Abstract
Objectives
The HIV care cascade provides milestones to track the progress of HIV-positive people from seroconversion through viral suppression. We propose a Motivational PrEP Cascade involving five stages based upon the Transtheoretical Model of Change.
Methods
We analyzed data from 995 men in One Thousand Strong, a longitudinal study of a national panel of HIV-negative gay and bisexual men in the United States.
Results
Nearly all (89%) participants were sexually active in the past 3 months, and 65% met CDC criteria for PrEP candidacy. Of those identified as appropriate candidates, 53% were Precontemplative (Stage 1; unwilling to take or believing they were inappropriate candidates for PrEP) and 23% were in Contemplation (Stage 2; willing and self-identified as appropriate candidates). Only 11% were in PrEParation (Stage 3; seeing PrEP as accessible and planning to initiate PrEP) and 4% were in PrEP Action (Stage 4; prescribed PrEP). Although few of those who were identified as appropriate candidates were on PrEP, nearly all PrEP users (98%) reported adhering to 4 or more doses per week and most (72%) were returning for recommended quarterly medical visits, resulting in 9% of PrEP candidates reaching Maintenance and Adherence (Stage 5).
Conclusions
A large majority of participants were appropriate candidates for PrEP, yet fewer than 1 in 10 were using and adherent to PrEP. These findings highlight the need for interventions tailored to address the unique barriers men face at each stage of the cascade, particularly at the earliest stages where the most dramatic losses were identified.
Keywords: gay and bisexual men, Pre-exposure prophylaxis (PrEP), HIV prevention, continuum of care, PrEP cascade
Introduction
In 2012, Truvada (emtricitabine/tenofovir) was approved for use as pre-exposure prophylaxis (PrEP) to prevent HIV [1]. The Centers for Disease Control (CDC) subsequently recommended PrEP for anyone at high risk for HIV infection [2]. When taken as prescribed, PrEP is highly effective [3]. A recent demonstration study of gay, bisexual, and other men who have sex with men (GBMSM) found no new HIV infections during 388 person years of follow-up [4]. Despite effectiveness, uptake has been slow, and focus has shifted toward implementation issues and barriers to accessing and maintaining a PrEP regimen [5]. Studies have examined facilitators and barriers of PrEP uptake [6, 7]. Common facilitators include perceptions of risk for HIV infection, having a means of paying for PrEP (e.g., health insurance), and accurate knowledge of PrEP. Barriers include concerns about side effects, stigma, lack of access to a provider, and poor patient-provider communication [7–11]. The actual process of initiating and actively maintaining a PrEP regimen, however, is less well understood.
The HIV care cascade provides concrete, measurable milestones used to track the progress of people living with HIV from seroconversion to viral suppression [12]. Intervention efforts have been directed towards closing “gaps” in the HIV care cascade. Meaningful progress has been made, but more than 14% of HIV-positive people still do not know their status [13]. It was recently suggested that PrEP use may be examined through an analogous cascade [14]. Kelley et al. [15] proposed such a PrEP cascade involving five milestones: being at risk for HIV infection (e.g., sexually active GBMSM), awareness of PrEP and willingness to use it, access to healthcare, obtaining PrEP, and adherence [15]. Using a sample of non-Latino White and Black GBMSM in Atlanta, they estimated that only 15.2% of PrEP candidates would reach the last stage. However, the motivations for healthcare pre- and post-diagnosis are often different [16, 17], so motivations for PrEP uptake to prevent HIV infection are likely to be different from motivations for taking care of one’s health once diagnosed HIV-positive. The ultimate goal of the care cascade is to prevent HIV transmission. As such, a PrEP cascade attuned to issues associated with HIV infection (i.e., acquisition) and primary prevention may complement the care cascade. In fact, one desirable feature of a PrEP cascade is that its final step should overlap with the first step of the care cascade. That is, regular HIV testing as part of ongoing PrEP engagement should facilitate early diagnosis among PrEP users who seroconvert, thus placing individuals within the first step of the care cascade.
The current study proposes a Motivational PrEP cascade based on the Transtheoretical Model of Change, which conceptualizes behavior change in the context of decision making across time [18, 19], and has been used to explain HIV medication adherence and movement along the HIV care cascade [20, 21]. The PrEP cascade examined herein is pictured in Figure 1 and contains many components similar to those proposed by Liu and colleagues [22], which we have grouped into stages consistent with the stages of the Transtheoretical model. The cascade should only be applied to those objectively identified as appropriate candidates for PrEP, based on risk for HIV infection using established CDC criteria [2], making it ideal for targeting only those for whom prevention is needed at a given time. Those who do not view themselves as candidates for PrEP or are unwilling to pursue PrEP would be considered precontemplative (i.e., Stage 1). Those who see themselves as a PrEP candidate and are willing to take it, but have no means or plans to do so are in contemplation (Stage 2). Individuals with a means of obtaining PrEP, making plans to initiate PrEP, but not yet prescribed PrEP are in preparation (Stage 3). Once individuals have spoken to their medical provider about PrEP and obtained a prescription, they are in action (Stage 4), as they have made a quantifiable effort to decrease their HIV risk. Finally, individuals are in maintenance (Stage 5) when they are consistently adhering to PrEP based on data suggesting a minimum of 4 doses per week [23] and following guidelines regarding quarterly HIV and STI testing [2]. Discontinuation of PrEP at any time should lead to regular re-assessment of risk and appropriateness of PrEP and an HIV-positive diagnosis at any time leads directly into the HIV Treatment Cascade—individuals consistently at low risk will never enter the HIV PrEP Cascade whereas those who transition in and out of risk will enter the cascade during times when PrEP is objectively indicated for them.
Figure 1.
This figure displays a flowchart of the stepped nature of the Motivational PrEP Cascade. The cascade begins with objective identification, which includes HIV testing and an assessment of HIV risk behavior—individuals for whom PrEP is indicated continued into the PrEP cascade whereas individuals for whom it is not indicated should be regularly reassessed and individuals who test HIV-positive should proceed to the HIV Treatment Cascade. Within the PrEP Cascade, individuals can move forwards and backwards from different stages and remain within the stages of the cascade as long as PrEP remains indicated.
The cascade we propose is distinct in several ways from the previously published PrEP cascade [15]. First, a precursor to entry into our cascade is objective identification as an appropriate PrEP candidate. Although it is possible that other men can be prescribed PrEP, particularly if requested, the inclusion of all sexually active GBMSM in the cascade can be detrimental because it overestimates the pool of individuals for whom PrEP is medically indicated, thus underestimating any success at reaching those most in need. Objective indicators of risk were considered within the previous cascade, though it was done within the third step when examining who was most likely to receive a PrEP prescription. Second, although our last two stages are similar to those of the previously published cascade, we consider three distinct stages of movement toward receiving a prescription that we believe better highlight unique processes acting as barriers to uptake. Finally, our use of a validated model of health behavior widely used in HIV prevention allows the proposed cascade to be translated easily into interventions targeted to specific issues associated with each motivational stage.
In addition to distinctions between the two cascades themselves, this study differs in significant ways from the previous—and important—work that has already been done [15]. The current study provides data from a national sample of GBM of all racial and ethnic backgrounds. As a result, the data provide useful insights into the cascade as it appears within the national rather than a local epidemic. Kelley et al. [15] used data from previous research to estimate the number of men expected to reach several steps along the continuum. For example, they estimate the proportion of men who would be adherent based on iPrEx data [24]. However, estimates based on those randomly assigned to receive PrEP or placebo may differ dramatically from those among men who seek out PrEP already aware of its high efficacy.
Utilizing data collected in the second half of 2015 from One Thousand Strong, a longitudinal panel study of HIV-negative GBM across the U.S., we examined the number of men who would be appropriate PrEP candidates, how many of them reach each stage of the Motivational PrEP Cascade, and end with a comparison of racial/ethnic and geographic differences.
Methods
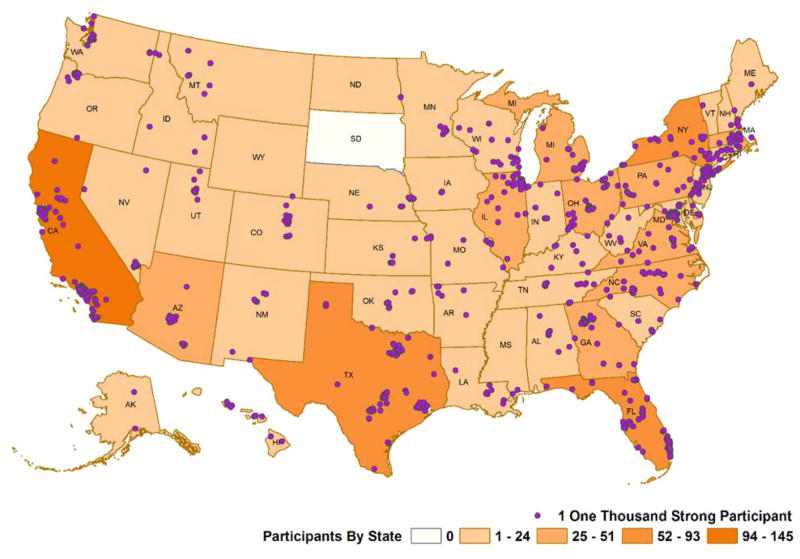
One Thousand Strong is a longitudinal study prospectively following a national panel of HIV-negative GBM for three years; specifics regarding recruitment and enrollment procedures are detailed elsewhere [25]. The sample was recruited to reflect census data on same-sex households in terms of racial and ethnic composition, age, and geographic distribution—the geographic distribution of the entire cohort at baseline can be found in Figure 2. Following consent, as part of the baseline assessment, participants completed an online survey, at-home self-administered rapid HIV testing, and sent in self-collected samples for urethral and rectal chlamydia/gonorrhea; all those enrolled had a confirmed HIV-negative test result [26]. These procedures are repeated every 12 months; data for this manuscript were taken from the 12-month follow-up. All procedures were approved by the Institutional Review Board of CUNY.
Figure 2.
This figure displays the geographic distribution of the full One Thousand Strong cohort at the time of baseline enrollment. Participants were targeted to represent the geographic distribution of same-sex households in the census.
Of the 1,071 men who enrolled, 5 men (0.5%) reported an HIV diagnosis in the year since baseline and were excluded. Of the remaining 1,066, 1,013 (95.0%) completed the 12-month survey. Men who had formerly been prescribed PrEP but were no longer (n = 18) were asked different questions and were not included within the present analyses, resulting in a final analytic sample of 995 HIV-negative GBM.
Measures
All PrEP questions were preceded by a standard description of PrEP [27]. Men reported on 10 processes involved in the Motivational PrEP Cascade. Processes were divided into 5 stages with 2 processes in each stage (Table 1). “Reaching” a stage involved meeting criteria for both processes. Stages were ordered so that a participant must have reached earlier stages in order to reach subsequent stages.
Table 1.
Overall progression through each stage of the Motivational PrEP Cascade
| Full Sample (N = 995)
|
||
|---|---|---|
| n | % | |
| Objective Identification | 636 | 63.9 |
| HIV-Negative and Sexually Active with Men | 887 | 89.1 |
| PrEP Candidate Using Modified CDC Criteria | 642 | 64.5 |
| Stage 2: PrEP Contemplation | 301 | 47.3 |
| Stage 2a: Willing to Take PrEP | 419 | 65.9 |
| Stage 2b: Self-Identified as PrEP Candidate | 346 | 54.4 |
| Stage 3: PrEParation | 152 | 50.5 |
| Stage 3a: Has Potential PrEP Provider | 244 | 81.1 |
| Stage 3b: Intending to Take PrEP | 173 | 57.5 |
| Stage 4: PrEP Action and Initiation | 82 | 53.9 |
| Stage 4a: Spoken to a Medical Provider about PrEP | 107 | 70.4 |
| Stage 4b: Currently Prescribed PrEP | 82 | 53.9 |
| Stage 5: PrEP Maintenance and Adherence | 58 | 70.7 |
| Stage 5a: Maintaining 4+ Doses per Week | 80 | 97.6 |
| Stage 5b: Returning for Quarterly Testing | 59 | 72.0 |
Note. Each stage contains only those men who met the criteria for the prior stage. Stage 1 is not shown as it contains all those individuals who are objectively identified and do not reach Stage 2.
Demographic characteristics
Participants were asked whether or not they were Hispanic/Latino and separately asked to report their race using definitions consistent with reporting of the National Institutes of Health. Men who reported multiple racial identities were coded as multiracial, men who reported one racial identity and being Hispanic or Latino were coded as Latino, and men who reported one racial identity and not being Hispanic or Latino were coded as that racial identity. Zip codes were utilized to classify men into the geographic regions in which they lived.
Objective identification
Participants were considered to have met objective criteria for being an appropriate PrEP candidate if they were HIV-negative, sexually active with men, and met CDC criteria [2]. All men in the sample were HIV-negative and sexually active with men in the 12 months prior to baseline, though we used sexual activity with another man in the past 3 months (compared with the CDC’s 6-month criteria) as the criterion for objective identification. Men were considered candidates if they: (1) were in a relationship with a partner not known to be HIV-negative; (2) were in a non-monogamous relationship; (3) had any sex with a casual male partner not known to be HIV-negative in the prior 3 months; (4) had any condomless anal sex with a casual male partner regardless of status in the prior 3 months; or (5) had a positive STI diagnosis within the prior 6 months. We included both self-reported diagnoses as well as the testing for urethral and rectal gonorrhea and chlamydia conducted as part of the 12-month assessment; 49 men (4.9%) did not complete the 12-month STI testing and we used self-report data alone.
Stage 1: PrEP precontemplation
Men were considered to have met criteria for this stage if they were objectively identified but did not meet the criteria for Stage 2.
Stage 2: PrEP contemplation
To assess willingness to take PrEP (Stage 2a), men were asked, “Suppose that PrEP is at least 90% effective in preventing HIV when taken daily. How likely would you be to take PrEP if it were available for free?” with responses ranging from “I would definitely take it” to “I would definitely not take it;” those indicating they would probably or definitely take PrEP were coded as willing to take it. To assess self-identification as a PrEP candidate (Stage 2b), men were asked “Do you believe that you are currently an appropriate candidate for PrEP?” with responses ranging from “Yes, I am definitely an appropriate candidate” to “No, I am definitely not an appropriate candidate;” those indicating themselves as probably or definitely appropriate candidates were coded as self-identifying as PrEP candidates.
Stage 3: PrEParation
Men were asked, “Suppose that you were interested in getting a new prescription for PrEP – do you have or know of a medical provider who you think would be willing to prescribe it for you?” (Stage 3a). To assess intentions for PrEP uptake, men were asked, “PrEP is currently available with a prescription from your doctor and research has shown that a majority of insurance companies cover most or all of the costs of PrEP. Do you plan to begin PrEP?” Response options ranged from “Yes, I will definitely begin taking PrEP” to “No, I definitely will not begin taking PrEP;” those indicating they would probably or definitely begin taking PrEP were coded as intending to begin PrEP.
Stage 4: PrEP action and initiation
Men were asked, “Have you ever spoken to a medical provider about starting PrEP?” (Stage 4a) and, “Have you ever been prescribed HIV medications (e.g., Truvada) for use as PrEP?” (Stage 4b).
Stage 5: PrEP maintenance and adherence
To assess optimal adherence of an average of 4 or more doses a week (Stage 5a), men on PrEP were asked, “In the last month (30 days), on how many days did you miss a dose of PrEP?” with responses fewer than 13 coded as having maintained sufficient adherence. Men were also asked, “How regularly do you return to the medical provider who prescribes you PrEP to receive HIV/STI testing?” with responses other than “At least 4 times per year (every 3 months)” coded as not returning for quarterly visits (Stage 5b).
Results
Overall, the sample was 7.6% Black, 12.1% Latino, 72.2% White, and 8.1% identified as another race or multiracial. The majority was gay-identified (95%) and had a 4-year college degree (58.7%). Nearly half (47.1%) made $50,000 per year or more. The average age was 41.9 years (Mdn = 40.0, SD = 13.9). More than one-third (n = 349, 35.1%) resided in the South, 19.3% (n = 192) in the Northeast, 18.2% (n = 182) in the Midwest, and 27.3% (n = 272) in the West. The online supplementary material contains a detailed map of the locations of our sample.
Table 1 shows the progression through each of the five stages of the PrEP cascade. As can be seen, 89.1% were sexually active (Stage 1a) and 64.5% met CDC criteria for PrEP candidacy (Stage 1b). Thus, nearly two-thirds (63.9%) met our criteria for “objective identification” as PrEP candidate. However, more than half (52.7%) did not move on to Stage 2, and were Precontemplative for PrEP uptake. The remaining 47.3% reached PrEP Contemplation (Stage 2); 54.4% self-identified as a PrEP candidate (Stage 2a) and 65.9% indicated willingness to take PrEP (Stage 2b). Among Contemplators, 81.1% had a provider willing to prescribe PrEP (Stage 3a) and 57.5% had a plan to begin taking PrEP (Stage 3b). Of those in PrEParation, 70.4% had spoken to a provider (Stage 4a) and 53.9% were currently prescribed PrEP (Stage 4b). Nearly all of those in the Action stage (97.6%) reported taking an average of 4 or more doses per week (Stage 5a) and most (72.0%) were attending recommended quarterly medical visits (Stage 5c).
Following objective identification within Stage 1, Table 1 shows that approximately half of men who reached the prior stage were lost at Stages 2 through 4, though more of the men stay actively engaged in PrEP within Stage 5 if they reached Stage 4. Figure 3 depicts the number and percentage of men objectively identified who reached each stage (as opposed to Table 1 which displays these as percentages of those who reached the former step). As can be seen, fewer than half reached Stage 2, fewer than one-quarter reached Stage 3, 12.9% reached Stage 4 and were on PrEP, and fewer than 1 in 10 of these men were benefiting from the efficacious HIV preventive effects of a PrEP regimen.
Figure 3.
The above figure displays the proportion of gay and bisexual men who were classified as being within each stage of the cascade. Unlike Table 1 which displays the proportion who reached each stage of those who reached the former stage, Figure 3 indicates the proportion for whom that was the final stage reached of all those who were objectively identified as PrEP candidates (n = 636).
Table 2 displays results of a series of chi-square tests comparing racial/ethnic groups and geographic regions in the extent to which they achieved each stage of the PrEP cascade. We found no significant racial/ethnic or geographic differences in any of the first four stages of the cascade and were unable to test the last stage due to such low numbers within each cell.
Table 2.
Comparisons of progression through the PrEP Cascade by race/ethnicity and region of residence.
| Racial/Ethnic Comparisons
|
χ2(3) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Black (n = 76)
|
Latino (n = 120)
|
White (n = 718)
|
Other (n = 81)
|
||||||
| n | % | n | % | n | % | n | % | ||
| Stage 1: Objective Identification (Precontemplation) | 47 | 61.8 | 74 | 61.7 | 460 | 64.1 | 55 | 67.9 | 0.97 |
| Stage 2: PrEP Contemplation | 28 | 59.6 | 39 | 52.7 | 207 | 45.0 | 27 | 49.1 | 4.75 |
| Stage 3: PrEParation | 11 | 39.3 | 18 | 46.2 | 108 | 52.2 | 15 | 55.6 | 2.21 |
| Stage 4: PrEP Action and Initiation | 5 | 45.5 | 9 | 50.0 | 62 | 57.4 | 6 | 40.0 | 2.13 |
| Stage 5: PrEP Maintenance and Adherence a | 4 | 80.0 | 5 | 55.6 | 44 | 71.0 | 5 | 83.3 | -- |
| Regional Comparisons
|
χ2(3) | ||||||||
| Northeast (n = 192)
|
Midwest (n = 182)
|
South (n = 349)
|
West (n = 272)
|
||||||
| n | % | n | % | n | % | n | % | ||
|
| |||||||||
| Stage 1: Objective Identification (Precontemplation) | 132 | 68.8 | 110 | 60.4 | 222 | 63.6 | 172 | 63.2 | 2.97 |
| Stage 2: PrEP Contemplation | 60 | 45.5 | 51 | 46.4 | 112 | 50.5 | 78 | 45.3 | 1.37 |
| Stage 3: PrEParation | 32 | 53.3 | 23 | 45.1 | 58 | 51.8 | 39 | 50.0 | 0.87 |
| Stage 4: PrEP Action and Initiation | 20 | 62.5 | 13 | 56.5 | 27 | 46.6 | 22 | 56.4 | 2.38 |
| Stage 5: PrEP Maintenance and Adherence a | 15 | 75.0 | 8 | 61.5 | 23 | 85.2 | 12 | 54.5 | -- |
Note:
Fisher’s exact test was used for these calculations due to small sample size and both had non-significant p-values.
Discussion
These findings illustrate the utility of a Motivational PrEP Cascade for GBM informed by the Transtheoretical Model of Change. The frequency of participants reaching each of the stages decreased across the cascade in a manner suggesting that they capture motivation to engage in PrEP consistent with this model. Arguably the most striking finding is the dramatic loss of participants across the early stages of the Motivational PrEP Cascade. Interpreting Figure 3 in terms of the final stage that men reached, 53% remained at Stage 1 (Precontemplation), 23% in Stage 2 (Contemplation), 11% in Stage 3 (PrEParation), 4% in Stage 4 (Action), and 9% reached Stage 5 (Maintenance).
These results underscore the importance of barriers to PrEP encountered in early and intermediate stages. In conceptualizing the transition from Precontemplation through Contemplation and PrEParation, the distinction between willingness versus intentions or opportunity emerged as a critical aspect of the Motivational PrEP Cascade based on earlier work [27]. Not all GBM who were open (i.e. willing; a Contemplation stage process) to the idea of PrEP intended to utilize it (a PrEParation stage process). Similarly, not all men with access to a PrEP provider (a PrEParation stage process) had actually spoke to their provider about PrEP (an Action stage process).
Compared to the previously published PrEP cascade which estimated large losses in the final stages [15], our results suggests these losses largely occur in earlier stages. As mentioned, these cascades differ both theoretically and methodologically, which may account for the differences. First, drawing from the Transtheoretical Model, the Motivational PrEP Cascade identified a wider range of processes involved in the progression to PrEP adherence. Kelley et al. began their cascade with Awareness/Willingness, which is most consistent with our second stage (Contemplation). We propose a precursor stage (Precontemplation) in which individuals are appropriate candidates for PrEP but unwilling to consider PrEP. We found 64% of GBM were appropriate PrEP candidates, though only 47% of those were willing to consider PrEP.
Our results also illustrate that intentions to access PrEP served as a greater barrier to achieving the PrEParation stage. Among the 301 GBM who completed both processes in the Contemplation stage (meaning they were willing to take PrEP and believed they were an appropriate candidate), the majority (81%) reported having access to a PrEP provider, though fewer (57.5%) reported intentions to begin PrEP. The incorporation of the motivational concept of “intentions” in this stage identifies a potentially critical point of intervention to enhance PrEP uptake [27]. Providers could consider a decisional balance exercise of the pros and cons of PrEP uptake [28, 29]. This technique, often utilized in motivational interviewing-based interventions, helps to consider short- and long-term benefits and drawbacks of behavior change (in this case, PrEP uptake), and has been shown to increase behavioral intentions [30, 31] and behavior change in a variety of relevant behaviors, including HIV medication adherence [32].
By distinguishing between those who have spoken to a provider about PrEP and those who are currently prescribed PrEP (two components of Step 4, Action), the Motivational PrEP Cascade highlights specific communication barriers to PrEP which should not be overlooked in understanding movement along the stages of PrEP uptake. Nearly a third of GBM intending to use PrEP had talked to their provider. Furthermore, nearly a quarter of participants who spoke to their provider did not obtain a PrEP prescription despite data indicating they are appropriate candidates for PrEP.
In contrast to the previous study of Black and White GBMSM in Atlanta [15] that estimated progression through many of their stages, the present study reported data observed from a national sample of GBM. This distinction is most critical when examining findings in these two studies. We found that the majority (80%) of our participants on PrEP reported an average of 4 or more doses per week and most (72%) returned for quarterly testing (compared to the previously published cascade study that estimated 51% of those likely to be prescribed PrEP would be adherent based on iPrEx results). It is likely that rates of PrEP adherence will be higher than that of HIV medications for HIV-positive persons. Truvada is a once-daily standalone pill, whereas HIV treatment often requires multiple medications. In addition, taking HIV medication as an HIV-positive person is often associated with stigma, reminders of being “infected,” and concerns about transmitting HIV to sexual partners [33, 34] – all of which has been associated with adherence challenges [35]. Adherence to PrEP, however, is about self-protection, and may be interpreted by some GBM as enabling them to engage in sexual activity without fear of infection [36].
We found no significant racial and ethnic differences, nor significant geographic differences in Motivational PrEP Cascade milestones. Kelley et al. [15] found that Black GBMSM faced greater barriers to navigating the PrEP cascade compared to White men in Atlanta, and a recent Los Angeles study found that Black GBMSM had higher awareness of PrEP than Hispanic GBMSM [37]. It is entirely plausible that real disparities exist within local areas and geographic regions even if such differences are not observed (or are more modest) at the national level. Over-sampling of racial and ethnic minority individuals may increase sensitivity to detect potential differences.
Limitations
These results should be considered in light of their limitations. Although the sampling was designed to reflect the distribution of census data on same-sex households, this led to a large majority being White GBM. We used CDC criteria to determine whether men were appropriate candidates for PrEP, though our sexual behavior data were based on three rather than six months, thus potentially underestimating the number of appropriate candidates. Some participants were missing STI testing data and we relied solely on self-report, and we were also unable to include those who had been formerly prescribed PrEP due to incomplete data on the questions of interest.
Conclusions
These results suggest that a comprehensive intervention strategy which employs policy, public health, and individual-level components will be necessary to achieve adequate PrEP uptake among GBMSM. The most dramatic losses within the cascade occurred at the first three stages, and both structural and individual intervention strategies at each level may help to address these losses. At the Contemplation stage, strategies that enhance awareness of criteria for PrEP candidacy may enhance self-identification and increase receptivity to the idea of PrEP. At the PrEParation stage, interventions that improve access to providers who can prescribe PrEP and facilitate planning to initiate PrEP may be most applicable. At the Action and Maintenance stages, interventions may need to target both providers and GBMSM. Programs that enhance provider knowledge and confidence in prescribing PrEP and patient comfort in discussing issues of sexuality and risk may help to ensure PrEP access among those for whom it is indicated.
Acknowledgments
This work was supported by research grants from the National Institute on Drug Abuse of the National Institutes of Health (grant numbers R01-DA036466 to JTP and CG, K01-DA039030 to HJR). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors would like to acknowledge the contributions of the other members of the One Thousand Strong study team (Ana Ventuneac, Demetria Cain, Mark Pawson, Ruben Jimenez, Chloe Mirzayi, Brett Millar, and Raymond Moody) and other staff from the Center for HIV/AIDS Educational Studies and Training (Chris Hietikko, Andrew Cortopassi, Brian Salfas, Doug Keeler, Qurrat-Ul Ain, Chris Murphy, and Carlos Ponton). We would also like to thank the staff at Community Marketing Inc. (David Paisley, Heather Torch, and Thomas Roth) as well as Patrick Sullivan, Jessica Ingersoll, Deborah Abdul-Ali, and Doris Igwe at the Emory Center for AIDS Research (P30 AI050409). Finally, we thank Jeffrey Schulden and Pamela Goodlow at NIDA, and all of our participants in the One Thousand Strong study.
Footnotes
Author Contributions: J.T.P, H.J.R, T.J.S., and C.G. were involved in the conception, design, and implementation of the project; J.M.L. and T.H.F.W. were involved in the acquisition of data; H.J.R. and J.T.P. were involved in the analysis and interpretation of data. All authors contributed to article writing and critical revisions of intellectual content. All authors reviewed a final version of the article and approved it for submission.
Conflicts of interest: None of the authors have conflicts of interest to disclose.
References
- 1.USFDA. FDA approves first drug for reducing the risk of sexually acquired HIV infection. 2012. [Google Scholar]
- 2.CDC. Preexposure prophylaxis for the prevention of HIV infection in the United States - 2014 A clinical practice guideline. 2014. [Google Scholar]
- 3.Spinner CD, Boesecke C, Zink A, Jessen H, Stellbrink H-J, Rockstroh JK, et al. HIV pre-exposure prophylaxis (PrEP): a review of current knowledge of oral systemic HIV PrEP in humans. Infection. 2015:1–8. doi: 10.1007/s15010-015-0850-2. [DOI] [PubMed] [Google Scholar]
- 4.Volk JE, Marcus JL, Phengrasamy T, Blechinger D, Nguyen DP, Follansbee S, et al. No new HIV infections with increasing use of HIV preexposure prophylaxis in a clinical practice setting. Clin Infect Dis. 2015;61:1601–1603. doi: 10.1093/cid/civ778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marcus JL, Volk JE, Pinder J, Liu AY, Bacon O, Hare CB, et al. Successful Implementation of HIV Preexposure Prophylaxis: Lessons Learned From Three Clinical Settings. Current HIV/AIDS Reports. 2016:1–9. doi: 10.1007/s11904-016-0308-x. [DOI] [PubMed] [Google Scholar]
- 6.Grov C, Whitfield TH, Rendina HJ, Ventuneac A, Parsons JT. Willingness to Take PrEP and Potential for Risk Compensation Among Highly Sexually Active Gay and Bisexual Men. AIDS Behav. 2015:1–11. doi: 10.1007/s10461-015-1030-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilton J, Senn H, Sharma M, Tan DHS. Pre-exposure prophylaxis for sexually-acquired HIV risk management: a review. HIV/AIDS (Auckland, NZ) 2015;7:125–136. doi: 10.2147/HIV.S50025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krakower D, Ware N, Mitty JA, Maloney K, Mayer KH. HIV providers’ perceived barriers and facilitators to implementing pre-exposure prophylaxis in care settings: a qualitative study. AIDS Behav. 2014;18:1712–1721. doi: 10.1007/s10461-014-0839-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eaton LA, Driffin DD, Bauermeister J, Smith H, Conway-Washington C. Minimal Awareness and Stalled Uptake of Pre-Exposure Prophylaxis (PrEP) Among at Risk, HIV-Negative, Black Men Who Have Sex with Men. AIDS Patient Care STDS. 2015 doi: 10.1089/apc.2014.0303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ayala G, Makofane K, Santos G-M, Beck J, Do TD, Hebert P, et al. Access to basic HIV-related services and PrEP acceptability among men who have sex with men worldwide: barriers, facilitators, and implications for combination prevention. Journal of Sexually Transmitted Diseases. 2013;2013 doi: 10.1155/2013/953123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Calabrese SK, Underhill K. How Stigma Surrounding the Use of HIV Preexposure Prophylaxis Undermines Prevention and Pleasure: A Call to Destigmatize “Truvada Whores”. American Journal of Public Health. 2015;105:1960–1964. doi: 10.2105/AJPH.2015.302816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.CDC. HIV stages of care. Atlanta, GA: 2014. [Google Scholar]
- 13.CDC. Vital signs: HIV diagnosis, care, and treatment among persons living with HIV — United States, 2011. Atlanta, GA: 2014. [PMC free article] [PubMed] [Google Scholar]
- 14.McNairy ML, El-Sadr WM. Antiretroviral therapy for the prevention of HIV transmission: what will it take? Clinical Infectious Diseases. 2014;58:1003–1011. doi: 10.1093/cid/ciu018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kelley C, Kahle E, Siegler A, Sanchez T, del Rio C, Sullivan P, et al. Applying a PrEP continuum of care for men who have sex with men in Atlanta, Georgia. Clinical Infectious Diseases. 2015;61:1590–1597. doi: 10.1093/cid/civ664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jayanti RK, Burns AC. The antecedents of preventive health care behavior: An empirical study. Journal of the Academy of Marketing Science. 1998;26:6–15. [Google Scholar]
- 17.Moorman C, Matulich E. A Model of Consumers’ Preventive Health Behaviors: The Role of Health Motivation and Health Ability. Journal of Consumer Research. 1993;20:208–228. [Google Scholar]
- 18.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 19.Velicer WF, Prochaska JO, Fava JL, Norman GJ, Redding CA. Smoking cessation and stress management: Applications of the transtheoretical model of behavior change. Homeost Health Dis. 1998;38:216–233. [Google Scholar]
- 20.Genberg BL, Lee Y, Rogers WH, Willey C, Wilson IB. Stages of Change for Adherence to Antiretroviral Medications. AIDS Patient Care and STDs. 2013;27:567–572. doi: 10.1089/apc.2013.0126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Longmire-Avital B, Golub SA, Parsons JT. Self-Reevaluation as a Critical Component in Sustained Viral Load Change for HIV+ Adults with Alcohol Problems. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 2010;40:176–183. doi: 10.1007/s12160-010-9194-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu A, Colfax G, Cohen S, Bacon O, Kolber M, Amico KR, et al. The Spectrum of Engagement in HIV Prevention: Proposal for a PrEP cascade. International Conference on HIV Treatment and Prevention Adherence; Miami, FL. 2012. [Google Scholar]
- 23.Anderson PL, Glidden DV, Liu A, Buchbinder S, Lama JR, Guanira JV, et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. 2012;4:151ra125–151ra125. doi: 10.1126/scitranslmed.3004006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amico K, Liu A, McMahan V, Anderson P, Lama J, Guanira J, et al. Adherence indicators and pre-exposure prophylaxis (PrEP) drug levels in the iPrEx study. 18th Conference on Retroviruses and Opportunistic Infections; 2011. [Google Scholar]
- 25.Grov C, Cain D, Whitfield TH, Rendina HJ, Pawson M, Ventuneac A, et al. Recruiting a US National sample of HIV-negative gay and bisexual men to complete at-home self-administered HIV/STI testing and surveys: challenges and opportunities. Sexuality Research and Social Policy. 2016;13:1–21. doi: 10.1007/s13178-015-0212-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grov C, Cain D, Rendina HJ, Ventuneac A, Parsons JT. Characteristics Associated With Urethral and Rectal Gonorrhea and Chlamydia Diagnoses in a US National Sample of Gay and Bisexual Men: Results From the One Thousand Strong Panel. Sex Transm Dis. 2016;43:165–171. doi: 10.1097/OLQ.0000000000000410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rendina HJ, Whitfield THF, Grov C, Starks TJ, Parsons JT. Distinguishing hypothetical willingness from behavioral intentions to initiate HIV pre-exposure prophylaxis (PrEP): Findings from a large cohort of gay and bisexual men in the U.S. Soc Sci Med. 2016 doi: 10.1016/j.socscimed.2016.10.030. published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Apodaca TR, Longabaugh R. Mechanisms of change in motivational interviewing: a review and preliminary evaluation of the evidence. Addiction. 2009;104:705–715. doi: 10.1111/j.1360-0443.2009.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prochaska JO, Velicer WF, Rossi JS, Goldstein MG, Marcus BH, Rakowski W, et al. Stages of change and decisional balance for 12 problem behaviors. Health Psychol. 1994;13:39. doi: 10.1037//0278-6133.13.1.39. [DOI] [PubMed] [Google Scholar]
- 30.Parsons JT, Halkitis PN, Bimbi DS, Borkowski T. Perceptions of the benefits and costs associated with condom use and unprotected sex among late adolescent college students. J Adolesc. 2000;23:377–397. doi: 10.1006/jado.2000.0326. [DOI] [PubMed] [Google Scholar]
- 31.Parsons JT, Lelutiu-Weinberger C, Botsko M, Golub SA. A randomized controlled trial utilizing motivational interviewing to reduce HIV risk and drug use in young gay and bisexual men. J Consult Clin Psychol. 2014;82:9. doi: 10.1037/a0035311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.MacDonell KE, Naar-King S, Murphy DA, Parsons JT, Harper GW. Predictors of medication adherence in high risk youth of color living with HIV. J Pediatr Psychol. 2009:jsp080. doi: 10.1093/jpepsy/jsp080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mahajan AP, Sayles JN, Patel VA, Remien RH, Ortiz D, Szekeres G, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS (London, England) 2008;22:S67. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rintamaki LS, Davis TC, Skripkauskas S, Bennett CL, Wolf MS. Social stigma concerns and HIV medication adherence. AIDS Patient Care & STDs. 2006;20:359–368. doi: 10.1089/apc.2006.20.359. [DOI] [PubMed] [Google Scholar]
- 35.Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. Journal of the International AIDS Society. 2013:16. doi: 10.7448/IAS.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brooks RA, Landovitz RJ, Kaplan RL, Lieber E, Lee S-J, Barkley TW. Sexual risk behaviors and acceptability of HIV pre-exposure prophylaxis among HIV-negative gay and bisexual men in serodiscordant relationships: a mixed methods study. AIDS patient care and STDs. 2012;26:87–94. doi: 10.1089/apc.2011.0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Davey DJ, Bustamante MJ, Wang D, Young S, Klausner JD. PrEP Continuum of Care for MSM in Atlanta and Los Angeles County. Clinical Infectious Diseases. 2016;62:402–403. doi: 10.1093/cid/civ890. [DOI] [PubMed] [Google Scholar]