Abstract
Background:
Multiple sclerosis (MS) is a chronic disease that commonly affects young women and is associated with sexual dysfunction (SD) and lower anourogenital dysfunction, which affect quality of life. We evaluated the importance of an integrated multidisciplinary approach in the Lower Female Ano-Uro-Genital Network (LFAUGN) to manage a variety of complex symptoms.
Methods:
A 40-year-old woman with MS and primary concerns about perineal pain and SD was treated by a trained midwife from the LFAUGN and a physical therapist after a multidisciplinary diagnostic process that included gynecologic evaluation for perineal pain and SD, physiatric assessment, urologic assessment for bladder retention (BR), and surgical examination for obstructed defecation syndrome (ODS). Physical therapy was integrated with pharmacologic therapy for ODS and with self-catheterization for BR.
Results:
After 5 months of treatment, the patient reported improvement in functional perineal parameters and perineal pain (visual analogue scale score: 9 at T1 vs. 5 at T2), with resolution of pelvic floor hypertonia. Furthermore, ODS and BR symptoms improved (5-item score: 18 of 20 at T1 vs. 10 of 20 at T2; 1 self-catheterization daily, with postvoid residual volume [PRV] <200 mL at T1 vs. 1 self-catheterization weekly, with PRV <100 mL at T2) and sexual satisfaction increased (Female Sexual Function Index score: 18 of 36 at T1 vs. 23 of 36 at T2).
Conclusions:
These results suggest that physical therapy, as an integral component of a multidisciplinary approach in a multiprofessional network, may play a pivotal role in improving anourogenital dysfunction and sexual satisfaction.
Multiple sclerosis (MS) is a chronic progressive neurologic disease that is most likely to affect young adults, when sexual activity is high. In addition to sensory disturbances, spasticity, tremors, weakness, depression, and cognitive problems, MS is well known to have significant detrimental effects on bowel, bladder, and sexual function, worsening the quality of life. Although sexual dysfunction (SD) is common in patients with MS, it remains underdiagnosed. According to a recent literature review,1 SD prevalence ranges from 34% to 85% in women with MS and is more common and more severe than in male patients.2 In particular, reduced sexual desire is reported in 31.4% to 74.4% of women with MS, decreased lubrication in 35.7% to 48.4%, and orgasmic dysfunction in 37.0% to 44.9%.3 These data derive from standard questionnaires used to assess SD in patients with MS, helping to alleviate the common barriers that are reported by professionals when addressing sexual issues. Despite the large numbers of women who chose not to answer questions about SD in the different studies, 42% of respondents report such dysfunction, confirming that SD seems to be a major concern.4 To achieve a common and shared definition, SD is categorized as being related to primary, secondary, and tertiary consequences of the disease. Primary consequences refer to the direct result of MS-related neurologic changes on sexual function, such as impaired genital sensation, decreased sexual desire, decreased vaginal lubrication, and orgasmic dysfunction. Secondary consequences refer to the physical changes that indirectly modify sexual response (fatigue, weakness, spasticity, bladder and bowel dysfunction, incoordination, and pain). Tertiary consequences refer to psychological, emotional, social, and cultural factors that indirectly affect the experience and perception of sexuality.5 In particular, primary SD is reported to be the most common disorder because MS seems to have a direct detrimental effect on female sexuality. Nevertheless, the important role of secondary and tertiary SD should also be considered when addressing the complex nature of SD in women. Female sexuality is a multidimensional subject for which a multidisciplinary approach is necessary. Recently, several organizations have attempted to educate health-care providers on the importance of pelvic floor disorders to improve SD treatment in women affected by MS,4 but despite these reports, little literature is found on the management of SD in women with MS.
Moving away from the assumption that primary SD in MS requires interdisciplinary urologic and neurologic expertise and should, therefore, preferably be treated by specialists, we are convinced that the optimal method to address SD and pelvic floor disorder is the multidisciplinary and multiprofessional integrated approach. Different professionals devoted to managing different and complex symptoms represent the starting point of the Lower Female Ano-Uro-Genital Network (LFAUGN) model of care. This network is intended to be a new clinical and organizational model entirely devoted to lower female anourogenital tract health through a coordinated and synergistic multidisciplinary approach based on an experience started in Italy in 2014. The network is not a concrete management unit for a single disease but a new concept of “center without walls” to treat different problems in the same patient.
The unitary view of the lower female anourogenital tract is the only way to ensure more rational and effective solutions for patients. Communication between different specialists regarding the same patient is frequently suboptimal, and too often the patient has to follow a fragmented management approach. This situation may be overcome with a new patient-centered care and coordinated approach, optimizing clinical outcomes. In this article, we describe this multidisciplinary model of care in a woman with MS, which resulted in patient satisfaction and improvement. This strategy could be a substantially more effective approach to the health-care needs of women with MS, resulting in improved treatment outcomes and liberating women from the embarrassment and social and sexual isolation that multiple symptoms can generate.
Case Report
This study is a detailed report of the symptoms, signs, diagnosis, treatment, and outcomes of a patient treated in the LFAUGN of Chivasso Civic Hospital, Turin, Italy.
Patient MS History
The patient was a 40-year-old woman who experienced sudden onset of neurologic symptoms in 2008 (fatigue, cognitive deficit, and lack of coordination), leading to a diagnosis of MS after neurologic evaluation. Between her diagnosis in 2008 and March 2015, she received interferon beta-1a in accordance with the clinical protocol of the Multiple Sclerosis Centre in Turin. Between April 2015 and May 2016, a new therapy with dimethyl fumarate was administered. Chronic symptoms related to MS included paraparesis, ataxia, severe fatigability, and lower anourogenital dysfunction (perineal pain, bladder retention, and obstructed defecation syndrome).
Clinical Evaluation at LFAUGN Admission
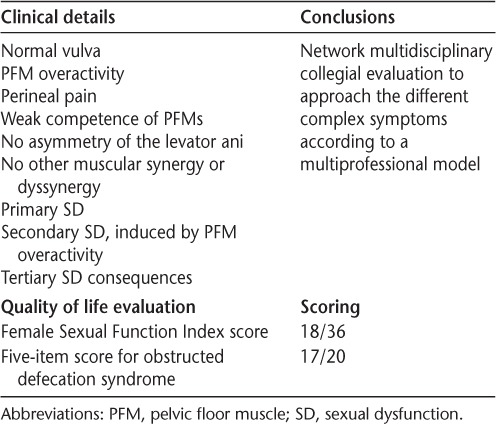
With perineal pain of 5 months' duration, the patient was admitted in June 2015 to the Pelvic Floor Rehabilitation Centre of the LFAUGN, managed by a trained midwife (Table 1).6–9
Table 1.
Clinical evaluation at admission to the Lower Female Ano-Uro-Genital Network
Network Multidisciplinary Collegial Assessment and Therapeutic Integrated Pathway
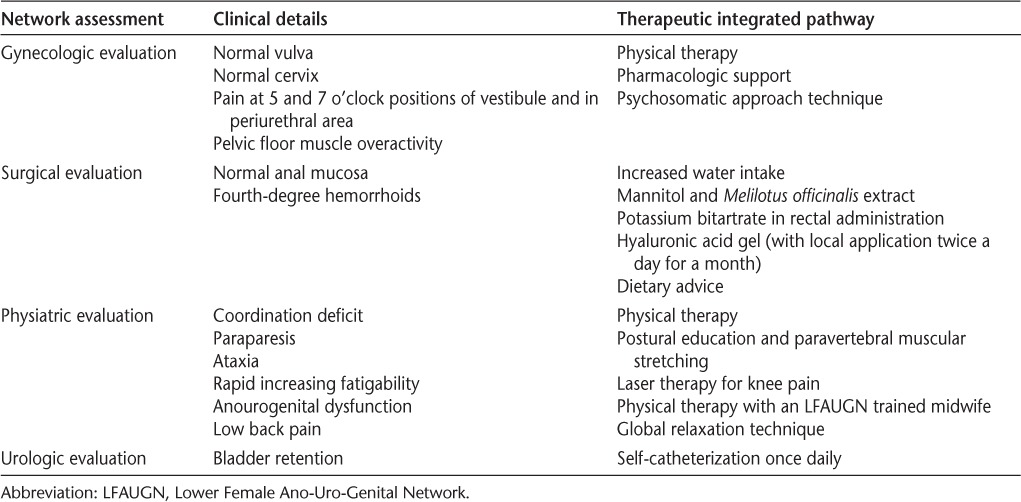
The results of the multidisciplinary collegial assessment are summarized in Table 2. Physical therapy, following an evidence-based approach,10–13 was characterized by pelvic floor muscle training, perineal massage, biofeedback, global relaxation techniques, posture correction, and self-training at home.
Table 2.
Network multidisciplinary collegial assessment and therapeutic integrated pathway
Improvement of clinical outcomes was evaluated in accordance with pelvic floor functional parameters (strength, contraction, and relaxation ability and pelvic floor muscle tone), sexual life quality (Female Sexual Function Index questionnaire score), perineal pain (visual analogue scale score), obstructed defecation syndrome symptoms (5-item score), and bladder retention (number of self-catheterizations, quantity of urine retained according to postvoid residual volume [PRV]) at LFAUGN admission (T1) and after treatment (T2). After 5 months of treatment, the woman reported the following: 1) an increase in the strength of pelvic floor muscle contractions (pelvic contraction test: 1 of 5 at T1 vs. 2 of 5 at T2); 2) correction of pelvic floor muscle overactivity, with improvement in contraction and relaxation ability; 3) augmentation of sexual satisfaction according to the Female Sexual Function Index score (18 of 36 at T1 vs. 23 of 36 at T2); 4) reduction of vulvar and perineal pain (visual analogue scale score: 9 at T1 vs. 5 at T2); 5) correction of obstructed defecation syndrome (5-item score: 18 of 20 at T1 vs. 10 of 20 at T2); and 6) decrease of bladder retention symptoms (1 self-catheterization per day, with PRV <200 mL at T1 vs. 1 self-catheterization per week, with PRV <100 mL at T2). Interestingly, the woman reported a high level of satisfaction with the clinical pathway, as revealed by a satisfaction questionnaire (100 of 100 points).
Discussion
MS is well known to encompass a variety of symptoms, including motor impairments (spasticity and muscle weakness), autonomic dysfunctions (bladder and bowel), pain, and cognitive impairments (pain, fatigue, cognition, affect/emotional, and depression), to which can be added the adverse effects of medications. Multiple symptoms require a multimodal approach, according to the literature.14,15 In the past few decades, research has addressed how these symptoms affect the quality of life of patients with MS; however, few studies assess the management of SD in women. Sexual dysfunction is a prevalent and destructive manifestation of the disease that severely affects quality of life. It can present even without a severe physical or neurologic impairment, and in young patients it is often considered the most devastating aspect of the disease because they may lose the physical ability to communicate, embrace, stimulate, engage in intercourse, and maintain urinary and bowel continence during sexual activity. Pelvic floor dysfunction is common in MS, and the importance of the interdependence of mechanical, neural, endocrine, and environmental factors in its development should be well recognized by health-care providers. In reality, functional pelvic floor problems are perceived to have low priority compared with other disorders in MS, and treatment remains suboptimal. There is a lack of data investigating the true prevalence, incidence, specific risk factors, poor outcomes of treatment, and subsequent prevention strategies for women with MS with multiple pelvic floor symptoms. Indeed, specific lesions, such as brainstem lesions and pyramidal impairments, have been correlated with SD, even if with contradictory results, but it is evident that SD affects sexual experience, determining changes in self-perception, feelings of being less sexually attractive, and worries about sexually satisfying the partner and communication difficulties. Because of the complexity of SD in patients with MS and the negative impact that SD can have on quality of life, multidisciplinary evaluations16 that include neurologic, urologic/gynecologic, and psychological components should be performed by the health-care team when treating patients with MS.
According to the present results, correct assessment of pelvic floor dysfunction permits improvement of the secondary and tertiary consequences of MS related to SD. In this light, physical therapy may play a pivotal role in improving symptoms and should be considered the first step of the integrated therapeutic multidisciplinary network system.17 In addition, the trained midwife, owing to her particular background, may help patients overcome embarrassment in talking about sexual problems and, initiating an assessment of the dysfunction and proceeding with a comprehensive clinical interview, should identify the SD; standardized questionnaires may be used to explore SD in detail. Consequently, counseling about convenient sexual positions, planning sexual activity in the early morning hours, performing bladder catheterization before sexual activity, and avoiding pressure on the bladder during the activity can help limit the effects of fatigue, spasticity, and bladder dysfunction on sexual experience.
In the present patient, after 5 months of therapy primarily addressing reduction of pelvic muscle overactivity, improvements were also observed in bladder and bowel dysfunctions. Pelvic floor overactivity acts on bladder function and plays a detrimental role in the defecation mechanism, and health-care providers should keep in mind this important issue, no matter what stage of disease the patient exhibits. Patients can be satisfied with the care they receive for their urinary and bowel symptoms but dissatisfied with the care they receive regarding SD issues. Similarly, patient satisfaction with the care received from health-care providers affects quality of life.
The literature supports the present multidisciplinary collegial assessment and therapeutic integrated pathway, in which trained health-care providers identify and develop comprehensive interdisciplinary, multiprofessional strategies that improve the assessment and treatment of MS disorders, with particular reference to SD and pelvic floor dysfunction.18
Conclusion
This article describes an innovative model of care for the provision of women's health-care services. In a health-care system based on the concept of resource optimization and clinical governance, a multiprofessional approach to different pelvic floor disorders related to MS could be the optimal strategy to achieve more effective care for women's health needs, resulting in improved treatment quality and clinical outcomes and liberating women from the embarrassment, social and sexual isolation, restriction of employment and leisure opportunities, and potential loss of independence that multiple symptoms can generate.
PracticePoints
Sexual and anourogenital tract dysfunction affects the quality of life of young women with MS.
We report positive outcomes for pelvic floor muscle function, pelvic pain, sexual satisfaction, and elimination dysfunction in a woman with MS using a multidisciplinary approach in a structured clinical network.
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose.
References
- 1. Ashtari F, Rezvani R, Afshar H.. Sexual dysfunction in women with multiple sclerosis: dimensions and contributory factors. J Res Med Sci. 2014; 19: 228– 233. [PMC free article] [PubMed] [Google Scholar]
- 2. Celik DB, Poyraz EÇ, Bingöl A, Idiman E, Ozakbaş S, Kaya D.. Sexual dysfunction in multiple sclerosis: gender differences. J Neurol Sci. 2013; 324: 17– 20. [DOI] [PubMed] [Google Scholar]
- 3. Lew-Starowicz M, Rola R.. Prevalence of sexual dysfunctions among women with multiple sclerosis. Sex Disabil. 2013; 31: 141– 153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mahajan ST, James R, Frasure H.. Pelvic floor disorders and multiple sclerosis. Int J MS Care. 2014; 16: 20– 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cordeau D, Courtois F.. Sexual disorders in women with MS: assessment and management. Ann Phys Rehabil Med. 2014; 57: 337– 347. [DOI] [PubMed] [Google Scholar]
- 6. Huskisson EC. Measurement of pain. Lancet. 1974; 2: 1127– 1131. [DOI] [PubMed] [Google Scholar]
- 7. Da Roza T, Mascarenhas T, Araujo M, Trinidade V, Jorge RN.. Oxford Grading Scale vs manometer for assessment of pelvic floor strength in nulliparous sports students. Physiotherapy. 2013; 99: 207– 211. [DOI] [PubMed] [Google Scholar]
- 8. Rosen R, Brown C, Heiman J, . et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000; 26: 191– 208. [DOI] [PubMed] [Google Scholar]
- 9. Renzi A, Brillantino A, Di Sarno G, D'Aniello F.. Five-item score for obstructed defecation syndrome: study of validation. Surg Innov. 2013; 20: 119– 125. [DOI] [PubMed] [Google Scholar]
- 10. Rosenbaum TY, Owens A.. The role of pelvic floor physical therapy in the treatment of pelvic and genital pain-related sexual dysfunctions (CME). J Sex Med. 2008; 5: 513– 523. [DOI] [PubMed] [Google Scholar]
- 11. Hartmann D, Sarton J.. Chronic pelvic floor dysfunction. Best Pract Res Clin Obstet Gynaecol. 2014; 28: 977– 990. [DOI] [PubMed] [Google Scholar]
- 12. Kessler TM, Fowler CJ, Panicker JN.. Sexual dysfunction in multiple sclerosis. Expert Rev Neurother. 2009; 9: 341– 350. [DOI] [PubMed] [Google Scholar]
- 13. Lucio AC, D'Ancona CA, Lopes MH, Perissinotto MC, Damasceno BP.. The effect of pelvic floor muscle training alone or in combination with electrostimulation in the treatment of sexual dysfunction in women with multiple sclerosis. Mult Scler. 2014; 20: 1761– 1768. [DOI] [PubMed] [Google Scholar]
- 14. Crayton HJ, Rossman HS.. Managing the symptoms of multiple sclerosis: a multimodal approach. Clin Ther. 2006; 28: 445– 460. [DOI] [PubMed] [Google Scholar]
- 15. Gallien P, Gich J, Sanchez-Dalmau BF, Feneberg W.. Multidisciplinary management of multiple sclerosis symptoms. Eur Neurol. 2014; 72( suppl 1): 20– 25. [DOI] [PubMed] [Google Scholar]
- 16. Fletcher SG, Castro-Borrero W, Remington G, Treadaway K, Lemack GE, Frohman EM.. Sexual dysfunction in patients with multiple sclerosis: a multidisciplinary approach to evaluation and management. Nat Clin Pract Urol. 2009; 6: 96– 107. [DOI] [PubMed] [Google Scholar]
- 17. Bronner G, Elran E, Golomb J, Korczyn AD.. Female sexuality in multiple sclerosis: the multidimensional nature of the problem and the intervention. Acta Neurol Scand. 2010; 121: 289– 301. [DOI] [PubMed] [Google Scholar]
- 18. Clavelou P. Can we optimize our teams? multidisciplinary care for multiple sclerosis. Expert Rev Neurother. 2013; 13( suppl): 39– 44. [DOI] [PubMed] [Google Scholar]


