROM of other joints.
Conclusion
Measuring the ROM of the wrist is an important physical examination conducted by clinicians for the purpose of evaluation, diagnosis, prognosis, and treatment of patients with various wrist pathologies. Numerous instruments have been introduced for this purpose (e.g. goniometers, inclinometers, measuring tapes). Smartphone goniometer apps have been developed in recent years which can enable the measurement of wrist ROM in a simpler and faster manner. The G‐pro© app has been developed recently for smartphones and can be used for goniometeric functions. This investigation demonstrated that the G‐pro© app possesses good to excellent reliability (ICC ≥ 0.73) and concurrent validity with a universal goniometer (r ≥ 0.80) for measuring wrist ROM. According to the results of the present study, it would appear that the app can be used for wrist ROM evaluation.
Highlights
What is already known on this topic
Normal wrist ROM is always required for daily activities, and measurement of wrist ROM with a valid and reliable instrument can help clinicians determine the amount of limitation, and monitor the effectiveness of rehabilitation process.
Numerous instruments have been introduced for the measurement of wrist ROM (e.g. goniometers, inclinometers, measuring tapes).
It has been shown that universal goniometers are reliable instruments available for clinicians to assess wrist ROM.
What this study adds
This study for the first time evaluated the reliability and concurrent validity of a new iPhone® app (G‐pro©) for measuring active wrist ROM in asymptomatic subjects.
Excellent intra‐ and inter‐rater reliability was demonstrated for the iPhone® app.
The concurrent validity between a universal goniometer and the iPhone® app was very good to nearly perfect.
It would appear that the iPhone® app can be used for the measurement of active wrist ROM.
This study provides the groundwork for further research in this area to assess the interchangeability of smartphone apps with other commonly used measurement tools.
Sources of support
The authors received no funding in support of this research.
Disclosure of interests
The authors declare that there are no competing interests regarding the publication of this paper.
Author contributions
M.R.P. conceived and designed the experiments, performed the experiments, analysed the data, contributed to the discussion and interpretation of the data, prepared figures and tables, wrote the paper, and reviewed drafts of the paper. I.E.T. conceived and designed the experiments, contributed to the discussion and interpretation of the data, and reviewed drafts of the paper. J.S. conceived and designed the experiments, contributed to the discussion and interpretation of the data, and reviewed drafts of the paper. M.B. performed the experiments, and reviewed drafts of the paper. M.A.M.B. contributed to the discussion and interpretation of the data, assisted in English‐editing the paper, and reviewed drafts of the paper. F.R. analysed the data, reviewed drafts of the paper. M.T. conceived and designed the experiments, analysed the data, prepared tables, and reviewed drafts of the paper.
Acknowledgements
The authors of the current study would like to thank all the subjects who participated, without whose support this study could not have been completed.
References
- Adams L, Greene L, Topoozian E (1992) Range of motion. Clin Assess Recommend 2, 55–70. [Google Scholar]
- Bain GI, Clifton T, Costi JJ, et al. (2016) Biomechanics of the rheumatoid wrist deformity In: Clinical Management of the Rheumatoid Hand, Wrist and Elbow. (ed. Chung KC.), pp. 75–86, Cham: Springer. [Google Scholar]
- Behnoush B, Tavakoli N, Bazmi E, et al. (2016) Smartphone and universal goniometer for measurement of elbow joint motions: a comparative study. Asian J Sports Med 7, e30668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beirer M, Serly J, Vester H, et al. (2016) The Munich Wrist Questionnaire (MWQ) – development and validation of a new patient‐reported outcome measurement tool for wrist disorders. BMC Musculoskelet Disord 17, 167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland JM, Altman DG (1999) Measuring agreement in method comparison studies. Stat Methods Med Res 8, 135–160. [DOI] [PubMed] [Google Scholar]
- Bovens AM, van Baak MA, Vrencken JG, Wijnen JA, Verstappen FT. (1990) Variability and reliability of joint measurements. Am J Sports Med 18, 58–63. [DOI] [PubMed] [Google Scholar]
- Bruton A, Ellis B, Goddard J (1999) Comparison of visual estimation and goniometry for assessment of metacarpophalangeal joint angle. Physiotherapy 85, 201–208. [Google Scholar]
- Carter TI, Pansy B, Wolff AL, et al. (2009) Accuracy and reliability of three different techniques for manual goniometry for wrist motion: a cadaveric study. J Hand Surg 34, 1422–1428. [DOI] [PubMed] [Google Scholar]
- Cauraugh J, Light K, Kim S, et al. (2000) Chronic motor dysfunction after stroke recovering wrist and finger extension by electromyography‐triggered neuromuscular stimulation. Stroke 31, 1360–1364. [DOI] [PubMed] [Google Scholar]
- Chaffin DB, Andersson G, Martin BJ (2006) Occupational Biomechanics, 4th edn New York: Wiley. [Google Scholar]
- Charlton PC, Mentiplay BF, Pua YH, et al. (2015) Reliability and concurrent validity of a Smartphone, bubble inclinometer and motion analysis system for measurement of hip joint range of motion. J Sci Med Sport 18, 262–267. [DOI] [PubMed] [Google Scholar]
- Cohen J. (1992) A power primer. Psychological Bulletin 112, 155–159. [DOI] [PubMed] [Google Scholar]
- Cuesta‐Vargas AI, Roldán‐Jiménez C (2016) Validity and reliability of arm abduction angle measured on smartphone: a cross‐sectional study. BMC Musculoskelet Disord 17, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dziedzic K, Hammond A (2010) Rheumatology: Evidence‐Based Practice for Physiotherapists and Occupational Therapists, 1st edn. Edinburgh: Elsevier Health Sciences. [Google Scholar]
- Ellis B, Bruton A (1998) Clinical assessment of the hand‐a review of joint angle measures. Br J Hand Ther 3, 5–8. [Google Scholar]
- Ellis B, Bruton A, Goddard JR (1997) Joint angle measurement: a comparative study of the reliability of goniometry and wire tracing for the hand. Clin Rehabil 11, 314–320. [DOI] [PubMed] [Google Scholar]
- Faurholt‐Jepsen M, Munkholm K, Frost M, et al. (2016) Electronic self‐monitoring of mood using IT platforms in adult patients with bipolar disorder: a systematic review of the validity and evidence. BMC Psychiatry 16, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fess EE (1998) Making a difference: The importance of good assessment tools. J Hand Ther 3, 3. [Google Scholar]
- Goniometer Pro [Internet] 2015. Available from: https://itunes.apple.com/us/app/goniometer-pro/id646925503?mt=8
- Guidetti L, Placentino U, Baldari C (2016) Reliability and criterion validity of the smartphone inclinometer application to quantify cervical spine mobility. Clin Spine Surg, in press. [DOI] [PubMed] [Google Scholar]
- Haley SM, Fragala‐Pinkham MA (2006) Interpreting change scores of tests and measures used in physical therapy. Phys Ther 86, 735–743. [PubMed] [Google Scholar]
- Hopkins WG (2008) Research designs: choosing and fine‐tuning a design for your study. Sportscience 12, 12–21. [Google Scholar]
- Horger MM (1990) The reliability of goniometric measurements of active and passive wrist motions. Am J Occup Ther 44, 342–348. [DOI] [PubMed] [Google Scholar]
- Kerlinger F, Lee H (2000) Foundations of Behavioral Research. New York: Harcourt College Publishers. [Google Scholar]
- Kim TS, Park DDH, Lee YB, et al. (2014) A study on the measurement of wrist motion range using the iPhone 4 gyroscope application. Ann Plast Surg 73, 215–218. [DOI] [PubMed] [Google Scholar]
- Kolber MJ, Pizzini M, Robinson A, et al. (2013) The reliability and concurrent validity of measurements used to quantify lumbar spine mobility: an analysis of an iphone® application and gravity based inclinometry. Int J Sports Phys Ther 8, 129–137. [PMC free article] [PubMed] [Google Scholar]
- LaStayo PC, Wheeler DL (1994) Reliability of passive wrist flexion and extension goniometric measurements: a multicenter study. Phys Ther 74, 162–174. [DOI] [PubMed] [Google Scholar]
- Ling FYY, Low SP, Wang SQ, et al. (2009) Key project management practices affecting Singaporean firms’ project performance in China. Int J Project Manage 27, 59–71. [Google Scholar]
- MacDermid JC (1996) Development of a scale for patient rating of wrist pain and disability. J Hand Ther 9, 178–183. [DOI] [PubMed] [Google Scholar]
- MacDermid JC, Turgeon T, Richards RS, et al. (1998) Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma 12, 577–586. [DOI] [PubMed] [Google Scholar]
- MacDermid JC, Richards RS, Donner A, et al. (2000) Responsiveness of the short form‐36, disability of the arm, shoulder, and hand questionnaire, patient‐rated wrist evaluation, and physical impairment measurements in evaluating recovery after a distal radius fracture. J Hand Surg 25A, 330–340. [DOI] [PubMed] [Google Scholar]
- Magee DJ (2014) Orthopedic Physical Assessment, 6th edn St. Louis, Missouri: Elsevier Health Sciences. [Google Scholar]
- McKenna L, Cunningham J, Straker L (2004) Inter‐tester reliability of scapular position in junior elite swimmers. Phys Ther Sport 5, 146–155. [DOI] [PubMed] [Google Scholar]
- McVeigh KH, Murray PM, Heckman MG, et al. (2016) Accuracy and validity of goniometer and visual assessments of angular joint positions of the hand and wrist. J Hand Surg 41, e21–35. [DOI] [PubMed] [Google Scholar]
- Milanese S, Gordon S, Buettner P, et al. (2014) Reliability and concurrent validity of knee angle measurement: Smart phone app versus universal goniometer used by experienced and novice clinicians. Man Ther 19, 569–574. [DOI] [PubMed] [Google Scholar]
- Neumann DA (2010) Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation. St. Louis: Elsevier Health Sciences. [Google Scholar]
- Norkin CC, White DJ (2009) Measurement of Joint Motion: A Guide to Goniometry. Philadelphia: FA Davis. [Google Scholar]
- Otter SJ, Agalliu B, Baer N, et al. (2015) The reliability of a smartphone goniometer application compared with a traditional goniometer for measuring first metatarsophalangeal joint dorsiflexion. J Foot Ankle Res 8, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pourahmadi MR, Ebrahimi Takamjani I, Hesampour K, et al. (2016a) Effects of static stretching of knee musculature on patellar alignment and knee functional disability in male patients diagnosed with knee extension syndrome: a single‐group, pretest‐posttest trial. Man Ther 22, 179–189. [DOI] [PubMed] [Google Scholar]
- Pourahmadi MR, Taghipour M, Jannati E, et al. (2016b) Reliability and validity of an iPhone® application for the measurement of lumbar spine flexion and extension range of motion. PeerJ 4, e2355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quek J, Brauer SG, Treleaven J, et al. (2014) Validity and intra‐rater reliability of an Android phone application to measure cervical range‐of‐motion. J Neuroeng Rehabil 11, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salamh PA, Kolber M (2014) The reliability, minimal detectable change and concurrent validity of a gravity‐based bubble inclinometer and iPhone application for measuring standing lumbar lordosis. Physiother Theory Pract 30, 62–67. [DOI] [PubMed] [Google Scholar]
- Shin YH, Lee YH (2016) Biomechanics of the wrist. J Korean Fracture Soc 29, 93–100. [Google Scholar]
- Shin SH, Lee OS, Oh JH, et al. (2012) Within‐day reliability of shoulder range of motion measurement with a smartphone. Man Ther 17, 298–304. [DOI] [PubMed] [Google Scholar]
- Squeri V, Masia L, Giannoni P, et al. (2014) Wrist rehabilitation in chronic stroke patients by means of adaptive, progressive robot‐aided therapy. IEEE Trans Neural Syst Rehabil Eng 22, 312–325. [DOI] [PubMed] [Google Scholar]
- Sullivan GM (2011) A primer on the validity of assessment instruments. J Grad Med Educ 3, 119–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonga E, Uysal SA, Karayazgan S, et al. (2015) Development and reliability of a Turkish version of the Short Form‐Joint Protection Behavior Assessment (JPBA‐S). J Hand Ther 29, 275–280. [DOI] [PubMed] [Google Scholar]
- Vohralik SL, Bowen AR, Burns J, et al. (2015) Reliability and validity of a smartphone app to measure joint range. Am J Phys Med Rehabil 94, 325–330. [DOI] [PubMed] [Google Scholar]
- Werner BC, Holzgrefe RE, Griffin JW, et al. (2014) Validation of an innovative method of shoulder range‐of‐motion measurement using a smartphone clinometer application. J Shoulder Elbow Surg 23, e275–e282. [DOI] [PubMed] [Google Scholar]


