Abstract
Primary cutaneous CD 30 (+) anaplastic large cell lymphoma (PCALCL) is a rare and indolent type of cutaneous T cell lymphoma, which usually presents as an asymptomatic solitary firm nodule that rapidly grows and often ulcerates without any systemic involvement.
A 64-year-old female presented to our outpatient clinic with a one-year history of multiple pink nodular lesions on the chest, back and gluteal regions. Dermoscopic examination of the nodular lesions revealed pink-to-yellow structureless areas and arborizing-to-polymorphous vessels. Histopathologic examination was consistent with CD30 (+) anaplastic large cell lymphoma. Systemic involvement was not detected. Local radiotherapy for large nodules and surgical excision for small nodules were performed. The large nodules had totally regressed after 10 sessions of radiotherapy.
Keywords: anaplastic large cell lymphoma, dermoscopy, radiotherapy
Introduction
Anaplastic large cell lymphoma (ALCL) is a rare and indolent type of mature T cell lymphoma, which is composed of large atypical lymphocytes with pleomorphic, anaplastic, or immunoblastic cytomorphology [1]. Clinical manifestations include primary cutaneous type and secondary cutaneous involvement from the systemic type of ALCL [1]. The primary cutaneous form is characterized by cutaneous lesions without systemic involvement and usually presents with asymptomatic, solitary, grouped, multicentric, or generalized tumors that may ulcerate and spontaneously regress [1,2].
The diagnosis of these tumoral lesions is usually made by clinical findings, histologic and immunophenotypic examinations. We present a case of primary cutaneous CD 30 (+) anaplastic large cell lymphoma assessed by dermoscopy that responded very well to local radiotherapy.
Case Report
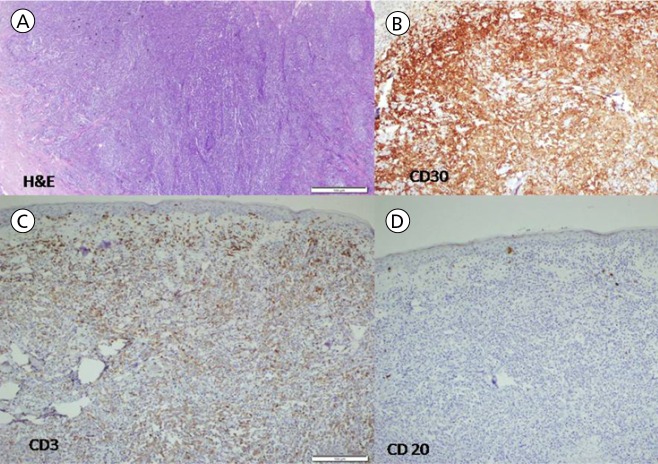
A 64-year-old female was admitted to our outpatient clinic with a one-year history of multiple pink nodular lesions of a few millimeters and centimeters in diameter on the chest, back and gluteal regions (Figure 1). Dermoscopic examination of the nodular lesions revealed pink-to-yellow structureless areas and polymorphous vessels (Figure 2). The largest nodular lesion on the right scapular region was totally excised for diagnosis. Total excision of the nodular lesion on the back revealed diffuse dermal cellular infiltration histologically (hematoxylin & eosin staining [H&E]). (Figure 3A) The infiltration consisted of large atypical cells with CD3, CD4 and CD30 positivity (Figure 3B and C) on immunohistochemical examination, as well as negativity for anaplastic lymphoma kinase and CD20 staining (Figure 3D). She was diagnosed as CD30 (+) ALK (−) anaplastic large cell lymphoma.
Figure 1.

Multiple pink nodular lesions of a few millimeters and centimeters in diameter on chest and back. [Copyright: ©2017 Uzuncakmak et al.]
Figure 2.
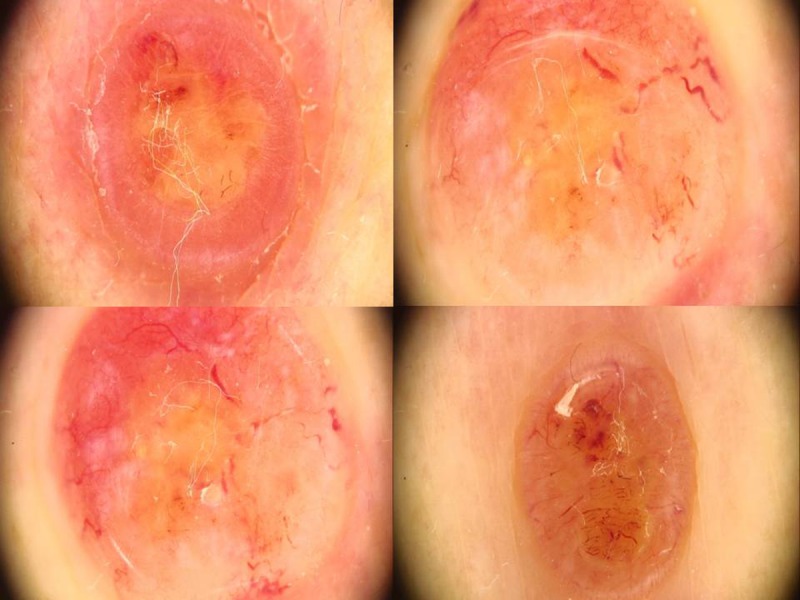
Pink-to-yellow structureless areas and arborizing-to-polymorphous vessels with non-polarized dermoscopy. [Copyright: ©2017 Uzuncakmak et al.]
Figure 3.
Total excision specimen of the nodular lesion on back revealed diffuse dermal cellular infiltration (H&E) (A). The infiltration consisted of large atypical cells with CD3, CD4 and CD30 positivity (B, C) immunohistochemically, as well as negativity for anaplastic lymphoma kinase and CD20 staining (D). [Copyright: ©2017 Uzuncakmak et al.]
Systemic scanning for metastasis, including complete blood count, routine biochemistry, flow cytometry and body scanning with tomography were totally normal.
Local radiotherapy for large nodules and surgical excision for small nodules were performed. Almost all of the nodular lesions had totally regressed after 10 sessions of radiotherapy. She has been under follow up without any recurrence for one year.
Discussion
Primary cutaneous anaplastic large cell lymphoma (PCALCL) is a rare type of CD 30 (+) cutaneous lymphomas, which represents 10% of all cases [3]. For the correct diagnosis, the following criteria are important: no evidence or history of lymphomatoid papulosis, mycosis fungoides or other lymphoma, no extracutaneous lesion at presentation, and predominance (>75%) of large clusters of CD30+ blast cells in the skin biopsy [3]. Although there are pediatric case reports in the literature, it is more common in adults aged between 45 and 60 years. The clinical presentation includes rashes, plaques, nodules and tumors with central ulceration on the trunk and extremities that may spontaneously regress [1,3–5]. Recurrence is common, but systemic involvement is rare, with secondary regional lymphadenopathy seen in only a quarter of cases [3]. Imaging tests, such as computerized tomography of the neck, chest and abdomen, are required for staging and in order to differentiate the primary from the systemic form involving the skin. Bone marrow biopsy and skin biopsy are also mandatory for staging. In our patient these tests were negative for systemic involvement.
Histologic and immunophenotypic examinations are mandatory for the diagnosis of PCALCL. Histologically PCALCL is characterized by diffuse, pleomorphic, anaplastic, or immunoblastic, non-epidermotropic lymphoid infiltrates with cohesive sheets of large CD30+ tumor cells, oval or irregularly shaped nuclei, prominent eosinophilic nucleoli and abundant cytoplasm with a high mitotic index. Immunohistochemistry is essential for the determination of the CTCL subtype and in the differentiation between primary and secondary disease [3,4].
Dermoscopic findings of cutaneous lymphomas are not very well known and usually focused on mycosis fungoides [6]. Mascolo et al recently reported the dermoscopic findings of a series of cutaneous B cell lymphomas. In their series, the most common dermoscopic features were white circles, yellow-to-salmon-colored background/areas, scales and/or arborizing vessels [7]. Similarly, in our patient we observed pink-to-yellow structureless areas and polymorphous vessels especially visible at the periphery of the nodular lesions. We think this yellow/salmon colored background may be helpful in the differential diagnosis of cutaneous lymphomas from amelanotic melanoma.
Surgical excision and local radiotherapy are the primary treatment options for localized PCALCL [2,8–10] Surgery is a highly effective treatment option, but relapse is also very common [2,3]. Chemotherapy is used mainly for patients with multifocal, generalized lesions or relapsed disease [3]. In our patient we performed surgical excision of the small nodules and local radiotherapy for the larger lesions, which almost totally regressed after 10 sessions of radiotherapy.
In conclusion, our case of anaplastic large cell lymphoma is a good example in underlining the importance of dermoscopy for the differential diagnosis of pink nodules. In the presence of the pink-yellow color and polymorphous vessels, the possibility of lymphoma should be taken into consideration.
Footnotes
Funding: None.
Competing interests: The authors have no conflicts of interest to disclose.
References
- 1.Asha LK, Thomas D, Binitha MP, Nandakumar G. Primary cutaneous multifocal CD30+ anaplastic large cell lymphoma. Indian J Dermatol Venereol Leprol. 2006;72:376–378. doi: 10.4103/0378-6323.27758. [DOI] [PubMed] [Google Scholar]
- 2.Huang BS, Chen WY, Wang CW, et al. Relapse pattern and treatment outcome of curative radiotherapy for primary cutaneous CD30 + anaplastic large-cell lymphoma: a retrospective cohort study. Acta Derm Venereol. 2016;96:394–395. doi: 10.2340/00015555-2260. [DOI] [PubMed] [Google Scholar]
- 3.Rao SD, Ravi R, Govindarajan M. Primary cutaneous CD 30+ anaplastic large cell lymphoma. Indian J Surg. 2010;72:283–285. doi: 10.1007/s12262-010-0091-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daar G, Küpeli S, Yalçin B, et al. Primary cutaneous anaplastic large cell lymphoma. Pediatr Hematol Oncol. 2010;27:558–563. doi: 10.3109/08880018.2010.493575. [DOI] [PubMed] [Google Scholar]
- 5.Cao C, Zeng K, Wang M, et al. Primary cutaneous anaplastic large-cell lymphoma: a case report. Dermatol Ther. 2016;29(4):224–227. doi: 10.1111/dth.12340. [DOI] [PubMed] [Google Scholar]
- 6.Lallas A, Apalla Z, Lefaki I, et al. Dermoscopy of early stage mycosis fungoides. J Eur Acad Dermatol Venereol. 2013;27(5):617–21. doi: 10.1111/j.1468-3083.2012.04499.x. [DOI] [PubMed] [Google Scholar]
- 7.Mascolo M, Piccolo V, Argenziano G, et al. Dermoscopy pattern, histopathology and immunophenotype of primary cutaneous B-cell lymphoma presenting as a solitary skin nodule. Dermatology. 2016;232:203–207. doi: 10.1159/000442251. [DOI] [PubMed] [Google Scholar]
- 8.Turrión-Merino L, Perez-Gala S, Hermosa-Zarza E, et al. Primary cutaneous CD30+ anaplastic large cell lymphoma treated with radiotherapy and methotrexate with development of xanthomas at the sites of prior disease. J Cutan Pathol. 2016;43:400–405. doi: 10.1111/cup.12661. [DOI] [PubMed] [Google Scholar]
- 9.Yokoi I, Ishikawa E, Koura A, et al. Successful treatment of primary cutaneous anaplastic large cell lymphoma with intralesional methotrexate therapy. Acta Derm Venereol. 2014;94:319–320. doi: 10.2340/00015555-1692. [DOI] [PubMed] [Google Scholar]
- 10.Patsinakidis N, Kreuter A, Moritz RK, et al. Complete remission of refractory, ulcerated, primary cutaneous CD30+ anaplastic large cell lymphoma following brentuximab vedotin therapy. Acta Derm Venereol. 2015;95:233–234. doi: 10.2340/00015555-1874. [DOI] [PubMed] [Google Scholar]