Abstract
Introduction
This meta-analysis aimed to characterize the nature and magnitude of amyloid (Aβ)-related cognitive impairment and decline in cognitively normal (CN) older individuals.
Method
MEDLINE Ovid was searched from 2012 to June 2016 for studies reporting relationships between cerebrospinal fluid or positron emission tomography (PET) Aβ levels and cognitive impairment (cross-sectional) and decline (longitudinal) in CN older adults. Neuropsychological data were classified into domains of episodic memory, executive function, working memory, processing speed, visuospatial function, semantic memory, and global cognition. Type of Aβ measure, how Aβ burden was analyzed, inclusion of control variables, and clinical criteria used to exclude participants, were considered as moderators. Random-effects models were used for analyses with effect sizes expressed as Cohen's d.
Results
A total of 38 studies met inclusion criteria contributing 30 cross-sectional (N = 5005) and 14 longitudinal (N = 2584) samples. Aβ-related cognitive impairment was observed for global cognition (d = 0.32), visuospatial function (d = 0.25), processing speed (d = 0.18), episodic memory, and executive function (both d's = 0.15), with decline observed for global cognition (d = 0.30), semantic memory (d = 0.28), visuospatial function (d = 0.25), and episodic memory (d = 0.24). Aβ-related impairment was moderated by age, amyloid measure, type of analysis, and inclusion of control variables and decline moderated by amyloid measure, type of analysis, inclusion of control variables, and exclusion criteria used.
Discussion
CN older adults with high Aβ show a small general cognitive impairment and small to moderate decline in episodic memory, visuospatial function, semantic memory, and global cognition.
Keywords: Cognition, Amyloid-beta, Impairment, Decline, Meta-analysis, Preclinical Alzheimer's disease
1. Introduction
There is now consensus that in cognitively normal (CN) older adults, abnormal levels of amyloid-beta (Aβ+) indicates that the pathophysiological process of Alzheimer's disease (AD) has begun, although it may still be up to 20 years before these individuals meet clinical criteria for dementia [1], [2], [3], [4]. Neuroimaging and fluid biomarkers allow for in vivo measurement of Aβ burden in older individuals using positron emission tomography (PET) and cerebrospinal fluid (CSF) sampling, respectively [5], [6]. Studies using these techniques have shown that Aβ burden increases with age, with approximately 10%–20% of CN older adults aged 60–70 years, 20%–30% of those aged 70–80 years, and 30%–40% of those aged 80–90 years being classified as Aβ+ [4], [7], [8]. Despite their CN classification, prospective studies indicate that cognitive decline is faster and progression to a clinical diagnosis of mild cognitive impairment (MCI) or AD more rapid, in those who are Aβ+ compared to matched CN adults with low Aβ levels (Aβ−) [2], [3]. Characterizing preclinical AD is therefore important for understanding the pathogenesis of AD.
Although PET Aβ imaging or CSF sampling identifies reliably the presence of AD pathology in individuals with no overt symptoms, these procedures are expensive, invasive, and must occur in specialized medical centers. Ideally, sensitive and cost-effective clinical measures could be used to identify CN adults who should be referred for these more expensive and invasive testing procedures. Neuropsychological assessment may be useful in this regard, where the presence of a subtle but specific profile of cognitive dysfunction could indicate that Aβ+ would be classified on CSF sampling or PET imaging. However, to date, there is no agreement on what constitutes subtle cognitive decline among individuals with Aβ+. Evidence in support of a cognitive profile indicative of Aβ+ comes from neuropsychological studies that use two types of experimental designs. First are studies that define Aβ+-related cognitive impairment on the basis of the comparison of performance on batteries of neuropsychological tests between Aβ+ CN older adults and Aβ− CN older adults at a single assessment. Such studies generally report only small and statistically nonsignificant differences in neuropsychological test performance between Aβ− and Aβ+ CN older adults [9], [10], [11], [12], [13]. Second are studies that define Aβ+-related cognitive decline by evaluating changes in performance on neuropsychological test batteries over time between Aβ+ and Aβ− CN older adults. Studies using this approach have consistently found evidence of Aβ+-related decline on measures of episodic memory, executive function, processing speed, visuospatial function, and language (e.g., [9], [11], [14], [15], [16], [17], [18], [19], [20], [21]). However, although individual studies have identified areas of cognitive impairment and decline associated with Aβ+, there is substantial variation between these studies in terms of the sample sizes enrolled, the domains of cognitive function assessed, the specific neuropsychological or cognitive tests used to measure these domains, and the statistical techniques used to compare Aβ+ and Aβ− groups. Furthermore, in many studies, conclusions about the effects of Aβ+ on cognition have been based only on the presence or absence of statistical significance. Consequently, small but important Aβ+-related effects may have been missed when sample sizes did not provide adequate statistical power to render such differences statistically significant. Meta-analyses of the existing literature on Aβ+-related cognitive impairment, and decline could therefore provide an effective method for overcoming the different limitations of individual studies to provide reliable estimates of Aβ+-related cognitive impairment and decline in preclinical AD.
To date, one meta-analysis evaluated this question and concluded that associations with Aβ burden were strongest for episodic memory (e.g., r = −0.12; Hedden et al., 2013 [16]). Additionally, when combining estimates across studies that measured Aβ using CSF, PET, plasma, and histopathologic methods, lower performance in executive function was also related significantly (r = 0.08) to Aβ burden. Post hoc analyses indicated that estimates of Aβ+-related cognitive dysfunction were unaffected by the experimental design used, the method of determining Aβ levels, or whether demographic or clinical variables were controlled statistically. Although this initial meta-analysis provides a good basis for understanding the effects of Aβ on cognition in CN older adults, its conclusions are limited because a large number of studies investigating relationships between Aβ+ and neuropsychological test performance have been conducted since its publication. Second, the number of studies using either cross-sectional or longitudinal designs is now sufficient to consider estimates of cognitive impairment and cognitive decline separately. Third, a broader sample of cognitive domains is now available for inclusion in meta-analyses. Finally, samples in studies using longitudinal designs have been followed for longer periods. As such, an updated meta-analysis of this literature is needed to understand the relation between Aβ and cognitive impairment and decline in preclinical AD. The aim of this study was therefore to systematically review the literature on the nature and magnitude of Aβ+-related cognitive impairment and decline in older adults who do not meet clinical criteria for MCI or dementia.
2. Methods
2.1. Study selection
2.1.1. Inclusion/exclusion criteria
Inclusion criteria for the meta-analyses were that (a) the study must include a sample of adults with an average age ≥60 years who did not meet clinical criteria for MCI or dementia and who had undergone assessment with standardized neuropsychological tests; (b) for each participant, Aβ levels were determined using PET or CSF sampling; and (c) studies must have provided sufficient information to allow for the computation of effect sizes.
Studies were excluded from the meta-analysis if they were one of a series of publications from the same specific cohort where, over time, sample sizes or the length of follow-up had increased. For studies meeting this criterion, data for the meta-analyses were taken from that study which was the most recent and which had the largest sample. If possible, data for any cognitive domain not reported in the chosen publication were derived from another publication from the same cohort with the next largest sample where relevant data were presented, so as to ensure as many cognitive domains as possible were represented for each cohort. Second, studies were excluded if neuropsychological data or clinical data had been used to classify CN adults “progressors/decliners” or “stable/nondecliners” independent of Aβ classification. Finally, for studies that reported results from both PET and CSF sampling, we focused on PET results as indicators of Aβ levels to maintain consistency across studies.
2.2. Systematic review methods
Supplementary Fig. A summarizes the outcome of the systematic review process. Initially, all studies included in the meta-analysis of Hedden et al. (2013) [16] were screened via title and abstract, to determine relevance to inclusion and exclusion criteria of the current meta-analysis. Fifteen articles were excluded at this stage. A systematic electronic database search was then conducted on Medline Ovid, on the 8th of June 2016, using the subject terms for amyloid, older adults and AD, and cognition that were used in the meta-analysis by Hedden et al. (2013) [16]. The terms are described below:
-
1.
(amyloid) AND (“Pittsburgh Compound B” OR PIB OR florbetapir OR AV-45 OR florbetaben OR flutemetamol OR PET) OR (CSF)
-
2.
(normal OR nondemented OR aging OR older OR Alzheimer's OR dementia OR “cognitive impairment” OR MCI)
-
3.
(cognitive OR cognition OR memory OR executive OR speed OR visuospatial OR semantic)
At this stage, 501 articles were identified to be screened via title and abstract. After removal of duplicates and review articles, 362 articles were screened via title and abstract, with 335 being excluded at this stage (Supplementary Fig. A). After this, full-text screening began of the articles identified from the Hedden et al. analysis and from those identified in the electronic search. Reference lists of articles were also screened for key citations, and newly published articles were screened for relevance. Fifty studies were excluded at this stage (see Supplementary Fig. A for details), leaving 69 studies meeting the full criteria. The largest samples from ongoing observational studies were chosen to represent the data for cognitive domains from that cohort. This process was completed separately for studies using cross-sectional or longitudinal designs. At completion, 38 studies met inclusion/exclusion criteria, consisting of 30 that used cross-sectional designs and 14 that used longitudinal designs.
2.3. Classification of outcome measures
For each study, performance data from neuropsychological tests were identified and organized according to the main cognitive domain measured by that test according to reference frameworks from previous meta-analyses of cognition [16], [22], [23] and standard neuropsychological compendia [24]. The cognitive domains used and the tests classified into each of those domains are summarized in Supplementary Table A.
2.4. Statistical analysis
Separate analyses were conducted for studies using cross-sectional and longitudinal designs using Comprehensive Meta-Analysis, version 3.3 software (Biostat, NJ). All results are reported using a random-effects model. Effect sizes were calculated using reported statistics such as means and standard deviations (Cohen's d) and results from analyses such as t tests, correlations, regressions (r), and linear mixed-effects models. If standard error was reported in a study, this was converted to standard deviation before the calculation of effect sizes. For each neuropsychological test or cognitive domain composite score, the sign of effect sizes was adjusted so that negative effect sizes reflected greater Aβ+-related impairment or decline. For studies that used more than one neuropsychological test to measure the same cognitive domain, effect sizes were averaged. All effects were weighted using inverse variance weighting based on sample size. All effect sizes were transformed into Cohen's d, and the magnitudes were classified as small, medium, or large according to Cohen (1992) [25]. A more lenient criterion was used to assess statistical significance of heterogeneity (P < .10) due to the lack of statistical power of these tests [26]. Where statistically significant heterogeneity was identified, post hoc subgroup analyses were conducted to seek the source of this heterogeneity [27]. These analyses investigated the extent to which heterogeneity in estimated mean effect sizes arose from variance due to moderators such as: (a) the type of Aβ measure (PET or CSF); (b) whether Aβ burden was defined as a continuous or categorical measure; (c) whether the study had controlled statistically the effects of demographic or clinical covariates (e.g., age, education, and so forth); and (d) the clinical classification criteria used to exclude participants from CN samples (i.e. the criteria for prodromal AD or MCI used). Where group mean effect sizes were based on 10 or more samples and there was no evidence of heterogeneity, publication bias was assessed by visual inspection of funnel plots and the Egger test, with the significance level set at P < .10 [28], [29]. This was done to assess whether the effect sizes of individual studies were distributed symmetrically around the overall mean effect size for the cognitive domain, or whether study size biased the results in a particular direction.
3. Results
3.1. Meta-analysis of studies using cross-sectional designs to measure cognitive impairment
Study characteristics and individual effect sizes for studies that used cross-sectional designs are presented in Supplementary Table B. Estimates of effect sizes from cross-sectional studies were based on 30 samples providing 5005 participants with study samples ranging between 23 and 564 participants. Of these, 2524 were females (50%), 1304 carried at least one APOE ε4 allele (26%), with the average ages of the individual samples ranging from 60.5 to 79 years. Nineteen studies contributed data for episodic memory (n = 2886), 13 for executive function (n = 2281), 10 for working memory (n = 1598), 13 for processing speed (n = 2530), nine for visuospatial function (n = 1984), 13 for semantic memory (n = 2585), and eight for global cognition (n = 1746).
For the majority of studies, Aβ levels were determined using PET neuroimaging (87%) with over half (63%) classifying Aβ levels categorically (e.g., positive vs. negative or high vs. low). Demographic and clinical variables such as age, premorbid IQ, sex, education, and APOE ε4 were controlled statistically in 53% of studies. The two main clinical criteria used to exclude participants with MCI/prodromal AD were the Clinical Dementia Rating (CDR; [30]) scale total score of 0.5 (53%) and the Petersen criteria [31]. Four studies [32], [33], [34], [35] used alternative criteria, such as the Mattis Dementia Rating Scale ([36]), the Jak and Bondi method [37], [38], and a combination of CDR 0.5 and Petersen criteria. For 77% of studies, the average age of participants was under 75 years.
3.2. Mean domain specific effect sizes of cognitive impairment
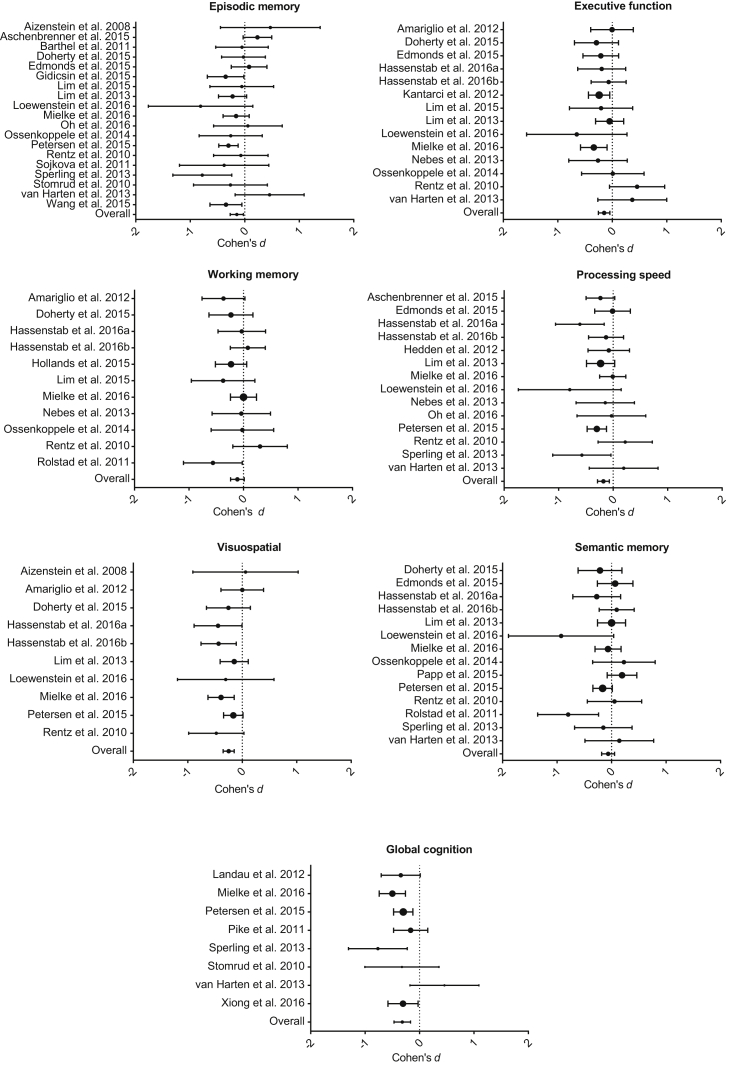
Mean effect sizes (Cohen's d) and associated 95% confidence intervals are listed in Table 1. Fig. 1 shows the forest plots for each cognitive domain with individual study effect sizes and 95% confidence intervals shown as well as the mean effect size for each domain. Worse performance in the presence of Aβ+ was evident for all cognitive domains, with the magnitude of effects, by convention, small. Aβ+-related cognitive impairment was statistically significant for the domains of global cognition, visuospatial function, processing speed, executive function, and episodic memory (Table 1). Stratifying the studies by participants' mean age showed that effect sizes for episodic memory and executive function were significant only for studies using samples aged 75 years and more (P's = .12 and .07 for the younger groups respectively), whereas visuospatial function was significant in the younger group only (P = .06 for older group). Statistically significant heterogeneity was detected for pooled estimates of effect sizes for episodic memory. No evidence of publication bias was found for the remaining domains.
Table 1.
Summary of pooled effect sizes and heterogeneity statistics from the meta-analyses
| Cognitive domain | n | Cross-sectional design |
n | Longitudinal design |
|---|---|---|---|---|
| Cohen's d (95% CI) | Cohen's d (95% CI) | |||
| Episodic memory | 2886 | −0.15 (−0.27 to −0.03)*† | 1781 | −0.24 (−0.44 to −0.03)*† |
| Executive function | 2281 | −0.15 (−0.26 to −0.05)** | 1074 | −0.04 (−0.31 to 0.22) |
| Working memory | 1598 | −0.11 (−0.24 to 0.01) | 740 | −0.26 (−0.65 to −0.13)† |
| Processing speed | 2530 | −0.18 (−0.29 to −0.07)*** | 1568 | −0.18 (−0.38 to 0.02)† |
| Visuospatial | 1984 | −0.25 (−0.35 to −0.15)*** | 1243 | −0.25 (−0.42 to −0.09)** |
| Semantic memory | 2585 | −0.06 (−0.18 to 0.06) | 1653 | −0.28 (−0.42 to −0.15)*** |
| Global cognition | 1746 | −0.32 (−0.47 to −0.17)*** | 1396 | −0.30 (−0.48 to −0.11)**† |
NOTE. Cohen's d represents the standardized difference in means between the amyloid positive and amyloid negative groups, where greater impairment is represented by a negative effect.
*P < .05; **P < .01; ***P < .001.
significant heterogeneity P > .05.
Fig. 1.
Forest plots from the meta-analysis of studies with cross-sectional designs. Effect sizes are presented as Cohen's d with 95% confidence intervals. The dotted lines represent no effect of amyloid on cognition. Negative values represent greater impairment in performance in the presence of high Aβ. The size of the dots represents study weighting due to sample size.
3.3. Moderator effects on studies of cognitive impairment
Table 2 shows the results of the post hoc analyses for episodic memory, where significant heterogeneity was detected. Group mean effect sizes remained statistically significant when these accounted for data from studies that had used PET to measure Aβ levels, classified Aβ as categorical, and had controlled statistically for demographic or clinical variables.
Table 2.
Pooled effect sizes and 95% confidence intervals adjusted for moderator variables
| Cognitive domain | Cross-sectional |
|||
|---|---|---|---|---|
| Amyloid measure |
Type of amyloid analysis |
|||
| CSF | PET | Continuous | Categorical | |
| Episodic memory | −0.07 [−0.34, 0.20] | −0.17 [−0.31, −0.03]* | −0.11 [−0.33, 0.12] | −0.16 [−0.31, −0.02]* |
| Control variables |
Normal criteria |
|||
|---|---|---|---|---|
| Yes | No | CDR = 0 | Petersen | |
| −0.21 [−0.39, −0.03]* | −0.10 [−0.25, 0.06] | −0.16 [−0.36, 0.03] | −0.15 [−0.34, 0.05] | |
| Longitudinal |
||||
|---|---|---|---|---|
| Amyloid measure |
Type of amyloid analysis |
|||
| CSF | PET | Continuous | Categorical | |
| Episodic memory | — | −0.27 [−0.50, −0.02]* | −0.04 [−0.24, 0.16] | −0.37 [−0.55, −0.18]***† |
| Processing speed | — | — | −0.02 [−0.33, 0.29] | −0.28 [−0.52, −0.03]* |
| Global cognition | — | −0.31 [−0.51, −0.10]** | −0.16 [−0.37, 0.05] | −0.43 [−0.67, −0.19]*** |
| Control variables |
Normal criteria |
|||
|---|---|---|---|---|
| Yes | No | CDR = 0 | Petersen | |
| Episodic memory | −0.29 [−0.53, −0.05]* | −0.03 [−0.53, 0.48] | −0.28 [−0.59, 0.03] | −0.20 [−0.48, −0.07] |
| Processing speed | — | — | −0.18 [−0.49, 0.13] | −0.20 [−0.51, 0.11] |
| Global cognition | −0.31 [−0.51, −0.10]** | — | −0.38 [−0.68, −0.08]* | −0.25 [−0.57, 0.07] |
NOTE. Effect sizes presented are Cohen's d, with associated 95% Confidence Intervals. Blank spaces represent only one study available for moderator in the domain. Control variables included clinical and demographic variables that were included as covariates in the analyses used to calculate effect sizes.
* P< .05 ** P< .01 *** P< .001.
group difference P < .05.
3.4. Meta-analysis of studies using longitudinal designs to measure cognitive decline
Study characteristics and individual effect sizes from studies using longitudinal designs included in the analysis are shown in Supplementary Table C. Estimates of effects from studies using longitudinal designs were based on 14 samples providing 2584 participants, with total samples ranging from 38 to 464 CN older adults. The sample included 1295 females (50%), and 743 APOE ε4 carriers (29%), with the average age at baseline of samples ranging between 60.5 and 78.2 years. The length of follow-up for studies ranged between 18 months and 23 years, approximate average of 5 years. Nine studies contributed data for episodic memory (n = 1781), five for executive function (n = 1074), three for working memory (n = 740), six for processing speed (n = 1568), five for visuospatial function (n = 1243), seven for semantic memory (n = 1653), and seven for global cognition (n = 1396).
Aβ analysis was conducted via PET neuroimaging in all but one study, with 57% of studies using a categorical classification for Aβ+. Demographic and clinical variables such as baseline age and test scores, education, sex, IQ, and family history were modeled as covariates in 79% of the studies. Exclusion of participants with prodromal AD or MCI at the baseline assessment was again split between the CDR (57%) and Petersen criteria. Approximately 71% of studies used participants with average ages <75 years.
3.5. Mean domain specific effect sizes of cognitive decline
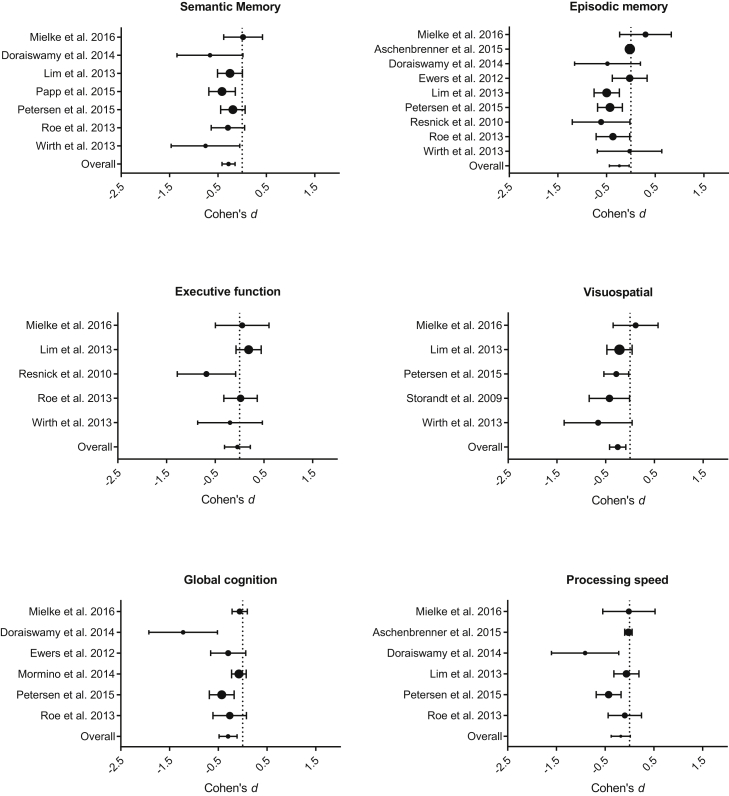
Mean effect sizes and associated 95% confidence intervals are shown in Table 1. Fig. 2 shows the forest plots representing the individual study effect sizes and 95% confidence intervals, as well as the mean effect size for each cognitive domain. Decreased performance in the presence of Aβ+ was evident for all cognitive domains with the magnitude of this decline small to moderate and statistically significant for episodic memory, visuospatial function, semantic memory, and global cognition. Stratifying the samples by participants' mean age did not change these results. Statistically significant heterogeneity was evident for the domains of episodic memory, working memory, processing speed, and global cognition (Table 1). Publication bias was unable to be assessed due to the small number of studies contributing to meta-analysis of studies using longitudinal designs [29].
Fig. 2.
Forest plots from the meta-analysis of studies with longitudinal designs. Effect sizes are presented as Cohen's d with 95% confidence intervals. The dotted lines represent no effect of amyloid on cognition. Negative values represent greater decline in performance in the presence of high Aβ. The domain of working memory is not included as only one study contributed data for this domain. The size of the dots represents study weighting due to sample size.
3.6. Moderator effects on studies of cognitive decline
Results of the moderator analysis of studies with longitudinal designs are listed in Table 2. Owing to the small number of studies available for the longitudinal meta-analysis, the moderator comparisons are limited; in many cases, only one study provided data for a particular subset (e.g., only one study used CSF [39]) and only three studies contributed effect sizes toward the working memory domain [40], [41], [42]; hence, post hoc analyses were conducted only where there were sufficient samples. For episodic memory, group mean effect sizes remained statistically significant when these accounted for data from studies that had classified Aβ as a categorical measure and had controlled statistically for the effects of demographic and clinical characteristics. For processing speed, effect sizes remained statistically significant when these accounted for data from studies that had classified Aβ as a categorical measure. For global cognition, group mean effect sizes remained statistically significant when these accounted for data from studies that had classified Aβ levels categorically, and had used the CDR criteria to exclude prodromal AD or MCI at baseline.
4. Discussion
The results of this meta-analysis indicate that, in CN older adults, reliable Aβ+ related cognitive impairment occurs in the domains of episodic memory, executive function, processing speed, visuospatial function, and global cognition. However, for each of these cognitive domains, impairment was by convention [25], small in magnitude with effect sizes ranging from d = 0.15 for episodic memory to d = 0.25 for visuospatial function. Interestingly, the largest effect size observed was for measures of global cognition, computed within studies by combining data across their neuropsychological tests measuring multiple cognitive domains. Nevertheless, even with data from all tests combined in this way, the magnitude of Aβ+-related impairment remained only small (d = 0.32). No statistically significant evidence of impairment was observed for the domains of working or semantic memory and in both cases, the magnitude of impairment was smaller than that observed for the other cognitive domains (d's < 0.12). As these estimates of cognitive impairment were based on data from 5005 subjects from 30 studies, we believe these effect sizes provide an accurate estimation of the nature and magnitude of cognitive impairment in Aβ+ CN older adults.
Aβ+-related cognitive decline was evident in the domains of episodic memory, semantic memory, visuospatial function, and global cognition, with the magnitude of decline in these cognitive domains ranging from d = 0.24 for episodic memory to d = 0.30 for global cognition. Again, the effect size for decline in global cognitive function was significant and small in magnitude (d = 0.30). No Aβ+-related decline was observed for working memory, processing speed, or executive function. Given the greater resources needed to conduct prospective studies, these estimates of cognitive decline in Aβ+ CN older adults were based on fewer data points than those for cognitive impairment. However, as data were obtained for 2584 subjects from 14 studies encompassing an average of approximately five years of follow-up that satisfied inclusion/exclusion criteria, therefore these estimates of cognitive decline in Aβ+ CN older adults are reliable. When considered together, data from both the cross-sectional and longitudinal meta-analyses suggest that in CN older adults, Aβ+ is associated with both subtle cognitive impairment and decline. There was no evidence for a specific profile of cognitive impairment associated with Aβ+. In fact, measures of global cognitive function, which typically combined multiple cognitive domains, provided the largest effect sizes. In contrast, analyses of longitudinal studies indicated that Aβ+ related cognitive decline manifests predominantly and moderately in episodic and semantic memory. While stratifying the samples by mean age moderated cognitive impairment in episodic memory and executive function, mean age did not influence the estimates of cognitive decline for any domain. These effects will be considered in turn.
4.1. Aβ+-related cognitive impairment
The results show that Aβ+ is associated with moderate but nonspecific levels of cognitive impairment in CN older adults. The pattern of neuropsychological impairments detected suggests that in CN older adults, Aβ+ was associated with small impairments across measures of episodic memory, executive function, processing speed, and visuospatial function. It was not associated with impairment in working memory or semantic fluency. This general decrease in attention, executive function, and memory, with relative sparing of verbal fluency is consistent with the observation that the Aβ+ related impairment with the greatest magnitude was for global cognition, a score which in most studies was computed by combining performance across all the neuropsychological tests used in that study. The presence of this subtle and general cognitive impairment in Aβ+ CN older adults indicates that even very early in the course of AD, increased deposition of Aβ is related to disrupted cognitive function, although this effect is small.
Estimates of Aβ+ cognitive impairment from this meta-analysis suggest that the neuropsychological tests used to date in studies of preclinical AD are unlikely to be useful for identifying those CN older adults who would have abnormal Aβ levels if they underwent PET or CSF assessment. For example, with a Cohen's d of 0.30 (as observed for global cognition), 88% of the scores for Aβ+ and Aβ− individuals would overlap [43]. Thus, there would be a 42% chance of picking an Aβ+ individual at random that would have a higher score on the task than a similarly chosen Aβ− individual. Clearly, the sensitivity of the neuropsychological tests analyzed here is insufficient to warrant their use in distinguishing Aβ+ CN older adults from Aβ− CN older adults. Zakzanis (2001) [44] suggested that the criteria for a useful clinical marker in neuropsychological disorders would be a Cohen's d of 3 or above. This corresponds to an overlap of just 13% and <2% chance of selecting at random an Aβ+ individual that would score higher on the task than a similarly chosen Aβ− individual. Therefore, while the results from our meta-analysis confirm that Aβ+ does manifest as cognitive impairment early in AD, the magnitude of this impairment is subtle and nonspecific and would therefore be unlikely to be useful clinically.
The analyses indicated heterogeneity between studies that provided estimates of episodic impairment in Aβ+ CN older adults. Post hoc analyses of this heterogeneity suggested it was due to methodological variation between studies. Indeed, the estimates of impairment in this domain increased when looking at subsets of studies based on moderator variables. The finding that studies using PET had greater memory impairment than those using CSF to measure Aβ might be because CSF Aβ42 reaches abnormal levels earlier than PiB-PET [45], and therefore, Aβ+ determined from PET occurs in those with more advanced disease. Similarly, the increased impairment in the subset of studies using CDR criteria could reflect the inclusion of individuals who would have otherwise been classified as MCI. Finally, the reduction of variance, or noise, through controlling for extraneous variables or using categorical classifications of Aβ could be why an increase in impairment was seen in these subsets of studies.
4.2. Aβ+-related cognitive decline
The results show that Aβ was associated with significant decline in the domains of episodic memory, semantic memory, visuospatial function, and global cognition. Although the magnitude of decline for each domain was small, the effect of Aβ extended beyond the domain of episodic memory, and this is important for understanding the nature of cognitive change in early AD. Unexpectedly, effect sizes for Aβ+-related decline in episodic memory were smaller than those in visuospatial function and semantic memory. Research from our group and others has continually identified decline in episodic memory as being central to clinical progression in early AD [18], [46], [47]. Furthermore, dysfunction in episodic memory has been associated with loss of hippocampal volume, in accord with models of the structural brain changes that occur early in AD [2], [48], [49], [50] and with brain-behavior models of episodic memory [51], [52]. The reliable decline observed here for semantic memory and visuospatial function is also consistent with the involvement of medial temporal lobe structures [53].
Consistent with the specificity of Aβ+-related cognitive decline to higher cognitive functions dependent on medial temporal lobe structures was the absence of any decline in processing speed. Neuropsychological models suggest that processing speed reflects lower order or more basic cognitive functions that subserve higher processes such as working memory, executive function, and episodic memory [54]. However, this raises an issue of why Aβ+ was not associated with decline in executive function, given this is dependent on the integrity of the frontal lobe [54]. One possible explanation for the absence of any decline in executive function is very early AD-related neuronal loss does not involve the prefrontal cortex [55], [56]. The lack of correlation between location of Aβ deposition and neuronal death has been noted in many pathologic studies (see review by Musiek & Holtzman [57]). In this context, the results of this meta-analysis suggest that early AD-related cognitive declines occur predominantly in domains that rely on the normal function of the hippocampus and entorhinal cortex, which are areas that are most sensitive to early neuronal death in AD [58]. Thus, in preclinical AD, despite the widespread deposition of Aβ [59], neuronal disruption and cognitive decline remain relatively specific. Although some neuropsychological studies have concluded that decline in executive function does occur in preclinical AD and can also predict clinical progression to MCI and AD [15], [60], the neuropsychological tests classified as measuring executive function have varied between studies. For example, some studies include measures of working memory [11], [61], [62] or tasks of verbal and semantic fluency [13], [15] as part of the domain of their executive function composite scores. Previous research suggests that a specific component of executive function, verbal switching, and inhibition is more sensitive to executive dysfunction before dementia than other measures, such as planning [63], [64]. In accord with previous meta-analyses and standard neuropsychological models, the current study classified tasks of semantic and verbal fluency as representing semantic memory, whereas working memory was classified as a domain separate from executive function. Thus, the definition of executive function used here reflected tests of planning, error monitoring, and inhibition. Therefore, should the data from the present study be considered in the context of a broader definition of executive function, one possible conclusion is that Aβ+-related decline in executive function in preclinical AD does not manifest in areas of inhibition, planning, error monitoring, or working memory but rather in semantic and phonemic fluency. This absence of any impairment in semantic and phonemic fluency from the analysis of cross-sectional designs reinforces the subtlety of the impairment and shows that repeated assessment is required for it to become evident.
The lower than expected estimates of Aβ+-related cognitive decline in episodic memory might have been due to the substantial heterogeneity between studies for measures of this domain (Table 1). First, given the centrality of memory dysfunction to early AD, all but one study measured episodic memory (i.e., [65]). This resulted in many more measures of episodic memory being included in the current meta-analysis than measures of other cognitive domains. Thus, there was also the potential for greater variation to be included in estimates of mean effect size. Methodologic differences between studies might also account for some of this heterogeneity. For example, estimates of decline in episodic memory were larger in the subgroups of studies that used PET imaging, categorical Aβ levels, statistically controlled for extraneous variables and in those which used the CDR criteria to exclude subjects. As discussed, the reason for a stronger effect under these conditions could be that the samples contain more individuals at later stages of preclinical AD. It is interesting to note that the largest increase in effect size could be attained if including only those studies which used both PET imaging and categorically defined Aβ levels (n = 8; d = 0.45). While, as mentioned, PiB-PET becomes abnormal much later than CSF Aβ42, adding the additional constraint of using a categorical classification for Aβ increased the effect above that of just PET alone.
4.3. Comparison with previous meta-analysis
The current results extend conclusions about Aβ+-related cognitive impairment and decline drawn from a previous meta-analysis [16]. Unlike for the current meta-analysis, Hedden et al. (2013) concluded that the greatest cognitive dysfunction in Aβ+ CN older adults occurred in the domain of episodic memory (r = 0.12). The additional domains of Aβ+-related cognitive impairment and decline identified in the present study is likely to have occurred because of the comparatively greater number of participants and studies now available and because the Hedden et al. study did not separate data from studies with cross-sectional and those with longitudinal designs. The inclusion/exclusion criteria for the current meta-analysis were also slightly different to that used previously. For example, the present study did not include data from histopathologic studies as the prevalence of comorbidities in these populations, and the substantial time between clinical assessment and death can reduce the reliability of clinicopathologic correlations [66]. The present study also excluded studies that classified Aβ from plasma, given that as yet there are no reliable blood-based biomarkers of CNS Aβ [67]. Most importantly, the current results were based on a much larger sample than the previous study. For example, 59% of studies included in the current meta-analysis were published after the period covered by Hedden et al. Furthermore, the length of prospective studies is now greater, enabling more reliable estimates of Aβ+-related cognitive decline. Thus, the findings from the present study provide a current and reliable foundation for understanding the nature and magnitude of cognitive impairment and decline in Aβ+ CN older adults.
4.4. Limitations and directions for future research
Although the estimates of Aβ+-related cognitive impairment and decline were based on large sample sizes measuring multiple cognitive domains, there are some important caveats on our conclusions. This study did not consider relationships between tau and cognitive impairment or decline. Given that post mortem studies of AD report that cognitive dysfunction is related more strongly to NFT burden than to amyloid burden [66], it is likely that the addition of levels of tau to meta-analyses will provide greater explanation of variability in cognitive outcomes. Second, as discussed above, there was bias toward the measurement of episodic memory in the studies included. Third, although we identified no evidence of publication bias in studies using cross-sectional designs, the limited number of studies using longitudinal designs meant that publication bias was unable to be assessed. This is indicative of the small number of independent, ongoing observational cohort studies. Furthermore, results from the same cohort are often published in multiple articles, so although there may be a wealth of articles reporting on cognitive decline, only a few can be chosen to represent the cohort. Importantly, 20% of the references that were screened in full were excluded due to not including sufficient information for effect size elicitation, and this lead to exclusion of information from some very important and influential studies in the area. While reporting of means and standard deviations is not always appropriate, the explicit reporting of effect sizes and confidence intervals around these should be standard practice, as basing conclusions solely on the absence or presence of statistical significance is inherently flawed [68]. Fourth, the small sample sizes for some estimates may have reduced the reliability of moderator analyses. Although 60% of studies using PET neuroimaging classified Aβ burden using a dichotomous outcome (e.g., low/negative or high/positive) in studies using the [11C] PiB-PET tracer, and calculating burden using distribution volume ratios, the criterion score used to define abnormality has ranged between 1.06 [35] and 1.80 [69]. Additionally, the neocortical areas contributing to these estimates of Aβ burden varied slightly. Recent recommendations outlined by Dubois et al. (2016) [70] highlighted the large methodological variation between studies with regard to their PET and CSF analyses, stating that differences in thresholds established, protocols and procedures used, and reference and target regions used are possible confounding variables.
These caveats notwithstanding, the conclusions here that Aβ is associated with small impairments in episodic memory, executive function, processing speed, visuospatial function, and global cognition, and with greater decline in episodic and semantic memory, visuospatial function, and global cognition, are based on a large sample that can be considered to provide a good representation of a preclinical AD population, with an average age of 70 years, approximately equal numbers of males and females, and the number of APOE ε4 carriers consistent with population prevalence rates [71]. Although these estimates can be considered representative of what would be seen in a preclinical AD population, it is clear that the effect of Aβ on cognition in this early stage is very subtle, and that current neuropsychological measures do not possess the sensitivity to reliably detect Aβ+ related cognitive dysfunction. Development or refinement of neuropsychological measures and procedures sensitive to early neurological changes will ultimately provide the sensitivity and specificity that is required to enable the use of cognitive outcomes as clinical markers of disease. This may mean focusing on tools that have characteristics such as the ability for use with increased frequency of testing, sensitivity to other biological markers of disease in addition to amyloid (such as tau or other markers of neurodegeneration) and which provide evidence of reliable change specific to clinical groups such as those with MCI and AD. The estimates generated here do provide a foundation for determination of the extent to which new tests of cognition or behavioral assays can be used to identify Aβ in CN adults.
Research in context.
-
1.
Systematic review: The authors conducted meta-analyses of the published literature examining relationships between amyloid levels and cognition in cognitively normal older adults using online database Medline OVID. Estimates of cognitive impairment from studies using cross-sectional designs and cognitive decline from studies using longitudinal designs were obtained.
-
2.
Interpretation: The findings indicate that subtle yet statistically significant cognitive impairment and cognitive decline occur in cognitively normal older people with high levels of amyloid. Cognitive impairment is general in nature and small in magnitude, whereas moderate cognitive decline manifests primarily in episodic memory, semantic memory, and visuospatial function.
-
3.
Future directions: The estimates of amyloid-related cognitive impairment and cognitive decline developed from the current meta-analyses provide a strong foundation for the design of studies that seek to improve the detection of amyloid in cognitively normal older adults through the development of new approaches to assessment. They also provide a basis for computing statistical power for secondary prevention clinical trials where slowing cognitive decline may determine the effectiveness of experimental drugs designed to reduce amyloid burden.
Acknowledgments
The authors acknowledge the financial support of the CRC for Mental Health. The Cooperative Research Centre (CRC) programme is an Australian Government Initiative. Y.Y.L is funded by the NHMRC-ARC Dementia Research Development Fellowship.
Footnotes
The authors list no conflicts related to the material presented in this article.
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.dadm.2016.09.002.
Supplementary data
References
- 1.Sperling R.A., Aisen P.S., Beckett L.A., Bennett D.A., Craft S., Fagan A.M. Toward defining the preclinical stages of Alzheimer's disease: Recommendations from the National Institute on Aging and the Alzheimer's Association workgroup. Alzheimers Dement. 2011;7:280–292. doi: 10.1016/j.jalz.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Risacher S.L., Saykin A.J. Neuroimaging and other biomarkers for Alzheimer's disease: The changing landscape of early detection. Annu Rev Clin Psychol. 2013;9:621–648. doi: 10.1146/annurev-clinpsy-050212-185535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rowe C.C., Bourgeat P., Ellis K.A., Brown B., Lim Y.Y., Mulligan R. Predicting Alzheimer disease with β-amyloid imaging: Results from the Australian imaging, biomarkers, and lifestyle study of ageing. Ann Neurol. 2013;74:905–913. doi: 10.1002/ana.24040. [DOI] [PubMed] [Google Scholar]
- 4.Jansen W.J., Ossenkoppele R., Knol D.L., Tijms B.M., Scheltens P., Verhey F.R. Prevalence of cerebral amyloid pathology in persons without dementia. JAMA. 2015;313:1924. doi: 10.1001/jama.2015.4668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rowe C.C., Ng S., Ackermann U., Gong S.J., Pike K., Savage G. Imaging beta-amyloid burden in aging and dementia. Neurology. 2007;68:1718–1725. doi: 10.1212/01.wnl.0000261919.22630.ea. [DOI] [PubMed] [Google Scholar]
- 6.Fagan A.M., Mintun M.A., Mach R.H., Lee S.Y., Dence C.S., Shah A.R. Inverse relation between in vivo amyloid imaging load and cerebrospinal fluid Abeta-42 in humans. Ann Neurol. 2006;59:512–519. doi: 10.1002/ana.20730. [DOI] [PubMed] [Google Scholar]
- 7.Jack C.R., Wiste H.J., Weigand S.D., Rocca W.A., Knopman D.S., Mielke M.M. Age-specific population frequencies of cerebral β-amyloidosis and neurodegeneration among people with normal cognitive function aged 50–89 years: A cross-sectional study. Lancet Neurol. 2014;4422:997–1005. doi: 10.1016/S1474-4422(14)70194-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ossenkoppele R., Jansen W.J., Rabinovici G.D., Knol D.L., van der Flier W.M., van Berckel B.N. Prevalence of amyloid PET positivity in dementia syndromes: A meta-analysis. JAMA. 2015;313:1939–1949. doi: 10.1001/jama.2015.4669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wirth M., Oh H., Mormino E.C., Markley C., Landau S.M., Jagust W.J. The effect of amyloid β on cognitive decline is modulated by neural integrity in cognitively normal elderly. Alzheimers Dement. 2013;9:997–1003. doi: 10.1016/j.jalz.2012.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lim Y.Y., Ellis K.A., Harrington K., Kamer A., Pietrzak R.H., Bush A.I. Cognitive consequences of high Aβ amyloid in mild cognitive impairment and healthy older adults: Implications for early detection of Alzheimer's disease. Neuropsychology. 2013;27:322–332. doi: 10.1037/a0032321. [DOI] [PubMed] [Google Scholar]
- 11.Monsell S.E., Mock C., Hassenstab J., Roe C.M., Cairns N.J., Morris J.C. Neuropsychological changes in asymptomatic persons with Alzheimer disease neuropathology. Neurology. 2014;83:434–440. doi: 10.1212/WNL.0000000000000650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kantarci K., Lowe V., Przybelski S.A., Weigand S.D., Senjem M.L., Ivnik R.J. APOE modifies the association between Aβ load and cognition in cognitively normal older adults. Neurology. 2012;78:232–240. doi: 10.1212/WNL.0b013e31824365ab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harrington M.G., Chiang J., Pogoda J.M., Gomez M., Thomas K., Marion S.D. Executive function changes before memory in preclinical Alzheimer's pathology: A prospective, cross-sectional, case control study. PLoS One. 2013;8:e79378. doi: 10.1371/journal.pone.0079378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ellis K.A., Lim Y.Y., Harrington K., Ames D., Bush A.I., Darby D. Decline in cognitive function over 18 months in healthy older adults with high amyloid-β. J Alzheimers Dis. 2013;34:861–871. doi: 10.3233/JAD-122170. [DOI] [PubMed] [Google Scholar]
- 15.Grober E., Hall C.B., Lipton R.B., Zonderman A.B., Resnick S.M., Kawas C. Memory impairment, executive dysfunction, and intellectual decline in preclinical Alzheimer's disease. J Int Neuropsychol Soc. 2008;14:266–278. doi: 10.1017/S1355617708080302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hedden T., Oh H., Younger A.P., Patel T.A. Meta-analysis of amyloid-cognition relations in cognitively normal older adults. Neurology. 2013;80:1341–1348. doi: 10.1212/WNL.0b013e31828ab35d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huijbers W., Mormino E.C., Wigman S.E., Ward A.M., Vannini P., McLaren D.G. Amyloid deposition is linked to aberrant entorhinal activity among cognitively normal older adults. J Neurosci. 2014;34:5200–5210. doi: 10.1523/JNEUROSCI.3579-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lim Y.Y., Pietrzak R.H., Ellis K.A., Jaeger J., Harrington K., Ashwood T. Rapid decline in episodic memory in healthy older adults with high amyloid-β. J Alzheimers Dis. 2013;33:675–679. doi: 10.3233/JAD-2012-121516. [DOI] [PubMed] [Google Scholar]
- 19.Resnick S.M., Sojkova J., Zhou Y., An Y., Ye W., Holt D.P. Longitudinal cognitive decline is associated with fibrillar amyloid-beta measured by [11C]PiB. Neurology. 2010;74:807–815. doi: 10.1212/WNL.0b013e3181d3e3e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Riley K.P., Jicha G.A., Davis D., Abner E.L., Cooper G.E., Stiles N. Prediction of preclinical Alzheimer's disease: Longitudinal rates of change in cognition. J Alzheimers Dis. 2011;25:707–717. doi: 10.3233/JAD-2011-102133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Snitz B.E., Weissfeld L.A., Lopez O.L., Kuller L.H., Saxton J., Singhabahu D.M. Cognitive trajectories associated with β-amyloid deposition in the oldest-old without dementia. Neurology. 2013;80:1378–1384. doi: 10.1212/WNL.0b013e31828c2fc8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scott J.C., Matt G.E., Wrocklage K.M., Crnich C., Jordan J., Southwick S.M. A quantitative meta-analysis of neurocognitive functioning in posttraumatic stress disorder. Psychol Bull. 2015;141:105–140. doi: 10.1037/a0038039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee R.S., Hermens D.F., Porter M.A., Redoblado-Hodge M.A. A meta-analysis of cognitive deficits in first-episode Major Depressive Disorder. J Affect Disord. 2012;140:113–124. doi: 10.1016/j.jad.2011.10.023. [DOI] [PubMed] [Google Scholar]
- 24.Strauss E., Sherman E.M.S., Spreen O. 3rd ed. Oxford University Press; New York: 2006. A compendium of neuropsychological tests: Administration, norms, and commentary. [Google Scholar]
- 25.Cohen J. A Power Primer. Psychol Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 26.Dickersin K., Berlin J.A. Meta-analysis: State-of-the-Science. Epidemiol Rev. 1992;14:154–176. doi: 10.1093/oxfordjournals.epirev.a036084. [DOI] [PubMed] [Google Scholar]
- 27.Ellis P.D. Cambridge University Press; New York: 2010. The essential guide to effect sizes: Statistical power, meta-analysis, and the interpretation of research results. [Google Scholar]
- 28.Egger M., Davey Smith G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sterne J.A.C., Gavaghan D., Egger M. Publication and related bias in meta-analysis: Power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000;53:1119–1129. doi: 10.1016/s0895-4356(00)00242-0. [DOI] [PubMed] [Google Scholar]
- 30.Morris J.C. The Clinical Dementia Rating: Current version and scoring rules. Neurology. 1993;43:2412–2414. doi: 10.1212/wnl.43.11.2412-a. [DOI] [PubMed] [Google Scholar]
- 31.Petersen R.C., Smith G.E., Waring S.C., Ivnik R.J., Tangalos E.G., Kokmen E. Mild cognitive impairment: Clinical characterization and outcome. Arch Neurol. 1999;56:303–309. doi: 10.1001/archneur.56.3.303. [DOI] [PubMed] [Google Scholar]
- 32.Edmonds E.C., Delano-Wood L., Galasko D.R., Salmon D.P., Bondi M.W. Subtle cognitive decline and biomarker staging in preclinical Alzheimer's disease. J Alzheimers Dis. 2015;47:231–242. doi: 10.3233/JAD-150128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oh H., Steffener J., Razlighi Q.R., Habeck C., Stern Y. β-amyloid deposition is associated with decreased right prefrontal activation during task switching among cognitively normal elderly. J Neurosci. 2016;36:1962–1970. doi: 10.1523/JNEUROSCI.3266-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Loewenstein D.A., Curiel R.E., Greig M.T., Bauer R.M., Rosado M., Bowers D. A novel cognitive stress test for the detection of preclinical Alzheimer's disease: Discriminative properties and relation to amyloid load. Am J Geriatr Psychiatry. 2016;24:804–813. doi: 10.1016/j.jagp.2016.02.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sojkova J., Zhou Y., An Y., Kraut M.A., Ferrucci L., Wong D.F. Longitudinal patterns of β-amyloid deposition in nondemented older adults. Arch Neurol. 2011;68:644–649. doi: 10.1001/archneurol.2011.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mattis S. Psychological Assessment Resources; Odessa: FL: 1988. Dementia Rating Scale (DRS) [Google Scholar]
- 37.Bondi M.W., Edmonds E.C., Jak A.J., Clark L.R., Delano-Wood L., McDonald C.R. Neuropsychological criteria for mild cognitive impairment improves diagnostic precision, biomarker associations, and prediction of progression. J Alzheimers Dis. 2014;42:275–289. doi: 10.3233/JAD-140276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jak A.J., Bondi M.W., Delano-Wood L., Wierenga C., Corey-Bloom J., Salmon D.P. Quantification of five neuropsychological approaches to defining mild cognitive impairment. Am J Geriatr Psychiatry. 2009;17:368–375. doi: 10.1097/JGP.0b013e31819431d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ewers M., Insel P., Jagust W.J., Shaw L., Trojanowski J.Q., Aisen P. CSF biomarker and PIB-PET-derived beta-amyloid signature predicts metabolic, gray matter, and cognitive changes in nondemented subjects. Cereb Cortex. 2012;22:1993–2004. doi: 10.1093/cercor/bhr271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Storandt M., Mintun M.A., Head D., Morris J.C. Cognitive decline and brain volume loss as signatures of cerebral amyloid-β peptide deposition identified with Pittsburgh compound B: Cognitive decline associated with Aβ deposition. Arch Neurol. 2009;66:1476–1481. doi: 10.1001/archneurol.2009.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lim Y.Y., Ellis K.A., Pietrzak R.H., Ames D., Darby D., Harrington K. Stronger effect of amyloid load than APOE genotype on cognitive decline in healthy older adults. Neurology. 2012;79:1645–1652. doi: 10.1212/WNL.0b013e31826e9ae6. [DOI] [PubMed] [Google Scholar]
- 42.Mielke M.M., Machulda M.M., Hagen C.E., Christianson T.J., Roberts R.O., Knopman D.S. Influence of amyloid and APOE on cognitive performance in a late middle-aged cohort. Alzheimers Dement. 2016;12:281–291. doi: 10.1016/j.jalz.2015.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Magnusson K. 2014. Interpreting Cohen's d effect size: An interactive visualization.http://rpsychologist.com/d3/cohend/ Available at: Accessed June 1, 2016. [Google Scholar]
- 44.Zakzanis K.K. Statistics to tell the truth, the whole truth, and nothing but the truth: Formulae, illustrative numerical examples, and heuristic interpretation of effect size analyses for neuropsychological researchers. Arch Clin Neuropsychol. 2001;16:653–667. [PubMed] [Google Scholar]
- 45.Xiong C., Jasielec M.S., Weng H., Fagan A.M., Benzinger T.L.S., Head D. Longitudinal relationships among biomarkers for Alzheimer disease in the Adult Children Study. Neurology. 2016;86:1–8. doi: 10.1212/WNL.0000000000002593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pietrzak R.H., Lim Y.Y., Ames D., Harrington K., Restrepo C., Martins R.N. Trajectories of memory decline in preclinical Alzheimer's disease: Results from the Australian Imaging, Biomarkers and Lifestyle Flagship Study of Ageing. Neurobiol Aging. 2015;36:1231–1238. doi: 10.1016/j.neurobiolaging.2014.12.015. [DOI] [PubMed] [Google Scholar]
- 47.Hassenstab J., Ruvolo D., Jasielec M., Xiong C., Grant E., Morris J.C. Absence of practice effects in preclinical Alzheimer's disease. Neuropsychology. 2015;29:940–948. doi: 10.1037/neu0000208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Braak H., Braak E., Bohl J. Staging of Alzheimer-related cortical destruction. Eur Neurol. 1993;33:403–408. doi: 10.1159/000116984. [DOI] [PubMed] [Google Scholar]
- 49.Gu Y., Razlighi Q.R., Zahodne L.B., Janicki S.C., Ichise M., Manly J.J. Brain amyloid deposition and longitudinal cognitive decline in nondemented older subjects: Results from a multi-ethnic population. PLoS One. 2015;10:e0123743. doi: 10.1371/journal.pone.0123743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chételat G., Villemagne V.L., Pike K.E., Ellis K.A., Bourgeat P., Jones G. Independent contribution of temporal β-amyloid deposition to memory decline in the pre-dementia phase of Alzheimer's disease. Brain. 2011;134:798–807. doi: 10.1093/brain/awq383. [DOI] [PubMed] [Google Scholar]
- 51.Wolk D.A., Dickerson B.C. Fractionating verbal episodic memory in Alzheimer's disease. Neuroimage. 2011;54:1530–1539. doi: 10.1016/j.neuroimage.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Squire L.R., Zola S.M. Structure and function of declarative and nondeclarative memory systems. Proc Natl Acad Sci U S A. 1996;93:13515–13522. doi: 10.1073/pnas.93.24.13515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moscovitch M., Rosenbaum R.S., Gilboa A., Addis D.R., Westmacott R., Grady C. Functional neuroanatomy of remote episodic, semantic and spatial memory: A unified account based on multiple trace theory. J Anat. 2005;207:35–66. doi: 10.1111/j.1469-7580.2005.00421.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Walsh K.W., Darby D. Churchill Livingstone; London: 1999. Neuropsychology: A clinical approach. [Google Scholar]
- 55.Chételat G., Villemagne V.L., Villain N., Jones G., Ellis K.A., Ames D. Accelerated cortical atrophy in cognitively normal elderly with high β-amyloid deposition. Neurology. 2012;78:477–484. doi: 10.1212/WNL.0b013e318246d67a. [DOI] [PubMed] [Google Scholar]
- 56.Jack C.R., Lowe V.J., Senjem M.L., Weigand S.D., Kemp B.J., Shiung M.M. 11C PiB and structural MRI provide complementary information in imaging of Alzheimer's disease and amnestic mild cognitive impairment. Brain. 2008;131:665–680. doi: 10.1093/brain/awm336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Musiek E.S., Holtzman D.M. Three dimensions of the amyloid hypothesis: Time, space and “wingmen”. Nat Neurosci. 2015;18:800–806. doi: 10.1038/nn.4018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Braak H., Braak E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol. 1991;82:239–259. doi: 10.1007/BF00308809. [DOI] [PubMed] [Google Scholar]
- 59.Rodrigue K.M., Kennedy K.M., Devous M.D., Rieck J.R., Hebrank A.C., Diaz-Arrastia R. β-Amyloid burden in healthy aging. Regional distribution and cognitive consequences. Neurology. 2012;78:387–395. doi: 10.1212/WNL.0b013e318245d295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ewers M., Brendel M., Rizk-Jackson A., Rominger A., Bartenstein P., Schuff N. Reduced FDG-PET brain metabolism and executive function predict clinical progression in elderly healthy subjects. Neuroimage Clin. 2014;4:45–52. doi: 10.1016/j.nicl.2013.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lim Y.Y., Maruff P., Pietrzak R.H., Ellis K.A., Darby D., Ames D. Aβ and cognitive change: Examining the preclinical and prodromal stages of Alzheimer's disease. Alzheimers Dement. 2014;10:743–751.e1. doi: 10.1016/j.jalz.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 62.Lim Y.Y., Pietrzak R.H., Bourgeat P., Ames D., Ellis K.A., Rembach A. Relationships between performance on the Cogstate Brief Battery, neurodegeneration, and Aβ accumulation in cognitively normal older adults and adults with MCI. Arch Clin Neuropsychol. 2015;30:49–58. doi: 10.1093/arclin/acu068. [DOI] [PubMed] [Google Scholar]
- 63.Clark L.R., Schiehser D.M., Weissberger G.H., Salmon D.P., Delis D.C., Bondi M.W. Specific measures of executive function predict cognitive decline in older adults. J Int Neuropsychol Soc. 2012;18:118–127. doi: 10.1017/S1355617711001524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Aschenbrenner A.J., Balota D.A., Tse C.S., Fagan A.M., Holtzman D.M., Benzinger T.L.S. Alzheimer disease biomarkers, attentional control, and semantic memory retrieval: Synergistic and mediational effects of biomarkers on a sensitive cognitive measure in non-demented older adults. Neuropsychology. 2015;29:368–381. doi: 10.1037/neu0000133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rolstad S., Berg A.I., Bjerke M., Blennow K., Johansson B., Zetterberg H. Amyloid-β42 is associated with cognitive impairment in healthy elderly and subjective cognitive impairment. J Alzheimers Dis. 2011;26:135–142. doi: 10.3233/JAD-2011-110038. [DOI] [PubMed] [Google Scholar]
- 66.Nelson P.T., Alafuzoff I., Bigio E.H., Bouras C., Braak H., Cairns N.J. Correlation of Alzheimer disease neuropathologic changes with cognitive status: A review of the literature. J Neuropathol Exp Neurol. 2012;71:362–381. doi: 10.1097/NEN.0b013e31825018f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Asih P.R., Chatterjee P., Verdile G., Gupta V.B., Trengove R.D., Martins R.N. Clearing the amyloid in Alzheimer's: Progress towards earlier diagnosis and effective treatments - An update for clinicians. Neurodegener Dis Manag. 2014;4:363–378. doi: 10.2217/nmt.14.29. [DOI] [PubMed] [Google Scholar]
- 68.Cumming G. The new statistics: Why and how. Psychol Sci. 2013;25:1–23. doi: 10.1177/0956797613504966. [DOI] [PubMed] [Google Scholar]
- 69.Aizenstein H.J., Nebes R.D., Saxton J.A., Price J.C., Mathis C.A., Tsopelas N.D. Frequent amyloid deposition without significant cognitive impairment among the elderly. Arch Neurol. 2008;65:1509–1517. doi: 10.1001/archneur.65.11.1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dubois B., Hampel H., Feldman H.H., Scheltens P., Aisen P., Andrieu S. Preclinical Alzheimer's disease: Definition, natural history, and diagnostic criteria. Alzheimers Dement. 2016;12:292–323. doi: 10.1016/j.jalz.2016.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu C.C., Kanekiyo T., Xu H., Bu G. Apolipoprotein E and Alzheimer disease: Risk, mechanisms and therapy. Nat Rev Neurol. 2013;9:106–118. doi: 10.1038/nrneurol.2012.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
References included in the meta-analyses
- 1.Van Harten A.C., Smits L.L., Teunissen C.E., Visser P.J., Koene T., Blankenstein M.A. Preclinical AD predicts decline in memory and executive functions in subjective complaints. Neurology. 2013;81:1409–1416. doi: 10.1212/WNL.0b013e3182a8418b. [DOI] [PubMed] [Google Scholar]
- 2.Edmonds E.C., Delano-Wood L., Galasko D.R., Salmon D.P., Bondi M.W. Subtle cognitive decline and biomarker staging in preclinical Alzheimer's disease. J Alzheimers Dis. 2015;47:231–242. doi: 10.3233/JAD-150128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Landau S.M., Mintun M.A., Joshi A.D., Koeppe R.A., Petersen R.C., Aisen P.S. Amyloid deposition, hypometabolism, and longitudinal cognitive decline. Ann Neurol. 2012;72:578–586. doi: 10.1002/ana.23650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hollands S., Lim Y.Y., Buckley R., Pietrzak R.H., Snyder P.J., Ames D. Amyloid-β related memory decline is not associated with subjective or informant rated cognitive impairment in healthy adults. J Alzheimers Dis. 2015;43:677–686. doi: 10.3233/JAD-140678. [DOI] [PubMed] [Google Scholar]
- 5.Pike K.E., Ellis K.A., Villemagne V.L., Good N., Chételat G., Ames D. Cognition and beta-amyloid in preclinical Alzheimer's disease: Data from the AIBL study. Neuropsychologia. 2011;49:2384–2390. doi: 10.1016/j.neuropsychologia.2011.04.012. [DOI] [PubMed] [Google Scholar]
- 6.Lim Y.Y., Maruff P., Pietrzak R.H., Ames D., Ellis K.A., Harrington K. Effect of amyloid on memory and non-memory decline from preclinical to clinical Alzheimer's disease. Brain. 2013;137:221–231. doi: 10.1093/brain/awt286. [DOI] [PubMed] [Google Scholar]
- 7.Sperling R.A., Johnson K.A., Doraiswamy P.M., Reiman E.M., Fleisher A.S., Sabbagh M. Amyloid deposition detected with florbetapir F 18 (18 F-AV-45) is related to lower episodic memory performance in clinically normal older individuals. Neurobiol Aging. 2013;34:822–831. doi: 10.1016/j.neurobiolaging.2012.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ossenkoppele R., Madison C., Oh H., Wirth M., Van Berckel B.N., Jagust W.J. Is verbal episodic memory in elderly with amyloid deposits preserved through altered neuronal function? Cereb Cortex. 2014;24:2210–2218. doi: 10.1093/cercor/bht076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sojkova J., Zhou Y., An Y., Kraut M.A., Ferrucci L., Wong D.F. Longitudinal patterns of β-amyloid deposition in nondemented older adults. Arch Neurol. 2011;68:644–649. doi: 10.1001/archneurol.2011.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lim Y.Y., Maruff P., Schindler R., Ott B.R., Salloway S., Yoo D.C. Disruption of cholinergic neurotransmission exacerbates Aβ-related cognitive impairment in preclinical Alzheimer's disease. Neurobiol Aging. 2015;36:2709–2715. doi: 10.1016/j.neurobiolaging.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 11.Stomrud E., Hansson O., Zetterberg H., Blennow K., Minthon L., Londos E. Correlation of longitudinal cerebrospinal fluid biomarkers with cognitive decline in healthy older adults. Arch Neurol. 2010;67:217–223. doi: 10.1001/archneurol.2009.316. [DOI] [PubMed] [Google Scholar]
- 12.Oh H., Steffener J., Razlighi Q.R., Habeck C., Stern Y. β-amyloid deposition is associated with decreased right prefrontal activation during task switching among cognitively normal elderly. J Neurosci. 2016;36:1962–1970. doi: 10.1523/JNEUROSCI.3266-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rolstad S., Berg A.I., Bjerke M., Blennow K., Johansson B., Zetterberg H. Amyloid-β42 is associated with cognitive impairment in healthy elderly and subjective cognitive impairment. J Alzheimers Dis. 2011;26:135–142. doi: 10.3233/JAD-2011-110038. [DOI] [PubMed] [Google Scholar]
- 14.Gidicsin C.M., Maye J.E., Locascio J.J., Pepin L.C., Philiossaint M., Becker J.A. Cognitive activity relates to cognitive performance but not to Alzheimer disease biomarkers. Neurology. 2015;85:48–55. doi: 10.1212/WNL.0000000000001704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Papp K.V., Mormino E.C., Amariglio R.E., Munro C., Dagley A., Schultz A.P. Biomarker validation of a decline in semantic processing in preclinical Alzheimer's disease. Neuropsychology. 2016;30:624–630. doi: 10.1037/neu0000246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Amariglio R.E., Becker J.A., Carmasin J., Wadsworth L.P., Lorius N., Sullivan C. Subjective cognitive complaints and amyloid burden in cognitively normal older individuals. Neuropsychologia. 2012;50:2880–2886. doi: 10.1016/j.neuropsychologia.2012.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hedden T., Mormino E.C., Amariglio R.E., Younger A.P., Schultz A.P., Becker J.A. Cognitive profile of amyloid burden and white matter hyperintensities in cognitively normal older adults. J Neurosci. 2012;32:16233–16242. doi: 10.1523/JNEUROSCI.2462-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Petersen R.C., Wiste H.J., Weigand S.D., Rocca W.A., Roberts R.O., Mielke M.M. Association of elevated amyloid levels with cognition and biomarkers in cognitively normal people from the community. JAMA Neurol. 2015;73:85–92. doi: 10.1001/jamaneurol.2015.3098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kantarci K., Lowe V., Przybelski S.A., Weigand S.D., Senjem M.L., Ivnik R.J. APOE modifies the association between Aβ load and cognition in cognitively normal older adults. Neurology. 2012;78:232–240. doi: 10.1212/WNL.0b013e31824365ab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mielke M.M., Machulda M.M., Hagen C.E., Christianson T.J., Roberts R.O., Knopman D.S. Influence of amyloid and APOE on cognitive performance in a late middle-aged cohort. Alzheimers Dement. 2016;12:281–291. doi: 10.1016/j.jalz.2015.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rentz D.M., Locascio J.J., Becker J.A., Moran E.K., Eng E., Buckner R.L. Cognition, reserve, and amyloid deposition in normal aging. Ann Neurol. 2010;67:353–364. doi: 10.1002/ana.21904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Loewenstein D.A., Curiel R.E., Greig M.T., Bauer R.M., Rosado M., Bowers D. A novel cognitive stress test for the detection of preclinical Alzheimer's disease: Discriminative properties and relation to amyloid load. Am J Geriatr Psychiatry. 2016;24:804–813. doi: 10.1016/j.jagp.2016.02.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barthel H., Gertz H.J., Dresel S., Peters O., Bartenstein P., Buerger K. Cerebral amyloid-β PET with florbetaben (18F) in patients with Alzheimer's disease and healthy controls: A multicentre phase 2 diagnostic study. Lancet Neurol. 2011;10:424–435. doi: 10.1016/S1474-4422(11)70077-1. [DOI] [PubMed] [Google Scholar]
- 24.Nebes R.D., Snitz B.E., Cohen A.D., Aizenstein H.J., Saxton J.A., Halligan E.M. Cognitive aging in persons with minimal amyloid-beta and white matter hyperintensities. Neuropsychologia. 2013;51:2202–2209. doi: 10.1016/j.neuropsychologia.2013.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aizenstein H.J., Nebes R.D., Saxton J.A., Price J.C., Mathis C.A., Tsopelas N.D. Frequent amyloid deposition without significant cognitive impairment among the elderly. Arch Neurol. 2008;65:1509–1517. doi: 10.1001/archneur.65.11.1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Doherty B.M., Schultz S.A., Oh J.M., Koscik R.L., Dowling N.M., Barnhart T.E. Amyloid burden, cortical thickness, and cognitive function in the Wisconsin Registry for Alzheimer's Prevention. Alzheimers Dement (Amst) 2015;1:160–169. doi: 10.1016/j.dadm.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aschenbrenner A.J., Balota D.A., Fagan A.M., Duchek J.M., Benzinger T.L.S., Morris J.C. Alzheimer disease cerebrospinal fluid biomarkers moderate baseline differences and predict longitudinal change in attentional control and episodic memory composites in the Adult Children Study. J Int Neuropsychol Soc. 2015;21:573–583. doi: 10.1017/S1355617715000776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xiong C., Jasielec M.S., Weng H., Fagan A.M., Benzinger T.L.S., Head D. Longitudinal relationships among biomarkers for Alzheimer disease in the Adult Children Study. Neurology. 2016;86:1–8. doi: 10.1212/WNL.0000000000002593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hassenstab J., Chasse R., Grabow P., Benzinger T.L.S., Fagan A.M., Xiong C. Certified normal: Alzheimer's disease biomarkers and normative estimates of cognitive functioning. Neurobiol Aging. 2016;43:23–33. doi: 10.1016/j.neurobiolaging.2016.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang L., Benzinger T.L., Hassenstab J., Blazey T., Owen C., Fagan A.M. Spatially distinct atrophy is linked to β-amyloid and tau in preclinical Alzheimer disease. Neurology. 2015;84:1254–1260. doi: 10.1212/WNL.0000000000001401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ewers M., Insel P., Jagust W.J., Shaw L., Trojanowski J.Q., Aisen P. CSF biomarker and PIB-PET-derived beta-amyloid signature predicts metabolic, gray matter, and cognitive changes in nondemented subjects. Cereb Cortex. 2012;22:1993–2004. doi: 10.1093/cercor/bhr271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lim Y.Y., Ellis K.A., Pietrzak R.H., Ames D., Darby D., Harrington K. Stronger effect of amyloid load than APOE genotype on cognitive decline in healthy older adults. Neurology. 2012;79:1645–1652. doi: 10.1212/WNL.0b013e31826e9ae6. [DOI] [PubMed] [Google Scholar]
- 33.Doraiswamy P., Sperling R.A., Johnson K., Reiman E.M., Wong T.Z., Sabbagh M.N. Florbetapir F 18 amyloid PET and 36-month cognitive decline: A prospective multicenter study. Mol Psychiatry. 2014;19:1044–1051. doi: 10.1038/mp.2014.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wirth M., Oh H., Mormino E.C., Markley C., Landau S.M., Jagust W.J. The effect of amyloid β on cognitive decline is modulated by neural integrity in cognitively normal elderly. Alzheimers Dement. 2013;9:997–1003. doi: 10.1016/j.jalz.2012.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Resnick S.M., Sojkova J., Zhou Y., An Y., Ye W., Holt D.P. Longitudinal cognitive decline is associated with fibrillar amyloid-beta measured by [11C]PiB. Neurology. 2010;74:807–815. doi: 10.1212/WNL.0b013e3181d3e3e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mormino E., Betensky R.A., Hedden T., Schultz A.P., Amariglio R.E., Rentz D.M. Synergistic Effect of β-Amyloid and Neurodegeneration on Cognitive Decline in Clinically Normal Individuals. JAMA Neurol. 2014;71:1379. doi: 10.1001/jamaneurol.2014.2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roe C.M., Fagan A.M., Grant E.A., Hassenstab J., Dreyfus D.M., Sutphen C.L. Amyloid imaging and CSF biomarkers in predicting cognitive impairment up to 7.5 years later. Neurology. 2013;80:1784–1791. doi: 10.1212/WNL.0b013e3182918ca6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Storandt M., Mintun M.A., Head D., Morris J.C. Cognitive decline and brain volume loss as signatures of cerebral amyloid-β peptide deposition identified with Pittsburgh compound B: Cognitive decline associated with Aβ deposition. Arch Neurol. 2009;66:1476–1481. doi: 10.1001/archneurol.2009.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.