Abstract
The 68Ga-prostate-specific membrane antigen ( 68Ga-PSMA) has been recently developed to be used, as a ligand, in positron emission tomography/computed tomography (PET/CT) prostate cancer imaging, to detect prostate disease. The main objective of this review was to collect data and findings from other studies and articles to assess, theoretically, if 68GA-PSMA PET/CT is a more appropriate prostate cancer diagnostic technique in comparison with others available such as CT, 18F-fluoro-2-deoxyglucose PET/CT, or 18F-fluoromethylcholine ( 18F-choline) PET/CT. For that purpose, PubMed, the online scientific articles’ database, was consulted where the keywords “PSMA” and “PET” were used to find relevant articles. The clinicaltrials.gov, clinical trials’ database, was also consulted where the keywords “68Ga-PSMA” and “prostate” were used to search clinical trials. Based on the reviewed scientific literature, several studies were conducted to assess and compare the 68Ga-PSMA PET/CT detection rate in prostate cancer with other available techniques. One of those studies, conducted by Giesel et al., concluded, within study sample, that 75% of patients with lymph nodes detected by 68Ga-PSMA PET/CT would have not been identified using other conventional morphological criteria based techniques. In Eiber et al.'s study, 68Ga-PSMA PET detected prostatic disease findings in 67% of patients with prostate-specific antigen levels <1 ng/mL, when compared with choline-based PET that presented detection rates between 19% and 36%. In Bluemel et al.'s study, 68Ga-PSMA identified positive prostatic disease in 43.8% of the patients with negative findings in F-choline PET/CT. Findings from this review demonstrate that 68Ga-PSMA PET/C is more effective in detecting metastases, lymph nodes, and recurrent prostate cancer when compared to 18F-choline-based PET/CT and CT. 68Ga-PSMA PET/CT presents also more imaging contrast and can be more cost-effective. 68Ga-PSMA has already been subjected to first-in-human trials, and it is now being tested in Phase II and III trials.
Keywords: 68 Ga-prostate-specific membrane antigen, positron emission tomography/computed tomography, prostate cancer
Introduction
Portugal, in 2012, presented 6022 individuals with prostate cancer, corresponding to 23% of all cancers reported.[1,2] Worldwide, in 2012, 1.1 million men had prostate cancer.[3,4] The therapeutic decision in these patients depends, essentially, on the prostate cancer staging and on the presence or absence of metastases.[5,6] For localized prostate cancer, usually, the first-line treatment is radical prostatectomy or radiation therapy. For localized recurrent disease, the treatment mostly used is salvage therapy; whereas for metastatic disease, the most indicated is systematic therapy. Several studies performed with computed tomography (CT), magnetic resonance imaging (MRI), 18F-fluoro-2-deoxyglucose positron emission tomography/CT ( 18F-FDG PET/CT), and 18F-fluoromethylcholine ( 18F-choline) PET/CT have provided unsatisfactory sensitivity rates in prostate cancer metastasis detection, specifically, lymph nodes detection. Particularly, in transrectal ultrasound or CT, the sensitivity varies between 25% and 54% for localized recurrent prostate cancer detection, while CT or MRI presents sensitivity rates of 30%-80% for metastases detection. For 11C and 11F-choline, in patients with prostate-specific antigen (PSA) levels <3 ng/mL, the detection rate ranges from 40% to 60%. It is extremely important to find the disease location in asymptomatic patients with PSA rising levels. There is a need to use a more accurate and sensitive mechanism to detect earlier recurrent disease extent and location in asymptomatic patients with biochemical recurrence, to improve diagnosis and therapies.[5,6,7,8]
The prostate-specific membrane antigen (PSMA), also known as glutamate carboxypeptidase II, is a membrane-type zinc protease which is overexpressed in almost all patients with prostate cancer. Practically, all prostate gland adenocarcinomas overexpress PSMA although it can be expressed in other tissues such as kidney, proximal small intestine, and salivary glands. This overexpression is proportional to tumor aggressiveness, metastatic disease, and disease recurrence.[6,9,10] Contrarily, choline metabolism is not overexpressed in a significant number of cases.[11] The potential of targeting PSMA with 68Ga and 123I-labelled in PET/CT was already demonstrated as clinically significant for prostate cancer imaging in first-in-human trials.[6,7,10]
The 68Ga-PSMA has been recently developed to be used as a PSMA ligand in PET/CT prostate cancer imaging to trace prostatic disease presence and location.[8,11]
Objective
This narrative review was conducted to collect data and findings from other studies and articles to assess, theoretically, if 68GA-PSMA PET/CT is a more appropriate diagnostic technique when compared with others available such as CT, 18F-FDG PET/CT, or 18F-choline PET/CT.
Methods
For the present review, PubMed, the online scientific articles’ database, was consulted where the keywords “PSMA” and “PET” were used to find relevant articles. Thirteen articles were selected with relevant data on 68Ga-PSMA and PET, with publication dates from 2014 to 2016. The clinicaltrials.gov, clinical trials’ database, was also consulted where the keywords “68Ga-PSMA” and “prostate” were used to search clinical trials. There are eight clinical trials registered, but only five of them include PET/CT procedure, being two of them in “not yet recruiting” phase, two in “recruiting” phase, and one “active but not recruiting.”
Discussion and Conclusions
Based on the reviewed scientific literature, several studies demonstrate the utility of 68Ga-PSMA PET/CT. Afshar-Oromieh et al. performed a study on 37 male patients with biochemical relapse, to compare 18F-choline PET/CT and the novel 68Ga-PSMA PET/CT, for the diagnosis of recurrent prostate cancer. The patients were subjected to 18F-choline PET/CT and then to 68Ga-PSMA PET/CT, within a 30-day period. In this study, 86.7% of patients presented at least one lesion of prostate cancer when using 68Ga-PSMA PET/CT, in comparison with 18F-choline PET/CT that only detected prostatic disease in 70.3% of patients [Table 1]. They also refer that lesions with lymph node metastases’ characteristics, using 68Ga-PSMA, presented, usually, very high contrast when compared with choline-based PET/CT. This higher contrast was also present in most skeletal metastases and local relapses.[12]
Table 1.
Summary of detection rates of 18F-flouromethylcholine versus 68Ga-prostate-specific membrane antigen positron emission tomography/computed tomography
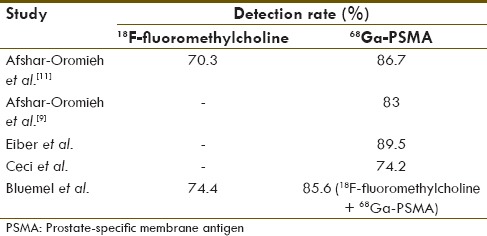
Afshar-Oromieh et al. performed a retrospective study of 319 patients who had been subjected to 68Ga-PSMA PET/CT examination from 2011 to 2014. About 83% of the patients presented at least one prostate cancer lesion with this technique [Table 1].[8,9,12,13,14] With this study, they were also able to provide information on Vitamin C, which demonstrated to have no influence in 68Ga-PSMA uptake in the salivary glands. The PSA levels and androgen deprivation therapy influenced positively the prostate cancer detection. In this study, 42 patients with lesions detected by 68Ga-PSMA PET/CT were subjected to further biopsy or surgery. The patient-based analysis revealed a sensitivity value of 88.1%. The lesion-based analysis presented values of 76.6% for sensitivity, 100% for specificity, 91.4% for negative predictive value (NPV), and 100% for positive predictive value (PPV).[9]
In the retrospective study performed by Ceci et al. with a sample of seventy patients, a detection rate of 74.2% was registered. Concerning PSA levels, patients with PSA <2 ng/mL and PSA doubling time of <6.5 months, the positivity rate was 85%; in PSA <2 ng/mL and PSA doubling time of ≥6.5 months, the positivity value was 18.7%; showing a negative relation between PSA doubling time and 68Ga-PSMA detection rate [Table 1].[13]
Giesel et al. compared 68Ga-PSMA PET/CT with three-dimensional CT volumetric lymph node assessment. It was demonstrated that in seven patients (total sample = 21) with 31 PSMA-positive nodes, only 11 of the nodes were morphologically positive based on diameters >8 mm on CT. In the other 14 patients, 18 of PSMA-positive nodes had diameters shorter than 8 mm, with a range between 2.4 and 7.9 mm. It was concluded within study population that 75% of patients with lymph nodes detected by 68Ga-PSMA PET/CT would have not been detected using conventional morphological criteria techniques.[15]
Eiber et al. conducted a retrospective study of 248 patients. About 89.5% of the patients showed disease findings in 68Ga-PSMA PET/CT [Table 1]. The detection rates were 96.8% for PSA ≥2, 93% for PSA 1 < 2, 72.7% for PSA 0.5 < 1, and 57.9% for PSA with levels 0.2 < 0.5 ng/mL/year [Table 2]. The detection efficacy was considered related to higher Gleason scores. They found that in 33% of patients, the site of recurrence could only be detected by PET. The literature refers that staging detection rates for 11C-choline range from 34% to 88%, for 18F-choline from 43% to 79%, for 11C-acetate from 59% to 80%, when compared to, as seen in this study, 57.9%-96.8% for 68Ga-PSMA PET/CT. In this study, 68Ga-PSMA PET/CT detected findings in 67% of patients with PSA levels of <1 ng/mL while choline-based PET presents a detection rate between 19% and 36%.[8]
Table 2.
Summary of detection rates of 68Ga-prostate-specific membrane antigen for different prostate-specific antigen levels
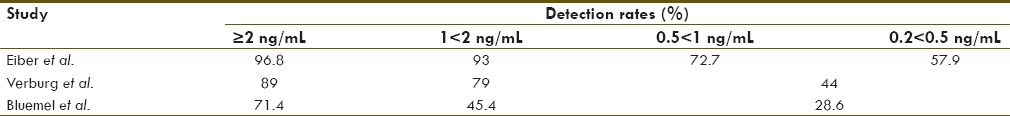
Bluemel et al. performed a study on 125 patients to assess the value of 68Ga-PSMA in patients with biochemical prostate cancer recurrence and negative 18F-choline PET/CT. Thirty-two patients showed negative results in 18F-choline PET/CT and were, then, subjected to 68Ga-PSMA. The detection rate calculated was 85.6% for the sequential imaging approach with 18F-choline followed by 68Ga-PSMA, while for 18F-choline PET/CT alone, the detection rate was only 74.4% [Table 1]. For 68Ga-PSMA patients, the detection rates were 28.6% for PSA levels of 0.2 < 1 ng/mL, 45.4% for 1–2 ng/mL, and 71.4% for ≥2 ng/mL [Table 2]. 68Ga-PSMA identified positive findings in 43.8% of the patients with negative 18F-choline PET/CT.[14]
Budδus et al. performed a study with thirty patients, where the intraprostatic tumor foci were correctly detected in 92.9% of them, using 68Ga-PSMA PET/CT. The sensitivity was 33.3%, specificity was 100%, PPV was 100%, NPV was 69.2%, and accuracy registered was 73.3%, for initial prostate cancer nodal staging [Table 2].[16]
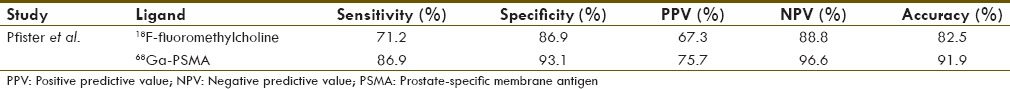
Pfister et al. studied the accuracy of 68Ga-PSMA PET/CT in comparison with 18F-choline PET/CT, in a sample of 66 patients. Thirty-eight patients underwent 18F-choline, while 28 were subjected to 68Ga-PSMA. The results were 71.2% of sensitivity for 18F-choline and 86.9% for 68Ga-PSMA; 86.9% of specificity for 18F-choline, and 93.1% for 68Ga-PSMA; PPV of 67.3% for 18F-choline and 75.7% for 68Ga-PSMA; NPV of 88.8% for 18F-choline and 96.6% for 68Ga-PSMA; and accuracy of 82.5% for 18F-choline and 91.9% for 68Ga-PSMA [Table 3].[11]
Table 3.
Summary of Pfister et al. study for 68Ga-prostate-specific membrane antigen positron emission tomography/computed tomography parameters
Verburg et al. conducted a retrospective study with 155 patients with recurrent prostate cancer, to assess the relation between extending of disease determined by 68Ga-PSMA PET/CT, PSA values, PSA doubling time, and Gleason score. The detection rate registered was 44% for PSA levels of ≤1, 79% for PSA levels of 1–2 ng/mL, and 89% for ≥2 ng/mL, showing a positive relation between PSA levels and 68Ga-PSMA detection rate [Table 2]. With PSA doubling time values of <6 months and PSA of ≥2 ng/mL, 95% showed a positive scan, while with PSA level of <1 ng/mL and PSA doubling time of >6 months, only 36% had a positive scan, which indicates, once more, a negative relation between PSA doubling time and 68Ga-PSMA detection rate.[17]
From the five clinical trials registered in clinicaltrials.gov, two correspond to Phase II (one not yet recruiting and one recruiting), two of Phase III (one not yet recruiting and one recruiting), and one feasibility (ongoing, not recruiting) which shows that the first-in-human trials have demonstrated positive results concerning safety issues, and further efficacy and safety studies, in larger populations, are being conducted.[10,18]
Conclusion
The literature consulted to elaborate this narrative review presents findings which demonstrate that 68Ga-PSMA PET/CT is more effective in detecting metastases, lymph nodes, and recurrent prostate cancer when compared with 18F-choline-based PET/CT and CT. The image acquired by 68Ga-PSMA PET/CT presents also more contrast, and the technique can be more cost-effective since 68Ga is made available by 68Ge/ 68Ga radionuclide generators and no cyclotron is needed. This hybrid imaging technique is also effective in patients with low PSA levels, being positively related with rising levels of this biomarker and tumor size. This early detection is crucial to stage the prostate cancer and to manage the most appropriate therapy for the patient. The technique was assessed in several retrospective studies which showed good safety profiles and better efficacy among others available. This method was also tested through first-in-human trials proving its safety, and it is now being subjected to Phase II and III clinical trials to explore 68Ga-PSMA safety and efficacy, in larger populations.[1,2,5,6,7,8,9,10,11,12,13,14,15,16,17,18]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Fact Sheets by Population. [Last cited on 2016 Apr 29]. Available from: http://www.globocan.iarc.fr/Pages/fact_sheets_population.aspx .
- 2.RORENO – Cancer Incidence in Portugal North Region. 2015. [Last cited on 2016 Apr 29]. Available from: http://www.file:///C:/Users/Utilizador/Downloads/factsh_norte2005(4).pdf .
- 3.Prostate Cancer Statistics. World Cancer Research Fund International. 2015. [Last cited on 2016 Jul 20]. Available from: http://www.wcrf.org/int/cancer-facts-figures/data-specific-cancers/prostate-cancerstatistics .
- 4.Globocan. Prostate Cancer Estimated Incidence, Mortality and Prevalence Worldwide in 2012. IARC. 2012. [Last cited on 2007 Jun 20]. Available from: http://www.globocan.iarc.fr/old/FactSheets/cancers/prostatenew.asp .
- 5.Kabasakal L, Demirci E, Ocak M, Akyel R, Nematyazar J, Aygun A, et al. Evaluation of PSMA PET/CT imaging using a 68Ga-HBED-CC ligand in patients with prostate cancer and the value of early pelvic imaging. Nucl Med Commun. 2015;36:582–7. doi: 10.1097/MNM.0000000000000290. [DOI] [PubMed] [Google Scholar]
- 6.Kabasakal L, Demirci E. PSMA PET/CT Imaging and Therapy. J Imaging Interv Radiol. 2015;1:49–52. [Google Scholar]
- 7.Eder M, Neels O, Müller M, Bauder-Wüst U, Remde Y, Schäfer M, et al. Novel preclinical and radiopharmaceutical aspects of [68Ga]Ga-PSMA-HBED-CC: A new PET tracer for imaging of prostate cancer. Pharmaceuticals (Basel) 2014;7:779–96. doi: 10.3390/ph7070779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eiber M, Maurer T, Souvatzoglou M, Beer AJ, Ruffani A, Haller B, et al. Evaluation of hybrid 68Ga-PSMA ligand PET/CT in 248 patients with biochemical recurrence after radical prostatectomy. J Nucl Med. 2015;56:668–74. doi: 10.2967/jnumed.115.154153. [DOI] [PubMed] [Google Scholar]
- 9.Afshar-Oromieh A, Avtzi E, Giesel FL, Holland-Letz T, Linhart HG, Eder M, et al. The diagnostic value of PET/CT imaging with the (68)Ga-labelled PSMA ligand HBED-CC in the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2015;42:197–209. doi: 10.1007/s00259-014-2949-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weineisen M, Schottelius M, Simecek J, Baum RP, Yildiz A, Beykan S, et al. 68Ga- and 177Lu-Labeled PSMA I and T: Optimization of a PSMA-targeted theranostic concept and first proof-of-concept human studies. J Nucl Med. 2015;56:1169–76. doi: 10.2967/jnumed.115.158550. [DOI] [PubMed] [Google Scholar]
- 11.Pfister D, Porres D, Heidenreich A, Heidegger I, Knuechel R, Steib F, et al. Detection of recurrent prostate cancer lesions before salvage lymphadenectomy is more accurate with (68)Ga-PSMA-HBED-CC than with (18)F-Fluoroethylcholine PET/CT. Eur J Nucl Med Mol Imaging. 2016;43:1410–7. doi: 10.1007/s00259-016-3366-9. [DOI] [PubMed] [Google Scholar]
- 12.Afshar-Oromieh A, Zechmann CM, Malcher A, Eder M, Eisenhut M, Linhart HG, et al. Comparison of PET imaging with a (68)Ga-labelled PSMA ligand and (18)F-choline-based PET/CT for the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2014;41:11–20. doi: 10.1007/s00259-013-2525-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ceci F, Uprimny C, Nilica B, Geraldo L, Kendler D, Kroiss A, et al. (68)Ga-PSMA PET/CT for restaging recurrent prostate cancer: which factors are associated with PET/CT detection rate? Eur J Nucl Med Mol Imaging. 2015;42:1284–94. doi: 10.1007/s00259-015-3078-6. [DOI] [PubMed] [Google Scholar]
- 14.Bluemel C, Krebs M, Polat B, Linke F, Eiber M, Samnick S, et al. 68Ga-PSMA-PET/CT in patients with biochemical prostate cancer recurrence and negative 18F-Choline-PET/CT. Clin Nucl Med. 2016;41:515–21. doi: 10.1097/RLU.0000000000001197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Giesel FL, Fiedler H, Stefanova M, Sterzing F, Rius M, Kopka K, et al. PSMA PET/CT with Glu-urea-Lys-(Ahx)-[68Ga(HBED-CC)] versus 3D CT volumetric lymph node assessment in recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2015;42:1794–800. doi: 10.1007/s00259-015-3106-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Budäus L, Leyh-Bannurah SR, Salomon G, Michl U, Heinzer H, Huland H, et al. Initial experience of (68)Ga-PSMA PET/CT imaging in high-risk prostate cancer patients prior to radical prostatectomy. Eur Urol. 2016;69:393–6. doi: 10.1016/j.eururo.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 17.Verburg FA, Pfister D, Heidenreich A, Vogg A, Drude NI, Vöö S, et al. Extent of disease in recurrent prostate cancer determined by [(68)Ga]PSMA-HBED-CC PET/CT in relation to PSA levels, PSA doubling time and Gleason score. Eur J Nucl Med Mol Imaging. 2016;43:397–403. doi: 10.1007/s00259-015-3240-1. [DOI] [PubMed] [Google Scholar]
- 18.Search of: 68Ga-PSMA | Prostate – List Results. [Last cited on 2016 Jul 20]. Available from: https://www.clinicaltrials.gov/ct2/results?term=68Ga&recr=&rslt=&type=&cond=Prostate&intr=&titles=&outc=&spons=&lead=&id=&state1=&cntry1=&state2=&cntry2=&state3=&cntry3=&locn=&gndr=&rcv_s=&rcv_e=&lup_s=&lup_e=


