Abstract
Ultra-pulsed fractional CO2 laser is an efficient, precise, and safe therapeutic intervention for skin refreshing, although accompanied with prolonged edema and erythema. In recent years, autologous platelet-rich plasma (PRP) has been proven to promote wound and soft tissue healing and collagen regeneration. To investigate whether the combination of PRP and ultra-pulsed fractional CO2 laser had a synergistic effect on therapy for facial rejuvenation. Totally, 13 facial aging females were treated with ultra-pulsed fractional CO2 laser. One side of the face was randomly selected as experimental group and injected with PRP, the other side acted as the control group and was injected with physiological saline at the same dose. Comprehensive assessment of clinical efficacy was performed by satisfaction scores, dermatologists' double-blind evaluation and the VISIA skin analysis system. After treatment for 3 months, subjective scores of facial wrinkles, skin texture, and skin elasticity were higher than that in the control group. Similarly, improvement of skin wrinkles, texture, and tightness in the experimental group was better compared with the control group. Additionally, the total duration of erythema, edema, and crusting was decreased, in the experimental group compared with the control group. PRP combined with ultra-pulsed fractional CO2 laser had a synergistic effect on facial rejuvenation, shortening duration of side effects, and promoting better therapeutic effect.
Keywords: : recovery time, adverse events, combination therapy, synergistic effect
Introduction
Skin aging is a common and complex biological process, characterized by wrinkles, epidermal and dermal atrophy, rough texture, pigmentation, telangiectasia, and skin laxity. It mainly results from chronological aging caused by factors in the internal environment such as heredity and photoaging induced by factors in the external environment such as ultraviolet radiation.1 Physical appearance is related to self-respect and personality, and influences acceptance level by others.2 Therefore, increasing attention have focused on the treatment of facial rejuvenation,3 and it is necessary to explore more effective treatment.
Aesthetic facial rejuvenation, can roughly be divided into operative and nonoperative procedures.4 Ultra-pulsed fractional CO2 laser, a nonoperative procedure, is widely used in antiaging because of its features of minimal invasion, simple operation, high tolerance, and favorable effect. It has therefore been regarded as the gold standard for facial rejuvenation treatment and severely photoaged skin.5 It works through creating multiple microthermal damage areas (called microscopic treatment zones, MTZ) with controllable width, depth, and density.6 Although the outcomes of resurfacing are optimistic, these are accompanied by adverse events such as erythema, edema, and pigmentation. These adverse effects extend recovery time and affect the normal work and life of recipients.
In recent years, platelet-rich plasma (PRP) has received extensive attention from oral surgery and craniofacial surgery.7 It is a small amount of plasma containing high concentration of platelets obtained from autologous whole blood after centrifugation. PRP plays a vital role in the process of wound healing through secretion of a large number of growth factors (GFs). These can stimulate cellular migration, proliferation, and angiogenesis.
A clinico-histopathologic study in rabbits confirmed that PRP treatment can achieve a faster wound healing rate.8 Autologous PRP application in oral surgery has been shown to significantly improve soft tissue healing.9 A pilot trial of full-thickness skin punch wounds conducted by Hom et al. indicated that autologous platelet gel (APG) may hasten wound closure and epithelialization. In addition, granulation formation appeared earlier when platelet count was six times as much as whole blood. In vitro experiments confirmed that APG was able to facilitate proliferation of endothelial cells.10 In the randomized controlled study of lumbar discogenic pain, participants who received intradiscal PRP injection showed improvement in pain.11 It is possible to expedite recovery and alleviate the burning sensation of laser treatment.
PRP, as a natural reservoir of GFs, is able to facilitate collagen of fibroblasts,12 keratinocyte proliferation, and hyaluronic acid generation to increase dermal elasticity, and may have a positive effect in facial rejuvenation.13
In this study, we aimed to investigate whether the combination of autologous PRP and ultra-pulsed fractional CO2 laser had a synergistic effect for facial rejuvenation and reduced occurrence of adverse reactions. We inferred that using PRP in ultra-pulsed fractional CO2 laser therapy may accelerate tissue repair and relieve pain. Combined application contributes to the reduction of adverse reactions produced by laser treatment and decreases downtime to achieve better results.
Materials and Methods
Participants
The study recruited a total of 13 female patients suffering from facial aging at the plastic surgery clinic of the General Hospital of Shenyang Military Region from January 2014 to August 2015. All participants were aged 32–57 years with the average age of 42.08 ± 7.37 and identified as skin type III or type IV according to the Fitzpatrick standard. Six patients were aged 30–40, five patients aged 40–50, and two patients were over age 50.
The exclusion criteria: (1) patients whose skin is prone to scar tissue; (2) patients with severe diabetes, hypertension, or cardiopulmonary insufficiency; (3) patients with a bleeding tendency or coagulation disorders; (4) patients with photosensitization or immunosuppressive diseases; (5) pregnant or lactating women; (6) patients who had received chemical peel, dermabrasion, soft tissue filling, botulinum toxin injection, mesotherapy or other resurfacing surgeries; (7) patients who had taken isotretinoin, vitamin A, vitamin C, or other drugs that affect collagen synthesis within 1 year; (8) patients who have suffered from mental disease, infectious disease, alcoholism, or drug abuse.
This study was conducted complying with the Declaration of Helsinki and with approval obtained from the Ethics Committee of the General Hospital of Shenyang Military Command. All the participants signed informed consent.
PRP preparation
PRP was extracted using a two-stage density gradient centrifugation method. About 30 mL venous blood were drawn in a sterile syringe containing 600 U heparin calcium (1 mL:10,000 U). The blood sample was centrifuged at 1200 r/min for 10 minutes. Subsequently, plasma, buffy coat, and 2–3 mm red blood cells were collected, mixed, and then centrifuged at 3500 r/min for 5 minutes. About 1/2 volume of platelet-poor plasma (PPP) was discarded, and the remaining PPP was resuspended to obtain PRP. Platelet count of all samples of whole blood and PRP were detected through Ac·T™ 5diff Hematology analyzer (Beckman Coulter, Inc., Brea, CA), and platelet concentration was 700 × 109/L to 1000 × 109/L. Lastly, PRP was adequately mixed with calcium gluconate at the ratio of 9:1 to activate platelets.
Treatment
Before treatment, all patients cleansed facial skin using a mild cleansing cream, medical records were written and images collected. The anesthetic compound lidocaine cream (Tsinghua Unisplendour Corporation Limited, Beijing, China) was coated on the facial treatment area for 1 hour. After satisfactory anesthesia, the treatment area was disinfected by iodophor, and then the iodine was removed using 75% alcohol for three times.
According to a random number table generated by Excel, PRP injection was performed to the left side of the face of the patients of the odd-numbered patients and to the right side of the face of the even-numbered patients. The side of the face receiving the PRP injection was considered the experimental side. The opposite side acted as the control and was injected with an equal dose of physiological saline. About nine points of PRP or physiological saline was injected into the cheeks, about six points was used to fill in the perioptic corium layer, and seven points in the forehead (0.1 mL per point) with a total volume of ∼2.2 mL.
After satisfactory injection, patients' eyes were carefully protected with eyeshades, and then both sides of the face were treated by ultra-pulsed fractional CO2 laser instrument (Mosaic eCO2; Lutronic Corporation, Goyang, Korea) with the same pulse energy. Instrument parameters: wavelength with 10,600 nm, pulse width 1.9–3.2 ms, pulse energy 125–225 mJ, micro hole density 100–120 MTZ/cm2, penetration depth 400 μm, spot size 3 × 3–6 × 6 mm in a rectangular or circular shape, treatment mode in static state, and repetition frequency one to two times. Ultimately, the laser treatment area was evenly coated with either PRP or physiological saline (about 1 mm) and covered with sterile gauze for 20–30 minutes.
All patients were warned to avoid water and sunshine for the following 7 days, and facial moisturizer and sunscreen care were conducted as previously after crusts spontaneously fell off. All 13 eligible subjects underwent three sessions of treatment at 3-month intervals.
Measurements
The VISIA Complexion Analysis System (Canfield Imaging Systems, Fairfield, NJ) was used to take images from the front, and 45° to the left and right lateral under the same conditions before treatment and after treatment for 3 months. Skin wrinkles, texture, and elasticity on both sides were objectively evaluated by the VISIA Complexion Analysis System.14
Subjective satisfaction was evaluated based on fine wrinkle status, skin texture, and elasticity after treatment. The scoring standard was as follows: no improvement, zero point; slight improvement, one point; mild improvement, two points and marked improvement, three points. Double-blind evaluation by two dermatologists: one point, postoperative images can be accurately identify a substantial improvement compared with preoperative images; −1 point, preoperative images were mistaken for postoperative images; zero point, preoperative images, and postoperative images could not be exactly distinguished. Neither dermatologist was aware of the scores given by the other. They didn't know which side injected PRP and which side injected physiological saline.
The duration of adverse events including erythema, edema, and crusting on bilateral face of all patients were recorded.
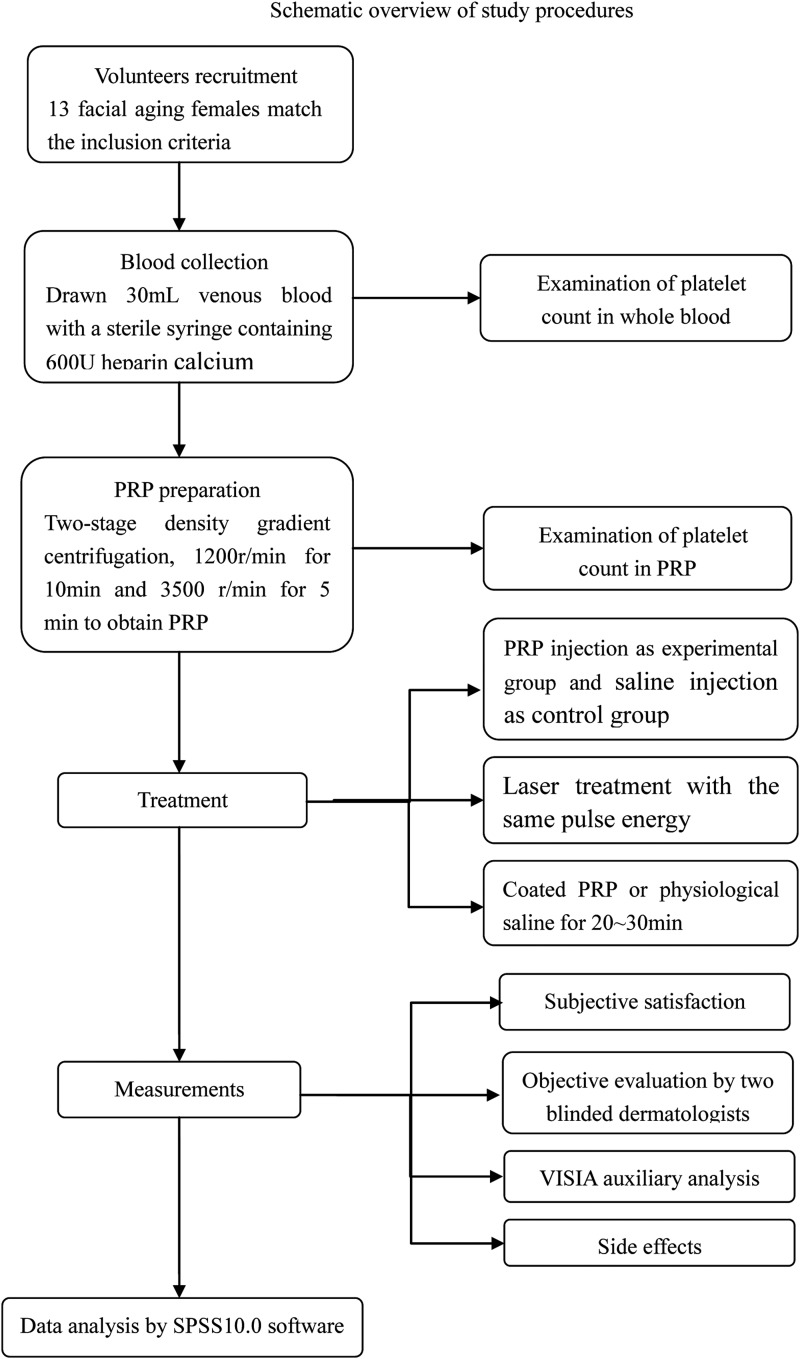
The study's procedures are presented in schematic overview (Fig. 1). Data were analyzed by SPSS10.0 software (IBM Corporation, New York, NY). The comparisons between before and after treatment were performed by paired t-test, p < 0.05 was considered statistically significant.
FIG. 1.
Schematic overview of autologous platelet-rich plasma (PRP) combined with ultra-pulsed fractional CO2 laser therapy for facial rejuvenation.
Results
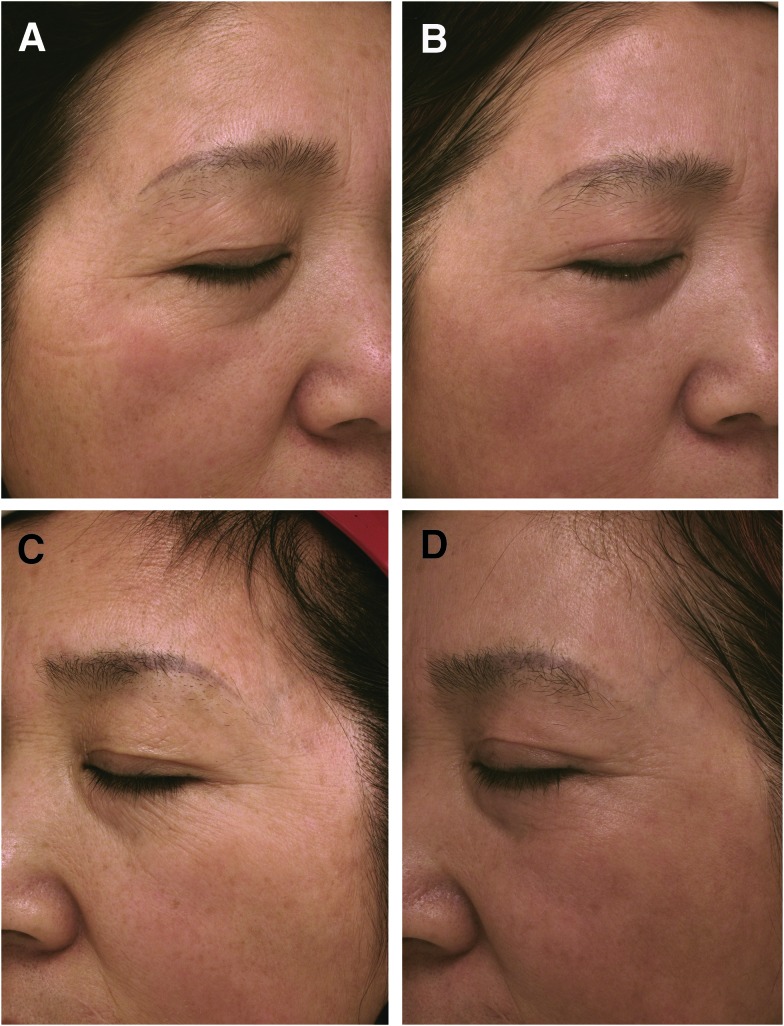
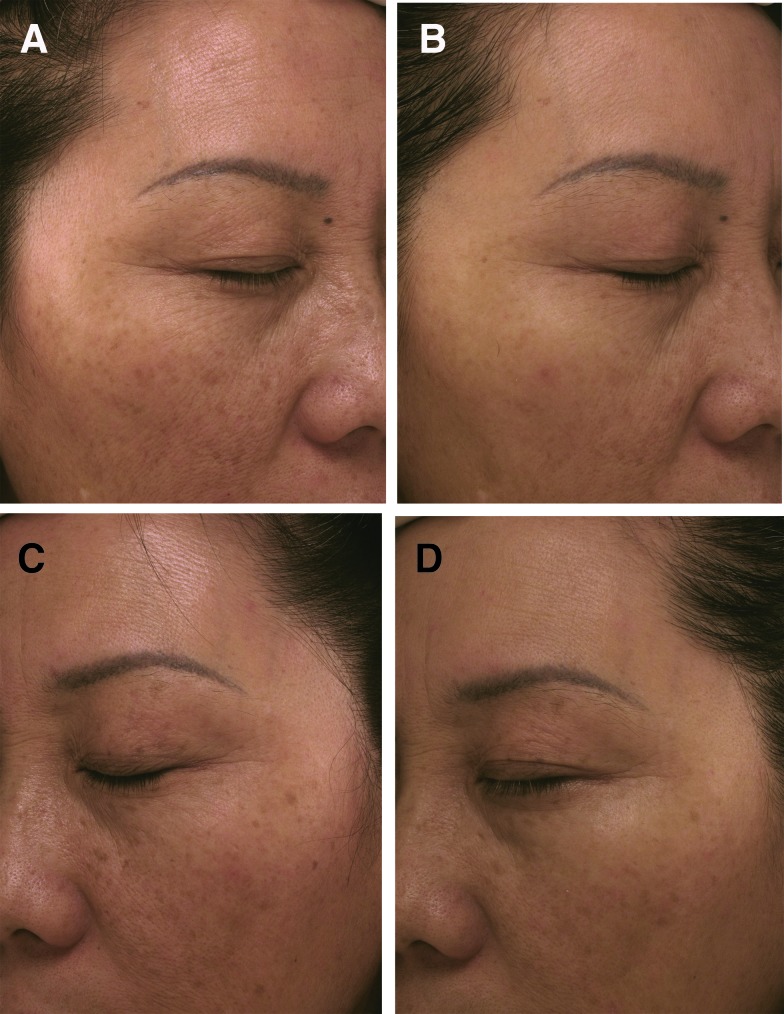
All patients completed treatment and postoperative follow-up and skin aging was significantly improved in the experimental group (Figs. 2 and 3).
FIG. 2.
A 57-year-old woman (A) experimental side before treatment, (B) experimental side after treatment for 3 months, (C) control side before treatment, (D) control side after treatment for 3 months. Skin aging was improved, wrinkles of forehead, periocular area were decreased, experimental side was better than that of control side.
FIG. 3.
A 52-year-old woman (A) experimental side before treatment, (B) experimental side after treatment for 3 months, (C) control side before treatment, (D) control side after treatment for 3 months. Skin aging was improved, wrinkles of forehead, periocular area were decreased, experimental side was better than that of control side.
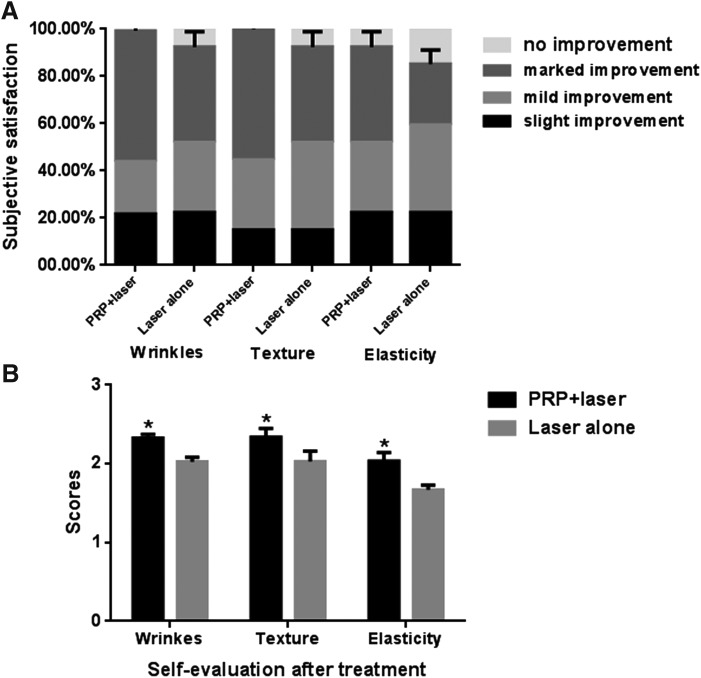
Self-evaluation
Satisfaction of patients in the experimental group and the control group were 76.92% and 69.23% in facial wrinkles, 84.62% and 76.92% in skin texture, 69.23% and 61.54% in skin elasticity, respectively. After treatment for 3 months, subjective scores of the PRP combined laser treatment group and the group treated by laser alone were 2.31 ± 0.85 and 2.01 ± 1.02 in facial wrinkles (p = 0.039), 2.38 ± 0.77 and 2.08 ± 0.95 in skin texture (p = 0.039), and 2.02 ± 0.90 and 1.69 ± 1.03 in skin elasticity (p = 0.040). There was significant difference between the two groups (Fig. 4).
FIG. 4.
Subjective satisfaction (A) of therapeutic effect on skin wrinkles, texture, and elasticity in experimental and control groups, self-evaluation scores (B) after treatment between experimental and control groups. Combination treatment of PRP and laser was superior to laser treatment alone. *p < 0.05 compared with control group.
The women were divided into three groups according to their age. Subjective scores of wrinkles, texture, and elasticity of the bilateral face were compared in different age ranges, separately. There were no significant differences between experimental and control groups (p > 0.05). The reason may be that the small sample would lead to a larger p value.
Objective clinical evaluation
Double-blind evaluation by two dermatologists showed that in experimental and control groups, satisfaction of improvement in facial wrinkles was 76.92% and 61.54%, respectively; satisfaction of improvement in skin texture was 84.62% and 69.23%, respectively; satisfaction of improvement in skin elasticity was 61.54% and 53.85%, respectively. The objective scores of the PRP combined laser treatment group and the group treated by laser alone were 0.77 ± 0.43 and 0.54 ± 0.66 in facial wrinkles, 0.85 ± 0.38 and 0.62 ± 0.65 in skin texture, and 0.54 ± 0.62 and 0.46 ± 0.60 in skin elasticity. Although the evaluation of combination therapy was better, there were no significant differences in objective scores of facial wrinkles, skin texture, and skin elasticity between the experimental and control groups.
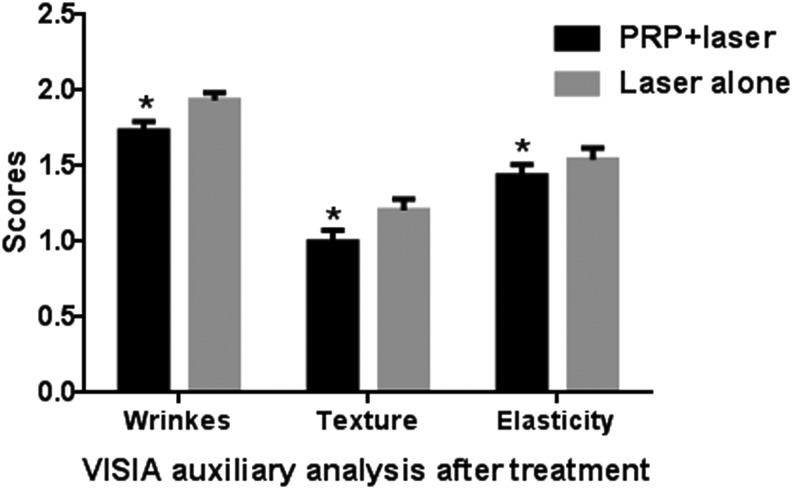
Furthermore, VISIA auxiliary analysis showed that there were no statistical differences in wrinkles (p = 0.466), texture (p = 0.507), and tightness (p = 0.325) before treatment between experimental and control groups. Obvious wrinkles, rough texture, and slack skin on both sides of the face were improved after treatment in both groups. In the experimental group and the control group after treatment, VISIA scores of skin wrinkles were 1.72 ± 0.58 and 1.94 ± 0.55, respectively (p = 0.145), texture was 0.99 ± 0.33 and 1.21 ± 0.42, respectively (p = 0.010), and elasticity was 1.41 ± 0.43 and 1.54 ± 0.47 (p = 0.026), respectively. Scores reflect area and density of wrinkles, texture and pores, and the smaller scores correspond to better skin status (Fig. 5).
FIG. 5.
VISIA auxiliary analysis of therapeutic effect on skin wrinkles, texture, and tightness before and after treatment in experimental and control groups. Combination treatment of PRP and laser was superior to laser treatment alone. Scores reflect area and density of wrinkles, texture, and pores, and the smaller scores correspond to better skin status. *p < 0.05 compared with control group.
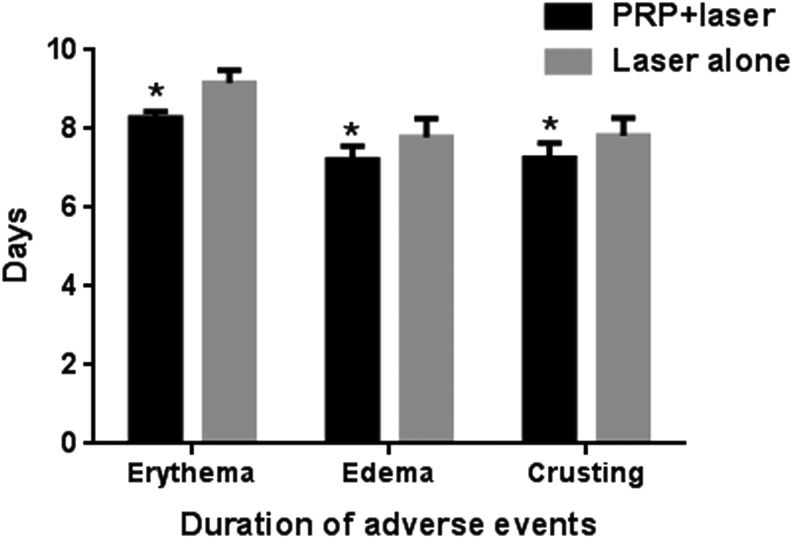
Side effects
The total duration of side effects in the experimental group and the control group was 8.31 ± 0.85 days and 9.08 ± 0.64 days of erythema (p = 0.025), 7.31 ± 0.48 days and 7.92 ± 0.64 days of edema (p = 0.013), 7.15 ± 0.38 days and 7.85 ± 0.80 of crusting (p = 0.032), respectively. Downtime in the combination group was shorter and the difference was statistically significant (Fig. 6).
FIG. 6.
Evaluation of total duration of adverse events in experimental and control groups. *p < 0.05 compared with control group.
Discussion
Facial rejuvenation is always a hot topic in the field of cosmetic plastic surgery. A variety of mechanisms causing skin aging have been proven, including declining growth capacity of skin tissue, decreased cell viability, disordered keratinocyte, reduced synthesis of collagen fiber in the dermis layer, and degeneration of elastic fibers.15 Currently, ultra-pulsed fractional CO2 laser is considered a safe, accurate, and effective treatment for facial rejuvenation,16 the mechanism was fractional photothermolysis theory.17,18
Ultra-pulsed fractional CO2 laser can promote fibroblasts metastasis, collagen regeneration and rearrangement, and connective tissue synthesis through creation of MTZ.19 The thermal effect of MTZ may not only induce hyperplasia and reorganization of collagen fiber, but also accelerate tissue recovery by directly vaporizing pigment group or pigment cells, accelerating skin metabolism, and promoting the regeneration of dermis and epidermis,20 thereby reducing or eliminating mild to moderate wrinkles, improving skin texture and color, shrinking pores, and relieving skin flabbiness, achieving the immediate and long-term effect of firming skin. However, because of activated pigment cells and darker skin color in Asian populations,21 several side effects caused by treatment, including long-term erythema, edema, and excessive pigmentation are inevitable.22,23
PRP plays a vital role in regulating angiogenesis through secreting a large number of GFs, including platelet-derived GF isoforms (PDGF-αα, PDGF-αβ, and PDGF-ββ), transforming GF-β isoforms (TGF-β1 and TGF-β2), vascular endothelial GF (VEGF), epithelial GF (EGF), basic fibroblast GF (bFGF), and insulin-like GF (IGF). The process of wound healing mainly depends on the formation of new blood vessels. As MTZ produced by ultra-pulsed fractional CO2 laser has similar histopathologic changes to those of wounds, we supposed that PRP-assisted laser therapy would accelerate healing and reduce side effects.
VEGF is involved in the control of proliferation, morphogenesis, migration and survival of endothelial cells, and regulation of angiogenesis. PDGF may assist vessels toward maturation. bFGF is known to participate in the inducing proliferation of endothelial progenitor cells, and inducing advanced endothelial progenitor to secrete VEGF in vitro. EGF is beneficial to endothelial cells proliferation and migration.24
VEGF may have a paracrine function on TGF-β indirect-acting angiogenesis. TGF-β has the ability to restrain kinase domain region gene expression in cultured endothelial cells, one of whose receptors bind to VEGF with high affinity.25 In the research regarding the embryonic stem cell differentiation model, TGF-β1 is provasculogenic in a VEGF-independent manner in the early stage of development. On the other hand, there is an inhibition effect on TGF-β1 sprouting angiogenesis when concentrations of VEGF exceed a certain value.26 Perhaps since the PRP was derived from patients themselves, TGF-β and VEGF exerted synergistic effects in appropriate proportion to promoted vascular regeneration, and then provided sufficient nutrition and oxygen for the repair of MTZs.
The network formed by fibrin and platelet further promoted the circulation of metabolites, and then shortened recovery phase of fractional laser treatment, and effectively reduced pigmentation.27,28 Antimicrobial proteins in PRP created an antibacterial environment through recruitment of some immune cells.29
In addition, PRP was reported to be associated with collagen expression, hyaluronic acid production, and fibroblast proliferation,30,31 which is the main mechanism in skin rejuvenation. The mechanism might be GFs such as IGF, EGF binding to the external surface of cell membranes of fibroblasts to activate signal protein to realize extracellular matrix synthesis and collagen remolding.32 TGF-β1 and PDGF is able to increase hyaluronic acid synthesis by upregulating the expression of hyaluronan synthase.30 Hyaluronic acid can draw water into the intercellular space and retain intracellular water, thus achieving skin elasticity.
We speculated that MTZs generated in the dermis by fractional photothermolysis provided a channel for PRP penetration and absorption. Subsequently, the synergistic effect of ultra-pulsed fractional CO2 laser and PRP provoked epidermal regrowth and dermal remodeling. Shin et al. verified that the amount of fibroblasts and collagen was higher in combination treatment via histological analysis.33
This is the first research to use the VISIA Complexion Analysis System in a clinical trial. The VISIA Complexion Analysis System is a convenient tool for dermatology detection. Our study referenced a split-face experiment to avoid individual differences, and to ensure that the skin had basically the same status before treatment. The data of subjective feelings and objective judgments both demonstrated that the experimental group had a faster recovery period, less duration of adverse events, and better therapeutic effect than that in the control group. This is probably the result of expedited repair of laser damage and collagen creation exerted by PRP.
Not all patients felt extremely satisfied with the resurfacing changes. This can probably be attributed to high expectations of patients. The relatively low satisfaction mainly comes from older woman with severe conditions. These patients need more treatments to achieve the desired effects. When these patients were divided into three groups based on their age, no statistical significance was found between combined treatment and single laser treatment. This may be attributed to small sample data in each age range.
Our study results proposed that PRP as an alternative method in laser therapy with the advantages of convenience, efficiency, and low cost. This test contributes to broaden the scope of cases in which ultra-pulsed fractional CO2 laser may be employed. To provide a personalized treatment strategy for every patient seeking cosmetic improvement, further research is necessary to develop the clinical application standard and determine the optimum concentration of PRP, and to establish a treatment course for different skin types.
Conclusion
Patients in the experimental group had faster recovery, less duration of adverse events, and better effects than that in the control group. No other side effects such as petechia, pigmentation, effusion, infection, keloid, blisters, and contact dermatitis were found after treatment. In the process of treatment, patients felt that searing pain caused by laser therapy was relieved by coating with PRP. In summary, combined application could not only effectively reduce facial wrinkles and texture, but also significantly relieve the coarse pores, pigmentation, and erythema caused by laser therapy. PRP and ultra-pulsed fractional CO2 laser had a synergistic effect on the therapy for facial rejuvenation.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Puizina-Ivic N. Skin aging. Acta Dermatovenerol Alp Pannonica Adriat 2008;17:47–54 [PubMed] [Google Scholar]
- 2.Kohl E, Meierhofer J, Koller M, Zeman F, Groesser L, Karrer S, Hohenleutner U, Landthaler M, Hohenleutner S. Fractional carbon dioxide laser resurfacing of rhytides and photoaged skin—a prospective clinical study on patient expectation and satisfaction. Lasers Surg Med 2015;47:111–119 [DOI] [PubMed] [Google Scholar]
- 3.Yaar M, Eller MS, Gilchrest BA. Fifty years of skin aging. J Investig Dermatol Symp Proc 2002;7:51–58 [DOI] [PubMed] [Google Scholar]
- 4.Kim BJ, Choi JH, Lee Y. Development of facial rejuvenation procedures: Thirty years of clinical experience with face lifts. Arch Plast Surg 2015;42:521–531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agrawal N, Smith G, Heffelfinger R. Ablative skin resurfacing. Facial Plast Surg 2014;30:55–61 [DOI] [PubMed] [Google Scholar]
- 6.Longo C, Galimberti M, De Pace B, Pellacani G, Bencini PL. Laser skin rejuvenation: Epidermal changes and collagen remodeling evaluated by in vivo confocal microscopy. Lasers Med Sci 2013;28:769–776 [DOI] [PubMed] [Google Scholar]
- 7.Freymiller EG, Aghaloo TL. Platelet-rich plasma: Ready or not? J Oral Maxillofac Surg 2004;62:484–488 [DOI] [PubMed] [Google Scholar]
- 8.Ostvar O, Shadvar S, Yahaghi E, Azma K, Fayyaz AF, Ahmadi K, Nowrouzian I. Effect of platelet-rich plasma on the healing of cutaneous defects exposed to acute to chronic wounds: A clinico-histopathologic study in rabbits. Diagn Pathol 2015;10:85. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 9.Dutta SR, Singh P, Passi D, Patter P. Mandibular third molar extraction wound healing with and without platelet rich plasma: A comparative prospective study. J Maxillofac Oral Surg 2015;14:808–815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hom DB, Linzie BM, Huang TC. The healing effects of autologous platelet gel on acute human skin wounds. Arch Facial Plast Surg 2007;9:174–183 [DOI] [PubMed] [Google Scholar]
- 11.Tuakli-Wosornu YA, Terry A, Boachie-Adjei K, Harrison JR, Gribbin CK, LaSalle EE, Nguyen JT, Solomon JL, Lutz GE. Lumbar intradiskal Platelet-Rich Plasma (PRP) injections: A prospective, double-blind, randomized controlled study. PM R 2016;8:1–10 [DOI] [PubMed] [Google Scholar]
- 12.Cho JM, Lee YH, Baek RM, Lee SW. Effect of platelet-rich plasma on ultraviolet b-induced skin wrinkles in nude mice. J Plast Reconstr Aesthet Surg 2011;64:e31–39 [DOI] [PubMed] [Google Scholar]
- 13.Yuksel EP, Sahin G, Aydin F, Senturk N, Turanli AY. Evaluation of effects of platelet-rich plasma on human facial skin. J Cosmet Laser Ther 2014;16:206–208 [DOI] [PubMed] [Google Scholar]
- 14.Goldsberry A, Hanke CW, Hanke KE. VISIA system: A possible tool in the cosmetic practice. J Drugs Dermatol 2014;13:1312–1314 [PubMed] [Google Scholar]
- 15.Makrantonaki E, Zouboulis CC. Molecular mechanisms of skin aging: State of the art. Ann N Y Acad Sci 2007;1119:40–50 [DOI] [PubMed] [Google Scholar]
- 16.Fitzpatrick RE, Goldman MP, Satur NM, Tope WD. Pulsed carbon dioxide laser resurfacing of photo-aged facial skin. Arch Dermatol 1996;132:395–402 [PubMed] [Google Scholar]
- 17.Cho SB, Jung JY, Ryu DJ, Lee SJ, Lee JH. Effects of ablative 10,600-nm carbon dioxide fractional laser therapy on suppurative diseases of the skin: A case series of 12 patients. Lasers Surg Med 2009;41:550–554 [DOI] [PubMed] [Google Scholar]
- 18.Helou J, Maatouk I, Obeid G, Moutran R, Stephan F, Tomb R. Fractional laser for vitiligo treated by 10,600 nm ablative fractional carbon dioxide laser followed by sun exposure. Lasers Surg Med 2014;46:443–448 [DOI] [PubMed] [Google Scholar]
- 19.Pinheiro NM, Crema VO, Millan BM, Carvalho FA, Mendonca AC. Comparison of the effects of carboxytherapy and radiofrequency on skin rejuvenation. J Cosmet Laser Ther 2015;17:156–161 [DOI] [PubMed] [Google Scholar]
- 20.Shamsaldeen O, Peterson JD, Goldman MP. The adverse events of deep fractional CO(2): A retrospective study of 490 treatments in 374 patients. Lasers Surg Med 2011;43:453–456 [DOI] [PubMed] [Google Scholar]
- 21.Omi T, Numano K. The role of the CO2 laser and fractional CO2 laser in dermatology. Laser Ther 2014;23:49–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alster TS, Bellew SG. Improvement of dermatochalasis and periorbital rhytides with a high-energy pulsed CO2 laser: A retrospective study. Dermatol Surg 2004;30(4 Pt 1):483–487; discussion 487. [DOI] [PubMed] [Google Scholar]
- 23.Fitzpatrick RE, Rostan EF, Marchell N. Collagen tightening induced by carbon dioxide laser versus erbium: YAG laser. Lasers Surg Med 2000;27:395–403 [DOI] [PubMed] [Google Scholar]
- 24.Martinez CE, Smith PC, Palma Alvarado VA. The influence of platelet-derived products on angiogenesis and tissue repair: A concise update. Front Physiol 2015;6:290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferrara N, Gerber HP. The role of vascular endothelial growth factor in angiogenesis. Acta Haematol 2001;106:148–156 [DOI] [PubMed] [Google Scholar]
- 26.Mallet C, Vittet D, Feige JJ, Bailly S. TGF beta1 induces vascu-logenesis and inhibits angiogenic sprouting in an embryonic stem cell differentiation model: Respective contribution of ALK1 and ALK5. Stem Cells 2006;24:2420–2427 [DOI] [PubMed] [Google Scholar]
- 27.Harris NL, Huffer WE, von Stade E, Larson AI, Phinney S, Purnell ML. The effect of platelet-rich plasma on normal soft tissues in the rabbit. J Bone Joint Surg Am 2012;94:786–793 [DOI] [PubMed] [Google Scholar]
- 28.Jeon YR, Kang EH, Yang CE, Yun IS, Lee WJ, Lew DH. The effect of platelet-rich plasma on composite graft survival. Plast Reconstr Surg 2014;134:239–246 [DOI] [PubMed] [Google Scholar]
- 29.Li H, Li B. PRP as a new approach to prevent infection: preparation and in vitro antimicrobial properties of PRP. J Vis Exp 2013. [Epub ahead of print]; doi: 10.3791/50351 [DOI] [PMC free article] [PubMed]
- 30.Anitua E, Sanchez M, Nurden AT, Zalduendo MM, de la Fuente M, Azofra J, Andia I. Platelet-released growth factors enhance the secretion of hyaluronic acid and induce hepatocyte growth factor production by synovial fibroblasts from arthritic patients. Rheumatology (Oxford) 2007;46:1769–1772 [DOI] [PubMed] [Google Scholar]
- 31.Kim DH, Je YJ, Kim CD, Lee YH, Seo YJ, Lee JH, Lee Y. Can platelet-rich plasma be used for skin rejuvenation? evaluation of effects of platelet-rich plasma on human dermal fibroblast. Ann Dermatol 2011;23:424–431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marx RE. Platelet-rich plasma: Evidence to support its use. J Oral Maxillofac Surg. 2004;62:489–496 [DOI] [PubMed] [Google Scholar]
- 33.Shin MK, Lee JH, Lee SJ, Kim NI. Platelet-rich plasma combined with fractional laser therapy for skin rejuvenation. Dermatol Surg. 2012;38:623–630 [DOI] [PubMed] [Google Scholar]