Abstract
Purpose
To determine recent trends for and sociodemographic/comorbid conditions associated with penetrating (PK) and lamellar keratoplasties (LK) in keratoconus (KCN).
Methods
KCN patients and subsequent PK and LK procedures were identified using ICD-9 and CPT billing codes. The change in surgical rates was calculated over a decade and multivariate analysis demonstrated factors associated with having surgery.
Results
21588 KCN patients had 1306 PK’s and 109 LK’s during the study period. Individuals were significantly less likely to undergo PK from 2009–2012 compared to 2001–2008 (odds ratio [OR] 0.57, 95% confidence interval [CI] 0.47–0.68, p <0.001). Multivariate analysis revealed the factors that increased the likelihood of PK alone and included age 20–40 (OR 1.90, 95% CI 1.19–3.04, p <0.001), black race (OR 1.36, 95% CI 1.06–1.74, p = 0.01), and education less than a bachelor degree or a high school diploma only (OR 1.94–2.84, p <0.001 for all comparisons). Female gender (OR 0.74, 95% CI 0.63–0.88, p <0.001) and household net worth either between 150 and 249K (OR 0.64, 95% CI 0.48–0.84, p <0.001) or more than $500,000 (OR 0.71, 95% CI 0.51–0.99, p = 0.03) were traits associated with a decreased odds of PK. No significant associations for LK were observed.
Conclusion
The rate of PK in KCN is decreasing in the United States. The 3rd or 4th decade of life, male gender, black race, lower education, and greater household net worth are associated with increased odds of PK.
Keywords: penetrating keratoplasty, keratoconus, lamellar keratoplasty, socioeconomic factors
Introduction
Keratoconus is typically a bilateral, progressive corneal ectasia with the usual onset occurring during puberty. Historically, penetrating keratoplasty (PK) has been the standard of care in the surgical management in keratoconus.1,2 More recently, the use of other procedures has been increasing, including deep anterior lamellar keratoplasty, intrastromal corneal ring segments, and collagen cross-linking.3 Numerous international retrospective studies have suggested that rates of penetrating keratoplasties are decreasing for keratoconus.4,5,6,7,8,9
However, studies from the United States (US) have failed to show the same trend. One study from a large practice in Indiana revealed that that the rate of transplantation in keratoconus was stable from 1982 to 1996.10 Similarly, a report from a large tertiary care center found that the rates of transplant remained constant from 1989 to 1995.11 Another study using data from the Eye Bank Association of America even found that penetrating keratoplasty (PK) rates for keratoconus were gradually increasing from 1990 to 2004, despite an overall decrease in PK’s for all indications.12 All of these US-based studies are now more than a decade old and the first two focused on results only from a single institution or practice, possibly explaining the discrepancy with the more recent international literature.
Recently, race, obstructive sleep apnea, asthma and Down syndrome have all been associated with an increased risk of being diagnosed with keratoconus, but how these and other socio-demographic and co-morbid factors relate to the risk of corneal transplantation has yet to be determined.13 The primary aim of this study is to investigate recent trends in corneal transplantation for keratoconus in the United States while also analyzing the socio-demographic and co-morbid factors associated with the rate of transplantation.
Materials and methods
Setting/Data Set
The Clinformatics™ Data Mart Database (OptumInsight, Eden Prairie, MN), which contains de-identified medical claims of all beneficiaries from a large national insurance provider in the United States, was used for this study. Included within the database are all outpatient medical claims (office visits, outpatient surgeries and associated diagnoses) and demographic data for all beneficiaries during their enrollment in the insurance plan. The subset of data available for this study included all patients in the database from January 1, 2000, to June 30, 2013. The University of Pennsylvania’s institutional review board deemed this study exempt from review owing to the de-identified nature of the data.
Cohorts
Cohorts were created comprised of each calendar year dating from 2001 to 2012. Every patient with a billing claim from an eye care provider with an ICD-9 diagnosis code for keratoconus (ICD-9 371.6x) (Table 1) was assigned an index date based on the date of first diagnosis. Each patient was then included in each following cohort year that a keratoconus diagnosis appeared. Additionally, patients were also included into subsequent cohort years if they had at least 6 months of continuous data in that year regardless of if they had a claim for keratoconus in that year. Patients were excluded from the analysis if they had less then 1 year prior to or less then 6 months of continuous data after the index date. Additionally, patients were excluded if they had any previous ICD-9 codes for other corneal disease that may require a corneal transplant (ICD-9 371.0x–371.5x; 371.7x–371.8x).
Table 1.
ICD-9 and CPT Codes Used in this Study
| Diagnosis/Procedure | ICD-9 or CPT Code |
|---|---|
|
| |
| Keratoconus | 371.6x |
|
| |
| Corneal Disease | 371.0x–371.5x, 371.7x–371.8x |
|
| |
| Comorbid Conditions | |
| Allergic rhinitis | 477.0x, 477.2x, 477.8x, 477.9x |
| Asthma | 493.xx |
| Dementia | 290.xx, 294.1x, 331.2x |
| Depression | 296.xx |
| Diabetes | 250.xx, 362.01–362.07 |
| Down Syndrome | 758.0x |
| Hyperlipidemia | 272.xx |
| Sleep apnea | 327.2x, 780.51, 780.53, 780.57 |
| Cataract | 366.0x–366.4x, 366.8x, 366.9x |
| Macular degeneration | 362.51, 362.52, 362.57 |
| Primary open angle glaucoma | 365.1x |
| Pseudophakia/aphakia | V431, 379.3, 379.3 |
|
| |
| Penetrating Keratoplasty | 65730, 65750, 65755 |
|
| |
| Lamellar Keratoplasty | 65710 |
Outcomes of interest
The primary outcome was the rate of corneal transplantation per patient over time. A corneal transplant was considered to have occurred on any date in which a CPT code was seen for either a PK (CPT4 codes 65730, 65750, 65755) or lamellar keratoplasty (LK) (CPT4 code 65710). Final rates were adjusted for age, gender, race, household net worth, education level, diabetes, asthma, allergic rhinitis, collagen vascular disease, aortic aneurysm, Down syndrome, sleep apnea, hyperlipidemia, depression, dementia, macular degeneration, primary open angle glaucoma, cataract, pseudophakia, aphakia, index year, region of the country and insurance plan type.
Statistical analysis
Demographic information and medical conditions were collected based on date of index date (except age, which could change with each additional year patient was entered into a cohort). Categorical variables were tested with chi-square in univariate testing. The univariate test for trend was used across each cohort year for rates of surgeries. Multiple logistic regression was used to calculate odds ratios for having a transplant surgery. All p-values less then 0.05 were considered significant.
Results
A total of 21,588 patients with an ICD-9 diagnosis of keratoconus were identified during the study period after exclusions were applied (Figure 1). 618 patients underwent 1306 penetrating keratoplasties and 66 patients underwent 109 lamellar keratoplasties. Demographic characteristics of the patients undergoing transplantation are summarized in Table 2.
Figure 1.
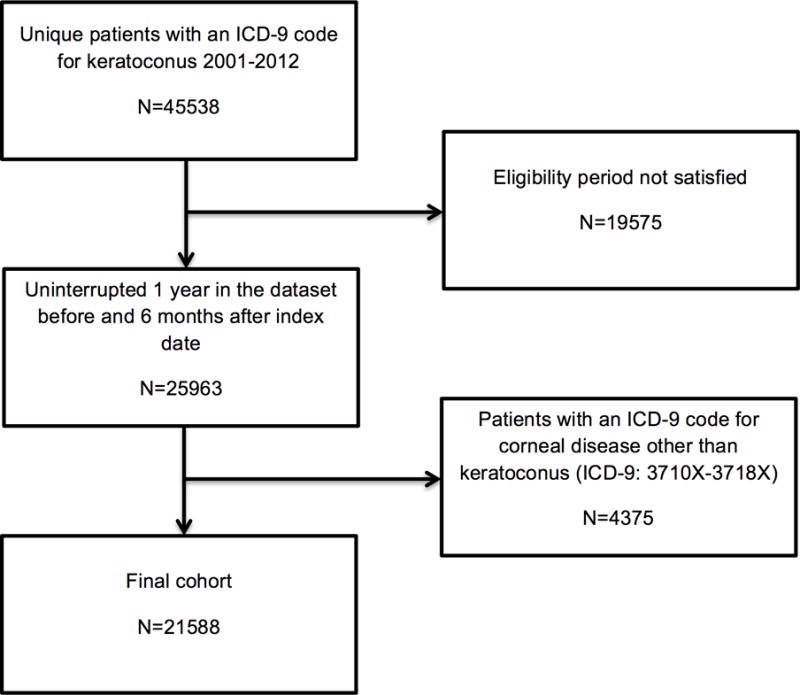
Flow chart for inclusion and exclusion criteria for study patients.
Table 2.
Baseline Characteristics
| Characteristic | Total Keratoconus Patients | Number of Penetrating Keratoplasty Surgeries (%) | Number of Lamellar Keratoplasty Surgeries (%) |
|---|---|---|---|
| Age | |||
| 0–20 | 1365 | 19 (1.4%) | 3 (0.2%) |
| 20–40 | 10848 | 290 (2.7%) | 39 (0.4%) |
| 40–60 | 15466 | 231 (1.5%) | 19 (0.1%) |
| 60–80 | 4749 | 73 (1.5%) | 5 (0.1%) |
| ≥80 | 309 | 5 (1.6%) | 0 (0.0%) |
| Gender | |||
| Male | 18670 | 386 (2.1%) | 42 (0.2%) |
| Female | 14067 | 232 (1.6%) | 24 (0.2%) |
| Region | |||
| Midwest | 9072 | 170 (1.9%) | 21 (0.2%) |
| Northeast | 4475 | 44 (1.0%) | 9 (0.2%) |
| South | 12771 | 255 (2.0%) | 27 (0.2%) |
| West | 6419 | 149 (2.3%) | 9 (0.1%) |
| Race | |||
| White | 22667 | 393 (1.7%) | 43 (0.2%) |
| Black | 3303 | 96 (2.9%) | 10 (0.3%) |
| Hispanic/Latino | 3157 | 57 (1.8%) | 10 (0.3%) |
| Other | 3610 | 72 (2.0%) | 3 (0.1%) |
| Education | |||
| Bachelor Degree Plus | 8717 | 84 (1.0%) | 12 (0.1%) |
| Less than Bachelor Degree | 16502 | 316 (1.9%) | 34 (0.2%) |
| High School Diploma | 6144 | 178 (2.9%) | 17 (0.3%) |
| Less than 12th Grade | 194 | 4 (2.1%) | 0 (0.0%) |
| Unknown | 1180 | 36 (3.1%) | 3 (0.3%) |
| Household Net Worth | |||
| <$25K | 2908 | 94 (3.2%) | 13 (0.4%) |
| $25–149K | 2314 | 56 (2.4%) | 8 (0.3%) |
| $150–249K | 8658 | 141 (1.6%) | 15 (0.2%) |
| $250–499K | 2880 | 49 (1.7%) | 6 (0.2%) |
| $500K+ | 7880 | 97 (1.2%) | 8 (0.1%) |
| Unknown | 8097 | 181 (2.2%) | 16 (0.2%) |
| Insurance Type | |||
| Medicare | 2103 | 40 (1.9%) | 2 (0.1%) |
| Commercial | 30406 | 569 (1.9%) | 63 (0.2%) |
| Medicaid | 228 | 9 (3.9%) | 1 (0.4%) |
| Comorbid Conditions | |||
| Allergic Rhinitis | 2407 | 31 (1.3%) | 4 (0.2%) |
| Asthma | 1354 | 21 (1.6%) | 1 (0.1%) |
| Depression | 810 | 13 (1.6%) | 0 (0.0%) |
| Diabetes | 2336 | 39 (1.7%) | 1 (0.0%) |
| Down Syndrome | 59 | 3 (5.1%) | 0 (0.0%) |
| Hyperlipidemia | 5740 | 78 (1.4%) | 6 (0.1%) |
| Sleep apnea | 1099 | 22 (2.0%) | 2 (0.2%) |
| Cataract | 3363 | 50 (1.5%) | 3 (0.1%) |
| Macular degeneration | 287 | 1 (0.3%) | 0 (0.0%) |
| Primary Open Angle Glaucoma | 548 | 4 (0.7%) | 1 (0.2%) |
| Pseudophakia/aphakia | 634 | 12 (1.9%) | 1 (0.2%) |
For the multivariate analysis for penetrating keratoplasty alone, with regards to demographic information, patients age 20–40 were significantly more likely to undergo PK (odds ratio [OR] 1.90, 95% confidence interval [CI] 1.19–3.04, p <0.001) than those aged 0–20. None of the other age groups showed a significant association with having a PK (p>0.05 for all comparisons). Black patients were significantly more likely to undergo PK than whites (OR 1.36, 95% CI 1.06–1.74, p = 0.01). No other race showed a significant association with the odds of having surgery (p>0.05 for all comparisons). Compared to patients in the geographic Midwest, patients in the Northeast were significantly less (OR 0.58, 95% CI 0.42–0.82, p <0.001) and the West significantly more (OR 1.48, 95% CI 1.18–1.86, p <0.001) likely to undergo PK. Factors found to be associated with a decreased odds of having a transplant included female gender (OR 0.74, 95% CI 0.63–0.88, p <0.001) and more than a bachelor’s degree of education (less than a bachelor’s degree OR 1.94, 95% CI 1.50–2.49, p < 0.001; high school diploma OR 2.84, 95% CI 2.12–3.81, p < 0.001). Patients with a household net worth of $150,000–249,000 (OR 0.64, 95% CI 0.48–0.84, p = 0.03) and > $500,000 (OR 0.71, 95% CI 0.51–0.99, p = 0.03) were also significantly less likely to undergo PK than those with household net worth < $25,000. Although several comorbid systemic and ocular conditions were significant in the univariate analysis, no associations achieved significance in the multivariate analysis (See Table 3).
Table 3.
Results of Univariate Analyses for Penetrating and Lamellar Keratoplasties
| Penetrating Keratoplasty | Lamellar Keratoplasty | |||
|---|---|---|---|---|
|
| ||||
| Characteristic | OR (95% CI) | P-value | OR (95% CI) | P-value |
| Age | <0.001 | 0.001 | ||
| 0–20 | ref | ref | ||
| 20–40 | 1.95 (1.22, 3.11) | 1.64 (0.51, 5.31) | ||
| 40–60 | 1.07 (0.67, 1.72) | 0.56 (0.17, 1.89) | ||
| 60–80 | 1.11 (0.67, 1.84) | 0.48 (0.11, 2.00) | ||
| ≥80 | 1.17 (0.43, 3.15) | NA | ||
| Female | 0.79 (0.67, 0.94) | 0.006 | 0.76 (0.46, 1.25) | 0.28 |
| Region | <0.001 | 0.65 | ||
| Midwest | ref | ref | ||
| Northeast | 0.52 (0.37, 0.73) | 0.87 (0.40, 1.90) | ||
| South | 1.07 (0.88, 1.30) | 0.91 (0.52, 1.62) | ||
| West | 1.24 (1.00, 1.55) | 0.61 (0.28, 1.32) | ||
| Race | <0.001 | 0.11 | ||
| White | ref | ref | ||
| Black | 1.70 (1.35, 2.13) | 1.60 (0.80, 3.18) | ||
| Hispanic/Latino | 1.04 (0.79, 1.38) | 1.67 (0.84, 3.33) | ||
| Other | 1.15 (0.89, 1.49) | 0.44 (0.14, 1.41) | ||
| Education | <0.001 | 0.47 | ||
| Bachelor Degree Plus | ref | ref | ||
| Less than Bachelor Degree | 2.01 (1.57, 2.56) | NA | ||
| High School Diploma | 3.07 (2.36, 3.98) | 2.01 (0.96, 4.22) | ||
| Less than 12th Grade | 2.16 (0.79, 5.96) | 1.50 (0.78, 2.89) | ||
| Unknown | 3.23 (2.18, 4.80) | 1.85 (0.52, 6.56) | ||
| Household Net Worth | <0.001 | 0.02 | ||
| <$25K | ref | ref | ||
| $25–149K | 0.74 (0.53, 1.04) | 0.77 (0.32, 1.87) | ||
| $150–249K | 0.50 (0.38, 0.65) | 0.39 (0.18, 0.81) | ||
| $250–499K | 0.52 (0.37, 0.73) | 0.46 (0.18, 1.22) | ||
| $500K+ | 0.37 (0.28, 0.50) | 0.23 (0.09, 0.55) | ||
| Unknown | 0.68 (0.53, 0.88) | 0.44 (0.21, 0.92) | ||
| Insurance Type | 0.08 | 0.41 | ||
| Medicare | ref | ref | ||
| Commercial | 0.98 (0.71, 1.36) | 2.18 (0.53, 8.92) | ||
| Medicaid | 2.12 (1.02, 4.43) | 4.63 (0.42, 51.24) | ||
| Allergic Rhinitis | 0.66 (0.46, 0.95) | 0.03 | 0.81 (0.30, 2.24) | 0.69 |
| Asthma | 0.81 (0.52, 1.26) | 0.35 | 0.36 (0.05, 2.57) | 0.31 |
| Depression | 0.84 (0.49, 1.47) | 0.55 | n/a | |
| Diabetes | 0.87 (0.63, 1.21) | 0.42 | 0.20 (0.03, 1.44) | 0.11 |
| Down Syndrome | 2.79 (0.87, 8.95) | 0.08 | n/a | |
| Hyperlipidemia | 0.67 (0.53, 0.86) | 0.001 | 0.47 (0.20, 1.09) | 0.08 |
| Sleep apnea | 1.06 (0.69, 1.64) | 0.78 | 0.90 (0.22, 3.68) | 0.88 |
| Cataract | 0.77 (0.57, 1.02) | 0.07 | 0.42 (0.13, 1.32) | 0.14 |
| Macular degeneration | 0.18 (0.03, 1.29) | 0.09 | n/a | |
| Primary Open Angle Glaucoma | 0.38 (0.14, 1.02) | 0.054 | 0.90 (0.13, 6.52) | 0.92 |
| Pseudophakia/aphakia | 1.00 (0.56, 1.79) | 0.99 | 0.78 (0.11, 5.62) | 0.80 |
| Year | <0.001 | 0.22 | ||
| 2001–2008 | ref | ref | ||
| 2009–2012 | 0.57 (0.48, 0.67) | 0.73 (0.45, 1.21) | ||
For lamellar keratoplasty, due to relatively small operative numbers in each cohort, few factors were found to be associated with LK surgery in either univariate or multivariate testing. Univariate analysis demonstrated that only a household net worth of $150,000–249,000 (OR 0.39, 95% CI 0.18–0.81, p = 0.02) and > $500,000 (OR 0.23, 95% CI 0.09–0.55 p = 0.02) showed significance. Multivariate analysis revealed that only age showed significance across all comparisons, although none of the individual comparisons were significant. (See Table 4).
Table 4.
Results of Multivariate Analyses for Penetrating and Lamellar Keratoplasties
| Penetrating Keratoplasty | Lamellar Keratoplasty | |||
|---|---|---|---|---|
|
| ||||
| Characteristic | OR (95% CI) | P-value | OR (95% CI) | P-value |
| Age | <0.001 | 0.001 | ||
| 0–20 | 1.00 | 1.00 | ||
| 20–40 | 1.90 (1.19, 3.04) | 1.64 (0.51, 5.32) | ||
| 40–60 | 1.25 (0.78, 2.01) | 0.56 (0.17, 1.90) | ||
| 60–80 | 1.45 (0.86, 2.45) | 0.50 (0.12, 2.11) | ||
| ≥80 | 1.76 (0.64, 4.84) | n/a | ||
| Female | 0.74 (0.63, 0.88) | <0.001 | n/a | |
| Region | <0.001 | n/a | ||
| Midwest | 1.00 | |||
| Northeast | 0.58 (0.42, 0.82) | |||
| South | 1.06 (0.86, 1.30) | |||
| West | 1.48 (1.18, 1.86) | |||
| Race | 0.01 | n/a | ||
| White | 1.00 | |||
| Black | 1.36 (1.06, 1.74) | |||
| Hispanic/Latino | 0.79 (0.59, 1.06) | |||
| Other | 0.93 (0.68, 1.28) | |||
| Education | <0.001 | n/a | ||
| Bachelor Degree Plus | 1.00 | |||
| Less than Bachelor’s | 1.94 (1.50, 2.49) | |||
| High School Diploma | 2.84 (2.12, 3.81) | |||
| Less than 12th Grade | 1.70 (0.60, 4.78) | |||
| Unknown | 2.55 (1.56, 4.17) | |||
| Household Net Worth | 0.03 | n/a | ||
| <$25K | 1.00 | |||
| $25–149K | 0.79 (0.56, 1.11) | |||
| $150–249K | 0.64 (0.48, 0.84) | |||
| $250–499K | 0.72 (0.49, 1.04) | |||
| $500K+ | 0.71 (0.51, 0.99) | |||
| Unknown | 0.86 (0.66, 1.13) | |||
| Allergic Rhinitis | 0.71 (0.49, 1.02) | 0.06 | n/a | |
| Down Syndrome | 2.94 (0.90, 9.60) | 0.07 | n/a | |
| Hyperlipidemia | 0.80 (0.62, 1.02) | 0.08 | n/a | |
| Macular Degeneration | 0.22 (0.03, 1.58) | 0.13 | n/a | |
| Primary Open Angle Glaucoma | 0.44 (0.16, 1.18) | 0.10 | n/a | |
| Year | <0.001 | 0.39 | ||
| 2001–2008 | ref | ref | ||
| 2009–2012 | 0.57 (0.47, 0.68) | 0.80 (0.49, 1.32) | ||
The percent of the study cohort undergoing penetrating keratoplasty each year showed a significantly decreasing trend (p < 0.001) (Figure 2). The rates ranged from a high of 8.8% in 2002 to a low of 2.4% in 2011. To better quantitate the decreasing rate of PK surgery, the study period was split into two groups, from 2001–2008 and 2009–2012. After controlling for sociodemographic and comorbid conditions, the odds of undergoing a penetrating keratoplasty was significantly less likely in the latter period (OR 0.57, 95% CI 0.48–0.67 p-value < 0.001). Lamellar keratoplasty occurred much less frequently than PK during the study period, ranging from a high of 0.63% in 2002 and 2006 to a low of 0.13% in 2001. (Figure 3) No difference in rates of LK was found throughout the study (univariate test for trend p = 0.10 & multivariate analysis: 2009–2012 OR 0.80, 95% CI 0.49–1.32; p=0.39).
Figure 2.
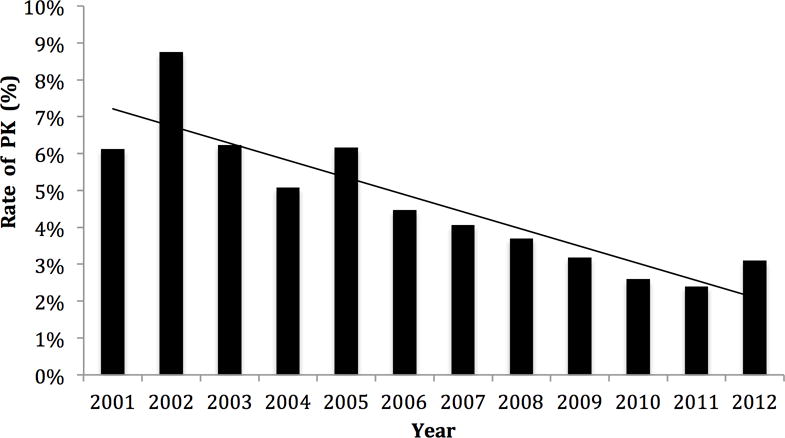
Penetrating keratoplasty (PK) rates over time.
Figure 3.
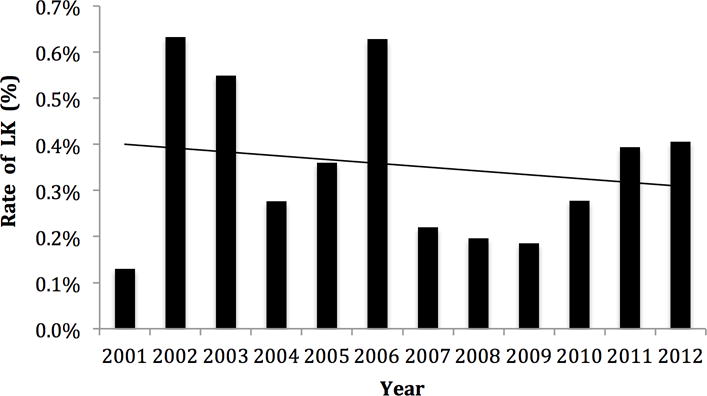
Lamellar keratoplasty (LK) rates over time.
Discussion
Our study found a decreasing rate of penetrating keratoplasty in keratoconus in the United States during the period 2001 to 2012 with the drop being most noticeable in the 2009–2012 period compared to the previous period. Age 20–40, male gender, black race, western geographic location, lower household net worth, and less education were all associated with increased rates of PK. No systemic or ocular comorbid conditions were associated with having a PK. Although several medical diagnoses have been associated with the development of keratoconus,13 these same conditions do not alter the risk of having surgery. Strengths of this study include the large sample size in a national database, making it less likely that practice patterns regionally or at an individual institution would influence results. We believe that this is the largest study to date looking at keratoconus. Additionally, we were able to collect a significant amount of demographic and medical history information to determine the associations of these variables on the rates of PK and LK.
We suspect that the trend of decreasing penetrating keratoplasty in keratoconus is multifactorial, but primarily related to advancements in alternative therapeutic modalities, including corneal cross linking, intrastromal ring segments, and likely most importantly for the time frame observed in this study, the advancement of contact lens technology. These procedures have the advantage of avoiding many of the potential complications associated with corneal transplantation, including short and long-term graft failure and dehiscence.3 Interestingly, the rate of lamellar keratoplasty was both relatively low and stable throughout the study period, meaning this procedure was unlikely to play a substantial role in the decreasing rate of penetrating keratoplasty during the same time period.
These results represent a dramatic shift from the previously reported trends in the United States. Darlington et al. reviewed data from 1980 to 2004 and found that despite an overall decreasing PK rate in the United States since 1990, PK rates in keratoconus increased.12 In another large single institution study, Lois et al. reported a stable rate of PK’s performed for keratoconus from 1989 to 1995.11 Similarly, Dobbins et al. described 481 PK’s for keratoconus performed at a single practice in Indiana from 1982 to 1996, also finding that there were no significant trends in frequency of PK for keratoconus.10 Although not specific to keratoconus, these results are in contrast to endothelial keratoplasty in the United States, which has been shown to be increasing.14
More recently, international studies have shown a trend towards decreasing corneal transplantation for keratoconus.4,5,6,7,8,9 These studies along with the present data indicate that decreasing PK for keratoconus is an international trend. Our findings are most likely a product of the substantial improvement in contact lens technology,15,16 as many patients who previously required a transplant may now be managed solely with contact lenses. This idea is further supported by a large epidemiologic study demonstrating the clear improvement in quality of life reported by contact lens wearers with KCN.17 Although LK may significantly influence PK rates in the future, there was no corresponding increase in LK in our study that could explain the decreasing PK. In addition, although crosslinking has been approved internationally for much longer and is used more widely, in the US, crosslinking was only FDA approved this past year and was not likely to have impacted our results.
It has been previously reported that transplantation in keratoconus is more likely in patients of younger age and non-Caucasian race.18 Additionally, our data suggests that lower socioeconomic factors, including less education and lower household net worth, are associated with increased odds of transplantation. To our knowledge, this has not been previously reported. We speculate that this finding is a consequence of the typically high out-of-pocket costs associated with fitting and purchasing contact lenses, making insurance covered surgery a more affordable option to improve visual acuity for these patients.
Wealthy patients were over-represented in this study. Although only 10.4% of the entire database had a net worth greater than $500,000, these individuals contributed 24.1% of the total patient years studied, indicating that the data from wealthy patients are clearly out of proportion to the underlying population. This suggests one of two things; either keratoconus occurs at higher rates in those with greater wealth, or more likely, socioeconomic barriers exist to seeking care for keratoconus even in those with health insurance. Together with the lower surgical rate, these data suggest that the wealthy group may be diagnosed at a less severe stage of disease, and that they may have better access to non-surgical alternatives, especially contact lenses.
Limitations of this study include several inherent to this type of data. Billing claims data rely on the individual practitioner’s diagnostic coding and cannot be verified with chart level data. Also due to the ambiguity of procedure coding, following patients on a per eye basis is difficult, necessitating a per patient based analysis and preventing us from differentiating between a primary or repeat surgery.
In addition, data for this study was obtained from a large private insurance population in the United States and may not be representative of the US population as a whole or other medical insurers (for example, uninsured people or the Veterans’ Administrative Health System). As noted above, the population in this study was much wealthier than the US population as a whole and this difference needs to be considered when extrapolating the results beyond the cohort included in this database. Lastly, since billing codes do not include visual acuity, intraocular pressure, or keratometry results, we were not able to control for these variables.
In conclusion, corneal transplantation in keratoconus is decreasing in the United States. Future studies should be directed at evaluating the outcomes associated with the change in management patterns for keratoconus. Additional studies are also warranted to better understand how lower socioeconomic status impacts transplantation rates and the resultant outcomes.
Acknowledgments
Financial Support: National Institutes of Health K23 Award (1K23EY025729 - 01) and University of Pennsylvania Core Grant for Vision Research (2P30EY001583-41). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Additional funding was provided by Research to Prevent Blindness and the Paul and Evanina Mackall Foundation. Funding from each of the above sources was received in the form of block research grants to the Scheie Eye Institute. None of the organizations had any role in the design or conduction of the study
Footnotes
Conflicts of Interest: No conflicting relationship exists for any author.
Portions of the data used in this study have been submitted for presentation at the American Academy of Ophthalmology Annual Meeting in October 2016.
References
- 1.P Troutman RC, Lawless MA. Penetrating keratoplasty for keratoconus. Cornea. 1987;6:298–305. doi: 10.1097/00003226-198706040-00013. [DOI] [PubMed] [Google Scholar]
- 2.Lim L, Pesudovs K, Coster DJ. Penetrating keratoplasty for keratoconus: visual outcome and success. Ophthalmology. 2000;107:1125–31. doi: 10.1016/s0161-6420(00)00112-3. [DOI] [PubMed] [Google Scholar]
- 3.Parker JS, van Dijk K, Melles GR. Treatment options for advanced keratoconus: A review. Surv Ophthalmol. 2015;60:459–80. doi: 10.1016/j.survophthal.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Cunningham WJ, Brookes NH, Twohill HC, et al. Trends in the distribution of donor corneal tissue and indications for corneal transplantation: the New Zealand National Eye Bank Study 2000–2009. Clin Experiment Ophthalmol. 2012;40:141–7. doi: 10.1111/j.1442-9071.2011.02681.x. [DOI] [PubMed] [Google Scholar]
- 5.Keenan TD, Jones MN, Rushton S, et al. National Health Service Blood and Transplant Ocular Tissue Advisory Group and Contributing Ophthalmologists (Ocular Tissue Advisory Group Audit Study 8) Trends in the indications for corneal graft surgery in the United Kingdom: 1999 through 2009. Arch Ophthalmol. 2012;130:621–8. doi: 10.1001/archophthalmol.2011.2585. [DOI] [PubMed] [Google Scholar]
- 6.Ting DS, Sau CY, Srinivasan S, et al. Changing trends in keratoplasty in the West of Scotland: a 10-year review. Br J Ophthalmol. 2012;96:405–8. doi: 10.1136/bjophthalmol-2011-300244. [DOI] [PubMed] [Google Scholar]
- 7.Zare M, Javadi MA, Einollahi B, et al. Changing indications and surgical techniques for corneal transplantation between 2004 and 2009 at a tertiary referral center. Middle East Afr J Ophthalmol. 2012;19:323–9. doi: 10.4103/0974-9233.97941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coster DJ, Lowe MT, Keane MC, et al. A comparison of lamellar and penetrating keratoplasty outcomes: a registry study. Ophthalmology. 2014;121:979–87. doi: 10.1016/j.ophtha.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 9.Frigo AC, Fasolo A, Capuzzo C, et al. Corneal transplantation activity over 7 years: changing trends for indications, patient demographics and surgical techniques from the Corneal Transplant Epidemiological Study (CORTES) Transplant Proc. 2015;47:528–35. doi: 10.1016/j.transproceed.2014.10.040. [DOI] [PubMed] [Google Scholar]
- 10.Dobbins KR, Price FW, Jr, Whitson WE. Trends in the indications for penetrating keratoplasty in the midwestern United States. Cornea. 2000;19:813–6. doi: 10.1097/00003226-200011000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Lois N, Kowal VO, Cohen EJ, et al. Indications for penetrating keratoplasty and associated procedures, 1989–1995. Cornea. 1997;16:623–9. [PubMed] [Google Scholar]
- 12.Darlington JK, Adrean SD, Schwab IR. Trends of penetrating keratoplasty in the United States from 1980 to 2004. Ophthalmology. 2006;113:2171–5. doi: 10.1016/j.ophtha.2006.06.034. [DOI] [PubMed] [Google Scholar]
- 13.Woodward MA, Blachley TS, Stein JD. The Association Between Sociodemographic Factors, Common Systemic Diseases, and Keratoconus: An Analysis of a Nationwide Heath Care Claims Database. Ophthalmology. 2016;123:457–465. doi: 10.1016/j.ophtha.2015.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shtein RM, Raoof-Daneshvar D, Lin HC, et al. Keratoplasty for corneal endothelial disease, 2001–2009. Ophthalmology. 2012;119:1303–10. doi: 10.1016/j.ophtha.2012.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barnett M, Mannis MJ. Contact lenses in the management of keratoconus. Cornea. 2011;30:1510–6. doi: 10.1097/ICO.0b013e318211401f. [DOI] [PubMed] [Google Scholar]
- 16.Downie LE, Lindsay RG. Contact lens management of keratoconus. Clin Exp Optom. 2015;98:299–311. doi: 10.1111/cxo.12300. [DOI] [PubMed] [Google Scholar]
- 17.Kymes SM, Walline JJ, Zadnik K, et al. Collaborative Longitudinal Evaluation of Keratoconus Study Group Quality of life in keratoconus. Am J Ophthalmol. 2004;138:527–35. doi: 10.1016/j.ajo.2004.04.031. [DOI] [PubMed] [Google Scholar]
- 18.Gordon MO, Steger-May K, Szczotka-Flynn L, et al. Baseline factors predictive of incident penetrating keratoplasty in keratoconus. Am J Ophthalmol. 2006;142:923–30. doi: 10.1016/j.ajo.2006.07.026. [DOI] [PubMed] [Google Scholar]


