Abstract
Background
Despite significant research examining mental health in conflict-affected populations we do not yet have a comprehensive epidemiological model of how mental disorders are distributed, or which factors influence the epidemiology in these populations. We aim to derive prevalence estimates specific for region, age and sex of major depression, and PTSD in the general populations of areas exposed to conflict, whilst controlling for an extensive range of covariates.
Methods
A systematic review was conducted to identify epidemiological estimates of depression and PTSD in conflict-affected populations and potential predictors. We analyse data using Bayesian meta-regression techniques.
Results
We identified 83 studies and a list of 34 potential predictors. The age-standardised pooled prevalence of PTSD was 12.9% (95% UI 6.9–22.9), and major depression 7.6% (95% UI 5.1–10.9) – markedly lower than estimated in previous research but over two-times higher than the mean prevalence estimated by the Global Burden of Disease Study [3.7% (95% UI 3.0–4.5) and 3.5% (95% UI 2.9–4.2) for anxiety disorders and MDD, respectively]. The age-patterns reveal sharp prevalence inclines in the childhood years. A number of ecological variables demonstrated associations with prevalence of both disorders. Symptom scales were shown to significantly overestimate prevalence of both disorders. Finding suggests higher prevalence of both disorders in females.
Conclusion
This study provides, for the first time, age-specific estimates of PTSD and depression prevalence adjusted for an extensive range of covariates and is a significant advancement on our current understanding of the epidemiology in conflict-affected populations.
Key words: Aetiology, conflict, depression, epidemiology, global mental health, post-traumatic stress disorder
Introduction
The significant association between war-trauma exposure and elevated mental disorder prevalence has been demonstrated repeatedly in epidemiological studies and a causal effect between war-trauma exposure and reduced mental health of a population is generally acknowledged. (Kalt et al. 2013; Karam et al. 2014) Recent years have seen increased interest and research into the effect of war and conflict on mental disorder epidemiology, resulting in an increase in published material on the topic. The overwhelming majority of the literature has investigated the association between trauma exposure and post-traumatic stress disorder (PTSD). Depression is the only other mental disorder featuring prominently in the literature, in this context. Despite these advances we do not yet have a comprehensive epidemiological profile (including prevalence, distribution and risk factors) of PTSD or depression in conflict-affected populations, which is essential for the development of effective mental health policy and programmes addressing the mental health needs of these populations.
In order to meet the challenges of post-conflict reconstruction, comprehensive and context-specific epidemiological models of mental disorders are crucial for both conflict-affected countries and the broader international health and humanitarian community. They provide the core data required for estimating disease prevalence, i.e. the number of cases of a given disease within conflict-affected populations at a particular point in time. This, when supplemented with a variety of adjunct data sources, forms the basis for estimating mental health service requirements during the post-conflict period and for comparisons with current service capacity (Bruckner et al. 2011; World Health Organization, 2011). Furthermore, prevalence data are an essential input to the estimation of years lived with disability – the non-fatal component of burden of disease estimates (Vos et al. 2012). These estimates of non-fatal disease burden can be used in conjunction with United Nation's population data (United Nations, 2011) to project changes in the burden of mental and substance use disorders during and after conflict and, subsequently, predict the mental health workforce required to meet future needs (Charlson et al. 2012, 2014).
Although several published papers review the epidemiology of mental disorders in conflict-affected populations, only two studies have conducted pooled analyses of surveys representative of the general population – one limited to examining prevalence of mental disorders among children exposed to war (Attanayake et al. 2009); and another limited to the same in the adult population (Steel et al. 2009). Quantitative assessment of predictors for mental disorder prevalence in conflict-affected populations has also been attempted previously (Porter & Haslam, 2005; Steel et al. 2009); however, significant methodological limitations were present. To-date, epidemiological modelling of mental disorder prevalence in conflict-affected populations across the different ages, and which incorporates an extensive range of covariates using advanced meta-regression techniques, has not yet been undertaken.
The Global Burden of Disease Study 2013 (GBD2013) provides the most recent and comprehensive epidemiological profile for a variety of mental disorders (Global Burden of Disease Study 2013 Collaborators, 2015). Prevalence estimates have been calculated at the region and country level and provide a useful benchmark for which to compare estimates from conflict-affected subpopulations (Ferrari et al. 2013; Baxter et al. 2014). In addition, the GBD methodology has developed a Bayesian meta-regression tool that can be drawn upon to develop robust epidemiological models, which are also able to explore the effect of predictor variables on prevalence (Flaxman et al. 2013).
This paper aims to derive a comprehensive epidemiological profile of major depression and PTSD in general (civilian) populations exposed to conflict by: (1) conducting a systematic review to identify studies investigating the epidemiology of major depression and PTSD in conflict-affected populations across different age groups; (2) identifying significant predictors of the prevalence of major depression and PTSD in conflict-affected populations; and (3) making use of the above data and GBD Bayesian meta-regression techniques to model the prevalence of major depression and PTSD by age, sex and region.
Methods
Systematic review
A systematic review of the literature was conducted following PRISMA guidelines (Liberati et al. 2009). A systematic search of electronic databases and grey literature sources identified data sources for the prevalence of major depression and PTSD cases which met criteria as per the Diagnostic and Statistical Manual of Mental disorders (DSM) or the International Classification of Diseases (ICD) (World Health Organization, 1992; American Psychiatric Association, 2000). Additional detail of the systematic review can be found in the Online appendix.
Inclusion and exclusion criteria
Inclusion criteria have been imposed on study selection requiring: (1) study samples be representative of the general conflict-affected population; (2) participants be situated in the country of origin, displaced, or resettled in another non-Western country; (3) studies report epidemiological estimates from either cross-sectional or longitudinal population-based surveys, (4) survey instruments map to DSM or ICD criteria; and (5) data be for the period 1980 onward. Study samples were excluded if they were seeking asylum or resettled in western countries, combatants (including child soldiers), family members of combatants, clinical samples, student samples, exposed to only isolated terrorist attacks (such as 9/11), torture victims, health workers, ex-prisoners of war or political detainees, and offender samples. Additional detail of the inclusion and exclusion criteria can be found in the appendix.
Statistical methods
One way in which to make important advances on current predictive modelling efforts is to develop epidemiological estimates specific to the country/region, age and sex, whilst adjusting for a range of covariates responsible for any heterogeneity within a dataset. Information pertaining to the epidemiological data surveyed and the survey methodology were extracted from each study. Additionally, a list of variables previously shown to have significant associations with mental disorder prevalence was identified from the literature. This included ecological variables which hold relationships with health and/or mental health extracted from online databases including the United Nations, World Bank, and GBD resources. A full list of variables explored can be found in the appendix.
Analysis was conducted in two stages. At stage one, we followed previously established GBD methodology for summarising and predicting epidemiological data while adjusting for heterogeneity between studies (Charlson et al. 2013; Ferrari et al. 2013). All relevant variables were initially assessed for significant associations with prevalence in univariate analyses in Stata 11 (StataCorp, 2009). For each disorder respectively, statistically significant variables (from univariate analyses) were included in a linear regression model with prevalence as the dependent variable. Independent variables were systematically added and removed based on their contribution and influence on prevalence. This was assessed by an overall adjusted R2, and coefficient and p value derived for each variable. The final decision on whether a variable was to be included as a covariate in the stage two modelling was dependent on these findings and/or whether the variable was considered to be integral to the core research questions (e.g. sex and world region).
At stage two, we made use of DisMod-MR, a Bayesian meta-regression tool designed specifically for GBD purposes (Vos et al. 2012; Flaxman et al. 2013). DisMod-MR is used to estimate age–sex–country-specific prevalence from heterogeneous and often sparse datasets such as in this study. DisMod-MR makes use of a negative-binomial model and fits models using a randomised Markov-Chain Monte Carlo algorithm. Further details on DisMod-MR and its assumptions can be found in the appendix of this paper and in the online supplementary material of Vos et al. 2013 (Vos et al. 2012) and Flaxman et al. 2014 (Flaxman et al. 2013).
Results
Systematic review
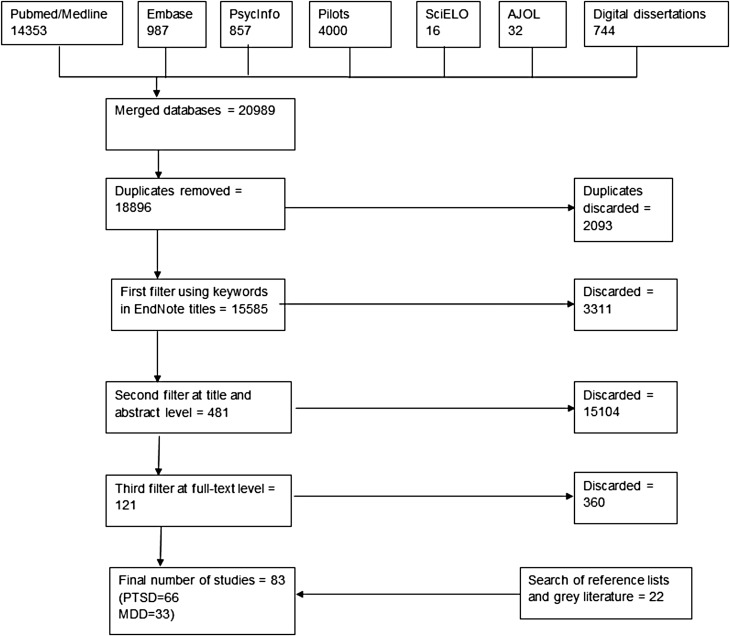
We identified a total of 83 studies; 66 studies providing 128 prevalence estimates for PTSD and 33 studies providing 69 prevalence estimates for major depression. Twenty separate conflict or post-conflict countries were represented for major depression and 27 conflict or post-conflict countries for PTSD. A summary of the search flow diagram and included studies can be found in Figure 1.
Fig. 1.
Search flow diagram.
Identifying significant covariates
Several potential predictors of prevalence were identified, and tested for univariate associations. Covariates assessed, p values from correlation tests and the final model inclusion/exclusion status based on the decision-making process outlined in the methods can be found in Table 1. A full description of covariates along with reasons for exclusion from models can be found in the appendix.
Table 1.
Covariate correlation test p values and final model inclusion/exclusion status
| PTSD | Major depression | |||
|---|---|---|---|---|
| Covariate name | Statistical significance of correlation test | Status | Statistical significance of correlation test | Status |
| Study-level covariates | ||||
| Study type | p = 0.169 | Excluded | p = 0.492 | Excluded |
| Coverage | p = 0.005 | Included | p = 0.701 | Excluded |
| Population description | p = 0.328 | Excluded | N/A | N/A |
| Education | p = 0.619 | Excluded | p = 0.895 | Excluded |
| Marital status | p = 0.439 | Excluded | p = 0.292 | Excluded |
| Diagnostic interview | p = 0.104 | Included | p = 0.000 | Included |
| Response rate | p = 0.001 | Included | p = 0.004 | Included |
| Urbanicity | p = 0.335 | Excluded | p = 0.264 | Excluded |
| Sex | p = 0.008 | Included | p = 0.050 | Included |
| Adults or children | p = 0.427 | Excluded | p = 0.864 | Excluded |
| Type of estimate | p = 0.000 | Excluded | p = 0.010 | Excluded |
| Trauma covariates | ||||
| Political terror scale rating | p = 0.230 | Excluded | p = 0.009 | Excluded |
| War-related events ratio | p = 0.001 | Included | p = 0.913 | Excluded |
| Country-level covariates | ||||
| World region | p = 0.049 | Included | p = 0.350 | Included |
| Time since conflict | p = 0.069 | Included | p = 0.104 | Included |
| Time since max PTS | p = 0.054 | Excluded | p = 0.000 | Excluded |
| Length of conflict | p = 0.675 | Excluded | p = 0.049 | Excluded |
| Alcohol usage | p = 0.094 | Excluded | p = 0.115 | Excluded |
| Drug usage | p = 0.000 | Excluded | p = 0.003 | Excluded |
Note: The war-related events ratio of an individual study is defined as the ratio of ‘the average number of war-related traumatic events with positive responses’ to ‘total number of events screened for’ (this does not include adversity related events which are captured in other variables such as unemployment). For example, if a study screened for 10 war-related events and the average number of positively responded items across subjects was 3, then the war-related events ratio for that particular study is 0.3.
Note: Covariates representing the social and economic conditions within a country excluded from modelling due to interactions with time are not included in Table 1.
Univariate tests confirmed some anticipated associations including an apparent sex difference in prevalence for both disorders, differences in prevalence as measured by diagnostic v. symptom-based instruments for both disorders, and an effect of trauma exposure on PTSD (as measured by the war-related events ratio). Notably, there was an association between the war-related events ratio and PTSD prevalence but not prevalence of major depression.
Assessment of country-level covariates showed a number of statistically significant associations. A large number of covariates representing the social and economic conditions within a country were associated with prevalence of both disorders (e.g. education index, life expectancy, and illicit drug use; see appendix for a full list). However, statistical testing confirmed the hypothesis that these variables and prevalence are likely to all vary with time. This interaction with time enhances the risk of apparent associations which are spurious and these country-level covariates were therefore excluded from modelling (Altman et al. 1983).
A covariate representing the number of years passed since the maximum rating on the Political Terror Scale for a country (time since max PTS) was used as an alternative measure of time since the end of conflict. Univariate tests showed that this covariate was strongly associated with major depression but not PTSD. However, when entered into a regression model ‘time since max PTS’ no longer contributed significantly to the prevalence of major depression. Time since conflict was a more influential covariate for both PTSD and major depression than time since max PTS and was included in the final model for both disorders.
Table 2 shows the relative risk (RR) of each of the included covariates as an output of DisMod-MR prevalence models. Relative trauma exposure from war-related events as measured by the ‘war-related events ratio’ demonstrated that study populations experiencing a ratio greater than 0.3 were 1.2 times at greater risk of PTSD than those with lower levels of conflict exposure, although this effect was not statistically significant (95% UI 0.9–1.6). Response rate did not have a statistically significant effect on prevalence. Symptom scales were shown to significantly overestimate prevalence of both PTSD and major depression. Differences across world regions or the post-conflict period were not evident.
Table 2.
Relative risks (RR) of covariates estimated from DisMod-MR modelling
| PTSD | RR (95% UI) | Major depression | RR (95% UI) |
|---|---|---|---|
| War-related events ratio | Instrument type | ||
| <0.3 | 1.0 | Diagnostic interview | 1.0 |
| >0.3 | 1.2 (0.9–1.6) | Symptom scale | 2.6 (1.7–4.0)* |
| Instrument type | Response rate | ||
| Diagnostic interview | 1.0 | >80% | 1.0 |
| Symptom scale | 1.7 (1.1–2.5)* | <80% | 0.9 (0.5–1.5) |
| Coverage | Sex | ||
| National | 1.0 | Females | 1.0 |
| Regional | 1.1 (0.7–1.6) | Males | 0.6 (0.4–1.0) |
| Community | 1.7 (0.7–1.6) | Time since conflict | |
| Response rate | 0 (still in conflict) | 1.0 | |
| >80% | 1.0 | 1–2 years | 1.6 (0.8–3.1) |
| 50–79% | 0.6 (0.4–0.9) | 3–4 years | 0.6 (0.4–1.1) |
| Sex | 5–7 years | 0.4 (0.2–1.1) | |
| Females | 1.0 | 8–10 years | 1.1 (0.5–2.9) |
| Males | 0.7 (0.5–1.0) | World region | |
| Time since conflict | North Africa/Middle East | 1.1 (0.9–1.3) | |
| 0 (still in conflict) | 1.0 | Southeast Asia | 1.0 (0.8–1.1) |
| 1–2 years | 0.8 (0.5–1.1) | Central Europe | 1.0 (0.9–1.3) |
| 3–4 years | 1.1 (0.7–1.7) | High-income countries | 1.0 (0.8–1.2) |
| 5–7 years | 1.3 (0.8–2.3) | Latin America | 1.0 (0.8–1.1) |
| 8–10 years | 0.8 (0.5–1.2) | Sub-Saharan Africa | 1.0 (0.8–1.1) |
| World region | South Asia | 1.0 (0.8–1.1) | |
| North Africa/Middle East | 1.1 (0.9–1.4) | ||
| Southeast Asia | 0.9 (0.7–1.1) | ||
| Central Europe | 1.1 (0.9–1.4) | ||
| High-income countries | 0.9 (0.7–1.1) | ||
| Latin America | 1.0 (0.8–1.2) | ||
| Sub-Saharan Africa | 1.2 (1.0–1.5) | ||
| South Asia | 0.9 (0.7–1.1) |
*Statistically significant RR.
DisMod-MR prevalence modelling
Unadjusted pooled prevalence was found to be 30.0% (95% UI 26.1–33.9) for PTSD and 20.2% (95% UI 15.0–25.8) for major depression. Making adjustments to prevalence using the covariates listed, DisMod-MR estimated the age-standardised pooled prevalence of PTSD for conflict-affected populations in our dataset at 12.9% (95% UI 6.9–22.9) and for major depression at 7.6% (95% UI 5.1–10.9). The latter is compared with a mean major depressive disorder (MDD) global prevalence of 3.5% (95% UI 2.9–4.2) estimated in GBD2013 (Institute of Health Metrics and Evaluation, 2015).
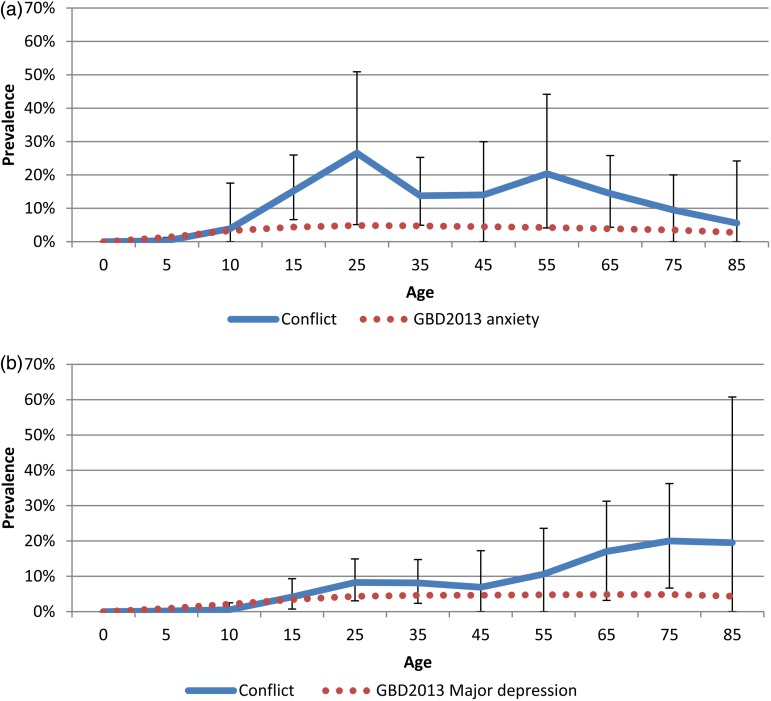
Figure 2a shows the modelled age-specific PTSD prevalence in conflict-affected populations benchmarked against the GBD2013 mean global prevalence of all anxiety disorders (Institute of Health Metrics and Evaluation, 2015). PTSD prevalence revealed a sharp incline in prevalence in childhood years peaking at around 25 years and a decline after 55 years. The age-specific prevalence for all anxiety disorders as estimated in GBD2013 was lower at all ages. Figure 2b shows the modelled age-specific major depression prevalence in conflict-affected populations benchmarked against the GBD2013 mean global prevalence of MDD. There was a steady upward trend in prevalence peaking around age 20. The second peak in the elderly is high but surrounded by overlapping bounds of uncertainty due to scarcity of data. It is important to note the ranges of uncertainty surrounding estimates when interpreting these findings.
Fig. 2.
(a) Age-specific prevalence of PTSD in conflict-affected populations (95% UI). (b) Age-specific prevalence of major depression in conflict-affected populations (95% UI). Note: GBD2013 modelled the prevalence of all anxiety disorders combined rather than PTSD specifically.
The data suggest a higher prevalence of both PTSD and major depression in females; however, this finding was not statistically significant (Table 2). There were no reported differences in exposure to war-trauma between males and females as assessed by the number of categories of war-related potentially traumatic events endorsed (not shown). No statistically significant variations in prevalence of either major depression or PTSD were found across conflict-affected populations stratified by region. However, comparison of the estimated mean major depression prevalence in conflict-affected populations with GBD2013 MDD estimates for countries contributing to our dataset, demonstrates that GBD estimates are lower than our estimated prevalence for several conflict-affected countries (Table 3).
Table 3.
Analysis of GBD 2013 country-specific MDD prevalence estimates for conflict-affected countries, 2013
| Country | GBD 2013 prevalence estimate (%, 95% uncertainty) | Difference from mean for conflict-affected populationsa |
|---|---|---|
| Bosnia-Herzegovina | 3.1 (2.7–3.6) | Lower |
| Mexico | 4.5 (2.8–6.1) | Not statistically different |
| Afghanistan | 3.4 (1.6–5.3) | Not statistically different |
| Iraq | 3.1 (2.3–3.9) | Lower |
| Lebanon | 3.5 (2.9–4.1) | Lower |
| Palestine | 7.7 (6.1–9.5) | Not statistically different |
| Nepal | 2.5 (1.8–3.5) | Lower |
| Pakistan | 4.5 (3.1–6.2) | Not statistically different |
| Indonesia | 2.2 (1.4–2.9) | Lower |
| Sri Lanka | 2.3 (1.5–3.0) | Lower |
| Timor-Leste | 1.9 (1.3–2.6) | Lower |
| Central African Republic | 5.0 (3.6–6.3) | Not statistically different |
| Democratic Republic of Congo | 5.1 (3.8–6.4) | Not statistically different |
| Ethiopia | 5.4 (4.4–6.7) | Not statistically different |
| Liberia | 4.0 (2.9–5.2) | Not statistically different |
| Nigeria | 4.4 (3.4–5.5) | Not statistically different |
| Rwanda | 6.5 (5.0–8.1) | Not statistically different |
| South Africa | 4.0 (3.3–4.8) | Lower |
| Sudan | 4.5 (3.4–6.0) | Not statistically different |
| Uganda | 6.9 (5.6–8.5) | Not statistically different |
| Israel | 3.1 (2.1–4.4) | Lower |
| Northern Ireland | 3.1 (2.7–3.6) | Lower |
| Cambodia | 2.2 (1.4–3.0) | Lower |
| Croatia | 3.1 (2.7–3.5) | Lower |
| Iran | 4.5 (2.7–6.3) | Not statistically different |
| Mozambique | 5.8 (4.3–7.5) | Not statistically different |
| Peru | 4.0 (3.1–4.8) | Lower |
| Somalia | 6.0 (4.4–7.6) | Not statistically different |
| Turkey | 3.2 (2.8–3.5) | Lower |
Mean major depression prevalence for conflict-affected populations is 7.6% (95% UI 5.1–10.9).
Heterogeneity in our datasets was large and the median value of the negative binomial model overdispersion parameter calculated by DisMod-MR for PTSD was 2.5 (where zero is completely uninformative, and infinity is a Poisson distribution). The equivalent for major depression was 1.9. Sensitivity analyses looking for outliers in both datasets were conducted by removing one input prevalence estimate at a time during meta-regression analyses to see if they significantly impacted upon results. Apparent outliers were deemed to have been sufficiently adjusted for by covariates in the meta-regression and there were no estimates removed from analyses as a result.
Discussion
This paper builds upon current knowledge, providing for the first time, age-specific prevalence estimates of major depression and PTSD in the general (civilian) populations of areas exposed to conflict within the past 10 years. It differentially assesses the population in conflict-affected areas who reside in the conflict region or have been displaced to neighbouring regions (not those resettled in Western countries) and is all-ages inclusive. The inclusion criteria are more stringent than that of previous literature in order to ensure optimum representativeness and reduced heterogeneity in prevalence estimates. Our review only included studies of participants from predefined conflict or post-conflict settings.
A key objective of this study was to derive findings that can be helpful in anticipating prevalence when a community-representative, diagnostic survey is not feasible – a necessity for informed policy and programming. This paper reiterates the elevated prevalence of major depression and PTSD in conflict-affected populations but estimates markedly lower unadjusted, age-specific and age-standardised prevalence than estimated by previous research of conflict-affected populations (Steel et al. 2009). The observed differences seen between the current study and previous work are largely due to more stringent inclusion and exclusion criteria, optimised search strategies and advances in statistical methods, but also demonstrate the importance of updating systematic reviews over time. Our optimised search strategy is not one that has been used in a systematic review of this topic before and was very effective in identifying additional relevant literature.
Contrasting our predictive estimates against estimates from GBD2013 highlights how relying on global or national estimates of mental disorders can be inherently misleading when dealing with conflict-affected sub-populations. Conflict-affected populations are often geographically constrained to only parts of a country and are typically underrepresented in broader national estimates of prevalence. The modelled prevalence of major depression in conflict-affected populations was over two-times higher than the mean global MDD prevalence estimated in GBD2013. Our findings also point to a highly elevated state of PTSD in conflict-affected populations – more than three times higher than the global mean prevalence of all anxiety disorders combined as estimated by GBD2013 [3.7% (95% UI 3.0–4.5)].
Our analysis of age trends suggested a rise in PTSD prevalence throughout childhood and adolescent years and a relative stabilisation of rates until around 60 years of age. The high rates of PTSD in children is a finding consistent with child-specific reviews (Attanayake et al. 2009) and suggests that children show particular sensitivity to developing adverse mental health outcomes following exposure to organised violence and mass conflict. That said, it is also possible that the observed differences in prevalence across ages may be partly driven by the different instruments used in assessing PTSD in children and adults.
In line with GBD2013, our findings for major depression show a peak in prevalence at around 20 years of age, with an increase in prevalence in the older ages. GBD2013 estimates did suggest a smaller increase in the oldest age group compared with our findings however large uncertainty around estimates due to scarcity of data at these ages makes parallel findings in conflict-affected populations difficult to interpret.
Our comprehensive and systematic assessment of potential predictors and selection of model covariates was a valuable aspect of this study and demonstrated a number of important findings. Furthermore, the importance of covariate adjustments in reducing inter study variability within DisMod-MR is demonstrated through the large adjustments made to the data. A covariate designed to adjust symptom scales towards diagnostic interviews found symptom scales to significantly overestimate major depression prevalence – RR 2.6 (95% UI 1.7–4.0). The same analysis for PTSD found a RR of 1.7 (95% UI 1.1–2.5). These findings should provide caution to mental health professionals when utilising prevalence data derived from symptom scales to describe clinically significant presentations of mental disorders. They may also be useful in the interpretation of other study findings by allowing for broad adjustments and/or more meaningful comparisons between estimates derived from symptom scales and those from diagnostic instruments.
In order to reflect the DSM-IV diagnostic criterion of necessarily being exposed to a traumatic event to meet diagnosis for PTSD, and the fact that we are attempting to assess populations affected by war, we elected to create a variable that would measure exposure to traumatic events directly related to war, the ‘war-related events ratio’. The derivation of this ratio drew on previous work by Steel and colleagues who created a variation of this ratio including adverse events not necessarily directly related to war (Steel et al. 2009). The odds ratio, derived from a meta-regression model using prevalence as the dependant variable, for Steel and colleagues’ covariate was greater than 3 for a ratio greater than 0.3. In our PTSD model, the war-related events ratio of greater than 0.3 revealed an effect size of only 1.2. This could be due to the more relaxed definition of exposure to ‘adverse’ events by Steel et al. more stringent inclusion criteria in terms of accepted populations, or differences in regression methods; however, our finding is likely to represent a more representative effect of exposure to traumatic events directly related to the war itself. Exposure to trauma as measured by the war-related events ratio was not significantly associated to the prevalence of major depression in the current analysis but played a role in PTSD prevalence, confirming findings of previous work (Steel et al. 2009; Roberts & Browne, 2011).
All United Nations and World Bank ecological variables (UNDP education index, World Bank GDP per capita, gender inequality index, government effectiveness, United Nations life expectancy, labour participation rate, housing, and improved water source) included in our analyses demonstrated high associations with the prevalence of major depression and PTSD. Unfortunately, they also demonstrated high multi-collinearity with each other and time since conflict hence were necessarily excluded from meta-regression models. The fact that these variables demonstrated high collinearity with time since maximum PTS rating is of interest however and a logical explanation is that as time passes after the end of a period of instability, general social and economic conditions within a country improve. There was also a strong association between major depression prevalence and time since maximum PTS which was not found for PTSD. This lends strength to a theory that major depression prevalence may be more sensitive to the effects of day-to-day challenges (represented by several UN/World Bank ecological variables) than PTSD.
Another potential predictor which is known to be associated with PTSD and major depression prevalence is intimate partner violence (IPV). However, as high quality, representative IPV prevalence data were available only for females the covariate could not be included in our analysis (Devries et al. 2013). Nonetheless, its impact on poor mental health should not be overlooked. The higher prevalence of both disorders found in females is consistent with the literature which has proposed the poor mental health of women may include social factors such as domestic and sexual violence which are prominent in conflict contexts (Roberts & Browne, 2011).
A final covariate that we attempted to include in our models is the Hofstede rating on Individualism. This covariate was chosen to reflect a level of social support experienced within a population which has been shown in many studies to act as a protective factor for mental disorders (Roberts & Browne, 2011). The Hofstede theory defines ‘individualist societies’ as those where people are expected to care and provide for themselves and their direct family only. ‘Collectivist’ societies represent a preference for a tightly-knit framework in society in which individuals can expect their relatives or members of a particular in-group to care and provide for them in exchange for unquestioning loyalty (The Hofstede Centre, 2014). This covariate was excluded from modelling due to multicollinearity with time since conflict; however, in univariate analyses it showed a strong association with PTSD in particular. That is, a loosely knit social framework may act as a risk for PTSD and, conversely, a tightly knit society may act as a protective factor for PTSD. More in-depth investigation into the association between this variable and the prevalence of major depression and PTSD is required for clearer conclusions.
Little is known about the natural history of major depression and PTSD over the post-conflict period. Although sparse and heterogeneous data produced non-significant time trends of prevalence, there may be value in creating hypotheses around these findings given what we know about the time course of MDD and PTSD from other research. Across the lifespan, remission rates of PTSD are relatively high; however, even in conflict-free settings in developed nations the median time to remission can be lengthy (Chapman et al. 2012). The lack of an observed time trend in our analyses of a 10-year post-conflict period could therefore be reasonable expected. Furthermore, a representative sample with war-related PTSD in five Balkan countries and three Western European countries were assessed on average 8 years after the war and reinterviewed 1 year later. Several years after the war, people with PTSD reported significant symptom improvement that may indicate remission. However, persistent co-morbid depression among refugees was noted (Priebe et al. 2012).
Despite an apparent association between disorder prevalence and drug and alcohol use, we were unable to include this in meta-regression models. Given that the literature supports the theory that trauma is associated with a host of adverse behavioural outcomes including substance use, independent analyses assessing alcohol and drug use as mediators of mental disorder prevalence in these populations may be a worthy exercise for future consideration.
Limitations
The most significant limitation in this study came from the raw data. Even with relatively strict inclusion criteria in place, there was considerable heterogeneity between reported estimates in the major depression and PTSD datasets which restricted analyses to some degree and created large uncertainty around the predicted estimates. This heterogeneity stemmed largely from differences across study designs which are inherently problematic in transcultural and psychiatric epidemiology, particularly following major emergencies (Rodin & Van Ommeren, 2009). Despite this limitation, the strengths of DisMod-MR in dealing with heterogeneity through adjustments to the data (if a significant bias for one or more of the covariates is detected) has allowed us to create an improved epidemiological profile of major depression and PTSD in conflict-affected populations.
A number of assumptions and proxy inputs were used in our estimations given the lack of data available on the epidemiology of major depression and PTSD in conflict-affected populations. Bayesian modelling allows us to integrate all available data on the epidemiology of a given disorder, even when they are sparse and heterogeneous; however, it requires expert-derived assumptions, in the form of ‘priors’, for the model parameters. We strove to limit the use of such expert-derived priors, and instead, to derive a more data-driven prevalence model; however, this led to estimates with large uncertainty intervals. As more and better quality prevalence data are made available, the assumptions made for this analysis can be more adequately tested. Until then, they are limitations which need to be considered when interpreting our findings.
Whilst many sources of variability are common across most fields of epidemiological research, a number of them are particularly intrinsic to mental health research. Variability is added through the use of different instruments used to measure major depression and PTSD. These are available in various versions reflecting the lack of a gold standard, the reliance on Western classification systems to measure major depression and PTSD in developing regions, and continual changes in diagnostic criteria (Whiteford et al. 2013). Cultural differences in terms of both culture-specific disorders and the outward expression of disorders create controversy in this respect, particularly within the conflict-affected populations included in this analysis.
Naturally, conducting epidemiological surveys in conflict or post-conflict settings carries its own inherent set of constraints. Limited resources and access to the affected population may result in sub-optimal sampling methods and lower representativeness. Quality of studies was kept at an optimum through the use of strict inclusion criteria, including the prerequisites of random sampling techniques and a general population sampling frame; in addition, we adjusted for methodological variability within the dataset through inclusion of several methodological covariates; however, methodological standards is an area which could be improved in future studies.
Conclusion
This study provides a significant advancement on our current understanding of the epidemiology of PTSD and major depression in conflict-affected populations. It provides for the first time, age-specific estimates of PTSD and major depression prevalence drawing on the body of research undertaken within post-conflict populations and methods developed for GBD2013. The research was also able to examine a more extensive range of covariates that had been previously examined. The results provide important input (together with information on cost-effectiveness and equity) for estimating health service requirements. Future research should strengthen study methodology and design, including longitudinal assessments, and allow investigations of whether the risk of other mental disorders is elevated by conflict.
Acknowledgements
This research received no specific grant from any funding agency, commercial or not-for-profit sectors. Core funding for the Queensland Centre of Mental Health Research is provided by the Queensland Department of Health, Australia. The Institute for Health Metrics and Evaluation receives funding from the Bill and Melinda Gates Foundation.
Declaration of Interest
None.
Ethical Standards
None. This research did not involve human or animal experiment = ation.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/gmh.2015.26.
click here to view supplementary material
References
- Altman DG, Gore SM, Gardner MJ, Pocock SJ (1983). Statistical guidelines for contributors to medical journals. British Medical Journal (Clinical Research ed.) 286, 1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2000). Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR). American Psychiatric Association: Washington, DC. [Google Scholar]
- Attanayake V, Mckay R, Joffres M, Singh S, Burkle FM, Mills E (2009). Prevalence of mental disorders among children exposed to war: a systematic review of 7,920 children. Medicine, Conflict and Survival 25, 4–19. [DOI] [PubMed] [Google Scholar]
- Baxter A, Vos T, Scott K, Ferrari A, Whiteford H (2014). The global burden of anxiety disorders in 2010. Psychological Medicine 44, 2363–2374. [DOI] [PubMed] [Google Scholar]
- Bruckner TA, Scheffler RM, Shen G, Yoon J, Chisholm D, Morris J, Fulton BD, Dal Poz MR, Saxena S (2011). The mental health workforce gap in low- and middle-income countries: a needs-based approach. Bulletin of the World Health Organization 89, 184–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman C, Mills K, Slade T, Mcfarlane A, Bryant R, Creamer M, Silove D, Teesson M (2012). Remission from post-traumatic stress disorder in the general population. Psychological Medicine 42, 1695–1703. [DOI] [PubMed] [Google Scholar]
- Charlson FJ, Steel Z, Degenhardt L, et al. (2012). Predicting the impact of the 2011 conflict in Libya on population mental health: PTSD and depression prevalence and mental health service requirements. PLoS ONE 7, e40593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson FJ, Ferrari AJ, Flaxman AD, Whiteford HA (2013). The epidemiological modelling of dysthymia: application for the Global Burden of Disease Study 2010. Journal of Affective Disorders 151, 111–120. [DOI] [PubMed] [Google Scholar]
- Charlson FJ, Diminic S, Lund C, Degenhardt L, Whiteford HA (2014). Mental and substance use disorders in Sub-Saharan Africa: predictions of epidemiological changes and mental health workforce requirements for the next 40 years. PLoS ONE 9, e110208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devries K, Mak J, Garcia-Moreno C, Petzold M, Child J, Falder G, Lim S, Bacchus L, Engell R, Rosenfeld L (2013). The global prevalence of intimate partner violence against women. Science 340, 1527–1528. [DOI] [PubMed] [Google Scholar]
- Ferrari AJ, Charlson FJ, Norman RE, Flaxman AD, Patten SB, Vos T, Whiteford HA (2013). The epidemiological modelling of major depressive disorder: application for the global burden of disease study 2010. PLoS ONE 8, e69637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flaxman AD, Vos T, Murray CJL (eds) (2013). An Integrative Metaregression Framework for Descriptive Epidemiology. University of Washington Press: Seattle. [Google Scholar]
- Global Burden of Disease Study 2013 Collaborators (2015). Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386, 743–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Health Metrics and Evaluation (2015). GBD Compare [Online]. (http://viz.healthmetricsandevaluation.org/gbd-compare/).
- Kalt A, Hossain M, Kiss L, Zimmerman C (2013). Asylum seekers, violence and health: a systematic review of research in high-income host countries. American Journal of Public Health 103, e30–e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karam EG, Friedman MJ, Hill ED, Kessler RC, Mclaughlin KA, Petukhova M, Sampson L, Shahly V, Angermeyer MC, Bromet EJ, De Girolamo G, De Graaf R, Demyttenaere K, Ferry F, Florescu SE, Haro JM, He Y, Karam AN, Kawakami N, Kovess-Masfety V, Medina-Mora ME, Browne MAO, Posada-Villa JA, Shalev AY, Stein DJ, Viana MC, Zarkov Z, Koenen KC (2014). Cumulative traumas and risk thresholds: 12-month PTSD in the world mental health (WMH) Surveys. Depression and Anxiety 31, 130–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Loannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009). The PRISMA Statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLOS Medicine 6, 1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter M, Haslam N (2005). Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: a meta-analysis. JAMA: Journal of the American Medical Association 294, 602–612. [DOI] [PubMed] [Google Scholar]
- Priebe S, Gavrilovic J, Bremner S, Ajdukovic D, Franciskovic T, Neri G, Kucukalic A, Lecic-Tosevski D, Morina N, Popovski M, Schutzwohl M, Bogic M, Matanov A (2012). Course of post-traumatic stress disorder following war in the Balkans: 1-year follow-up study. Psychological Medicine 43, 1837–1847. [DOI] [PubMed] [Google Scholar]
- Roberts B, Browne J (2011). A systematic review of factors influencing the psychological health of conflict-affected populations in low- and middle-income countries. Glob Public Health 6, 814–829. [DOI] [PubMed] [Google Scholar]
- Rodin D, Van Ommeren M (2009). Commentary: explaining enormous variations in rates of disorder in trauma-focused psychiatric epidemiology after major emergencies. International Journal of Epidemiology 38, 1045–1048. [DOI] [PubMed] [Google Scholar]
- STATACORP (2009). Stata Statistical Software: Release 11. StatCorp LP: College Station, Texas. [Google Scholar]
- Steel Z, Chey T, Silove D, Marnane C, Bryant RA, Van Ommeren M (2009). Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA: Journal of the American Medical Association 302, 537–549. [DOI] [PubMed] [Google Scholar]
- The Hofstede Centre (2014). National Culture [Online]. Available: http://geert-hofstede.com/dimensions.html Accessed 26 June 2014.
- United Nations. 2011. World Population Prospects - The 2010 Revision [Online]. New York. Available: http://esa.un.org/unpd/wpp/Excel-Data/population.htm.
- Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basáñez M.-G, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabé E, Bhalla K, Bhandari B, Bikbov B, Abdulhak AB, Birbeck G, Black JA, Blencowe H, Blore JD, Blyth F, Bolliger I, Bonaventure A, Boufous S, Bourne R, Boussinesq M, Braithwaite T, Brayne C, Bridgett L, Brooker S, Brooks P, Brugha TS, Bryan-Hancock C, Bucello C, Buchbinder R, Buckle G, Budke CM, Burch M, Burney P, Burstein R, Calabria B, Campbell B, Canter CE, Carabin H, Carapetis J, Carmona L, Cella C, Charlson F, Chen H, Cheng AT-A, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, De Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahiya M, Dahodwala N, Damsere-Derry J, Danaei G, Davis A, De Leo D, Degenhardt L, Dellavalle R, Delossantos A, Denenberg J, Derrett S, Des Jarlais DC, Dharmaratne SD, Dherani M, et al. (2012). Supplement to: years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2163–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, Charlson FJ, Norman RE, Flaxman AD, Johns N (2013). Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 382, 1575–1586. [DOI] [PubMed] [Google Scholar]
- World Health Organization (1992). The ICD-10 Classification of Mental and Behavioural Disorders. Clinical Descriptions and Diagnostic Guidelines. World Health Organization: Geneva. [Google Scholar]
- World Health Organization (2011). Project Atlas: Resources for Mental Health and Neurological Disorders [Online]. Available: http://apps.who.int/globalatlas/default.asp.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/gmh.2015.26.
click here to view supplementary material