Abstract
Objectives:
To develop and determine convergent validity and reliability of a simple and inexpensive clinical test to quantify back extensor muscle strength.
Methods:
Two testing sessions were conducted, 7 days apart. Each session involved three trials of standing maximal isometric back extensor muscle strength using both the novel test and isokinetic dynamometry. Lumbar spine bone mineral density was examined by dual-energy X-ray absorptiometry. Validation was examined with Pearson correlations (r). Test–retest reliability was examined with intraclass correlation coefficients and limits of agreement. Pearson correlations and intraclass correlation coefficients are presented with corresponding 95% confidence intervals. Linear regression was used to examine the ability of peak back extensor muscle strength to predict indices of lumbar spine bone mineral density and strength.
Results:
A total of 52 healthy adults (26 men, 26 women) aged 46.4 ± 20.4 years were recruited from the community. A strong positive relationship was observed between peak back extensor strength from hand-held and isokinetic dynamometry (r = 0.824, p < 0.001). For the novel back extensor strength test, short- and long-term reliability was excellent (intraclass correlation coefficient = 0.983 (95% confidence interval, 0.971–0.990), p < 0.001 and intraclass correlation coefficient = 0.901 (95% confidence interval, 0.833–0.943), p < 0.001, respectively). Limits of agreement for short-term repeated back extensor strength measures with the novel back extensor strength protocol were −6.63 to 7.70 kg, with a mean bias of +0.71 kg. Back extensor strength predicted 11% of variance in lumbar spine bone mineral density (p < 0.05) and 9% of lumbar spine index of bone structural strength (p < 0.05).
Conclusion:
Our novel hand-held dynamometer method to determine back extensor muscle strength is quick, relatively inexpensive, and reliable; demonstrates initial convergent validity in a healthy population; and is associated with bone mass at a clinically important site.
Keywords: Bone mineral density, isometric strength test, muscle strength, test–retest reliability
Introduction
Osteoporosis, a condition of reduced bone mass and increased risk of fracture, affects around 1.2 million Australians,1 10.2 million (10.3%) Americans,2 and 15 million European men and women over 50 years of age.3 Most osteoporotic fractures occur at the spine and are associated with reduced quality of life4 and increased risk of further fractures.5 Deficiency in back extensor muscle strength is thought to contribute to an elevation in risk of falling6–9 and poor bone mass.10–13 The accurate determination of back extensor strength could therefore contribute to the recognition of risk for osteoporotic fracture of the spine and guide strategies to mitigate that risk.
Isokinetic dynamometry is considered a valid and reliable device used to determine the force, or torque, generated by a muscle group for a specific action,14 having good-to-excellent reliability (intraclass correlation coefficients (ICCs) of 0.81–0.85 in sitting,15 and 0.87–0.95 in standing14). Isokinetic dynamometry, however, is not universally accessible and is rarely used clinically owing to its high cost, requirement for considerable user expertise, and protracted testing time. Hand-held dynamometry (HHD) is an appealing alternative to isokinetic dynamometry, being simple, quick, and inexpensive and therefore highly practical for use in the clinical setting. Measurement validity for upper16–18 and lower19–21 extremity muscle strength has been established for HHD. Reliability of HHD-measured back extensor strength has also been examined; however, no acceptable technique has been identified.22
Currently, the most widely used test of isometric back extensor strength is the prone Biering-Sørensen test, in which a HHD is held over the interscapular region by the examiner against which the participant is asked to exert maximal counter pressure.23 Not surprisingly, in light of the variable degree of potential resistance on the HHD from the examiner, the open-chain Biering-Sørensen test exhibits poor measurement reliability (ICC = 0.24).23 The original study investigated whether this physical performance measure (trunk muscle isometric endurance) could predict first time occurrence of nonspecific low back pain at 1-year follow-up; however, approximately one-quarter of the sample had to discontinue the test due to acute test-related back pain.24 Furthermore, the Biering-Sørensen method was intended for application in healthy, able-bodied athletic populations to examine isometric trunk muscle endurance from a performance perspective.25 Modification of the Biering-Sørensen test to incorporate a hand-held dynamometer to determine isometric trunk muscle strength in the prone position does not provide a useful surrogate test of functional back extensor strength in the standing position, nor does it account for the influence of upper body mass on performance; both of which may influence the ability to detect longitudinal changes in functional muscle strength. Our novel test is free of those limitations and is validated in an older, more clinically relevant population. A recent modification of the test that introduced passive HHD fixation (closed-chain) improved test reliability (ICC = 0.90);26 however, the testing technique requires participants to hyperextend their spine, which often cannot be achieved or tolerated by patients with hyperkyphosis, and may present an injury risk.27 In order to be clinically useful, a more feasible, comfortable test that provides an accurate and reliable measure of back extensor strength in a range of ages is required.
The aims of this study, therefore, were to: (1) develop a clinically amenable test of back extensor strength, (2) determine convergent validity of the novel test against a recognised valid and reliable device, (3) establish short- and long-term test–retest reliability of the novel back extensor strength test, and (4) determine the relationship between back extensor strength from the novel test and lumbar spine bone mass. We hypothesised the novel method would exhibit strong convergent validity and high test–retest reliability and anticipated back extensor strength would be positively associated with lumbar spine bone mineral density (BMD).
Methods
Ethical approval
The study was approved by the Griffith University Human Research Ethics Committee (Protocol number AHS/39/14/HREC), and all research activities were conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants prior to testing.
Participants, recruitment and screening
Apparently healthy, able-bodied men and women over 18 years of age were recruited from the community. Volunteers were excluded if they had symptomatic back pain in the past 3 months, low back or lower extremity injury, recent surgery, metal implants, or medical conditions affecting muscle. Pregnant women or individuals who had undertaken multiple recent radiographic investigations were also excluded to avoid further radiation exposure.
Study design
Each participant attended two testing sessions, session 1 (S1) and session 2 (S2), 7 days apart. The period was chosen to allow for the resolution of any muscle soreness following unaccustomed maximal isometric contractions, but to limit any potential muscle training adaptations between sessions. At S1, anthropometrics were measured and back extensor strength from both the novel HHD test and the isokinetic dynamometer were determined. The order of tests was randomised with the aid of a random number generator (Excel 2003, Microsoft Office, USA). The same testing order was followed at S2, and participants additionally underwent testing of lumbar spine BMD. All assessments were performed by an exercise scientist and physiotherapist.
Anthropometric measures
Height was measured to the nearest 0.1 cm via the stretch stature method with a wall-mounted stadiometer (Model S-220; Seca, Hamburg, Germany) with shoes and socks removed. Weight was measured to the nearest 0.1 kg using a mechanical beam scale (Model 700; Seca, Hamburg, Germany). Body mass index (BMI) was determined from measures of height and weight per the accepted method (BMI = weight/height2, kg/m2).
Isokinetic dynamometer back extensor muscle strength test
The isokinetic dynamometer (System 4 Pro™, Biodex Medical Systems, Shirley, NY, USA), a device commonly used to determine muscle force, was selected as the technique to validate the novel back extensor strength test against in this study (Figure 1). To mimic our HHD back extensor strength task, the standard manufacturer support plate was secured vertically to the front of the Biodex chair so it was positioned behind the participant’s pelvis and buttocks. Chair height was adjusted so that the top of the plate was aligned with the posterior superior iliac spines of the pelvis. Once standing in position, the participant was firmly secured against the plate, using the same inelastic belt used in the novel HHD test strapped 1 cm below the anterior superior iliac spines. The Biodex attachment arm was positioned so that the middle of the pad was aligned over the spinous process of the seventh thoracic vertebra. Participants positioned their arms as for the novel test.
Figure 1.
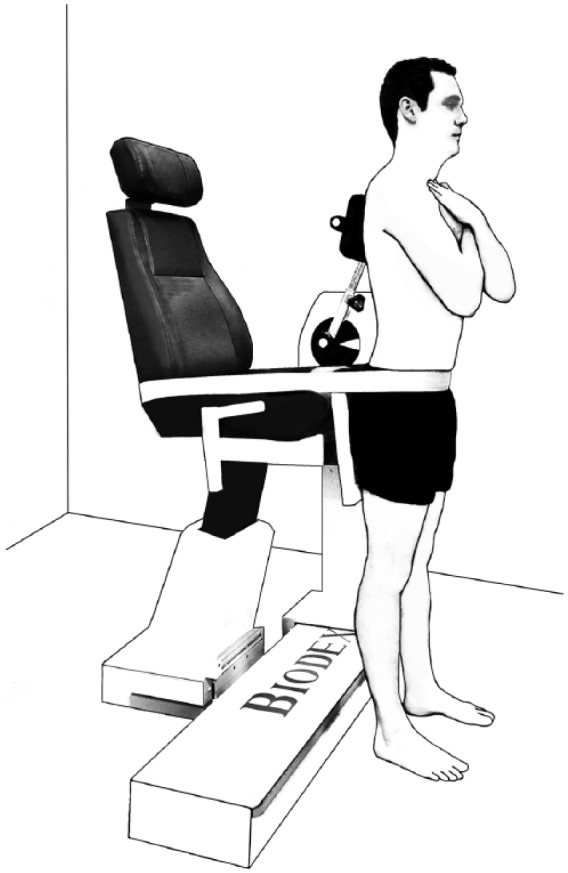
Participant and dynamometer positioning for isometric back extensor strength measures with the isokinetic dynamometer.
Once positioned, each participant performed one to two submaximal practice trials for familiarisation. Instructions were given that included the following: ‘We are going to do a test of your back muscle strength with this machine called a Biodex dynamometer. You need to push back as hard as you can with your shoulders into the pad’. To initiate each trial, participants were instructed to gently extend their back to place some counter pressure on the pad. From this position, a standard count of 3 was given before the participant initiated each trial. Commensurate with the HHD task, participants were instructed to ‘push, push, push, and relax’ during each 5-s trial. A 30-s rest period was inserted between trials. Peak torque (N m) achieved during each trial was recorded as the index of back extensor strength for comparison with the novel HHD method.
Novel back extensor muscle strength test
The novel back extensor strength task involved the participant standing in full extension with their back to a wall, midway between two vertically oriented anchor rails, and feet flat on the floor with heels touching the wall (Figure 2). An inelastic belt was looped through the anchor rails, and secured firmly around the participant, 1 cm below the anterior superior iliac spines in order to restrain movement and maintain participant contact with the wall during the test. To standardise posture, arms were crossed over the chest, with finger tips level with the contralateral shoulders. The participant was instructed to flex forward approximately 15° at the hips so the HHD (Lafayette Manual Muscle Testing Systems; Lafayette, USA) could be positioned posterior to the spinous process of the seventh thoracic vertebrae. In this way, counter pressure was provided by the fixed wall behind the participants’ back so that variations in resistance by an examiner were avoided. To minimise excessive local bony pressure, the curved pressure plate of the HHD (1 cm × 3 cm padded with 2 mm high density foam) was positioned perpendicularly to the long axis of the vertebral column, directing pressure to either side of the spinous process.
Figure 2.
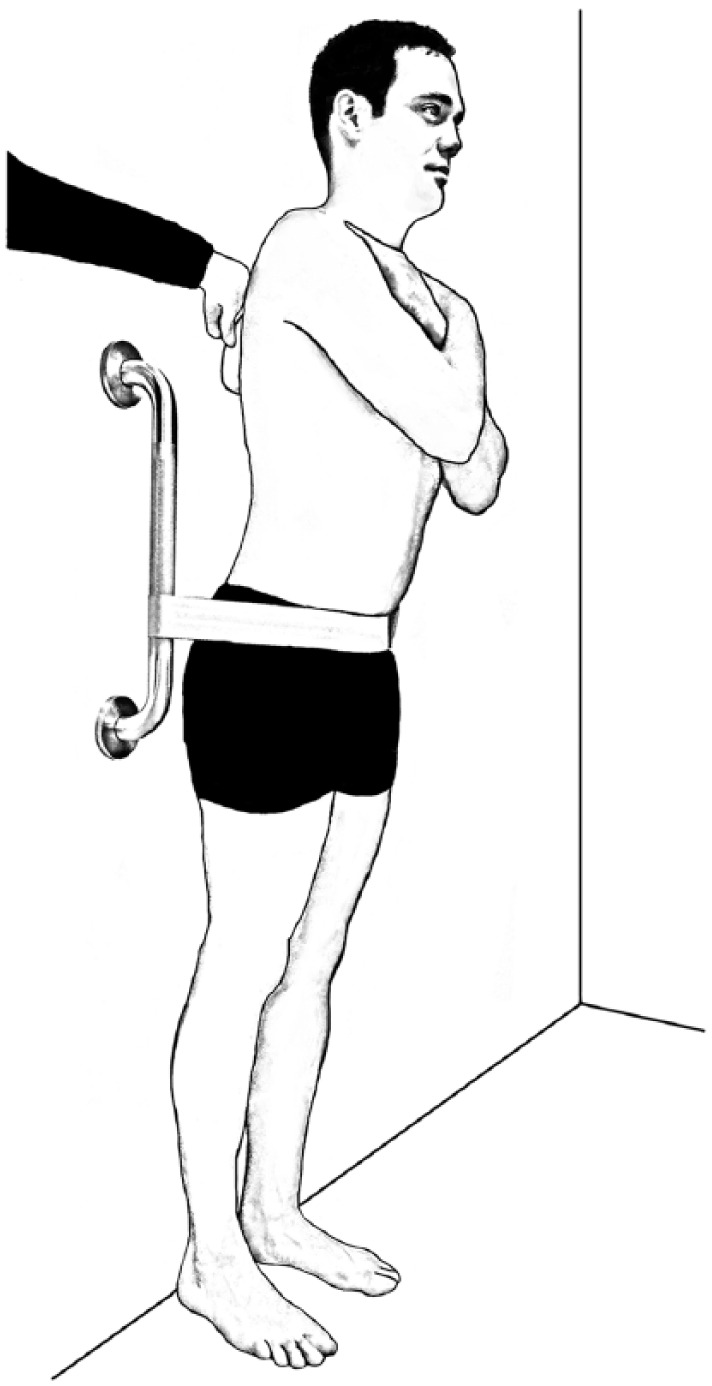
Participant and dynamometer positioning for the novel back extensor strength test, utilising a hand-held dynamometer for maximal isometric back extensor strength measurement.
Preliminary instructions were provided, and the examiner demonstrated correct positioning and technique to each participant. Verbal instructions followed a standardised script designed to optimise participant motivation to exert maximal effort, as follows: ‘We are going to do a test of your back muscle strength with this device called a dynamometer. You need to push back as hard as you can with your shoulders into the wall’. Additional verbal encouragement was provided during each trial whereby the investigator instructed the participant to ‘push, push, push, and relax’. A single familiarisation trial was performed, followed by 3 × 5-s maximal isometric trials, separated by 30-s rest to reduce potential fatigue, as recommended by others.28 If it appeared that maximal effort was not provided or instructions were not followed, the trial was repeated. Peak back extensor force (kg) was recorded for each successful trial. To avoid observer bias, a second investigator was engaged to record the force of each successful attempt, without informing the tester or participant of the outcome. The dynamometer was zeroed before each trial.
Lumbar spine BMD
BMD, bone mineral content (BMC), and area of the second to fourth lumbar vertebrae were examined with dual-energy X-ray absorptiometry (DXA; XR-800, Norland, Cooper Surgical, USA) using standard manufacturer procedures and host software for analysis. The index of bone structural strength (IBS) was also calculated according to previously described formulae.29,30 One investigator conducted and analysed all scans. Daily scans of the manufacturer-provided calibration wedge and spine phantom were undertaken to maintain quality control. The coefficient of variation for lumbar spine BMD measures in our lab is 0.8%.
Statistical analyses
Descriptive statistics of participant characteristics were presented as means ± standard deviations. Peak values from the novel HHD task were validated against peak isokinetic dynamometry-derived back extensor torque values with a two-tailed Pearson correlation (r) with 95% confidence intervals (95% CIs). More traditional methods of validation, such as limits of agreement, were not appropriate in this case due to the difference in units of measurement between the devices. By convention, an r value between 0.7 and 0.9 was taken to indicate a strong correlation, 0.5–0.7 a moderate correlation, and 0.3–0.5 a low correlation.31 In keeping with recommendations to assess consistency and reproducibility of measurement methods,32 ICCs were calculated using a 1-way random model to evaluate short- and long-term intrarater reliability. ICCs are reported with corresponding 95% CIs. Short-term reliability was examined using the Bland–Altman method,33 calculating 95% limits of agreement and mean bias between the second and third trials at S1. Heteroscedasticity was examined by plotting the absolute differences in repeated measures against the paired measurement means and running a Pearson correlation. Minimum detectable difference at the 95% confidence level (MDD95) was calculated as: standard error of the mean × 1.96 × √2. Back extensor strength measured with the novel task was classified as low, medium, or high strength categories for S1 and S2, then sensitivity analyses were undertaken. Linear regression was used to examine the ability of peak back extensor strength from our novel test to predict indices of lumbar spine bone mass and strength. Statistical significance was determined at p < 0.05. All statistical analyses were performed using SPSS for Windows, version 23.0 (IBM, Chicago, IL, USA).
Results
Participant characteristics
A total of 54 individuals volunteered to participate. Two were excluded due to late disclosure of musculoskeletal conditions, and two female participants were unable to attend S2 due to illnesses unrelated to the study on the day. Data from excluded participants were not included in the final analysis. Thus, a total of 52 healthy participants aged 21–80 years undertook the first session (26 men, 26 women), 50 of whom returned for testing at follow-up (26 men, 24 women) (Table 1). DXA-derived lumbar spine T-scores ranged from −2.7 to 3.1, with 10 participants in the osteopenic range (T-score between −1.0 and −2.5) and one participant in the osteoporotic range (T-score −2.5 and below) according to World Health Organisation diagnostic criteria. Peak back extensor strength obtained with the novel protocol at S1 and S2 was 53.7 ± 19.4 kg and 58.8 ± 19.3 kg, respectively. Peak back extensor torque measured during S1 (n = 52) and S2 (n = 50) with the Biodex was 175.2 ± 67.3 N m and 179.1 ± 63.3 N m, respectively. Both reflect a mild learning effect.
Table 1.
Participant characteristics (mean ± standard deviation).
| Characteristic | Men (n = 26) |
Women (n = 26) | Combined (n = 52) |
|---|---|---|---|
| Age (years) | 47.7 ± 23.3 | 45.5 ± 17.7 | 46.5 ± 20.5 |
| Height (m) | 1.79 ± 0.06 | 1.64 ± 0.07 | 1.71 ± 0.10 |
| Weight (kg) | 84.4 ± 7.7 | 66.7 ± 13.3 | 75.6 ± 14.0 |
| BMI (kg/m2) | 26.5 ± 2.4 | 24.8 ± 4.5 | 25.6 ± 3.7 |
| Lumbar spine | |||
| BMD (g/cm2) | 1.221 ± 0.174 | 1.033 ± 0.184 | 1.130 ± 0.201 |
| BMC (g) | 65.69 ± 12.40 | 47.24 ± 10.39 | 56.84 ± 14.69 |
| Area (cm2) | 53.65 ± 5.19 | 45.56 ± 3.81 | 49.77 ± 6.10 |
| IBS (g2/cm4) | 1.93 ± 0.56 | 1.40 ± 0.52 | 1.68 ± 0.60 |
| BMAD (g/cm3) | 0.167 ± 0.023 | 0.153 ± 0.026 | 0.160 ± 0.026 |
BMAD: bone mineral apparent density; BMC: bone mineral content; BMD: bone mineral density; BMI: body mass index; IBS: index of bone structural strength.
Validity
Peak back extensor strength measured with the novel HHD task showed a strong positive association with Biodex-derived peak torque for both S1 (r = 0.824 (95% CI, 0.708–0.894), p < 0.001) and S2 (r = 0.853 (95% CI, 0.750–0.913), p < 0.001).
Reliability
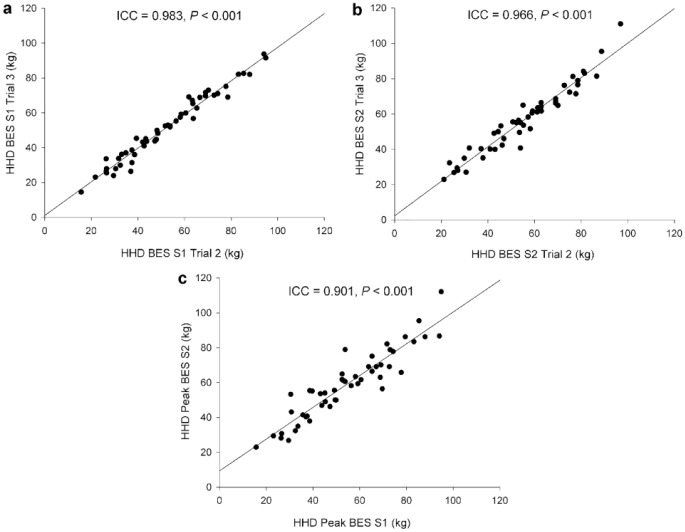
Short-term reliability (trial 2 vs trial 3) for our novel HHD test was excellent, showing strong positive associations between repeated measures for S1 (ICC = 0.983 (95% CI, 0.971–0.990), p < 0.001) (Figure 3(a)) and S2 (ICC = 0.966 (95% CI, 0.940–0.980), p < 0.001) (Figure 3(b)). MDD95 for S1 (trial 2 vs trial 3) was 7.14 kg (relative MDD95 13.59%). Long-term reliability (S1 vs S2) of peak back extensor strength with the novel HHD test was also excellent (ICC = 0.901 (95% CI, 0.833–0.943), p < 0.001) (Figure 3(c)). Intersession MDD95 (S1 vs S2) was 16.92 kg (relative MDD95 31.51%). Limits of agreement for short-term repeated measures with the novel HHD were −6.63 to 7.70 kg with a mean bias of +0.71 kg (Figure 4). Homoscedasticity was confirmed by the lack of relationship between absolute differences in back extensor strength and the mean of paired measures (r = 0.031, p = 0.826).
Figure 3.
Repeated measures of maximal isometric back extensor muscle strength with the novel hand-held dynamometer protocol for (a) short-term reliability at session 1 (n = 52), (b) short-term reliability at session 2 (n = 50), and (c) long-term reliability (n = 50).
BES: back extensor strength; HHD: hand-held dynamometer; S1: session 1; S2: session 2.
Figure 4.
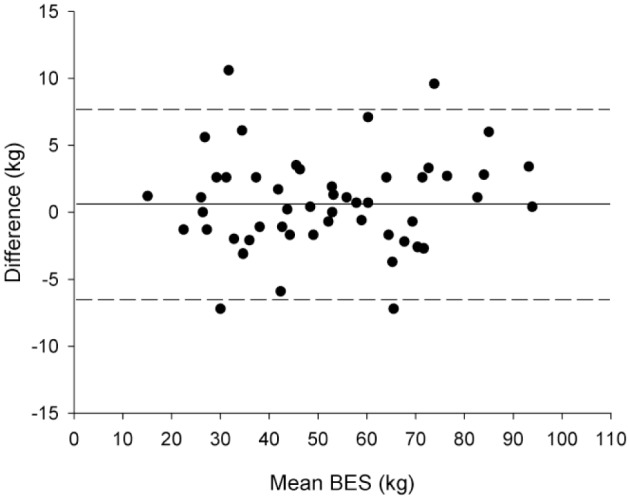
Bland–Altman plot illustrating mean bias (solid line) and limits of agreement (upper and lower dashed lines) for short-term repeated back extensor strength measures with the novel hand-held dynamometer task (n = 52).
BES: back extensor strength.
Short-term reliability (trial 2 vs trial 3) of strength measured using the isokinetic dynamometry was also excellent for S1 (ICC = 0.976 (95% CI, 0.959–0.986), p < 0.001) and S2 (ICC = 0.978 (95% CI, 0.961–0.987), p < 0.001). Long-term reliability (S1 vs S2) of peak strength from isokinetic dynamometry was also acceptable (ICC = 0.953 (95% CI, 0.919–0.973), p < 0.001).
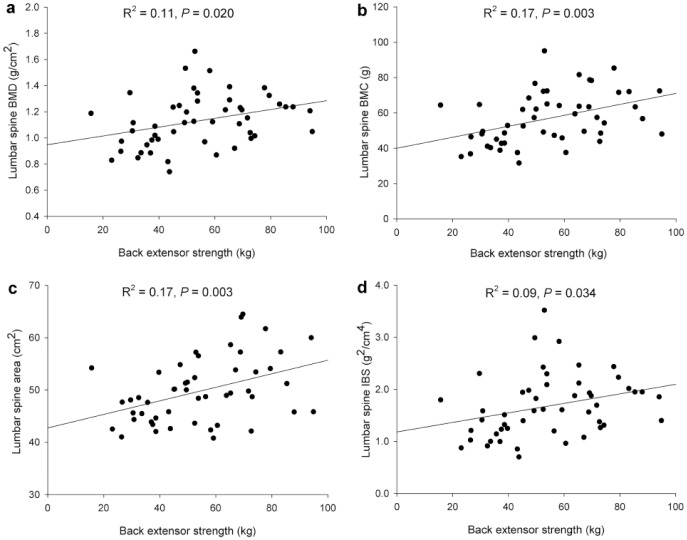
Relationship between back extensor strength and bone measures
Peak isometric strength obtained with our novel HHD test was predictive of variance in lumbar spine BMD (R2 = 0.11, p = 0.020), BMC (R2 = 0.17, p = 0.003), area (R2 = 0.17, p = 0.003), and IBS (R2 = 0.09, p = 0.034) (Figure 5).
Figure 5.
Relationship between maximal isometric back extensor strength measured with the novel hand-held dynamometer method at session 1 and indices of lumbar spine bone mass and strength: (a) lumbar spine bone mineral density (n = 50), (b) lumbar spine bone mineral content (n = 50), (c) lumbar spine area (n = 50), and (d) lumbar spine index of bone structural strength (n = 50).
BMC: bone mineral content; BMD: bone mineral density: IBS, index of bone structural strength.
Discussion
The aims of this study were to develop and test the convergent validity and reliability of a novel, simple, clinically amenable test of back extensor strength against isokinetic dynamometry-derived muscle force and to determine if isometric back extensor strength derived from our novel test was predictive of indices of lumbar spine strength. We found our novel method to be highly correlated with peak torque measures from the isokinetic dynamometry, demonstrating high measurement validity. The novel protocol also displayed excellent short- and long-term test–retest reliability. Finally, we observed that peak back extensor strength measured from the novel HHD task was predictive of indices of lumbar spine strength. Findings suggest that the assessment of isometric strength with our simple, novel HHD task produces valid and reliable outcomes and are of clinical relevance to bone health.
Although previously published reviews34,35 have indicated a level of inter-instrument validity between hand-held and isokinetic muscle strength testing for upper and lower limb muscles, no study has established validity for the trunk extensors. To our knowledge, our work is the first to investigate the validity of maximal isometric extensor muscle strength measures from a HHD against the reference standard.
Previous reports of back extensor strength measurement reliability
Direct comparison of previously reported results of maximal isometric strength testing is limited by incomplete protocol descriptions and heterogeneous methodology. A small number of studies have examined isometric strength across different populations using HHD devices.23,26 One examined the inter-rater reliability of maximal isometric back extensor strength using a variant of the prone Biering-Sørensen test.23 A total of 15 women and 24 men, from 22 to 57 years, volunteered to perform three trials separated by 30-s rest periods. The Biering-Sørensen test, however, has numerous shortcomings. When conducted with external examiner HHD fixation, performance is open-chain and highly dependent on examiner strength; examiner HHD fixation is also influenced by gender, lean body mass, and grip strength.36 Furthermore, performance of the Biering-Sørensen test is influenced by the mass of the upper extremities and torso, along with hip extensor activation, which introduces a marked source of inter-individual variation.15
External belt system fixation of the HHD improved test–retest reliability of the modified Biering-Sørensen test in a sample of 48 women with evidence of low-trauma vertebral fractures and diagnosed osteopenia.26 However, the tendency to extend the spine from the prone position has the potential to produce discomfort, limiting the ability to generate a true maximal isometric contraction for some. In fact, one participant was reportedly unable to undergo repeat testing due to exacerbation of back pain following the first session. Another was unable to raise their chest from the examination table due to muscle weakness, and one had to discontinue testing due to dyspnoea when prone.26 Indeed, an important disincentive for clinical testing is the risk of inducing pain.27 By contrast, our protocol involves closed-chain wall fixation, thereby eliminating examiner-based variability, is not influenced by upper body mass, is feasible for all but the most kyphotic individual, is not unduly tiring, and did not induce pain during or after treatment in our broad sample of apparently healthy individuals. Furthermore, the standing position of our novel test more closely mirrors common everyday activities than previous protocols.
In addition to the strong linear relationships observed between repeated measures, we detected a relatively small mean bias of +0.71 kg for repeated trials, and modest limits of agreement of −6.63 to 7.7 kg indicating a level of between-test variance that is not clinically significant. Both short- and long-term reliability results were excellent with ICCs between 0.901 and 0.983 for the novel test. In the absence of published data for back extensor strength, we note our results are comparable to those obtained in previous HHD reliability studies of maximal isometric knee extension strength in healthy young37 and older adults.38
Relationship to indices of lumbar spine bone strength
Cross-sectional studies in postmenopausal women have previously observed positive associations between BMD at the lumbar spine and supine isokinetic dynamometry-derived maximal isometric trunk extension strength (r = 0.14, p < 0.05)10 or seated maximal isometric trunk extension torque (r = 0.31, p < 0.05).39 Prone isometric back extensor strength has also been shown to be significantly lower in women with diagnosed osteoporosis than women of similar age with normal bone mass.40 In one group of healthy older participants, spine BMD was positively associated with isometric strength in men (r = 0.47, p < 0.01), but not women.13 Others have observed no relationship between trunk extensor muscle strength measured by isokinetic dynamometry and lumbar spine BMD in sedentary postmenopausal women.12
We observed a positive relationship between maximal isometric strength of the back extensor muscles and DXA-derived indices of lumbar spine bone strength. It is possible that the difference in findings reported in the aforementioned studies reflect variation in training and/or hormonal status of the study participants. We are the first to report an association between a mechanical index of vertebral bone strength (IBS) and maximal isometric back extensor strength in apparently healthy men and women aged 21–80 years.
Study limitations
Three limitations warrant discussion. First, when maximal contractions are requested, participant effort introduces an inherent element of measurement variability that is difficult to fully control.41 In order to reduce the influence of motivation on performance, we employed a single tester who gave uniform instructions and equivalent verbal encouragement to all participants. We also analysed the best of three efforts in order to record maximal performance on the day. Second, while participant numbers were adequate to examine questions of reliability and validity, a larger sample size may have improved the ability to detect potential relationships between muscle strength and parameters of lumbar spine strength. Nevertheless, our exploratory analysis of pooled male and female data detected significant, albeit modest, relationships across several bone strength parameters. Third, as participants were apparently healthy and ambulatory results may not apply to other populations. Further research is therefore required to determine whether the use of the novel testing protocol is feasible for individuals with musculoskeletal injury. It is intended that ongoing studies of larger samples to further clarify the relationship between isometric back extensor muscle strength and bone strength, determine the influence of gender, and develop reference ranges for a healthy population will be performed.
Conclusion
This report describes a simple, novel test of back extensor strength developed for the clinical and research setting. The test exhibited convergent validity against back extensor strength determined using the isokinetic dynamometer and high short- and long-term reliability in men and women across a broad age range. The benefits of the newly developed strength test include the relative simplicity, portability, availability, safety, and low cost of the HHD devices in comparison with isokinetic dynamometers. Findings show that in our sample of apparently healthy men and women, our novel test is, therefore, a viable and practical alternative to the previously utilised isometric back muscle strength measures. Furthermore, that back extensor strength measured with our novel HHD test is positively associated with indices of lumbar spine bone strength suggests clinical and research relevance.
Acknowledgments
The authors thank the participants who volunteered for the study.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from Griffith University Human Research Ethics Committee (Protocol number AHS/39/14/HREC).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from all participants before the study.
References
- 1. Henry MJ, Pasco JA, Nicholson GC, et al. Prevalence of osteoporosis in Australian men and women: Geelong Osteoporosis Study. Med J Aust 2011; 195: 321–322. [DOI] [PubMed] [Google Scholar]
- 2. Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res 2014; 29: 2520–2526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ström O, Borgström F, Kanis JA, et al. Osteoporosis: burden, health care provision and opportunities in the EU. Arch Osteoporos 2011; 6: 59–155. [DOI] [PubMed] [Google Scholar]
- 4. Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 2006; 17: 1726–1733. [DOI] [PubMed] [Google Scholar]
- 5. Klotzbuecher CM, Ross PD, Landsman PB, et al. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 2000; 15: 721–739. [DOI] [PubMed] [Google Scholar]
- 6. Sinaki M, Brey RH, Hughes CA, et al. Balance disorder and increased risk of falls in osteoporosis and kyphosis: significance of kyphotic posture and muscle strength. Osteoporos Int 2005; 16: 1004–1010. [DOI] [PubMed] [Google Scholar]
- 7. Sinaki M, Brey RH, Hughes CA, et al. Significant reduction in risk of falls and back pain in osteoporotic-kyphotic women through a Spinal Proprioceptive Extension Exercise Dynamic (SPEED) program. Mayo Clin Proc 2005; 80: 849–855. [DOI] [PubMed] [Google Scholar]
- 8. Granacher U, Gollhofer A, Hortobágyi T, et al. The importance of trunk muscle strength for balance, functional performance, and fall prevention in seniors: a systematic review. Sports Med 2013; 43: 627–641. [DOI] [PubMed] [Google Scholar]
- 9. Granacher U, Lacroix A, Muehlbauer T, et al. Effects of core instability strength training on trunk muscle strength, spinal mobility, dynamic balance and functional mobility in older adults. Gerontology 2013; 59: 105–113. [DOI] [PubMed] [Google Scholar]
- 10. Zhou Z, Zheng L, Wei D, et al. Muscular strength measurements indicate bone mineral density loss in postmenopausal women. Clin Interv Aging 2013; 8: 1451–1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Calmels P, Vico L, Alexandre C, et al. Cross-sectional study of muscle strength and bone mineral density in a population of 106 women between the ages of 44 and 87 years: relationship with age and menopause. Eur J Appl Physiol Occup Physiol 1995; 70: 180–186. [DOI] [PubMed] [Google Scholar]
- 12. Bayramoğlu M, Sözay S, Karataş M, et al. Relationships between muscle strength and bone mineral density of three body regions in sedentary postmenopausal women. Rheumatol Int 2005; 25: 513–517. [DOI] [PubMed] [Google Scholar]
- 13. Bevier WC, Wiswell RA, Pyka G, et al. Relationship of body composition, muscle strength, and aerobic capacity to bone mineral density in older men and women. J Bone Miner Res 1989; 4: 421–432. [DOI] [PubMed] [Google Scholar]
- 14. Guilhem G, Giroux C, Couturier A, et al. Validity of trunk extensor and flexor torque measurements using isokinetic dynamometry. J Electromyogr Kinesiol 2014; 24: 986–993. [DOI] [PubMed] [Google Scholar]
- 15. Gruther W, Wick F, Paul B, et al. Diagnostic accuracy and reliability of muscle strength and endurance measurements in patients with chronic low back pain. J Rehabil Med 2009; 41: 613–619. [DOI] [PubMed] [Google Scholar]
- 16. Hayes K, Walton JR, Szomor ZL, et al. Reliability of 3 methods for assessing shoulder strength. J Shoulder Elbow Surg 2002; 11: 33–39. [DOI] [PubMed] [Google Scholar]
- 17. Kolber MJ, Beekhuizen K, Cheng M-SS, et al. The reliability of hand-held dynamometry in measuring isometric strength of the shoulder internal and external rotator musculature using a stabilization device. Physiother Theory Pract 2007; 23: 119–124. [DOI] [PubMed] [Google Scholar]
- 18. Leggin BG, Neuman RM, Iannotti JP, et al. Intrarater and interrater reliability of three isometric dynamometers in assessing shoulder strength. J Shoulder Elbow Surg 1996; 5: 18–24. [DOI] [PubMed] [Google Scholar]
- 19. Arnold CM, Warkentin KD, Chilibeck PD, et al. The reliability and validity of handheld dynamometry for the measurement of lower-extremity muscle strength in older adults. J Strength Cond Res 2010; 24: 815–824. [DOI] [PubMed] [Google Scholar]
- 20. Bohannon RW, Kindig J, Sabo G, et al. Isometric knee extension force measured using a handheld dynamometer with and without belt-stabilization. Physiother Theory Pract 2012; 28: 562–568. [DOI] [PubMed] [Google Scholar]
- 21. Martin H, Yule V, Syddall H, et al. Is hand-held dynamometry useful for the measurement of quadriceps strength in older people? A comparison with the gold standard Biodex dynamometry. Gerontology 2006; 52: 154–159. [DOI] [PubMed] [Google Scholar]
- 22. Bohannon RW. Hand-held dynamometry: a practicable alternative for obtaining objective measures of muscle strength. Isokinet Exerc Sci 2012; 20: 301–315. [Google Scholar]
- 23. Moreland J, Finch E, Stratford P, et al. Interrater reliability of six tests of trunk muscle function and endurance. J Orthop Sports Phys Ther 1997; 26: 200–208. [DOI] [PubMed] [Google Scholar]
- 24. Biering-Sørensen F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine 1984; 9: 106–119. [DOI] [PubMed] [Google Scholar]
- 25. Evans KA, Refshauge KM, Adams R. Trunk muscle endurance tests: reliability, and gender differences in athletes. J Sci Med Sport 2007; 10: 447–455. [DOI] [PubMed] [Google Scholar]
- 26. Valentin G, Maribo T. Hand-held dynamometry fixated with a tripod is reliable for assessment of back extensor strength in women with osteoporosis. Osteoporos Int 2014; 25: 2143–2149. [DOI] [PubMed] [Google Scholar]
- 27. Ito T, Shirado O, Suzuki H, et al. Lumbar trunk muscle endurance testing: an inexpensive alternative to a machine for evaluation. Arch Phys Med Rehabil 1996; 77: 75–79. [DOI] [PubMed] [Google Scholar]
- 28. Katoh M, Yamasaki H. Test-retest reliability of isometric leg muscle strength measurements made using a hand-held dynamometer restrained by a belt: comparisons during and between sessions. J Phys Ther Sci 2009; 21: 239–243. [Google Scholar]
- 29. Sievänen H, Kannus P, Nieminen V, et al. Estimation of various mechanical characteristics of human bones using dual energy x-ray absorptiometry: methodology and precision. Bone 1996; 18: S17–S27. [DOI] [PubMed] [Google Scholar]
- 30. Bachrach LK, Marcus R, Ott SM, et al. Bone mineral, histomorphometry, and body composition in adults with growth hormone receptor deficiency. J Bone Miner Res 1998; 13: 415–421. [DOI] [PubMed] [Google Scholar]
- 31. Mukaka MM. Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med J 2012; 24: 69–71. [PMC free article] [PubMed] [Google Scholar]
- 32. Eliasziw M, Young SL, Woodbury MG, et al. Statistical methodology for the concurrent assessment of interrater and intrarater reliability: using goniometric measurements as an example. Phys Ther 1994; 74: 777–788. [DOI] [PubMed] [Google Scholar]
- 33. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 327: 307–310. [PubMed] [Google Scholar]
- 34. Kolber MJ, Cleland JA. Strength testing using hand-held dynamometry. Phys Ther Rev 2005; 10: 99–112. [Google Scholar]
- 35. Stark T, Walker B, Phillips JK, et al. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. PM R 2011; 3: 472–479. [DOI] [PubMed] [Google Scholar]
- 36. Wadsworth CT, Nielsen DH, Corcoran DS, et al. Interrater reliability of hand-held dynamometry: effects of rater gender, body weight, and grip strength. J Orthop Sports Phys Ther 1992; 16: 74–81. [DOI] [PubMed] [Google Scholar]
- 37. Katoh M. Reliability of isometric knee extension muscle strength measurements made by a hand-held dynamometer and a belt: a comparison of two types of device. J Phys Ther Sci 2015; 27: 851–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Katoh M, Isozaki K. Reliability of isometric knee extension muscle strength measurements of healthy elderly subjects made with a hand-held dynamometer and a belt. J Phys Ther Sci 2014; 26: 1855–1859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Halle JS, Smidt GL, O’Dwyer KD, et al. Relationship between trunk muscle torque and bone mineral content of the lumbar spine and hip in healthy postmenopausal women. Phys Ther 1990; 70: 690–699. [DOI] [PubMed] [Google Scholar]
- 40. Sinaki M, Khosla S, Limburg PJ, et al. Muscle strength in osteoporotic versus normal women. Osteoporos Int 1993; 3: 8–12. [DOI] [PubMed] [Google Scholar]
- 41. Wang C-Y, Olson SL, Protas EJ. Test-retest strength reliability: hand-held dynamometry in community-dwelling elderly fallers. Arch Phys Med Rehabil 2002; 83: 811–815. [DOI] [PubMed] [Google Scholar]