Abstract
Skills for Psychological Recovery (SPR) is a brief skills-based approach to assist community members to better cope after a disaster or other tragedy. This paper reports on an evaluation of a large SPR training and support program following floods and cyclones in Queensland, Australia. The program sought to recruit, train and support competent SPR trainers; provide systematic high-quality training in SPR skills for practitioners; improve the confidence of a large number of practitioners to use SPR; and encourage practitioners' use of SPR with community members. Trainers recruited to the program facilitated 49 training sessions for 788 practitioners across Queensland. Trainers were assessed by practitioners to have high-level competencies to run training sessions. Practitioners reported improved confidence to use each SPR intervention following training and at 6 months post-training. Based on available data, more than 6 out of 10 practitioners used an SPR intervention during the follow up period, with each intervention used by over half of the practitioners at both 3 and 6 months. The most frequently reported barrier to using SPR was not having seen a community member with problems requiring SPR. For trainers, a psychology background and cognitive-behavioral therapy (CBT) orientation were unrelated to their competencies to facilitate practitioner training sessions. For practitioners, a psychology background and to some extent a CBT orientation were related to confidence to use SPR interventions. In summary, this study provides details of an evaluation of a large-scale mental health training and support program to enhance response to meet the mental health needs of those affected by disaster.
Keywords: disaster, mental health, recovery, Skills for Psychological Recovery, training program
Introduction
Disasters can cause or exacerbate a range of mental health problems of varying severity in the affected population.1 A significant number of individuals will display resilience with transient distress and then a return to their usual level of functioning by relying on their existing coping strategies and support networks,2 while a minority will develop a mental health disorder such as posttraumatic stress disorder (PTSD), depression or anxiety.3 In addition, many individuals will experience mild to moderate severity or sub-clinical mental health or related problems such as dysphoria, anxiety, stress, substance misuse, psychosocial loss and disruptions in relationships and social functioning.1
In Australia, in order to plan for and meet the varied mental health needs of those affected by disasters, a 3-level stepped-care framework of treatment and support has been developed by local experts to guide the training and practices of lay personnel and practitioners.4-7 In the framework, Level 1 refers to early response in the immediate aftermath of disaster, which includes providing advice, information and support at an individual and community level to all willing recipients.8,9 Given that many people will display a resilient or recovery trajectory following trauma, the priority and focus of level 1 is advice and support rather than mental health diagnosis and treatment. This level is consistent with Psychological First Aid (PFA) which is a recommended approach for assisting people in the hours, days and weeks following disaster.10,11 Level 1 support can often be provided by community members with basic training and is often sufficient for individuals with acute or mild reactions. Where mild to moderate distress persists despite the provision of level 1 support, individuals can be taught simple strength-based skills to improve coping and promote recovery (level 2).12 These simple strategies can be provided by practitioners with basic counselling skills working in primary care, mental health, and community-based settings. Finally, those individuals who display persistent and severe distress in the weeks and months following a disaster should be provided with and/or referred for more intensive mental health treatment (level 3) including evidence-based psychological and pharmacological interventions provided by mental health specialists.3 Of course there is no replacement for good judgement and a stepped-care approach may not always be practical or appropriate. For example, individuals presenting with extreme distress including suicidality should be referred to mental health specialists regardless of the time since the disaster or trauma.
Although many individuals with persistent or intermittent mild to moderate distress in the weeks and months following disaster may not meet diagnostic criteria for a mental health disorder, their level of distress can disrupt their functioning in various aspects of their lives, place additional burden on those around them, and increase the risk for later development of a mental health disorder. Moreover, these individuals may recover more quickly with assistance from a practitioner to develop improved coping skills. Until the recent development of Skills for Psychological Recovery (SPR), there has been no formal and structured level 2 approach to address these types of difficulties. SPR is a brief skills-based approach designed to assist children, adolescents, adults and families to better cope with a range of practical, emotional and psychosocial problems after experiencing a disaster or other trauma.12 SPR was developed by the National Center for PTSD (NC-PTSD) and the National Child Traumatic Stress Network (NCTSN) in the United States, and is consistent with empirically supported principles following disaster.8 The goals of SPR are to (i) protect the mental health of disaster survivors; (ii) enhance their own ability to address their needs and concerns; (iii) teach skills to promote the recovery of individuals and families; and (iv) prevent maladaptive behaviors while identifying and supporting adaptive behaviors.12 SPR is intended for use by health and community practitioners with varying levels of expertise, to build upon their existing competence to assist disaster-affected community members. The SPR Field Guide consists of a brief screening module of presenting problems - ‘Gathering Information and Prioritising Assistance’ - as well as 5 skills-based interventions that are informed by available evidence e.g.13,14,15 The 5 skills-based interventions are designed to be delivered in a flexible and tailored manner. These include ‘Building Problem Solving Skills’ to identify the steps to address practical problems; ‘Promoting Positive Activities’ to plan and carry out activities that create well-being and address dysphoria and inactivity; ‘Managing Reactions’ to learn skills to better manage distressing psychological reactions and triggers; ‘Promoting Helpful Thinking’ to identify and address unhelpful appraisals and self-talk; and ‘Rebuilding Healthy Social Connections’ to access social and community supports in a practical way.
A previous Australian study assessed perceptions of SPR among practitioners who had attended a training program as part of the mental health response to the Victorian bushfires in 2009.4 The majority of practitioners rated SPR interventions as potentially useful for working with disaster-affected clients. Moreover, those practitioners who did use SPR following training reported that the interventions were useful to clients. The findings also indicated that practitioners' negative perceptions of evidence-based approaches and manualized interventions were associated with lower motivation to use SPR with clients. A second study from the United States assessed perceptions of a training and community-based outreach and education support program (that incorporated SPR and other evidence-based interventions) among practitioners working in Louisiana following Hurricanes Katrina and Rita.16 The training and post-training support provided by expert consultants were rated highly by staff, and the majority thought that the program was helpful to affected community members.
The current paper reports on the evaluation of a large SPR training and support program for health and community practitioners following a disaster. During late December 2010 and early January 2011, significant flooding, cyclones and other extreme weather events occurred in many areas of Queensland, Australia. Three-quarters of the state was declared a disaster zone: 35 people died and approximately 1.3 million people and 45,000 properties in rural and urban locations were affected. In partnership with the Queensland and Commonwealth governments, Phoenix Australia developed the SPR training and support program as part of the Queensland Mental Health Natural Disaster Recovery Plan 2011 – 2013 to support disaster-affected community members. The program adopted a train-the-trainer approach: first, suitable local trainers were recruited and trained, and second, these trainers subsequently trained practitioners to use SPR interventions with community members. Orfaly and colleagues (2005) have noted potential benefits of the train-the-trainer approach including that it harnesses existing social capital, uses credible local trainers, promotes self-reliance within communities, and has the potential for lower-cost sustainability. On the other hand, potential risks of the approach include reduced quality, fidelity and effectiveness of the training program due to use of intermediate trainers, as well as lack of follow through by these trainers to deliver training sessions.17 There may be many ways to ameliorate some of these risks, such as imposing selection criteria for trainers participating in a train-the-trainer program. Cross and colleagues (2010) found that prior trainer experience predicted how many people were trained following a disaster mental health train-the-trainer program. They recommended behavioral rehearsal and role-play practice, small group problem-solving, and expert feedback to increase self-efficacy and readiness to train following the train-the-trainer training.18
Evaluation of the current SPR training and support program was based on the 3 main aims of the program: (1) recruit, train and support competent trainers; (2) improve the confidence of a large number of practitioners to use SPR; and (3) encourage practitioners' use of SPR with community members in disaster-affected areas. In addition, we were particularly interested in examining whether a psychology professional background and cognitive-behavioral therapy (CBT) theoretical orientation of trainers and practitioners involved in the program influenced their performance and behavior.
Methods
The program was funded by the Queensland and Commonwealth governments as part of the Queensland Mental Health Natural Disaster Recovery Plan 2011-2013. All program activities were overseen by a working group that comprised Queensland Health, via the Center for Trauma, Loss and Disaster Recovery, the Department of Communities, General Practice Queensland (GPQ), and Phoenix Australia. The Center for Trauma, Loss and Disaster Recovery, the Department of Communities, and GPQ were responsible for the logistical arrangements that supported delivery of the program. Phoenix Australia was responsible for the development, delivery, and evaluation of the program.
Participants
Participants comprised 2 groups: trainers and practitioners. To recruit trainers, a request for expressions of interest was sent to child/adolescent and adult health and community services in disaster-affected areas across Queensland. Trainers were required to meet the following selection criteria that were endorsed by their line manager: demonstrated experience in the use of cognitive-behavioral or similar evidence-based psychological interventions, excellent teaching and communication skills, excellent interpersonal skills, and a willingness to conduct training of practitioners.
Practitioners were recruited through health and community services in disaster-affected areas. Training was free and available to those working in a wide range of services including disaster recovery, primary care, mental health, education, and community support services. The prerequisites for practitioners to attend this training were as follows: providing direct support to people in disaster-affected communities in their current work role, basic proficiency in counselling and personal support, and a willingness to adopt brief skills-based interventions.
Materials
The primary resource for the program was the Skills for Psychological Recovery: Field Operations Guide which provides detailed information about each intervention as well as worksheets and handouts to use in practice.12 Other materials developed for the program included information about the statewide recovery plan, training handouts and Powerpoint slides, online self-assessment and support modules, and evaluation materials. Trainers completed a brief online support module at 3 and 6 months following initial training. Practitioners also completed a brief online module at 3 and 6 months following their training. The online modules provided an opportunity for all program participants to be reminded about key competencies of the SPR approach using multiple-choice ‘quiz’ questions with immediate feedback provided on their answers to questions. In addition, each module strongly encouraged participants to review the relevant sections of the SPR Field Guide or other materials for any topics requiring further revision. The modules also provided an opportunity for participants to complete the program evaluation measures.
Measures
Trainer and practitioner characteristics
At the initial training, basic data was collected on the trainer and practitioner demographic and other characteristics, including professional background and theoretical orientation of counselling approach.
Trainer competencies
At practitioner training sessions, practitioners rated each trainer on 8 competencies including (i) confident facilitation, (ii) effective facilitation, (iii) participant engagement, (iv) management of time, (v) explanation of program content, (vi) explanation of program evaluation, (vii) effectiveness of answering participants' questions, and (viii) facilitation of skills rehearsal. Ratings were made on a 5-point scale from 1 ‘strongly disagree’ to 5 ‘strongly agree’ on statements such as “The trainer demonstrated an ability to facilitate the training with confidence.”
Practitioner confidence to use SPR interventions
Prior to and at the end of practitioner training, as well as at 3 and 6 months post-training, practitioners were asked to rate how confident they were to use SPR interventions in their usual practice. Specifically, practitioners were provided with a description of each SPR intervention to rate (e.g., ‘How confident are you to teach someone problem-solving skills?’). Ratings were made on a 5-point scale from 1 ‘not at all confident’ to 5 ‘very confident’.
Practitioner use of SPR
At 3 and 6 months, practitioners were asked to estimate the number of community members with whom they had used any SPR intervention as well as individual SPR interventions. They were also asked to indicate what barriers (if any) had prevented them from using SPR interventions during the previous 3 months.
Procedure
Prospective trainers attended a 2-day face-to-face ‘train-the-trainer’ session run by Phoenix Australia experts to prepare them to facilitate practitioner training sessions. On the second day, individuals were assessed to establish the meeting of minimum competency standards, including clear speech, professional delivery, audience engagement, and ability to clearly explain SPR content. Those individuals who met the requisite accreditation standard were then eligible to facilitate practitioner training sessions. Additional post-training support for these trainers included (i) brief online modules completed at 3 and 6 months (as described); (ii) a one-hour teleconference facilitated by Phoenix Australia at 3 and 6 months to receive advice, support and feedback on running practitioner training; and (iii) Phoenix Australia personnel attending 10 practitioner training sessions facilitated by trainers to provide support and feedback to a subgroup of the trainers.
Practitioners attended a one-day face-to-face training session (facilitated by a trainer) to develop their competencies to deliver SPR interventions. Following training, practitioners were asked to complete brief online modules at 3 and 6 months (as described).
All trainer and practitioner training sessions followed a structured plan with scheduled group exercises and facilitated discussion.
Data Analysis
Assessment of group differences on nominally measured variables was undertaken by cross-tabulating the data and performing chi-square tests of independence. Group differences for normally distributed variables were assessed using independent samples t-tests. Non-parametric tests undertaken included Mann-Whitney U tests to assess for any between-group differences on ratings of confidence or competency; Wilcoxon signed-ranks tests to assess to assess for any within-group changes in ratings over time; and Spearman's rank order correlations to assess for any relationships between 2 continuous variables. We used an α level of 0.05 for all statistical tests. All analyses were conducted using IBM SPSS version 17.
Results
Practitioner training sessions
Forty-nine practitioner training sessions were run for 788 practitioners in 35 urban and regional locations across Queensland between August 2011 and June 2012. Thirty-eight (77.6%) sessions were co-facilitated by 2 trainers, and 11 (22.4%) were facilitated by a single trainer.
Trainers
Forty of 48 prospective trainers met the minimum competency standard to facilitate practitioner training sessions. The average age of these 40 trainers was 43.3 years (SD = 10.4) and the majority were female (n = 26; 65%). Twenty (50.0%) of the trainers had a professional background in psychology, with the remainder from social work (n = 8), nursing (n = 7), medicine (n = 1), occupational therapy (n = 1) and other (n = 3) backgrounds. In terms of theoretical orientation, 21 (52.5%) trainers endorsed cognitive-behavioral therapy (CBT) while the others nominated eclectic (n = 7), systemic (n = 5), person-centered (n = 3), solution-focused (n = 2), narrative (n = 1) and psychodynamic (n = 1) orientations.
Of the 40 accredited trainers, 10 (25.0%) trainers facilitated only one practitioner training session, 17 (43%) facilitated 2 sessions, and 12 (30%) facilitated 3 to 7 sessions. One trainer (2%) did not run any sessions due to relocating to another Australian state.
Trainer competencies
As shown in Figure 1, practitioners rated trainers as having high-level competencies to deliver SPR training. These ratings were made at the end of the first workshop facilitated by each trainer. There were no significant associations between ratings of trainer competencies and the trainer's professional background or theoretical orientation. The total number of sessions facilitated by a trainer was positively correlated with ratings of the following trainer competencies: confident facilitation (r = 0.10, p = 0.02), effective facilitation (r = 0.10, p = 0.03), management of time (r = 0.09, p = 0.04), explanation of program content (r = 0.11, p = 0.02), answering participants’ questions (r = 0.13, p = 0.004), and facilitation of skills rehearsal (r = 0.11, p = 0.02). There was no significant association between total number of sessions facilitated by a trainer and the competencies of participant engagement or explanation of program evaluation.
Figure 1.
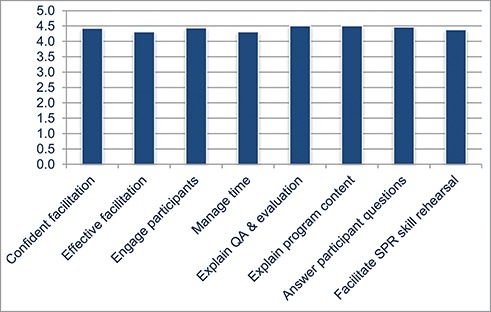
Mean practitioner ratings of competencies of trainers to deliver SPR training. Note: QA = quality assurance; SPR = Skills for Psychological Recovery; n = 506 practitioners and n = 36 trainers due to missing data.
Practitioners
Of the 788 practitioners who attended a training session, 730 provided consent to participate in the program evaluation. Of these, 46 were excluded from further analyses because they did not provide data at the pre- and post-training time-points (n = 14) or because their work role did not involve direct client contact (n = 32). Of the remaining 684 practitioners, 78.8% (n = 539) were female. The professional backgrounds of the practitioners were as follows (n = 682 due to missing data): psychology (n = 169, 24.8%), social work (n = 153, 22.4%), other mental health (n = 146, 21.3%), nursing (n = 115, 16.8%), medicine (n = 39, 5.7%), community worker (n = 33, 4.8%), and occupational therapy (n = 27, 3.9%). The practitioners’ theoretical orientations were as follows (n = 574 due to missing data): cognitive-behavioral therapy (CBT: n = 204, 35.5%), eclectic (n = 166, 28.9), person-centered (n = 88, 15.3%), solution-focused (n = 69, 12.0%), narrative (n = 23, 4.0%), systemic (n = 16, 2.8%), and psychodynamic (n = 8, 1.4%).
Practitioner confidence to use SPR
Comparisons between practitioners with confidence ratings at pre- and post-training only (n = 416) and those with additional confidence ratings at 6 months (n = 268) showed that the former were somewhat younger (M (SD): 45.2 (12.0) versus 47.0 (10.37); t (669) = −2.0, p = 0.04). There were no between-group differences on gender, professional background (psychology vs. non-psychology), or theoretical orientation (CBT versus non-CBT). For those practitioners (n = 268) who provided data at pre-training, post-training and 6 months, there was a significant increase in the ratings of their confidence to use each of the SPR interventions from pre-training to post-training, and pre-training to 6 months (Table 1). There was also a significant decrease in their confidence ratings to use each of the interventions from post-training to 6 months.
Table 1.
Practitioner confidence to use SPR interventions at pre- and post-training and 6 month follow-up (n = 268)
| SPR module | Pre-training M (SD) | Post-training M (SD) | 6 months M (SD) | Comparisons over timez |
|---|---|---|---|---|
| Gathering information | 2.9 (1.0) | 4.4 (0.7) | 3.9 (0.9) | a = −13.4*** b = −11.0*** c = −7.8*** |
| Problem Solving | 3.1 (1.0) | 4.4 (0.7) | 3.9 (0.9) | a = −13.1*** b = −10.6*** c = −7.4*** |
| Positive Activities | 3.2 (0.9) | 4.5 (0.7) | 4.0 (0.9) | a = −13.1*** b = −10.5*** c = −7.2*** |
| Managing Reactions | 3.0 (1.0) | 4.3 (0.8) | 3.9 (1.0) | a = −12.9*** b = −10.5*** c = −6.2*** |
| Helpful Thinking | 3.2 (0.9) | 4.4 (0.7) | 4.0 (0.9) | a = −12.9*** b = −10.6*** c = −7.2*** |
| Social Connections | 3.1 (1.0) | 4.5 (0.7) | 4.0 (0.9) | a = −13.4*** b = −10.7*** c = −6.7*** |
Note: a= pre-training vs. post-training; b= pre-training versus 6 months; c= post-training vs. 6 months; *p < 0.05, **p < 0.01, ***p < 0.001; SPR = Skills for Psychological Recovery; CBT = cognitive-behavioral therapy.
As shown in Table 2, psychologists were more confident than other practitioners to use 3 interventions at all 3 time-points: Building Problem Solving Skills, Promoting Positive Activities, and Promoting Helpful Thinking. In addition, psychologists were more confident to use Managing Reactions at pre-training and 6 months, Rebuilding Healthy Social Connections at post-training and 6 months, and Gathering Information at post-training. CBT practitioners were more confident than non-CBT practitioners to use Promoting Helpful Thinking at pre-training and 6 months, and Managing Reactions at 6 months.
Table 2.
Associations between practitioner confidence to use SPR interventions at pre-training, post-training and 6 month follow-up and practitioner professional background (n = 268) and theoretical orientation (n = 227)
| SPR module | Psychology versus non-psychology z | CBT vs. non-CBT z |
|---|---|---|
| Gathering Information | Pre: −0.6 Post: −2.0* 6 mth: −1.9 |
Pre: −0.4 Post: −1.1 6 mth: −1.2 |
| Problem Solving | Pre: −3.0** Post: −2.3* 6 mth: −3.5*** |
Pre: −0.7 Post: −1.1 6 mth: −1.7 |
| Positive Activities | Pre: −2.4* Post: −3.0** 6 mth: −3.1** |
Pre: −0.7 Post: −0.4 6 mth: −1.5 |
| Managing Reactions | Pre: −4.1*** Post: −1.5 6 mth: −4.1*** |
Pre: −1.7 Post: −0.4 6 mth: −2.5* |
| Helpful Thinking | Pre: −4.3*** Post: −2.1* 6 mth: −3.6*** |
Pre: −2.1* Post: −0.4 6 mth: −2.1* |
| Social Connections | Pre: −1.8 Post: −2.7** 6 mth: −2.7** |
Pre: −0.4 Post: −1.2 6 mth: −2.0 |
*p < 0.05, **p < 0.01, ***p < 0.001; SPR = Skills for Psychological Recovery; CBT = cognitive-behavioral therapy.
Practitioner use of SPR
Practitioners provided feedback on how many community members they had used SPR with at 3 and 6 months post-training. As shown in Figure 2, more than 60% of practitioners with data available at 3 months and 6 months used at least one SPR intervention with one or more community members during the previous 3 months: 64.2% (n = 221) and 61.6% (n = 162), respectively. It is worth noting that any single community member may have received more than one SPR intervention. Of those practitioners who used any intervention, the majority used it with up to 10 community members during each time period. More than half of the practitioners used each of the SPR interventions during the respective time periods (n = 262 at 6 months due to missing data for one practitioner): Gathering Information (54.1%, 51.1%), Building Problem Solving Skills (56.7%, 51.9%), Promoting Positive Activities (57.6%, 54.2%), Managing Reactions (53.8%, 51.5%), Promoting Helpful Thinking (59.3%, 56.5%), and Rebuilding Healthy Social Connections (51.7%, 50.0%). There was no significant association between practitioners’ professional background and theoretical orientation, and use of any SPR intervention or individual SPR interventions at 3 months and 6 months.
Figure 2.
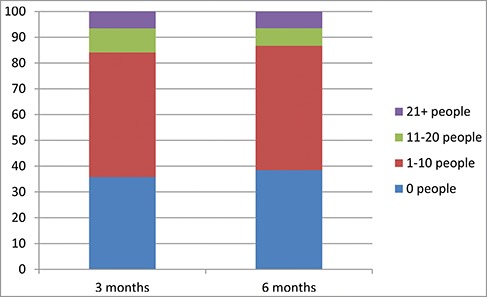
Practitioners′ use of any SPR intervention at 3 months (n = 344) and 6 months (n = 263).
As shown in Table 3, practitioners provided feedback on barriers to using SPR at 3 and 6 months. The most frequently reported barrier was not having seen any clients with problems requiring the use of SPR: 37.3% at 3 months and 42.4% at 6 months. The next most frequent reasons for not using SPR were being satisfied with their existing approach and lack of time, although only a relatively small percentage of practitioners (approximately 6-8%) reported these barriers. There were no significant associations between these 3 barriers at 3 and 6 months and practitioners’ professional background or theoretical orientation.
Table 3.
Barriers to practitioner use of SPR at 3 months (n = 343) and 6 months (n = 257) post-trainin
| Barrier | n (%)3 months | n (%)6 months |
|---|---|---|
| Not seen anyone with problems requiring the use of SPR | 128 (37.3%) | 109 (42.4%) |
| Satisfied with existing approach | 22 (6.4%) | 20 (7.8%) |
| Lack of time | 23 (6.7%) | 17 (6.6%) |
| Concerned about client reaction | 9 (2.6%) | 3 (1.2%) |
| Insufficient organisational support | 8 (2.3%) | 4 (1.6%) |
| Not a good fit with my existing approach | 6 (1.7%) | 1 (0.4%) |
| Insufficient skill level | 3 (0.9%) | 1 (0.4%) |
| Lack of confidence in skills | 4 (1.2%) | 1 (0.4%) |
| Lack of confidence in the benefit of SPR | 1 (0.3%) | 0 (0%) |
Discussion
This paper reports on the evaluation of a large SPR training and support program which formed part of the government-funded mental health recovery plan in response to the Queensland floods and cyclones of 2010-2011. The aims of the program were to recruit, train and support competent trainers; provide systematic high-quality training in SPR skills for practitioners; improve the confidence of a large number of practitioners to use SPR; and promote practitioners’ use of SPR with community members in disaster-affected areas. The evaluation findings suggest that the aims of the program were largely met. Trainers recruited to the program were assessed by practitioners to have high-level competencies to run local practitioner training sessions. These trainers facilitated training sessions for 788 practitioners in 35 urban and regional disaster-affected locations. Practitioners who attended these training sessions reported improved confidence to use each of the SPR interventions following training and at 6-month follow-up. Based on available data, more than 6 out of 10 practitioners used an SPR intervention, with each of the SPR interventions used by over half of the practitioners, at both 3 and 6 months following training. Of those practitioners who used any intervention, the majority did so with up to 10 clients during each 3 month time period. The most commonly reported barrier to using SPR was not having seen any clients with problems requiring SPR.
In addition to the training itself, it seems likely that the explicit selection criteria and processes that were used in the recruitment of trainers (including the criterion of demonstrated experience in CBT or other evidence-based psychological interventions) and the need for trainers to meet minimum competency standards at the initial ‘train-the-trainer’ session contributed to the high-level competencies demonstrated by trainers. Also, following their initial training, trainers were provided with ongoing support, including face-to-face feedback on performance, teleconference meetings and use of online training modules. Ongoing program support for trainers has been identified as an important component of successful train-the-trainer programs.17 In addition, the manualised and highly structured nature of SPR may have enabled trainers to more readily develop the competencies to teach these interventions to practitioners.19
The finding that 29 of 40 trainers facilitated 2 or more practitioner training sessions, and that only one trainer (who moved to another state) did not facilitate a session, suggests that the trainers were committed to their role in the program. In part, this may be due to the fact that trainers were provided with organizational and logistical support to run practitioner training sessions by Queensland Health, the Department of Communities, and GPQ. Some trainers mentioned during post-training teleconferences that substantive work commitments, lack of staff backfill, and lack of time prevented them from facilitating further sessions. Interestingly, we found that trainers who facilitated more practitioner training sessions had higher-level competencies. Given that the ratings of competencies were assessed during the first session facilitated by a trainer, it appears that the greater skill and confidence of some trainers may have influenced their preparedness to facilitate further sessions during the course of the program.
A positive finding is that the confidence of practitioners to use each of the SPR interventions improved after attending training, with improvement still evident at 6 months. It seems feasible that the post-training online modules designed to reinforce key competencies for practitioners helped to maintain their confidence to use SPR interventions. Despite these encouraging findings, the confidence of practitioners did reduce during the 6 month period following training. Consistent with the notion that practitioner confidence reduces following training, the mean confidence ratings of practitioners at 3 months reported by Forbes and colleagues (2010) were, in general, slightly lower than the post-training ratings and slightly higher than the 6-months ratings in the current study. It should be noted that outcome data for clients is a consistently neglected aspect of training studies.20 In this study, a self-report measure of confidence is obviously not sufficient to assess practitioner competence to deliver these interventions at an acceptable standard.21 As a result, it is not possible to determine the quality of the interventions delivered by practitioners or the extent to which community members who received these interventions derived any benefit. However, an evaluation of these outcomes was beyond the aims, scope and resources of the current program.
A significant finding is that the majority of practitioners reported using SPR with local community members during the follow-up period. Of those practitioners who used any intervention, the majority used it with up to 10 community members during each time period. The data on practitioners’ use of SPR with community members was based on specified ranges (0, 1-10, 11-20, >20 people) that do not allow us to calculate the specific number of community members who received an SPR intervention. However, it is possible to estimate the minimum number of community members who received an SPR intervention in the 6 months following a practitioner attending training. During the first 3 months following practitioner training, practitioners reported using an SPR intervention with approximately 1,000 community members ((166 × 1) + (32 × 11) + (23 × 21) = 1001). During the subsequent 3 months, a minimum of almost 700 community members received an SPR intervention from a practitioner ((127 × 1) + (18 × 11) + (17 × 21) = 682). These conservative calculations suggest that many hundreds of community members received a SPR intervention provided by a practitioner in the 6 months following training of practitioners.
The most common barrier to using SPR interventions reported by practitioners was not having seen anyone with problems that required the use of those interventions. There are a number of potential explanations for this finding. First, some practitioners may have been working with clients who were coping well following the disaster, such as more resilient individuals or those who experienced minimal impact of the disaster. Second, given that the practitioner training sessions were run between August 2011 and June 2012, it is possible that some clients were coping and functioning reasonably well by the time practitioners were trained and in a position to commence using SPR interventions. Third, some practitioners may not have identified distress or coping difficulties in clients who were appropriate recipients of SPR interventions. Fourth, some practitioners may have judged, accurately or inaccurately, that SPR interventions were not appropriate for their client group (e.g., clients with a serious intellectual disability or mental health disorder). Unfortunately, it is not possible to determine which (or which combination) of these factors would help to explain practitioner reports that they had not seen anyone with problems requiring the use of SPR interventions.
Given that the SPR approach is derived from empirically-supported cognitive-behavioral psychological treatments, we were interested to assess whether a psychology professional background or CBT theoretical orientation of trainers and practitioners influenced their performance in the program. For trainers, professional background and theoretical orientation were unrelated to their competencies to facilitate SPR training sessions for practitioners. These findings suggest that, although SPR is derived from psychological interventions based on a CBT orientation, a diverse range of trainers were willing and able to deliver high quality SPR training for practitioners. For practitioners, psychologists were more confident in their ability to use SPR interventions compared with practitioners from other professional backgrounds. Specifically, psychologists were more confident to use all 5 ‘active’ SPR interventions at more than one time-point: Building Problem Solving Skills, Promoting Positive Activities, Managing Reactions, Promoting Helpful Thinking, and Rebuilding Healthy Social Connections. This may be explained by the fact that most psychologists would already be familiar with empirically-supported psychological interventions for mental health problems via their professional training. There was also some evidence that CBT practitioners were more confident to use Promoting Helpful Thinking and Managing Reactions than practitioners using other counselling approaches. These two interventions have considerable ‘cognitive’ content which may make it more difficult for non-CBT practitioners to develop their confidence and proficiency in these interventions. The findings that practitioners’ professional background and theoretical orientation were related to their confidence to use SPR interventions suggest that some practitioners may require additional support to assist them to use SPR interventions. Potentially, this additional support could include more opportunities to practice skills during extended training and/or case-based consultation or supervision following training. Ongoing supervision is likely to be necessary to bring about complex behavior change in less experienced trainees. Lyon and colleagues (2011) suggest that this could be augmented by the use of reminders such as the online modules utilized in the current program. As supervision is gradually tapered, a transition to peer coaching and reminders could continue to support sustained provider implementation of new practices. The supervision and peer support may be further enhanced by focusing on applying SPR to case examples (i.e., problem-based learning).
In conclusion, the evaluation of the SPR training and support program suggests that the aims of the program were largely met. The program developed enhanced capacity for many practitioners across Queensland to better respond to the needs of those affected by disasters and other stressful events. In addition, the program established a register of experienced SPR trainers that could be mobilized relatively quickly in the event of a future disaster or mass trauma. Most importantly, a substantial number of community members across Queensland affected by the devastating floods and cyclone in 2010-2011 were taught evidence-informed psychological skills to reduce distress and better cope with the adverse psychosocial effects of the disaster. We emphasize that a major goal of SPR is to provide early intervention to limit psychological distress; we did not evaluate the actual outcomes of the interventions, and so the efficacy of the SPR program remains untested. Despite this limitation, the current evaluation findings suggest that the program should be given consideration as a feasible and beneficial component of other psychosocial and mental health responses to Australian communities affected by disaster.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Acknowledgements
The authors would like to sincerely thank the trainers and practitioners who participated in the program. David Crompton from Queensland Health assisted with reviewing and writing the article.
Funding
The program was funded by the Queensland and Commonwealth governments as part of the Queensland Mental Health Natural Disaster Recovery Plan 2011-2013. The Queensland and Commonwealth governments as funders were not involved in the design of the evaluation, data analyses or interpretation of findings.
Ethical Statement
The program evaluation was approved by a Human Research Ethics Committee of the Queensland Government.
References
- 1.Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981-2001. Psychiatry 2002; 65:207-39. [DOI] [PubMed] [Google Scholar]
- 2.Bonanno GA, Galea S, Bucciarelli A, Vlahov D. What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. J Consulting Clinical Psychol 2007; 75:671-82. [DOI] [PubMed] [Google Scholar]
- 3.North CS, Pfefferbaum B. Mental health response to community disasters: A systematic review. JAMA 2013; 310:507-18; PMID:23925621; http://dx.doi.org/ 10.1001/jama.2013.107799 [DOI] [PubMed] [Google Scholar]
- 4.Forbes D, Fletcher S, Wolfgang B, Varker T, Creamer M, Brymer MJ, Ruzek JI, Watson P, Bryant RA. Practitioner perceptions of Skills for Psychological Recovery: a training programme for health practitioners in the aftermath of the Victorian bushfires. Australian and New Zealand J Psychiatry 2010; 44:1105-11. [DOI] [PubMed] [Google Scholar]
- 5.Australian Emergency Management Institute Disaster Health Handbook 1 Canberra: Australian Emergency Management Institute, 2011. [Google Scholar]
- 6.Wade D, Howard A, Fletcher S, Cooper J, Forbes D. Early response to psychological trauma: What GPs can do. Australian Family Physician 2013; 42:610-4; PMID:24024219 [PubMed] [Google Scholar]
- 7.Wade D, Forbes D, Nursey J, Creamer M. A multi-level framework to guide mental health response following a natural disaster. Bereavement Care 2012; 31:109-13; http://dx.doi.org/ 10.1080/02682621.2012.740285 [DOI] [Google Scholar]
- 8.Hobfoll SE, Watson P, Bell CC, Bryant RA, Brymer MJ, Friedman MJ, Friedman M, Gersons BP, de Jong JT, Layne CM. Five essential elements of immediate and mid-term mass trauma intervention: Empirical evidence. Psychiatry 2007; 70:283-315; http://dx.doi.org/ 10.1521/psyc.2007.70.4.283 [DOI] [PubMed] [Google Scholar]
- 9.Wade D, Varker T, Coates S, Fitzpatrick T, Shann C, Creamer M. A mental health training program for community members following a natural disaster. Disaster Health 2013; 1:9-12; http://dx.doi.org/ 10.4161/dish.22658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brymer M, Layne C, Jacobs A, Pynoos R, Ruzek J, Steinberg A, Vernberg E, Watson P. Psychological First Aid: Field operations guide, 2nd edition. 2006. [Google Scholar]
- 11.Forbes D, Creamer M, Bisson JI, Cohen JA, Crow BE, Foa EB, Friedman MJ, Keane TM, Kudler HS, Ursano RJ. A guide to guidelines for the treatment of PTSD and related conditions. J Traumatic Stress 2010; 23:537-52; PMID:20839310; http://dx.doi.org/ 10.1002/jts.20565 [DOI] [PubMed] [Google Scholar]
- 12.Berkowitz S, Bryant R, Brymer M, Hamblen J, Jacobs A, Layne C, Macy R, Osofsky H, Pynoos R, Ruzek J, et al.. Skills for Psychological Recovery: Field operations guide. The National Center for PTSD & the National Child Traumatic Stress Network, 2010. [Google Scholar]
- 13.Ehlers A, Clark DM, Hackmann A, McManus F, Fennell M. Cognitive therapy for post-traumatic stress disorder: development and evaluation. Behav Res Ther 2005; 43:413-31; PMID:15701354; http://dx.doi.org/ 10.1016/j.brat.2004.03.006 [DOI] [PubMed] [Google Scholar]
- 14.Roehrle B, Strouse J. Influence of social support on success of therapeutic interventions: A meta-analytic review. Psychotherapy 2008; 45:464-76; http://dx.doi.org/ 10.1037/a0014333 [DOI] [PubMed] [Google Scholar]
- 15.Cuijpers P, Van Straten A, Warmerdam L. Behavioral activation treatments of depression: A meta-analysis. Clinical Psychol Rev 2007; 27:318-26; PMID:17184887; http://dx.doi.org/ 10.1016/j.cpr.2006.11.001 [DOI] [PubMed] [Google Scholar]
- 16.Hansel TC, Osofsky HJ, Steinberg AM, Brymer MJ, Landis R, Riise KS, Gilkey S, Osofsky JD, Speier A. Louisiana spirit specialized crisis counseling: Counselor perceptions of training and services. Psychological Trauma-Theory Research Practice Policy 2011; 3:276-82; http://dx.doi.org/ 10.1037/a0024644 [DOI] [Google Scholar]
- 17.Orfaly RA, Frances JC, Campbell P, Whittemore B, Joly B, Koh H. Train-the-trainer as an educational model in public health preparedness. J Public Health Manag Pract 2005; 11:S123-S7; http://dx.doi.org/ 10.1097/00124784-200511001-00021 [DOI] [PubMed] [Google Scholar]
- 18.Cross W, Cerulli C, Richards H, He H, Herrmann J. Predicting dissemination of a disaster mental health “train-the-trainer” program. Disaster Med Public Health Prep 2010; 4:339-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hinds PJ, Patterson M, Pfeffer J. Bothered by abstraction: The effect of expertise on knowledge transfer and subsequent novice performance. J Applied Psychol 2001; 86:1232-43; PMID:11768064; http://dx.doi.org/ 10.1037/0021-9010.86.6.1232 [DOI] [PubMed] [Google Scholar]
- 20.Lyon AR, Stirman SW, Kerns SE, Bruns EJ. Developing the mental health workforce: review and application of training approaches from multiple disciplines. Adm Policy Ment Health 2011; 38:238-53; PMID:21190075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fairburn CG, Cooper Z. Therapist competence, therapy quality, and therapist training. Behav Res Ther 2011; 49:373-8; PMID:21492829; http://dx.doi.org/ 10.1016/j.brat.2011.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]


