Report of Cases
Case 1
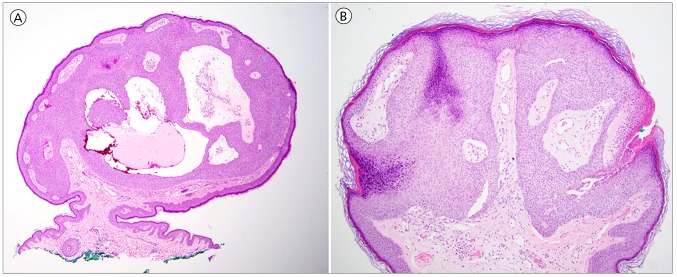
A man in his fifties with a history of Hodgkin lymphoma treated 20 years prior with the Stanford V protocol and mantle field radiation (total dose: 36 Gray) presented for skin examination. A 3 mm pedunculated pink papule was found on the right chest within the prior radiation field (Figure 1A). The lesion was asymptomatic and of unknown duration. There was no history of change, bleeding, or itching. Polarized dermoscopy of the papule revealed irregular linear and looped branching vessels that terminated in a semicircular or circular fashion, also termed “cherry-blossom” vessels (Figure 2A).
Figure 1.

Non-pigmented eccrine poroma. A) Clinical image showing a pink papule on the right upper chest. B) Clinical image showing a pink papule on the presternal chest. [Copyright: ©2017 Wolner et al.]
Figure 2.
Non-pigmented eccrine poroma. Polarized, non-contact dermoscopy images of a pedunculated pink papule with irregular branching vessels that terminate in circular and semi-circular structures. A is from Case 1 and B is from Case 2. [Copyright: ©2017 Wolner et al.]
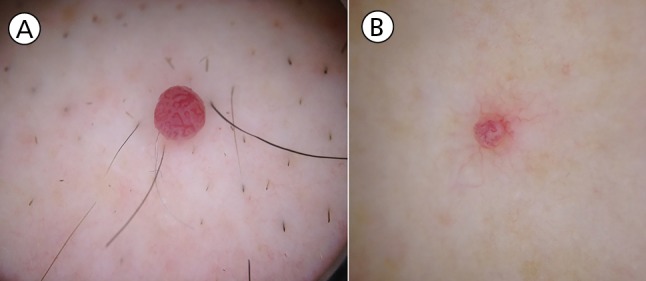
Histopathologic examination revealed a pedunculated well-circumscribed nodular epithelial tumor composed of uniform cuboidal cells with round basophilic monomorphic nuclei. Multiple broad cords of the anatomizing tumor epithelium connected to the overlying epidermis, surrounding characteristic sclerotic well-vascularized stroma (Figure 3A).
Figure 3.
A) Non-pigmented eccrine poroma: photomicrograph showing an exophytic, well-circumscribed nodular epithelial tumor with uniform cuboidal cells, round basophilic monomorphic nuclei, and sclerotic vascularized “poroma stroma” (hematoxylin-eosin stain, original magnification X20). B) Non-pigmented eccrine poroma: photomicrograph showing a pedunculated epithelial proliferation characterized by sharply demarcated broad epithelial downgrowths of cuboidal cells and characteristic sclerotic and vascular stroma (hematoxylin-eosin stain, original magnification X20). [Copyright: ©2017 Wolner et al.
Case 2
A woman in her fifties with a history of basal cell carcinoma and B-cell acute lymphoblastic leukemia status post two allogenic hematopoietic stem cell transplants (total body irradiation induction dose of: 13.75 Gy) presented for skin examination. A new, asymptomatic 2 mm pedunculated pink papule was found on the presternal chest (Figure 1B). Polarized dermoscopy of the lesion revealed semicircular/circular branching vessels originating from a common stem vessel (Figure 2B).
Histopathological examination revealed a polypoid epithelial tumor comprised of broad downgrowths of cuboidal epithelium clearly demarcated from overlying epidermis amidst a background of hyalized/sclerotic highly vascular stroma. Small ducts with a pink cuticle were noted within epithelial bands (Figure 3B).
What is the diagnosis?
Answer
Eccrine poroma
Discussion
Eccrine poromas are benign cutaneous adnexal neoplasms with terminal eccrine duct differentiation. In 2016, Ito et al reviewed 376 lesions and found that eccrine poromas occur most frequently on the lower extremities (44.4%), followed by the scalp (16.2%), trunk (11.7%), upper extremities (11.4%), face (9.8%), and neck (3.7%) [1]. Typically eccrine poromas appear as solitary plaques, papules, or nodules, but multiple tumors can be seen. Poromas commonly contain highly vascularized stroma but can uncommonly have pigmentation [2].
The differential diagnosis of a non-pigmented papule arising in the field of prior radiotherapy should include amelanotic melanoma, squamous cell carcinoma, adnexal neoplasm, and basal cell carcinoma. Interestingly, eccrine poromas have been associated with radiotherapy and hematologic malignancy [3,4].
The dermoscopic features of nonpigmented eccrine poromas are variable (Table 1). A “polymorphous” vascular pattern consisting of hairpin, glomerular, and irregular linear vessels in a single lesion has been frequently described [3,5–15]. The most common features include a structureless pink-white background (48%), hairpin (loop) vessels (47%), “frog-egg appearance” (39%), glomerular vessels (35%), red lacunae (27%), ulcers (24%), linear-irregular vessels (23%), and leaf-like or cherry-tree vessels (21%). The cases described herein showed irregular branching and looped vessels that terminated in semicircular or circular structures, which raised the suspicion for eccrine poroma [7,11]. These vascular structures may correlate with localization of proliferative vessels within the curved “canals” of tumor stroma.
TABLE 1.
A literature search identified eleven case reports and series identifying dermoscopic characteristics of nonpigmented eccrine poromas [3,5–15]
| Author/Year | Cases N | Hairpin or Loop Vessels N (%) | Dotted Vessels N (%) | Linear-Irregular Vessels N (%) | Vascular Blush N (%) | Comedo-Like Openings N (%) | Milia-like cysts N (%) | Ulcer N (%) | Cherry-blossom vessels N (%) | Structureless-Pink white areas N (%) | Glomerular vessels N (%) | Red Lacunae N (%) | Frog egg or reddish/white globules w/interlacing white cords N (%) | White-to-pink halo N (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Shalom et al (2012) | 19 | 9 (47%) | – | – | 12 (63%) | – | – | 8 (42%) | 8 (42%) | 15 (79%) | 10 (53%) | 2 (11%) | 9 (47%) | – |
| Espinosa et al (2012) | 13 | 5 (38%) | – | 3 (23%) | – | – | – | 3 (23%) | 4 (31%) | 9 (69%) | 2 (15%) | 9 (69%) | 5 (38%) | – |
| Minagawa et al (2010) | 10 | 4 (40%) | 3 (30%) | 2 (20%) | – | 1 (10%) | 1 (10%) | 1 (10%) | – | – | – | – | 9 (90%) | – |
| Ferrari et al (2009) | 7 | 5 (71%) | – | 3 (43%) | – | – | – | 1 (14%) | – | 5 (71%) | 5 (71%) | – | 1 (14%) | 5 (71%) |
| Lallas et al (2015) | 6 | 2 (33%) | 2 (33%) | 2 (33%) | – | 1 (17%) | – | 1 (17%) | – | – | 1 (17%) | 1 (17%) | – | 2 (33%) |
| Avilés–Izquierdo et al (2009) | 2 | 2 (100%) | – | 2 (100%) | – | – | – | – | – | – | 2 (100%) | 2 (100%) | – | – |
| dos Santos (2015) | 1 | – | 1 (100%) | – | – | – | – | – | – | – | – | 1 (100%) | – | 1 (100%) |
| Aydingoz (2009) | 1 | – | – | – | – | – | – | – | 1(100%) | – | – | – | – | – |
| Nicolino et al (2007) | 1 | – | – | 1 (100%) | – | – | – | – | – | – | 1 (100%) | 1 (100%) | – | 1 (100%) |
| Altamura et al (2005) | 1 | 1 (100%) | 1 (100%) | 1 (100%) | – | – | – | 1 (100%) | – | – | – | 1 (100%) | – | – |
| Sgouros et al (2013) | 1 | 1 (100%) | – | 1 (100%) | – | – | – | – | – | 1 (100%) | 1 (100%) | – | – | – |
| TOTAL | 62 | 29 (47%) | 7 (11%) | 15 (24%) | 12 (19%) | 2 (3%) | 1 (2%) | 15 (24%) | 13 (21%) | 30 (48%) | 22 (35%) | 17 (27%) | 24 (39%) | 9 (15%) |
Variation among dermoscopic characteristics reported in the literature can depend on whether contact and/or polarized dermoscopy was used, the location of the lesion, or variation in the angles of the tumor and the dermatoscope [10]. Larger studies are needed to determine the sensitivity and specificity of the dermoscopic criteria for eccrine poroma.
References
- 1.Ito K, Ansai SI, Fukumoto T, Anan T, Kimura T. Clinicopathological analysis of 384 cases of poroid neoplasms including 98 cases of apocrine type cases. J Dermatol. 2016 May 14; doi: 10.1111/1346-8138.13421. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 2.Bolognia J, Jorizzo JL, Schaffer JV. Dermatology. Philadelphia: Elsevier Saunders; 2012. [Google Scholar]
- 3.Miura T, Yamamoto T. Eruptive poromatosis following radiotherapy. Am J Dermatopathol. 2013;35(5):615–617. doi: 10.1097/DAD.0b013e3182743abe. [DOI] [PubMed] [Google Scholar]
- 4.Mahlberg MJ, McGinnis KS, Draft KS, Fakharzadeh SS. Multiple eccrine poromas in the setting of total body irradiation and immunosuppression. J Am Acad Dermatol. 2006;55(2 Suppl):S46–49. doi: 10.1016/j.jaad.2006.02.052. [DOI] [PubMed] [Google Scholar]
- 5.Altamura D, Piccolo D, Lozzi GP, Peris K. Eccrine poroma in an unusual site: a clinical and dermoscopic simulator of amelanotic melanoma. J Am Acad Dermatol. 2005;53(3):539–541. doi: 10.1016/j.jaad.2005.02.057. [DOI] [PubMed] [Google Scholar]
- 6.Ferrari A, Buccini P, Silipo V, et al. Eccrine poroma: a clinical-dermoscopic study of seven cases. Acta Derm Venereol. 2009;89(2):160–164. doi: 10.2340/00015555-0608. [DOI] [PubMed] [Google Scholar]
- 7.Aydingoz IE. New dermoscopic vascular patterns in a case of eccrine poroma. J Eur Acad Dermatol Venereol. 2009;23(6):725–726. doi: 10.1111/j.1468-3083.2009.03182.x. [DOI] [PubMed] [Google Scholar]
- 8.Aviles-Izquierdo JA, Velazquez-Tarjuelo D, Lecona-Echevarria M, Lazaro-Ochaita P. [Dermoscopic features of eccrine poroma]. Actas Dermosifiliogr. 2009;100(2):133–136. [PubMed] [Google Scholar]
- 9.Minagawa A, Koga H, Takahashi M, Sano K, Okuyama R. Dermoscopic features of nonpigmented eccrine poromas in association with their histopathological features. Br J Dermatol. 2010;163(6):1264–1268. doi: 10.1111/j.1365-2133.2010.10017.x. [DOI] [PubMed] [Google Scholar]
- 10.Shalom A, Schein O, Landi C, Marghoob A, Carlos B, Scope A. Dermoscopic findings in biopsy-proven poromas. Dermatol Surg. 2012;38(7 Pt 1):1091–1096. doi: 10.1111/j.1524-4725.2012.02407.x. [DOI] [PubMed] [Google Scholar]
- 11.Espinosa AED, Ortega BC, Venegas RQ, Ramírez RG. Dermoscopy of non-pigmented eccrine poromas: study of Mexican cases. Dermatol Pract Concept. 2013;3(1):25–28. doi: 10.5826/dpc.0301a07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sgouros D, Piana S, Argenziano G, et al. Clinical, dermoscopic and histopathological features of eccrine poroid neoplasms. Dermatology. 2013;227(2):175–179. doi: 10.1159/000354152. [DOI] [PubMed] [Google Scholar]
- 13.dos Santos BS. Clinical and dermoscopic features of eccrine poroma. Indian J Dermatol Venereol Leprol. 2015;81(3):308–309. doi: 10.4103/0378-6323.154787. [DOI] [PubMed] [Google Scholar]
- 14.Nicolino R, Zalaudek I, Ferrara G, et al. Dermoscopy of eccrine poroma. Dermatology. 2007;215(2):160–163. doi: 10.1159/000104270. [DOI] [PubMed] [Google Scholar]
- 15.Lallas A, Chellini PR, Guimaraes MG, et al. Eccrine poroma: the great dermoscopic imitator. J Eur Acad Dermatol Venereol. 2016;30(10):e61–e63. doi: 10.1111/jdv.13302. [DOI] [PubMed] [Google Scholar]