Abstract
Cardiac output (CO) is an important indicator of cardiovascular function. Several invasive and non-invasive methods have been developed and validated to assess CO in the clinical setting. These are often computationally complex or proprietarily-restricted, and thus, not feasible in ambulatory investigations and the laboratory research setting. Simple mathematical transforms have been proposed to estimate CO from pulse pressure (PP = mean systolic blood pressure (SBP) minus mean diastolic blood pressure (DBP)), and mean heart rate (HR). Recently we evaluated one such simple technique [CO=(PPxHR)x.002], and found moderate correlation between the CO estimate and Modelflow-derived CO. Here we aimed to evaluate a more sophisticated formula, proposed in 1940 by Liljestrand and Zander. CO was estimated (COEST) dividing PP by the sum of SBP and DBP and multiplying the product by HR. This index was correlated with the Modelflow (3 element Windkessel) -derived CO. Baseline beat-to-beat blood pressure data from 67 young (mean age = 19.94± 2.8), healthy men (n = 30) and women (n = 37) was available for analysis. Overall, the correlation of COEST and CO was moderate (r = .42, p <.0001) and stronger in men (r = .66, p < .0001) compared to women (r = .36, p < .05). These results suggest that at least in some situations the Liljestrand and Zander method may provide an adequate measure of CO when other methods are not available.
Keywords: Cardiac Output, Pulse Pressure, Systolic, Diastolic, Blood Pressure, Heart Rate
INTRODUCTION
Cardiac output (CO) is thought to be the primary compensatory mechanism in response to oxygen demand (e.g., exercise), making CO an important indicator of both blood flow and cardiovascular function [1]. CO has a number of clinical applications and thus, several invasive and non-invasive techniques have been developed to track CO in the clinical setting.
Although non-invasive techniques are often cheaper and easier to implement in comparison to invasive techniques, non-invasive techniques that have been employed are not without complications. Specifically, both non-invasive and invasive techniques that have been proposed are often computationally complex or proprietarily-restricted [2, 3]. Therefore, such techniques may not be feasible in clinical work undertaken in both the laboratory research and ambulatory settings.
To address such difficulties, we recently evaluated a simple mathematical transform based on arterial blood pressure (BP) to estimate CO [3]. The single element Windkessel formula included pulse pressure (PP = mean systolic blood pressure (SBP) minus mean diastolic blood pressure (DBP)), and mean heart rate (HR) measures [CO=(PPxHR)*2ml]. We found good agreement between the estimated CO and Modelflow-derived CO, suggesting that such a formula may be optimal in determining CO in various settings. However recently, we have turned focus toward a more sophisticated approach to derive CO proposed by Liljestrand and Zander [2, 4].
The Liljestrand and Zander (1940) mathematical transformation is more sophisticated in the sense that it is based on empiric features (e.g., total pressure) of arterial BP [2, 4, 5]. In 1928, Liljestrand and Zander proposed a formula to derive stroke volume (SV) using arterial blood pressure – they proposed that SV equaled PP (SBP-DBP) divided by the sum of SBP and DBP. Previous research have provided evidence that SV multiplied by HR is a suitable estimate of CO and thus, it is proposed that the Liljestrand and Zander SV equation could be multiplied by HR to derive an estimate of CO [2, 5]. The aim of the present investigation is to test the validity of this formula against Modelflow derived CO.
METHODS
We evaluated this mathematical transformation in 67 (37 female) apparently healthy undergraduate students (Mean Age 19.94 ± 2.8).
Resting beat-to-beat blood pressure was assessed for 5 minutes using the Finometer® MIDI non-invasive blood pressure monitoring device (FMS Medical Systems, The Netherlands). The Finometer estimates CO using the Modelflow method based on a three-element Windkessel model which has been previously described [6] and shown to produce values comparable to those obtained via thermodilution [7]. Finally, height and weight were recorded and body mass index (BMI) – a measure that adjusts body weight for height – was calculated.
The equation used to derive the estimate of cardiac output (COEST) was as follows: COEST = PP / (SBP+DBP) * HR
Pulse pressure (PP) was calculated as the mean systolic blood pressure (SBP) minus the mean diastolic blood pressure (DBP). PP was then divided by the sum of SBP and DPB, and the product multiplied by HR. All COEST values were then multiplied by a constant (k) to obtain COEST-ADJ values. This constant was calculated by dividing CO by COEST for each participant [2], and the mean of the product was regarded as k. The k value was then multiplied by each COEST value, giving COEST-ADJ values, which were comparable to Modelflow derived CO.
All statistical tests were conducted using SPSS (ver. 19, IBM Chicago, IL, USA). Independent sample t-tests were used to determine any gender differences between variables. Pearson’s r correlation coefficients were used to evaluate the association between Modelflow derived CO and COEST (all results were identical when using COEST-ADJ). Bland-Altman plots were constructed to assess the level of agreement between Modelflow derived CO and COEST-ADJ overall [8].
RESULTS
Table 1 shows descriptive statistics of all participants. Results indicate that all participants were comparable in age, BMI, and BP indices. Males had higher resting SBP and DPB in comparison to female participants. Males also exhibited higher baseline CO though interestingly, this difference was not statistically significant and this pattern was reversed when COEST was considered. Overall, COEST was larger than CO obtained via the Modelflow method, suggesting that this procedure produces an inflated parameter estimate.
Table 1.
Descriptive Statistics of All Participants
| Males | Females | Total | |
|---|---|---|---|
| n | 30 | 37 | 67 |
| Age | 19.87 (2.0) | 20.00 (3.38) | 19.94 (2.84) |
| BMI | 24.90 (4.35) | 24.66 (3.95) | 24.77 (4.11) |
| SPB* | 124.77 (15.63) | 116.15 (13.00) | 120.01 (14.77) |
| DBP* | 69.29 (11.27) | 63.61 (9.59) | 66.15 (10.68) |
| HR | 71.81 (8.89) | 76.20 (10.56) | 74.23 (10.02) |
| PP | 55.49 (9.81) | 52.53 (9.75) | 53.86 (9.82) |
| CO | 6.07 (1.04) | 5.82 (1.25) | 5.93 (1.16) |
| COEST | 20.54 (3.46) | 22.41 (5.18) | 21.57 (4.56) |
| COEST-ADJ | 5.79 (0.98) | 6.32 (1.46) | 6.08 (1.29) |
Table 1 displays total sample (and split by gender) mean values (standard deviation in brackets) of age (in years), body mass index (BMI | kg/m2), systolic blood pressure (SBP | mmHg), diastolic blood pressure (DBP | mmHg), heart rate (HR | bpm), pulse pressure (PP | mmHg), Modelflow derived cardiac output (CO | L/min), estimated cardiac output derived using the Liljestrand and Zander mathematical transformation (COEST), and COEST multiplied by k (COEST-ADJ | L/min).
An asterisk
denotes p < .05 between gender groups.
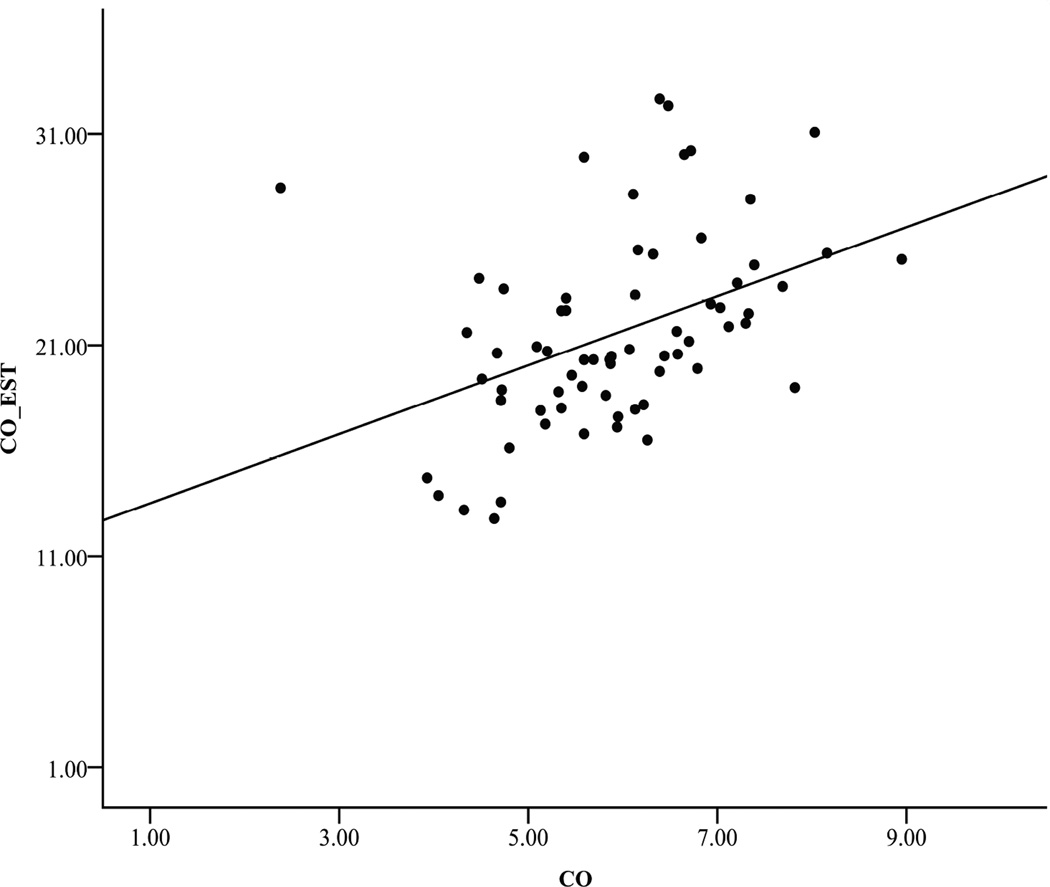
Correlational results showed a significant and moderate correlation between CO and COEST (r = .42, p <.0001). This relationship appeared to be stronger in men (r = .66, p <.001) in comparison to women (r = .36, p <.05). Figure 1 illustrates a scatterplot of CO and COEST for the entire sample.
Figure 1. Scatterplot of CO and COEST.
depicts a scatterplot between baseline Modelflow derived cardiac output (CO) and baseline estimated cardiac output derived using the Liljestrand and Zander mathematical transformation (COEST).
As determined by the calculation of the anomaly index of Modelflow derived CO, one outlier was removed, and as a result, the correlation between CO and COEST significantly increased in both the overall sample (r = .535, p < .001) and women (r = .520, p = .001).
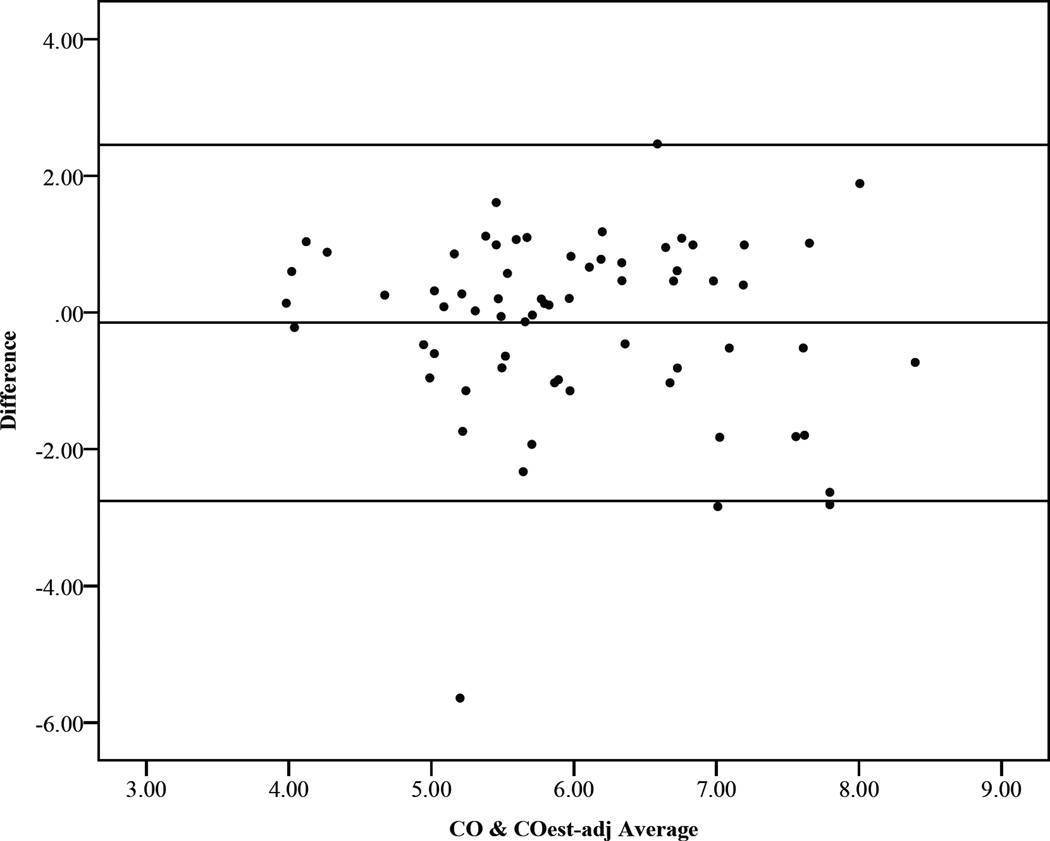
A Bland-Altman plot for the entire sample is shown in Figure 2. The mean difference between CO and COEST-ADJ was −0.15, with a standard deviation (SD) of 1.33. With an upper limit of 2.75 and a lower limit of −2.46, results revealed that 94% of the cases fell within these limits of agreement. The remaining 6% (4 cases) fell outside of the 95% limit of agreement.
Figure 2. Bland-Altman plot of CO and COEST-ADJ.
shows a Bland-Altman plot of CO and COest. 94% of cases fall within the 95% limits of agreement.
DISCUSSION
Invasive and non-invasive techniques that have been proposed to estimate cardiac output are often proprietarily-restricted or computationally complex and thus, this investigation sought to evaluate the utility of the non-invasive and sophisticated, yet simple, Liljestrand and Zander technique in order to estimate CO. Correlational results showed a moderate correlation between CO and COEST suggesting that these two measure are closely related.
In order to show good agreement between COEST and CO, we (and others [2]) proposed that COEST be multiplied by a constant (k), giving COEST-ADJ values that are in better agreement with CO in comparison to COEST. The above Bland-Altman plot supports this idea, showing that CO and COEST-ADJ were in good agreement (94% of data fell within limits of agreement). Overall, these data are in line with others [9], suggest that the Liljestrand and Zander mathematical transformation may be good where other methods are less easy to implement, especially in clinical or ambulatory settings. Future studies should validate this formula against CO derived via thermodilution to further validate the current results.
CONCLUSIONS
We evaluated a simple, yet sophisticated, formula to approximate CO. Our results suggest that, at least in the resting position, the Liljestrand and Zander [2] formula serves as a good estimate of CO. These findings have many clinical implications, as researchers are often interested in deriving CO in a relatively inexpensive and sophisticated, yet simple, manner. These results suggest that at least in some situations the Liljestrand and Zander method may provide an adequate measure of CO when other methods are not available.
Acknowledgments
We would like to thank all of those who participated at The Ohio State University
REFERENCES
- 1.Mathews L, Singh KR. Cardiac output monitoring. Ann. Cardiac Anaesthesia. 2008;11(1):56. doi: 10.4103/0971-9784.38455. [DOI] [PubMed] [Google Scholar]
- 2.Sun JX, et al. Estimating cardiac output from arterial blood pressure waveforms: a critical evaluation using the mimic ii database. Computers in Cardiology. 2005:295–298. [Google Scholar]
- 3.Hill LK, et al. Evaluation of a simple estimation method for the derivation of cardiac output from arterial blood pressure and heart rate. Biomed Sciences Instrumentation. 2011;48:165–170. [PubMed] [Google Scholar]
- 4.Liljestrand G, Zander E. Vergleichen die Bestimmungen des Minutenvolumens des Herzens beim Menschen mittels der Stichoxydulmethode und durch Blutdruckmessung. Ztschr ges exper med. 1928;59:105–122. [Google Scholar]
- 5.Nima F, Hahn J. Estimation of cardiac output and peripheral resistance using square-wave-approximated aortic flow signal. Frontiers in Physiology. 2012;3 doi: 10.3389/fphys.2012.00298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sollers JJ, et al. Comparison of arterial compliance indices derived via beat-to-beat blood pressure waveforms: aging and ethnicity. Biomedical Sciences Instrumentation. 2005;42:518–523. [PubMed] [Google Scholar]
- 7.Jansen JRC, et al. A comparison of cardiac output derived from the arterial pressure wave against thermodilution in cardiac surgery patients. British journal of Anaesthesia. 2001;87(1):212–222. doi: 10.1093/bja/87.2.212. [DOI] [PubMed] [Google Scholar]
- 8.Bland JM, et al. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986:307–310. [PubMed] [Google Scholar]
- 9.Sun JX. The cardiac output from blood pressure algorithms trial. Critical care medicine. 2009;37(1) doi: 10.1097/CCM.0b013e3181930174. [DOI] [PMC free article] [PubMed] [Google Scholar]