Abstract
Background and aims
Fetal undernutrition is a risk factor for heart disease in both genders, despite the protection of women against hypertension development. Using a rat model of maternal undernutrition (MUN) we aimed to assess possible sex differences in the development of cardiac alterations and the implication of hypertension and cardiac oxidative stress.
Methods
Male and female offspring from rats fed ad libitum (control) or with 50% of the normal daily intake during the second half of gestation (MUN) were used. Heart weight/body weight ratio (HW/BW), hemodynamic parameters (anaesthetized rats) and plasma brain natriuretic peptide (BNP, ELISA) were assessed in 21-day, 6-month and 22-month old rats. Plasma testosterone (ELISA) and cardiac protein expression of enzymes related to reactive oxygen species synthesis (p22phox, xanthine-oxidase) and degradation (catalase, Cu/Zn-SOD, Mn-SOD, Ec-SOD) were evaluated in 21-day and 6-month old rats (Western Blot). Heart structure and function was studied at the age of 22 months (echocardiography).
Results
At the age of 21 days MUN males exhibited significantly larger HW/BW and cardiac p22phox expression while females had reduced p22phox expression, compared to their respective sex-matched controls. At the age of 6-months, MUN males showed significantly larger blood pressure and cardiac xanthine-oxidase expression; MUN females were normotensive and had a lower cardiac expression of antioxidant enzymes, compared to their respective sex-matched controls. At the age of 22 months, both MUN males and females showed larger HW/BW and left ventricular mass and lower ejection fraction compared to sex-matched controls; only MUN males exhibited hypertension and a larger plasma BNP compared to aged male controls.
Conclusions
1) During perinatal life females exposed to fetal undernutrition are protected from cardiac alterations, but in ageing they exhibit ventricular hypertrophy and functional loss, like MUN males; 2) cardiac oxidative stress might be implicated in the observed heart alterations in both sexes and 3) the severity of cardiac damage might be greater in males due to hypertension.
Introduction
Low birth weight -due to inadequate maternal nutrition, placental alterations or other causes-is associated with several adverse outcomes in adult life; a process known as fetal programming. Among others, low birth weight due to fetal stress has been linked to the development of heart diseases and some of its risk factors such as hypertension [1–5]. Epidemiological studies have been corroborated in experimental animals showing evidence that hypoxia, nutrient deficiency or other stressors during intrauterine life, induce left ventricular hypertrophy (LVH) [6,7], increased susceptibility to ischemia-reperfusion injury [8,9] or arrhythmias [10].
Despite the well known differences between men and women in cardiovascular physiology [11] and the influence of sex in the development and progression of disease, sex as biological variable is not taken into account sufficiently [12]. In the clinical setting this leads to underestimation of the risk of heart disease in women and also to inadequate treatment [13]. Regarding the influence of sex on fetal programming, there is some evidence pointing at a lower impact of fetal programming on hypertension development in women [14]. Despite this fact, cohort studies have evidenced that the association between low birth weight and adult heart disease is comparable in men and women [15,16], particularly after menopause [17]. Therefore, the impact of ageing and the mechanisms implicated in the sex differences in fetal programming of heart disease are not completely elucidated and deserve further studies [18].
Hypertension is one of the possible links between fetal stress and heart disease development. On one hand, hypertension is one of the cardiovascular risk factors most consistently associated with low birth weight [3,14]. Secondly, high blood pressure is a well known stimulus for LVH and myocardial ischemia [8,9]. Furthermore, fetal programming of hypertension exhibits a sexual dimorphism and studies in animal models have demonstrated that females exposed to several stress factors during intrauterine life do not develop hypertension or exhibit milder forms [14,19–21]. This finding has led to exclude females from the majority of studies and few have evaluated the impact of fetal stress on female heart, particularly in ageing.
Oxidative stress is another possible mechanism which might contribute to fetal programming of cardiac disease. The heart is an active source of reactive oxygen species (ROS) since it is the organ with the highest oxygen uptake and largest density of mitochondria and, therefore, it might be particularly vulnerable to redox disbalance. In addition, there is evidence that oxidative stress is implicated in cardiac remodeling [22,23]. Oxidative stress associated to fetal programming is also influence by sex [18]. In this regard, we have evidence, in a rat model of maternal undernutrition during pregnancy (MUN), that females exhibit a better plasma antioxidant status at weaning, while males have a reduced antioxidant capacity and increased plasma carbonyl levels already at the age of 21 days. Furthermore, in this rat model, males, but not females developed hypertension at adult age [24]. Given the role of hypertension and oxidative stress in cardiac structural and functional alterations, in the present study we hypothesize that MUN females might be less susceptible to develop long-term cardiac alterations particularly if they remain normotensive at advanced age. The aims of the present study were to test this hypothesis, assessing in MUN rats at different age points: 1) the development of alterations in cardiac structure and function, through echocardiography and brain natriuretic peptide (BNP) measurements and 2) the role of hypertension and cardiac oxidative stress, through assessment of hemodynamic parameters and heart enzymatic systems responsible for ROS production and degradation. We have also evaluated the possible implication of testosterone in the sex-differences observed in this rat model of fetal programming.
Materials and methods
Experiments were performed in Sprague Dawley rats from the colony maintained at the Animal House facility of the Universidad Autónoma de Madrid. All experimental procedures conformed to the Guidelines for the Care and Use of Laboratory Animals (NIH publication No. 85–23, revised in 1996), the Spanish legislation (RD 1201/2005) and they were approved by the Ethics Review Board of Universidad Autónoma de Madrid and of the local Government (Comunidad Autónoma de Madrid).
The rats were housed in buckets 36.5/21.5/18.5 cm (length/width/height) on aspen wood bedding and maintained under controlled conditions (temperature 22°C, relative humidity 40% and 12/12 light/dark photoperiod). They were fed with breeding diet (EuroRodent Diet 22; 5LF5, Labdiet, Spain) containing 55% carbohydrates, 22% protein, 4.4% fat, 4.1% fiber and 5.4% mineral, being sodium content 0.26%. Drinking water was provided ad libitum in all cases. The animals were free from any pathogen that could interact with the study. The health and welfare of the animals was monitored by staff at least once a day.
Maternal Undernutrition Model (MUN)
The model of global nutrient restriction in Sprague Dawley pregnant rats (MUN) was established as previously described [24]. Briefly, day 1 of gestation was determined in the dams by observation of sperm in the vaginal smear. Thereafter, they were allocated to one of the experimental groups: control, fed ad libitum throughout pregnancy and lactation (C, n = 5 dams) and MUN, fed ad libitum during the first 10 days of gestation and with 50% of the averaged control daily intake from day 11 to the end of pregnancy, returning to ad libitum diet during lactation (MUN, n = 5 dams). 24h after birth the pups were sexed and weighed individually and the litter was standardized to 12 individuals, 6 males and 6 females if possible (smaller litters were not used).
Experimental procedures
To avoid litter effect, each experimental protocol described below was performed in male and female offspring from the different litters. Experiments were performed in rats of the following ages: 21 days, 6 months and 22 months.
Intra-arterial blood pressure measurements
Intra-arterial blood pressure was assessed as previously described [25]. Briefly, the rats were anaesthetized with 37.5 mg/kg Ketamine hydrochloride and 0.25 mg/kg Medetomidine hydrochloride i.p. Thereafter, a cannula was inserted in the iliac artery and the pressure wave was recorded through a pressure transducer (Statham; Harvard Apparatus) on a PowerLab system (ADInstruments) during approximately 60 minutes. Diastolic and systolic blood pressures (DBP, SBP) and heart rate (HR) were measured in the trace, averaging the data from approximately 1 min recording period and mean arterial pressure (MAP) and pulse pressure (PP) were calculated.
Western blot
Hearts were excised, atria removed, weighted and quickly snap frozen to quantify protein expression of NADPH oxidase subunit p22phox, xanthine oxidase (XO), catalase and superoxide dismutase (SOD) isoforms (Cu-Zn-SOD, Mn-SOD and extracellular, EC-SOD). Western blotting was performed as previously described [26]. Briefly, 30 μg protein samples were separated by 15% SDS-PAGE gels. Primary antibodies against p22phox (Santa Cruz Biotechnology; Germany; 1:400 final dilution), Cu/Zn-SOD and Mn-SOD (SantaCruz Biotechnology; Germany; 1:1000 final dilution), EC-SOD (Enzo Life Sciences; USA; 1:1000 final dilution); XO (Santa Cruz Biotechnology; Germany; 1:1000 final dilution) and catalase (Sigma-Aldrich; USA; 1:2000 final dilution) were applied overnight at 4°C. After washing, secondary antibodies (anti-rabbit or anti-mouse IgG-peroxidase conjugated) were applied for 1 h. Blots were washed, incubated in commercial enhanced chemiluminescence reagents (ECL Prime, Amersham Bioscence, UK) and bands were detected by ChemiDoc XRS+Imaging System (Bio-Rad, USA). To prove equal loadings of samples, blots were re-incubated with GADPH antibody (Sigma-Aldrich; USA; 1:3000 final dilution). Blots were quantified using Image Lab 3.0 software (Bio-Rad, USA). Expression values ofp22phox, Cu/Zn-SOD, Mn-SOD, EC-SOD, XO and catalase were normalized with GADPH to account for variations in gel loading. Examples of gels used for densitometric analysis are shown in S1 Fig.
Transtoracic Echocardiography (TTE)
TTE was performed in 22 month-old rats as previously described [27]. Briefly, the rats were anesthetized with 80 mg/kg Ketamine hydrochloride and 10 mg/kg Diazepam, i.p. An Acuson Sequoia C512 system equipped with a 13-MHz transducer was used (Acuson, Mountain View, CA, USA). The images were acquired with the animals in left lateral decubitus. M-mode imaging of the parasternal short-axis (papillary level) view allowed measurement of end-diastolic internal diameter (LVIDd) and end-systolic internal diameter (LVIDs), posterior wall thickness at diastole (PWd) and interventricular septum thickness at diastole (IVSd); HR was also recorded. Values were determined by averaging the measurements of three consecutive cardiac cycles in accordance with the American Society of Echocardiography guidelines. The above measurements were used to calculate left ventricular mass (LVM), expressed in grams, as previously described [28], using the following equation:
Plasma hormones
Brain Natriuretic Peptide (BNP). Plasma BNP levels were assessed in 21-day, 6-month and 22-month old rats, by a competitive enzyme immunoassay kit (Abbexa rat BNP ELISA kit; UK), according to manufacturer’s instructions. BNP was expressed as pg/ml.
Testosterone. Plasma testosterone levels were assessed in 21-day old and 6-month old rats, by a competitive enzyme immunoassay kit (Testosterone ELISA Demeditec Diagnostics GmbH; Germany), according to manufacturer’s instructions. Testosterone was expressed as ng/ml.
Statistical analysis
Sample size was calculated assuming a probability error of alpha type of 5% (p<0.05) and potency of 80%. Statistical analyses were performed by Graph-Pad Prism (version 5) and SPSS (version 22). The data are expressed as mean ± SEM. Statistical differences between MUN and control rats of each sex were analyzed by Student´s t test and the interaction between sex and maternal nutrition was analyzed by 2-way ANOVA.
Results
Body weight
24h after birth body weight of MUN rats was significantly smaller compared to controls in both males (MUN = 4.50±0.13g, n = 30; control = 6.48±0.14g, n = 30; p<0.01) and females (MUN = 4.72±0.13g, n = 30; control = 6.73±0.10g, n = 30; p<0.01). During lactation MUN rats accelerated growth and by weaning (21 days old) body weight was not statistically different between MUN and control males (MUN = 49.7±1.4, n = 12; control = 51.3±1.5, n = 12) or between MUN and control females (MUN = 49.1±1.3, n = 12; control = 47.5±1.2, n = 12). At the ages of 6 months and 22 months there was no significant difference between MUN and control male or between MUN and control female rats.
Heart weight
At the age of 21 days heart weight/body weight ratio (HW/BW) was significantly larger in MUN males compared to control rats, while we did not detect statistical differences between MUN and control females (Table 1). The interaction between sex and fetal nutrition was also statistically significant (Table 2).
Table 1. HW/BW at different age points in MUN and control offspring.
| 21 days (Weaning) | 6 months (Adult) | 22 months (Aged) | ||||
|---|---|---|---|---|---|---|
| Males | Females | Males | Females | Males | Females | |
| Control | 4.9±0.09 | 4.9±0.10 | 2.7±0.03 | 2.9±0.07 | 2.8±0.10 | 2.7±0.07 |
| (12) | (12) | (12) | (11) | (7) | (7) | |
| MUN | 5.5±0.10* | 4.8±0.08 | 2.8±0.05 | 3.1±0.08 | 3.6±0.06* | 3.0±0.10* |
| (12) | (12) | (12) | (11) | (5) | (5) | |
HW/BW, heart weight/body weight (x1000); Control rats were fed ad libitum in pregnancy; MUN rats were exposed to 50% of the normal daily intake during the second half of pregnancy. In parenthesis is shown the number of rats;
*p<0.05 when compared to sex and age-matched control rats.
Table 2. Interaction between sex and fetal nutrition for the studied variables.
| 21-day old | 6-month old | 22-month old | |
|---|---|---|---|
| Variable | P value | P value | P value |
| HW/BW | 0.013 | 0.293 | 0.465 |
| SBP | 0.179 | 0.023 | 0.066 |
| DBP | 0.269 | 0.098 | 0.092 |
| MBP | 0.429 | 0.031 | 0.080 |
| PP | 0.969 | 0.982 | 0.069 |
| HR (M/K) | 0.448 | 0.604 | 0.987 |
| HR (D/K) | - | - | 0.071 |
| p22phox | 0.029 | 0.889 | - |
| XO | 0.689 | 0.010 | - |
| Cu/Zn-SOD | 0.932 | 0.035 | - |
| Mn-SOD | 0.021 | 0.097 | - |
| EC-SOD | 0.184 | 0.037 | - |
| Catalase | 0.412 | 0.048 | - |
| IVSd | - | - | 0.299 |
| PWd | - | - | 0.944 |
| LVIDd | - | - | 0.378 |
| LVIDs | - | - | 0.763 |
| LVM | - | - | 0.730 |
| LVEF | - | - | 0.583 |
| Testosterone | 0.070 | 0.908 | - |
| BNP | 0.666 | 0.520 | 0.056 |
P values for the variables studied, evaluated by 2-way ANOVA. SBP, DBP. MBP, systolic, diastolic and mean blood pressure; PP, pulse pressure; HR (M/K), heart rate under Medetomidine/Ketamine anesthesia; HR (D/K), heart rate under Diazepam/Ketamine anesthesia; HW/BW, heart weight/body weight; XO, xanthine oxidase; SOD, superoxide dismutase; IVSd, interventricular septum at diastole; PWd, posterior wall thickness at diastole; LVIDd, left ventricular internal diameter at diastole; LVIDs, left ventricular internal diameter at systole; LVM, left ventricular mass; LVEF, left ventricular ejection fraction; BNP, brain natriuretic peptide; p< 0.05 was considered statistically significant.
At the age of 6 months no statistical difference in HW/BW were found between MUN and control rats, either in males or females.
At the age of 22 months HW/BW was significantly larger in MUN rats, both in males and in females compared to their respective sex-matched controls (Table 1).
Haemodynamic parameters
A reduction in blood pressure was observed following Medetomidine/Ketamine anesthesia. After around 30–45 min blood pressure remained stable. This was observed at all ages studied and in all the experimental groups (S2 Fig).
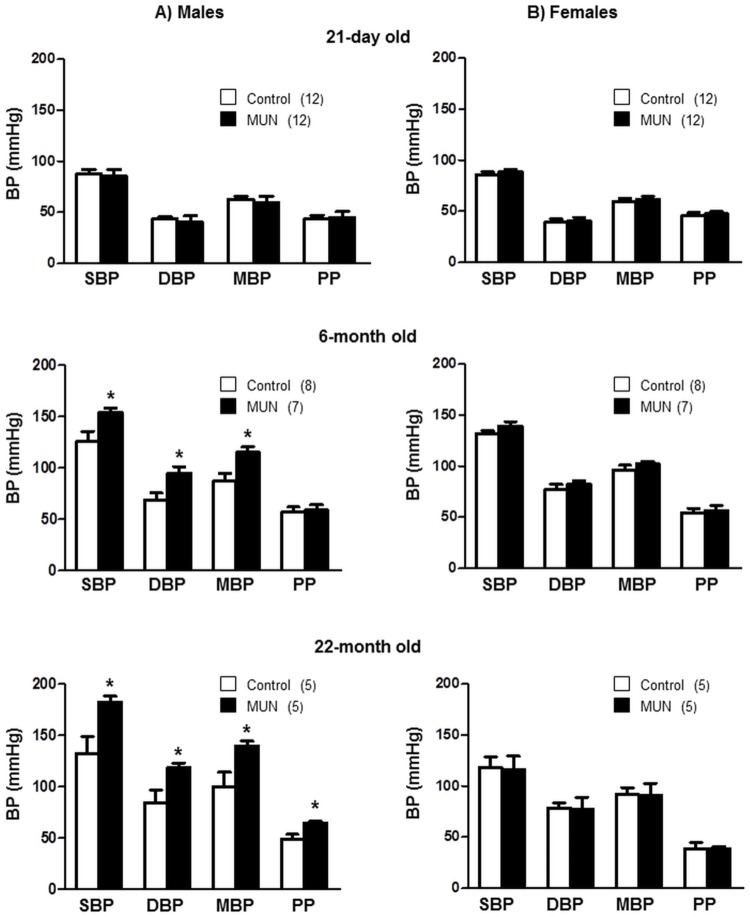
At the age of 21 days we did not detect statistical differences in SBP, DBP, MBP or PP between MUN and control rats, either in males or in females. At the age of 6 months SBP, DBP and MBP, but not PP, were significantly larger in MUN males compared to sex-matched controls (Fig 1A), while we did not detect differences between MUN and control females (Fig 1B). The interaction between sex and maternal nutrition was statistically significant for SBP and MBP. At the age of 22 months MUN males exhibited a significantly larger SBP, DBP, MBP and PP compared to control males (Fig 1A), while we did not detect statistical differences in blood pressure between MUN and control females (Fig 1B). The interaction between sex and fetal nutrition was near statistical significance for SBP and PP (Table 2).
Fig 1. Blood pressure measurements in anesthetized MUN and control rats at different age points.
Intra-arterial systolic, diastolic and mean blood pressure (SBP, DBP, MBP) and pulse pressure (PP) in rats under Medetomidine/Ketamine anesthesia. (A) male and (B) female offspring from rats exposed to maternal undernutrition during pregnancy (MUN) and rats fed ad libitum (Control). In parenthesis the number or rats used at each age point; *p<0.05 compared to sex and age-matched control rats.
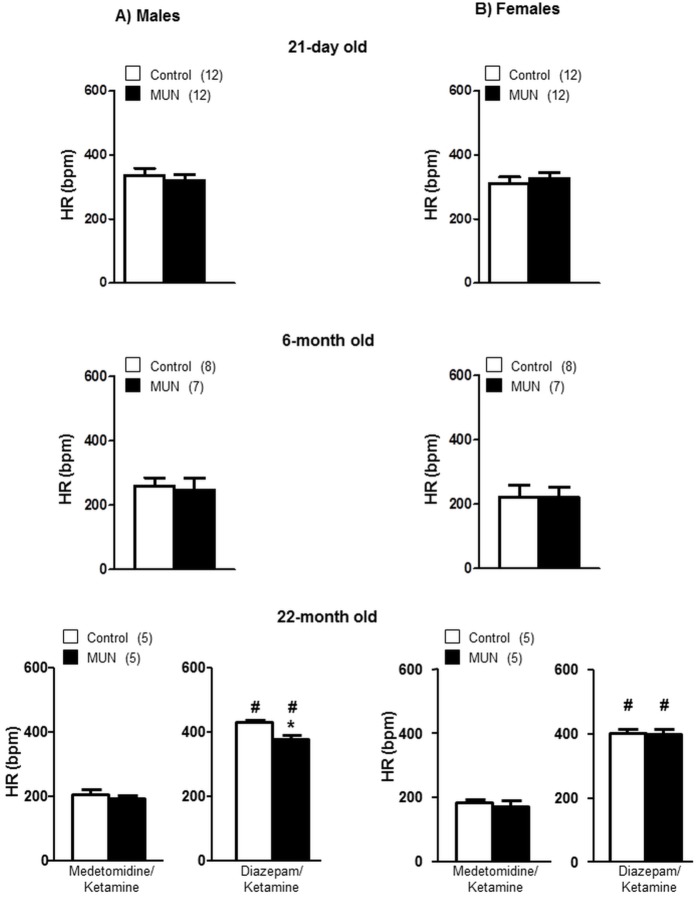
Under Diazepam/Ketamine anesthesia (used for echocardiography study in 22 month old rats) HR was significantly larger compared to HR under Medetomidine/Ketamine. Under Medetomidine/Ketamine anesthesia, HR was not statistically different between MUN and control rats of either sex at any of the ages studied. Under Diacepan/Ketamine anesthesia 22-month old MUN males rats exhibited a significantly reduced HR compared to control males. This difference was not observed in MUN females (Fig 2). The interaction between sex and fetal nutrition was near significance in 22-month old rats (Table 2).
Fig 2. Heart rate (HR) measured in anesthetized MUN and control rats at different age points.
HR was measured under Medetomidine/Ketamine anesthesia at all age points. In 22-month old rats HR was also measured under Diazepam/Ketamine anesthesia. (A) male and (B) female offspring from rats exposed to maternal undernutrition during pregnancy (MUN) and rats fed ad libitum (Control). In parenthesis the number or rats used at each age point; *p<0.05 compared to sex and age-matched control rats; #p<0.05 compared to Medetomidine/Ketamine anesthesia.
Expression of enzymes related to ROS production and degradation
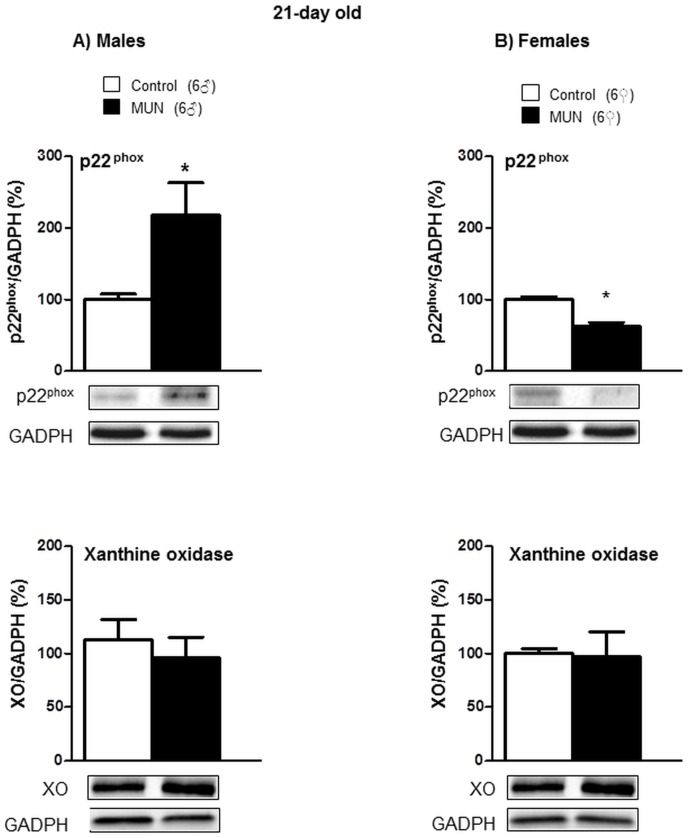
In 21-day old rats, p22phox expression was significantly higher in MUN males compared to sex-matched controls, while we did not detect statistical differences between groups in XO expression (Fig 3A). MUN females exhibited significantly lower expression levels of p22phox compared to female controls; no differences were detected in XO expression between MUN and control females (Fig 3B). The interaction between sex and fetal nutrition was statistically significant for p22phox expression (Table 2).
Fig 3. Protein expression of p22phox and xanthine oxidase (XO) in cardiac tissue from 21-day old rats.
(A) male and (B) female offspring from rats exposed to maternal undernutrition during pregnancy (MUN) and rats fed ad libitum (Control). Diagram bars show the results of densitometric analysis, relativized to GADPH expression. In parenthesis it is shown the number or rats; *p<0.05 compared to sex-matched control rats.
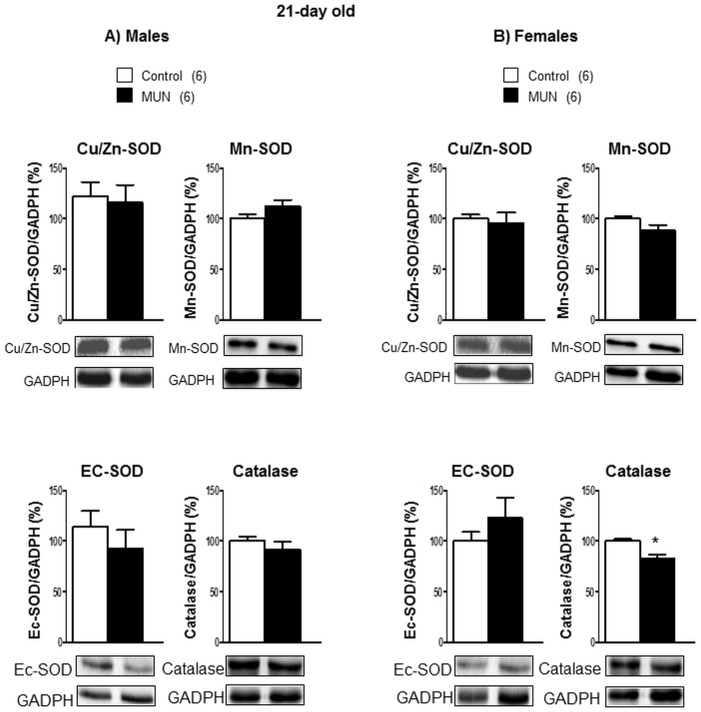
In 21-day old rats we did not detect statistical differences in any of the enzymatic systems responsible for ROS degradation between MUN and control males (Fig 4A). Catalase expression was significantly lower in MUN females compared to sex-matched control rats (Fig 4B). The interaction between sex and fetal nutrition was statistically significant for Mn-SOD expression (Table 2).
Fig 4. Protein expression of SOD isoforms and catalase in cardiac tissue from 21-day old rats.
Superoxide dismutase (SOD) isoforms, Cu/Zn-SOD, Mn-SOD and extracellular SOD (EC-SOD). (A) male and (B) female offspring from rats exposed to maternal undernutrition during pregnancy (MUN) and rats fed ad libitum (Control). Diagram bars show the results of densitometric analysis, relativized to GADPH expression. In parenthesis it is shown the number or rats; *p<0.05 compared to sex-matched control rats.
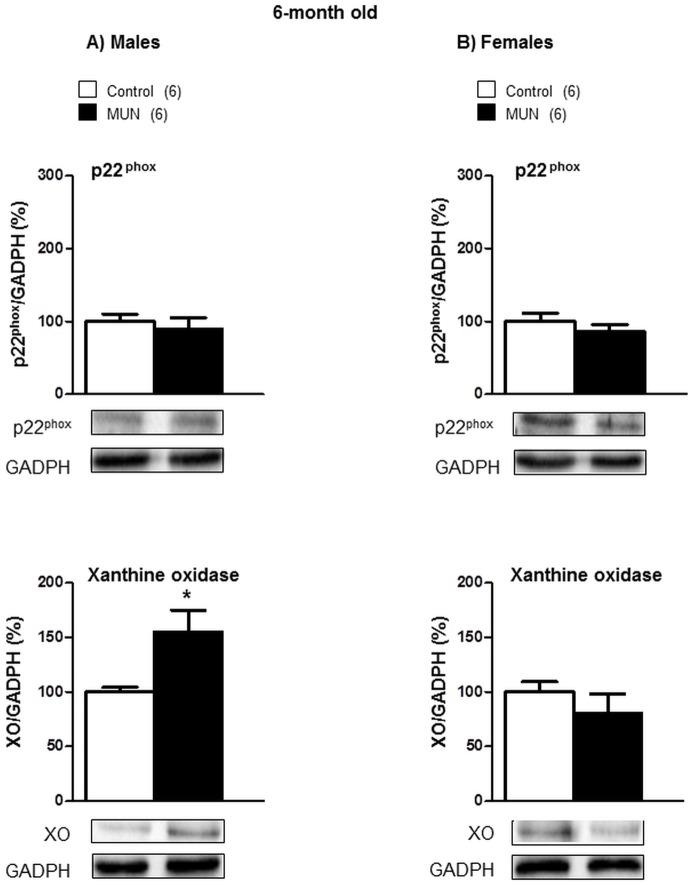
At the age of 6 months, there was no statistical difference in p22phox expression between MUN and control rats males. However, a significantly higher XO protein expression levels were found in MUN males compared to sex-matched controls (Fig 5A). Regarding females, no statistical differences were detected between MUN and control rats in either p22phox or XO expression (Fig 5B). The interaction between sex and fetal nutrition was statistically significant for XO expression (Table 2).
Fig 5. Protein expression of p22phox and xanthine oxidase (XO) in cardiac tissue from 6-month old rats.
(A) maleand (B) female offspring from rats exposed to maternal undernutrition during pregnancy (MUN) and rats fed ad libitum (Control). Diagram bars show the results of densitometric analysis, relativized to GADPH expression. In parenthesis it is shown the number or rats; *p<0.05 compared to sex-matched control rats.
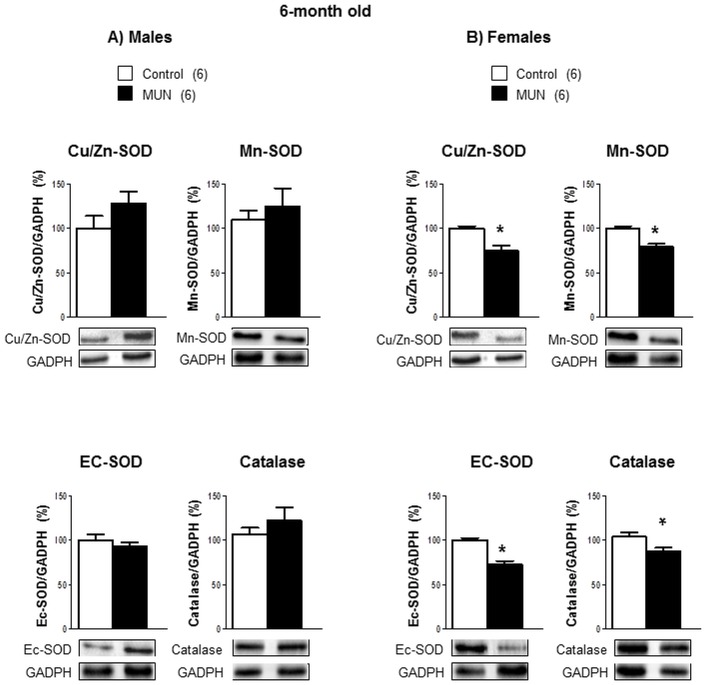
In 6-month old rats, we did not detect statistical differences between MUN and control males in any of the enzymes related to ROS degradation (Fig 6A). Female MUN rats had a significantly lower expression of all the enzymatic systems evaluated compared to female controls (Fig 6B). The interaction between sex and fetal nutrition was statistically significant for Cu/Zn-SOD, EC-SOD and catalase expression (Table 2).
Fig 6. Protein expression of SOD isoforms and catalase in cardiac tissue from 6-month old rats.
Superoxide dismutase (SOD) isoforms, Cu/Zn-SOD, Mn-SOD and extracellular SOD (EC-SOD) and catalase. (A) maleand (B) female offspring from rats exposed to maternal undernutrition during pregnancy (MUN) and rats fed ad libitum (Control). Diagram bars show the results of densitometric analysis, relativized to GADPH expression. In parenthesis it is shown the number or rats; *p<0.05 compared to sex-matched control rats.
Transthoracic Echocardiography
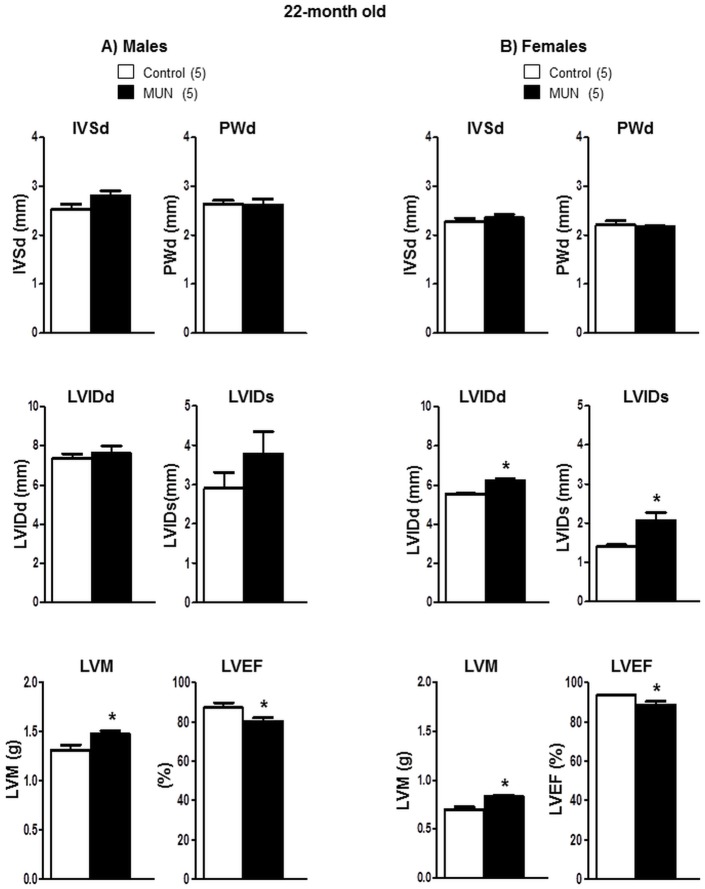
At the age of 22 months MUN males showed no differences in PWd, IVSd, LVIDd or LVIDs, but a significantly larger LVM compared to controls. MUN males also exhibited a significantly lower ejection fraction compared to sex-matched controls (Fig 7A).
Fig 7. Echocardiographic parameters in 22-month old rats.
(A) male and (B) female offspring from rats exposed to maternal undernutrition during pregnancy (MUN) and rats fed ad libitum (Control). Interventricular septum at diastole (IVSd), posterior wall thickness at diastole (PWd), left ventricular internal diameter at diastole (LVIDd) and at systole (LVIDs), left ventricular mass (LVM) and left ventricular ejection fraction (LVEF). In parenthesis it is shown the number of rats; *p<0.05 compared to sex-matched control rats.
At old age, PWd, IVSd, were not significantly different between MUN and control females. However, LVIDd and LVIDs were significantly larger in MUN females compared to controls. In addition, a significantly larger LVM and smaller ejection fraction was observed in MUN females compared to female controls (Fig 7B).
Plasma hormones
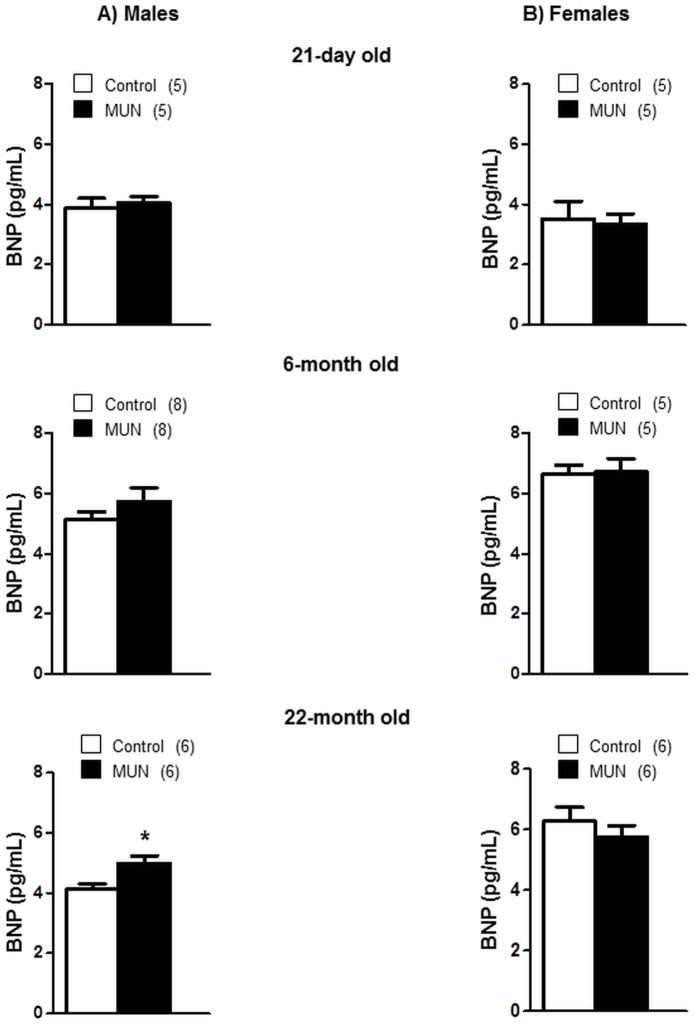
In 21-day old rats BNP plasma levels were not significantly different between MUN and control males or females. Similarly, we did not detect statistical differences between MUN and control rats at the age of 6 months either in males or in females. At the age of 22 months, MUN male rats exhibited significantly larger plasma BNP levels compared to male controls. No significant differences were found in females (Fig 8). The interaction between sex and fetal nutrition was near significance at the age of 22 months (p = 0.056, Table 2).
Fig 8. Plasma brain natriuretic peptide (BNP) levels in MUN and control rats of different ages.
(A) maleand (B) female offspring from rats exposed to maternal undernutrition during pregnancy (MUN) and rats fed ad libitum (Control). In parenthesis it is shown the number of rats; *p<0.05 compared to sex-matched control rats.
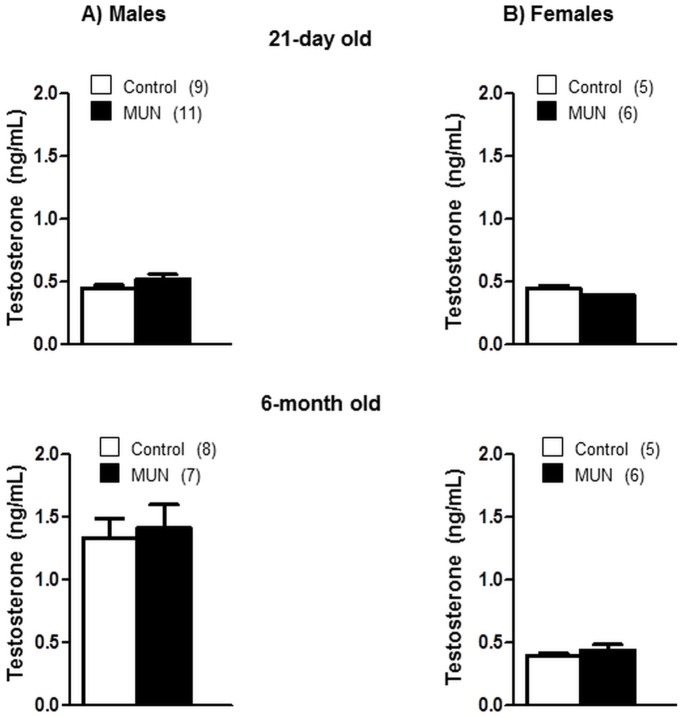
At the age of 21 days we did not detect statistical differences in testosterone levels between MUN and control males or between MUN and control females, although there was a tendency towards higher levels in MUN males (Fig 9) and the interaction between sex and fetal nutrition was near statistical significance (p = 0.07, Table 2). At the age of 6 months testosterone levels were larger in male rats compared to 21-day old rats, with no significant difference between MUN and control rats. In 6-month old female rats testosterone levels remained low with no statistical differences between MUN and control rats (Fig 9).
Fig 9. Plasma testosterone levels in 21-day and 6-month old rats.
(A) male and (B) female offspring from rats exposed to maternal undernutrition during pregnancy (MUN) and rats fed ad libitum (Control). In parenthesis it is shown the number of rats.
Discussion
Epidemiological studies worldwide have demonstrated that sub-optimal fetal growth is associated to later development of cardiovascular diseases and some of its risk factors, particularly hypertension. Despite the protection of women against fetal programming of hypertension, the association between low birth weight and heart disease is similar in men and women, particularly when the factor ageing is taken into account [15–17]. Therefore, the influence of sex on fetal programming of heart disease and the role of hypertension as risk factor is not completely elucidated. This is likely due to the difficulty to conduct longitudinal studies in humans and the number of variables which might obscure the interpretation of results. In animal models, which provide a good mean to perform long-term studies controlling environmental influences, there is clear evidence of sex influence in hypertension programming, but few studies have evaluated cardiac alterations taking into account the variable sex and ageing process. Therefore, the present work was conducted to shed light on this aspect, using a rat model of low birth weight induced by maternal global nutrient restriction. Our main findings are that: 1) in male rats fetal undernutrition induced early LVH, sustained hypertension from adult to old age and a reduction in left ventricular function in ageing; 2) females exposed to fetal undernutrition did not develop early LVH, remained normotensive throughout life, but also developed left ventricular functional loss in old age; 3) cardiac tissue oxidative disbalance might contribute to the observed heart alterations in both sexes and 4) cardiac damage at old age might be greater in males due to the presence of sustained hypertension.
MUN males developed LVH in the perinatal period, which is a critical developmental window during which the alterations induced by undernutrition in fetal life might further develop. One of the consequences of fetal undernutrition is a reduction in cell number or functional units in several tissues. In this sense, fetus or newborn animals exposed to fetal stress exhibit reduced cardiomyocyte number [29,30]. Thereafter, during postnatal development in a context of accelerated weight gain, hypertrophic responses and increased HW/BW ratio have been reported in several animal models at weaning [6,7,31,32]. We suggest that a similar process took place in MUN male rats. Despite a similar acceleration of weight in both sexes during the perinatal period, only MUN males exhibited heart hypertrophy. Hypertension can be ruled out as possible stimulus, since at the age of 21 days both MUN males and females were still normotensive. We suggest that this early cardiac hypertrophy might be related to an excess of ROS production by NADPH oxidase—an enzyme implicated in LVH [22]- based on the observed elevation of cardiac p22phox expression in MUN males. Similar findings have been previously demonstrated in male offspring from rats exposed to protein restriction in pregnancy, followed by postnatal accelerated growth, where LVH was associated with cardiac oxidative and nitrosative damage [32]. In the present study we did not evaluate markers of heart oxidative stress. However, we suggest it might also be present, based on our previous finding that MUN males, but not females, had increased plasma carbonyls at weaning [24], a parameter which exhibits a good correlation with protein oxidative damage in cardiac tissue [33].
Regarding the possible mechanism behind an early induction of NADPH oxidase in MUN males, we evaluated the possible role of testosterone, which has been implicated in sex-differences in fetal programming of hypertension [14]. Testosterone has been shown to alter renin-angiotensin-system (RAS) expression in a sex-specific manner [34] and it is well known that angiotensin II activates NADPH oxidase through AT1receptors [35]. Although we did not detect statistical differences in plasma testosterone at the age of 21 days, MUN males tended to have higher levels compared to male controls. Thereafter, in adult life, there were no differences in testosterone levels between MUN and control rats. We suggest that testosterone might have been higher in MUN males during the fetal period. To the best of our knowledge, there are no reports on fetal testosterone levels in animal models of fetal undernutrition, but there is evidence that testosterone influences placental and fetal growth with a sex-dependent pattern. For example, maternal testosterone elevation during pregnancy has been shown to induce intrauterine growth restriction [36] and a decrease in uterine arterial blood flow and placental growth, with a greater effect on males [37]. In this regard, we have previous evidence of differences between MUN males and females in placental and fetal growth at the end of gestation [38].
The molecular mechanisms responsible for the predisposition to cardiovascular disease after exposure to fetal stress are not completely elucidated. Among others, epigenetic processes—including alterations in DNA methylation, histone acetylation or non coding microRNAs- have been suggested to play a role. Furthermore, epigenetic modulation has been suggested to be responsible for cardiovascular disease transmission from one generation to another in animals exposed to fetal stress (18). In cardiac tissue, differential expression of miRNA has been reported in males exposed to global nutrient deficiency and suggested to play a role in cardiac hypertrophy (6). On the other hand, the placenta also seems to be sensitive to maternal nutrition in terms of epigenetic marks and a clear sexual dimorphism in the placental response to maternal environment has been reported [39]. The contribution of epigenetic modulation to the sex-differences in fetal programming of CVD deserves further analysis.
MUN males developed hypertension in adult age, as previously demonstrated in other rat models of fetal stress [20] and our previous report [24]. We also found that blood pressure remained elevated until ageing in MUN males, while females remained normotensive at the age of 22 months. Heart rate was not different between MUN and control rats, either in males or females, in young or adult age. However, HR was significantly reduced in 22 month old MUN males compared to controls. We only detected this difference in rats anesthetized with Diazepam/Ketamine (used as anesthesia for Echocardiography) and not in rats under Medetomidine/Ketamine anesthesia. We also found that HR was lower in animals under Medetomidine/Ketamine compared to Diazepam /Ketamine anesthesia. This is likely due to the alpha 2-adrenergic agonist effects of Medetomidine. It has been reported that this anesthesia reduces noradrenaline outflow within the central nervous system, dampening the central sympathetic tone and resulting in bradycardia [40,41]. In rats Medetomidine has also been reported to exert an initial increased in blood pressure followed by normalization [40]. We also observed that blood pressure was reduced after anesthesia and thereafter remained stable; that was the reason to obtain blood pressure measurements after 45 min. We do not have direct evidence of an increase in sympathetic activity in MUN rats, but it is likely that it occurs in this rat model, since it seems to be common to different animal models of fetal stress [18]. Therefore, under our experimental conditions, where sympathetic activity is blunted by anesthesia, it is possible that blood pressure in MUN rats, both in males and females might have been underestimated. MUN females remained normotensive at 22 months of age. However, there are some reports showing hypertension development at late stages of life in females exposed to other types of fetal stress [19,42]. Since hypertension development in females exposed to fetal stress factors seems to be related to sympathetic hyperactivation [43], we cannot rule out that, under our experimental conditions (in the presence of a reduced sympathetic activity by Medetomidine anesthesia) we failed to detect a modest increase in blood pressure in MUN females.
6-month old MUN males did not show signs of LVH measured by HW/BW. This was unexpected, given the fact of the initial hypertrophy found at weaning and the presence of high blood pressure, which is a well known stimulus for LVH [6]. Furthermore, at the age of 22 months MUN males exhibited increased HW/BW and echocardiographic signs of increased LV mass. Similar results have been described in male rats exposed to fetal low oxygen, i.e. an early heart hypertrophy, followed by normalization of HW/BW in the adult age and LVH at the age of 12 months [44]. These data support the hypothesis that different fetal insults lead to the development of similar cardiac alterations [18].
Oxidative stress is a possible mechanism responsible for the cardiac alterations found in the present study, although the enzymatic systems responsible for this disequilibrium between ROS production and elimination might be different in males and females. At the age of 6 months we found alterations in oxidative balance in MUN males due to an increase in XO, without a concomitant elevation of antioxidant enzymes. Female rats also showed oxidative disbalance, but in this case due to a generalized decrease in the enzymatic systems responsible for ROS degradation. In both cases an excess ROS is likely to take place and might be responsible for the hypertrophic response observed in ageing. A link between altered redox balance and cardiac hypertrophy has previously been reported in adult female offspring exposed to Na+ deficient diet during fetal life [45]. We cannot explain why MUN females exhibited a loss of antioxidant systems along maturation. We can suggest that the enzymatic systems responsible for ROS degradation might have been down-regulated due to a low ROS synthesis at early age (suggested by the observed reduction in NADPH oxidase expression), in a similar fashion as an increase in ROS production up-regulates antioxidant systems [46].
In both sexes, fetal undernutrition led to ventricular hypertrophy in old age, but the type of cardiac remodeling process seems to be different in MUN males and females. Thus, chamber dilatation was only observed in MUN females, but not in males, suggesting an eccentric growth. Hypertrophy was accompanied by reduction in ventricular function in both sexes, as shown by the lower ejection fraction in MUN rats. This functional loss might be related to excess collagen deposition which would reduce heart mechanical performance. It is possible that MUN heart exhibits increased collagen, since ROS elevation is known to participate in fibrosis and we found a pro-oxidative state in MUN cardiac tissue. Furthermore, increased fibrillar collagen has been reported in adult male rats exposed to fetal hypoxia and also in rats exposed to undernutrition [8], suggesting that it might be a common alteration induced by fetal stress. Cardiac fibrosis is likely to be larger in MUN males, due to the presence of both a pro-oxidative state from early age and hypertension, which is another stimulus for collagen synthesis. Hypertension might also be responsible for the observed increase in plasma BNP levels in aged MUN males, since natriuretic peptides, including atrial natriuretic peptide (ANP) and BNP, are released from the heart in response to overload [47]. Natriuretic peptides are considered biomarkers of cardiac disease, particularly in systolic heart failure. For example, circulating levels of these peptides correlate with echocardiographic evidence and with plasma markers of cardiac dysfunction in a pig model of malnutrition in early life [48]. Despite the similar reduction in ejection fraction in aged MUN males and females, plasma BNP was only elevated in males. These data suggest that males exposed to fetal undernutrition develop a larger degree of cardiac damage along ageing.
Regarding our initial hypothesis we conclude that females exposed to fetal undernutrition are better adapted than males at early stages of postnatal development and do not present cardiac alterations. However, in ageing females, like males, develop LVH and loss of heart function, although the severity of the cardiac damage might be lower, due to the absence of hypertension. These data, obtained in an experimental animal model, might explain the similar risk of heart disease in women exposed to fetal undernutrition, despite their relative protection against hypertension development.
Supporting information
SOD, superoxide dismutases; Cu/Zn-SOD, Mn-SOD and extracellular SOD (EC-SOD); catalase; p22phox and XO, xanthine oxidase, in cardiac tissue from 21-day and 6-month old male and female offspring from rats exposed to maternal undernutrition during pregnancy (MUN) and rats fed ad libitum (Control), relativized to GADPH expression.
(DOCX)
Blood pressure was recorded under Medetomidine/Ketamine anesthesia. MUN, rats exposed to maternal undernutrition during pregnancy; Control, rats fed ad libitum; M, males; F, females. Each chart represents 10 min recording period of the pressure wave at the beginning of the experiment (10 min after anesthesia) and at 45 min after anesthesia.
(TIF)
Acknowledgments
This work was supported by Ministerio de Economía y Competitividad (Spain); Grant number: FEM2015-63631-R to SMA.
We would like to acknowledge the aid of David Muñoz, Responsible for the Animal House Facility of Universidad Autónoma de Madrid, for his help in the maintenance and care of the animals and Dr. M Rosario López-Giménez for her help with statistical analysis.
There are no conflicts of interest.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by Ministerio de Economía y Competitividad (Spain), Grant number: FEM2015-63631-R to SMA. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Barker D, Osmond C. Infant mortality, childhood nutrition, and ischaemic heart disease in England and Wales. The Lancet 1986;327(8489):1077–1081. [DOI] [PubMed] [Google Scholar]
- 2.Stein C, Fall C, Kumaran K, Osmond C, Barker D, Cox V. Fetal growth and coronary heart disease in South India. The Lancet 1996;348(9037):1269–1273. [DOI] [PubMed] [Google Scholar]
- 3.Barker D, Clark P. Fetal undernutrition and disease in later life. Rev Reprod 1997;2(2):105–112. [DOI] [PubMed] [Google Scholar]
- 4.Eriksson JG, Forsen T, Tuomilehto J, Winter PD, Osmond C, Barker DJ. Catch-up growth in childhood and death from coronary heart disease: longitudinal study. BMJ 1999;318(7181):427–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Painter R, Roseboom T, Bleker O. Prenatal exposure to the Dutch famine and disease in later life: an overview. Reproductive Toxicol 2005;20(3):345–352. [DOI] [PubMed] [Google Scholar]
- 6.Gray C, Li M, Patel R, Reynolds C, Vickers M. Let-7 miRNA Profiles Are Associated With the Reversal of Left Ventricular Hypertrophy and Hypertension in dult Male Offspring From Mothers Undernourished During Pregnancy After Preweaning Growth Hormone Treatment. Endocrinology 2014;155(12):4808–4817. 10.1210/en.2014-1567 [DOI] [PubMed] [Google Scholar]
- 7.Gezmish O, Tare M, Parkington H, Morley R, Porrello E, Bubb K, et al. Maternal vitamin D deficiency leads to cardiac hypertrophy in rat offspring. Reprod Sci 2010;17(2):168–176. 10.1177/1933719109349536 [DOI] [PubMed] [Google Scholar]
- 8.Xu Y, Williams S, O'Brien D, Davidge S. Hypoxia or nutrient restriction during pregnancy in rats leads to progressive cardiac remodeling and impairs postischemic recovery in adult male offspring. FASEB J 2006;20(8):1251–1253. 10.1096/fj.05-4917fje [DOI] [PubMed] [Google Scholar]
- 9.Elmes M, Gardner D, Langley-Evans S. Fetal exposure to a maternal low-protein diet is associated with altered left ventricular pressure response to ischaemia–reperfusion injury. Br J Nutr 2007;98(01):93–100. [DOI] [PubMed] [Google Scholar]
- 10.Hu X, Levy A, Hart E, Nolan L, Dalton G, Levi A. Intra-uterine growth retardation results in increased cardiac arrhythmias and raised diastolic blood pressure in adult rats. Cardiovasc Res 2000;48(2):233–243. [DOI] [PubMed] [Google Scholar]
- 11.Huxley VH. Sex and the cardiovascular system: the intriguing tale of how women and men regulate cardiovascular function differently. Adv Physiol Educ 2007;31(1):17–22. 10.1152/advan.00099.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miller VM, Reckelhoff JF, Sieck GC. Physiology'simpact: stop ignoring the obvious-sex matters! Physiology (Bethesda) 2014;29(1):4–5. [DOI] [PubMed] [Google Scholar]
- 13.Mosca L, Barrett-Connor E, Wenger NK. Sex/gender differences in cardiovascular disease prevention: what a difference a decade makes. Circulation 2011;124(19):2145–2154. 10.1161/CIRCULATIONAHA.110.968792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dasinger JH, Alexander BT. Gender differences in developmental programming of cardiovascular diseases. Clin Sci (Lond) 2016;130(5):337–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Osmond C, Barker D, Winter P, Fall C, Simmonds S. Early growth and death from cardiovascular disease in women. BMJ 1993;307(6918):1519–1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rich-Edwards J, Stampfer M, Manson J, Rosner B, Hankinson S, Colditz G, et al. Birth weight and risk of cardiovascular disease in a cohort of women followed up since 1976. BMJ 1997;315(7105):396–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lawlor DA, Davey Smith G, Ebrahim S. Birth weight is inversely associated with coronary heart disease in post-menopausal women: findings from the British women's heart and health study. J Epidemiol Community Health 2004;58(2):120–125. 10.1136/jech.58.2.120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alexander B, Dasinger J, Intapad S. Fetal programming and cardiovascular pathology. Comprehensive Physiology 2015; 5(2):997–1025. 10.1002/cphy.c140036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ozaki T, Nishina H, Hanson M, Poston L. Dietary restriction in pregnant rats causes gender-related hypertension and vascular dysfunction in offspring. J Physiol (Lond) 2001;530(1):141–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grigore D, Ojeda N, Alexander B. Sex differences in the fetal programming of hypertension. Gender Medicine 2008;5:S121–S132. 10.1016/j.genm.2008.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Woods LL, Ingelfinger JR, Rasch R. Modest maternal protein restriction fails to program adult hypertension in female rats. Am J Physiol (Regul Integr Comp Physiol) 2005;289(4):R1131–R1136. [DOI] [PubMed] [Google Scholar]
- 22.Sirker A, Zhang M, Murdoch C, Shah A. Involvement of NADPH oxidases in cardiac remodelling and heart failure. Am J Nephrol 2007;27(6):649–660. 10.1159/000109148 [DOI] [PubMed] [Google Scholar]
- 23.Byrne JA, Grieve DJ, Cave AC, Shah AM. Oxidative stress and heart failure. Arch Mal Coeur Vaiss 2003;96(3):214–221. [PubMed] [Google Scholar]
- 24.Rodríguez-Rodríguez P, de Pablo A, Condezo-Hoyos L, Martín-Cabrejas M, Aguilera Y, Ruiz-Hurtado G, et al. Fetal undernutrition is associated with perinatal sex-dependent alterations in oxidative status. J Nutr Biochem 2015;26(12):1650–1659. 10.1016/j.jnutbio.2015.08.004 [DOI] [PubMed] [Google Scholar]
- 25.Condezo-Hoyos L, Arribas S, Abderrahim F, Somoza B, Gil-Ortega M, Diaz-Gil J, et al. Liver growth factor treatment reverses vascular and plasmatic oxidative stress in spontaneously hypertensive rats. J Hypertens 2012; 30(6):1185–1194. [DOI] [PubMed] [Google Scholar]
- 26.Somoza B, Guzman R, Cano V, Merino B, Ramos P, Diez-Fernandez C, et al. Induction of cardiac uncoupling protein-2 expression and adenosine 5′-monophosphate-activated protein kinase phosphorylation during early states of diet-induced obesity in mice. Endocrinology 2007;148(3):924–931. 10.1210/en.2006-0914 [DOI] [PubMed] [Google Scholar]
- 27.Quintana-Villamandos B, Delgado-Martos MJ, Sánchez-Hernández JJ, Gómez de Diego Jose Juan, del Carmen Fernández-Criado M, Canillas F, et al. Early regression of left ventricular hypertrophy after treatment with esmolol in an experimental rat model of primary hypertension. Hypertens Res 2013;36(5):408–413. 10.1038/hr.2012.191 [DOI] [PubMed] [Google Scholar]
- 28.Devereux R. Detection of left ventricular hypertrophy by M-mode echocardiography. Anatomic validation, standardization, and comparison to other methods. Hypertension 1987;9(2 Pt 2):II19–26. [DOI] [PubMed] [Google Scholar]
- 29.Corstius H, Zimanyi M, Maka N, Herath T, Thomas W, Van Der Laarse A, et al. Effect of intrauterine growth restriction on the number of cardiomyocytes in rat hearts. Pediatr Res 2005;57(6):796–800. 10.1203/01.PDR.0000157726.65492.CD [DOI] [PubMed] [Google Scholar]
- 30.Stacy V, De Matteo R, Brew N, Sozo F, Probyn M, Harding R, et al. The influence of naturally occurring differences in birth weight on ventricular cardiomyocyte number in sheep. Anat Rec 2009;292(1):29–37. [DOI] [PubMed] [Google Scholar]
- 31.Tappia P, Guzman C, Dunn L, Aroutiounova N. Adverse cardiac remodeling due to maternal low protein diet is associated with alterations in expression of genes regulating glucose metabolism. Nutr Metabol Cardiovasc Dis 2013;23(2):130–135. [DOI] [PubMed] [Google Scholar]
- 32.Tarry-Adkins J, Martin-Gronert M, Fernandez-Twinn D, Hargreaves I, Alfaradhi M, Land J, et al. Poor maternal nutrition followed by accelerated postnatal growth leads to alterations in DNA damage and repair, oxidative and nitrosative stress, and oxidative defense capacity in rat heart. FASEB J 2013;27(1):379–390. 10.1096/fj.12-218685 [DOI] [PubMed] [Google Scholar]
- 33.Veskoukis A, Nikolaidis M, Kyparos A, Kouretas D. Blood reflects tissue oxidative stress depending on biomarker and tissue studied. Free Radical Biol Med 2009;47(10):1371–1374. [DOI] [PubMed] [Google Scholar]
- 34.Fischer M, Baessler A, Schunkert H. Renin angiotensin system and gender differences in the cardiovascular system. Cardiovasc Res 2002;53(3):672–677. [DOI] [PubMed] [Google Scholar]
- 35.Balakumar P, Jagadeesh G. A century old renin–angiotensin system still grows with endless possibilities: AT 1 receptor signaling cascades in cardiovascular physiopathology. Cell Signal 2014;26(10):2147–2160. 10.1016/j.cellsig.2014.06.011 [DOI] [PubMed] [Google Scholar]
- 36.Manikkam M, Crespi EJ, Doop DD, Herkimer C, Lee JS, Yu S, et al. Fetal programming: prenatal testosterone excess leads to fetal growth retardation and postnatal catch-up growth in sheep. Endocrinology 2004;145(2):790–798. 10.1210/en.2003-0478 [DOI] [PubMed] [Google Scholar]
- 37.Gopalakrishnan K, Mishra JS, Chinnathambi V, Vincent KL, Patrikeev I, Motamedi M, et al. Elevated Testosterone Reduces Uterine Blood Flow, Spiral Artery Elongation, and Placental Oxygenation in Pregnant Rats. Hypertension 2016;67(3):630–639. 10.1161/HYPERTENSIONAHA.115.06946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reyes-Hernández CG, Ramiro-Cortijo D, Rodríguez-Rodríguez P, Gutiérrez-Arzapalo PY, González MC, López de Pablo AL, et al. Differences in the response of male and female rats to maternal undernutrition during gestation. J Physiol Biochem 2016;72: 1 ( S64–S65). [Google Scholar]
- 39.Tarrade A, Panchenko P, Junien C, Gabory A. Placental contribution to nutritional programming of health and diseases: epigenetics and sexual dimorphism. J Exp Biol 2015;218(Pt 1):50–58. 10.1242/jeb.110320 [DOI] [PubMed] [Google Scholar]
- 40.Savola JM. Cardiovascular actions of medetomidine and the irreversal by atipamezole. Acta Vet Scand Suppl 1989;85:39–47. [PubMed] [Google Scholar]
- 41.Sinclair MD. A review of the physiological effects of alpha2-agonists related to the clinical use of medetomidine in small animal practice. Can Vet J 2003;44(11):885–897. [PMC free article] [PubMed] [Google Scholar]
- 42.Franco M, Akamine E, Rebouças N, Carvalho M, Tostes R, Nigro D, et al. Long-term effects of intrauterine malnutrition on vascular function in female offspring: implications of oxidative stress. Life Sci 2007;80(8):709–715. 10.1016/j.lfs.2006.10.028 [DOI] [PubMed] [Google Scholar]
- 43.Intapad S, Tull FL, Brown AD, Dasinger JH, Ojeda NB, Fahling JM, et al. Renal denervation abolishes the age-dependent increase in blood pressure in female intrauterine growth-restricted rats at 12 months of age. Hypertension 2013; 61(4):828–834. 10.1161/HYPERTENSIONAHA.111.00645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rueda-Clausen CF, Morton JS, Davidge ST. Effects of hypoxia-induced intrauterine growth restriction on cardiopulmonary structure and function during adulthood. Cardiovasc Res 2009;81:713–722. 10.1093/cvr/cvn341 [DOI] [PubMed] [Google Scholar]
- 45.Battista M, Calvo E, Chorvatova A, Comte B, Corbeil J, Brochu M. Intra-uterine growth restriction and the programming of left ventricular remodelling in female rats. J Physiol (Lond) 2005;565(1):197–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jauniaux E, Watson AL, Hempstock J, Bao Y, Skepper JN, Burton GJ. Onset of maternal arterial blood flow and placental oxidative stress: a possible factor in human early pregnancy failure. Am J Pathol 2000;157(6):2111–2122. 10.1016/S0002-9440(10)64849-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Daniels LB, Maisel AS. Natriuretic peptides. J Am Coll Cardiol 2007;50(25):2357–2368. 10.1016/j.jacc.2007.09.021 [DOI] [PubMed] [Google Scholar]
- 48.Fabiansen C, Lykke M, Hother A, Koch J, Nielsen OB, Hunter I, et al. Cardiac dysfunction in a porcine model of pediatric malnutrition. PloSone 2015;10(10):e0140472. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SOD, superoxide dismutases; Cu/Zn-SOD, Mn-SOD and extracellular SOD (EC-SOD); catalase; p22phox and XO, xanthine oxidase, in cardiac tissue from 21-day and 6-month old male and female offspring from rats exposed to maternal undernutrition during pregnancy (MUN) and rats fed ad libitum (Control), relativized to GADPH expression.
(DOCX)
Blood pressure was recorded under Medetomidine/Ketamine anesthesia. MUN, rats exposed to maternal undernutrition during pregnancy; Control, rats fed ad libitum; M, males; F, females. Each chart represents 10 min recording period of the pressure wave at the beginning of the experiment (10 min after anesthesia) and at 45 min after anesthesia.
(TIF)
Data Availability Statement
All relevant data are within the paper.