Abstract
Objective
The aims of this paper were to report on the global psychosocial functioning of 5-year-old DHH children and examine the risk and protective factors that predict outcomes.
Design
A cross-sectional analysis of data collected from a prospective, population-based longitudinal study.
Study Sample
Parents/caregivers of 356 children completed questionnaires on psychosocial development (CDI, SDQ), functional communication (PEACH) and demographic information. Children completed standardised assessments of non-verbal cognitive ability (WNV) and language (PLS-4).
Results
On average, global psychosocial functioning was within the range of typically developing children; however, variability was high and 12% of children had scores that were more than 2 SDs below the norm. Non-verbal cognitive ability, presence of additional disabilities, language and functional communication significantly predicted outcomes. In contrast, type of hearing device, severity of hearing loss and age at intervention did not.
Conclusion
The global psychosocial functioning of this cohort of 5-year-old DHH children fell within the range of typically developing children. . The findings suggest that spoken language ability and functional communication skills are vital for healthy psychosocial development.
Keywords: Deaf or Hard of Hearing, Hearing loss, Pediatric, Psychosocial/Emotional, Emotional and Behavioral, Social Skills, Language, Communication
Introduction
The presence of permanent childhood hearing loss can have significant adverse effects on all areas of development including language, speech, literacy, education, cognitive and psychosocial functioning (Ching, Day, et al., 2013). However, psychosocial development has been rated as one of the highest areas of concern by parents of children who are deaf or hard of hearing (DHH) (Wake, Hughes, Collins, & Poulakis, 2004). The majority of the literature has reported that, although not inevitable, DHH children have higher rates of psychosocial problems including internalising (e.g., anxiety and depression), and externalising (e.g., hyperactivity and conduct problems) disorders compared to normal-hearing peers (J. Fellinger, Holzinger, Sattel, & Laucht, 2008; Hintermair, 2007; Stevenson, Kreppner, Pimperton, Worsfold, & Kennedy, 2015; Theunissen, Rieffe, Netten, et al., 2014).
In recent years, it has been expected that the implementation of universal newborn hearing screening (UNHS), improved hearing technologies, and early intervention and education efforts would lead to improved outcomes for DHH children. Despite these advances, the research has been inconsistent about whether these developments have resulted in improved psychosocial outcomes (Moeller, 2007; Stevenson et al., 2011; Yoshinaga-Itano & Apuzzo, 1998). Moeller (2007) stressed the need for longitudinal, prospective studies on this new generation of DHH children who have had access to early intervention to identify the intrinsic and extrinsic factors that promote healthy social-emotional development. In line with this recommendation, the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study (Ching, Leigh, & Dillon, 2013) has prospectively measured the language, psychosocial, and educational outcomes of a large cohort of Australian DHH children.
Previous findings for the LOCHI cohort at 3 years of age showed that on average, children were performing within the normal range on psychosocial and motor development as measured on the Child Development Inventory (CDI) (Leigh et al., 2015). Nonetheless, the researchers cautioned that the early language deficits found in some of these young children could adversely impact subsequent psychosocial development at an older age. The LOCHI study has provided the opportunity to investigate this question and in addition, to examine whether the significant predictor variables of psychosocial development at 3 years would remain robust predictors of outcomes at 5 years, or whether other risk/protective factors may become more influential over time.
Psychosocial Problems in DHH children
Using meta-analysis, Stevenson et al. (2015) assessed the presence and extent of emotional and behavioural problems in children with and without hearing loss. Forty-five studies of emotional and behavioural outcomes in DHH children and adolescents (aged 1–21 years) were reviewed. Although various measures were used, Goodman’s Strengths and Difficulties Questionnaire (SDQ) was the most commonly used (n=12). The SDQ is a questionnaire that measures 4 domains of emotional, hyperactivity, conduct, and peer difficulties. Results are summarised to give a ‘total difficulties’ score, and one ‘strength’ domain of prosocial behaviour (e.g., considerate of others feelings, shares with other children). Reviewing all SDQ studies, Stevenson et al. concluded that DHH children and adolescents were at higher risk for developing peer problems than their hearing peers. Parents also rated DHH children as having significantly lower prosocial behaviour and more emotional symptoms, but found no differences were found for behavioural problems such as hyperactivity. Compared to normative data, the authors found the magnitude of difference between DHH and hearing children was relatively small, with a difference of 0.23 and 0.34 standard deviations (SDs) as rated by parents and teachers respectively. For non-SDQ studies, children scored on average, 0.36 SDs below the normative population.
It may be concluded that although DHH children and adolescents show more emotional and behavioural problems than normal-hearing children, the difference appears to be small and not clinically significant. Stevenson et al. (2015) contended that, because the majority of SDQ studies were published after 2000, their findings might reflect improvements in the provision of UNHS and psychological/educational support. However, notably the use of average scores does not take into account individual variation in psychosocial outcomes. Although prevalence rates of psychosocial problems tend to be elevated in DHH children, there is a large proportion of children who do not develop psychosocial difficulties. Therefore Stevenson et al. suggested that the specific interpersonal and intrapersonal processes that mediate the impact between hearing loss and psychosocial problems should be investigated.
Risk and Protective Factors of Psychosocial Functioning
Language and Communication Ability
Psychosocial development is deeply intertwined with language development (Marschark, 1993). Consequently, the social problems observed in DHH populations have been typically attributed to limited abilities in verbal communication, production of intelligible speech and language comprehension (Stevenson, McCann, Watkin, Worsfold, & Kennedy, 2010). However, as many studies have only used correlational analyses (e.g., J. Fellinger, Holzinger, Sattel, Laucht, & Goldberg, 2009; Netten, Rieffe, Theunissen, Soede, Dirks, Korver, et al., 2015; Theunissen, Rieffe, Kouwenberg, et al., 2014), it has been difficult to tease apart whether deficits in language or communication lead directly to psychosocial problems, or whether the two are independent outcomes of a more general delayed developmental process (Barker et al., 2009).
A number of recent studies have directly examined this link using multiple regression or statistical modelling methods. Language ability has been found to independently predict various indices of psychosocial functioning in DHH children including social competence (Hoffman, Quittner, & Cejas, 2015), theory of mind (Schick, De Villiers, De Villiers, & Hoffmeister, 2007), and internalising and externalising behaviour problems measured on the SDQ (Stevenson et al., 2010) and Child Behaviour Checklist (Barker et al., 2009); supporting the idea that deficits in language development have cascading effects on psychosocial development. Both Barker et al. (2009) and Stevenson et al. (2010) found that once receptive and expressive language abilities were controlled, no differences were evident between DHH children and normal-hearing controls in emotional, social, or behavioural problems. They concluded that language is a social tool that is necessary to provide opportunities to interact with others, but also aids the development of emotional and behavioural control.
A recent review reported that the crucial factor related to social interactions for DHH children is not hearing loss or language ability per se, but communication competence (Batten, Oakes, & Alexander, 2014). Studies have reported that DHH children differ from hearing peers in regards to their interaction and communication skills such as turn-taking, joint attention, improvisation in conversation, requests for clarification, eye contact and gesture, and interpreting intonation or innuendo (Jeanes, Nienhuys, & Rickards, 2000; Lederberg & Everhart, 2000; Tait, De Raeve, & Nikolopoulos, 2007; Vaccari & Marschark, 1997). DHH children have been reported to have more difficulties in group situations or noisy environments, compared to one-on-one interactions, which some researchers have coined “social deafness” (Punch & Hyde, 2011). It is likely, therefore, that other personal, audiological and family characteristics may play a role in the nature of DHH children’s social participation, competence and well-being.
Early Identification and Amplification
There is a growing body of evidence showing a positive effect of early intervention for language development (Moeller, 2000; Yoshinaga-Itano, Sedey, Coulter, & Mehl, 1998). It is likely this in turn is associated with improved psychosocial development. By way of example, Yoshinaga-Itano and Apuzzo (1998), found that young DHH children (under 5 years) identified through newborn hearing screening programs had better language and social developmental outcomes as measured by the Child Development Inventory (CDI) compared to those who were identified later. Laugen and colleagues (2016) recently found that younger age at identification significantly predicted better psychosocial functioning in 4-year old DHH children, whereas degree of hearing loss and level of vocabulary were not related. Similarly, studies have reported significant negative correlations between age of hearing aid (HA) fit and various psychosocial indices, including quality of life (Hind & Davis, 2000) and social competence (Hoffman et al., 2015).
Importantly, this link has not been found consistently. Stevenson et al. (2011) reported that although early confirmation of hearing impairment (<9 months age) had a beneficial effect on receptive language, there were no differences in emotional/behavioural problems measured by the Strength and Difficulties Questionnaire (SDQ) between early and later identified children at 5–11 years of age. Similarly Leigh et el. (2015) found that age at intervention was not a significant predictor of psychosocial outcomes for the children from the LOCHI study at 3-years. Stevenson et al. (2011) concluded that improved language ability achieved by early confirmation of hearing loss is not sufficient to alter the risk of psychosocial problems.
Several studies looking at the influence of hearing device on various psychosocial factors, have found that receiving a cochlear implant (CI) is associated with a decreased risk of psychopathology (Huber & Kipman, 2011; Theunissen et al., 2012). Children with CIs have been reported to have lower levels of social anxiety (Theunissen et al., 2012) and lower incidences of behavioural problems compared to HA users (Theunissen, Rieffe, Kouwenberg, et al., 2014). A recent review of the literature by these authors reported that no study has found children with HAs to perform better than those with CIs on psychopathology measures, despite their lower initial hearing losses (Theunissen, Rieffe, Netten, et al., 2014). On the other hand, Peterson (2004) found no differences in theory of mind (i.e., the ability to attribute mental states) between 4–12 year old DHH children with CIs or HAs, and the children performed no better than age peers with autism. In addition, Leigh et al (2015) found neither device nor age of CI switch on were related to social development in the children from the LOCHI cohort at 3 years of age.
Child and Family-Related Factors
Child-related factors such as non-verbal cognitive ability and presence of additional disabilities have been frequently observed to be associated with language, communication and psychosocial outcomes. In DHH children, higher intelligence has been associated with fewer emotional and social problems (Van Eldik, 2005); aggression and behavioural problems (Theunissen, Rieffe, Kouwenberg, et al., 2014); and better adaptive functioning and motor skills (Kushalnagar et al., 2007). DHH children with significant additional disabilities (including intellectual, physical, visual impairments and autism spectrum disorder) may face further difficulties in developing sign or oral communication, increasing their risk of psychosocial problems (Cupples et al., 2014; Dammeyer, 2010). The presence of additional disabilities has been found to predict global language and social-emotional outcomes in DHH children (Dammeyer, 2010; Theunissen, Rieffe, Netten, et al., 2014; Yoshinaga-Itano, 2003), and in the LOCHI study additional disabilities was the strongest and most consistent predictor of psychosocial and motor outcomes for the children at age 3 years (Leigh et al., 2015).
Studies looking at the relationship between severity of hearing loss and psychosocial development have produced varied results (J. Fellinger et al., 2008; Wake et al., 2004). Nevertheless, Theunissen et al.’s (2014) systematic review reported that the majority of studies have found no influence of degree of hearing loss on psychopathology. Consistent with this finding, no relationship was found between 4 frequency average (4FA) hearing loss and social development in the children in the LOCHI study at 3 years (Leigh et al., 2015).
Family factors such as socio-economic status (SES) and level of maternal education have been found to have significant influence over child developmental outcomes. Maternal education is often used as a proxy for SES, however, previous research has found that it uniquely predicts infant development over maternal and paternal occupation (Bornstein, Hahn, Suwalsky, & Haynes, 2003). In DHH children, levels of maternal education have been consistently found to predict a range of outcomes including social and motor development (Korver et al., 2010) and global language outcomes (Ching et al., 2013). Surprisingly, although maternal education was found to predict language ability at 3 years in the LOCHI study (Ching et al., 2013), it did not predict psychosocial outcomes (Leigh et al., 2015).
Finally, mode of communication (i.e., sign, spoken or a combination of both) at home and/or in intervention/education may also be associated with psychosocial development. A number of studies in children with CIs have found oral only communication mode to be linked to better outcomes in language, speech production and perception, compared to mixed communication or sign language (Kirk, Miyamoto, Ying, Perdew, & Zuganelis, 2000; Percy-Smith, Cayé-Thomasen, Breinegaard, & Jensen, 2010; Percy-Smith et al., 2008); but again the findings have been mixed (Hintermair, 2006; Polat, 2003). It has been proposed that regardless of modality, the consistent communication mode match between deaf children and parents, and/or satisfaction with communication at home is more influential on psychosocial outcomes (Batten et al., 2014). The LOCHI study showed that, at 3 years of age, children with spoken-only communication mode scored better than those with mixed mode on self-help and gross motor domains, but there was no difference on the social quotient from the CDI.
Summary and Aims of the Study
This overview of the literature demonstrates the wide heterogeneity among studies of psychosocial development in children with hearing loss in terms of age ranges, outcome measures used, and findings. Overall the findings have been inconsistent regarding the direct and indirect contribution of specific risk/protective factors including language, communication ability, age of identification, severity of hearing loss, communication mode, and family demographics. Further, the majority of studies have investigated older children or those with a much wider age range who did not have access to UNHS and early intervention. It may be that the findings to date are not applicable to the current generations of DHH children. The finding that children from the LOCHI cohort were performing in the normal range on psychosocial development at 3-years possibly reflects the benefits of early intervention and education, but the question remained whether delays in language could potentially impact on psychosocial development at a later age (Leigh et al., 2015).
The current paper reports on the psychosocial outcomes of children from the LOCHI study at 5 years old. At this age, the majority of children are transitioning from preschool to formal schooling which is one of the major steps in the education continuum and a successful transition to school is important for future emotional, physical and intellectual development (Dobbs, Doctoroff, Fisher, & Arnold, 2006; Yeboah, 2002). The aims of the study were to: 1) investigate the psychosocial development of 5-year-old DHH children and compare with normative populations; 2) examine the risk or protective factors associated with psychosocial outcomes including non-verbal cognitive ability, presence of additional disabilities, severity of hearing loss, hearing device, age at intervention (age of first HA fit, or CI switch on), communication mode and maternal education; and 3) investigate the relationship between language and communication abilities and global psychosocial functioning.
Method
Participants
Families with children born between May 2002 and August 2007 in the Australian states of New South Wales, Victoria and Queensland who were identified with hearing loss and fitted with amplification before 3 years of age were invited to participate in the study. The data presented here were collected as part of the LOCHI study, but here we specifically focused on children’s psychosocial outcomes, and relate those outcomes to data collected at 5 years of age on the children’s language, communication, and cognitive outcomes, and demographic characteristics. Detailed information about the LOCHI study has been presented previously by Ching and colleagues (2013; 2013). Data on psychosocial outcomes were available for 356 children enrolled in the LOCHI study when they were turning 5-years old (M = 61.6 months, SD = 1.9; range 58 to 76 months). Children who had not been fitted with a hearing aid or cochlear implant, or who were no longer using hearing aids at 5-years (n=3), were excluded from the current study analyses.
Procedure
Each child’s caregiver completed a number of questionnaires which were analysed for this report including the Child Development Inventory (CDI; Ireton, 2005), Strengths and Difficulties Questionnaire (SDQ; Goodman, 1997), Parents’ Evaluation of Aural/Oral Performance of Children (PEACH; Ching & Hill, 2007), and a custom-designed demographic questionnaire. Each of these measures are explained in detail below.
Data regarding children’s age at first hearing aid fitting, degree of hearing loss (4 frequency average [4FA]), type of hearing device, and age at cochlear implant switch-on, were provided by Australian Hearing (the Australian Government agency which provides audiological services for all Australian children who are residents or citizens). A speech pathologist administered the Preschool Language Scale Fourth Edition (PLS-4; Zimmerman, Steiner, & Pond, 2002) either at the child’s home or school. Non-verbal cognitive ability was assessed by a psychologist using the Wechsler Nonverbal Scale of Ability (WNV; Wechsler, Naglieri, & Petermann, 2006).
Outcome Measures
Psychosocial Outcomes
Child Development Inventory (CDI)
The CDI (Ireton, 1992) is a parent-rated standardized questionnaire designed to assess children’s development from 15 months to 6 years of age. Although the CDI has eight subscales, we focus on one CDI subscale that describes aspects of social skills development. The Social subscale of the CDI (40 items) measures aspects of personal and group interaction and social behaviours including care and concern for others (e.g., “shows sympathy to other children”), initiative (e.g., “asks for help in doing things”), independence (e.g., “shows leadership among children his/her age”), and social interaction (e.g., “makes or builds things with other children”).
Published normative data (Ireton & Glascoe, 1995) were used to recalculate children’s individual results into developmental ages, which were then used to derive quotient and Z-scores. Quotients were calculated by dividing the child’s developmental age by their chronological age, expressed as a percentage. Children whose developmental age for a particular subscale matched their chronological age received a quotient of 100, a quotient between 70 and 80 is considered ‘borderline’, and a quotient of 70 or less is considered ‘delayed’ (Ireton & Glascoe, 1995). Z-scores were calculated by subtracting the child’s chronological age from developmental age, and dividing this by 1 standard deviation (i.e., 15% of the chronological age (Ireton & Glascoe, 1995)). There were 317 CDI forms completed by parents. Missing data were most commonly due to the forms not being returned.
Strengths and Difficulties Questionnaire (SDQ)
The SDQ (Goodman, 1997) is a 25-item screening measure designed to identify behavioural and emotional problems in children. The instrument consists of five subscales: conduct problems (e.g., fights with others), hyperactivity (e.g., restless/easily distracted), emotional symptoms (e.g., many worries, often unhappy), peer problems (e.g., picked on or bullied) and prosocial behaviour (e.g., considerate of others feelings). Each subscale consists of 5 items rated on a 3-point response scale from 0= ‘not true’, 1= ‘somewhat true’ to 2= ‘certainly true’. Scores from each domain (excluding prosocial behaviour) were summed to make a ‘total difficulties score’. Higher scores on the prosocial domain reflect strengths, whereas higher scores on the remaining sub-scales and total difficulties scores indicate greater psychopathology. Z-scores were calculated from recent Australian normative data of children aged 5 years (Kremer et al., 2015). All difficulties scores were reversed so that higher Z-scores reflected better psychosocial functioning. There were 333 completed forms returned for the SDQ. Missing data were most commonly due to the forms not being returned.
Language Outcomes
Preschool Language Scale-fourth edition (PLS-4)
The PLS-4 (Zimmerman et al., 2002) is a standardised language test used to identify language disorders between birth and 6;11 (years; months). The test contains two subscales of Expressive Communication (EC) and Auditory Comprehension (AC), which are combined to derive a ‘Total language score’. The EC subscale items for preschool age include naming of common objects, using concepts to describe objects, defining words, and using grammatical constructions. The AC subscale includes items that assess comprehension of vocabulary, concepts, complex sentences and drawing inferences. Standard scores and age-equivalent scores were calculated using normative data. There were 25 children in the study who were not able to complete the PLS-4 due to various reasons including: being from a non-English speaking background (n=4), not wearing their HA on the day of testing (n=1), not being available for testing (n=5), compliance issues (n=2), or unable to cope with the level of testing (n=13). There were also 21 children who required the PLS-4 to be administered using simultaneous communication methods (i.e., a combination of signed and oral communication) making calculation of standard scores inappropriate for this group.
The Parents’ Evaluation of Aural/Oral Performance of Children (PEACH)
The PEACH (Ching & Hill, 2007) is a measure of functional communicative performance in everyday life as judged by caregivers. The test contains 13 questions, two of which address the child’s use of sensory devices. The remaining 11 questions solicit information about the child’s ability to listen and communicate in quiet and in noise, to use the telephone, and to respond to environmental sounds in everyday situations. An overall functional performance score was calculated using the summed ratings provided by caregivers in response to the 11 questions. Higher scores reflect better listening outcome for all sounds. Z-scores were derived from published normative data on children with normal hearing (Ching & Hill, 2007). There were 299 PEACH forms completed and returned. Missing data were mostly due to the forms not being returned.
Non-verbal Cognitive Ability
Non-verbal cognitive ability was assessed using the Wechsler Non-verbal Scale of Ability (WNV; Wechsler et al., 2006), which is a standardised assessment specifically devised for linguistically diverse populations, including people with hearing loss. The assessment comprises 4 subtests – matrices, coding, object assembly and recognition (for children ages 4;0 – 7;11) which combine to provide a full-scale IQ score. WNV scores were obtained from 291 children. There were 68 children who were unable to complete the WNV test. This was due to inability to cope with the demands of the test (n=22), not being available for testing (n=38), or ‘other’ reasons (n=8).
Demographic questionnaire
The custom-designed questionnaire that was completed by caregivers provided demographic information, including children’s birth weight, diagnosed disabilities in addition to hearing loss, communication mode at home (speech only, sign only, or a combination), location (residential postcode), and the caregivers’ own educational experience. Socio-economic status was measured using the Index of Relative Socio-economic Advantage and Disadvantage (IRSAD; Australian Bureau of Statistics, 2006) that is scored in deciles (1–10) with higher scores indicating greater advantage.
Data analysis
All statistical analysis was conducted using SPSS Statistics Package 21. With respect to device, children were grouped into those with HAs or CIs. A single child who used sign language only to communicate was grouped with children who used a combination of speech and sign communication for analysis purposes. Multivariate analyses of variance were conducted to investigate for any differences according to gender or hearing device on psychosocial scores from the CDI and SDQ. Spearman Rho correlation analysis was conducted to test for associations among psychosocial outcomes, child, family and audiological predictor variables and language outcomes.
To reduce the effect of measurement error and other random variations in individual test scores across the SDQ and CDI, all scales were combined to make an aggregate ‘global psychosocial score’. This approach was supported by a factor analysis which indicated one underlying factor that accounted for 62% of the variance. The global score was calculated by averaging the Z-scores from SDQ total difficulties score, SDQ prosocial score and CDI social skills score.
For missing data, basal scores on the WNV were given to 3 children who were unable to complete the tests due to severe intellectual disabilities. One child was given a basal score on the PLS-4 due to an inability to cope with the material and a corresponding severely impaired score on the CDI parent-rated language ability. For the regression analyses, a multiple imputations method (with 10 imputations) was used for handling the remaining missing data in predictor variables.
To examine the predictive value of child, family, intervention and language/communication variables on psychosocial variables, separate hierarchical multiple regression analyses were run with the aggregate global psychosocial Z-score as the dependent variable. In total there were 9 predictor variables. These included nonverbal cognitive ability (WNV standard score), presence of additional disabilities (no/yes), severity of hearing loss (4FA), device (HA vs. CI), age at intervention (first HA fitting for children with HAs or age at first switch-on for children with CIs), communication mode at home (spoken only vs. combination of sign and spoken), maternal education (<12 years, diploma/certificate, or university education), language ability (PLS-4 total Z-score) and functional communication scores (PEACH Z-score).
To address the second and third aims of the study, data were analysed in a two-step model. Demographic (non-verbal cognitive ability, presence of additional disabilities, severity of hearing loss, home communication mode, and maternal education) and intervention (device, age at intervention) factors were entered in the first step of the model. As language and communication scores are thought to be the key determinants of psychosocial outcomes in DHH children, PLS-4 Total and PEACH Z-scores were entered into the second step to examine the direct effects of these predictors after controlling for all child, family and intervention factors. A significance value of p<.05 was used for all analyses.
Results
Demographics
Demographic information describing the children and their caregivers is presented in Table 1. There were 194 males and 162 females. More children wore hearing aids (66.3%) than cochlear implants (33.7%). Of the 37.5% of children who had additional disabilities, the most common were developmental delay (n=38), visual disability (n=22), cerebral palsy (n=20) and autism spectrum disorder (n=12). Most of the children used spoken only communication (270, 79.9%), followed by a combination of oral and manual communication (67, 19.8%). Only 1 child used sign only. Children were generally from areas of less disadvantage with a median IRSAD decile of 7. Approximately 40% of mothers had some university education. Non-verbal cognitive ability of the children was on average in the normal range (M=101.8, SD=16.96). Ten children scored <70 (i.e. 2 SDs below the normative population) on the WNV indicating intellectual impairment.
Table 1.
Demographic characteristics of participants (N=356)
| Child characteristics | ||
|---|---|---|
| Gender | Male Female |
194 (54.5%) 162 (44.5%) |
| Device | Hearing aid Cochlear implant |
236 (66.3%) 120 (33.7) |
| Additional disabilities | Absent Present Not reported |
222 (64.0%) 125 (36.0%) 9 |
| Severity of hearing loss | Mild (20–40 dB HL) Moderate (41–60 dB HL) Severe (61–80 dB HL) Profound (>80 dB HL) |
60 (16.9%) 122 (34.3%) 57 (16.0%) 117 (32.9%) |
| Age at first hearing aid fitting (months) | Mean (SD) Median Interquartile range |
9.79 (10.68)5.0 2–15 |
| Age at first cochlear implant switch-on (months) |
Mean (SD) Median Interquartile range |
24.55 (19.21) 18.47 10.2–31.77 |
| Maternal education | School Diploma or certificate University Not reported |
106 (31.6%) 88 (26.3%) 141 (42.1%) 21 |
| Socio-economic status (IRSAD Decile) |
Mean Median Interquartile range |
7.0 7.0 5.25–9 |
| Communication mode in intervention | Aural/oral only Oral and sign Sign only Not reported |
277 (79.4%) 70 (20.1%) 2 (0.6%) 7 |
| Nonverbal cognitive ability (WNV scaled score) (n=291) |
Mean (SD) Range |
101.81 (16.96) 30–136 |
Psychosocial outcomes compared to normative data
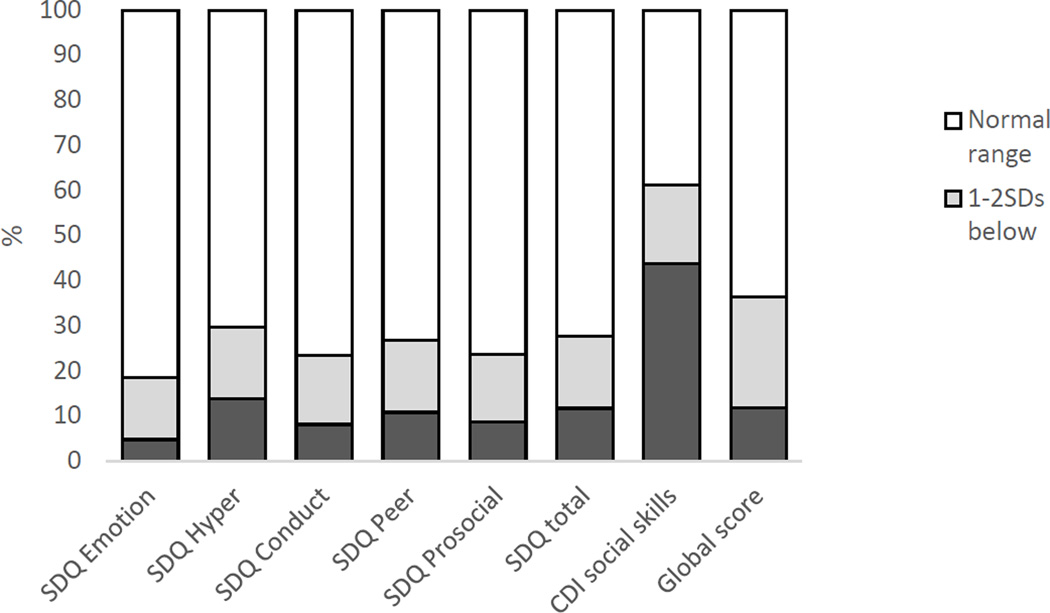
The means, standard deviations and Z-scores derived from published normative data (Ireton & Glascoe, 1995; Kremer et al., 2015) for each psychosocial and language measure are presented in Table 2. On average, the children fell in the borderline range (mean quotient = 78.44, Z=-1.42) on social skills development on the CDI. However, the standard deviation was very high (SD=29.32) suggesting a wide variability of scores. In contrast, the average Z-scores for all domains of the SDQ fell within the normal range, although again variability was high. The aggregated global psychosocial score was also in the average range (Mean Z = −0.67). Using published normative data (Kremer et al, 2015), the proportion of children falling more than 2SDs below the norm were calculated. Scores in this range is thought to indicate a clinically significant problem. Approximately 14% of the children fell ≥2SDs below the norm in the hyperactivity domain, 11% in the peer problems and total difficulties domain, and 8% for conduct problems and prosocial behaviour (see Figure 1). The aggregated global psychosocial score was in the average range (Mean Z= −.67). Thirty-six percent of children fell 1 SD below the norm for the global psychosocial score. A large proportion (44%) fell ≥2SD below the norm of the CDI social skills score. Twelve percent of children fell 2 SDs below the norm for the global psychosocial score. Multivariate analyses revealed no significant differences between CI and HA users, and no difference between the genders. There was no significant interaction between gender and device on any psychosocial domain.
Table 2.
Means (SDs) for Psychosocial and Language Outcomes
| Total | Males | Females | ||
|---|---|---|---|---|
| CDI | (n=317) | (n=173) | (n=143) | |
| Social |
Mean Quotient (SD) Z-score (SD) |
78.44 (29.32) -1.42 (1.95) |
76.66 (30.15) -1.55 (2.01) |
80.81 (28.16) -1.26 (1.88) |
| SDQ | (n=333) | (n=181) | (n=152) | |
| Emotion |
Raw Score (SD) Z-score (SD) |
1.38 (1.63) -.027 (1.01) |
1.27 (1.49) .012 (.935) |
1.52 (1.77) -.074 (1.10) |
| Conduct |
Raw Score (SD) Z-score (SD) |
1.67 (1.57) -.542 (1.18) |
1.77 (1.64) -.333 (1.16) |
1.55 (1.47) -.413 (1.14) |
| Hyperactivity |
Raw Score (SD) Z-score (SD) |
3.95 (2.61) -.370 (1.13) |
4.40 (2.68) -.556 (1.17) |
3.42 (2.41) -.525 (1.19) |
| Peer problems |
Raw Score (SD) Z-score (SD) |
1.62 (1.79) -.279 (1.22) |
1.85 (1.92) -.427 (1.27) |
1.36 (1.58) -.102 (1.13) |
| Prosocial |
Raw Score (SD) Z-score(SD) |
8.64 (5.09) -.254 (1.17) |
7.36 (2.24) -.339 (1.20) |
8.26 (1.92) -.152 (1.13) |
| Total |
Raw Score (SD) Z-score (SD) |
8.63 (5.09) -.467 (1.05) |
9.29 (5.29) -.478 (1.06) |
7.86 (4.74) -.453 (1.06) |
|
Global psychosocial Score |
Z-score (SD) |
(n=296) -.663 (1.05) |
(n=162) -.745 (1.13) |
(n=134) -.562 (.936) |
| PLS-4 | (n=301) | (n=165) | (n=136) | |
| EC |
SS (SD) Z-score (SD) |
83.48 (19.91) -1.10 (1.33) |
81.99 (19.27) -1.20 (1.28) |
85.27 (20.58) -.982 (1.37) |
| AC |
SS (SD) Z-score (SD) |
85.12 (19.77) -.992 (1.32) |
84.19 (19.56) -1.05 (1.30) |
86.23 (20.03) -.918 (1.34) |
| Total |
SS (SD) Z-score (SD) |
83.38 (20.58) -1.11 (1.37) |
81.98 (20.13) -1.21 (1.34) |
85.07 (21.05) -.996 (1.40) |
| (n=298) | (n=162) | (n=137) | ||
|
PEACH Parent |
SS (SD) Z-score |
89.71 (13.47) -.686 (.898) |
75.03 (18.32) -.743 (.926) |
78.07 (16.26) -.620 (.862) |
Note: EC=expressive communication, AC=auditory comprehension, SS=scaled score
Figure 1.
Proportion of children falling below 1 and 2SDs from normative data
Table 3 presents the Spearman’s Rho correlations between all child, family and intervention factors with language, communication, and global psychosocial functioning. As expected, the majority of subscales were significantly correlated with each other. As seen, psychosocial functioning was significantly associated with all child and family factors including non-verbal cognitive ability, presence of disabilities, home communication mode, and maternal education. It was also significantly correlated with both PLS-4 and PEACH scores. There were no significant relationships found among severity of hearing loss, device used, and age at intervention.
Table 3.
Spearman Rho’s correlations between predictor variables and global psychosocial function
| Disabil | 4FA | Comm mode |
Maternal ed |
Device | Age int | PLS-4 | PEACH | Psychosoc | |
|---|---|---|---|---|---|---|---|---|---|
| WNV | −.365** | −.123 | −.166 | .224** | −.058 | −.037 | .493** | .194* | .352** |
| Disabil (N:Y) | −.001 | .292** | −.015 | −.027 | .017 | −.334** | −.258** | −.344** | |
| 4FA | .260** | .022 | .778** | .198** | −.258** | .020 | −.012 | ||
| Comm mode (O:C) | −.020 | −.204** | .092 | −.304** | −.166** | −.183** | |||
| Maternal ed | −.044 | −.110 | .269** | .247** | .219** | ||||
| Device (HA:CI) | .395** | −.149 | .089 | .056 | |||||
| Age int | −.183* | −.097 | −.043 | ||||||
| PLS-4 | .318** | .451** | |||||||
| PEACH | .401** |
Note: Disabil = presence of additional disabilities; Age int= age of HA fit or CI switch on; Psychosoc = global psychosocial score
p<.01,
p<.001
Demographic and Audiological Predictors
To examine the intrinsic and extrinsic predictors of psychosocial development, a multiple regression analysis was conducted with the aggregate global psychosocial score as dependent variables. Child (WNV, presence of disabilities [No:Yes]), audiological (device [HA:CI], severity of hearing loss, and age at intervention [first HA fit or CI switch on], and family (home communication mode [Oral:Combined] and maternal education) factors were entered simultaneously as predictors. The first column (i.e., Model 1) in Table 4 below shows the effect sizes and p-values for demographic predictors for the psychosocial scores. For the categorical variables, the change in predictor is expressed as a change in value from the reference value.
Table 4.
Effect size and 95%CI predicting global psychosocial outcomes (Z-score) for DHH children
| Model 1 | Model 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| B | 95%CI | p | B | 95%CI | p | |||
| WNV | .021 | .013 | .029 | <.001 | .015 | .007 | .023 | .000 |
| Add disabilities | −.433 | −.693 | −.173 | .001 | −.277 | −.530 | −.025 | .031 |
| Device (HA:CI) | .246 | −.171 | .663 | .248 | .066 | −.336 | .468 | .748 |
| Severity of HL | −.007 | −.182 | .168 | .934 | .078 | −.092 | .248 | .369 |
| Age at intervention | .002 | −.008 | .012 | .689 | .007 | −.003 | .016 | .174 |
| Comm mode (O:C) | −.309 | −.609 | −.010 | .043 | −.149 | −.441 | .143 | .318 |
| Maternal Ed | .146 | .009 | .283 | .036 | .004 | −.138 | .146 | .956 |
| PLS-4 Total Z | .174 | .077 | .271 | <.001 | ||||
| PEACH Z | .279 | .138 | .421 | <.001 | ||||
| Adjusted r2 | .227 | .322 | ||||||
Note: O=oral only, C=combined communication
As seen, non-verbal cognitive ability and additional disabilities, were the strongest predictors of global psychosocial functioning. Controlling for other variables, children with additional disabilities scored 0.43 SDs lower than children without disabilities. The two other significant factors in the first model were home communication and maternal education. Children with combined communication mode scored 0.31 SDs lower than children with spoken only communication mode; and higher maternal education level was related to better global psychosocial outcomes. In contrast, audiological factors including device, severity of hearing loss and age at intervention were not significant predictors of any psychosocial outcome. All together, the variables accounted for 22.7% of the variance in global psychosocial development.
Language and Communication Abilities
As seen in Table 3, better language and communication skills were the factors most strongly correlated with psychosocial outcomes. To examine the direct effect of these variables on psychosocial outcomes after controlling for audiological and demographic factors, language and communication measures were entered into the second step of the regression analyses (see Model 2 of Table 4). The addition of the PLS-4 and PEACH scores significantly increased the proportion of variance explained for all psychosocial scores by 9.5%. After controlling for all other factors, both the PLS-4 and PEACH scores were strongly and significantly associated with outcomes, however, the PEACH had a higher effect size than the PLS-4. After controlling for language and communication scores, only non-verbal cognitive ability and additional disabilities remained significant predictors of outcomes, whereas maternal education and communication mode were no longer significant.
Discussion
This study set out to 1) evaluate the psychosocial development of DHH children at 5 years of age relative to age norms, 2) identify the potential risk and protective factors, and 3) examine the relationship between psychosocial outcomes and language. Against these aims, the results showed that by 5 years of age, Australian DHH children are on average within the typical range on global psychosocial functioning (Z-score = −.67). However, the variability was high (SD=1.05) and a relatively high proportion (11.7%) of DHH children were falling more than 2 SDs below the norm on the global score, in contrast to 2.5% of the normative population. This indicates a higher proportion of DHH children still show an increased risk of psychopathology or social developmental problems. The factors that significantly predicted better global psychosocial functioning included absence of additional disabilities, higher non-verbal cognitive ability, language ability, and functional communication skills.
Psychosocial Outcomes at 5 years
In line with the previous findings at 3 years, (Leigh et al., 2015), the current results show that on average, children in the LOCHI study are within the range of typically developing children on global psychosocial outcomes at 5 years. The results for this cohort are consistent with findings from the meta-analysis of 12 SDQ studies by Stevenson et al. (2015) that found that DHH children and adolescents (aged 3–18 years) were on average in the normal range, with a total difficulties score only 0.23 SDs different from hearing children. Stevenson et al. (2015) suggested that this low overall estimate of effect size may reflect improvements in the provision of educational support, newborn hearing screening, and early intervention for DHH children. Stevenson et al. also cautioned that there may have been a reduction in effect size associated with the use of a general population comparison sample that covered wide age ranges. The comparison population was a UK sample with age ranges from 5–10 and 11–18 years (Meltzer, Gatward, Goodman, & Ford, 2000). In the current study, the most recent Australian community data (Kremer et al., 2015) were used, which specified norms at age 5 and by gender. The results showed that all mean SDQ subscales scores were within 1SD of the normative population. This suggests that, on average, the current generation of DHH children are not showing significantly more emotional and/or behavioural problems than their hearing peers, at least on this particular measure.
It warrants close attention that there were still a relatively high proportion of children falling more than 2 SDs below the norm, in the majority of sub-domains except for emotional difficulties (see Figure 1).These higher rates are more similar to those reported in previous studies using the SDQ (J. Fellinger et al., 2008; Hintermair, 2007). Stevenson et al.’s (2015) review found that peer problems were the most common area of concern across studies using the SDQ. This supports the general notion that peer/social relationships are difficult for DHH children and they suggested this could be due to delays in pragmatic language development. Stevenson et al. did not find elevated rates of problems in hyperactivity or conduct; however, there were very few studies included in their review that focused on younger age groups. A recent study that used the SDQ in a small group (n=35) of 4–5 year old DHH children in Norway found higher rates of emotional, hyperactivity, and peer problems in DHH children compared to a hearing community sample (Laugen et al., 2016). However, despite a number of studies finding increased executive deficits in DHH children, including problems with impulsivity and sustained attention (Barker et al., 2009; Khan, Edwards, & Langdon, 2005), there appears to be no evidence that DHH children have higher rates of attention deficit disorders (ADDs). Nevertheless, the ‘hyperactivity’ subscale of the SDQ includes aspects of both hyperactivity and inattention, which are symptoms of two related but distinct types of ADDs. Future studies could examine if there are differences between these two subtypes of attentional problems in DHH children.
Although on average SDQ scores fell within normal limits, CDI social skills scores were on average 1.4 SDs below age level and fell in the borderline range which is a decrease from the results at 3 years (Leigh et al., 2015). The discrepancy between the two scales may be related to the fact that CDI has a bimodal response format (yes/no), and the items cover social expressive and receptive communicative skills (e.g. greets people with ‘hi’; says ‘I can’t’, ‘I don’t know’ or ‘You do it’; understands ‘wait a minute’) and pragmatic language skills (e.g. apologizes when doing something wrong, asks for help, plays games that involve turn-taking) compared to the SDQ. Therefore the two subscales cover quite different domains of psychosocial development. Nevertheless, developmental research in hearing children has found that early social isolation and peer rejection are linked to later internalising and externalising problems (Hymel, Rubin, Rowden, & LeMare, 1990); and in turn, early behavioural problems are a relatively stable risk factor for later maladjustment, particularly in the presence of family dysfunction and stress (Campbell, Shaw, & Gilliom, 2000; Hinshaw, 1992). Therefore, early identification, monitoring and intervention is crucial to improve later psychosocial functioning. It is still not clear whether emotional/behavioural difficulties might increase with age in this cohort, and whether self-report rather than parent-rated reports might reveal further differences when the children enter adolescence (Punch & Hyde, 2011).
Risk/Protective Factors Predicting Global Psychosocial Functioning
The second aim of this study was to investigate the potential child, audiological and family-related factors that influence global psychosocial outcomes. The results showed that non-verbal cognitive ability and the presence of additional disabilities were the strongest predictors of global psychosocial outcomes, followed by home communication mode and maternal education. The results are fairly consistent with the findings at 3 years of age, where the presence of disabilities and birth weight were the two factors associated with the Social and Self-Help subscales of the CDI (Leigh et al., 2015). At 3 years, non-verbal cognitive ability could not be reliably measured; but birth weight is known to be significantly correlated with cognitive ability in childhood (Shenkin, Starr, & Deary, 2004).
Low IQ and presence of disabilities have frequently been found to be significant predictors of both language and psychosocial outcomes in DHH children across multiple studies (Dammeyer, 2010; Geers, Nicholas, & Sedey, 2003; Kushalnagar et al., 2007; Polat, 2003; Theunissen, Rieffe, Kouwenberg, et al., 2014; Van Eldik, 2005). The relationship between additional disabilities and outcomes in the same cohort are discussed in a separate paper in this issue (Cupples et al., under review). The findings suggest that children with additional disabilities are at high risk for psychosocial problems, even after controlling for the effects of cognitive ability. Future research could also investigate which specific additional disabilities or comorbidities have the greatest impact on psychosocial outcomes.
In line with the data at 3 years, audiological factors including device, age at intervention and severity of hearing loss did not predict global psychosocial outcomes. Similarly Theuniessen and colleagues (2014) reported that the majority of literature found no influence of the degree of hearing loss on psychopathology, but in contrast, found children with CIs to have better psychosocial outcomes than children with HAs, and that age at intervention significantly influenced outcomes. Two factors might have contributed to this difference in findings. It could be that previous studies were typically carried out on older children/adolescents, or that the average age of identification and intervention has typically been later in previous studies. To illustrate, the average age of amplification for the newborn hearing screening group was 15.7 months in Korver et al., (2010), and 22.8 months in Laugen et al., (2016). In contrast, the average age of fit for the current cohort was 9 months, and 58% were fitted before 6 months of age. Consistent with the current findings, Stevenson et al. (2011) found no effect of age at identification (before and after 9 months of age) on SDQ scores in DHH children aged 5–12 years, despite the fact that children who were earlier identified had better language scores. Leigh et al. (2015) previously suggested that there may be an interaction between hearing loss, engagement in school education and psychosocial well-being such that hearing loss may only affect psychosocial functioning once children are engaged in formal schooling. At 5 years, many of the children were only just transitioning between pre-school and formal schooling. The prospective nature of the LOCHI study will allow us to see whether changes in psychosocial functioning and predictive factors develop into older school-age as the demands of school and classroom dynamics become more complex.
Both family-related factors of home communication mode and maternal education were also found to be significantly related to global psychosocial outcomes in the first regression model. Children who used spoken-only communication scored 0.31SDs higher on global psychosocial functioning than those who used a combination of sign and spoken mode after controlling for other demographic and audiological factors. However, use of a combined communication mode are likely related to limitations of the child’s oral language skills, for example, due to additional disabilities. In line with this, communication mode was found to no longer predict global psychosocial outcomes once language and functional communication abilities were controlled for.
Developmental literature in hearing children has shown that higher maternal education is associated with higher quantity and quality of speech, more speech that elicits conversation (Hoff, 2003), and lower rates of psychopathology (Bradley & Corwyn, 2002). At age 3, maternal education was a significant predictor of language outcomes in the children from the LOCHI study (Ching, Dillon, et al., 2013), but not social development as rated on the CDI (Leigh et al., 2015). This change over time is consistent with research indicating that the relationship between indices of SES and socioemotional well-being only begin to emerge in early childhood, and become more stable in middle childhood (Bradley & Corwyn, 2002; McLeod & Shanahan, 1993). Mothers with higher education may have greater social capital, social support, adaptive coping skills, and lower stress levels (Bornstein & Bradley, 2014; Bradley & Corwyn, 2002; Richman, Miller, & LeVine, 1992). As these aspects all have the potential to be modified, investigation into these areas in DHH children will be important for informing therapeutic and educational responses for children from more diverse SES backgrounds. Nevertheless, the current results showed that the relationship between maternal education and psychosocial functioning was mainly driven by the children’s language and communication abilities.
Language and Communication Skills Predict Global Psychosocial Functioning
The final aim of this study was to investigate the relationship between language, communication and psychosocial outcomes. In line with the results at 3 years, both the PLS-4 and PEACH scores were significantly correlated with the majority of psychosocial domains. The current study tested the direct predictive relationship between language/communication abilities and global psychosocial functioning holding all other variables constant, and showed that both factors were highly significant predictors of global psychosocial outcomes. These two variables significantly increased the proportion of variance explained by almost 10%. This result supports the general contention that better language and communication in DHH children is directly related to their psychosocial functioning (Barker et al., 2009; Stevenson et al., 2010). This finding has important implications for DHH children given that, delays in language ability have been found despite early identification through UNHS, early amplification and intervention (Ching et al., 2010).
PEACH scores were on average slightly better than PLS-4 scores, and had the strongest effect size on psychosocial outcomes. Netten et al. (2015) found communication skills (on the MacArhur Bates Communicative Development Inventory) correlated significantly with social and behavioural outcomes on the SDQ, whereas language scores did not. This suggests that even children who develop good language ability with the help of a hearing device may have psychosocial difficulties if they struggle to communicate at a functional level. For the DHH population this might occur particularly in difficult listening environments such as talking in a group of people, in a classroom or playground situation (Punch & Hyde, 2011). The PLS-4 is a standardised test carried out in ‘ideal’ listening situations (i.e., one-on-one in a quiet room), whereas the PEACH specifically asks parents to rate the child’s listening/attention/communication skills in both quiet and in noisy situations, and also asks questions that relate to social skills at a certain level (e.g., whether the child regularly initiates conversations or can follow a conversation). In this way, it could be considered to provide a reflection of more pragmatic aspects of language. In sum, the findings indicate that the PEACH may be a useful screening tool. It has the benefit of being suitable for use with very young children and children who cannot complete standardised testing due to additional disabilities. As the PEACH is available in a range of languages, it is also suitable for use with families from non-English speaking backgrounds (NESB).
Although speech and language are typically targeted as the focus of early intervention in DHH children, developing functional social communicative skills may also benefit DHH children’s psychosocial well-being (e.g., teaching pragmatic skills such as understanding turn-taking, active listening, and nuances/intonation, as well as providing greater exposure to group play among hearing children). DHH children may have difficulties hearing peer discussions or teacher directions, particularly in a noisy classroom environment (Punch & Hyde, 2011), highlighting the importance of environmental modifications such as classroom acoustics, seating position, and use of FMs. Improving both language and functional communication skills would be particularly beneficial for children from families with lower SES and maternal education; and increased intervention efforts should be targeted at children with lower cognitive ability and/or additional disabilities who are more at risk of psychosocial dysfunction.
Limitations and Future Directions
One of the main limitations of the current study was the reliance on parent-report for assessing child psychosocial outcomes. However, because children as young as those in the current study do not yet have the metacognitive abilities to reliably answer questions, parent-report reflects the current clinical practice in identifying behavioural problems in this population. It is recognised that parents from low educational backgrounds may have difficulties accurately reporting developmental progress. Ireton (1995) reported that the CDI may not be appropriate for all parents as it requires a reading level above 7–8th grade and the normative sample was predominately white and working/middle class. Although the issue of parent reading level remains in question, the present study used translated versions of the CDI and SDQ for families from NESB backgrounds to mitigate the problem of language mismatch.
Typically, clinical diagnoses of childhood emotional and behavioural disorders, would use cross-informant ratings from parents and teachers to demonstrate difficulties across multiple contexts (e.g., at home and school) (Achenbach, McConaughy, & Howell, 1987). Previous studies comparing parent and teacher reports on the SDQ found that parents typically rate more behavioural problems and teachers rate more peer problems (Kolko & Kazdin, 1993). Further, Nicalasen and Dammeyer (2015) found that teacher ratings of DHH children on the SDQ had better psychometric properties including higher internal consistency and better model fit for the 5 factor structure compared to parent ratings. Although the current study only reports on parent-reported psychosocial functioning, the LOCHI study has also collected SDQ data from teachers, and future analyses will directly compare parent and teacher reports of psychosocial functioning.
The final regression model including all variables accounted for 32.2% of the variance in global psychosocial functioning, indicating that there are still other unaccounted for factors that could be directly contributing to outcomes. Other contributing factors to psychosocial functioning to be explored in future research include the child’s emotion recognition and theory of mind (Netten, Rieffe, Theunissen, Soede, Dirks, Briaire, et al., 2015; Slaughter, Imuta, Peterson, & Henry, 2015), executive function (Hintermair, 2013), motor problems (M. J. Fellinger, Holzinger, Aigner, Beitel, & Fellinger, 2015), educational program (i.e., mainstream or school for the deaf) (Nunes, Pretzlik, & Olsson, 2001), pragmatic language abilities (Gilmour, Hill, Place, & Skuse, 2004), understanding of speech in noise (Huber et al., 2015) and parental social capital, stress and depression (Hintermair, 2006; Kushalnagar et al., 2007). Our future studies will investigate some of these potential factors in relation to child outcomes, and whether the psychosocial functioning of at 3 years predicts the 5 year outcomes. We will also examine the relationship between parent, teacher and self-reported psychosocial difficulties when the children are older.
Conclusion
On average, the overall global psychosocial functioning of 5 year old DHH children was within the range of typically developing children. Nevertheless, the variability in outcomes was high and consistent with previous research, approximately 12% of children were falling more than 2SDs below the norm on the global psychosocial score (compared to 2.5% of the normative population). The results showed that for DHH children, those with higher non-verbal cognitive ability, no additional disabilities, and higher language and functional communication abilities had better global psychosocial outcomes. The findings have implications for development of tailored interventions for young DHH children at risk of psychosocial dysfunction, and support the general contention that development of good language and functional communication is necessary for developing sound psychosocial skills. The population-based, longitudinal design of the LOCHI study will enable us to investigate whether there are further changes to psychosocial outcomes over time.
Acknowledgments
We gratefully thank all the children, their families and their teachers for participation in this study. We are also indebted to the many persons who served as clinicians for the study participants or assisted in other clinical or administrative capacities at Australian Hearing, Catherine Sullivan Centre, Hear and Say Centre, National Acoustic Laboratories, Royal Institute for Deaf and Blind Children, Royal Victorian Eye and Ear Hospital Cochlear Implant Centre, the Shepherd Centre, and the Sydney Cochlear Implant Centre.
The project described was partly supported by the National Institute on Deafness and Other Communication Disorders (Award Number R01DC008080). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Deafness and Other Communication Disorders or the National Institutes of Health.
We acknowledge the financial support of the HEARing CRC, established and supported under the Cooperative Research Centres Program – an initiative of the Australian Government. The project was also partly supported by the Commonwealth of Australia through the Office of Hearing Services. We also acknowledge the support provided by New South Wales Department of Health, Australia; Phonak Ltd.; and the Oticon Foundation.
Abbreviations
- 4FA
4 frequency average
- CDI
Child Development Inventory
- CI
Cochlear implant
- DHH
Deaf or hard of hearing
- HA
Hearing aid
- IRSAD
Index of Relative Socio-economic Advantage and Disadvantage
- LOCHI
Longitudinal Outcomes of Children with Hearing Impairment Study
- PEACH
Parent evaluation of Aural/Oral Performance of Children
- PLS-4
Preschool Language Scale Fourth Edition
- NESB
Non-English Speaking Backgrounds
- SD
Standard deviation
- SDQ
Strength and Difficulties Questionnaire
- SES
Socio-economic status
- UNHS
Universal Newborn Hearing Screening
- WNV
Wechsler Nonverbal Scale of Ability
Footnotes
Declaration of Interest
The authors report no declarations of interest.
References
- Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: implications of cross-informant correlations for situational specificity. Psychol. Bull. 1987;101(2):213. [PubMed] [Google Scholar]
- Barker DH, Quittner AL, Fink NE, Eisenberg LS, Tobey EA, et al. Predicting behavior problems in deaf and hearing children: The influences of language, attention, and parent-child communication. Dev. Psychopathol. 2009;21(02):373–392. doi: 10.1017/S0954579409000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batten G, Oakes PM, Alexander T. Factors associated with social interactions between deaf children and their hearing peers: A systematic literature review. J. Deaf Stud. Deaf Edu. 2014;19(3):285–302. doi: 10.1093/deafed/ent052. [DOI] [PubMed] [Google Scholar]
- Bornstein MH, Bradley RH. Socioeconomic status, parenting, and child development. New Jersery: Lawrence Erlbaum Associates Inc.; 2014. [Google Scholar]
- Bornstein MH, Hahn C-S, Suwalsky JT, Haynes OM. The Hollingshead four-factor index of social status and the socioeconomic index of occupations. In: Bornstein MH, editor. Socioeconomic status, parenting, and child development. New Jersey: Lawrence Erlbaum Associates; 2003. pp. 29–81. [Google Scholar]
- Bradley RH, Corwyn RF. Socioeconomic status and child development. Annu. Rev. Psychol. 2002;53(1):371–399. doi: 10.1146/annurev.psych.53.100901.135233. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Shaw DS, Gilliom M. Early externalizing behavior problems: Toddlers and preschoolers at risk for later maladjustment. Dev. Psychopathol. 2000;12(03):467–488. doi: 10.1017/s0954579400003114. [DOI] [PubMed] [Google Scholar]
- Ching TY, Crowe K, Martin V, Day J, Mahler N, et al. Language development and everyday functioning of children with hearing loss assessed at 3 years of age. Int. J. Speech Lang. Pathol. 2010;12(2):124–131. doi: 10.3109/17549500903577022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching TY, Day J, Seeto M, Dillon H, Marnane V, et al. Predicting 3-year outcomes of early-identified children with hearing impairment. B-ENT. 2013;99 [PMC free article] [PubMed] [Google Scholar]
- Ching TY, Dillon H, Marnane V, Hou S, Day J, et al. Outcomes of early-and late-identified children at 3 years of age: findings from a prospective population-based study. Ear Hear. 2013;34(5):535–552. doi: 10.1097/AUD.0b013e3182857718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching TY, Leigh G, Dillon H. Introduction to the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study: Background, design, sample characteristics. Int. J. Audiol. 2013;52(S2):S4–S9. doi: 10.3109/14992027.2013.866342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cupples L, Ching TY, Button L, Leigh G, Marnane V, et al. Predicting outcomes in 5-year-old children with hearing loss and additional disabilities. Int. J. Audiol. doi: 10.1080/14992027.2016.1228127. (under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cupples L, Ching TY, Crowe K, Seeto M, Leigh G, et al. Outcomes of 3-year-old children with hearing loss and different types of additional disabilities. J. Deaf Stud. Deaf Edu. 2014;19(1):20–39. doi: 10.1093/deafed/ent039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dammeyer J. Psychosocial development in a Danish population of children with cochlear implants and deaf and hard-of-hearing children. J. Deaf Stud. Deaf Edu. 2010;15(1):50–58. doi: 10.1093/deafed/enp024. [DOI] [PubMed] [Google Scholar]
- Dobbs J, Doctoroff GL, Fisher PH, Arnold DH. The association between preschool children’s socio-emotional functioning and their mathematical skills. J. Appl. Dev. Psychol. 2006;27(2):97–108. [Google Scholar]
- Fellinger J, Holzinger D, Sattel H, Laucht M. Mental health and quality of life in deaf pupils. Eur. Child Adolesc. Psychiatry. 2008;17(7):414–423. doi: 10.1007/s00787-008-0683-y. [DOI] [PubMed] [Google Scholar]
- Fellinger J, Holzinger D, Sattel H, Laucht M, Goldberg D. Correlates of mental health disorders among children with hearing impairments. Dev. Med. Child Neurol. 2009;51(8):635–641. doi: 10.1111/j.1469-8749.2008.03218.x. [DOI] [PubMed] [Google Scholar]
- Fellinger MJ, Holzinger D, Aigner M, Beitel C, Fellinger J. Motor performance and correlates of mental health in children who are deaf or hard of hearing. Dev. Med. Child Neurol. 2015;57(10):942–947. doi: 10.1111/dmcn.12814. [DOI] [PubMed] [Google Scholar]
- Geers AE, Nicholas JG, Sedey AL. Language skills of children with early cochlear implantation. Ear Hear. 2003;24(1):46S–58S. doi: 10.1097/01.AUD.0000051689.57380.1B. [DOI] [PubMed] [Google Scholar]
- Gilmour J, Hill B, Place M, Skuse D. Social communication deficits in conduct disorder: a clinical and community survey. J. Child Pyschol. Psyc. 2004;45(5):967–978. doi: 10.1111/j.1469-7610.2004.t01-1-00289.x. [DOI] [PubMed] [Google Scholar]
- Goodman R. The Strengths and Difficulties Questionnaire. J. Child Pyschol. Psyc. 1997;38(5):581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Hind S, Davis A. Outcomes for children with permanent hearing impairment; Paper presented at the A sound foundation through early amplification: proceedings of an international conference.2000. [Google Scholar]
- Hinshaw SP. Externalizing behavior problems and academic underachievement in childhood and adolescence: causal relationships and underlying mechanisms. Psychol. Bull. 1992;111(1):127. doi: 10.1037/0033-2909.111.1.127. [DOI] [PubMed] [Google Scholar]
- Hintermair M. Parental resources, parental stress, and socioemotional development of deaf and hard of hearing children. J. Deaf Stud. Deaf Edu. 2006;11(4):493–513. doi: 10.1093/deafed/enl005. [DOI] [PubMed] [Google Scholar]
- Hintermair M. Prevalence of socioemotional problems in deaf and hard of hearing children in Germany. Am. Ann. Deaf. 2007;152(3):320–330. doi: 10.1353/aad.2007.0028. [DOI] [PubMed] [Google Scholar]
- Hintermair M. Executive functions and behavioral problems in deaf and hard-of-hearing students at general and special schools. J. Deaf Stud. Deaf Edu. 2013;18(3):344–359. doi: 10.1093/deafed/ent003. [DOI] [PubMed] [Google Scholar]
- Hoff E. Causes and consequences of SES-related differences in parent-to-child speech. In: Bornstein MH, Bradley RH, editors. Socioeconomic status, parenting, and child development. New Jersey: Lawrence Erbaum Associates; 2003. pp. 147–160. [Google Scholar]
- Hoffman MF, Quittner AL, Cejas I. Comparisons of social competence in young children with and without hearing loss: A dynamic systems framework. J. Deaf Stud. Deaf Edu. 2015;20(2):115–124. doi: 10.1093/deafed/enu040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber M, Burger T, Illg A, Kunze S, Giourgas A, et al. Mental health problems in adolescents with cochlear implants: peer problems persist after controlling for additional handicaps. Front. Psychol. 2015;6 doi: 10.3389/fpsyg.2015.00953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber M, Kipman U. The mental health of deaf adolescents with cochlear implants compared to their hearing peers. Int. J. Audiol. 2011;50(3):146–154. doi: 10.3109/14992027.2010.533704. [DOI] [PubMed] [Google Scholar]
- Ireton H. Child development inventory manual. Minneapolis, MN: Behavior Science Systems; 1992. [Google Scholar]
- Ireton H, Glascoe FP. Assessing Children’s Development Using Parents’ Reports: The Child Development Inventory. Clin. Pediatr. (Phila.) 1995;34(5):248–255. doi: 10.1177/000992289503400504. [DOI] [PubMed] [Google Scholar]
- Jeanes RC, Nienhuys TG, Rickards FW. The pragmatic skills of profoundly deaf children. J. Deaf Stud. Deaf Edu. 2000;5(3):237–247. doi: 10.1093/deafed/5.3.237. [DOI] [PubMed] [Google Scholar]
- Khan S, Edwards L, Langdon D. The cognition and behaviour of children with cochlear implants, children with hearing aids and their hearing peers: a comparison. Audiology and Neurotology. 2005;10(2):117–126. doi: 10.1159/000083367. [DOI] [PubMed] [Google Scholar]
- Kirk KI, Miyamoto RT, Ying EA, Perdew AE, Zuganelis H. Cochlear implantation in young children: effects of age at implantation and communication mode. Volta review. 2000;102(4):127–144. [Google Scholar]
- Kolko DJ, Kazdin AE. Emotional/behavioral problems in clinic and nonclinic children: correspondence among child, parent and teacher reports. J. Child Pyschol. Psyc. 1993;34(6):991–1006. doi: 10.1111/j.1469-7610.1993.tb01103.x. [DOI] [PubMed] [Google Scholar]
- Korver AM, Konings S, Dekker FW, Beers M, Wever CC, Frijns JH, Group DCS. Newborn hearing screening vs later hearing screening and developmental outcomes in children with permanent childhood hearing impairment. JAMA. 2010;304:1701–1708. doi: 10.1001/jama.2010.1501. [DOI] [PubMed] [Google Scholar]
- Kremer P, Silva A, Cleary J, Santoro G, Weston K, et al. Normative data for the Strengths and Difficulties Questionnaire for young children in Australia. Journal of paediatrics and child health. 2015 doi: 10.1111/jpc.12897. [DOI] [PubMed] [Google Scholar]
- Kushalnagar P, Krull K, Hannay J, Mehta P, Caudle S, et al. Intelligence, parental depression, and behavior adaptability in deaf children being considered for cochlear implantation. J. Deaf Stud. Deaf Edu. 2007;12(3):335–349. doi: 10.1093/deafed/enm006. [DOI] [PubMed] [Google Scholar]
- Laugen NJ, Jacobsen KH, Rieffe C, Wichstrøm L. Predictors of Psychosocial Outcomes in Hard of Hearing Preschool Children. J. Deaf Stud. Deaf Edu. 2016:enw005. doi: 10.1093/deafed/enw005. [DOI] [PubMed] [Google Scholar]
- Lederberg AR, Everhart VS. Conversations between deaf children and their hearing mothers: Pragmatic and dialogic characteristics. J. Deaf Stud. Deaf Edu. 2000;5(4):303–322. doi: 10.1093/deafed/5.4.303. [DOI] [PubMed] [Google Scholar]
- Leigh G, Ching TY, Crowe K, Cupples L, Marnane V, et al. Factors affecting psychosocial and motor development in 3-year-old children who are deaf or hard of hearing. J. Deaf Stud. Deaf Edu. 2015;20(4):331–342. doi: 10.1093/deafed/env028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marschark M. Origins and interactions in the social, cognitive, and language development of deaf children. Psychological perspectives on deafness. 1993:7–26. [Google Scholar]
- McLeod JD, Shanahan MJ. Poverty, parenting, and children’s mental health. Am. Sociol. Rev. 1993:351–366. [Google Scholar]
- Meltzer H, Gatward R, Goodman R, Ford T. Mental health of children and adolescents in Great Britain. London: The Stationary Office; 2000. [DOI] [PubMed] [Google Scholar]
- Moeller MP. Early intervention and language development in children who are deaf and hard of hearing. Pediatrics. 2000;106(3):e43–e43. doi: 10.1542/peds.106.3.e43. [DOI] [PubMed] [Google Scholar]
- Moeller MP. Current state of knowledge: psychosocial development in children with hearing impairment. Ear Hear. 2007;28(6):729–739. doi: 10.1097/AUD.0b013e318157f033. [DOI] [PubMed] [Google Scholar]
- Netten AP, Rieffe C, Theunissen SC, Soede W, Dirks E, et al. Low Empathy in Deaf and Hard of Hearing (Pre) Adolescents Compared to Normal Hearing Controls. PLoS One. 2015;10(4) doi: 10.1371/journal.pone.0124102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netten AP, Rieffe C, Theunissen SC, Soede W, Dirks E, et al. Early identification: Language skills and social functioning in deaf and hard of hearing preschool children. Int. J. Pediatr. Otorhinolaryngol. 2015;79(12):2221–2226. doi: 10.1016/j.ijporl.2015.10.008. [DOI] [PubMed] [Google Scholar]
- Niclasen J, Dammeyer J. Psychometric Properties of the Strengths and Difficulties Questionnaire and Mental Health Problems Among Children With Hearing Loss. J. Deaf Stud. Deaf Edu. 2015:env067. doi: 10.1093/deafed/env067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunes T, Pretzlik U, Olsson J. Deaf children’s social relationships in mainstream schools. Deafness & Education International. 2001;3(3):123–136. [Google Scholar]
- Percy-Smith L, Cayé-Thomasen P, Breinegaard N, Jensen JH. Parental mode of communication is essential for speech and language outcomes in cochlear implanted children. Acta Otolaryngol. 2010;130(6):708–715. doi: 10.3109/00016480903359939. [DOI] [PubMed] [Google Scholar]
- Percy-Smith L, Hedegaard Jensen J, Cayé-Thomasen P, Thomsen J, Gudman M, et al. Factors that affect the social well-being of children with cochlear implants. Cochlear Implants International. 2008;9(4):199–214. doi: 10.1179/cim.2008.9.4.199. [DOI] [PubMed] [Google Scholar]
- Peterson CC. Theory-of-mind development in oral deaf children with cochlear implants or conventional hearing aids. J. Child Pyschol. Psyc. 2004;45(6):1096–1106. doi: 10.1111/j.1469-7610.2004.t01-1-00302.x. [DOI] [PubMed] [Google Scholar]
- Polat F. Factors affecting psychosocial adjustment of deaf students. J. Deaf Stud. Deaf Edu. 2003;8(3):325–339. doi: 10.1093/deafed/eng018. [DOI] [PubMed] [Google Scholar]
- Punch R, Hyde M. Social participation of children and adolescents with cochlear implants: A qualitative analysis of parent, teacher, and child interviews. J. Deaf Stud. Deaf Edu. 2011;16(4):474–493. doi: 10.1093/deafed/enr001. [DOI] [PubMed] [Google Scholar]
- Richman AL, Miller PM, LeVine RA. Cultural and educational variations in maternal responsiveness. Dev. Psychol. 1992;28(4):614. [Google Scholar]
- Schick B, De Villiers P, De Villiers J, Hoffmeister R. Language and theory of mind: A study of deaf children. Child Dev. 2007;78(2):376–396. doi: 10.1111/j.1467-8624.2007.01004.x. [DOI] [PubMed] [Google Scholar]
- Shenkin SD, Starr JM, Deary IJ. Birth weight and cognitive ability in childhood: a systematic review. Psychol. Bull. 2004;130(6):989. doi: 10.1037/0033-2909.130.6.989. [DOI] [PubMed] [Google Scholar]
- Slaughter V, Imuta K, Peterson CC, Henry JD. Meta-Analysis of Theory of Mind and Peer Popularity in the Preschool and Early School Years. Child Dev. 2015 doi: 10.1111/cdev.12372. [DOI] [PubMed] [Google Scholar]
- Stevenson J, Kreppner J, Pimperton H, Worsfold S, Kennedy C. Emotional and behavioural difficulties in children and adolescents with hearing impairment: a systematic review and meta-analysis. Eur. Child Adolesc. Psychiatry. 2015;24(5):1–20. doi: 10.1007/s00787-015-0697-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson J, McCann D, Watkin P, Worsfold S, Kennedy C. The relationship between language development and behaviour problems in children with hearing loss. J. Child Pyschol. Psyc. 2010;51(1):77–83. doi: 10.1111/j.1469-7610.2009.02124.x. [DOI] [PubMed] [Google Scholar]
- Stevenson J, McCann DC, Law CM, Mullee M, Petrou S, et al. The effect of early confirmation of hearing loss on the behaviour in middle childhood of children with bilateral hearing impairment. Dev. Med. Child Neurol. 2011;53(3):269–274. doi: 10.1111/j.1469-8749.2010.03839.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tait M, De Raeve L, Nikolopoulos T. Deaf children with cochlear implants before the age of 1 year: comparison of preverbal communication with normally hearing children. Int. J. Pediatr. Otorhinolaryngol. 2007;71(10):1605–1611. doi: 10.1016/j.ijporl.2007.07.003. [DOI] [PubMed] [Google Scholar]
- Theunissen S, Rieffe C, Kouwenberg M, De Raeve L, Soede W, et al. Anxiety in children with hearing aids or cochlear implants compared to normally hearing controls. The Laryngoscope. 2012;122(3):654–659. doi: 10.1002/lary.22502. [DOI] [PubMed] [Google Scholar]
- Theunissen S, Rieffe C, Kouwenberg M, De Raeve LJ, Soede W, et al. Behavioral problems in school-aged hearing-impaired children: the influence of sociodemographic, linguistic, and medical factors. Eur. Child Adolesc. Psychiatry. 2014;23(4):187–196. doi: 10.1007/s00787-013-0444-4. [DOI] [PubMed] [Google Scholar]
- Theunissen S, Rieffe C, Netten AP, Briaire JJ, Soede W, et al. Psychopathology and its risk and protective factors in hearing-impaired children and adolescents: a systematic review. JAMA pediatrics. 2014;168(2):170–177. doi: 10.1001/jamapediatrics.2013.3974. [DOI] [PubMed] [Google Scholar]
- Vaccari C, Marschark M. Communication between Parents and Deaf Children: Implications for Social-emotional Development. J. Child Pyschol. Psyc. 1997;38(7):793–801. doi: 10.1111/j.1469-7610.1997.tb01597.x. [DOI] [PubMed] [Google Scholar]
- Van Eldik T. Mental health problems of Dutch youth with hearing loss as shown on the Youth Self Report. Am. Ann. Deaf. 2005;150(1):11–16. doi: 10.1353/aad.2005.0024. [DOI] [PubMed] [Google Scholar]
- Wake M, Hughes EK, Collins CM, Poulakis Z. Parent-reported health-related quality of life in children with congenital hearing loss: a population study. Ambul. Pediatr. 2004;4(5):411–417. doi: 10.1367/A03-191R.1. [DOI] [PubMed] [Google Scholar]
- Wechsler D, Naglieri JA, Petermann F. Wechsler nonverbal scale of ability: WNV. PsychCorp.; 2006. [Google Scholar]
- Yeboah DA. Enhancing transition from early childhood phase to primary education: Evidence from the research literature. Early Years: An International Journal of Research and Development. 2002;22(1):51–68. [Google Scholar]
- Yoshinaga-Itano C, Apuzzo M-RL. The development of deaf and hard of hearing children identified early through the high-risk registry. Am. Ann. Deaf. 1998;143(5):416–424. doi: 10.1353/aad.2012.0118. [DOI] [PubMed] [Google Scholar]
- Yoshinaga-Itano C, Sedey AL, Coulter DK, Mehl AL. Language of early-and later-identified children with hearing loss. Pediatrics. 1998;102(5):1161–1171. doi: 10.1542/peds.102.5.1161. [DOI] [PubMed] [Google Scholar]
- Yoshinaga-Itano C. Early intervention after universal neonatal hearing screening: impact on outcomes. Mental retardation and developmental disabilities research reviews. 2003;9(4):252–266. doi: 10.1002/mrdd.10088. [DOI] [PubMed] [Google Scholar]
- Zimmerman IL, Steiner VG, Pond RE. Preschool language scale. Vol. 3. San Antonio, TX: Psychological Corporation; 2002. [Google Scholar]