Abstract
Background:
Shoulder activity level may be a risk factor for shoulder instability, an indication for surgical intervention, and a risk factor for failure of operative stabilization.
Hypothesis:
Patients undergoing shoulder stabilization surgery have a higher activity level compared with sex- and age-matched healthy controls.
Study Design:
Cross-sectional study.
Level of Evidence:
Level 2.
Methods:
Patients undergoing shoulder stabilization surgery aged 18 to 50 years were prospectively enrolled. As part of data collection, patients completed a previously validated shoulder activity scale, which generates a score reporting frequency of activity ranging from 0 (least active) to 20 (most active). The activity level of these patients was compared with sex- and age-matched norms for a healthy population with no history of shoulder disorders.
Results:
A total of 409 subjects (343 male, 66 female) undergoing shoulder instability surgery completed the activity scale. Seventy-seven percent of patients had higher shoulder activity level than sex- and age-matched controls. Seventy-nine percent aged 18 to 30 years had a higher shoulder activity level than controls, with an identical distribution for men (79%) and women (79%). Among patients aged 31 to 50 years, 70% had higher activity than controls. However, men were more likely to have a higher activity level than controls (72%) versus women (59%). In patients aged 18 to 30 years, median activity level for instability patients was 14 in men compared with 10 in controls, and 13 in women compared with 8 in controls. In patients aged 31 to 50 years, median activity level was 13 in men compared with 10 in controls and 10 in women compared with 8 in controls.
Conclusion:
Patients undergoing shoulder stabilization surgery have a higher activity level than sex- and age-matched healthy controls.
Clinical Relevance:
Shoulder activity is especially elevated in younger, male instability patients.
Keywords: shoulder, activity level, instability, stabilization surgery, labral tear
Shoulder instability is a common problem, particularly in patients participating in contact sports.12 Although shoulder instability is often treated initially with nonoperative treatment, many patients will ultimately undergo shoulder stabilization surgery because of the high risk for recurrence.5 A patient’s level of activity is often proposed as a risk factor for increasing the likelihood of undergoing surgical treatment for shoulder instability6 and potentially a risk factor for failure of operative stabilization.8
Activity level is coming under greater scrutiny as a potential prognostic and outcome variable in orthopaedic surgery.4 Activity level measures how often a patient engages in specific tasks, as opposed to what tasks a patient can do. A shoulder activity scale,1 measuring the frequency of 5 shoulder tasks as well as participation in contact and overheads sports, with excellent reliability and construct validity has been studied in patients with rotator cuff disease2,10 and a normative population.7 Although the shoulder activity scale varies by shoulder diagnosis,3 with higher activity in patients with instability than in patients with rotator cuff disease or osteoarthritis, there are no data on how activity level in instability patients compares with that of sex- and age-matched controls. Therefore, the purpose of this study was to compare the shoulder activity score in patients undergoing shoulder stabilization surgery with sex- and age-matched healthy controls to test the hypothesis that instability patients are more active with their shoulders.
Methods
In this institutional review board–approved study, patients gave consent and were prospectively enrolled and filled out the shoulder activity scale1 (Appendix, available at http://sph.sagepub.com/content/by/supplemental-data), which asks how often patients have participated in 5 specific activities at their most active state over the previous 12 months. A multicenter, prospective study group involving 11 geographic sites with shoulder and/or sports medicine fellowship–trained surgeons followed patients undergoing surgery for symptomatic shoulder instability, including anterior instability, posterior instability, or combined patterns. The questionnaire generates a numeric score from 0 (least active) to 20 (most active). In addition, there are 2 questions that assess the level of involvement in overhead and contact sports.
In a previous study, age- and sex-based normative data from individuals older than 18 years without shoulder complaints were collected through a marketing research firm that maintains a large database of people matched to the March 2010 Current Population Survey Social and Economic Supplement and the 2009 American Community Survey.7 In the current study, the activity level of each patient in the instability group was compared with the median activity level for a healthy control patient of the same sex and age (in years). Normative data were not available for patients younger than 18 years. Because of the extremely low number of patients older than 50 years undergoing shoulder stabilization surgery (n = 6), they were excluded from the study. The percentage of instability patients above the median for healthy controls was then calculated for patients aged 18 to 30 and 31 to 50 years. The 25th, 50th, and 75th percentile of activity was calculated for the instability patients in male and female patients from both age groups. Finally, the distribution of participation in overhead and contact sports was also calculated and compared with that of matched controls. Chi-square test was used to compare this distribution.
Results
A total of 409 subjects, 343 (84%) male, who underwent shoulder stabilization surgery completed the activity scale.
Overall, 77% of the patients in the study had a higher shoulder activity level than sex- and age-matched controls. Broken down by age, 79% of the patients aged 18 to 30 years had a higher shoulder activity level than controls, with an identical distribution for men (79%) and women (79%). Among patients aged 31 to 50 years, 70% of patients overall had a higher activity level than controls. In this age group, however, men undergoing shoulder stabilization surgery were more likely to have a higher activity level compared with controls (72%) than women (59%).
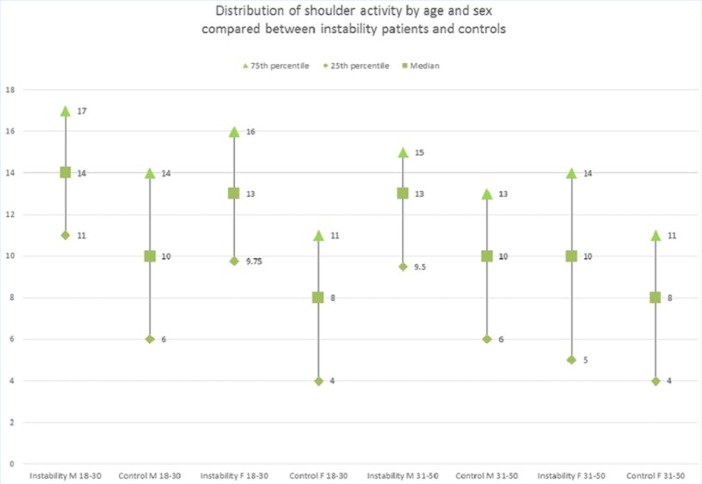
The median shoulder activity level in male instability patients aged 18 to 30 years was 14 compared with 10 in healthy controls. For women, instability patients had a median activity level of 13 compared with 8 for controls. In patients aged 31 to 50 years, median activity level was 13 in male instability patients compared with 10 in controls, and 10 in female instability patients compared with 8 in controls. The distribution of shoulder activity among instability patients was clearly shifted toward higher activity overall compared with controls (Figure 1).
Figure 1.
Comparing distribution of shoulder activity between instability patients and controls.
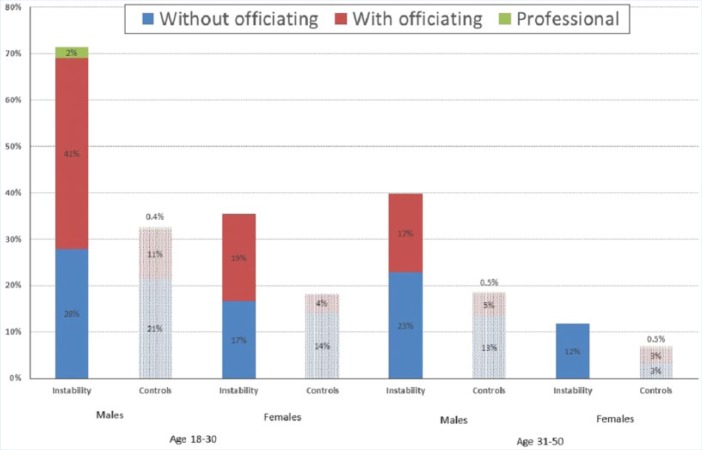
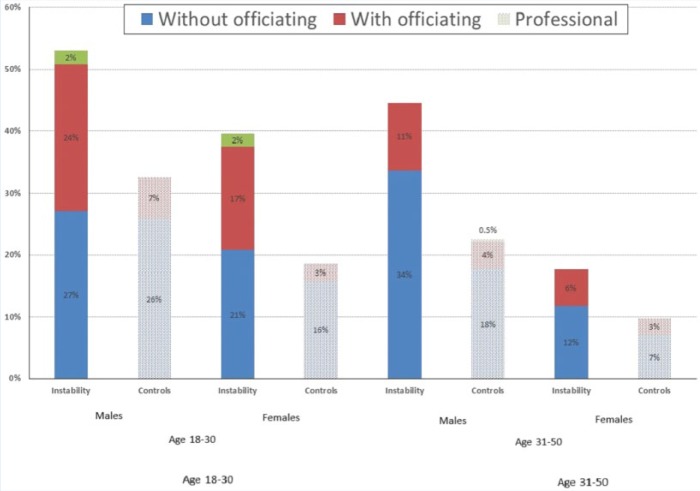
Instability patients were significantly more likely to participate in contact (Figure 2) and overhead (Figure 3) sports, and at higher levels of intensity, than matched controls (P < 0.001). For example, 71% of male instability patients aged 18 to 30 years participated in contact sports compared with 33% of controls. In women aged 18 to 30 years, 33% of instability patients participated in contact sports compared with 18% of controls. Even in women aged 31 to 50 years, 12% of instability patients participated in contact sports compared with 7% of controls. Similarly, 18% of female instability patients aged 31 to 50 years participated in overhead sports, compared with 10% of controls.
Figure 2.
Participation in contact sports.
Figure 3.
Participation in overhead sports.
Discussion
Elevated shoulder activity is associated with patients undergoing shoulder surgery compared with sex- and age-matched controls. This holds true for men and women, and includes patients up to age 50 years.
The current findings are consistent with a prior study demonstrating that shoulder activity level varies by age and shoulder diagnosis.3 Shoulder activity level was significantly higher in patients with instability (14 ± 5.2; range, 1-20) than in patients with rotator cuff disease (10 ± 5.1; range, 0-20; P = 0.027) or osteoarthritis (7 ± 4.7; range, 0-18; P < 0.001). Although that previous study found that shoulder activity varied by age, it did not adjust for patient age or sex when comparing activity by diagnosis and did not include patients without shoulder pathology.
Shoulder activity level is a predictor of nonoperative treatment in atraumatic rotator cuff tears.6 Our findings raise the possibility that shoulder activity level may also predict the success of nonoperative treatment for shoulder instability.
A prospective study investigated factors that might predict recurrent instability.11 At an average follow-up of 4 years in a cohort of 131 patients, about one-third of shoulders had recurrent instability (33), and 22% underwent surgical stabilization. Patients participating in contact or collision sports or used their arm at or above chest level in their occupation were much more likely to undergo surgery (49%). Patients aged 12 to 19 years at the time of their initial dislocation had a much higher rate of recurrent instability (56%) and slightly higher rate of surgical stabilization (28%). In a logistic regression analysis, age less than 25 years at the time of the initial dislocation was clearly associated with a higher risk of subsequent instability, while occupational use of the arm at or above chest level was very close to statistical significance (P = 0.066). Participation in collision/contact sports also approached significance. A long-term study with minimum follow-up of 20 years after open Bankart repair for anterior shoulder instability showed that increased shoulder activity was associated with a higher risk for recurrent instability after surgery.8 These findings are consistent with our data demonstrating that instability patients undergoing surgery are more likely to participate in contact sports than healthy matched controls, and stress the potential importance of this increased activity level to the outcome of treatment.
Instability patients are more active prior to surgery, making return to activity level an important outcome variable for surgical shoulder stabilization. One-third of patients who underwent arthroscopic Bankart repair for chronic glenohumeral instability reported no benefit from surgery in terms of sporting activity.9 Improvement in sporting proficiency was negatively correlated with preoperative activity and performance but positively correlated with age. Overall, while a significant number of patients did get back to activity after surgery, there was no benefit in duration, frequency, or performance level and no increased return to high-level activities.9 These findings emphasize the importance of using a validated activity scale for instability patients.
This study does have limitations and may not be generalizable to all patient populations. These findings are limited to the cohort studied, which included patients undergoing surgery to treat shoulder instability. Patients who are able to manage shoulder instability without surgical intervention may have different shoulder activity than patients undergoing surgical stabilization. This study only includes patients aged 18 to 50 years. While patients older than 50 years are relatively unlikely to have shoulder instability, patients younger than 18 years are more likely than older patients to have shoulder instability. Unfortunately, data for controls younger than 18 years were not available. There is a preponderance of men (84%) in this cohort, which may limit its applicability to women. Finally, this study only focuses on baseline activity level at the time of surgery and not on activity at the time of initial injury or at follow-up from treatment.
Despite these limitations, this study demonstrates that shoulder activity is higher in patients undergoing shoulder stabilization surgery than matched controls, especially for men and young adults. Shoulder activity is a relevant variable for shoulder instability patients.
Supplementary Material
Acknowledgments
The authors would like to acknowledge the contributions of the research staff who are essential to the success of the MOON Instability Group.
Footnotes
The following author declared potential conflicts of interest: Brian R. Wolf, MD, MS, reports grants from Orthopaedic Education and Research Foundation, Arthrex, and Smith & Nephew, and personal fees from ConMed.
Contributing Authors: Keith M. Baumgarten, MD (Orthopedic Institute Sioux Falls); Asheesh Bedi, MD (University of Michigan); Julie Y. Bishop, MD (Ohio State University Medical Center); Matthew J. Bollier, MD (University of Iowa); Jonathan T. Bravman, MD (University of Colorado); James L. Carey, MD, MS (University of Pennsylvania); Charlie L. Cox, MD (Vanderbilt University); Warren Dunn, MD, MPH (University of Wisconsin); Brian T. Feeley, MD (University of California–San Francisco); Grant L. Jones, MD (Ohio State University Medical Center); John D. Kelly, MD (University of Pennsylvania); John E. Kuhn, MD (Vanderbilt University); C. Benjamin Ma, MD (University of California–San Francisco); Robert G. Marx, MD (Hospital for Special Surgery); Bruce S. Miller, MD (University of Michigan); Brian J. Sennett, MD (University of Pennsylvania); Matthew V. Smith, MD (Washington University School of Medicine); Rick W. Wright, MD (Washington University School of Medicine); Alan Zhang, MD (University of California–San Francisco).
Contributor Information
MOON Shoulder Instability Group:
Keith M. Baumgarten, Asheesh Bedi, Julie Y. Bishop, Matthew J. Bollier, Jonathan T. Bravman, James L. Carey, Charlie L. Cox, Warren Dunn, Brian T. Feeley, Grant L. Jones, John D. Kelly, John E. Kuhn, C. Benjamin Ma, Robert G. Marx, Bruce S. Miller, Brian J. Sennett, Matthew V. Smith, Rick W. Wright, and Alan Zhang
References
- 1. Brophy RH, Beauvais RL, Jones EC, Cordasco FA, Marx RG. Measurement of shoulder activity level. Clin Orthop Relat Res. 2005;439:101-108. [DOI] [PubMed] [Google Scholar]
- 2. Brophy RH, Dunn WR, Kuhn JE, MOON Shoulder Group. Shoulder activity level is not associated with the severity of symptomatic, atraumatic rotator cuff tears in patients electing nonoperative treatment. Am J Sports Med. 2014;42:1150-1154. [DOI] [PubMed] [Google Scholar]
- 3. Brophy RH, Levy B, Chu S, Dahm DL, Sperling JW, Marx RG. Shoulder activity level varies by diagnosis. Knee Surg Sports Traumatol Arthrosc. 2009;17:1516-1521. [DOI] [PubMed] [Google Scholar]
- 4. Brophy RH, Lin K, Smith MV. The role of activity level in orthopaedics: an important prognostic and outcome variable. J Am Acad Orthop Surg. 2014;22:430-436. [DOI] [PubMed] [Google Scholar]
- 5. Brophy RH, Marx RG. The treatment of traumatic anterior instability of the shoulder: nonoperative and surgical treatment. Arthroscopy. 2009;25:298-304. [DOI] [PubMed] [Google Scholar]
- 6. Dunn WR, Kuhn JE, Baumgarten KM, et al. Defining indications for rotator cuff repair: predictors of failure of nonoperative treatment of chronic, symptomatic, full-thickness rotator cuff tears. J Shoulder Elbow Surg. 2013;22:E23. [DOI] [PubMed] [Google Scholar]
- 7. Hepper CT, Smith MV, Steger-May K, Brophy RH. Normative data of shoulder activity level by age and sex. Am J Sports Med. 2013;41:1146-1151. [DOI] [PubMed] [Google Scholar]
- 8. Moroder P, Odorizzi M, Pizzinini S, Demetz E, Resch H, Moroder P. Open Bankart repair for the treatment of anterior shoulder instability without substantial osseous glenoid defects: results after a minimum follow-up of twenty years. J Bone Joint Surg Am. 2015;97:1398-1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Plath JE, Feucht MJ, Saier T, et al. Sporting activity after arthroscopic Bankart repair for chronic glenohumeral instability. Arthroscopy. 2015;31:1996-2003. [DOI] [PubMed] [Google Scholar]
- 10. Ryliskis S, Brophy RH, Kocius M, Marx RG. Shoulder activity level in the preoperative assessment of patients with rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2009;17:1522-1528. [DOI] [PubMed] [Google Scholar]
- 11. Sachs RA, Lin D, Stone ML, Paxton E, Kuney M. Can the need for future surgery for acute traumatic anterior shoulder dislocation be predicted? J Bone Joint Surg Am. 2007;89:1665-1674. [DOI] [PubMed] [Google Scholar]
- 12. Simonet WT, Melton LJ, 3rd, Cofield RH, Ilstrup DM. Incidence of anterior shoulder dislocation in Olmsted County, Minnesota. Clin Orthop Relat Res. 1984;(186):186-191. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.