Abstract
Primary optic nerve sheath meningiomas (ONSM) are rare, benign and slow growing tumor involving the intra-orbital/intra-canalicular segment of the optic nerve. Untreated, they can potentially lead to visual deterioration. Magnetic resonance (MR) is the gold standard imaging modality for diagnosing the entity. Often, a clinical dilemma exists to narrow the differential diagnosis of an enhancing intra-orbital mass on MR. Molecular imaging provides a high degree of precision in diagnosing meningioma in view of relatively high levels of somatostatin receptor expression by these tumors. The following case demonstrates the potential clinical utility of somatostatin receptor SPECT using 99mTc- labeled HYNIC-TOC in clinical diagnosis of ONSM.
Keywords: HYNIC TOC, MR, optic nerve sheath meningioma, somatostatin receptor, SPECT
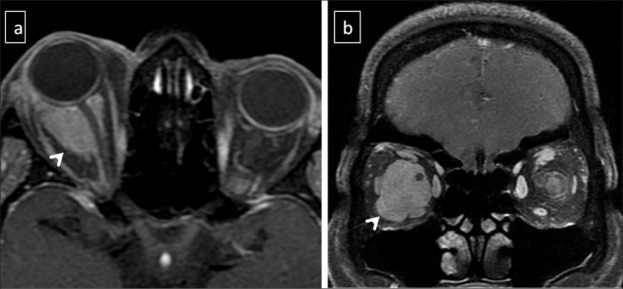
A 54 years old female, presented with mild diminution of vision and proptosis of the right eye with reddening since 3 months. On visual examination, both eyes had visual acuity more than 6/6 and the patient was able to recognize faces at > 12 feet with bilateral pupils showing brisk reflex. Trans-axial and coronal post contrast T1 weighted Magnetic resonance (MR) [Figures 1a and 1b, arrow heads] showed a well defined 2.2 x 2.5cm ovoid homogenously enhancing lesion in the intra-conal compartment of the right orbit. It encases the anterior 2/3rd of the intra-orbital segment of the optic nerve with minimal extension into the extra-conal fat. In view of relatively preserved vision, an invasive biopsy was obviated and for further characterization, patient was referred for somatostatin receptor scintigraphy (SRS). SRS was done 4 hours after intravenous injection of 99mTc labeled hydrazinonicotinyl-Tyr3-octreotide (HYNIC-TOC). Whole body planar image did not show significant tracer uptake in the orbits (Figure 2a). On single photon emission computed tomography/computed tomography (SPECT/CT) images [Figures 2b and 2c] showed focal increased tracer uptake in ovoid lesion encasing the right optic nerve (thin white arrow), consistent with diagnosis of primary optic nerve sheath meningioma. The patient was treated with radiotherapy (a dose of 5040cGy in 28 fractions over 5 weeks) and follow up MR [Figure 2d, bold white arrow] showed interval decrease in the size of the lesion in enhancing lesion.
Figure 1.
Trans-axial and coronal post contrast T1 weighted Magnetic resonance (MR) [Figures 1a and 1b, arrow heads] showed a well defined 2.2 x 2.5cm ovoid homogenously enhancing lesion in the intra-conal compartment of the right orbit encasing the anterior 2/3rd of the intra-orbital segment of the optic nerve with minimal extension into the extra-conal fat.
Figure 2.
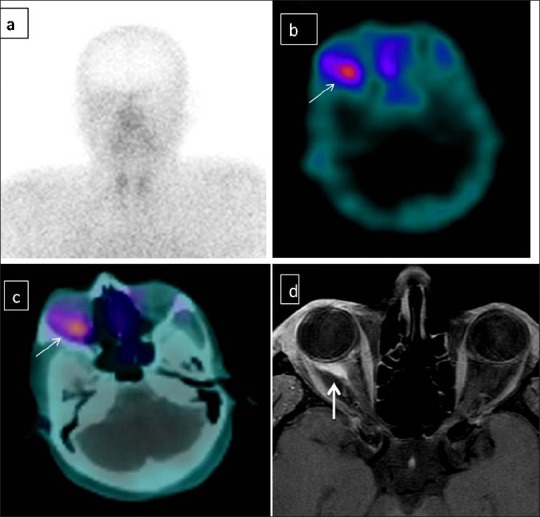
99mTc labeled hydrazinonicotinyl-Tyr3 (HYNIC-TOC) scan. Anterior planar image does show significant tracer uptake in the orbits [Figure 2a]. Single photon emission computed tomography/computed tomography (SPECT/CT) images [Figures 2b and 2c] showed focal increased tracer uptake in ovoid lesion encasing the right optic nerve (thin white arrow). Post radiotherapy follow up MR showed interval decrease in the size of the lesion in enhancing lesion [Figure 2d, bold white arrow].
Optic nerve sheath meningiomas (ONSM) constituting about 2% of all orbital tumors, is a broad term encompassing primary and secondary meningiomas of the optic nerve. Primary ONSM are rare tumors, arising from the meningoepithelial cells of arachnoid villi and can develop at any site along the course of the optic nerve. Secondary OSNM, relatively common, are extensions of meningiomas from other locations (cavernous sinus, planumsphenoidale, sphenoid wing) and involving optic nerve.[1] This disease has a stable clinical course in most patients and treatment is generally reserved for patients with poor visual acuity on initial examination.[2] Definite treatment of primary ONSM requires accurate identification and differentiation from other commoner causes of an enhancing mass encasing the orbital nerve (pseudo-tumor, hemangioma, lymphoma and glioma).[3] Biopsy is difficult given the location of ONSM and its relationship to the pial vascular supply, and diagnosis is usually based on combination of clinical and imaging findings.[3,4]
Molecular imaging using SPECT/CT and PET/CT have shown high sensitivity and specificity in diagnosis of ONSM due to relatively high abundance of somatostatin receptor expression in ONSM.[5,6,7] Semi-quantitative SPECT/CT using threshold lesion/brain uptake ratio of 5.9 has been shown to be 97.2% specific and 100% sensitive for diagnosis of ONSM, differentiating it from other intra-orbital tumors, which show absence or low grade somatostatin receptors expression. Similarly, 68Ga- DOTA-D Phe (1)-Tyr (3)-Octreotide (DOTATOC) PET/CT has been utilized to evaluate symptomatic lesions of optic pathway. The mean standardized uptake value of meningioma in this study was higher (mean SUV-14.3 and that of other non-meningioma lesions like metastasis and inflammatory tissues (mean SUV 2.1).[7] This high diagnostic precision of SPECT/CT and PET/CT aids advanced MR imaging and may obviate the need for a vision-threatening biopsy, as seen in our case. Beyond diagnosis, SRS using 68Ga- DOTATOC PET/CT has been shown to improve the gross tumor volume (GTV) delineation, in comparison to MR, for planning radiotherapy.[8,9] SPECT/CT using Indium-111 labeled octreotide have also been used to follow up patients with ONSM who were treated with stereotactic radiotherapy. SPECT showed significant decrease in the serial tumor uptake in patients who responded to treatment, thereby complementing MR in evaluation of tumor control.[9]
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- 1.Eddleman CS, Liu JK. Optic nerve sheath meningioma: current diagnosis and treatment. Neurosurg Focus. 2007;23:E4. doi: 10.3171/FOC-07/11/E4. [DOI] [PubMed] [Google Scholar]
- 2.Egan RA, Lessell S. A contribution to the natural history of optic nerve sheath meningiomas. Arch Ophthalmol. 2002;120:1505–8. doi: 10.1001/archopht.120.11.1505. [DOI] [PubMed] [Google Scholar]
- 3.Turbin RE, Pokorny K. Diagnosis and treatment of orbital optic nerve sheath meningioma. Cancer Control. 2004;11:334–41. doi: 10.1177/107327480401100508. [DOI] [PubMed] [Google Scholar]
- 4.Lindblom B, Truwit CL, Hoyt WF. Optic nerve sheath meningioma. Definition of intraorbital, intracanalicular, and intracranial components with magnetic resonance imaging. Ophthalmology. 1992;99:560–6. doi: 10.1016/s0161-6420(92)31932-3. [DOI] [PubMed] [Google Scholar]
- 5.Saeed P, Tanck MW, Freling N, Baldeschi L, Mourits MP, Bennink RJ. Somatostatin receptor scintigraphy for optic nerve sheath meningiomas. Ophthalmology. 2009;116:1581–6. doi: 10.1016/j.ophtha.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 6.Schulz S, Pauli SU, Schulz S, Händel M, Dietzmann K, Firsching R, et al. Immunohistochemical determination of five somatostatin receptors in meningioma reveals frequent overexpression of somatostatin receptor subtype sst2A. Clin Cancer Res. 2000;6:1865–74. [PubMed] [Google Scholar]
- 7.Klingenstein A, Haug AR, Miller C, Hintschich C. Ga-68-DOTA-TATE PET/CT for discrimination of tumors of the optic pathway. Orbit. 2015;34:16–22. doi: 10.3109/01676830.2014.959185. [DOI] [PubMed] [Google Scholar]
- 8.Gehler B, Paulsen F, Oksüz MO, Hauser TK, Eschmann SM, Bares R, et al. [68Ga]-DOTATOC-PET/CT for meningioma IMRT treatment planning. Radiat Oncol. 2009;4:56. doi: 10.1186/1748-717X-4-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andrews DW, Faroozan R, Yang BP, Hudes RS, Werner-Wasik M, Kim SM, et al. Fractionated stereotactic radiotherapy for the treatment of optic nerve sheath meningiomas: preliminary observations of 33 optic nerves in 30 patients with historical comparison to observation with or without prior surgery. Neurosurgery. 2002;51:890–902. doi: 10.1097/00006123-200210000-00007. [DOI] [PubMed] [Google Scholar]