Abstract
Objectives
Gout is increasingly recognized as the most common form of inflammatory arthritis worldwide; however, no Canadian data on the disease burden of gout are available. We estimated the prevalence, incidence, prescription patterns, and comorbidity burden of gout in an entire Canadian province (British Columbia [BC]) over the last decade.
Methods
We utilized PopulationData BC, a province-wide database, to estimate temporal trends in the prevalence and incidence of gout from 2000-2012, as well as according to age category. Annual estimates were age-sex-standardized using 2012 as the reference. We also examined annual trends in prescription patterns of common gout medications and assessed the comorbidity burden among gout patients in 2012.
Results
The 2012 prevalence of gout was 3.8% among the overall population, and the incidence rate was 2.9 per 1,000 person-years. Both gout prevalence and incidence increased substantially over the study period. This burden additionally increased according to age category, affecting over 8% of those ages 60-69 years in 2012. Approximately 22% of gout patients received a prescription for urate-lowering therapy (ULT), which remained stable over the study period, while colchicine and oral glucocorticoid use both increased modestly. By 2012, 72%, 52%, and 18% of prevalent gout patients had been diagnosed with hypertension, hyperlipidemia, and diabetes, respectively.
Conclusions
The burden of gout in BC, Canada, is substantial, and both the prevalence and incidence have increased over the past decade, while prescription of ULT remains low. These data support the need to improve gout prevention and care.
Keywords: Gout, Epidemiology, Prevalence, Incidence, Urate-Lowering Therapy, Prescription Patterns, Canada
INTRODUCTION
Gout is an excruciatingly painful form of inflammatory arthritis caused by hyperuricemia [1]. The disease is associated with a substantial comorbidity burden [2, 3], as well as premature mortality [4, 5], reduced quality of life [6], and a high cost of illness [7]. Gout is increasingly becoming recognized as the most common form of inflammatory arthritis worldwide. For example, gout has been estimated to affect as many as 3.9% of adults (8.3 million individuals) in the US according to the National Health and Nutrition Examination Survey (NHANES) 2007-2008, a significant increase since the NHANES III (i.e., prevalence of 2.7% in 1988–1994) [8]. Moreover, a recent study conducted using a UK primary care database reported a gout prevalence of 2.5% among the overall population in 2012, which had increased substantially from 1.5% in 1997 [9]. Although more limited, studies of gout incidence have also reported substantial and increasing trends. For instance, according to findings from the Rochester Epidemiology Project, the incidence of primary gout had doubled between the 1970's and 1990's [10], and a more recent UK-based study also found an increase in gout incidence over nearly two decades [9].
Despite these findings, no Canadian general population-based data on the disease burden of gout are available. To address this, we estimated contemporary trends in the incidence and prevalence of gout in the Canadian province of British Columbia (BC) from 2000-2012 using a large administrative health database spanning the entire province. We also examined annual trends in prescription patterns of common gout medications and assessed the comorbidity burden among gout patients in 2012.
METHODS
Data Source and Study Population
Universal health coverage is a feature of Canada, including the province of BC (approximately 4.5 million individuals), and PopulationData BC (PopData) is a population-based database from the provincial health care system that includes all patients who received care in BC. PopData captures all provincially funded health services since 1990, including health professional visits [11], hospital admissions and discharges [12], demographic data [13], cancer registry files [14], and vital statistics [15]. Furthermore, PopData encompasses a comprehensive prescription drug database, PharmaNet [16], which includes detailed medication dispensation information for all BC residents since 1996.
Gout Case Definition
Our study was comprised of all individuals who contributed data to PopData from 1 January 1990 until 31 December 2012. To facilitate comparisons with prior studies of gout prevalence and incidence in other countries [9, 17-21], our primary case definition of gout required at least one recorded principal diagnosis of gout (ICD-9-CM 274 or ICD-10-CA M10) at either a physician or hospital visit. We additionally applied a more restrictive case definition of gout comprised of individuals with at least two recorded principal diagnoses of gout from an outpatient visit on separate dates or at least one recorded principal diagnosis of gout from a hospital visit over the study period.
Estimation of Prevalence and Incidence
We estimated trends of gout prevalence and incidence according to calendar year from 2000-2012 for the overall population as well as according to sex. To remove the effect of different age and sex structures over the study period, all annual estimates were age-sex-standardized using the population distribution of BC in 2012 as the reference. We additionally estimated the prevalence and incidence of gout by age category in 2012, both in the overall population as well as according to sex.
To estimate the prevalence of gout, we defined prevalent cases as those who had received a diagnosis of gout by 1 July of each calendar year, with the number of individuals in BC at the same time point as the denominator. Population estimates were obtained from BC Stats.
To estimate the incidence of gout, we defined new cases as those who met our case definitions for the first time in each calendar year. To ensure incident gout cases, we required all newly diagnosed individuals to have at least ten years of prior registration (i.e., “run-in” period) without any record of a gout diagnosis. Individuals previously diagnosed with gout during this run-in period were not eligible to become incident cases. We estimated person-years of at-risk time using population data obtained from BC Stats.
Patterns of Gout Treatment
We examined treatment patterns for the following medications commonly used in gout care: urate-lowering therapy (ULT; i.e., allopurinol, febuxostat, probenecid, and sulfinpyrazone), colchicine, oral glucocorticoids, and non-steroidal anti-inflammatory drugs (NSAIDs). All medications were identified using their unique Drug Identification Number provided by the Health Canada Drug Product Database [22]. We ascertained the proportion of prevalent gout cases where the patient received at least one prescription for these medications in each calendar year over the study period.
Assessment of Comorbidities
We assessed key comorbidities (i.e., hypertension, hyperlipidemia, diabetes mellitus, chronic kidney disease, heart failure, myocardial infarction, and ischemic stroke) among 2012 prevalent and incident gout cases. Patients were considered to have a given comorbidity of interest if they had received at least one recorded diagnosis for the condition at either an outpatient or hospital visit (a) anytime during the study period for prevalent cases and (b) within 10 years prior to the index date for incident cases.
Statistical Analysis
We analyzed annual trends in incidence, prevalence, and medication use using Poisson regression models that included a variable representing the linear trend from the baseline year of 2000. All p-values were 2-sided with a significance threshold of p<0.05. All statistical analyses were performed using SAS Version 9.4 (SAS Institute, Cary, North Carolina).
No personal identifying information was made available as part of this study. All procedures used were conducted in compliance with BC's Freedom of Information and Privacy Protection Act. Ethics approval was obtained from the University of British Columbia.
RESULTS
Prevalence and Incidence of Gout in 2012
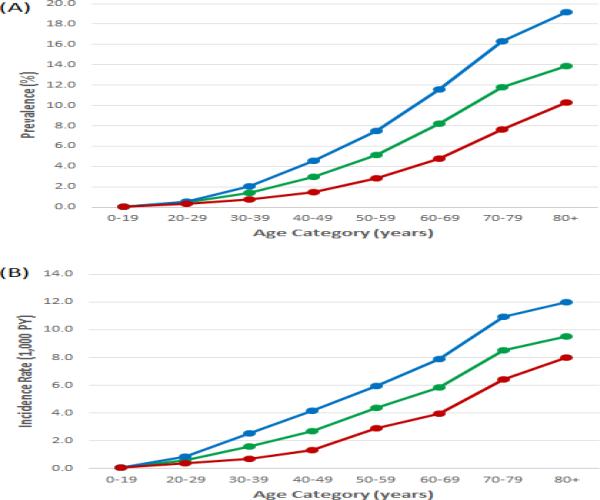
Of 4,542,508 individuals in BC in 2012, we identified 171,165 prevalent gout cases (68% male, mean age 63 years [standard deviation 15.4]), corresponding to an overall prevalence of 3.8%. Males had a higher overall prevalence of gout as compared to females (5.2% and 2.4%, respectively), and this sex difference persisted across all age categories (Figure 1a). Gout prevalence was low among individuals younger than 30 years of age (less than 1%), and the prevalence increased according to age category thereafter. Among individuals aged 50-59 years, 5.1% of individuals had received a diagnosis of gout, and by 70-79 years, 11.8% had received a diagnosis of gout.
Figure 1.
Trends in prevalence (A) and incidence (B) of gout in 2012 according to age category. Green: overall, blue: male, red: female.
There were a total of 4,384,315 person-years of follow-up in 2012, during which we identified 12,672 incident gout cases, corresponding to an overall incidence rate of 2.9 new cases per 1,000 person-years. As in gout prevalence, males had a higher incidence of gout as compared to females (3.8 and 2.0 cases per 1,000 person-years, respectively), and this sex difference persisted across all age categories (Figure 1b). The incidence rate also increased according to age category, reaching nearly 10 new cases per 1,000 person-years among individuals at least 80 years old.
Annual Trends of Prevalence and Incidence
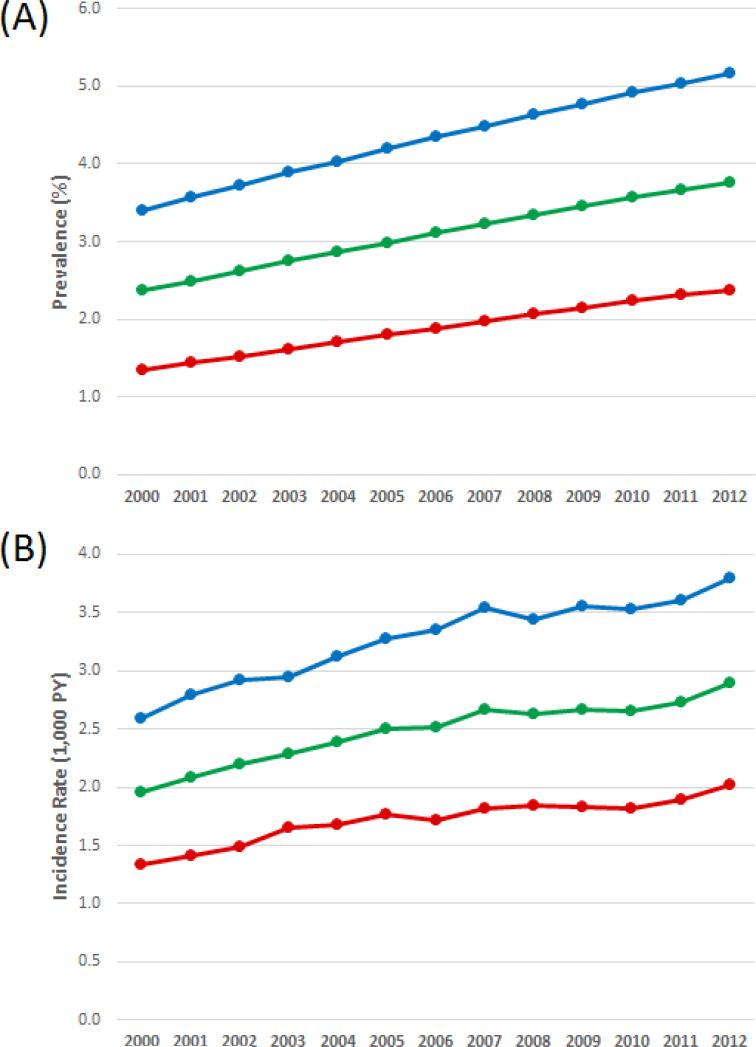
The age-sex-standardized trends in gout prevalence and incidence from 2000-2012 are shown in Figures 2a and 2b. Both the prevalence and incidence rates increased over the study period. The standardized prevalence among the overall population increased by 59% from 2.4% in 2000 to 3.8% in 2012 (p for trend <0.001) (Figure 2a and Table 1). Increasing prevalence trends were seen among both males and females (p for both trends <0.001). We also observed similar increasing trends in gout incidence over the study period, with a standardized incidence rate of nearly 2 new cases per 1,000 PY in 2000 which rose to 2.9 new cases per 1,000 PY by 2012 (i.e., a 48% increase; p for trend <0.001) (Figure 2b and Table 2). Similar increasing trends were seen among males and females (p for both trends <0.001).
Figure 2.
Age-sex-standardized trends in prevalence (A) and incidence (B) of gout from 2000-2012. Green: overall, blue: male, red: female.
Table 1.
Crude and standardized prevalence of gout in British Columbia, Canada from 2000-2012
| Overall (%) | Males (%) | Females (%) | ||||
|---|---|---|---|---|---|---|
| Year | Crude Prevalence | Standardized Prevalence | Crude Prevalence | Standardized Prevalence | Crude Prevalence | Standardized Prevalence |
| 2000 | 2.01 | 2.37 | 2.85 | 3.40 | 1.17 | 1.35 |
| 2001 | 2.14 | 2.49 | 3.04 | 3.56 | 1.25 | 1.43 |
| 2002 | 2.28 | 2.61 | 3.23 | 3.72 | 1.35 | 1.52 |
| 2003 | 2.44 | 2.74 | 3.44 | 3.89 | 1.45 | 1.61 |
| 2004 | 2.59 | 2.86 | 3.63 | 4.03 | 1.56 | 1.70 |
| 2005 | 2.74 | 2.99 | 3.82 | 4.19 | 1.67 | 1.80 |
| 2006 | 2.89 | 3.11 | 4.03 | 4.35 | 1.77 | 1.88 |
| 2007 | 3.03 | 3.22 | 4.21 | 4.49 | 1.87 | 1.97 |
| 2008 | 3.18 | 3.34 | 4.40 | 4.64 | 1.97 | 2.06 |
| 2009 | 3.31 | 3.45 | 4.57 | 4.77 | 2.06 | 2.14 |
| 2010 | 3.46 | 3.56 | 4.77 | 4.91 | 2.17 | 2.23 |
| 2011 | 3.61 | 3.66 | 4.97 | 5.04 | 2.28 | 2.31 |
| 2012 | 3.77 | 3.77 | 5.17 | 5.17 | 2.38 | 2.38 |
Table 2.
Crude and standardized incidence of gout in British Columbia, Canada from 2000-2012
| Overall (1,000 PY) | Males (1,000 PY) | Females (1,000 PY) | ||||
|---|---|---|---|---|---|---|
| Year | Crude Incidence | Standardized Incidence | Crude Incidence | Standardized Incidence | Crude Incidence | Standardized Incidence |
| 2000 | 1.71 | 1.95 | 2.25 | 2.59 | 1.18 | 1.34 |
| 2001 | 1.85 | 2.09 | 2.47 | 2.80 | 1.25 | 1.41 |
| 2002 | 1.97 | 2.19 | 2.63 | 2.92 | 1.34 | 1.49 |
| 2003 | 2.09 | 2.29 | 2.68 | 2.94 | 1.51 | 1.65 |
| 2004 | 2.22 | 2.39 | 2.90 | 3.13 | 1.56 | 1.68 |
| 2005 | 2.35 | 2.51 | 3.08 | 3.28 | 1.65 | 1.76 |
| 2006 | 2.38 | 2.52 | 3.18 | 3.35 | 1.62 | 1.71 |
| 2007 | 2.55 | 2.66 | 3.39 | 3.55 | 1.73 | 1.82 |
| 2008 | 2.53 | 2.63 | 3.32 | 3.44 | 1.78 | 1.84 |
| 2009 | 2.59 | 2.67 | 3.45 | 3.55 | 1.77 | 1.83 |
| 2010 | 2.60 | 2.66 | 3.46 | 3.53 | 1.78 | 1.82 |
| 2011 | 2.70 | 2.73 | 3.57 | 3.60 | 1.87 | 1.89 |
| 2012 | 2.89 | 2.89 | 3.79 | 3.79 | 2.03 | 2.03 |
PY = person-years
We observed reduced estimates in gout burden after applying our secondary case definition, although we found similar increasing trends over the study period (p for all trends <0.001). Specifically, the standardized annual prevalence of gout increased from 1.2% to 2.0% among the overall population from 2000 to 2012. The standardized annual incidence rate also increased from 1.1 to 1.7 new cases per 1,000 PY among the overall population from 2000 to 2012.
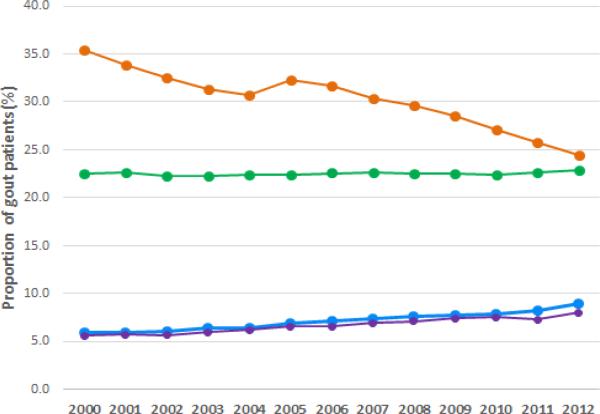
Patterns of Gout Treatment
The temporal trend in anti-gout medication use among prevalent gout patients from 2000-2012 is shown in Figure 3. Approximately one in five patients received treatment with ULT over the study period (range 22.3% to 22.9%). Allopurinol use constituted the majority of ULT prescriptions, with less than 1% of prevalent cases receiving a dispensation of febuxostat, probenecid, or sulfinpyrazone over the study period (i.e., prevalence of use=0.6%, 0.04%, and 0.02%, respectively, in 2012). Both colchicine and glucocorticoid use showed increasing trends (p for both trends <0.001) over the study period (Figure 3). Specifically, colchicine use increased by 50%, reaching nearly 9% of prevalent gout cases in 2012, while glucocorticoid use increased by 43%, reaching 8.5% of cases in 2012. Conversely, the prescription of traditional NSAIDs declined by 31% over the study period from 35.4% in 2000 to 24.5% in 2012 (p for trend <0.001) (Figure 3).
Figure 3.
Proportion of prevalent gout cases who received treatment with ULT (green), traditional NSAIDs (orange), colchicine (blue), and glucocorticoids (purple) over the study period.
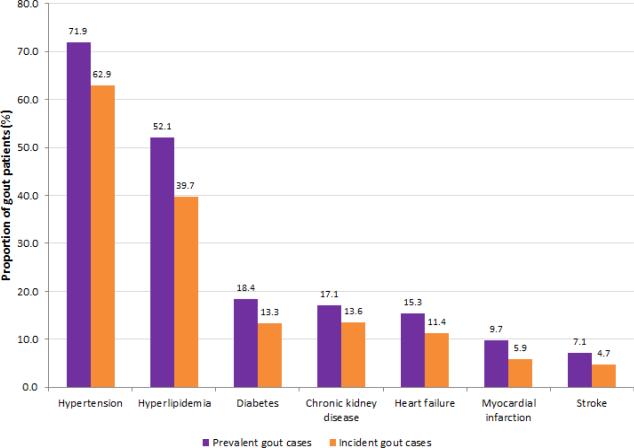
Comorbidity Burden
Of the 171,165 prevalent gout cases identified as of 2012, 71.9% had ever received a diagnosis of hypertension, compared to 62.9% of incident gout cases over the 10 years prior to gout onset, and 17% of prevalent gout patients had received a prescription for diuretics that year (Figure 4). Similar trends were seen for other key comorbid conditions (Figure 4), including hyperlipidemia (52.1% vs. 39.7% among prevalent and incident cases, respectively), diabetes mellitus (18.4% vs. 13.3%), chronic kidney disease (17.1% vs. 13.6%), heart failure (15.3% vs. 11.4%), myocardial infarction (9.7% vs. 5.9%), and ischemic stroke (7.1% vs. 4.7%).
Figure 4.
Comorbidity burden among prevalent and incident gout cases in 2012. Comorbidities were assessed anytime during the study period for prevalent cases and within 10 years prior to the index date for incident cases.
DISCUSSION
In this large general population-based study, we found that both the prevalence and incidence of gout have increased substantially over the past decade, constituting a modern gout epidemic. Specifically, the annual prevalence of gout increased by 59% such that 3.8% of individuals in BC had received a diagnosis of gout by 2012. Moreover, the annual incidence rate increased by 48% over the study period, reaching 2.9 new cases per 1,000 person-years in 2012. These increasing trends persisted when we applied a more restrictive definition of gout. Our analysis of treatment patterns showed a stable trend of ULT prescription over the study period, with approximately one in five patients receiving treatment with ULT, whereas colchicine and glucocorticoid use increased modestly. Finally, we also found a substantial comorbidity burden among those with gout. These findings collectively provide the first contemporary trend data on the burden of gout and pattern of gout treatment in a Canadian general population context.
Gout prevalence had increased substantially over the study period, which is consistent with prior literature from other countries, and particularly with estimates from other western societies. Specifically, we observed a prevalence of 3.8% among the overall BC population in 2012 (5.2% and 2.4% among males and females, respectively), which coincides with the US general population prevalence estimate of 3.9% (5.9% and 2.0% among males and females, respectively) from the NHANES 2007-2008 (based on self-reported physician-diagnosed gout) [8]. These data based on the NHANES 2007-2008 were significantly higher than those in the NHANES-III (which reported prevalence of 2.7% in 1988-1994) [8]. Moreover, another study conducted among a US managed care population also found an increasing prevalence over a ten-year period, from 2.9 to 5.2 cases per 1000 enrollees [18]. Such increasing trends in gout prevalence have also been reported in other countries from other continents, including the UK [9, 23], Italy [24], China [25], New Zealand [26], and urban African communities [27]. Our age-specific prevalence estimates also tended to agree with previously reported ranges. For example, we observed 2012 prevalence estimates of 5.1% and 13.9% among individuals 50-59 years of age and at least 80 years old, respectively; the NHANES 2007-2008 data found age-specific prevalence estimates of 3.7% and 12.6% among individuals 50-59 years and at least 80 years old, respectively, similar to our estimates [8] Further, a UK-based study reported a 2012 prevalence of approximately 5% and 10% among those 55-59 and 80-84 years old, respectively, also similar to our estimates [9].
Our gout incidence trends were also consistent with data from other western countries, although prior incidence data are more limited. We found incidence rates of 2.9, 3.8, and 2.0 per 1,000 person-years among the overall population, males, and females, respectively, in 2012, which coincides with US-based estimates of 4.0 and 1.4 per 1,000 person-years among men and women, respectively (based on prospectively collected, community-based data from the Framingham Heart Study) [28]. Similarly, a UK-based study found an incidence rate of 2.7 new cases per 1,000 person-years (4.4 and 1.3 in men and women, respectively) among adults during 2000-2007 [29]. The increasing trend in gout incidence found in our study has also been previously reported in other settings. For example, the Rochester Epidemiology Project found that the incidence of those with gout had doubled between 1977-1978 and 1995-1996 [10], as in the increasing trends reported here. Similarly, in the UK, the incidence rate among the overall population reached 1.8 new cases per 1,000 person-years in 2012 [9], corresponding to a 30% increase since 1997.
This rising gout burden identified in our study may be explained by similar increasing Canadian trends of associated conditions, including those of obesity [30-32] and hypertension [33]. Thus, efforts to stop or reduce this increasing disease burden could focus on modifiable risk factors for gout and its causal precursor (hyperuricemia), including the presence of other chronic conditions (e.g., obesity [34]), the use of certain medications (e.g., choice of antihypertensive agent [35]), and dietary and lifestyle factors (e.g., consumption of red meat [36, 37], alcohol [38, 39], and sugar-sweetened soft drinks [40, 41]).
Our analysis of prescription patterns showed a stable trend of ULT use from 2000 to 2012 (ranging from 22.3% to 22.9%), which has also been observed in other countries worldwide. For instance, two recent studies from the UK and Taiwan also found unchanging trends in ULT treatment among prevalent gout patients, with approximately 25-35% of patients receiving ULT over the study period [9, 17]. In an earlier UK-based study (i.e., 1990-1999), Mikuls et al. also reported a stable proportion of allopurinol use, ranging from 25-30% [20]. We additionally found a substantial decreasing trend of NSAID use (i.e., from 35% to 25%) from 2000 to 2012. In the decade immediately prior (i.e., 1990-1999), Mikuls et al. reported a similar declining trend in the UK, with a decrease from 67% at the beginning of the study to 41% by 1999 [20]. The continuing decline in NSAID use observed in our study was contrasted by a modest increase in both colchicine and glucocorticoid use among gout patients over the study period. By comparison, a recent US-based study reported an increasing trend of colchicine initiation among those with newly diagnosed gout until the medication's substantial price increase in the US, after which colchicine initiation declined [42, 43]. Meanwhile, such a decline was not observed in the current Canadian setting where colchicine remains at its original low cost.
Our study also found a substantial comorbidity burden among gout patients, similar to many prior studies from other countries [2, 3, 20, 24, 44]. Specifically, approximately 72% of prevalent gout patients had been diagnosed with hypertension as of 2012, as well as 52% with hyperlipidemia, 18% with diabetes, 17% with kidney disease, 15% with heart failure, 10% with myocardial infarction, and 7% with ischemic stroke. These findings are highly consistent with prior findings from other countries; for example, according to the 2007-2008 NHANES in the US, 74% of those with gout had hypertension, 26% had diabetes, 14% had a myocardial infarction, and 11% had heart failure [2]. We additionally identified a large level of prior comorbidity among those who were newly diagnosed with gout in 2012. In our analysis of incident gout cases, 63% had already been diagnosed with hypertension, 40% with hyperlipidemia, and 13% with diabetes, showing a substantial comorbidity burden even in the ten years prior to gout diagnosis.
The strengths and limitations of our study deserve comment. First, we used a population-based dataset covering the entire province of BC, thereby capturing all provincial residents enrolled in BC's universal healthcare program. Thus, our analysis is free of recall and selection bias. Our study spanned over two decades, thereby providing a 23-year ascertainment period to maximize the capture of prevalent cases. Our primary case definition was employed on the basis of multiple prior studies using similar methodology, thereby allowing for comparisons [9, 17-21]; however, we did not require the observation of urate crystals or ascertainment of the recently published gout classification criteria [45] for logistic purposes. We are not aware of prior studies addressing the accuracy of this case definition against either method, which calls for future studies. Nevertheless, we restricted our case definitions to include only those with a diagnosis of gout in the primary position, which has previously been shown to substantially improve the validity of the case definition and thus minimize misclassification bias [46-48]. Moreover, our estimates agreed very well with findings from other countries as discussed above, and we additionally applied a more restrictive definition, which also showed increasing trends in both incidence and prevalence. Furthermore, to reduce the potential misclassification of prevalent cases as incident cases, we applied a rigorous 10-year run-in period during which individuals could have no prior gout diagnosis. Finally, we did not have access to certain data in our administrative dataset, including ethnicity, body mass index, or laboratory values such as serum uric acid.
In conclusion, these contemporary findings from an entire Canadian province demonstrate that both the prevalence and incidence of gout have increased substantially over the past decade, constituting a substantial disease burden. By 2012, nearly 4% of individuals in BC had received a diagnosis of gout, while only one in five patients have received treatment with ULT. These data support the need to improve gout prevention and care.
ACKNOWLEDGEMENTS
Funding and Support
This study was funded by a Team Grant from the Canadian Institutes of Health Research (Grant ID 135235). This study was also supported in part from a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01AR065944).
Role of the Funding Source
The funding sources had no role in the design, conduct, or reporting of the study or the decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributorship Statement
Study conception and design: Rai, Choi
Acquisition, analysis, and/or interpretation of data: All authors
Drafting or critical revision of manuscript: All authors
Final approval: All authors
Data Access, Responsibility, and Analysis
SKR and HKC had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. The BC Ministry of Health approved access to and use of the data facilitated by PopulationData BC for this study.
Competing Interest Statement
HKC has served on advisory boards for Takeda Pharmaceuticals and Astra-Zeneca Pharmaceuticals.
REFERENCES
- 1.Choi HK, Mount DB, Reginato AM. Pathogenesis of Gout. Annals of Internal Medicine. 2005;143:499–516. doi: 10.7326/0003-4819-143-7-200510040-00009. [DOI] [PubMed] [Google Scholar]
- 2.Zhu Y, Pandya BJ, Choi HK. Comorbidities of gout and hyperuricemia in the US general population: NHANES 2007-2008. Am J Med. 2012;125:679–687 e1. doi: 10.1016/j.amjmed.2011.09.033. [DOI] [PubMed] [Google Scholar]
- 3.Kuo CF, Grainge MJ, Mallen C, Zhang W, Doherty M. Comorbidities in patients with gout prior to and following diagnosis: case-control study. Ann Rheum Dis. 2014 doi: 10.1136/annrheumdis-2014-206410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi HK, Curhan G. Independent Impact of Gout on Mortality and Risk for Coronary Heart Disease. Circulation. 2007;116:894–900. doi: 10.1161/CIRCULATIONAHA.107.703389. [DOI] [PubMed] [Google Scholar]
- 5.Kuo CF, See LC, Luo SF, et al. Gout: an independent risk factor for all-cause and cardiovascular mortality. Rheumatology (Oxford) 2010;49:141–6. doi: 10.1093/rheumatology/kep364. [DOI] [PubMed] [Google Scholar]
- 6.Roddy E, Zhang W, Doherty M. Is gout associated with reduced quality of life? A case-control study. Rheumatology. 2007;46:1441–1444. doi: 10.1093/rheumatology/kem150. [DOI] [PubMed] [Google Scholar]
- 7.Rai SK, Burns LC, De Vera MA, et al. The economic burden of gout: A systematic review. Semin Arthritis Rheum. 2015;45:75–80. doi: 10.1016/j.semarthrit.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 8.Zhu Y, Pandya BJ, Choi HK. Prevalence of gout and hyperuricemia in the US general population: the National Health and Nutrition Examination Survey 2007-2008. Arthritis Rheum. 2011;63:3136–41. doi: 10.1002/art.30520. [DOI] [PubMed] [Google Scholar]
- 9.Kuo CF, Grainge MJ, Mallen C, Zhang W, Doherty M. Rising burden of gout in the UK but continuing suboptimal management: a nationwide population study. Ann Rheum Dis. 2015;74:661–7. doi: 10.1136/annrheumdis-2013-204463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arromdee E, Michet CJ, Crowson CS, O'Fallon WM, Gabriel SE. Epidemiology of gout: is the incidence rising? J Rheumatol. 2002;29:2403–6. [PubMed] [Google Scholar]
- 11.British Columbia Ministry of Health . Data Extract. MOH (2013) Population Data BC; 2013. Medical Services Plan (MSP) Payment Information File. [creator] http://www.popdata.bc.ca/data. [Google Scholar]
- 12.British Columbia Ministry of Health . Data Extract. MOH (2013) Population Data BC; 2013. Discharge Abstract Database (Hospital Separations). [creator] http://www.popdata.bc.ca/data. [Google Scholar]
- 13.British Columbia Ministry of Health . Data Extract. MOH (2013) Population Data BC; 2013. Consolidation File (MSP Registration & Premium Billing). http://www.popdata.bc.ca/data. [Google Scholar]
- 14.BC Cancer Agency Registry Data . Data Extract. BC Cancer Agency (2013) Population Data BC; 2014. http://www.popdata.bc.ca/data. [Google Scholar]
- 15.BC Vital Statistics Agency . Data Extract BC Vital Statistics Agency (2013) Population Data BC; 2012. Vital Statistics Deaths. [creator] http://www.popdata.bc.ca/data. [Google Scholar]
- 16.BC Ministry of Health . Data Extract. Data Stewardship Committee (2013) BC Ministry of Health; 2013. PharmaNet. [creator] http://www.popdata.bc.ca/data. [Google Scholar]
- 17.Kuo CF, Grainge MJ, See LC, et al. Epidemiology and management of gout in Taiwan: a nationwide population study. Arthritis Res Ther. 2015;17:13. doi: 10.1186/s13075-015-0522-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wallace KL, Riedel AA, Joseph-Ridge N, Wortmann R. Increasing prevalence of gout and hyperuricemia over 10 years among older adults in a managed care population. J Rheumatol. 2004;31:1582–1587. [PubMed] [Google Scholar]
- 19.Winnard D, Wright C, Taylor WJ, et al. National prevalence of gout derived from administrative health data in Aotearoa New Zealand. Rheumatology. 2012;51:901–909. doi: 10.1093/rheumatology/ker361. [DOI] [PubMed] [Google Scholar]
- 20.Mikuls T, Farrar J, Bilker W, et al. Gout epidemiology: results from the UK General Practice Research Database, 1990-1999. Ann Rheum Dis. 2005;64:267–72. doi: 10.1136/ard.2004.024091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dehlin M, Drivelegka P, Sigurdardottir V, Svärd A, Jacobsson LTH. Incidence and prevalence of gout in Western Sweden. Arthritis Res Ther. 2016;18:1–7. doi: 10.1186/s13075-016-1062-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. [March 3 2016];Health Canada Drug Product Database (DPD) http://www.hc-sc.gc.ca/dhp-mps/prodpharma/databasdon/index-eng.php.
- 23.Harris CM, Lloyd DC, Lewis J. The prevalence and prophylaxis of gout in England. J Clin Epidemiol. 1995;48:1153–8. doi: 10.1016/0895-4356(94)00244-k. [DOI] [PubMed] [Google Scholar]
- 24.Trifirò G, Morabito P, Cavagna L, et al. Epidemiology of gout and hyperuricaemia in Italy during the years 2005–2009: a nationwide population-based study. Ann Rheum Dis. 2012 doi: 10.1136/annrheumdis-2011-201254. [DOI] [PubMed] [Google Scholar]
- 25.Miao Z, Li C, Chen Y, et al. Dietary and lifestyle changes associated with high prevalence of hyperuricemia and gout in the Shandong coastal cities of Eastern China. J Rheumatol. 2008;35:1859–64. [PubMed] [Google Scholar]
- 26.Klemp P, Stansfield SA, Castle B, Robertson MC. Gout is on the increase in New Zealand. Ann Rheum Dis. 1997;56:22–26. doi: 10.1136/ard.56.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cassim B, Mody GM, Deenadayalu VK, Hammond MG. Gout in black South Africans: a clinical and genetic study. Ann Rheum Dis. 1994;53:759–62. doi: 10.1136/ard.53.11.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bhole V, de Vera M, Rahman MM, Krishnan E, Choi H. Epidemiology of gout in women: Fifty-two-year followup of a prospective cohort. Arthritis Rheum. 2010;62:1069–76. doi: 10.1002/art.27338. [DOI] [PubMed] [Google Scholar]
- 29.Cea Soriano L, Rothenbacher D, Choi HK, Garcia Rodriguez LA. Contemporary epidemiology of gout in the UK general population. Arthritis Res Ther. 2011;13:R39. doi: 10.1186/ar3272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Torrance GM, Hooper MD, Reeder BA. Trends in overweight and obesity among adults in Canada (1970-1992): evidence from national surveys using measured height and weight. Int J Obes Relat Metab Disord. 2002;26:797–804. doi: 10.1038/sj.ijo.0801991. [DOI] [PubMed] [Google Scholar]
- 31.Katzmarzyk PT, Mason C. Prevalence of class I, II and III obesity in Canada. Canadian Medical Association Journal. 2006;174:156–157. doi: 10.1503/cmaj.050806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tremblay MS, Katzmarzyk PT, Willms JD. Temporal trends in overweight and obesity in Canada, 1981-1996. Int J Obes Relat Metab Disord. 2002;26:538–43. [PubMed] [Google Scholar]
- 33.Tu K, Chen Z, Lipscombe LL, Taskforce ftCHEPOR Prevalence and incidence of hypertension from 1995 to 2005: a population-based study. Canadian Medical Association Journal. 2008;178:1429–1435. doi: 10.1503/cmaj.071283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Choi HK, Atkinson K, Karlson EW, Curhan G. Obesity, weight change, hypertension, diuretic use, and risk of gout in men: the health professionals follow-up study. Archives of Internal Medicine. 2005;165:742–748. 7. doi: 10.1001/archinte.165.7.742. [DOI] [PubMed] [Google Scholar]
- 35.Choi HK, Soriano LC, Zhang Y, Rodríguez LAG. Antihypertensive drugs and risk of incident gout among patients with hypertension: population based case-control study. BMJ. 2012:344. doi: 10.1136/bmj.d8190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choi HK, Atkinson K, Karlson EW, Willett W, Curhan G. Purine-Rich Foods, Dairy and Protein Intake, and the Risk of Gout in Men. New England Journal of Medicine. 2004;350:1093–1103. doi: 10.1056/NEJMoa035700. [DOI] [PubMed] [Google Scholar]
- 37.Choi HK, Liu S, Curhan G. Intake of purine-rich foods, protein, and dairy products and relationship to serum levels of uric acid: The Third National Health and Nutrition Examination Survey. Arthritis & Rheumatism. 2005;52:283–289. doi: 10.1002/art.20761. [DOI] [PubMed] [Google Scholar]
- 38.Choi HK, Atkinson K, Karlson EW, Willett W, Curhan G. Alcohol intake and risk of incident gout in men: a prospective study. Lancet. 2004;363:1277–81. doi: 10.1016/S0140-6736(04)16000-5. [DOI] [PubMed] [Google Scholar]
- 39.Choi HK, Curhan G. Beer, liquor, and wine consumption and serum uric acid level: the Third National Health and Nutrition Examination Survey. Arthritis Rheum. 2004;51:1023–9. doi: 10.1002/art.20821. [DOI] [PubMed] [Google Scholar]
- 40.Choi HK, Curhan G. Soft drinks, fructose consumption, and the risk of gout in men: prospective cohort study. BMJ. 2008;336:309–12. doi: 10.1136/bmj.39449.819271.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Choi JW, Ford ES, Gao X, Choi HK. Sugar-sweetened soft drinks, diet soft drinks, and serum uric acid level: the Third National Health and Nutrition Examination Survey. Arthritis Rheum. 2008;59:109–16. doi: 10.1002/art.23245. [DOI] [PubMed] [Google Scholar]
- 42.Kesselheim AS, Franklin JM, Kim SC, Seeger JD, Solomon DH. Reductions in Use of Colchicine after FDA Enforcement of Market Exclusivity in a Commercially Insured Population. J Gen Intern Med. 2015;30:1633–8. doi: 10.1007/s11606-015-3285-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kesselheim AS, Solomon DH. Incentives for Drug Development — The Curious Case of Colchicine. New England Journal of Medicine. 2010;362:2045–2047. doi: 10.1056/NEJMp1003126. [DOI] [PubMed] [Google Scholar]
- 44.Annemans L, Spaepen E, Gaskin M, et al. Gout in the UK and Germany: prevalence, comorbidities and management in general practice 2000–2005. Ann Rheum Dis. 2008;67:960–966. doi: 10.1136/ard.2007.076232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Neogi T, Jansen TL, Dalbeth N, et al. 2015 Gout classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2015;74:1789–98. doi: 10.1136/annrheumdis-2015-208237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tieder JS, Hall M, Auger KA, et al. Accuracy of administrative billing codes to detect urinary tract infection hospitalizations. Pediatrics. 2011;128:323–30. doi: 10.1542/peds.2010-2064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Roumie CL, Mitchel E, Gideon PS, et al. Validation of ICD-9 codes with a high positive predictive value for incident strokes resulting in hospitalization using Medicaid health data. Pharmacoepidemiol Drug Saf. 2008;17:20–6. doi: 10.1002/pds.1518. [DOI] [PubMed] [Google Scholar]
- 48.Tamariz L, Harkins T, Nair V. A systematic review of validated methods for identifying ventricular arrhythmias using administrative and claims data. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):148–53. doi: 10.1002/pds.2340. [DOI] [PubMed] [Google Scholar]