Abstract
Background:
In patients who have undergone anterior cruciate ligament reconstruction (ACLR), the effect of neuromuscular re-education (NMR) programs on standard hop tests outcomes, including limb symmetry indices (LSIs), is unknown.
Hypothesis:
Both legs will show improvement in hop test–measured units after neuromuscular training, but the involved leg will show relatively greater improvement leading to improved limb symmetry. Patients younger than 18 years will show more improvement than patients who are older.
Study Design:
Retrospective cohort study.
Level of Evidence:
Level 3.
Methods:
Patients self-selected their participation in this NMR program, which was completed after traditional outpatient physical therapy. Pre– and post–hop test scores were recorded as the primary outcome measure.
Results:
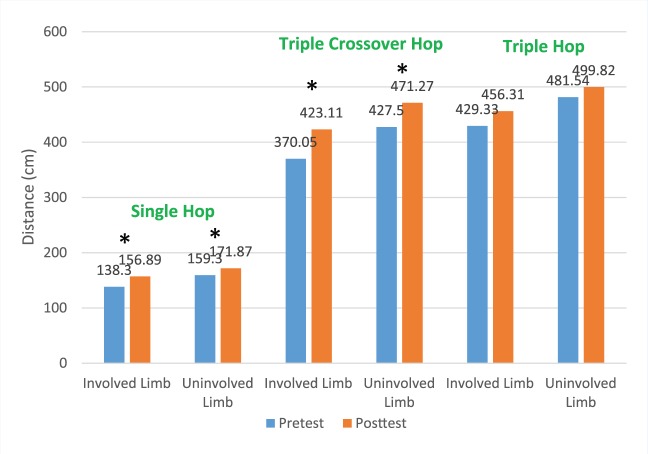
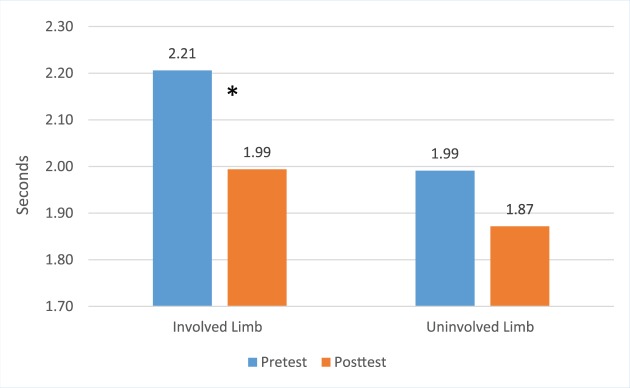
Seventy-one patients met the inclusion criteria and completed hop testing. Overall, the involved leg showed significant improvements (pretest/posttest) for single-leg hop (138.30 cm/156.89 cm), triple crossover hop (370.05 cm/423.11 cm), and timed hop (2.21 s/1.99 s). Similarly, on the uninvolved leg, improvements were seen for the single-leg hop (159.30 cm/171.87 cm) and triple crossover hop (427.50 cm/471.27 cm). Overall mean limb symmetry improved across all 4 hop tests, but there was significant improvement only on the single-leg hop (87% pretest to 92% posttest). Patients younger than 18 years showed mean significant LSI improvement on the triple crossover hop.
Conclusion:
Utilizing an intensive 6-week NMR program after ACLR prior to return to sport can improve quantitative hop test measurements. Patients younger than 18 years had greater improvement than those 18 years and older.
Clinical Relevance:
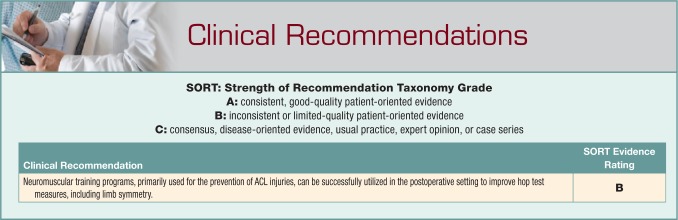
Advanced NMR programs can be successfully utilized in the postoperative ACLR setting to improve quantitative limb symmetry.
Keywords: ACL, hop testing, neuromuscular re-education, limb symmetry
Anterior cruciate ligament (ACL) injuries are common in the young, active population and necessitate a large percentage of patients to undergo ACL reconstruction (ACLR) surgery at a substantial cost, both monetarily and in time invested in rehabilitation and recovery. This procedure is commonly performed with the dual goals of returning to sport and potentially avoiding secondary injuries to the articular cartilage, menisci, and other ligamentous restraints.7 A large percentage of these ACL injuries, especially in female adolescents, are noncontact and occur during a deceleration, lateral pivoting, or landing task often associated with high external joint load.10,12 Poor form or technique such as increased knee abduction moments12 or frontal plane trunk displacement30 coupled with a high-risk sporting maneuver may occur due to a lack of neuromuscular control. This may be a modifiable risk factor for reducing both primary12,30 and secondary25 ACL injuries. Previous studies address these common neuromuscular control deficits with specific exercises targeted at improving technique and fundamental strength required to control knee joint kinematics and therefore reducing injury risk.9,11,18,20
One example of a neuromuscular re-education (NMR) program aimed at preventing ACL injuries is the Prevent injury and Enhance Performance (PEP) program.9 It was specifically designed to be performed as a 15-minute warm-up prior to soccer practices 3 days per week. Significant decreases in ACL injuries were observed during the soccer season9 and at 2-year follow-up16 for athletes who received this intervention. A progressive 3-phase jump training program has shown decreased ACL injuries in a trained group of female high school athletes.11 Similarly, plyometric, core strengthening, resistance, and speed training exercises in uninjured female athletes improved valgus torques after landing from a jump.20 In a more intensive NMR program18 that advances through 5 stages of progressively challenging plyometric, hamstring, and core strengthening exercises, uninjured controls showed decreased valgus knee angles after a drop vertical jump,11 increased hamstring torques,13 and overall reduced noncontact ACL injury risk.20 Previous meta-analyses have found conflicting evidence in support of ACL injury prevention programs.28,29
Although ACLR is a common procedure and rehabilitation approaches are constantly evolving,21,30 current data indicate that only 40% to 60%1,2,8 of patients are able to return to prior level of sporting activities. In addition to fear of reinjury, poor knee function is commonly cited as one of the primary reasons athletes choose to terminate athletic participation.2,19 Returning to prior level of competitive sport may necessitate increased levels of intervention not attained via traditional rehabilitation. To address this possibility, plyometric-based training is commonly performed to reduce reinjury risk via education of proper jump landing technique, while also potentially improving athletic function. While multiple studies have shown that prophylactic preventative NMR programs decrease the incidence of primary ACL injuries,11,12,19 it is unknown whether postoperative neuromuscular training leads to a decrease in secondary ACL injuries.
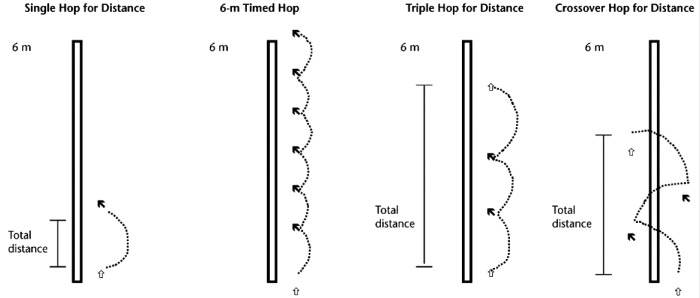
A successful outcome after ACLR relies not only on proper surgical intervention and evidence-based rehabilitation programs but also appropriate testing to gauge physical readiness for return to sport. Whereas previous return to sport clearance was predominantly time dependent,3,14 use of functional assessments can facilitate a safer return to sports for competitive athletes.21 The most frequently utilized comparative testing metrics are the 4 hop tests23: single-hop for distance, triple-hop for distance, triple crossover hop for distance, and 6-meter single-leg timed hop (Figure 1). A combination of the 4 hop tests is a reliable and valid performance-based outcome measure for patients undergoing rehabilitation after ACLR.26 Additionally, the timed hop and triple crossover hop are predictors of self-reported knee function after ACLR.15
Figure 1.
The 4 hop tests. Reprinted with permission from Reid et al.26
The primary purpose of this study was to determine whether ACL prevention programs can be implemented as a postoperative ACLR tool to improve hop tests and limb symmetry. The secondary purpose was to determine whether a group of younger age patients would benefit more than older patients. Our hypothesis was that both legs would show absolute improvements but that the reconstructed leg would show greater relative improvements. We also hypothesized that younger patients would show relatively greater improvement in limb symmetry index (LSI) scores compared with older patients.
Methods
This study was approved by the University of Minnesota Institutional Review Board prior to initiation of the study.
Prior to the 6-month functional assessment, traditional physical therapy sessions included an emphasis on restoring basic impairments of range of motion, strength, and proprioception before progressing to later-stage exercise progressions of agility, plyometrics, and core strengthening. Based on acceptable functional testing results and physician clearance, patients could then choose to voluntarily enroll in our sport-specific NMR program prior to return to sport.
Inclusion criteria for this study were postoperative primary ACLR in patients of any age. Concomitant meniscectomy, meniscus repair, or chondroplasty were included. Exclusion criteria were previous ACLR, multiligament reconstructions, or significant biologic cartilage repairs, meniscus transplant, or previous contralateral knee injury. Patients who had a pretest less than 4 months or longer than 7 months from ACLR were excluded, as were those who had longer than 60 days between pre- and posttest. Chart reviews were performed on patients who met inclusion criteria, and demographic data, including age, sex, and body mass index (BMI), were recorded.
The unique sport-specific rehabilitation program used in this study is a trunk and hip NMR program based on previously published programs: the PEP program9 (approximately 20 minutes) and plyometric exercise progressions18 (approximately 60 minutes). Additional independently generated agility and core stabilization exercises designed to target common deficits in the postoperative ACLR patient (approximately 30 minutes) are also included. This training is of a significantly increased intensity, frequency, and duration compared with traditional therapy. Similar to comparable programs, the program meets twice per week for 5 weeks with each training session lasting 2 hours, combining for a total of 20 hours of training. In addition to the functional testing required for acceptance to the program, pre- and postprogram testing is completed on separate sessions 6 weeks apart, of which the hop tests are included. The program is conducted in a group gym setting of no more than 6 participants, with 1 physical therapist and 1 certified athletic trainer who give frequent feedback to ensure proper technique and modified exercise progressions based on individual needs.
The results of the standard hop tests were evaluated as the primary outcome measure. Comparing the involved to uninvolved leg for the 4 tests generates the LSI, which is expressed as a percentage. Scores were calculated for single-hop for distance, triple-hop for distance, triple crossover hop for distance, and 6-meter timed hop. Hop tests were conducted by having individuals perform 3 trials of each exercise beginning with the uninvolved limb followed by the involved limb. For the 3 distance hop tests, the LSI was calculated by taking the best score of the involved limb and dividing it by the best score of the uninvolved limb. The opposite calculation was performed for the timed hop, where the uninvolved limb was divided by the involved limb. A stopwatch was used for timing the 6-meter timed hop test, and best times were used to calculate the percentage.
A paired Student t test was performed to determine differences between mean pre– and post–hop test scores in the involved leg, uninvolved leg, and LSI. The Student t test was significant when P < 0.05. The Student t test was also used to compare hop test improvement based on age group (age ≥18 years vs <18 years).
Results
There were 71 nonconsecutive, self-selected subjects (44 women) who participated in the NMR program after ACLR. The overall mean age was 20.15 years (range, 12-46 years), and the mean BMI was 24.39 kg/m2 (Table 1). Patients started the program a mean 174 days postoperative, and the mean duration from pretest to posttest was 37 days.
Table 1.
Study population demographic information
| ≥18 y | <18 y | Total | |
|---|---|---|---|
| Total | 27 | 44 | 71 |
| Men | 14 | 13 | 27 |
| Women | 13 | 31 | 44 |
| Body mass index, kg/m2 | 26.2 | 23.3 | 24.4 (range, 15.9-34.1) |
| Age, y | 26.1 | 15.9 | 20.2 (range, 12-46) |
| Days postoperative to pretest | 175 | 172 | 174 (range, 120-210) |
| Days between pre- and posttest | 37 | 37 | 37 (range, 21-57) |
The overall mean hop test scores for both the involved and uninvolved legs across the 4 hop tests can be found in Table 2, with Figures 2 and 3 representing the data graphically. Figure 4 demonstrates mean LSI scores across the 4 hop tests at both pre- and posttest. Tables 3 and 4 list the hop test scores broken down by age stratification.
Table 2.
Overall mean hop test scores
| Pretest | Posttest | CI Pretest | CI Posttest | P Value a | |
|---|---|---|---|---|---|
| Single-leg hop | |||||
| Involved limb, cm | 138.30 | 156.89 | 2.90 | 3.37 | 0.001 |
| Uninvolved limb, cm | 159.30 | 171.87 | 2.96 | 3.59 | 0.038 |
| LSI, % | 0.87 | 0.92 | 0.03 | 0.03 | 0.023 |
| Triple crossover hop | |||||
| Involved limb, cm | 370.05 | 423.11 | 8.45 | 7.88 | 0.001 |
| Uninvolved limb, cm | 427.50 | 471.27 | 9.62 | 9.27 | 0.012 |
| LSI, % | 0.87 | 0.91 | 0.03 | 0.02 | 0.089 |
| Triple-hop distance | |||||
| Involved limb, cm | 429.33 | 456.31 | 11.16 | 12.01 | 0.206 |
| Uninvolved limb, cm | 481.54 | 499.82 | 11.94 | 13.79 | 0.440 |
| LSI, % | 0.90 | 0.92 | 0.04 | 0.03 | 0.489 |
| Timed hop | |||||
| Involved limb, s | 2.21 | 1.99 | 0.12 | 0.10 | 0.008 |
| Uninvolved limb, s | 1.99 | 1.87 | 0.09 | 0.08 | 0.060 |
| LSI, % | 0.91 | 0.95 | 0.03 | 0.02 | 0.066 |
CI, confidence interval; LSI, limb symmetry index.
Boldfaced numbers indicate statistical significance.
Figure 2.
Group mean hop test distances for both involved and uninvolved limbs in the single hop, triple crossover hop, and triple hop (cm) at both pretest and posttest. *Statistical significance.
Figure 3.
Group mean hop test results for both involved and uninvolved limbs in the timed hop, both pretest and posttest. *Statistical significance.
Figure 4.
Mean limb symmetry index scores across the 4 hop tests. Limb symmetry index was calculated at both pretest and posttest. *Statistical significance.
Table 3.
Mean hop test scores for patients <18 years
| Pretest | Posttest | CI Pretest | CI Posttest | P Value a | |
|---|---|---|---|---|---|
| Single-leg hop | |||||
| Involved limb, cm | 134.82 | 154.19 | 3.69 | 4.44 | 0.011 |
| Uninvolved limb, cm | 154.22 | 169.17 | 3.39 | 4.57 | 0.045 |
| LSI, % | 0.87 | 0.91 | 0.04 | 0.02 | 0.082 |
| Triple crossover hop | |||||
| Involved limb, cm | 361.62 | 424.18 | 11.08 | 10.12 | 0.002 |
| Uninvolved limb, cm | 415.96 | 464.17 | 11.41 | 10.52 | 0.018 |
| LSI, % | 0.87 | 0.91 | 0.03 | 0.02 | 0.043 |
| Triple-hop distance | |||||
| Involved limb, cm | 427.95 | 447.3 | 14.46 | 14.05 | 0.462 |
| Uninvolved limb, cm | 479.31 | 478.04 | 13.87 | 13.88 | 0.960 |
| LSI, % | 0.90 | 0.94 | 0.05 | 0.05 | 0.260 |
| Timed hop | |||||
| Involved limb, s | 2.22 | 1.95 | 0.14 | 0.12 | 0.005 |
| Uninvolved limb, s | 2.02 | 1.85 | 0.10 | 0.09 | 0.022 |
| LSI, % | 0.92 | 0.96 | 0.03 | 0.03 | 0.055 |
CI, confidence interval; LSI, limb symmetry index.
Boldfaced numbers indicate statistical significance.
Table 4.
Mean hop test scores for patients ≥18 years
| Pretest | Posttest | CI Pretest | CI Posttest | P Value | |
|---|---|---|---|---|---|
| Single-leg hop | |||||
| Involved limb, cm | 143.89 | 161.24 | 4.66 | 5.14 | 0.058 |
| Uninvolved limb, cm | 167.48 | 176.20 | 5.32 | 5.84 | 0.397 |
| LSI, % | 0.87 | 0.93 | 0.05 | 0.05 | 0.142 |
| Triple crossover hop | |||||
| Involved limb, cm | 383.30 | 421.43 | 13.00 | 12.81 | 0.111 |
| Uninvolved limb, cm | 445.64 | 482.42 | 16.99 | 17.29 | 0.245 |
| LSI, % | 0.88 | 0.89 | 0.05 | 0.05 | 0.664 |
| Triple-hop distance | |||||
| Involved limb, cm | 431.05 | 467.58 | 17.96 | 20.86 | 0.312 |
| Uninvolved limb, cm | 484.34 | 527.03 | 21.05 | 25.30 | 0.323 |
| LSI, % | 0.90 | 0.90 | 0.07 | 0.05 | 0.867 |
| Timed hop | |||||
| Involved limb, cm | 2.18 | 2.06 | 0.21 | 0.18 | 0.385 |
| Uninvolved limb, cm | 1.95 | 1.90 | 0.16 | 0.17 | 0.688 |
| LSI, % | 0.90 | 0.93 | 0.05 | 0.04 | 0.477 |
CI, confidence interval; LSI, limb symmetry index.
Discussion
Asymmetries after ACLR persist for years after surgery,4,24,27 and more dynamic tasks that reproduce sport-specific movements will typically accentuate the movement abnormalities of these athletes.22 The drop vertical jump landing task has shown significant kinematic asymmetries at both the hip and knee, as well as force generation and attenuation in athletes up to 4 years after ACLR.4,6,24 Previous research has demonstrated hop test improvements after NMR programs in an uninjured population.20 Our data demonstrate significant quantitative improvements in standardized hop testing after an intensive 6-week NMR program in the postoperative ACLR population. Specifically, the hop tests demonstrated absolute improvements in both involved and uninvolved legs and an improved LSI score for the single-leg hop. Despite the unknown clinical significance, post–hop test scores cleared the 85% to 90% LSI threshold that has been recommended as normal hop test function,17,23 and this improvement occurred in a relatively short period of time.
All hop tests across both groups showed pre- to posttest improvement, but only the changes in the younger group demonstrated significant improvement in P value. Another trend that becomes clear when comparing age categories is that across the majority of the hop tests, the older age group showed the same or lower pre- and posttest LSI numbers compared with the younger age group. Although there was improvement on all 4 tests in the older age group, it appears there may be a ceiling effect in this group.
In addition to being used to gauge readiness for return to sport, hop tests can be predictive of self-reported function in the postoperative ACLR population. Patients who have undergone ACLR with subjectively rated knee function below normal ranges were more likely to have a 6-meter timed hop less than the 88% cutoff than those with knee function within normal ranges.15 Also, patients with normal ranges of knee function were more likely to have a triple crossover hop LSI of greater than 95% than those with knee function below normal ranges. Lower LSI scores were seen in ACLR patients who did not return to sports compared with those who did.17 Taken together, it is understood that poor performance on hop tests is often correlated with worse subjectively reported function. After 6 weeks of intensive plyometric training, significant improvement can occur in hop test scores and may improve patient subjective reporting as well.
Limitations of this study include that there was no control group. Although hop test symmetry remains a common objective tool to measure return to sport readiness, this does not guarantee return to preinjury status.5 Because of the retrospective nature of the study, surgical methodology or graft type was not controlled for, and the total number of ACLRs performed is unknown. In addition, it was not possible to determine the compliance of patients to traditional rehabilitation prior to entering the NMR program, although patients were required to complete a functional test and get physician clearance prior to beginning the NMR program. The generalizability to other postoperative knee populations remains unknown.
Conclusion
Utilizing an intensive 6-week NMR program after ACLR prior to return to sport, improvements in standard hop measures in both involved and uninvolved limbs as well as improved LSI scores were achieved. Patients younger the than age of 18 may benefit most from such programs.
Acknowledgments
The authors would like to acknowledge Gregory Govrik, PT, DPT; Rachel Hakanson, PT, DPT, OCS; Chad Kofoed, PT, DPT, OCS; Amanda LeValley, MS, ATC; William Yungtum, MS, ATC; and Michael Obermeier, MS, ATC.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Arden CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45:596-606. [DOI] [PubMed] [Google Scholar]
- 2. Arden CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011;39:538-543. [DOI] [PubMed] [Google Scholar]
- 3. Barber-Westin SD, Noyes FR. Objective criteria for return to athletics after anterior cruciate ligament reconstruction and subsequent reinjury rates: a systematic review. Phys Sportsmed. 2011;39:100-110. [DOI] [PubMed] [Google Scholar]
- 4. Castanharo R, da Luz BS, Bitar AC, D’Elia CO, Castropil W, Duarte M. Males still have limb asymmetries in multijoint movements tasks more than 2 years following anterior cruciate ligament reconstruction. J Orthop Sci. 2011;16:531-535. [DOI] [PubMed] [Google Scholar]
- 5. Chung KS, Ha JK, Yeom CH, et al. Are muscle strength and function of the uninjured lower limb weakened after anterior cruciate ligament injury? Two-year follow-up after reconstruction. Am J Sports Med. 2015;43:3013-3021. [DOI] [PubMed] [Google Scholar]
- 6. Delahunt E, Sweeney L, Chawke M, et al. Lower limb kinematic alterations during drop vertical jumps in female athletes who have undergone anterior cruciate ligament reconstruction. J Orthop Res. 2012;30:72-78. [DOI] [PubMed] [Google Scholar]
- 7. Dunn WR, Spindler KP. Predictors of activity level two years after anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010;38:2040-2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eitzen I, Moksnes H, Snyder-Mackler L, Risberg MA. A progressive 5 week exercise therapy program leads to significant improvement in knee function early after anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2010;40:705-721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gilchrist J, Mandelbaum BR, Melancon H, et al. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008;36:1476-1483. [DOI] [PubMed] [Google Scholar]
- 10. Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:216-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hewett TE, Lindenfeld TN, Riccobene JB, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999;27:699-706. [DOI] [PubMed] [Google Scholar]
- 12. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33:492-501. [DOI] [PubMed] [Google Scholar]
- 13. Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes: decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24:765-773. [DOI] [PubMed] [Google Scholar]
- 14. Kvist J. Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports Med. 2004;34:269-280. [DOI] [PubMed] [Google Scholar]
- 15. Logerstedt D, Grindhem H, Lynch A, et al. Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: the Delaware-Oslo ACL cohort study. Am J Sports Med. 2012;40:2348-2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing the incidence of anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33:1003-1010. [DOI] [PubMed] [Google Scholar]
- 17. Muller U, Kruger-Franke M, Schmidt M, Rosemeyer B. Predictive parameters for return to pre-injury level of sport 6 months following anterior cruciate ligament reconstruction surgery. Knee Surg Sports Traumatol Arthrosc. 2015;23:3623-3631. [DOI] [PubMed] [Google Scholar]
- 18. Myer G, Chu DA, Brent JE, Hewett TE. Trunk and hip control neuromuscular training for the prevention of knee joint injury. Clin Sports Med. 2008;27:425-448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Myer GD, Ford KR, Brent JL, Hewett TE. Differential neuromuscular training effects on ACL injury risk factors in “high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007;8:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower extremity biomechanics in female athletes. J Strength Cond Res. 2005;19:51-60. [DOI] [PubMed] [Google Scholar]
- 21. Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36:385-402. [DOI] [PubMed] [Google Scholar]
- 22. Myer GD, Schmitt LC, Brent JL, et al. Utilization of modified NFL Combine testing to identify functional deficits in athletes following ACL reconstruction. J Orthop Sports Phys Ther. 2011;41:377-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Noyes FR, Barber SD, Mangine RE. Abnormal limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513-518. [DOI] [PubMed] [Google Scholar]
- 24. Paterno MV, Ford KR, Myer GD, Heyl R, Hewett TE. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sports Med. 2007;17:258-262. [DOI] [PubMed] [Google Scholar]
- 25. Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968-1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR. Hop testing provides a reliable and valid outcome measuring during rehabilitation after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2007;87:337-349. [DOI] [PubMed] [Google Scholar]
- 27. Roewer BD, Di Stasi SL, Snyder-Mackler L. Quadriceps strength and weight acceptance strategies continue to improve two years after anterior cruciate ligament reconstruction. J Biomech. 2011;44:1948-1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sadoghi P, von Keudell A, Vavken P. Effectiveness of anterior cruciate ligament injury prevention training programs. J Bone Joint Surg. 2012;94:769-776. [DOI] [PubMed] [Google Scholar]
- 29. Stevenson JH, Beattie CS, Schwartz JB, Busconi BD. Assessing the effectiveness of neuromuscular training programs in reducing the incidence of anterior cruciate ligament injuries in female athletes: a systematic review. Am J Sports Med. 2014;43:482-490. [DOI] [PubMed] [Google Scholar]
- 30. Zazulak BT, Hewett TE, Reeves NP, Golderg B, Chokewick J. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med. 2007;35:1123-1130. [DOI] [PubMed] [Google Scholar]