Abstract
Objective:
To introduce athletic trainers to the benefits of using a population-based approach to injury and illness prevention and to explore opportunities for partnering with public health professionals on these initiatives.
Background:
Athletic trainers play leading roles in individual injury and illness prevention but are less familiar with policy development, evaluation, and implementation from a population-level standpoint. The Athletic Training and Public Health Summit was convened to understand, explore, and develop the intersection of athletic training and public health.
Conclusions:
To further the integration of athletic training within the public health arena, athletic trainers must expand their professional focus beyond the individual to the population level.
Key Words: population health, injury prevention, policy development, policy evaluation
Since the beginning of the athletic training profession, injury and illness prevention has been a hallmark of the work done by athletic trainers (ATs). Much of this work has been, and continues to be, appropriately focused on the individual. However, many of the most pressing problems facing physically active children and adults—such as sport-related concussion, osteoarthritis (OA), and sudden cardiac death—require population-level approaches to maximize the effectiveness of primary and secondary prevention initiatives. Although ATs are well positioned to take leading roles in injury and illness prevention at the individual level, most are unfamiliar with how to successfully develop policies, conduct policy assessments, and implement large-scale translation to practice initiatives through the application of common public health approaches. To this end, the Athletic Training and Public Health Summit (ATPHS) was convened to introduce ATs to population health and to explore opportunities for partnering with public health professionals.
The genesis of the ATPHS can be traced to a meeting held to discuss the research needs of the profession during the 2013 Athletic Training Educators' Conference in Dallas, Texas. Attending that meeting were leaders of the National Athletic Trainers' Association (NATA) and NATA Research & Education Foundation. Those discussions identified the need for a venue and the beginning of a dialogue to understand, explore, and develop the intersections of athletic training and public health. The inaugural ATPHS was held on the campus of Oregon State University on August 27–29, 2015. The NATA, NATA Research & Education Foundation, and Oregon State University College of Public Health and Human Sciences were founding sponsors, and the Datalys Center for Sports Injury Research and Prevention, Inc, was a supporting sponsor.
The program of the ATPHS was designed to meet the following learning objectives:
Describe the benefits of using a population-based approach to address concerns important to ATs,
Identify specific skill sets and potential partnerships that would be beneficial for maximizing the prevention of injuries and illnesses commonly treated by ATs, and
Identify and develop potential solutions to challenges that arise in the development, translation, adoption, and assessment of preventive policies, guidelines, and practices.
The purpose of this article is to provide a summary and description of 3 symposia delivered at the ATPHS, discuss the areas of emphasis identified during the road-mapping session, and finally, offer direction for the further integration of athletic training with public health.
A Public Health Approach
The Centers for Disease Control and Prevention Foundation1 defines public health as
“the science of protecting and improving the health of families and communities through promotion of healthy lifestyles, research for disease and injury prevention and detection and control of infectious diseases.”
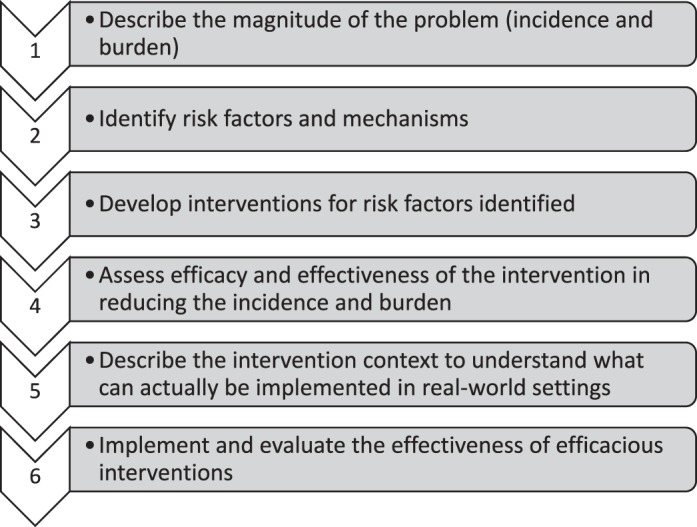
Public health approaches emphasize prevention over treatment, populations over individuals, and engagement at multiple levels. As described by Van Mechelen et al,2 the basis of the public health approach is a critical 4-step process commonly used to address health problems: (1) describe the magnitude of the problem (incidence and burden), (2) identify risk factors and mechanisms, (3) develop interventions for the risk factors identified, and (4) assess the efficacy and effectiveness of the intervention in reducing the incidence and burden of the problem. For example, in athletic training, the approaches taken to address sport-related concussion, anterior cruciate ligament injuries in girls and women, and sudden cardiac death have all followed these steps, although significant work in assessing and monitoring effectiveness continues. Finch3 described the Translating Research Into Injury Prevention Practice (TRIPP) framework that added 2 steps to the foundational model of Van Mechelen et al2: (5) describe the intervention context in order to understand what can actually be implemented in real-world settings and (6) implement and evaluate the effectiveness of efficacious interventions from step 4 using the TRIPP model, which is applicable to multiple aspects of injury prevention (Figure). Primary prevention focuses on interventions before the injury or illness occurs (eg, neuromuscular training programs to prevent knee injuries), whereas secondary prevention focuses on interventions immediately after the injury or illness has happened (eg, early treatment, slowing of disease). Tertiary prevention focuses on improving outcomes for those with long-term injuries or illnesses (eg, knee or ankle OA). Given the role ATs currently play in preventing injury and illness (in both the primary and secondary realms), it is imperative that they understand the influence they can have on public health and identify specific areas of clinical practice on which to focus. Similarly, policy development and assessment (ie, TRIPP steps 5 and 6) are 2 fundamental aspects of public health that are highly applicable to the practice of athletic training. Because ATs are often involved in the development of policies to prevent sport injury and illness, such as rule or equipment changes, a detailed understanding of policy development is important. Athletic trainers are direct participants in and observers of the intervention context, which is a critical part of policy creation (TRIPP step 6). A key aspect of policy development is evaluation after implementation. Not only do new policies need an assessment plan, but current policies and practices often need ongoing assessment (TRIPP step 6). Athletic trainers can play an important role in these processes.
Figure. .
Symposium Overview
The ATPHS was organized into 3 symposia and a road-mapping session. By combining keynote addresses from international experts with presentations by medical and public health professionals (Table), the symposia were designed to highlight topics important to ATs and introduce a population approach to promote preventive practices. The topics and speakers were identified as models for how public health practices have been used in areas of interest directly related to the practice of athletic training. The road-mapping session was an open discussion among the attendees and the speakers that focused on identifying areas where athletic training and public health practices intersect and developing a plan for advancing the discussion of athletic training and public health integration. It is important to note the diversity of work settings represented by the attendees: high school clinicians, university professors, physicians, health department employees, and a recent bachelor's degree graduate.
Table. .
Athletic Training and Public Health Summit Speakers
| Symposium |
Speaker |
Title |
Institution |
| “Sudden Cardiac Death and Development and Implementation of Policies/Guidelines for Injury Prevention” | Jonathan Drezner, MD | Professor, Department of Family Medicine; team physician | University of Washington; Seattle Seahawks |
| Michael Koester, MD, AT Ret | Pediatric and adolescent sports medicine physician | Slocum Center for Sports Medicine, OR | |
| Laurel Kincl, PhD | Assistant professor | Oregon State University College of Public Health and Human Sciences, Corvallis | |
| “Sport-Related Concussion and Program/Policy Evaluation” | Kevin M. Guskiewicz, PhD, ATC, FNATA, FACSM | Kenan Distinguished Professor and senior associate dean for Natural Sciences, College of Arts and Sciences | The University of North Carolina at Chapel Hill |
| Emily Tosoni, MS, ATC, CHES, CLC | Nutrition and physical activity program health specialist | Montana Department of Public Health and Human Services, Helena | |
| Lisa Schmidt, MPH, ATC | Epidemiologist | Montana Department of Public Health and Human Services, Helena | |
| Viktor Bovbjerg, PhD, MPH, NREMT | Associate professor | Oregon State University College of Public Health and Human Sciences, Corvallis | |
| “Osteoarthritis and Translation to Practice” | Kenneth L. Cameron, PhD, MPH, ATC | Director of Orthopaedic Research, John A. Feagin Sports Medicine Fellowship | Keller Army Community Hospital, West Point, NY |
| Jennifer M. Hootman, PhD, ATC, FNATA, FACSM | Epidemiologist | Centers for Disease Control and Prevention, Atlanta, GA | |
| Roger Rennekamp, PhD | Associate dean for outreach and engagement | Oregon State University College of Public Health and Human Sciences, Corvallis |
Sudden Cardiac Death and Development and Implementation of Policies and Guidelines for Injury Prevention
Sudden cardiac arrest is the most common cause of death among high school and collegiate athletes.4 Kimberly Harmon, MD, delivered the keynote address on sudden cardiac arrest and emphasized the need for primary prevention but stressed that a “one-size-fits-all” approach to cardiac screening may not be appropriate for all populations. She highlighted the existing challenges and controversies associated with implementing cardiac screening in settings ranging from the National Football League to high school basketball. Michael Koester, MD, AT Ret, the former chair of the National Federation of State High School Associations' Sports Medicine Advisory Committee and current chair of the Oregon School Activities Association's Sports Medicine Advisory Committee, focused on practical examples of developing and implementing preventive policies. He stressed the need to engage stakeholders from the outset and noted that mandates without stakeholder engagement are generally unsuccessful. Finally, Laurel Kincl, PhD, contributed her experience with child labor laws to address how the political landscape and organizational self-interests can be substantial barriers to policy and guideline implementation.
Sport-Related Concussion and Program and Policy Evaluation
Since the first concussion law went into effect in 2009, all 50 states have adopted legislation addressing concussion safety for young athletes; however, the effect of this legislation remains unknown. The keynote address in this symposium was delivered by Kevin M. Guskiewicz, PhD, ATC, FNATA, FACSM, who emphasized that the effectiveness of concussion policies should not be based on the increased incidence of concussion. Rather, greater reporting of concussion, likely due to improved awareness, is evidence that the concussion laws adopted nationwide are making a difference. However, we need to rigorously evaluate the concussion policies that have been put into place nationwide. Emily Tosoni, MS, ATC, CHES, CLC, and Lisa Schmidt, MPH, ATC, who are employed by the Montana Department of Public Health and Human Services, discussed their work evaluating the level of knowledge of, resources for implementation of, and willingness of communities to comply with Montana's concussion legislation. Most of the schools surveyed had policies in place that included all of the components required by the Montana act as related to the identification of concussed athletes and their referral to health care providers. However, the policy evaluation identified key gaps in that the act did not apply to non–school-sponsored activities, nor did it address the general understaffing of schools by health care professionals. Building on the ideas presented by the previous speakers, Viktor Bovbjerg, PhD, MPH, NREMT, discussed how evaluating process (policy implementation) and structure (infrastructure changes to support policy) is as essential as evaluating health outcomes when determining the effectiveness of policies and guidelines, and he provided specific examples of how to conduct these different types of evaluations.
Osteoarthritis and Translation to Practice
Acute traumatic knee-joint injuries are common in young athletic populations, and these injuries significantly increase the risk for posttraumatic osteoarthritis. Kenneth Cameron, PhD, MPH, ATC, delivered the final keynote address and stressed that the problem is not a lack of guidelines for OA management but deficiencies in the dissemination and implementation of those guidelines. He called for OA management to take an approach similar to that currently used for chronic disease management and for ATs to embrace their role in implementing behavioral interventions that are vital for primary (eg, injury-prevention programs) and secondary (eg, employing weight-management strategies after an injury) prevention of joint disease. He also identified potential strategic partners, including the Athletic Trainers' Osteoarthritis Consortium, the OA Action Alliance, and the Chronic Osteoarthritis Management Initiative, for the prevention and management of OA. Jennifer M. Hootman, PhD, ATC, FNATA, FACSM, echoed these thoughts and provided specific examples of dissemination and implementation approaches used by the Centers for Disease Control and Prevention and the Arthritis Foundation. Roger Rennekamp, PhD, then offered an overview of the Cooperative Extension System as a potential model for public health engagement at the state and national levels.
Road-Mapping Session
The discussion throughout the ATPHS resulted in 4 areas of emphasis: (1) Who needs to be involved in the discussions moving forward? (2) What skills, knowledge, and abilities do ATs need in order to see their work through a public health lens? (3) What educational opportunities and activities will promote the integration of athletic training and public health and further realize the goals of this summit? (4) In which areas are ATs already taking the lead in public health-related initiatives and in what other areas might ATs' expertise and public health-related initiatives overlap? The last session focused on developing a road map of future directions for the group and the profession. The following ideas were generated by attendees during a facilitated discussion led by the ATPHS Chair, Mark Hoffman, PhD, ATC, FNATA:
-
1.
Who needs to be involved in the discussions moving forward?
-
•
The Athletic Training Strategic Alliance, consisting of the Board of Certification, the Commission on Accreditation of Athletic Training Education, the NATA, and the NATA Research & Education Foundation, must be part of the discussion to ensure that the progress made at the summit serves as the foundation for ongoing action and so they can provide future support.
-
•
Athletic training educators play an important role in helping the profession advance in the areas discussed. Attendees considered the potential need for educational competencies related to athletic training and public health.
-
•
The NATA should explore more robust partnerships with the American Public Health Association that extend beyond reciprocal liaisons.
-
•
Those ATs who are interested in public health should consider becoming involved with state public health associations.
-
•
Universities with both accredited schools or colleges of public health and accredited athletic training programs should work with their deans to promote the intersection of these disciplines.
-
•
Athletic trainers should work with insurance companies, coordinated care organizations, and risk managers, for example, to discuss the role of ATs in injury and illness prevention.
-
•
-
2.
What skills, knowledge, and abilities do ATs need to see their work through a public health lens?
-
•
Athletic trainers should continue to educate the public regarding the role of ATs in primary and secondary injury and illness prevention.
-
•
Knowledge of policy development is essential. Policy development can be thought of on a continuum from governing body mandates and laws to best-practice recommendations and guidelines.
-
•
Athletic trainers must have the background knowledge and skills to work with risk managers at their institutions or companies in order to explore the development of policies and procedures specific to athletic training and athlete safety. Working with sponsors (eg, foundations or companies) that have an interest in specific policies is another possibility.
-
•
Considering the large increase in policies related to athlete health and safety, policy evaluation is an important area of study. The focus should be on assessing not only the outcomes of the policy but also the process and the structure of the policy implementation to include unintended consequences of programs and policies.
-
•
Athletic trainers should be knowledgeable about health behavior theory to increase the reach of efficacious and effective injury- and illness-prevention programs. Dr Hootman highlighted this idea in her talk: “An efficient dissemination approach is just as important as the evidence-based intervention.”
-
•
Health disparities are an important area for ATs to be aware of and to take steps to limit.
-
•
-
3.
What educational opportunities and activities will promote the integration of athletic training and public health?
-
•
Much of what ATs currently do could be considered population-level health. Conducting preparticipation physical examinations, planning for emergencies, tracking injuries, and instructing athletes to keep the lid on a cooler to prevent the spread of germs from dipping of cups are all considered population-level health concerns. Considering the role of ATs through a public health lens will require ATs to undergo a paradigm shift and think about populations differently. Although some ATs may pursue formal public health education, a more immediate way to foster this shift is to encourage ATs to present at public health conferences and to engage public health experts at ATs' professional conferences.
-
•
Athletic trainers and public health experts could also be integrated into educational programs. A professional education program that requires athletic training students to obtain clinical education experiences treating patients with musculoskeletal injuries at a public health clinic is an example of this type of integration.
-
•
An athletic training and public health special interest group should be developed to advance the discussion of the intersection of these disciplines.
-
•
Funding opportunities to support collaboration between athletic training and public health researchers, clinicians, and practitioners should be created.
-
•
-
4.
In which areas are ATs already taking the lead in public health-related initiatives and in what other areas might ATs' expertise and public health-related initiatives overlap?
-
•
Osteoarthritis in general and the chronic management of posttraumatic OA specifically,
-
•
Concussion management and return-to-participation guidelines,
-
•
Sudden cardiac death prevention as related to emergency action plans and screening initiatives,
-
•
Heat-illness prevention as related to heat-acclimatization and environmental policies,
-
•
Prevention of overuse injuries (eg, ulnar collateral ligament and shoulder injuries in youth baseball players),
-
•
Disaster-relief efforts, and
-
•
Shifting to models of wellness, optimal performance, and disease and injury prevention rather than the treatment of injury and illness.
-
•
CONCLUSIONS
The ATPHS clearly identified the progress that needs to be made toward increasing ATs' awareness and understanding of the public health practices they engage in on a regular basis (eg, injury surveillance) and the fact that they are public health practitioners. Much of the work done every day and many of the policies and practices followed by ATs are connected to public health. It is critical to expand this discussion to include a wider set of stakeholders; this is an important strategic opportunity for the profession to position itself as a legitimate and valuable player in the public health arena and to increase the effects ATs have on the patients and the populations they serve. Strengthening the relationship with these stakeholders will help to move the ideas from the summit forward. Last, ATs need to equip themselves with the knowledge, skills, and abilities to view their work in the context of public health practices. The profession of athletic training must broaden its focus from the individual's health and well-being to populations ranging from the teams and athletes they work with at their institutions to all physically active individuals.
REFERENCES
- 1. What is public health? Centers for Disease Control and Prevention Web site . http://www.cdcfoundation.org/content/what-public-health. Accessed March 8, 2016. [Google Scholar]
- 2. Van Mechelen W, Hlobil H, Kemper H. Incidence, severity, aetiology and prevention of sports injuries: a review of concepts. Sports Med. 1992; 14 2: 82– 99. [DOI] [PubMed] [Google Scholar]
- 3. Finch C. A new framework for research leading to sports injury prevention. J Sci Med Sport. 2006; 9 1−2: 3– 10. [DOI] [PubMed] [Google Scholar]
- 4. Casa D, Guskiewicz K, Anderson S, et al. National Athletic Trainers' Association position statement: preventing sudden death in sports. J Athl Train. 2012; 47 1: 96– 118. [DOI] [PMC free article] [PubMed] [Google Scholar]


