Abstract
Context:
Low back pain is reported by more than half of cyclists. The pathomechanics and association of risk factors of lumbar spine overuse injuries in cycling are not clearly understood.
Objective:
To determine whether relationships exist between body positioning, spinal kinematics, and muscle activity in active cyclists with nontraumatic low back pain.
Data Sources:
In August of 2015 and April of 2016, a comprehensive search of the PubMed, CINAHL, Ovid MEDLINE, and Scopus databases was performed independently by 5 reviewers.
Study Selection:
Included articles consisted of biomechanical studies examining factors relating to low back pain in cyclists as agreed upon by group consensus.
Study Design:
Systematic review.
Level of Evidence:
Level 4.
Data Extraction:
Five reviewers appraised by consensus each article using the Downs and Black checklist.
Results:
Eight studies met criteria for this review. There is evidence that cyclists with lower handlebar heights displayed increased lumbosacral flexion angles during cycling. Core muscle activation imbalances, back extensor endurance deficits, and increased lumbar flexion while cycling were found to be present in cyclists with low back pain.
Conclusion:
Spinal and core muscle activation imbalances in a prolonged flexed posture associated with cycling may lead to maladaptive spinal kinematics and increased spinal stresses contributing to overuse low back pain.
Keywords: cycling, low back pain, muscle activity, spinal kinematics
In cycling, the occurrence of traumatic and nontraumatic (overuse) injuries is about equal,12 with approximately 23 million cyclists developing at least 1 overuse injury in their lifetime in the United States alone.6,22,35 The majority (51.5%) of cycling-related injuries reported over a 4-year period were considered due to overuse.5,12 Of these overuse injuries, low back pain (LBP) is the most prevalent.10,13 Fifty-eight percent of professional cyclists reported LBP, of which 41% sought medical attention, and up to 22% of cyclists with LBP lost time from activity.10
During cycling, various positions are used to achieve proper aerodynamics to increase speed and efficiency, including lumbar spine flexion.7,20,31,32 A flexed spinal position commonly adopted by cyclists inverts the physiologic intervertebral angle, changing the area of spinal loading.32 Sustained or repeated lumbar flexion is associated with LBP,8,11,29 and the term flexion pattern disorder describes positional changes that occur in conjunction with nontraumatic LBP.7,14,28 Core stability is essential to increase cycling power.1,32 Bicycle component settings affect spine position during cycling, which subsequently impacts cycling efficiency.19 Thus, it is hypothesized that altered spinal kinematics or core muscle activation patterns, combined with the prolonged repetitive nature of the activity, lead to lumbar overuse injury.
Several mechanisms are hypothesized for the pathomechanics of LBP in cyclists, including mechanical creep (a deformation or strain of ligaments that occurs with constant loading), disc ischemia, muscle fatigue, and overactivation of back extensors. Another mechanism is the flexion-relaxation phenomenon, in which deactivation of the erector spinae and/or multifidus muscles with a flexed spine causes vertebral body loading to shift to the passive spine structures of the spine, thus increasing risk to ligaments and intervertebral discs.15,21,22 However, there is little scientific evidence to support these mechanisms.15,22 Furthermore, several risk factors are related to LBP in cyclists, including muscle activation asymmetries, flexibility, bicycle fit, and training volume; however, the evidence in an early systematic review was not strong.22,24 Of these risk factors, bike fit shows the strongest relationship with LBP in cyclists.13,17,22,31 A 10° to 15° change in anterior tilt of the saddle eliminated LBP in 29 of 40 cyclists and decreased pain in 8 others.31 However, the impact of bike fit on overuse LBP in cyclists in relation to the other risk factors is unclear. Thus, the aim of this systematic review is to determine whether relationships exist between body positioning, spinal kinematics, and spinal muscle activity in cyclists with nontraumatic LBP and how bike fit affects these factors.
Methods
Search Strategy
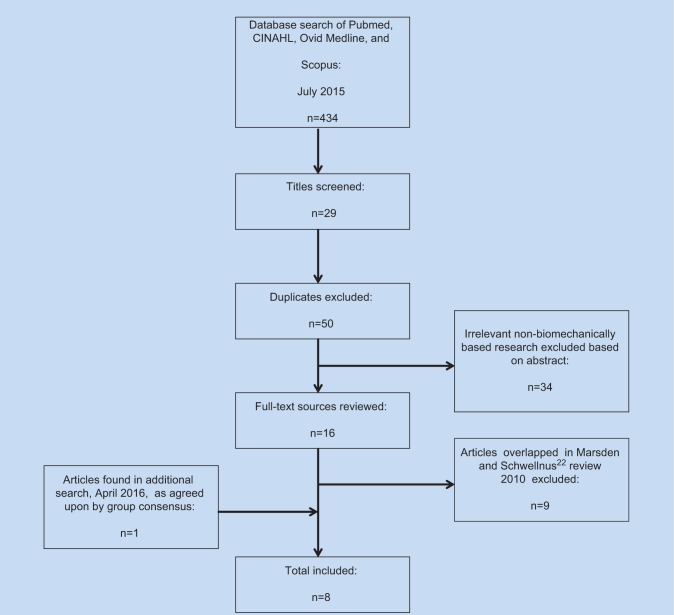
The initial search was performed on July 16, 2015, using the following databases: PubMed, CINAHL, Ovid MEDLINE, and Scopus, focusing on cyclists with nontraumatic LBP. The initial search included the general terms cycling, cyclists, bicycling, LBP, overuse injury, and back pain in the following combinations across databases: cycling AND low back pain, cyclists AND low back pain, cyclists AND overuse injury, bicycling AND back pain. Search results were compiled and screened for titles of relevance using group consensus. Duplicates across databases were removed, resulting in 50 articles (Figure 1).
Figure 1.
Flowchart of the systematic search and article inclusion for the studies analyzed in this systematic review.
Selection Criteria
Of the 50 articles selected, abstracts were screened based on inclusion criteria of biomechanical studies examining LBP in cyclists as agreed upon by group consensus. Studies included were comparison studies, cross-sectional studies, and case-based studies evaluating muscle activity and characteristics, spinal position or angles, and bicycle in subjects experiencing nontraumatic LBP, nonspecific LBP, or overuse LBP. Studies prior to 2007 that were included in the systematic review by Marsden and Schwellnus22 were excluded to focus on the most current literature (Figure 1). An additional search was conducted on April 1, 2016, using the same methodology as the original search (Figure 1).
Data Collection
Five reviewers read and then discussed articles meeting the selection criteria. Articles were graded using the Downs and Black quality assessment scale for assessment of methodological quality and risk of bias, and all grades were assigned based on group consensus.16 The Downs and Black scale is considered a valid and reliable checklist for nonrandomized studies and was deemed most appropriate due to the observational nature of the included studies.16,18 Data extracted from articles included participant population, variables measured, and conclusions (see the Appendix, available at http://sph.sagepub.com/content/by/supplemental-data).
Results
Study Selection
Of the 50 articles in the initial search, 16 were deemed eligible based on inclusion criteria. Nine articles were excluded due to inclusion in the review by Marsden and Schwellnus.22 From the second search, 1 additional article was deemed eligible, resulting in a total of 8 included studies (see the Appendix). The number of subjects ranged from 1 to 120 subjects, with a total of 255 subjects.
Study Characteristics
Studies included only men, aged 18 to 57 years (weight, 54.43-72.57 kg; height, 1.6-1.85 m). Four studies utilized a within-participant study design, 3 a case-control design, and 1 was a single case study. Six studies included participants with cycling experience, ranging from elite,25 master,25 professional,23 professional competitive off-road,30 competitive,34 and unspecified,4 with no definitions provided for these categories. Two studies3,9 included participants without cycling experience. Four studies23,25,33,34 reported cycling experience ranging from 6 to 17 years. Three studies4,30,33 compared participants with and without LBP.
Assessment of Included Studies
Four studies3,4,33,34 had sample sizes of less than 20 participants, which limits statistical power. The median Downs and Black score of the studies was 12 of 27, with the highest score of 20. Therefore, studies were of low to moderate quality.18 No blinding occurred in any studies.
Methodology and Outcomes Measured Across Studies
Methodology and outcomes measured varied across studies. Four studies3,4,30,34 utilized surface electromyography (sEMG), ultrasound, and biofeedback techniques to measure muscle fatigue, flexibility, and/or strength. Another study3 examined 3 different frame types and their impact on muscle activity using sEMG. The frames included a rigid frame (rigid fork, fixed rear, no suspension), suspension frame (rear triangle attached by links to rear shock for a progressive spring rate), and sports frame (racing handlebar, narrow tires, no suspension).3
Three studies9,23,25 examined spinal kinematics with different handlebar heights. Selected handlebar height, defined as the difference in height between the handlebars and the saddle,9 was inconsistent across studies. Two of 3 studies23,25 used an upper, middle, and lower handlebar-hand position, with 1 study also including an aerodynamic position with forearms on aerobars.23 The remaining study9 analyzed 5 specific handlebar height conditions.
One kinematic study33 measured spinal flexion using a posture-monitoring system, which consisted of a lightweight strain gauge attached to the cyclist’s lumbar spine that detected changes in spinal flexion during cycling. Other studies used video motion capture to measure spinal angles9 or a surface-based computerized technique using a mouse placed over landmarks to identify sagittal spinal range of motion and intervertebral angles.23,25 Measures used to assess pain also varied across studies and included the Rehabilitation Bioengineering Group pain scale3 and the Numeric Pain Rating Scale.33,34
Bicycle Fit, Muscle Activity, and Low Back Pain
Two studies3,4 applied sEMG to spinal and arm musculature to measure muscle fatigue. Subjects with LBP experienced fatigue in arm and spinal musculature associated with postural support and stability.4 Balasubramanian et al3 reported greatest arm and spinal muscle fatigue with a sports frame as compared with rigid or suspension frames. Utilizing ultrasound, Rostami et al30 determined that participants with LBP had reduced abdominal and back musculature thickness at rest and during contraction compared with the asymptomatic group (see the Appendix).
Bicycle Fit and Spinal Kinematics
Three studies examined the effects of various handlebar heights on pelvic and spinal position.9,23,25 Chen and He9 used handlebar heights of 16, 8, 0, −8, and −16 cm, while Muyor23 investigated upper, middle, lower, and aerodynamic handlebar-hand positions (defined by the position of the hand placement on the handlebar). These studies reported that lower handlebar heights increased lumbar flexion,9,23 decreased lumbosacral angle,9 and increased anterior pelvic tilt relative to the vertical plane (see the Appendix).23,25
Spinal Kinematics, Motor Control, and Low Back Pain
Spinal kinematics of cyclists with and without nonspecific LBP were compared during an on-road cycling task.33 Subjects with LBP adopted greater lumbopelvic flexion and spent more time in end-range lumbopelvic flexion. In a case study,34 a cognitive functional therapy intervention using lumbar biofeedback significantly reduced lumbopelvic flexion and reported pain after intervention (see the Appendix).
Discussion
The results of this systematic review provide support for the hypothesis that muscle activation imbalances of the core and spinal musculature are risk factors for LBP in cyclists. There is also some evidence that the prolonged, flexed-spine position during cycling is related to LBP. These findings thus add more evidence than the 2009 review by Marsden and Schwellnus,22 which found limited empirical support for any proposed mechanism or associated risk factors other than proper saddle angle positioning.
The 3 studies that examined the relationship between bicycle positioning and muscle activity provide different insight into LBP in cyclists. The relationship seen between upper extremity fatigue in cyclists with LBP suggests that cycling with LBP may increase exertion by the upper extremity on the handlebars to compensate for pain.4 Increased muscle recruitment and fatigue was also seen when subjects were positioned in an aerodynamic flexed posture on a sports cycle.3 Cyclists with LBP also demonstrated asymmetrical co-contraction of the lumbar multifidi muscles,7,22 decreased thickness of the transverse abdominus and lumbar multifidi,30 and decreased back extensor endurance when compared with cyclists without LBP.30 As back extensor muscle activity is proportional to pedaling intensity,32 these alterations may decrease desired performance.
The 3 studies9,24,25 examining the relationship between position on the cycle and spinal kinematics all demonstrated that lower handlebar positioning resulted in greater lumbar flexion. The correlation between lumbar stability and nontraumatic LBP has significant support in the literature, and lumbar positioning, including prolonged flexion, negatively affects spinal pathology and symptoms.14,26-28,34 This concept is supported by Van Hoof et al,33 who showed that cyclists who reported significant increases in LBP during a 2-hour cycling task adopted greater lumbopelvic flexion and spent more time in end-range lumbopelvic flexion compared with age-matched asymptomatic controls. Burnett et al7 also demonstrated increased lumbar spinal flexion and rotation in symptomatic cyclists compared with controls. Spinal kinematics in subjects with LBP in the study by Van Hoof et al33 did not significantly change during the 2-hour cycling task, but the LBP group assumed greater lumbopelvic flexion at the start of the task.
It is unclear which comes first: muscle imbalances affecting spinal kinematics or altered spinal kinematics, which lead to muscle activation imbalance. Cyclists with LBP assume a more flexed position at the start of cycling, and this position does not change during cycling; however, pain increases. These findings may indicate maladaptive motor control of the spine during cycling as a causative factor.33 Another implication is that decreased endurance of the low back musculature may play a role in spinal kinematics or spinal loading. If there are existing endurance deficits of the musculature supporting the spine, then it is possible that when fatigued, the spine may absorb an increased load and stress as stated by the flexion-relaxation hypothesis. This shift in spinal forces and load displacement reinforces the concept that it may not be the body positioning on the bike that matters but the time spent in that position and concurrent muscle activation imbalances or endurance deficits that may contribute to overuse LBP.
Only 1 study in this systematic review included an intervention for cyclists with LBP. Improved motor control of spinal kinematics during a bout of cycling and improved LBP symptoms were found after biofeedback training.34 As the intervention is based on the subject’s conscious motor control of spinal kinematics while cycling, there are implications that impaired motor control may result in more end-range flexed posture, including a loss of lumbar lordosis34 while cycling, potentially contributing to flexion-related lumbar pain. The participant may have had difficulty maintaining lumbar lordosis due to back extensor endurance impairments, which matches the findings of Rostami et al.30
There are limitations in this systematic review, including small sample sizes, differing measurement techniques, varied populations, and varying areas of study focus. Studies were prone to selection bias as participants were not randomly selected from the population. Furthermore, participants and examiners were not blinded. The variance of participant’s cycling experiences creates another limitation: the generalizability of the results. A categorization of cycling based on activity level has been proposed by Ansley and Cangley2 to improve the ability to compare results across studies. Overall, these limitations impact the ability to compare findings directly across studies.
Based on this systematic review, there is greater evidence for altered muscle activity and increased spinal flexion in cyclists with LBP.
Conclusion
The results of this review suggest that there are relationships between common risk factors that warrant further exploration. Spinal and core muscle activation imbalances in a prolonged flexed posture associated with cycling may lead to maladaptive spinal kinematics and increased spinal stresses contributing to LBP.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Abt JP, Smoliga JM, Brick MJ, Jolly JT, Lephart SM, Fu F. Relationship between cycling mechanics and core stability. J Strength Cond Res. 2007;21:1300-1304. [DOI] [PubMed] [Google Scholar]
- 2. Ansley L, Cangley P. Determinants of “optimal” cadence during cycling. Eur J Sport Sci. 2009;9:61-85. [Google Scholar]
- 3. Balasubramanian V, Jagannath M, Adalarasu K. Muscle fatigue based evaluation of bicycle design. Appl Ergon. 2014;45:339-345. [DOI] [PubMed] [Google Scholar]
- 4. Balasubramanian V, Jayaraman S. Surface EMG based muscle activity analysis for aerobic cyclist. J Bodywork Movement Ther. 2009;13:34-42. [DOI] [PubMed] [Google Scholar]
- 5. Barrios C, Bernardo ND, Vera P, Laíz C, Hadala M. Changes in sports injuries incidence over time in world-class road cyclists. Int J Sports Med. 2015;36:241-248. [DOI] [PubMed] [Google Scholar]
- 6. Bini RR, Hume PA, Croft J, Kilding A. Optimizing bicycle configuration and cyclists’ body position to prevent overuse injury using biomechanical approaches. In: Bini RR, Carpes FP, eds. Biomechanics of Cycling. New York, NY: Springer; 2014:71-83. [Google Scholar]
- 7. Burnett AF, Cornelius MW, Dankaerts W, O’Sullivan PB. Spinal kinematics and trunk muscle activity in cyclists: a comparison between healthy controls and non-specific chronic low back pain subjects-a pilot investigation. Man Ther. 2004;9:211-219. [DOI] [PubMed] [Google Scholar]
- 8. Caldwell JS, McNair PJ, Williams M. The effects of repetitive motion on lumbar flexion and erector spinae muscle activity in rowers. Clin Biomech (Bristol, Avon). 2003;18:704-711. [DOI] [PubMed] [Google Scholar]
- 9. Chen YL, He KC. Changes in human cervical and lumbar spine curves while bicycling with different handlebar heights. Work. 2012;41(suppl 1):5826-5827. [DOI] [PubMed] [Google Scholar]
- 10. Clarsen B, Krosshaug T, Bahr R. Overuse injuries in professional road cyclists. Am J Sports Med. 2010;38:2494-2501. [DOI] [PubMed] [Google Scholar]
- 11. Dankaerts W, O’Sullivan P, Burnett A, Straker L. Altered patterns of superficial trunk muscle activation during sitting in nonspecific chronic low back pain patients: importance of subclassification. Spine. 2006;31:2017-2023. [DOI] [PubMed] [Google Scholar]
- 12. De Bernardo N, Barrios C, Vera P, Laiz C, Hadala M. Incidence and risk for traumatic and overuse injuries in top-level road cyclists. J Sports Sci. 2012;30:1047-1053. [DOI] [PubMed] [Google Scholar]
- 13. Deakon RT. Chronic musculoskeletal conditions associated with the cycling segment of the triathlon; prevention and treatment with an emphasis on proper bicycle fitting. Sports Med Arthrosc. 2012;20:200-205. [DOI] [PubMed] [Google Scholar]
- 14. Delitto A, George SZ, Van Dillen LR, et al. Low back pain. J Orthop Sports Phys Ther. 2012;42:A1-A57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dettori N, Norvell D. Non-traumatic bicycle injuries: a review of the literature. Sports Med. 2006;36:7-18. [DOI] [PubMed] [Google Scholar]
- 16. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fanucci E, Masala S, Fasoli F, Cammarata R, Squillaci E, Simonetti G. Cineradiographic study of spine during cycling: effects of changing the pedal unit position on the dorso-lumbar spine angle. Radiol Med. 2002;104:472-476. [PubMed] [Google Scholar]
- 18. Hootman J, Driban J, Sitler M, Harris K, Cattano N. Reliability and validity of three quality rating instruments for systematic reviews of observational studies. Res Synth Methods. 2011;2:110-118. [DOI] [PubMed] [Google Scholar]
- 19. Johnston TE. Biomechanical considerations for cycling interventions in rehabilitation. Phys Ther. 2007;87:1243-1252. [DOI] [PubMed] [Google Scholar]
- 20. Kyle CR. Energy and aerodynamics in bicycling. Clin Sports Med. 1994;13:39-73. [PubMed] [Google Scholar]
- 21. Macintosh JE, Bogduk N. The biomechanics of the lumbar multifidus. Clin Biomech (Bristol, Avon). 1986;1:205-213. [DOI] [PubMed] [Google Scholar]
- 22. Marsden M, Schwellnus M. Lower back pain in cyclists: a review of epidemiology, pathomechanics and risk factors. Int Sportmed J. 2010;11:216-225. [Google Scholar]
- 23. Muyor JM. The influence of handlebar-hands position on spinal posture in professional cyclists. J Back Musculoskelet Rehabil. 2015;28:167-172. [DOI] [PubMed] [Google Scholar]
- 24. Muyor JM, Alacid F, Lopez-Minarro PA. Influence of hamstring muscles extensibility on spinal curvatures and pelvic tilt in highly trained cyclists. J Hum Kinet. 2011;29:15-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Muyor JM, Lopez-Minarro PA, Alacid F. Spinal posture of thoracic and lumbar spine and pelvic tilt in highly trained cyclists. J Sports Sci Med. 2011;10:355-361. [PMC free article] [PubMed] [Google Scholar]
- 26. Ng L, Burnett A, O’Sullivan P. Spino-pelvic kinematics and trunk muscle activation in prolonged ergometer rowing: mechanical etiology of non-specific low back pain in adolescent rowers. 26th International Conference on Biomechanics in Sports. 2008:14-18. https://ojs.ub.uni-konstanz.de/cpa/article/download/2051/1917. Accessed October 2015.
- 27. O’Sullivan P. Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism. Man Ther. 2005;10:242-255. [DOI] [PubMed] [Google Scholar]
- 28. O’Sullivan PB. Lumbar segmental ‘instability’: clinical presentation and specific stabilizing exercise management. Man Ther. 2000;5:2-12. [DOI] [PubMed] [Google Scholar]
- 29. O’Sullivan PB, Mitchell T, Bulich P, Waller R, Holte J. The relationship beween posture and back muscle endurance in industrial workers with flexion-related low back pain. Man Ther. 2006;11:264-271. [DOI] [PubMed] [Google Scholar]
- 30. Rostami M, Ansari M, Noormohammadpour P, Ali Mansournia M, Kordi R. Ultrasound assessment of trunk muscles and back flexibility, strength and endurance in off-road cyclists with and without low back pain. J Back Musculoskelet Rehabil. 2015;28:634-644. [DOI] [PubMed] [Google Scholar]
- 31. Salai M, Brosh T, Blankstein A, Oran A, Chechik A. Effect of changing the saddle angle on the incidence of low back pain in recreational bicyclists. Br J Sports Med. 1999;33:398-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Usabiaga J, Crespo R, Iza I, Armendi J, Terrados N, Poza J. Adaptation of the lumbar spine to different positions in bicycle racing. Spine. 1997;22:1965-1969. [DOI] [PubMed] [Google Scholar]
- 33. Van Hoof W, Volkaerts K, O’Sullivan K, Verschueren S, Dankaerts W. Comparing lower lumbar kinematics in cyclists with low back pain (flexion pattern) versus asymptomatic controls—field study using a wireless posture monitoring system. Man Ther. 2012;17:312-317. [DOI] [PubMed] [Google Scholar]
- 34. Van Hoof W, Volkaerts K, O’Sullivan K, Verschueren S, Dankaerts W. Cognitive functional therapy intervention including biofeedback for LBP during cycling: a single case study. Sport Geneeskunde. 2011;44(4):20-26. [Google Scholar]
- 35. Wilber CA, Holland GJ, Madison RE, Loy SF. An epidemiological analysis of overuse injuries among recreational cyclists. Int J Sports Med. 1995;16:201-206. [DOI] [PubMed] [Google Scholar]