Abstract
Background:
The impact of diabetes on health-care expenditures has been increasingly recognized. To formulate an effective health planning and resource allocation, it is important to determine economic burden.
Objective:
The objective of this study is to assess the cost of illness (COI) for diabetic inpatients with or without complications.
Methodology:
The study was conducted in the medicine wards of tertiary care hospital after ethical approval by the Institutional Ethical Committee. A total of 116 each diabetic with or without complications were selected and relevant data were collected using COI questionnaire and data were analyzed using SPSS version 20. Mann–Whitney U test is used to assess the statistical significant difference in the cost of treatment of diabetes alone and with complications’. P ≤ 0.05 was considered statistically significant.
Results:
Total COI includes the cost of treatment, investigation, consultation fee, intervention cost, transportation, days lost due to work, and hospitalization. The median of total COI for diabetic care without any complication was Rs. 22,456.97/- per patient per annum and with complication was Rs. 30,634.45/-. Patients on dialysis had to spend 7.3 times higher, and patients with cardiac intervention had to spend 7.4 times higher than diabetic patients without any complication.
Conclusion:
Treatment costs were many times higher in patients with complications and with cardiac and renal interventions. Complications in diabetic patients will increase the economic burden to family and also to the society.
KEY WORDS: Cost of illness, diabetes mellitus, diabetic complications, direct medical cost, economic burden
The demand for and hence the cost of health care are increasing in all countries as the improvement and sophistication of health technologies increase. Medicines form a small but significant proportion of total health-care costs and one that has been growing consistently as new medicines are marketed. Many governments are focusing their activities on promoting the effective and economic use of resources allocated to health care.[1]
Pharmacoeconomics can be defined as the measurement of both the costs and consequences of therapeutics decision-making. Pharmacoeconomics can assist in the planning process and help assign priorities where, for example, medicines with a worse outcome and lower cost can be compared with medicines with higher cost and better outcomes.[1] There are number of methods available for pharmacoeconomic assessment like cost-effectiveness analysis, cost of illness (COI), each of which will be used depending on the outcomes desired and interventions targeted.
The impact of diabetes on expenditure of health care has been increasingly recognized. A number of studies on “COI” have shown a 3 times raise in the direct costs of diabetic patients compared with nondiabetic patients in the different health-care systems. Recent studies have shown that people with diabetes are more likely to develop acute and chronic complications related to uncontrolled diseases. Moreover, these complications have impact on increase in the costs of hospitalization and drugs. The excess costs were mainly due to an increased hospital admission, costly outpatient's treatments, higher costs for nursing home care, and increased drug usage. Diabetes is closely associates with other chronic conditions, which further increase the cost of treatment, especially hypertension, lipid disorders, and cardiovascular disease.[2,3] In a study at Canada on the cost of management of diabetes, it has been reported that cardiovascular disease was the main risk factor to the direct cost of diabetes. Therefore, it has been suggested that prevention of cardiovascular disease in the patient with diabetes should become an imperative.[4] In India, cost studies in diabetes were conducted by the Kapur, Ramachandran, and Grover at Bengaluru urban district, Chennai, and North India, respectively. Whereas the present study was conducted in a major tertiary care hospital of Udupi district of South Karnataka. Many patients from rural area and nearby states were also getting treatment in this hospital. Although COI studies are done in India, it was not done in this locality. Furthermore, we wanted to compare the results of COI studies conducted in other parts of India.
Objectives
The objective of this study is to determine the COI for diabetic inpatients in South Indian tertiary care hospital.
Methodology
The study was conducted in the general medicine units of Kasturba Hospital, Manipal, after obtaining ethical approval from the Institutional Ethics Committee.
To collect the data, COI questionnaire was prepared by referring literatures to document relevant cost involved in the treatment of the diabetic patients.
The questionnaire was validated for suitability and appropriateness by a group of physicians and clinical pharmacists. It includes demographic of the patients such as age, sex, educational information, and occupation. It also contains direct medical cost such as cost of drugs, investigations, consultation, interventions and hospitalization, and direct nonmedical cost such as transportation and days lost from work.
The sample size for the study was calculated by absolute precision method. The expected rate of admission of diabetes patients in our hospital is approximately 7% of total admissions per year with a margin of error (precision) fixed at 5% and 95% confidence level. The sample size was calculated using nMaster version 2.0, Christian Medical College, Vellore, India. The calculated sample size was 100 patients. However, 116 patients were included in the study purpose.
A total of 116 each of diabetic patients with (any) or without complications admitted in the medicine wards in the year 2011 who were ready to give consent were interviewed and relevant data's were documented in validated COI questionnaire and evaluated for following parameters.
-
Demography of Type 2 diabetic patients with or without complications
- Gender-wise patient distribution
- Age group-wise patients distribution
- Body mass index (BMI) status of the patients
- Educational status of the patients
- Occupation of the patients
- Year of diagnosis of diabetes
- Regarding place of residence (urban/rural).
Complications status of diabetic patients with complications
Drugs used in the treatment of these patients
Various direct medical, direct nonmedical costs, and total cost involved in the diabetes care.
Statistical analysis
All the data were presented as descriptive statistics using SPSS version 20.0, IBM Corporation, New York, USA, as statistical software. Mann–Whitney U test is used to assess the statistical significant difference between the total costs involved in the treatment of diabetes alone and diabetes with complications. P < 0.05 was considered statistically significant.
Results
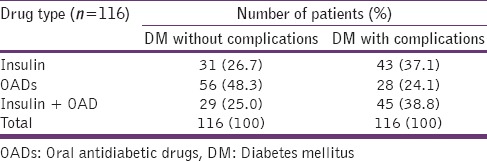
Demographic/social characteristic of the diabetic patients
For the study purpose, patients were categorized into two groups: diabetic patients without complications and diabetic patients with complications. A total of 116 subjects were enrolled in both the groups. Various demographic and social characteristics of diabetic patients such as gender-wise distribution, age group-wise distribution, and BMI of the diabetic patients, educational status, occupational status, duration of diabetic history, and residential status of the patients are represented in Tables 1 and 2.
Table 1.
Demographic characteristics of diabetic patients
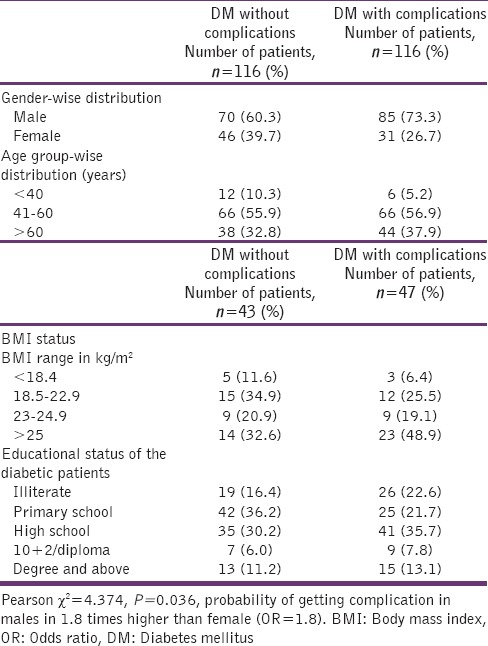
Table 2.
Socioeconomic characteristic of the diabetic patients
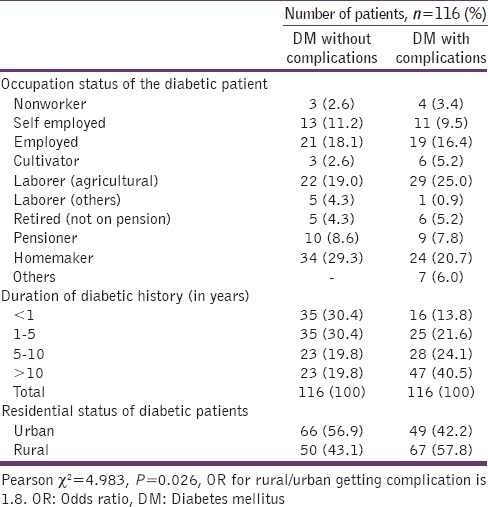
Diabetic complications
Among 116 diabetes mellitus (DM) patients with complications, 43 (37.1%) had microvascular complications, 16 (13.8%) had macrovascular complications, 50 (12.9%) had infections, 23 (19.8%) had microvascular complication and infections, 9 (7.8%) had combination of micro- and macro-vascular complications, and 10 (8.6%) had combination of macrovascular complication and infection. Data are presented in Table 3.
Table 3.
Diabetic complications
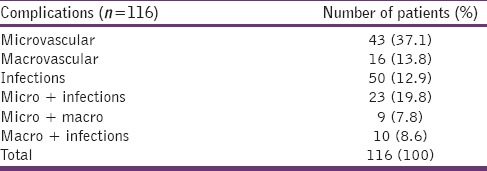
Types of drugs prescribed
On the evaluation of management of diabetes, out of 116 patients without complications, 31 (26.7%) patients received insulin alone, 56 (48.3%) patients received oral antidiabetic drug (OAD) alone, and 29 (25.0%) patients received both insulin and OADs.
Among 116 DM patients with complications, 43 (37.1%) received insulin alone, 28 (24.1%) were received OADs, and 45 (38.8%) received both insulin with OADs. Data are presented in Table 4.
Table 4.
Types of drugs prescribed
Cost of illness
Various components of cost in terms of Indian Rupees (Rs.) for diabetic without complications and diabetes with complications for patients who are admitted in the medicine wardsare given in the following tables with its median and inter quartile range (IQR).
Direct costs
Direct medical cost
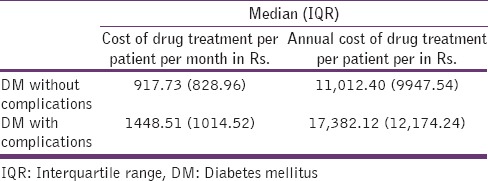
It includes the cost of medications required for each month per patient. On average, diabetic patient without complications spend Rs. 917.73 compared to the diabetic patients with complications who spends on an average of Rs. 1448.51 per month. Annual cost of drug treatment per patient with or without diabetes is represented in Table 5. Annual cost of medication is 1.6 times higher for diabetes with complication compared to diabetic patients without complications.
Table 5.
Cost of drug treatment per month per patient
Annual cost of insulin, oral antidiabetic drugs, and insulin plus oral antidiabetic drugs per patients
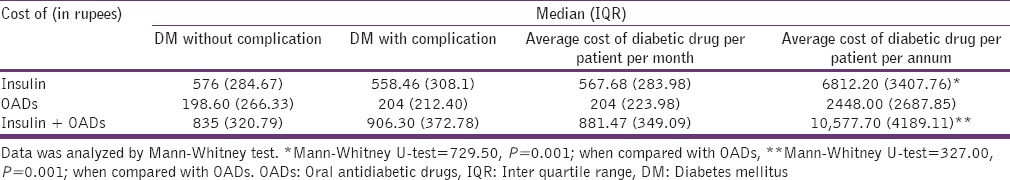
Annual cost of therapy per patient, who are on insulin alone, OADs alone and insulin with OAD combination in the both the groups is given in the Table 6. Patients who were on insulin had to spend 2.8 times higher, and patients who were on insulin plus OADs have to spend 4.3 times higher than patients who were on OADs alone.
Table 6.
Cost of insulin, oral antidiabetic drugs, and insulin plus oral antidiabetic drugs per patients per month
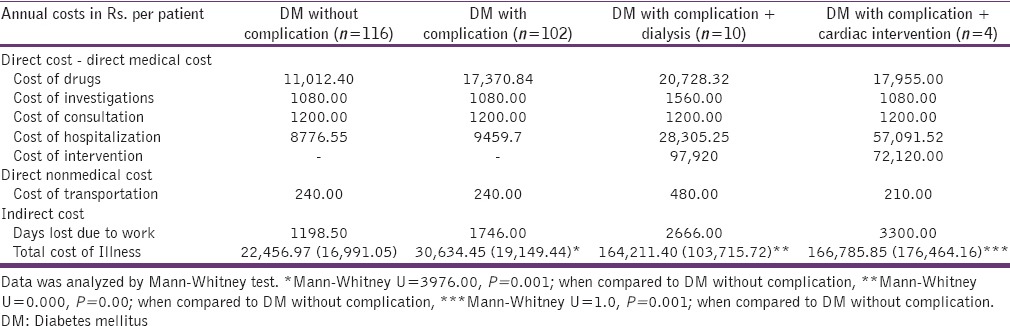
Total cost of illness or total cost of diabetic care per patient
Total COI includes all the cost of treatment, investigation, consultation fee, intervention cost, transportation, days lost due to work, and hospitalization. Table 7 describes COI for patient groups such as diabetic patients without or with complications and groups having additional interventions such as dialysis and cardiac interventions. Common complications of diabetes include peripheral neuropathy and infections. COI for DM with complication is 1.4 times higher than those without complications. Those patients who undergo dialysis in addition to the complications spend 7.3 times higher than those without complications. Patients who undergo cardiology intervention along with complications spend 7.4 times higher than patients who do not have complications. All the values are represented in either in median or median with IQR.
Table 7.
Annual cost of Illness of diabetes care per patient
Discussion
An increase in the prevalence of diabetes all over the worldwide due to raise in population, aging, urbanization, and lifestyle changes that is physical inactivity results in an increase of obesity. Unlike in the West, where older people are the most affected, diabetes in Asian countries, it is high in the young to middle-aged adults. This could have long-lasting adverse effects on a nation's health and economy, especially for developing countries. According to the fifth report of the International Diabetes Federation, the second highest numbers of diabetics are present in India.[5] The increase in the prevalence of Type 2 diabetes produces a major clinical, economic, and societal burden in India. The cost of diabetes care is more and is increasing worldwide.[6]
Recently, many studies on the impact of diabetes on cost concluded three major observations. First, diabetes imposes a financial burden on people with diabetes and their families. Second, diabetes leads to loss in productivity and economic growth. Last, the highest economic burden caused by diabetes is the monetary value associated with disability and loss of life as a result of the disease itself and its related chronic complications.[7] The present study is aimed at assessing the cost of diabetes care with or without complications. In this study, 116 diabetes patients with complications and 116 patients without complications were enrolled. Among them, majority were males, 60.3% in without complication group, and 73.3% in the complication group. The study showed that probability of getting complications in males (P = 0.036) is 1.8 times higher than in female (odds ratio is 1.8). Approximately 80% of diabetic patients in both the groups were above 40 years. Moreover, majority of them were in the age group of 40–60 years, namely, 55.9% in noncomplication group and 56.9% in with complication group.
Diabetes has long been linked to obesity and being overweight. Obesity causes insulin resistance and thereby DM.[8] In our study, we observed that 53% of diabetic patients without complications were overweight or obese and in diabetes with complication group, 68% of patients were either obese or overweight. Boffetta et al. reported that there is a strong association between BMI and the prevalence of diabetes in Asian populations.[9]
When we observed, the education background, we found that 80% of diabetic patients in the both the groups were below high school education and some were illiterate. Many socioeconomic factors such as education and occupation will affect the time of diagnosis and thus the outcome of diabetes and cost of management. The diagnosis was delayed by 3–7 years in the less-educated and illiterate division of the population according to the cost of diabetes in India (CODI) study.[10] The age of diagnosis was directly related to the level of education: Educated people were diagnosed 7 years before people with no literacy. Moreover, diabetes-related complications are less in educated people despite of longer duration of disease compared to low or no literacy. Education appears to play a role in the development of diabetes complications. For people with a similar duration of diabetes, 45% of those who finished higher education had no complications, compared to 20% for the no-literacy group.[11]
Although in our study, unemployed people were very few, many of them were laborers and house wives. Symptoms produced by Type 2 diabetes are often weakness and tiredness. This can be ignored by unemployed people, but those working are more likely to recognize these symptoms as these influence their efficiency in the work. Among people with similar diabetes duration, less complications are observed in people with higher socioeconomic group compared to the lower socioeconomic group.[11]
Regarding the duration of diabetes in the study population, 60.8% diabetic patients in without complication group had <5 years of history of diabetes, whereas in diabetes with complication group, 64.6% of diabetic patients had above 5 years of history of disease.
In the present study, diabetic patients were from both urban and rural areas. Majority from rural area (57.8%) were in the group DM with complications. When we studied the association between complication and status of residence, there is an association between complications of diabetes and residential status (P = 0.026). The odds ratio of rural/urban is 1.8. It means chances of getting complications in rural diabetic patients are 1.8 times higher than urban population. In the prevalence of diabetes in India study, reported prevalence of diabetes based on the WHO criteria was 5.6% and 2.7% among urban and rural areas, respectively.[12] Reports from various parts of India showed further raise in the prevalence of diabetes in urban areas. Moreover, the diabetes prevalence was also found to be increasing rapidly in rural areas as a result of the recent socioeconomic transitions.[13]
In the CODI study, it was reported that people in urban area diagnosed early compared to rural areas. Even place of residence plays an indirect role in the development of diabetic complications. People with diabetes living in the semi-urban or rural areas have higher rates of complication - despite less duration of diabetes - than those in urban areas.[14]
In the present study, we observed that majority of DM patients without complications were on oral anti-diabetic drugs, i.e., 48.3%. Those who had complications were either on insulin (37.1%) or on Insulin with OADs (38.8%). This may be due to the severity of their disease. Among complications, majority of them had microvascular complication (37.1%). 8 patients were on dialysis and 4 patients had cardiac intervention.
The CODI study was a large community-based survey of diabetes, and it showed that ambulatory care constitutes 65% cost; whereas hospitalization costs 35% and therapy costs 31% of which specific anti-diabetic drug cost was only 17%. Ambulatory care included monitoring and doctor visits constituting 34% of cost.[14] In a study conducted by Grover et al. in North India reported that the total cost of diabetes was estimated at 14517.42 rupees per person annually. Moreover, the direct cost of care of diabetes was estimated to be 71.25% of the total cost; indirect cost was 28.75%, and providers cost was 2.83% of the total cost. The greatest amount of money was spent by the patients to buy the drugs that are 42.38% of total cost.[15]
Ramachandran et al. and others reports that the average annual expenditure of those who attend the specialty center is quite high averaging from Rs. 3000 to Rs. 48,000 depending upon the center where patients are treated or type of complications they have.[16,17,18,19]
In the present study, we calculated direct medical cost, which includes the cost of drugs, investigations, consultation, hospitalization, and any intervention cost. Direct nonmedical cost which includes the cost of transportation and indirect cost which include days lost due to work. Finally, total COI for diabetes without complication, with complication, with dialysis, and with cardiac intervention was calculated.
Under direct medical cost, median annual drug treatment cost was Rs. 11,012.40 for DM without complication and Rs. 17,382.12 for DM with complication, which is 1.7 times higher than cost of drug treatment for DM without complication. Diabetic patient who are on insulin and OADs has to spend 2.8 times and 4.3 times more, respectively than who are on OADs alone.
Hospitalization charge was 1.2 times higher for DM with complications. For any DM patients on dialysis (usually 2 times per week), they have to spend Rs. 97,920.00 per annum. DM patients, who underwent cardiac intervention, had to spend median of Rs. 72,120.00 per intervention. It showed that annual cost of treatment for those who were on dialysis was 6.8 times higher, and annual cost of treatment for cardiac intervention was 5 times higher than patients who did not have any intervention. Moreover, there may not be much difference in the cost of investigations, consultation cost, transportation, and indirect cost involved in diabetic care.
We found that total COI for diabetic care without any complication was Rs. 22,456.97/- per patient per annum. Median of total COI for diabetic care with complication was Rs. 30,634.45/- per patient per annum, it was 1.4 times higher, median of COI for diabetic care with complication plus dialysis was Rs. 164,211.40/-per patient per annum, it is 7.3 times higher and the median COI for diabetic care with complication plus cardiac intervention was Rs. 166,785.85/- per patient per annum which is 7.4 times higher and statistically significant difference observed between these groups. A similar study conducted by Metgud[20] showed that cost of outpatient care for diabetic patient with chronic renal failure (CRF) requiring dialysis was 15 times higher than the cost of outpatient care for a diabetic patient without CRF (excluding dialysis cost). Grover et al.[15] reported that total annual cost of diabetic care was Rs. 14.508. It was reported that by Kapur et al. that complications were responsible for most of the diabetes-related direct health costs in India.[11]
The studies have reported the cost of managing diabetic patients with or without microvascular and macrovascular complications. Patients with microvascular complications had higher the cost of management, and those with macrovasular complications had even higher cost of management. Patients with both microvascular and macrovascular complications had highest cost compared with those without these complications.[14,16,21,22,23]
Difference in the cost and proportions in different studies may be due to the period of study, place, method of collecting the data, and economic values. However, all the studies have concluded that diabetes is a costly disease, and diabetes complication makes it more costly. It is not only a burden to the patient, his family but also to the nation. The cost of diabetes increases manifolds with complications. When it comes to complications, the poor people in the urban and rural areas are more vulnerable because of the delay in diagnosis of the condition and incomplete follow-up and treatment. These groups are also economically vulnerable when they develop diabetes complications. As our country still does not have universal health coverage, it is important to target interventions to these groups in terms of accessibility to education, training, investigation tests, and medications to manage diabetes effectively.
Conclusion
In this study, COI of diabetes patients with and without complications were compared. The total cost of treatment per annum in patients without complications was Rs. 22,457/- compared to Rs. 30,634/- in patients with complications. Cost was 7.3 times higher with renal complications and 7.4 times higher with cardiac intervention. It shows that cost of diabetes care is high and escalating. Treatment costs were many times higher in patients with cardiac and renal complications. Complications in diabetic patients will increase the economic burden to family and also to the society. Findings of this study highlight need for early identification and prevention of complications to control the cost of management in diabetes patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank Head of all medicine units of Kasturba Hospital, Manipal, for allowing collection of the data from their patient.
References
- 1.Cooke J. Pharmacoeconomics. In: Roger W, Cate W, editors. Clinical Pharmacy and Therapeutics. 4th ed. London: Churchill Livingstone, Elsevier; 2007. pp. 101–7. [Google Scholar]
- 2.Rathmann W, Haastert B, Roseman JM, Gries FA, Giani G. Prescription drug use and costs among diabetic patients in primary health care practices in Germany. Diabetes Care. 1998;21:389–97. doi: 10.2337/diacare.21.3.389. [DOI] [PubMed] [Google Scholar]
- 3.Wang W, Fu CW, Pan CY, Chen W, Zhan S, Luan R, et al. How do type 2 diabetes mellitus-related chronic complications impact direct medical cost in four major cities of urban China? Value Health. 2009;12:923–9. doi: 10.1111/j.1524-4733.2009.00561.x. [DOI] [PubMed] [Google Scholar]
- 4.Dawson KG, Gomes D, Gerstein H, Blanchard JF, Kahler KH. The economic cost of diabetes in Canada, 1998. Diabetes Care. 2002;25:1303–7. doi: 10.2337/diacare.25.8.1303. [DOI] [PubMed] [Google Scholar]
- 5.Ramachandran A, Das AK, Joshi SR, Yajnik CS, Shah S, Prasannakumar KM. Current status of diabetes in India and need for novel therapeutic agent. J Assoc Physicians India. 2010;58:7–9. [Google Scholar]
- 6.Ramachandran A. Socio-economic burden of diabetes in India. J Assoc Physicians India. 2007;55(Suppl):9–12. [PubMed] [Google Scholar]
- 7.Mazid MA. On Economic Impact of Diabetes. The Financial Express. Views and Analysis: [Diabetes Awareness Day] 2012. Feb 28, [Last cited on 2012 Nov 15]. Available from: http://www.thefinancialexpress-bd.com/more.php?news_id=121542 and date=2012-02-28 .
- 8.Triplitt LC, Reasner CA. Diabetes mellitus. In: Dipiro JT, Talbert RL, Yee GC, Matzke G, Barbara W, Posey LM, editors. Pharmacotherapy A Pathophysiologic Approach. 8th ed. New York: The McGraw-Hill; 2011. [Google Scholar]
- 9.Boffetta P, McLerran D, Chen Y, Inoue M, Sinha R, He J, et al. Body mass index and diabetes in Asia: A cross-sectional pooled analysis of 900,000 individuals in the Asia Cohort Consortium. PLoS One. 2011;6:e19930. doi: 10.1371/journal.pone.0019930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kapur A. Cost of Diabetes in India-The CODI Study Paper Presented at the Novo Nordisk Diabetes Update. 2000 [Google Scholar]
- 11.Kapur A, Bjork S, Nair J, Kelkar S, Ramachandran A. Socio-economic determinants of the cost of diabetes in India. Diabetes Voice. 2004;49:18–21. [Google Scholar]
- 12.Mohan V, Sandeep S, Deepa R, Shah B, Varghese C. Epidemiology of type 2 diabetes: Indian scenario. Indian J Med Res. 2007;125:217–30. [PubMed] [Google Scholar]
- 13.Ramachandran A, Snehalatha C. Current scenario of diabetes in India. J Diabetes. 2009;1:18–28. doi: 10.1111/j.1753-0407.2008.00004.x. [DOI] [PubMed] [Google Scholar]
- 14.Kapur A. Economic analysis of diabetes care. Indian J Med Res. 2007;125:473–82. [PubMed] [Google Scholar]
- 15.Grover S, Avasthi A, Bhansali A, Chakrabarti S, Kulhara P. Cost of ambulatory care of diabetes mellitus: A study from North India. Postgrad Med J. 2005;81:391–5. doi: 10.1136/pgmj.2004.024299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramachandran A, Ramachandran S, Snehalatha C, Augustine C, Murugesan N, Viswanathan V, et al. Increasing expenditure on health care incurred by diabetic subjects in a developing country: A study from India. Diabetes Care. 2007;30:252–6. doi: 10.2337/dc06-0144. [DOI] [PubMed] [Google Scholar]
- 17.Shobhana R, Rama Rao P, Lavanya A, Williams R, Vijay V, Ramachandran A. Expenditure on health care incurred by diabetic subjects in a developing country – A study from Southern India. Diabetes Res Clin Pract. 2000;48:37–42. doi: 10.1016/s0168-8227(99)00130-8. [DOI] [PubMed] [Google Scholar]
- 18.Kapur A. Cost of diabetes in India – The CODI study. In: Kapur A, Joshi JK, editors. Proceedings of the Novo Nordisk Diabetes Update. Bangalore: Healthcare Communications Ltd; 2000. pp. 71–7. [Google Scholar]
- 19.Rayappa PH, Raju KN, Kapur A, Bjork S, Sylvest C, Kumar KM. The Bangalore urban district diabetic study: Economic cost of diabetes care. Indian J Diabetes Dev Ctries. 1999;19:87–96. [Google Scholar]
- 20.Metgud CS. A Study of Diabetes Mellitus Type 2 Patients Visiting Kasturba Hospital, Manipal with Referenceto the Economics Involved in the Management.[MD Thesis] Manipal, Karnataka: Manipal Academy of Higher Education – A Deemed University; 2003. [Google Scholar]
- 21.Al-Maskari F, El-Sadig M, Nagelkerke N. Assessment of the direct medical costs of diabetes mellitus and its complications in the United Arab Emirates. BMC Public Health. 2010;10:679. doi: 10.1186/1471-2458-10-679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tharkar S, Devarajan A, Kumpatla S, Viswanathan V. The socioeconomics of diabetes from a developing country: A population based cost of illness study. Diabetes Res Clin Pract. 2010;89:334–40. doi: 10.1016/j.diabres.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 23.Bahia LR, Araujo DV, Schaan BD, Dib SA, Negrato CA, Leão MP, et al. The costs of type 2 diabetes mellitus outpatient care in the Brazilian public health system. Value Health. 2011;14(5 Suppl 1):S137–40. doi: 10.1016/j.jval.2011.05.009. [DOI] [PubMed] [Google Scholar]


