Abstract
On July 6th 2013, a train derailment occurred in the small town of Lac-Mégantic, Quebec, Canada, causing a major human and environmental disaster. In this case study, we comprehensively describe and analyze actions taken by the Public Health Department of the Eastern Townships, in close collaboration with community-based organizations, during both the impact phase emergency response and the post-impact recovery operations that continued for months. Due to the complexity of the event, public health actions needed to be broadly diversified. Preventive measures targeted chemical, physical, biological, and psychosocial hazards in the short-, medium- and long-term. Our analyses yielded valuable lessons that will improve and inform our response to future events while serving as a basis for developing a conceptual framework for public health emergency preparedness.
Keywords: anthropogenic disaster, disaster cascade, human-generated disaster, rail disaster, risk landscape, transportation disaster, technological disaster
In the middle of the night of July 6, 2013, an unmanned Montreal Maine and Atlantic Company oil train with no engineer at the controls spontaneously began rolling downhill from its night stop location – on the main line near Nantes - toward the town of Lac-Mégantic approximately 11 km away. Lac-Mégantic (population: 6,000 residents) is the seat of the Regional County Municipality (RCM) of Le Granit, one of 7 RCMs in the Eastern Townships region of Quebec, Canada. The town of Lac-Mégantic is situated on the shores of Lac-Mégantic from which the community derives its name. The lake forms the historic center and the heart of Lac-Mégantic's downtown and also serves as the origin of the Chaudière River that flows through the town and then northward for 175 km before emptying into the St. Lawrence River (Fig. 1).
Figure 1.
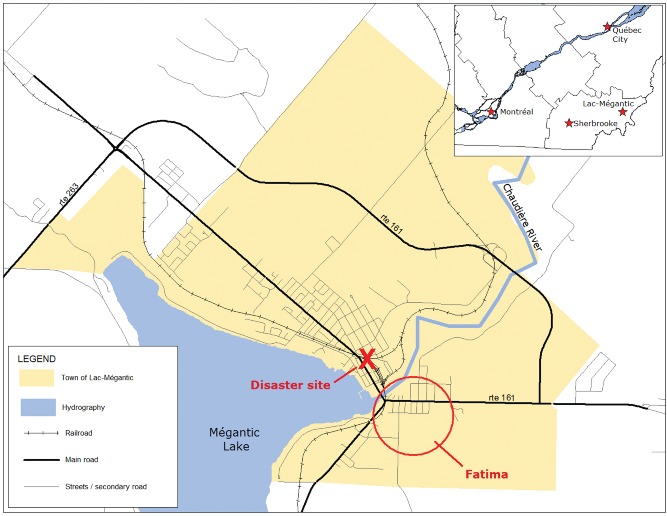
Map of Lac-Mégantic, Quebec, Canada.
The train was in motion, powered by gravity. Behind the 5 head-end locomotives was a Locotrol equipment car, a loaded boxcar, and 72 oil tank cars filled with Bakken formation crude oil – 79 units in all. With a relatively constant downhill slope between its initial location and Lac-Mégantic, the train's descent accelerated to almost 100 kph by the time the locomotives encountered a sharp curve in downtown Lac-Mégantic and most of the trailing cars derailed. The coupled tank cars ended their trajectory, splayed alongside the tracks in an accordion-like manner, sandwiched against one another (Fig. 2).
Figure 2.

Aerial photograph of the train derailment in downtown Lac-Mégantic (July 6th 2013). Source: Railway Investigation Report R13D0054. Transportation Safety Board of Canada.
As they derailed, multiple tank cars ruptured and escaping crude oil ignited, leading to a succession of powerful explosions and a raging conflagration. A dense cloud of smoke rose above the flames and the dark plume remained visible throughout the night and the next day. The fire spread rapidly to nearby structures, destroying 40 homes and businesses, and triggered a prolonged power outage. The Lac-Mégantic derailment and explosion resulted in 47 deaths and necessitated the mass evacuation of 2,000 persons, equivalent to one-third of the town's population.
Environmental contamination was a prominent feature in the post-disaster landscape. Each tank car had the capacity to haul 100,000 liters of light crude oil. The perforated tank cars disgorged an estimated 6 million liters of oil, much of which caught fire and burned, or seeped into the soil, but about 100,000 liters spilled into the waters of the Mégantic lake and the Chaudière River. As a complicating feature, the area experienced a heat wave in the days immediately following the train crash, adding to the environmental stressors experienced by the response personnel.
Coupled with the human suffering and the environmental degradation, the Lac-Mégantic derailment also caused serious social and economic consequences. Many citizens lost their jobs (temporarily or permanently) and many local businesses – including some that had been spared destruction – closed for months before relocating elsewhere in town.
For public health professionals, one question immediately became paramount: How should the regional Public Health Department respond to this tragedy? An ongoing challenge for public health practitioners is defining what it means to be prepared and how to best anticipate and respond during and after an acute event that endangers the community's collective health, such as the Lac-Mégantic train derailment. This requires an emergency preparedness and response framework.
Lesson 1: At the federal level, no public health emergency preparedness framework has identified essential elements applicable to Canada. In Canada, in contrast to the United States, public health addresses population-level preparedness, distinct from clinical care and health care facility preparedness.1 There is an urgent need for a national framework, applicable to the Canadian context, to guide public heath actions before, during, and after a disaster. Such a framework could help local authorities better handle challenges specific to major disasters when response must be rapid and timely, matched to the magnitude of the event, and well-coordinated.
Despite the absence of a comprehensive national framework, The Quebec Civil Protection Act aims to protect people and property through risk reduction measures, emergency response planning, response operations in actual disasters or situations of imminent threat, and recovery operations.2 It is structured with different missions corresponding to event-specific needs that allow the necessary flexibility to adapt response to a variety of types of disasters. Each mission falls under a ministry or a government organization with the appropriate expertise. Public health is a component of the health mission, under the jurisdiction of the Ministry of Health, and encompasses 4 core functions: surveillance, health protection, disease prevention, and health promotion.3
Emergency Response Operations Phase: July – August, 2013
Given the impact of this extreme event on the community's population, the involvement of public health personnel and resources was critical throughout the emergency response operations. The regional Public Health Department responded immediately, within the first hours, to provide direct services that were needed to protect the citizens of Lac-Mégantic and the on-site responders from health hazards, including exposure to chemical, physical, and biological agents (Table 1).
Table 1.
Public health actions in the immediate aftermath of the Lac-Mégantic train derailment
| Potential threats | Sources | Health effects | Preventive actions |
|---|---|---|---|
| Chemical | |||
| Toxic cloud (PAH, NOx, TSP, PM2.5, PM10) | Outdoor air (near the crash site) | Eye or respiratory tract irritation |
|
| Soot fallout | Surfaces, including surface water (near the crash site) | Skin irritation or cancer risks |
|
| Oil vapors (VOC, benzene, CO) and dust from debris (asbestos, PM10) | Outdoor air (at the site – risks to onsite workers) | Central nervous system depression, respiratory tract irritation or cancer risks |
|
| Oil spilt on the ground (C10-C50, BTEX, PAH) | Surfaces (at the site - – risks to onsite workers) | Eye or skin irritation |
|
| Oil seepage into the soil (benzene, CO) | Indoor air (basements around the site) | Central nervous system depression or asphyxia |
|
| Oil seepage into the soil (C10-C50, BTEX, PAH) | Drinking water (aqueduct network) | Cancer risks |
|
| Oil spilt into the lake and river (C10-C50, BTEX, PAH) | Drinking and recreational water | Cancer risks |
|
| Physical | |||
| Building collapse and explosions | Working environment | Injuries |
|
| Heat wave | Working environment | Heat stroke and exhaustion |
|
| Biological | |||
| Bacteriological contamination due to water main break | Drinking water (aqueduct network) | Bacterial gastroenteritis |
|
| Bacteriological contamination due to power outage | Perishable food | Bacterial gastroenteritis |
|
This initial public health response was provided within a particularly challenging context. Operating in Lac-Mégantic, a long distance from the home office in Sherbrooke, with a skeleton staff during the peak summer vacation period, the regional Public Health Department needed to deliver a time-urgent response to a devastated community and facilitate close coordination among involved partners, while under constant and intensive mass-media scrutiny.
Coordination of a multi-sectoral response
In the first weeks, partners from national, regional, and local levels converged on the scene. Prominent partners included municipal leaders; fire services personnel; criminal investigators; coroners and environmental services, health, and social services professionals. The Ministry of Civil Protection provided overarching coordination. Each of the partners arrived with different priorities and their diverse skills needed to be melded in a manner that facilitated timely and constructive information sharing, decision-making, and joint communications to public and professional audiences. Within the realm of public health, a variety of actors were involved including the national Ministry of Health, the national public health expertise center (Institut National de Santé Publique du Québec), 2 regional Public Health Departments, and the local health and social services center. Together these partners needed to craft a concerted response.
The public health emergency response addressed several short-term health issues. Our priority at that time was to assess and control health risks associated with the environmental impact. This obviously necessitated identifying the chemical products involved.
Lesson 2: Although the civil protection partners immediately briefed public health professionals – verbally – about the contents of the tank cars, it was very difficult to obtain accurate, confirmatory documentation (documents were withheld because they were considered as evidence for the ongoing criminal investigation). With regard to the timely sharing of sensitive information, agreement among key partners should be settled prior to the occurrence of future disasters.
Risk assessment of citizens, response personnel, and the environment
Another challenge was the need to conduct simultaneous risk assessments for various populations of affected citizens including Lac-Mégantic residents who were evacuated and reintegrated, Lac-Mégantic citizens who were exposed to the cloud of smoke, and populations from the municipalities along the oil-contaminated river. Concurrently, risk assessments were performed for on-site responders and clean-up personnel including firefighters, police, decontamination team members, railway specialists, and contractors.
A major focus of the risk assessment was on a variety of potential hazardous exposures including:
outdoor air contamination at the derailment site and nearby;
indoor air contamination (especially in basements) of evacuated residences;
drinking water contamination from the municipal water system and private wells;
recreational water contamination in the lake (Lac-Mégantic) and the Chaudière River;
soil contamination at the derailment site and nearby;
contamination of surfaces located under the toxic cloud.
Evacuation and reintegration of Lac-Mégantic citizens
Early in the morning of July 6, 2013, about 1,000 residents whose residences were close to the derailment site and the intense fires were pre-emptively evacuated by firefighters to create a large safety perimeter. At 8:30 AM, initial air quality samples were gathered from the disaster site and surrounding area by a mobile laboratory from the Ministry of Environment and results were transmitted to the Public Health Department around 10:00 AM.
Elevated concentrations of polycyclic aromatic hydrocarbons (PAH), nitrogen oxide, and total suspended particles (TSP) were detected in the Fatima sector, downwind from the disaster site. This sector had not been previously evacuated because it was located outside the established fire hazard perimeter (Fig. 1). However, due to the detection of hazardous levels of contaminants, the Medical Health Officer immediately requested the evacuation of an additional 1,000 residents located in the Fatima sector, including persons with cognitive disorders living in a private senior residence. Confirmatory laboratory data received later in the day (e.g. total PAH > 1,000 ng/m3) supported the timely evacuation decision. Moreover, the decision to evacuate proved to be especially appropriate because the fires continued to burn until July 8, 2015, 2 d later.
Lesson 3: No specific guideline values have been specified for mixtures of compounds like total PAH and TSP. A major challenge faced by the Public Health Department was to rapidly interpret the initial air quality data and to request citizen evacuation in the absence of available guidelines regarding risk thresholds for mixtures of multiple contaminants. A guide to safety thresholds for a range of contaminants should be created and available at all times for public health physicians on duty.
The Public Health Department describes the process of returning evacuated citizens to their homes as “reintegration.” Reintegration required consensus among partners with the Public Health Department playing a pivotal role in assessing health risks, a key component for ensuring citizen safety. The earliest reintegration activities were initiated by law enforcement without Public Health Department involvement but this oversight was rapidly corrected. Thereafter, the Public Health Department conducted a health risk assessment, and provided information and recommendations for returning residents, prior to their reintegration (Lesson 4). Sectors closest to the “ground zero” derailment site required more time prior to reintegration. In fact, 2 y following the derailment, access to one heavily contaminated area continues to be restricted for both residents and business operators.
Lesson 4: Partners, including the Public Health Department, need to collaborate effectively during a disaster. Misunderstandings regarding respective roles and responsibilities may hamper operations. Ideally, partner operations should be well coordinated prior facing the challenges of a real tragedy. This can be facilitated through joint emergency preparedness planning and exercising on an ongoing basis.
Epidemiological investigation
In the context of real or apparent chemical, physical, or biological threats to population health, the Public Health Department initiated an epidemiological investigation starting within the first week. The investigation included case-finding (“case declarations”) in area emergency rooms and local medical clinics. Occupational health teams were mobilized in all regions. All occupational safety and health incidents affecting disaster workers, and all potential hazardous exposures for residents of Lac-Mégantic or surrounding municipalities, were rapidly reported to the Public Health Department using a declaration form. One dozen cases of possible exposure to chemical contaminants were reported, with the majority of these cases occurring in responders. There were no severe cases. Presenting symptoms included headache, weakness, difficulty breathing, and eye irritation. Symptoms could be traced to accidental inhalation of oil fumes (5 cases), accidental projection of liquid (3 cases), and exhaustion (4 cases).
Risk communication
Risk communication, based on the Quebec risk management framework,4,5 was a key component of the public health emergency response. Multiple factors were found to increase perceived risk for health consequences on the part of citizens of Lac-Mégantic6,7 Risk perception was related to the nature of event and the degree of exposure to hazardous materials. The event combined the elements of a runaway train derailment in a downtown area that precipitated a cascade of explosions and a massive fire of extreme intensity that required 2 d to extinguish, combined with hazardous materials contamination of air, water, and soil.
This train crash was appropriately characterized as human-generated, involuntary, uncontrollable, unpredictable, and unfamiliar. Moreover, the incident appeared to produce an inequitable distribution of risks and benefits. Citizens expressed understandable suspicion and distrust of institutions (government, railway system). The degree of media attention was both overwhelming and distressing. Perceived risk was also related to the dramatic and fear-provoking impact phase, the violent of loss of life, and the enduring health effects. The event was catastrophic, with both identifiable and unrecovered victims, premature death of young citizens, severe and sometimes irreversible injuries, population exposure to hazardous materials, and potential, though poorly defined, health risks for future generations.
Risk communications employed several channels to reach the general public and the disaster workers. Press conferences were conducted every day, beginning on the first day. This daily briefing was supplemented with timely press releases, expert media interviews, and informational meetings for both citizens and disaster workers. A handout was developed on occupational safety and health for disaster workers. A second handout, available in both print and online formats, provided guidance for citizen reintegration following protective evacuation. Upon review it was determined that this handout was somewhat difficult to read for people with low literacy skills,8 a relevant issue in the Granit RCM where the educational attainment level for half of adults (51.2%), ages 25–64, is a high-school diploma or less.9,10 Another lesson learned focused on the competing demands for communicating to the local population during a disaster of national significance and international publicity. For the first 2 days, the Public Health Department experienced intense media pressure from journalists and networks from throughout the nation and around the globe that converged on Lac-Mégantic to cover the story. Dozens of press conferences were convened but local communications suffered as a result. Thereafter the Public Health Department consciously shifted its media strategy to prioritize communications directed toward affected citizens using local radio and direct outreach.
Lesson 5: The most affected residents did not have access to television or Internet because of the power outage and the evacuation of one-third of the population from their homes. Local radio, person-to-person communications, and door-to-door distribution of printed informational materials were judged to be more effective for information sharing to affected citizens than regional or national media. The Public Health Department must maintain expertise and skills in crisis communication and should prepare event-specific written documents for the general population in advance and during a disaster.
The Recovery Operations Phase: September 2013 – present
Disaster recovery subsumes the overall decisions and actions taken following a disaster to restore the social, economic, physical, and environmental conditions of the community and to decrease future disaster risks.11 The operational domain of Public Health extends beyond health protection to also include health promotion and prevention of diseases, psychosocial problems, and injuries; therefore, the participation of the Public Health Department is integral throughout the recovery operations phase (Table 2).
Table 2.
Public health actions in the months following the Lac-Mégantic train derailment
| Component of recovery | Brief description of actions |
|---|---|
| Coordination | Regular discussions with local partners (e.g. health care network, municipality) and interdisciplinary government partners (e.g., environment and municipal affairs). |
| Health surveillance | Surveillance system based on set of several health indicators to keep track of the potential after-effects of the tragedy. Health diagnosis was sent to partners quarterly. |
| Research | Random survey among 811 adults in Granit, one year following the tragedy, examining prevalence of health and psychological issues according to the level of exposure to the tragedy (in terms of human losses, material losses, and negative perceptions). A similar survey with an improved version of the questionnaire will be conducted in 2015, i.e. 2 y after the tragedy. Collaboration to a mixed methods study (Social Sciences and Humanities Research Council Grant, 2015–2020) that will provide in-depth exploration of the consequences of such disasters and ways to enhance the well-being of survivors and the affected community. This study aims to better understand the recovery process and factors positively or negatively associated with personal and community resilience for people exposed to disaster stressors. |
| Community development | Support of local leaders and partners. Mentoring and sharing expertise to promote local initiatives, stimulate the redevelopment of the community, and promote resilience in the wake of the train derailment. |
| Occupational health | Both the physical health and psychological health of workers were considered. In the first month after the event, more than 24 of 39 (62%) of the workers compensation claims related to the train derailment involved psychological injuries. Workplace psychosocial interventions targeted 3 components: post-traumatic stress disorder (PTSD), suicide prevention, and psychosocial risks/organizational factors. |
| Environmental health | Continuous interpretation of the results of analyses performed at different locations along the water distribution system, at municipal wells, and at 3 fixed sampling air stations at different sites in the town. No risks to health related to drinking water or outdoor air have been identified. Attempting to “measure” perceived risks, through:
|
| Health impact assessment | Evaluation of the impacts on health linked to the reconstruction of the downtown area, with special focus on where to locate the railroad corridor. Main issues examined: job creation, local economic development, noise and vibration, medical trauma risks, anxiety and psychological distress and trauma, derailment risks and environmental contamination |
Health surveillance
The Public Health Department has implemented a local surveillance system focusing on health issues related to the train derailment to keep track of potential after-effects of the tragedy (Fig. 3).
Figure 3.
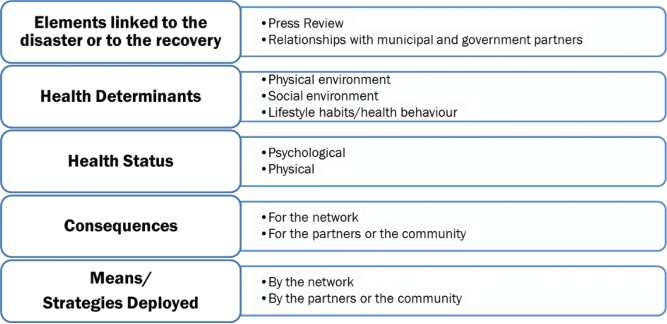
Health surveillance in the recovery phase: Conceptual framework.
Creation of the surveillance system required the thoughtful selection of a set of indicators ranging from health determinants to disaster consequences. These indicators operate on different timescales (short term, medium term, long term) and include data that are compiled monthly (e.g., environmental monitoring, volume of new requests for psychological support), annually (e.g. hospital morbidity), and over a multi-year period of observation (e.g., incidence of cancer). The surveillance system draws upon available information from the health care network (e.g. medical/administrative information systems, calls to health hotlines, reportable disease notifications, absenteeism/sickness reports within the health care network, ambulance transports) and databases located within partner organizations (e.g., air quality, soil characterization, drinking water analyses, crime and road accident data, workers' compensation). Four health update bulletins were produced and published during the recovery period. Each bulletin presented information categorized into 4 topic areas (news, psychological health, environment, physical health). The bulletins were disseminated throughout the health care network and distributed to local and government partners involved in the recovery.
Research
With the collaboration of researchers in the field of psychosocial recovery, the Public Health Department conducted a study entitled “Enquête de santé populationnelle estrienne” in summer 2014, one year following the tragedy, using a representative population-based sample of 8,737 adults in the Eastern Townships (including 811 respondents from the Granit RCM).
Participants completed a telephone or web-based questionnaire with a relatively good response rate (48%). Three types of exposure were measured: 1) human losses (e.g., loss of loved one, perceived threat to life for self or loved one, physical injury), 2) material losses (e.g., evacuation, home damage, job loss), and 3) self-reported negative perceptions of the train derailment (e.g., stressful event, interruption of important life events, adverse effects on the future, significant losses). Exposure was then categorized as intense (e.g., all three exposure types were endorsed), moderate (e.g., one or 2 exposure types were endorsed), or no exposure.
Among citizens comprising the Granit population, we observed that two-thirds (64%) of participants suffered human losses, 23% suffered material losses, and 54% held negative perceptions of the event. One-in-six Granit participants (17%) experienced “intense exposure” while one-in-four (25%) had “no exposure.” Community strengths were observed in Granit, including a strong sense of belonging, access to medical and psychosocial resources (at higher rates than elsewhere in the Eastern Townships), and a sustained high level of resilience - comparable to elsewhere in the region.
However, important differences were observed according to exposure intensity. Self-reported depressive episode over the past year was twice as frequent in intensely exposed adults in Granit compared to those with no exposure (Fig. 4). Anxiety disorders, alcohol abuse (≥1 episode/week), and consumption of anxiolytic medications were more frequent among those who were intensely exposed (13%, 17%, 20%, respectively) compared to those with no exposure (4%, 4%, 9%, respectively). Use of psychosocial services was also found to be 4 times more frequent among intensely exposed persons (31%) relative to non-exposed persons (7%). These findings, consistent with the current scientific knowledge,12 suggest that the population of Granit has suffered psychologically and still does.
Figure 4.
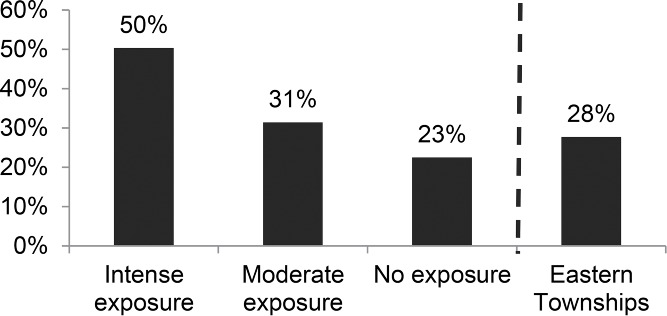
Prevalence of self-reported depressive episode in the past 12 months according to exposure intensity, random sample of 8,737 adults in Eastern Townships, including 811 adults in the Granit RCM, summer 2014.
Indeed, most studies have found significant differences between persons who are exposed to a catastrophic disaster and those who are not, and the accumulation of losses and disruptive events increases the risk of developing health problems.13-16 The psychological consequences of disasters can persist over time, particularly when there is insufficient social support from the family members or friends, and also when governmental or community assistance is delayed or lacking.17-19 These findings underscore the importance of promoting and protecting population health.
It is noteworthy that the survey results were rapidly shared with community and regional partners involved in the response, and with the general public, through a press conference and media interviews. Several weeks following the media broadcasts, a decision was made to secure funding to support psychosocial recovery in Lac-Mégantic.
Lesson 6: People should never underestimate the long-term impacts of a tragedy, especially on mental health and psychological well-being. To ensure that this major issue is not overlooked, the Public Health Department should quickly implement a monitoring system based on a set of easily available indicators of psychological health and functioning and, in the ideal world, conduct a survey to capture data that are really population-based.
Environmental health (the case of asbestos)
Due to the crude oil saturation from the leaking tank cars, contaminated soil from the train crash site, and from areas destroyed or severely damaged by the fires, was excavated and transported to a temporary treatment center during Fall, 2013. When asbestos was found in soil samples, the excavation/transport operations were suspended while multiple agencies (Departments of Public Health, Environment, Occupational and Health Safety, Municipal Affairs) conducted a thorough risk assessment of both soil and airborne exposures to asbestos for the onsite workers and also for residents living near the crash site. The Public Health Department determined that the risks for the general public and for onsite workers (who had been wearing respiratory protective equipment) were very low. The Public Health Department recommended implementation of an air quality surveillance system at the train crash site, nearby areas, and soil treatment centers, and preventive measures specific for asbestos for onsite workers if warranted based on the results of the soil analyses.
Lesson 7: The Public Health Department and response partners made a public presentation describing the results of the risk assessment for general public citizens and onsite workers potentially exposed to asbestos in air or soil. Meeting attendees and media indicated their confidence in the veracity of the assessment, showing low or minimal risk, as reported by the Public Health Department. This underscores that, for the sake of transparency, complete and accurate relevant information should be disclosed as far as possible.
Concluding Comments
Our comprehensive analysis of the public health emergency response and recovery operations over the past 2 y in Lac-Mégantic illustrates the broad spectrum of public health actions required for ensuring that the medical, psychological, and environmental impacts of such a disaster are minimized. The analysis also presents a series of lessons that should be taken into account for future public health emergency events. Most of these lessons can be generalized to a spectrum of incidents including emerging infectious diseases, chemical spills, terrorist attacks, and natural disasters, events that pose both immediate and ongoing threats to population health and well-being.
Our work contributes to the development of a conceptual framework for public health emergency preparedness that clearly identifies the essential elements of emergency and recovery operations during all-hazards emergencies. Our framework is particularly relevant within the context of the Canadian public health system. It is also essential to continue research in this area to identify the different social and community factors related to the resilience of individuals and communities.
To conclude, this unique experience demonstrates the need for the Public Health Department to establish bonds of cooperation with the various organizations in the community, in a manner that is respectful of each other's mandates, in order to be ready to intervene at any time in the case of emergencies. However, public health actions continue long after emergency response operations have concluded, particularly because of the protracted duration of 1) disaster-related psychological consequences,20 2) some types of medical complications including disabling injury and risks for future disease, and 3) environmental impact. In the case of the Lac-Mégantic train derailment, the public health professionals who responded, representing a wide range of subspecialties, deserve to be acknowledged for their rigorous and sustained work over the past two years.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Acknowledgments
We wish to thank each member of our team (i.e., Public Health Department of the Eastern Townships) as well as our partners at all levels, from the local community to the health ministry, for their valuable input into public health interventions in Lac-Mégantic since July 2013. It is acknowledged that the source of the conclusion related to development of a conceptual framework for and the definition of public health emergency preparedness is based on work by a collaborative research team led by Drs. Yasmin Khan and Brian Schwartz and on which MG is a co-investigator (with funding from the Canadian Institutes of Health Research grant - #MOP142292) and as published in Khan et al. (2015).21
References
- 1.Centers for Disease Control and Prevention Public health preparedness capabilities: National standards for state and local planning March 2011. Atlanta (United States of America): Department of Health and Human Services/Center for Disease Control and Prevention; 2011 [Google Scholar]
- 2.Quebec Government Civil protection act August 2015. Québec (Canada): Quebec Government; 2015. [Google Scholar]
- 3.Fortier M, Saucier A, Simard M, Allaire A, Auger D, Bardou HD, Duranleau F, Fagy MF, Fréchette M, Garceau M, et al.. Politique ministérielle de sécurité civile: Santé et services sociaux. Québec: Gouvernement du Québec, 2014. [In French] http://publications.msss.gouv.qc.ca/msss/fichiers/2013/13-860-15W.pdf. [Google Scholar]
- 4.Richard S, Bolduc D, Delage G, Duval B, Plante R, Poirier A, Poulin M, Dontigny A, Dupont S, Malenfant R, et al.. Cadre de référence en gestion des risques pour la santé dans le réseau québécois de la santé publique. Québec: Institut national de santé publique du Québec, 2003. [In French] https://www.inspq.qc.ca/pdf/publications/163_CadreReferenceGestionRisques.pdf. [Google Scholar]
- 5.Centers for Disease Control and Prevention Crisis emergency risk communication 2012 edition Atlanta (United States of America): Department of Health and Human Services/Center for Disease Control and Prevention; 2012 [Google Scholar]
- 6.Slovic P. Perception of risk. Science 1987; 236:280-5; PMID:3563507; http://dx.doi.org/ 10.1126/science.3563507 [DOI] [PubMed] [Google Scholar]
- 7.Covello VT, Peters RG, Wojtecki JG, Hyde RC. Risk communication, the West Nile virus epidemic, and bioterrorism: Responding to the communication challenges posed by the intentional or unintentional release of a pathogen in an urban setting. J Urban Health 2001; 78:382-91; PMID:11419589; http://dx.doi.org/ 10.1093/jurban/78.2.382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rootman I, Gordon-El-Bihbety D. A vison for a health literate Canada: Report of the expert panel on health literacy. Ottawa (Ontario, Canada: ): Public Health Agency of Canada; 2008 [Google Scholar]
- 9.Centers for Disease Control and Prevention Simply Put: A guide for creating easy to understand material Atlanta (United States of America: ): Department of Health and Human Services/Center for Disease Control and Prevention; 2010. [Google Scholar]
- 10.DuBay WH. The principles of readability. Impact Information 2014. [Google Scholar]
- 11.Morin M. Approches et principes en sécurité civile. Québec: Gouvernement du Québec, 2008. [In French] http://www.securitepublique.gouv.qc.ca/fileadmin/Documents/securite_civile/publications/concepts_base/concepts_base.pdf. [Google Scholar]
- 12.Messiah A, Acuna JM, Castro G, de la Vega PR, Vaiva G, Shultz JM, Neria Y, De La Rosa M. Mental health impact of the 2010 Haiti earthquake on the Miami Haitian population: A random-sample survey. Disaster Health 2015; 2:1-8; http://dx.doi.org/ 10.1080/21665044.2015.1014216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arnberg FK, Eriksson NG, Hultman CM, Lundin T. Traumatic bereavement, acute dissociation, and posttraumatic stress: 14 years after the MS estonia disaster. J Traumatic Stress 2011; 24:183-90; http://dx.doi.org/ 10.1002/jts.20629 [DOI] [PubMed] [Google Scholar]
- 14.Auger PL, Verger P, Dab W, Guerrier P, Lachance A, Lajoie P, Leroux R, Rhainds M, Roy LA. Sinistres naturels et accidents technologiques In: Gérin M. (ed.): Environnement et santé publique: fondements et pratiques (pp. 517-35). Québec, Canada: Éditions Tec et Doc, 2003. [In French]. [Google Scholar]
- 15.Maltais D. Catastrophes en milieu rural. Chicoutimi (Québec, Canada: ): Éditions JCL, 2003. [In French]. [Google Scholar]
- 16.Maltais D, Lachance L, Richard MC, Gauthier S. Effets à long-terme d'une inondation sur la santé psychologique: Étude longitudinale auprès de sinistrés et de non-sinistrés. Revue Francophone du Stress et du Trauma 2009; 9:155-66. [In French] [Google Scholar]
- 17.Suzuki Y, Tsutsumi A, Fukasawa M, Honma H, Someya T, Kim Y. Prevalence of mental disorders and suicidal thoughts among community-dwelling elderly adults 3 years after the Niigata-Chuetsu earthquake. J Epidemiol 2011; 21:144-50; PMID:21325733; http://dx.doi.org/ 10.2188/jea.JE20100093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maltais D, Lachance L, Brassard A, Dubois M. Soutien social perçu, stratégies d'adaptation et état de santé psychologique post-désastre de victimes d'un désastre. Sciences sociales et santé 2005; 23:5-38. [In French]; http://dx.doi.org/ 10.3406/sosan.2005.1648 [DOI] [Google Scholar]
- 19.Maltais D, Lachance L, Brassard A. Satisfaction face à l'aide reçue et état de santé biopsychosociale post-désastre, Revue canadienne de service social 2003; 20:39-61. [In French]. [Google Scholar]
- 20.Shultz JM. Perspectives on disaster public health and disaster behavioral health integration, Disaster Health 2014; 2: 69-74; http://dx.doi.org/ 10.4161/dish.24861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khan Y, Fazli G, Henry B, de Villa E, Tsamis C, Grant M, Schwartz B. The evidence base of primary research in public health emergency preparedness: a scoping review and stakeholder consultation. BMC Public Health 2015; 15(1): 432. [DOI] [PMC free article] [PubMed] [Google Scholar]


