Abstract
Objective
The aim of this study was to investigate whether post-hospital syndrome (PHS) places patients undergoing elective hernia repair at increased risk for adverse postoperative events.
Summary of Background Data
PHS is a transient period of health vulnerability following inpatient hospitalization for acute illness. PHS has been well studied in nonsurgical populations, but its effect on surgical outcomes is unclear.
Methods
State-specific datasets for California in 2011 available through the Healthcare Cost and Utilization Project (HCUP) were linked. Patients older than 18 years who underwent elective hernia repair were included. The primary exposure variable was PHS, defined as any inpatient admission within 90 days of an elective hernia repair performed in an ambulatory surgery center. The primary outcome was an adverse event, defined as any unplanned emergency department visit or inpatient admission within 30 days postoperatively. Mixed-effects logistic models were used for multivariable analyses.
Results
A total of 57,988 patients met inclusion criteria. The 30-day risk-adjusted adverse event rate was significantly higher for PHS patients versus non-PHS patients (11.8% vs 5.8%, P < 0.001). PHS patients were more likely than non-PHS patients to experience postoperative complications (odds ratio 2.2, 95% confidence interval 1.6–3.0). Adverse events attributable to PHS cost an additional $63,533.46 per 100 cases in California. The risk of adverse events due to PHS remained elevated throughout the 90-day window between hospitalization and surgery.
Conclusions
Patients hospitalized within 90 days of an elective surgery are at increased risk of adverse events postoperatively. The impact of PHS on outcomes is independent of baseline patient characteristics, medical comorbidities, quality of center performing the surgery, and reason for hospitalization before elective surgery. Adverse events owing to PHS are costly and represent a quality improvement target.
Keywords: ambulatory surgery, elective hernia repair, post-hospital syndrome
Post-hospital syndrome (PHS) is a transient period of health vulnerability following hospitalization for acute illness. PHS is characterized by the risk of early re-hospitalization towing to physiologic stressors from the initial admission, including disruption in sleep-wake cycles, inadequate pain control, deconditioning, and changes in nutritional status.1,2 Nearly 20% of Medicare patients discharged from a hospital are readmitted within 30 days with an acute medical problem, many of which are unrelated to the initial diagnosis.1 Additionally, PHS has been shown to coincide with high rates of readmission in Medicare patients initially hospitalized for heart failure, acute myocardial infarction, or pneumonia,3 as well as with generally higher risk for adverse events for these patients in the year following hospitalization compared to the elderly general population.4
It is unclear whether PHS impacts postoperative outcomes in patients undergoing elective surgical procedures. Readmissions after inpatient surgery generally have been associated with postdischarge complications related to the procedure as opposed to exacerbations of complications during a previous hospitalization.5 For patients undergoing surgery in the ambulatory surgical setting, acute care revisits are not uncommon and represent a potential quality improvement target.5
Although there are known risk factors for hospital admission after ambulatory surgery,7,8 more work is needed to determine whether PHS influences adverse event rates after low-risk, elective surgery. For example, does an inpatient admission within 90 days of elective, outpatient surgery increase the risk of adverse postoperative events? Should patients recently discharged from the hospital, and therefore currently in a vulnerable state, undergo elective, ambulatory surgery?We sought to determine whether PHS is an unrealized or previously unmeasured risk to patients undergoing elective surgery in ambulatory surgery centers (ASCs).
Methods
Data Source
We used the entire spectrum of datasets for the state of California available through the Healthcare Cost and Utilization Project (HCUP) to follow patients through inpatient, ambulatory surgical, and emergency department visits. The Agency of Health Research and Quality (AHRQ) sponsored the development of HCUP to inform health-related decisions.6 Data are deidentified, protected, and include >100 clinical and nonclinical variables.
The specific datasets used were the State Inpatient Database (SID), which includes all patient discharge records for all payers, the State Ambulatory Surgical and Services Database (SASD), which provides encounter-level data for ambulatory surgery and other outpatient services from hospital-owned facilities, and the State Emergency Department Database (SEDD), which captures discharge information on all emergency department visits that do not result in an admission.
Patient Inclusion
Patients were identified using HCUP SASD in the state of California for the year 2011. The Clinical Classification Software (CCS) for International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM), was used to define the population of interest. CCS is a categorization tool developed as part of HCUP to collapse >3900 ICD-9-CM procedure codes into clinically meaningful categories to facilitate research.7 Any patient 18 years or older who underwent an elective hernia repair (CCS codes 85 and 86) was included for study.
Encounters identified in HCUP SASD were then linked to the HCUP SID and HCUP SEDD. This allowed identification of patients with previous inpatient admissions and inpatient or emergency department visits following their surgery. Patients with multiple encounters in the SASD with the same CCS code were excluded to ensure our evaluation of patients with a single operation.
Exposure and Outcome Variables
Following previous literature,4 the primary exposure variable of PHS was defined as any inpatient admission within 90 days of an elective hernia repair performed in an ASC. The primary outcome of interest was an adverse event, defined as any unplanned emergency department visit or inpatient admission within 30 days postoperatively. Type of adverse event was mapped from CCS codes to corresponding ICD-9-CM diagnosis chapters based on the primary reason for requiring postoperative acute care. Supplementary Figure 1, http://links.lww.com/SLA/B85 is a graphical schematic of the study design.
Elective hernia repair was selected as a representative operation to study PHS because it is a commonly performed operation by general surgeons in multiple healthcare environments. Additionally, in the elective setting, it is a low-risk operation that should be associated with minimal morbidity. As a result, we considered any unplanned emergency department or inpatient admission to be an adverse event following surgery.
Analytic Approach
Descriptive statistics are reported with arithmetic means (standard deviation), medians (interquartile range), or frequencies (proportions). Parametric univariate statistical testing for comparisons between groups was done using t tests or chi-square tests.
Multilevel, mixed-effects logistic models were used for both unadjusted and adjusted analyses with a random effect assigned for patients within ASCs. Adjusted odds are based on multivariable analysis controlling for age, sex, race, income level, payer status, comorbid disease severity [Deyo modification of Charlson Comorbidity Index (CCI)], and reason for inpatient admission before elective surgery. Model fit was assessed using the Akaike information criterion (AIC) and significance compared to null models with the likelihood ratio test. Classification sensitivity was assessed using area under the curve (AUC). Sensitivity analysis using propensity matching was conducted, yielding similar results (Supplementary Figure 2, http://links.lww.com/SLA/B85).
Variation of quality across ASCs was measured using observed over expected (O/E) adverse event ratios with corresponding 95% confidence intervals (CIs) and shrinkage adjustment. Observed (predicted) events were based upon the best linear unbiased prediction (BLUP) incorporating both random and fixed effects, and expected events were based on predictions from the fixed portion of fitted hierarchical models. Centers were ranked based on O/E ratios, with lower quality ASCs defined as those with an O/E ratio significantly >1.0, average-quality ASCs with an O/E ratio with a 95% CI that crossed 1.0, and higher-quality ASCs with an O/E significantly <1.0.
Time to event analysis was performed using the Kaplan-Meier failure function. Follow-up was restricted to 30 days following elective surgery. The log-rank test was used to compare between-group differences in stratified measures. Cost analysis was conducted by converting total charge data to costs. Wilcoxon rank-sum/Mann-Whitney test was used to compare non-normally distributed costs of inpatient readmission between groups.
Statistical analyses were performed in STATA MP Version 13 (64 bit) and R x64 v.3.0.2. This study was deemed exempt from Institutional Review Board approval based on the use of deidentified records.
Results
A total of 57,988 patients met our inclusion criteria. Elective hernia repairs were performed at 382 different ambulatory surgical centers. Baseline demographic and socioeconomic characteristics of the study population are shown in Table 1. The mean age of the study population was 55.3 years (SD 15.6). Patients were grouped as either not having PHS (n = 56,656) or having PHS (n = 1332). Notable differences between the PHS and no PHS groups were observed during univariate testing. Patients with PHS were older (59.8 vs 55.2 years, P < 0.001) and more likely to have comorbid disease (CCI 0.7 vs 0.3, P < 0.001). In addition, there were differences in primary payer mix, with PHS patients predominately insured by Medicare (46.0%), whereas no PHS patients were most commonly privately insured (55.2%, P < 0.001). The mean time from previous inpatient admission and surgery was 48.7 days and the median length of stay for those admissions was 2 days [interquartile range (IQR) 1–4 days).
Table 1. Baseline Characteristics of Study Population Comparing Exposed (PHS) and Unexposed (no PHS) Groups.
| Characteristic | No PHS (n = 56,656) | PHS (n = 1332) | P |
|---|---|---|---|
| Age, y | 55.2 (SD = 15.5) | 59.8 (SD = 17.1) | <0.001 |
| Sex (% female) | 14,459 (25.5%) | 426 (32.0%) | <0.001 |
| Race | <0.001 | ||
| White | 37,015 (65.3%) | 915 (68.7%) | |
| Hispanic | 2753 (4.9%) | 87 (6.5%) | |
| African-American | 9413 (16.6%) | 222 (16.7%) | |
| Asian | 2480 (4.4%) | 45 (3.4%) | |
| Other | 4995 (8.8%) | 63 (4.7%) | |
| Income | <0.001 | ||
| 1st Quartile | 12,128 (21.4%) | 346 (26.0%) | |
| 2nd Quartile | 13,305 (23.5%) | 324 (24.3%) | |
| 3rd Quartile | 15,095 (26.6%) | 335 (25.2%) | |
| 4th Quartile | 14,836 (26.2%) | 297 (22.3%) | |
| Unknown | 1292 (2.3%) | 30 (2.3%) | |
| Primary payer | <0.001 | ||
| Medicare | 15,446 (27.3%) | 613 (46.0%) | |
| Medicaid | 3943 (7.0%) | 142 (10.7%) | |
| Private | 31,243 (55.2%) | 500 (37.5%) | |
| Self-Pay | 1373 (2.4%) | 11 (0.8%) | |
| Other | 4651 (8.2%) | 66 (5.0%) | |
| Comorbidity | |||
| CCI | 0.3 (SD = 0.7) | 0.7 (SD = 1.2) | <0.001 |
| Time to elective surgery (mean days, SD) | 48.7 (SD = 24.5) | ||
| Length of stay (median days, IQR) | 2 (1–4) |
CCI indicates Charlson comorbidity index; IQR, interquartile range; PHS, post-hospital syndrome.
For patients exposed to PHS, the 30-day risk-adjusted adverse event rate was significantly higher than that of patients not exposed to PHS (11.8% vs 5.8%, P < 0.001; Figure 1). Types of adverse events were compared between patients with and without PHS (Table 2). Overall, PHS patients were significantly more likely than non-PHS patients to experience postoperative complications [odds ratio (OR) 2.2, 95% CI: 1.6–3.0). Adverse events owing to digestive (OR 1.4, 95% CI0.8–2.6) causes did not differ between groups. Adverse event rate varied across ASCs (Figure 2). Lower-quality ASCs had a higher adverse event rate compared with higher-quality ASCs (OR 2.7, 95% CI 2.4–3.0). After controlling for ASC quality, PHS remained an independent predictor of adverse events (OR 2.7, 95% CI 2.3–3.2).
Figure 1.
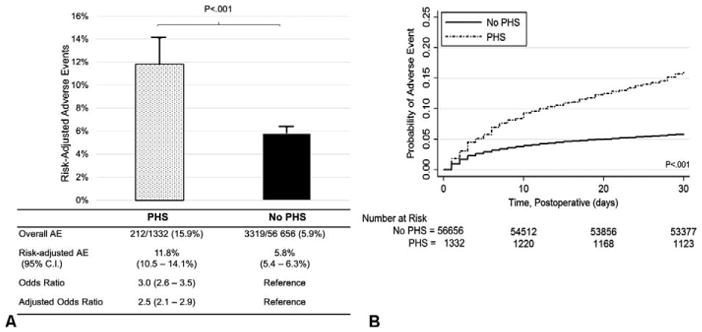
(A) Postoperative outcomes following elective hernia repair in exposed (PHS) and unexposed (no PHS) groups. (B) Kaplan-Maier failure curves for 30-day postoperative adverse events, by exposure. AE indicates adverse event; PHS, post-hospital syndrome.
Table 2. Characterizing Type and Frequency of Adverse Events Following Elective Hernia Repair.
| Type of Adverse Event*,† | PHS (n = 1332, %) | No PHS (n = 56,656, %) | Adjusted Odds‡ | 95% CI |
|---|---|---|---|---|
| Postoperative complication | 44 (3.3%) | 707 (1.3%) | 2.2 | 1.6–3.0 |
| Genitourinary system | 19 (1.4%) | 411 (0.7%) | 1.6 | 1.0–2.6 |
| Nervous system | 18 (1.4%) | 306 (0.5%) | 2.3 | 1.4–3.8 |
| Digestive system | 16 (1.2%) | 303 (0.5%) | 1.4 | 0.8–2.6 |
| Abdominal pain | 23 (1.7%) | 293 (0.5%) | 2.8 | 1.8–4.4 |
| Circulatory system | 22 (1.7%) | 218 (0.4%) | 3.2 | 2.0–5.1 |
| Injury/poison | 12 (0.9%) | 154 (0.3%) | 2.7 | 1.5–5.1 |
| Respiratory system | 11 (0.8%) | 143 (0.3%) | 2.8 | 1.5–5.2 |
| Unknown | 14 (1.1%) | 61 (0.1%) | 7.2 | 3.9–13.3 |
CI indicates confidence interval; PHS, post-hospital syndrome.
CCS codes were matched with ICD-9-CM diagnostic code chapters to create 17 distinct categories.
The following adverse event categories were omitted from reporting because of HCUP restrictions (frequency <10 in a tabulated cell): other specified, other postoperative care unspecified, musculoskeletal system, mental illness, nausea and vomiting, infectious disease, skin and subcutaneous tissue, nutritional and endocrine disorder, and unknown.
Multilevel, mixed-effects logistic models for each adverse event. Odds comparing PHS to no PHS (reference group). Adjustment with age, sex, comorbid disease severity (Deyo modification of Charlson Comorbidity Index), and reason for inpatient admission before surgery.
Figure 2.
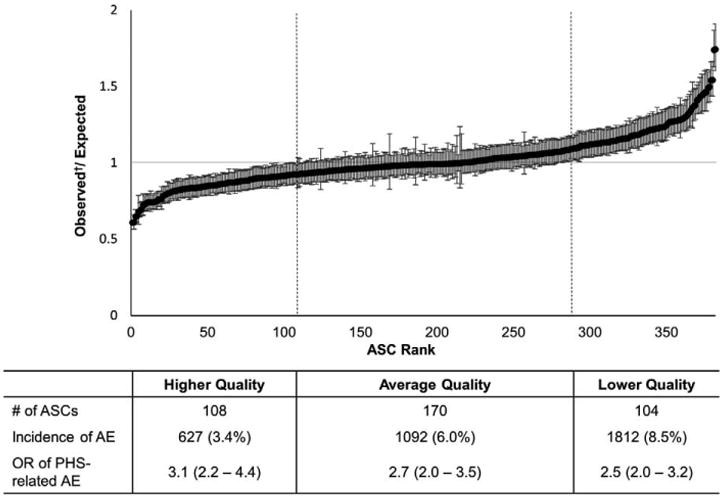
Observed over expected adverse event rate, by ASC (ranked from lowest to highest) with 95% confidence intervals. †Predicted observed, with shrinkage adjustment. AE indicates Adverse event; ASC, ambulatory surgery center.
Next, cost analysis revealed that although there was no significant difference in cost for adverse events requiring inpatient hospitalization between groups [$9545.53 (IQR $6,818.53– $15,819.27) vs $10,698.92 (IQR $5843.10–$19,642.17), P = 0.523], the higher frequency of inpatient readmission (7.6% vs 1.6%) for the PHS group resulted in an additional expenditure of $63,533.46 per 100 elective hernia repairs (Figure 3).
Figure 3.
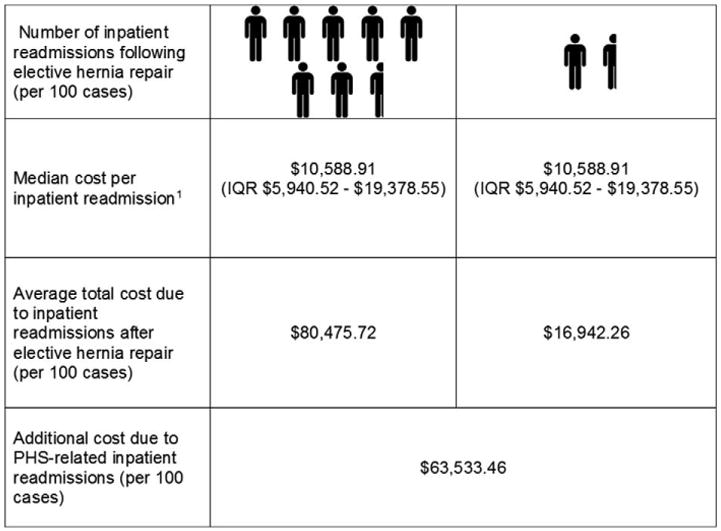
Costs associated with increased rate of postoperative adverse events for patients exposed to PHS. IQR indicates interquartile range; PHS, post-hospital syndrome. 1Median cost of inpatient readmission in PHS group = $9545.53 (IQR: $6818.53–$15,819.27) vs median cost of inpatient readmission in non-PHS group = $10,698.92 (IQR: $5843.10–$19,642.17), P = 0.523. Median cost of inpatient readmission regardless of group = $10,588.91 (IQR: $5940.52–$19,378.55).
Finally, we examined changes in the risk of adverse events owing to PHS over the 90-day window between initial hospitalization and elective hernia repair. We found that the elevated risk of postoperative adverse events associated with PHS did not decline significantly during the 90-day window before surgery (Figure 4), and at no point did the risk return to normal levels. Although there was an overall downward trend in risk over the time period, there remained a marked increase in risk of adverse events after hernia repair at 30, 60, and 90 days postdischarge.
Figure 4.
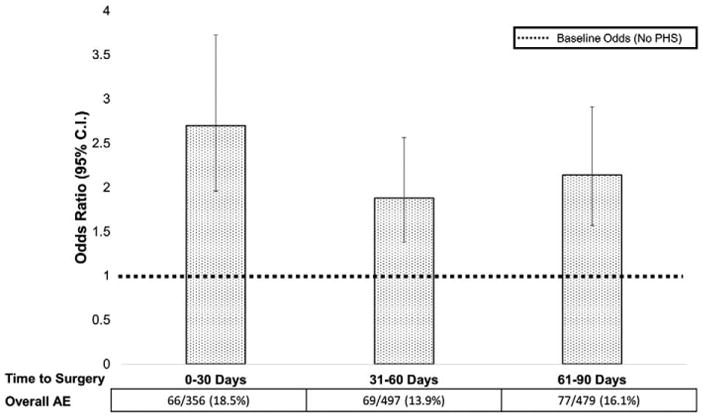
Adjusted odds and frequency of adverse events based on number of days between hospital discharge and elective hernia repair. AE indicates adverse event; CI, confidence interval; PHS, post-hospital syndrome.
Discussion
Patients hospitalized within 90 days before an elective surgery are at an increased risk of adverse events following surgery, particularly postoperative complications. PHS persists after controlling for baseline patient characteristics and medical comorbidities, as well as for surgical center quality and reason for hospitalization before elective surgery. Adverse postoperative events in patients exposed to PHS do not appear to be exacerbations of conditions they were hospitalized with before surgery, and most appear to be directly related to the surgery itself.
Before attributing the increase in risk of postoperative adverse events to PHS, we considered alternative explanations, including increased severity of comorbid disease in these patients, the need for or urgency of hernia repair in PHS patients, presurgical diagnosis, quality of the ASC performing the repair, and the possibility that the readmission is simply an exacerbation of previous conditions. In each analysis, even after controlling for confounders, the association between PHS and adverse outcome remained. These data support the idea that PHS defines a vulnerable population at elevated risk when undergoing even elective, low-risk surgery.
An alternate explanation for our finding is that this population is otherwise predisposed to high rates of acute care utilization. For example, patients who live farther away from care centers8 as well as those in minority,9 elderly,10 and lower socio-economic groups11 tend to lack primary care providers,12 and therefore utilize acute care such as emergency departments more frequently.13–15 Although these types of covariates are not entirely captured by our data, they all are additional symptoms of PHS and should be part of a comprehensive preoperative evaluation before elective surgery to determine who may be at increased risk for an adverse event.
Previous literature has found that for medical patients hospitalized once, there is increased risk for subsequent readmission unrelated to the first admission. This risk has been attributed to PHS, caused by disruption in sleep-wake cycles, inadequate pain control, deconditioning, and changes in nutritional status. Together, this may lead to PHS creating a state of physiologic depletion and an impaired ability to heal against new health insults, including surgery. By comparing a cohort of patients undergoing elective, low-risk surgery that are either exposed or unexposed to PHS, we were able to measure the risk of patients developing specific postoperative adverse events including postoperative complications, abdominal pain, and visits related to postoperative care. The increased odds for developing these hernia repair-specific adverse events provide more direct evidence than previous studies for the mechanism by which PHS impacts recently discharged patients.
Dharmarajan et al4 hypothesized that the risk of adverse events associated with PHS may remain high for several months after hospitalization. Indeed, we found that the risk remained high throughout the 90 days after discharge and observed no time at which the risk declined to normal. One possibility for this observation is an unexplained interaction between the physiologic vulnerability created by PHS and the demands of the recovery process after surgery to which only surgical patients are exposed. Therefore, additional studies are needed to elucidate the risk trajectory and identify how long the elevated risk persists.
From a policy perspective, our observations suggest the need for additional preoperative testing for patients undergoing elective surgery who have been hospitalized in the 90 days before the elective procedure; or, at minimum, further risk assessment. Importantly, the risks of postponing the procedure should be weighed against those derived from PHS. Efforts to promote patient well-being during and after inpatient hospitalization should be emphasized to improve patients' physiological reserve, possibly through greater attention to sleep, nutrition, activity levels, and careful symptom management.1,16 Since elective surgery should be associated with minimal morbidity and mortality, using lessons from high-risk elective surgery (eg, prehabilitation, standardized postoperative care pathways) may be a way to mitigate any increased risk found in PHS patients undergoing elective surgery.17,18
Furthermore, decreasing the number of adverse events, particularly postoperative complications, associated with PHS has the potential to provide a focus for significant cost savings. Our data suggest a potential saving to the healthcare system of over $10,000 for each PHS-related inpatient readmission. Postoperative complications, especially preventable ones, have previously been identified as a primary target for quality improvement as well as for reducing costs associated with readmission.19 Postoperative complications owing to PHS fit these criteria, and reduction in PHS-related readmissions could be a straightforward step toward meeting this goal.
Limitations of this study include a focus on a single operation, elective hernia repair, to measure the role of PHS on outcomes after elective surgery. Although this procedure was chosen for its simplicity and low rates of associated morbidity and mortality,5 our choice could affect the generalizability of the results. Second, defining an adverse event as readmission to the hospital can be debated: in some cases, the reason for readmission may be unavoidable (eg, urinary retention requiring an emergency department visit). Importantly, the nature of the study design does not allow a precise estimate of how much more the risk of adverse events increases among patients recently admitted who undergo hernia repair. Finally, we cannot answer why patients with recent hospitalizations are being operated on soon after an inpatient admission. Our data highlight the need to understand this process better.
Conclusion
In conclusion, patients who are exposed to PHS before an elective hernia repair are at increased risk for adverse events, particularly postoperative complications, following surgery. Among this population, these complications are the leading cause for adverse events, which are costly and potentially avoidable, possibly through additional preoperative testing or strategies that promote patient well-being during their initial hospitalization. More work is needed to determine when the increased risk of adverse events after elective surgery associated with PHS declines.
Supplementary Material
Acknowledgments
This work was supported by NIH T32 GM08750-16.
Footnotes
The authors report no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.annalsofsurgery.com).
References
- 1.Krumholz HM. Post-hospital syndrome–an acquired, transient condition of generalized risk. N Engl J Med. 2013;368:100–102. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Detsky AS, Krumholz HM. Reducing the trauma of hospitalization. JAMA. 2014;311:2169–2170. doi: 10.1001/jama.2014.3695. [DOI] [PubMed] [Google Scholar]
- 3.Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dharmarajan K, Hsieh AF, Kulkarni VT, et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: Retrospective cohort study. BMJ. 2015;350:h411. doi: 10.1136/bmj.h411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Steiner CA, Maggard-Gibbons M, Raetzman SO, et al. Return to acute care following ambulatory surgery. JAMA. 2015;314:1397–1399. doi: 10.1001/jama.2015.12210. [DOI] [PubMed] [Google Scholar]
- 6.Agency for Health Research and Quality. Healthcare cost and utilization project (HCUP) [Accessed February 15 2016]; Available at: http://www.ahrq.gov/research/data/hcup/index.html. Updated 2016. [PubMed]
- 7.Agency for Healthcare Research and Quality. Clinical classifications software (CCS) 2014. [Accessed February 15 2016]; Available at: https://www.hcup-us.ahrq.gov/toolssoftware/ccs/CCSUsersGuide.pdf. Updated 2014.
- 8.Parchman ML, Culler SD. Preventable hospitalizations in primary care shortage areas. an analysis of vulnerable medicare beneficiaries. Arch Fam Med. 1999;8:487–491. doi: 10.1001/archfami.8.6.487. [DOI] [PubMed] [Google Scholar]
- 9.Oster A, Bindman AB. Emergency department visits for ambulatory care sensitive conditions: Insights into preventable hospitalizations. Med Care. 2003;41:198–207. doi: 10.1097/01.MLR.0000045021.70297.9F. [DOI] [PubMed] [Google Scholar]
- 10.Culler SD, Parchman ML, Przybylski M. Factors related to potentially preventable hospitalizations among the elderly. Med Care. 1998;36:804–817. doi: 10.1097/00005650-199806000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Pappas G, Hadden WC, Kozak LJ, et al. Potentially avoidable hospitalizations: inequalities in rates between US socioeconomic groups. Am J Public Health. 1997;87:811–816. doi: 10.2105/ajph.87.5.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Petersen LA, Burstin HR, O'Neil AC, et al. Nonurgent emergency department visits: the effect of having a regular doctor. Med Care. 1998;36:1249–1255. doi: 10.1097/00005650-199808000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Tang N, Stein J, Hsia RY, et al. Trends and characteristics of US emergency department visits, 1997–2007. JAMA. 2010;304:664–670. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xu KT, Nelson BK, Berk S. The changing profile of patients who used emergency department services in the United States: 1996 to 2005. Ann Emerg Med. 2009;54:805–810.e1–e7. doi: 10.1016/j.annemergmed.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 15.Bindman AB, Grumbach K, Osmond D, et al. Preventable hospitalizations and access to health care. JAMA. 1995;274:305–311. [PubMed] [Google Scholar]
- 16.Dharmarajan K, Krumholz HM. Strategies to reduce 30-day readmissions in older patients hospitalized with heart failure and acute myocardial infarction. Curr Geriatr Rep. 2014;3:306–315. doi: 10.1007/s13670-014-0103-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Snowden CP, Prentis JM, Anderson HL, et al. Submaximal cardiopulmonary exercise testing predicts complications and hospital length of stay in patients undergoing major elective surgery. Ann Surg. 2010;251:535–541. doi: 10.1097/SLA.0b013e3181cf811d. [DOI] [PubMed] [Google Scholar]
- 18.Grocott MP, Martin DS, Mythen MG. Enhanced recovery pathways as a way to reduce surgical morbidity. Curr Opin Crit Care. 2012;18:385–392. doi: 10.1097/MCC.0b013e3283558968. [DOI] [PubMed] [Google Scholar]
- 19.Lawson EH, Hall BL, Louie R, et al. Association between occurrence of a postoperative complication and readmission: Implications for quality improvement and cost savings. Ann Surg. 2013;258:10–18. doi: 10.1097/SLA.0b013e31828e3ac3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


