Abstract
Introduction
Understanding how pharmacy technicians and other pharmacy support workforce cadres assist pharmacists in the healthcare system will facilitate developing health systems with the ability to achieve universal health coverage as it is defined in different country contexts. The aim of this paper is to provide an overview of the present global variety in the technician and other pharmacy support workforce cadres considering; their scope, roles, supervision, education and legal framework.
Material and methods
A structured online survey instrument was administered globally using the Survey Monkey platform, designed to address the following topic areas: roles, responsibilities, supervision, education and legislation. The survey was circulated to International Pharmaceutical Federation (FIP) member organisations and a variety of global list serves where pharmaceutical services are discussed.
Results
193 entries from 67 countries and territories were included in the final analysis revealing a vast global variety with respect to the pharmacy support workforce.
Roles and competency
From no pharmacy technicians or other pharmacy support workforce cadres in Japan, through a variety of cadre interactions with pharmacists, to the autonomous practice of pharmacy support workforce cadres in Malawi.
Responsibilities
From strictly supervised practice with a focus on supply, through autonomous practice for a variety of responsibilities, to independent practice.
Supervision
From complete supervision for all tasks, through geographical varied supervision, to independent practice.
Education
From on the job training, through certificate level vocational courses, to 3–4 year diploma programs.
Legislation, regulation and liability
From well-regulated and registered, through part regulation with weak implementation, to completely non-regulated contexts.
Conclusion
This paper documents wide differences in supervision requirements, education systems and supportive legislation for pharmacy support workforce cadres globally. A more detailed understanding of specific country practice settings is required if the use of pharmacy support workforce cadres is to be optimized.
1. Introduction
1.1. The sustainable development goals
In 2016 the United Nations transitioned from a focus on the Millennium Development Goals (MDGs) to a renewed focus on international equity through the cross-sectional application of 17 Sustainable Development Goals (SDGs).1, 2 Although significant progress has been made to address medicines access, inequality continues in many countries and regions of the world.3 The lack of sufficient human resources to provide pharmaceutical services is a significant factor in many environments, and often pharmacy technicians and other pharmacy support workforce cadres are used extensively to ensure basic services, as pharmacists are unavailable.3, 4 This is in contrast to high-income environments where pharmacy technicians and other pharmacy support workforce cadres are working more closely with pharmacists to allow delivery of a greater range of more complex pharmaceutical services.5
The SDGs adopted in 2015 aim to ‘end poverty, protect the planet, and ensure prosperity for all’ as part of a new sustainable development agenda focusing on equity.2 Each goal has specific targets to be achieved over the next 15 years, with a recognition of the interrelationship between poverty, sustainability and prosperity and a link to health outcomes. Goal 3, increased health and wellbeing, provides the focus for health improvements with the acknowledgment that pharmaceutical service delivery will be essential for progress to be noted in many countries.2 Specifically, SDG Goal 3 includes financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all.
Understanding how pharmacy technicians and other pharmacy support workforce cadres assist pharmacists in the healthcare system will facilitate developing health systems with the ability to achieve this SDG goal.
1.2. Medicines availability, access and people centred health systems
The World health Organization (WHO) published The World Medicines Situation report in 2011 which alarmingly notes that one third of the world's population does not have access to regular life-saving medicines.3 This reality sees large numbers of the world population suffering from death and significant morbidities from preventable or treatable diseases such as pneumonia, malaria, HIV/AIDs, tuberculosis, malnutrition and dehydration from diarrhoea.1 In many high income countries, aging populations, polypharmacy, use of more complex medicines and rising costs of healthcare is placing pressure on health systems.6, 7 The pharmacy workforce has a role to play to deal with these pressures.8 The International Pharmaceutical Federation (FIP), acknowledges that there is a need to both increase medicines access to patients in low-income environments while also ensure the optimal use of the pharmacist in a variety of clinical settings.9, 10
1.3. Global human resources for health
In 2006, the WHO brought to the world's attention the vast shortage of the human resources required for minimum health service delivery.11 At that time an estimated global shortage of 4.3 million health workers was noted, with critical shortages in 57 of the poorest countries in the world. Since that time increased urbanisation, an increased middle class in low- and middle-income countries and an ageing population in many high-income countries has seen increasing demands on health services with a corresponding increase in the number of health workers required to meet this need, including the pharmacy workforce.12, 13 The FIP 2012 Workforce Report and recent workforce trends report also highlights the shortage of pharmacy workforce cadres in many countries.8, 14
In 2016, the WHO Health Assembly accepted the ‘Global Human Resources for Health Strategy’.12 The strategy includes reference to pharmacy workforce requirements and presents recommendations on how countries may meet their human resources for health (HRH) needs. Within this WHO strategy, mid-level cadres play a significant role in meeting HRH needs due to their wider availability, country specific nature, lower cost and shorter ‘production’ times.4, 15 WHO describes mid-level providers as ‘health workers with 2–3 years of post-secondary school healthcare training who undertake tasks usually carried out by doctors, nurses, or other health professionals.16 Technicians and other pharmacy support workforce cadres are a key subset of mid-level cadres.12
1.4. FIP guidelines and standards that engage pharmacy support workforce
FIP has had a focus on pharmacy workforce for many years, with the 2009–2012 ‘Pharmacy Education Taskforce’ documenting the global shortage of pharmacists, technicians and pharmacy support workforce cadres in their 2009 and 2012 Global Pharmacy Workforce Reports.14, 17 Other articles published by experts in this field have further documented the shortage of pharmacists, technicians and other pharmacy support workforce cadres, with an emphasis on exploring local ‘needs-based’ approaches to human resources issues.18, 19 That is, approaches that consider local issues rather than impose global standards. In 2014 FIP Education Initiatives (FIPEd) introduced a new structure that incorporates pharmacy workforce planning issues and provides the platform for ongoing work in this area by FIP. Under this new structure the ‘Global Pharmacy Workforce Intelligence: Trends Report 2015’ was published.8 This report highlighted two workforce issues relevant to technician and pharmacy support workforce considerations:
-
•
The aspiration of many countries towards establishing universal health coverage will require an enhanced health workforce, including pharmacists that can meet the need for pharmaceutical expertise in the population it serves. It is important to monitor trends in the workforce over time.
-
•
There is still much to be done, with some regions and low-income countries still displaying a disproportionately low number of pharmacists or limited overall capacity for delivering pharmacy services.
1.5. Roles and scope
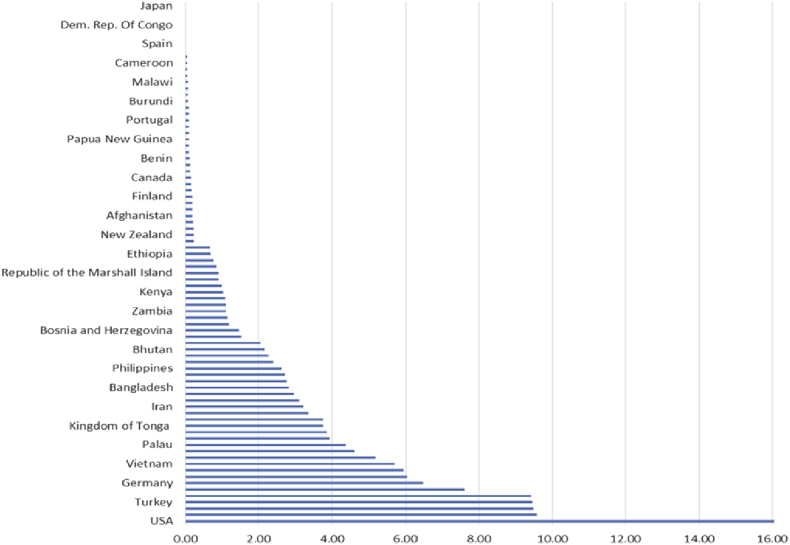
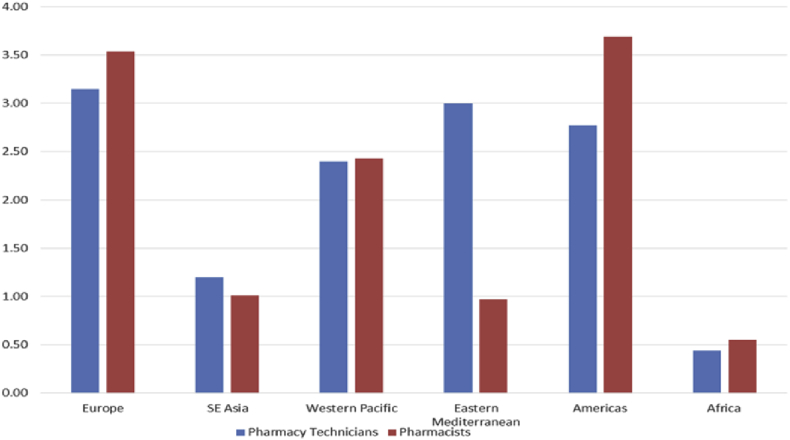
FIP 2012 pharmacy workforce data further documents the large variation of numbers of pharmacy support workforce cadres between countries and WHO regions, with low income regions having less pharmacy workforce compared to higher income regions (Fig. 1). It is also interesting to note the large variation in the ratio of pharmacy technicians to pharmacists in different countries (Fig. 2). More detailed data documenting this variation in terms of education, supervision and legislation requirements, is not available.
Fig. 1.
Density of Pharmacy Technicians per 10,000 population (FIP Pharmacy Workforce data 2012, Christopher John, Royal Pharmaceutical Society).
Fig. 2.
Comparison of pharmacy technician and pharmacist average density per 10,000 population by WHO region (FIP Pharmacy Workforce data 2012, Christopher John, RPS).
Globally the roles and scope of work for technicians and pharmacy support workforce cadres vary greatly according to country and practice areas within that country. Clear scope of practice documentation for a variety of pharmacy technician and other pharmacy support workforce cadres exists in many countries but not every country. The general trend is for middle- and high-income countries to have more detailed documentation and legislation supporting all cadres that contribute to the delivery of pharmaceutical services. It is interesting to note that current international labour definitions for pharmaceutical technicians and assistants reflect the core functions of these cadres but do not reflect how these cadres practice in many countries of the world.20 For example, registered pharmacy technicians in the United Kingdom and Denmark practice dispensing without the supervision of a pharmacist.21
In recent years there have been a number of papers exploring new and expanding roles for the pharmacy support workforce cades. Many of these new roles have been explored with the aim of ‘freeing-up’ the pharmacist, while in countries with few pharmacists these workers have extended roles due to necessity. Table 1 provides a summary of examples of some of these different roles as noted by a variety of publications from different countries.
Table 1.
Studies on different roles for the pharmacy support workforce.
| Year | Practice area | Role or service | Country | Ref. |
|---|---|---|---|---|
| 2009 | Hospital | Facilitation of admission and discharge of elderly patients | Portugal | 22 |
| 2012 | Hospital | Hospital ward stock top up service | Denmark | 23 |
| 2012 | Hospital | Check Tech Check | United States | 21, 24 |
| 2013 | Hospital | Clinical pharmacy technician roles | United States | 25 |
| 2013 | Community | Medication therapy management | United States | 26 |
| 2013 | Hospital Community |
Medication Reconciliation | United States | 27, 28 |
| 2013 | Hospital | Contributing to geriatric treatment in bed-wards | Denmark | 29 |
| 2014 | Community | Vaccine advocacy | United States | 30 |
| 2014 | Medical center | Medication history taking | United States | 31 |
| 2014 | Community | In home medication therapy | United States | 32 |
| 2014 | Hospital | Subacute aged care ward service | Australia | 33 |
| 2014 | Health center | Enhanced cadre of pharmacy assistants for health centers | Malawi | 34, 35 |
| 2014 | Community | Community pharmacy-based adherence programs | Multiple | 36 |
1.6. Objective
The aim of this study was to provide an overview of the present global variety in pharmacy technician and other pharmacy support workforce cadres considering their roles, responsibilities, supervision, education and legal framework.
2. Methods
Previous research investigating global aspects of technician and pharmacy support workforce cadres was conducted in 2012 using a structured online survey approved by the University of Canberra ethics committee and administered through the ‘Survey Monkey’ online platform.37 The structured survey instrument consisted of closed questions with answer options and open ended questions covering the following topic areas: roles, responsibilities, supervision, education and legislation. The 2012 survey tool was initially trialled with respondents from seven countries (Australia, Laos, New Zealand, Papua New Guinea, Rwanda, Uganda, and United States of America) for reliability and validity.37 The survey instrument captures the experiences and perceptions of individuals in their work environments, rather than specific country workforce profiles. In the 2012 survey, further data were collected via oral interviews and more detailed case studies. Triangulation of these three methods produced similar results.37
With the aim of this study to gain an overview of the global variety of aspects of pharmacy support workforce cadres, the 2012 tool was considered an appropriate tool (detailed case studies published in this journal issue provide validated country specific data.) The 2012 tool was reviewed by the FIP ‘Pharmacy Support Workforce Technical Working Group’ with minor edits made to contextualise the survey. Specifically, the order of the sections was rearranged to that in Table 2. Extra questions regarding scope and responsibilities were added and education questions expanded to include continuing professional development. The technical working group determined that such changes would not affect the reliability and validity of the survey. A full copy of the revised survey instrument is available here: https://www.surveymonkey.net/r/?sm=0gCNE_2FF_2F4S7rFHQzcg75EM6qyzqalW4RqVQo3kAoEo8_3D.
Table 2.
Summary of survey areas, purpose and example questions.
| Survey topic area | Purpose | Example questions |
|---|---|---|
|
Orientate the participant to the purpose and scope of the survey | N/A |
|
Capture the range of titles that are attributed to pharmacy support workforce cadres internationally | In the country that YOU work, NOT including pharmacists, nurses and doctors, who are the MAIN CADRES providing pharmaceutical services in your country? |
|
Explore the extent of supervision, by whom and variations with respect to competency type and geography | Does the Pharmacy Support Workforce (PSW) cadres you have identified work independently, without face to face supervision, on a day to day basis? What are the main competences that require supervision for the PSW cadre you have identified? Briefly describe the circumstances (e.g. regulations, geographical, health facility type etc.) where different PSW cadres are allowed to work independently in your country. |
|
Explore the range, satisfaction and quality assurance aspects of education | What is the minimum expected level of education that is required for PSW cadres in your country? Overall, are you satisfied with the PSW education which occurs in your country? Please briefly outline the quality assurance procedures for the PSW education in your country. |
|
Capture the scope and legal requirements for PSW cadres | For each of the cadres you have identified, does a defined 'SCOPE of Practice' exist? For each of the cadres you have identified do they need to be REGISTERED by the government in order to work? |
|
Understand the profile of the participants who took the survey | Standardised questions were used |
The survey was circulated to International Pharmaceutical Federation (FIP) member organisations (country based pharmaceutical societies from around the world), through the FIP Office and a variety of global list-servs where pharmaceutical services are discussed [e.g. E-DRUG (global list serve of individuals interested in a range of medicines access issues), International Association of Public Health Logisticians (IAPHL) (a list serve of individuals that have a direct interest in health logistics and supply chain), FIP CoP (a community practice of individuals interested in pharmaceutical education and practice)]. Additional exposure was provided through professional LinkedIn networks. The survey was conducted between October 2015 and January 2016 with a total of three reminder notices provided through the above listservs.
Consistent with the use of online ‘opt-in’ surveys individual consent was assumed when a respondent chose to participate in the survey. Introductory information regarding the purpose of the survey, anonymity and use of survey data was provided.
3. Results
3.1. Demographics
A total of 193 entries from 67 countries and territories representing each of the WHO regions were included in the final analysis. Of these, 62 (35%) completed the whole survey. These completion results are similar to those experienced by Brown and Bruno in their separate research using similar workforce surveys.38, 39, 40 The data collected represents the individual opinions and experiences of those in their country context. The open nature of the survey did not allow us to verify specific country profiles but the data collectively provides a picture of global variety from the perspective of the pharmacy workforce. Comparison of multiple data points within countries or comparisons across regions was not undertaken.
The full list of countries and number of respondents per country appears in Table 3.
Table 3.
List of countries and number of respondents per country.
| Country | Number of respondents | Country | Number of respondents | Country | Number of respondents |
|---|---|---|---|---|---|
| Afghanistan | 1 | Iceland | 2 | Slovenia | 1 |
| Algeria | 2 | India | 7 | Solomon Islands | 1 |
| Australia | 4 | Iraq | 2 | South Africa | 17 |
| Belgium | 1 | Ireland | 3 | Spain | 6 |
| Botswana | 1 | Japan | 2 | Sri Lanka | 2 |
| Brazil | 4 | Kenya | 1 | Sudan | 2 |
| Cameroon | 1 | Lebanon | 2 | Swaziland | 1 |
| Canada | 3 | Malawi | 4 | Sweden | 1 |
| China | 1 | Malaysia | 3 | Switzerland | 3 |
| China Taiwan | 2 | Mongolia | 1 | Thailand | 2 |
| Croatia | 3 | Morocco | 2 | Tonga | 1 |
| Democratic Republic of the Congo | 6 | Nepal | 4 | Uganda | 3 |
| Denmark | 3 | Netherlands | 2 | Ukraine | 1 |
| Dominican Republic | 1 | New Zealand | 5 | United Arab Emirates | 3 |
| Ecuador | 1 | Nigeria | 10 | United Kingdom | 9 |
| Ethiopia | 3 | Norway | 1 | United Republic of Tanzania | 5 |
| Fiji | 3 | Pakistan | 6 | United States of America | 14 |
| France | 1 | Papua New Guinea | 1 | Vanuatu | 1 |
| Germany | 3 | Philippines | 1 | Viet Nam | 1 |
| Ghana | 5 | Portugal | 1 | Zambia | 2 |
| Greece | 1 | Romania | 1 | Zimbabwe | 2 |
| Grenada | 1 | Senegal | 1 | ||
| Hungary | 1 | Sierra Leone | 1 |
Of those respondents who completed the demographic section (n = 105), the majority of respondents were pharmacists (Table 4) with most respondents having significant experience both in their profession and current role (33% with more than 5yrs experience). Respondents distributed well across the main practice areas of pharmacy, noting that 21 (11%) of participants were from professional associations within the ‘Other’ category, academia (18%), hospital (16%), government ministry or department (14%), and community (12%) (supplementary file 1 participant demographics).
Table 4.
Respondents' profile.
| Senior medical professionals | Pharmacist | Pharmacy assistant/technician | Managerial/leadership role | Administrative service professionals | Other | No response |
|---|---|---|---|---|---|---|
| 3 (2%) | 72 (37%) | 7 (4%) | 13 (7%) | 4 (2%) | 6 (3%) | 88 (45%) |
3.2. Cadre names
The most frequent name given to the predominant pharmacy support workforce cadre in countries was ‘Technician’, 75%, with a multitude of other titles used across countries (Fig. 3).
Fig. 3.
Word cloud documenting the variety of names used globally for pharmacy support workforce cadres emphasising the predominance of the term ‘technician’ and ‘assistant’.20
Where no technicians or pharmacy support workforce cadres were identified participants noted that this was the case because there were sufficient pharmacists available (Japan), or that there was no existing legislation to support other cadres working in this space, or the current legislation did not reflect what was actually happening in the country context.
3.3. Scope
Only 28% (N = 193) of our respondents indicated that a ‘scope of practice document’ existed for the main pharmacy support workforce cadre in that country (10% did not know).
3.4. Supervision
There is a global variety in the supervision requirements of technicians and pharmacy support workforce cadres. With 10% (N = 193) of respondents indicating that these cadres work independently all the time, 58% indicating that they work independently some or most of the time and 17% of respondents indicating that technician and pharmacy support workforce cadres never work independently, that is, they are always supervised. Pharmacists (61%, N = 193) were noted as the main supervising cadre.
Respondents (23%, N = 193) indicated that supervision requirements were different in urban compared to rural environments with 30% of respondents indicating unchanged supervision when considering urban rural distribution. A further 15% of participants reported that supervision requirements were ‘somewhat different’ and 8% very different when comparing urban and rural environments.
The most supervised competency area is ‘patient consultation and diagnosis’, while ‘procurement and stock ordering’ was the least supervised competency area (Table 5). Of those competency areas listed in the survey ‘receiving donations of medicines’ and ‘patient consultation and diagnosis’ were competency areas not practiced (not considered relevant to pharmacy support workforce cadres), by one third of respondents (Table 4).
Table 5.
The main competency areas that require supervision for the main PSW cadre in respondent's country.
| What are the competences that require supervision for the main PSW cadre in your country? (N = 193) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Answer Options | Full supervision | Some supervision | No supervision | Competency area NOT practiced | Not answered | ||||
| Procurement (Stock Ordering) | 40 | 21% | 69 | 36% | 41 | 21% | 11 | 6% | 32 |
| Receiving donations of medicines | 33 | 17% | 42 | 22% | 24 | 12% | 62 | 32% | 32 |
| Distribution of medicines to facilities | 47 | 24% | 68 | 35% | 34 | 18% | 11 | 6% | 33 |
| Packing/repacking of medicines | 44 | 23% | 70 | 36% | 33 | 17% | 13 | 7% | 33 |
| Disposal of medicines | 49 | 25% | 65 | 34% | 32 | 17% | 15 | 8% | 32 |
| Budget and Reimbursement | 46 | 24% | 44 | 23% | 22 | 11% | 43 | 22% | 38 |
| Giving medicines information and advice to patients | 55 | 28% | 57 | 30% | 30 | 16% | 19 | 10% | 32 |
| Health promotion of non-medicine strategies | 34 | 18% | 67 | 35% | 32 | 17% | 29 | 15% | 31 |
| Patient consultation and diagnosis | 66 | 34% | 27 | 14% | 16 | 8% | 50 | 26% | 34 |
| Taking a medication history of patients, including ‘medication reconciliation’ | 53 | 27% | 45 | 23% | 19 | 10% | 44 | 23% | 32 |
| Dispensing medicines to patients | 57 | 30% | 62 | 32% | 29 | 15% | 13 | 7% | 32 |
| Reconstituting of medicines | 60 | 31% | 50 | 26% | 26 | 13% | 23 | 12% | 34 |
| Preparation or compounding of medications | 64 | 33% | 52 | 27% | 25 | 13% | 20 | 10% | 32 |
| Consult with other healthcare professionals | 44 | 23% | 60 | 31% | 26 | 13% | 31 | 16% | 32 |
| Checking prescriptions | 61 | 32% | 49 | 25% | 27 | 14% | 23 | 12% | 33 |
3.5. Education
From a global perspective there is significant variety in pharmacy support workforce education approaches with respondents reporting certificate (one to two years) and diploma (three to four years) as the most common, spanning the vocational and academic education pathways. Table 6 further documents the variation around aspects of education.
Table 6.
Variation around aspects of education.
| What is the minimum expected level of education that is required for the main PSW cadre in your country? | ||||||
|---|---|---|---|---|---|---|
| Type of education? | ||||||
| No education required | Work based education | Certificate level (vocational) | Diploma level | Degree level (academic) | Other | Not Answered |
| 7 (4%) | 9 (5%) | 42 (22%) | 40 (21%) | 14 (7%) | 8 (4%) | 73 |
| Length of education? (choosing the most relevant time frame) | |||||
|---|---|---|---|---|---|
| <1yr | <2ys | <3yrs | <4yrs | >4yrs | Not answered |
| 20 (10%) | 22 (11%) | 43 (22%) | 16 (8%) | 9 (5%) | 83 |
| What type of institution mainly gives this education? | |||||||
|---|---|---|---|---|---|---|---|
| Non Govt. Org. | Govt. | Public technical college (vocational) | Private technical college (vocational) | Public university | Private university | Other | Not answered |
| 8 (4%) | 13 (7%) | 36 (19%) | 18 (9%) | 13 (7%) | 4 (2%) | 19 (10%) | 82 |
| Who has the main responsibility for paying for the education? | |||||
|---|---|---|---|---|---|
| Student | Govt. | Non govt. org. | Employer | Other | Not answered |
| 45 (23%) | 27 (14%) | 2 (1%) | 20 (10%) | 6 (3%) | 93 |
Public and private institutions both play a significant role in providing education with payment for this education nearly equally distributed between students and other sources (government, employer, donation).
Satisfaction regarding current education approaches was varied with only 32% of respondents noting some degree of satisfaction with the education provided, 10% of respondents were neutral on the issue. When asked ‘how could education for pharmacy support workforce cadres be improved’ the top four responses from 123 respondents were:
-
•
There should be sufficient financial and academic resources available (#16)
-
•
There needs to be a ‘Needs-based’ review of education approaches (#15)
-
•
Education should be more practice based (#11)
-
•
Education approaches need improved accreditation and quality assurance processes (#13)
Quality assurance is the system put in place at a country and or institutional level to ensure that the curriculum content and delivery meets minimum and expected standards.41 When asked ‘how could quality assurance (QA) of education for pharmacy support workforce cadres be improved’ respondents noted the following answers (top 4):
-
•
Improve the supervision around implementation and accountability regarding QA processes (#17)
-
•
QA processes for PSW Cadres should be introduced or strengthened (#15)
-
•
Nothing to do as the process is currently working well (#10)
-
•
Improve transparency and feedback during the quality control (QC) process for education (#8)
3.6. Legislation, regulation and liability
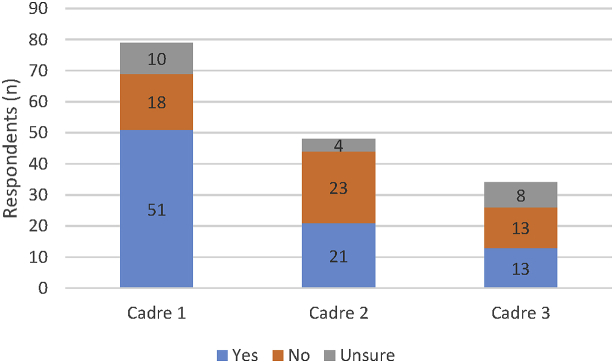
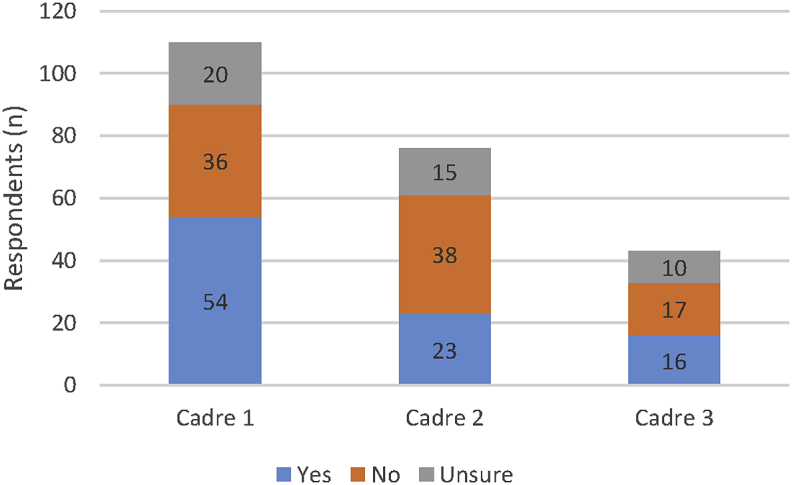
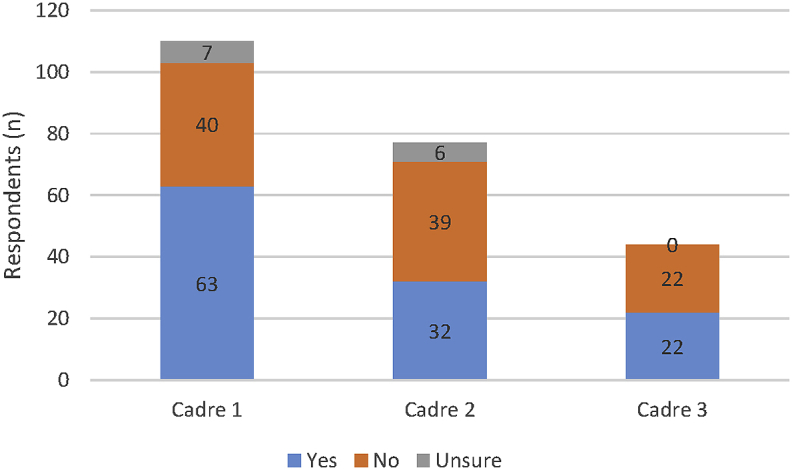
Participants were asked to comment on legislation & regulations (Fig. 4), scope of practice (Fig. 5), and registration (Fig. 6), for up to three PSW cadres present in their country context.
Fig. 4.
Legislation (i.e. national, state or provincial laws) and regulation (i.e. rules) to frame the practice of each of the national PSW cadres. (N.B. Cadre 1 refers to the ‘main’ PSW cadre as identified by the respondent, with cadre 2 and cadre 3 the next most common PSW cadres.
Fig. 5.
Existence of a defined ‘Scope of Practice’ for each of the national PSW cadres (N.B. Cadre 1 refers to the ‘main’ PSW cadre as identified by the respondent, with cadre 2 and cadre 3 the next most common PSW cadres.
Fig. 6.
Need of the national PSW cadres to be registered by government in order to work (N.B. Cadre 1 refers to the ‘main’ PSW cadre as identified by the respondent, with cadre 2 and cadre 3 the next most common PSW cadres.
The data again points to significant global variety; from robustly regulated and registered, through part regulation with weak implementation to completely non-regulated contexts. It is interesting to note that cadres apart from those listed as the main pharmacy support workforce cadre are less likely to be regulated by legislation and have reduced requirements for registration. Scope of practice definitions were also reported as being absent by a large number of respondents.
When asked ‘how could legislation and regulatory requirements’ for PSW cadres be improved’ respondents noted the following (top 3):
-
•
Call for registration or re-registration requirements for PSW cadres (#26)
-
•
Review and updating of legislation and regulations (#10)
-
•
Enforcement of legislation (#5)
4. Discussion
The results of this survey document the significant global variety of pharmacy technician and pharmacy support workforce cadres globally, in regard to role, scope, supervision, education and regulation. Four different country specific workforce models emerge from the data:
-
•
Countries where there are no pharmacy support workforce cadres, only pharmacists, e.g., Japan
-
•
Countries where pharmacy support workforce cadres are supervised by the pharmacist by direct or delegated methods, e.g., Australia and South Africa
-
•
Countries where certain pharmacy support workforce cadres are regulated. They have accountability to undertake independent practice in a team with pharmacists. (e.g., Canada and Denmark)
-
•
Countries that have weak or outdated legislative structures but where, out of necessity, pharmacy support workforce cadres work by themselves. (i.e., current legislation may not reflect actual practice.
4.1. Supervision
The supervision of technicians and other pharmacy support cadres may vary in a country depending on geographical location and the availability of other pharmacists or medical cadres. In general, high-income countries (World Bank groupings), with well-developed health systems have strong regulatory systems and sufficient numbers of pharmacists to deliver pharmaceutical services with limited need for non-supervised activity by other pharmacy cadres. In remote locations ‘telepharmacy’ or other remote pharmacist supervised mechanism may be used, where technology, funding and legislation allows (e.g., Kansas (U.S. State)).42 There are also a number of countries for example; United Kingdom and Denmark where pharmacy support cadres practice a variety of activities unsupervised in a regulated environment (e.g., final checking of prescriptions after dispensing).
A variety of pharmacy professional associations (e.g., Australia and United Kingdom), have published guidelines to support quality supervision of pharmacy technicians and other pharmacy support workforce cadres.43, 44
In low-to middle-income countries with less well developed health systems, less funding and a lower number of pharmacists and other medical staff, pharmacy technicians and other pharmacy support workforce cadres take on a greater role in the delivery of pharmaceutical services without supervision. Pharmacists and other medical staff are less likely to be found in rural and remote environments. It is in these environments that other pharmacy cadres often work unsupervised to ensure the delivery of services, even if they are required to do so in urban environments (e.g., South Africa). This may be the case even if there is no legislation or special government policies to support the practice (e.g., Vanuatu and Papua New Guinea).45, 46 These arrangements are contextually specific within countries and regions of countries depending on the local health needs and availability of staff.
Reports in the literature also discuss a variety of supervision situations. The issue of ‘situational competence’ was documented by Brown in his study of the Vanuatu pharmaceutical system, where across the country he noted that the supervisory circumstances varied according to the availability of staff and the competence they were expected to demonstrate.38, 45 In the extreme sense, if the driver of the delivery van was the only person in the pharmacy then they would be responsible for dispensing medication directly to patients without further supervision. A similar situation was noted in Papua New Guinea.46 The overriding principle was that pharmaceutical service delivery to patients and clinics must go on irrespective of the cadres that were present in the pharmacy section. Results from this current study suggest that this is a more global phenomena, especially in low- and middle-income country contexts. Indeed, ‘situational competence’ can be expected in any country experiencing a shortage of pharmaceutical workforce cadres.13, 14
4.2. Education
FIP encourages a ‘needs-based’ approach to pharmaceutical education where the services required to be delivered in a context are locally determined, the competencies required for specific cadres who deliver these services are agreed and education approaches are developed to meet local development needs for these competencies.19, 47 Further, FIP suggests guarding against seeking globally standardised curriculum approaches, noting that any country education efforts for the pharmaceutical workforce must be relevant to local service delivery.19, 48 Efforts taken to apply this approach to the pharmacy support workforce cadres of small island states of the Pacific Islands is one example where excellent engagement and local acceptability can be demonstrated.49
For any extended role for pharmacy technicians and pharmacy support workforce cadres to be effective the education requirements must change to meet this new need. The USA Report of the ‘2013–2014 Professional Affairs Standing Committee: advancing the pharmacy profession together through pharmacy technician and pharmacy education partnerships’ notes this in detail and suggests that education institutions should consider forming effective collaborations to ensure appropriate education, training, and certification of pharmacy technicians.50 This USA report was tabled, noting a call for improved accountability regarding pharmacy technician education in 2011.51
Other countries are also pursuing this aim, including South Africa who has recently reviewed the roles of pharmacy support workforce cadres and related education requirements.52, 53, 54 An overview of the approach taken to educate pharmacy technicians cadres in the United States was recently published, where a state based system is in force.55 The paper notes that rigorous debate and discussion is needed regarding the future of pharmacy technician roles and the training required fitting those roles. The United Kingdom takes a wider view when it comes to the education of pharmacy technicians and has published a robust review of education and training with a view to ensuring it was aligned with the changing scope of practice in that context.56, 57 Intense discussion regarding the appropriateness of pharmacy support workforce training in Germany formed part of the ‘Future congress’ (a national pharmacy congress held in Germany in 2015), and reflects a robust review of roles and associated supportive education structures.58
4.3. Legislation
In 2010, the Global Health Workforce Alliance (GHWA) released a report summarising the importance of mid-level cadres in meeting healthcare needs. This paper suggests that all who practice health related competencies, including pharmacy technicians and pharmacy support workforce cadres, should work under and be held accountable by appropriate legislation.16 Registration of healthcare workers further aids in ensuring accountability and patient protection in the healthcare sector, but as our data shows, registration of pharmacy technicians and other pharmacy support workforce cadres is not routine across countries, with even OECD countries (Organization for Economic Cooperation and Development) such as Australia and Spain, not requiring the registration of these cadres.
4.4. Future research
The data presented in this paper presents an introductory overview regarding the variety of roles, responsibilities, supervision, education and legislation that governs pharmacy technicians and other pharmacy support workforce cadres around the world. Research into specific country jurisdictions and comparisons between regions may provide insights into optimal use of pharmacy support workforce cadres and improve patient care.
4.5. Limitations
Using a web-based survey limited the data collected to those who had access to a computer and were members of one of the organisations or listservs through which the survey was circulated. Denominator values are not publicly available for the associations and listservs used and so percentage response statistics cannot be calculated. A total of 193 responses would be considered a small number compared to the anticipated global numbers within the pharmaceutical workforce numbers but the data presented provides some insight into the variety of pharmacy support workforce cadres globally, which was the aim of this survey.
5. Conclusion
The data presented through this research documents a variety of roles and responsibilities for pharmacy technicians and other pharmacy support workforce cadres globally, with wide differences in supervision requirements, education systems and supportive legislation noted. A more detailed understanding of specific country practice settings is required if the use of pharmacy support workforce cadres is to be optimized.
Acknowledgment
The authors would like to acknowledge the contribution of the pharmacy support workforce technical working group co-chaired by Ashok Soni (Royal Pharmaceutical Society, Great Britain) and Susan James (Education Development Team, Pharmacy Support Workforce, Canada), with the input and support of the following working group members (in alphabetical order): Jaime Acosta – Community Pharmacy Section (Spain), Hazel Bradley – Hospital Pharmacy Section (South Africa), Andrew Brown – FIP Education Initiative (Australia), Christina Durinck – Farmakonomforeningen (Denmark), Sylvain Grenier – Military and Emergency Pharmacy Section (Canada), Christopher John – Royal Pharmaceutical Society (Great Britain), Tamara Koehler - FIP Intern (Netherlands), Zuzana Kusynová - FIP Policy Advisor and Project Manager (Netherlands), Rob Moss – Hospital Pharmacy Section (Netherlands).
Footnotes
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.sapharm.2016.12.004.
Contributor Information
Tamara Koehler, Email: t.c.koehler@saxion.nl.
Andrew Brown, Email: anbrown.hss@gmail.com.
Appendix A. Supplementary data
The following are the supplementary data related to this article:
References
- 1.United Nations . 2015. The Millennium Development Goals Report.http://www.un.org/millenniumgoals/2015_MDG_Report/pdf/MDG%202015%20rev%20(July%201).pdf New York, 2015. Accessed 10th Oct 2016. [Google Scholar]
- 2.United Nations . 2016. Sustainable Development Goals. New York.http://www.un.org/sustainabledevelopment/sustainable-development-goals/ Accessed 10th Oct 2016. [Google Scholar]
- 3.World Health Organisation (WHO) Availability and Affordability; Geneva: 2011. The World Medicines Situation 2011 Medicines Prices.http://www.who.int/medicines/areas/policy/world_medicines_situation/WMS_ch6_wPricing_v6.pdf Accessed 10th Oct 2016. [Google Scholar]
- 4.Brown A., Cometto G., Cumbi A. Mid-level health providers: a promising resource. Rev Peru Med Exp Salud Publ. 2011;28:308–315. [PubMed] [Google Scholar]
- 5.Zellmer W. The future of health-system pharmacy: opportunities and challenges in practice model change. Ann Pharmacother. 2012;46:S41–S45. doi: 10.1345/aph.1Q805. [DOI] [PubMed] [Google Scholar]
- 6.Armstrong B., G J., Leeder S., Rubin G., Russell L. Challenges in health and health care for Australia. Med J Aust. 2007;187:485–489. doi: 10.5694/j.1326-5377.2007.tb01383.x. [DOI] [PubMed] [Google Scholar]
- 7.Reich M., S K. The future of Japan's health system — sustaining good health with equity at low cost. N Engl J Med. 2015;373:1793–1797. doi: 10.1056/NEJMp1410676. [DOI] [PubMed] [Google Scholar]
- 8.International Pharmaceutical Federation (FIP) 2015. Global Pharmacy Workforce. Intelligence Trends Report.https://www.fip.org/files/FIPEd_Trends_report_2015_web.pdf Hague, 2015. Accessed 10h Oct 2016. [Google Scholar]
- 9.International Pharmaceutical Federation (FIP) 2005. FIP Statement of Policy on Improving Access to Medicines in Developing Countries.https://www.fip.org/www/uploads/database_file.php?id=156&table_id= Hague, 2005. Accessed 10th October 2016. [Google Scholar]
- 10.International Pharmaceutical Federation (FIP) 2011. Joint FIP/WHO Guidelines on Good Pharmacy Practice: Standards for Quality of Pharmacy Services.https://www.fip.org/www/uploads/database_file.php?id=331&table_id= Hague, 2011. Assessed 10th Ocober 2016. [Google Scholar]
- 11.World Health Organisation (WHO) 2006. The World Health Report 2006-Working Together for Health. Geneva.http://www.who.int/whr/2006/whr06_en.pdf?ua=1 Accessed 10th Oct 2016. [Google Scholar]
- 12.World Health Organisation (WHO) WHO; Geneva: 2016. Global Strategy on Human Resources for Health: Workforce 2030.http://apps.who.int/iris/bitstream/10665/250368/1/9789241511131-eng.pdf (Accessed) [Google Scholar]
- 13.World Health Organisation (WHO) WHO; Geneva, Switzerland: 2013. A Universal Truth: No Health without a Workforce Third Global Forum on Human Resources for Health Report. [Google Scholar]
- 14.International Pharmaceutical Federation (FIP) 2012. FIP Global Pharmacy Workforce Report. Hague.http://fip.org/files/members/library/FIP_workforce_Report_2012.pdf 2012. Accessed 10th Oct 2016. [Google Scholar]
- 15.Fulton B.D., Scheffler R.M., Sparkes S.P., Auh E.Y., Vujicic M., Soucat A. Health workforce skill mix and task shifting in low income countries: a review of recent evidence. Hum Resour Health. 2011;9 doi: 10.1186/1478-4491-9-1. 1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Global Health Workforce Allia (GHWA) and WHO . 2010. Mid-level Health Providers - a Promising Resource to Achieve the Health Millenium Development Goals.http://www.who.int/workforcealliance/knowledge/resources/Final_MLP_web_2.pdf?ua=1 Final Report. Geneva. Accessed 10th Oct 2016. [Google Scholar]
- 17.International Pharmaceutical Federation (FIP) 2009. FIP Global Pharmacy Workforce Report.http://fip.org/files/fip/publications/2009_FIP_Global_Pharmacy_Workforce_Report.pdf Hauge, 2009. Accessed 10th Oct 2016. [Google Scholar]
- 18.Hawthorne N., Anderson C. The global pharmacy workforce: a systematic review of the literature. Hum Resour Health. 2009;7 doi: 10.1186/1478-4491-7-48. 48–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson C., Bates I., Futter B., Gal D., Rouse M. Global perspectives of pharmacy education and practice. World Med Health Policy. 2010;2:5–18. [Google Scholar]
- 20.International Labour Organisation (ILO) 2009. International Standard Classification of Occupations Draft ISCO 08 Group Definitions in Health.http://www.ilo.org/wcmsp5/groups/public/–-dgreports/–-dcomm/–-publ/documents/publication/wcms_172572.pdf Accessed 10th Oc 2016. [Google Scholar]
- 21.Gabay M. Tech-check-tech: an overview. Hosp Pharm. 2012;47:444–445. [Google Scholar]
- 22.Scott J., Lumsden C., Taylor J., Todd G. Developing the role of a ward based pharmacy technician in facilitation of admission and discharge of elderly patients. Pharm World Sci. 2009;31 99–99. [Google Scholar]
- 23.Mud A. Pharmacist activities in the pharmacy technician lead ward top up service. Eur J Hosp Pharm Sci Pract. 2012;19:108. [Google Scholar]
- 24.Adams AJ, Martin SJ, Stolpe SF, “Tech-check-tech”: a review of the evidence on its safety and benefits, Am J Health Syst Pharm, Vol. 68: 1824-1833. [DOI] [PubMed]
- 25.Cho J., Chen S. Development and evaluation of clinical pharmacy technician roles in a safety net organization. Pharmacotherapy. 2013;33:e263. [Google Scholar]
- 26.Fuller K., Pope N., Lawson K., Weems J., Montemayor D. Addressing the barriers to medication therapy management: training community pharmacy technicians for roles in medication therapy management. J Am Pharm Assoc. 2013;53:e57–e58. [Google Scholar]
- 27.Siemianowski L.A., S S., George J.M. Impact of pharmacy technician-centered medication reconciliation on optimization of antiretroviral therapy and opportunistic infection prophylaxis in hospitalized patients with HIV/AIDS. J Pharm Pract. 2013;26:428–433. doi: 10.1177/0897190012468451. [DOI] [PubMed] [Google Scholar]
- 28.Smith S., M M. Pharmacy-based medication reconciliation program utilizing pharmacists and technicians: a process improvement initiative. Hosp Pharm. 2013;48:112–119. doi: 10.1310/hpj4802-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grønkjær L.S., R J. Pharmacy technicians can contribute to an improvement in the drug treatment in geriatric bed-wards. Eur Geriatr Med. 2013:4. [Google Scholar]
- 30.Humphries C., Gatton O., Cates L., Ferreri S., Marciniak M. Addressing barriers to pneumococcal vaccination: training pharmacy technicians for roles in vaccine advocacy. J Am Pharm Assoc. 2014;54:e114. [Google Scholar]
- 31.Kobayashi K., Le H. Determining the impact of a new medication-history pharmacy technician program. Pharmacotherapy. 2014;34:e243. [Google Scholar]
- 32.O'Connor S., Akers J. Impact of a pharmacy technician on cost of providing in-home medication therapy management services. J Am Pharm Assoc. 2014;54:e208. [Google Scholar]
- 33.Elliott R.A., Perera D., Mouchaileh N. Impact of an expanded ward pharmacy technician role on service-delivery and workforce outcomes in a subacute aged care service. J Pharm Pract Res. 2014;44:95–104. [Google Scholar]
- 34.Ziba M., Babigumira J., Crawford J. Introducing an enhanced cadre of pharmacy assistants to improve dispensing, management, and availability of medicines at the health centre level in Malawi. J Pharm Policy Pract. 2014;7:1–2. [Google Scholar]
- 35.Lubinga S.J., Jenny A.M., Larsen-Cooper E. Impact of pharmacy worker training and deployment on access to essential medicines and health outcomes in Malawi: protocol for a cluster quasi-experimental evaluation. Implement Sci. 2014;9:156. doi: 10.1186/s13012-014-0156-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kadia NK, Schroeder MN, Community Pharmacy-Based Adherence Programs and the Role of Pharmacy Technicians: A Review, J Pharm Technol, 31:51. [DOI] [PMC free article] [PubMed]
- 37.Doherty K. Faculty of Health, University of Canberra; Canberra: 2014. A Review of the Current Global Pharmacy Support Workforce : How Scarcity and Need Drive the Development of a New Competent Workforce. [Google Scholar]
- 38.Brown A.N. School of Health, University of Canberra; Canberra, Australia: 2013. New Tools for Culturally Appropriate Training, to Develop Competency in Pacific Island Countries in Pharmaceutical Healthcare Service Delivery. [Google Scholar]
- 39.Bruno A., Bates I., Brock T., Anderson C. Towards a global competency framework. Am J Pharm Educ. 2010;74:56. doi: 10.5688/aj740356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bruno A. The School of Pharmacy, University of London; London: 2011. The Feasibility, Development and Validation of a Global Competency Framework for Pharmacy Education. [Google Scholar]
- 41.International Pharmaceutical Federation (FIP) 2009. FIP Statement of Policy Quality Assurance of Pharmacy Education. Hauge.https://www.fip.org/www/uploads/database_file.php?id=302&table_id= Accessed 10h Oct 2016. [Google Scholar]
- 42.Gebhart F. Kansas launches remote supervision for hospital pharmacy techs. Drug Top. 2012:156. [Google Scholar]
- 43.Acres S. APTUK's view on supervision [1] Pharm J. 2011;287:491. [Google Scholar]
- 44.Taylor G., Leversha A., Archer C. Staffing levels and structure for the provision of clinical pharmacy services. J Pharm Pract Res. 2013;43:32–35. [Google Scholar]
- 45.Brown A., Gilbert B. The Vanuatu medical supply system - documenting opportunities and challenges to meet the millennium development goals. South Med Rev. 2012;5:14–21. [PMC free article] [PubMed] [Google Scholar]
- 46.Brown A., Gilbert B. The Papua New Guinea medical supply system - documenting opportunities and challenges to meet the millennium development goals. J Pharm Policy Pract. 2014;7:5. doi: 10.1186/2052-3211-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Claire A., Bates I., Brock T. Needs-based education in the context of globalization. Am J Pharm Educ. 2012;76 doi: 10.5688/ajpe76456. Article 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brock T., Brown A., Rennie T., Rouse M. Global pharmacy education: are we there yet? Int Pharm J. 2012;28:4–11. [Google Scholar]
- 49.Brown A. Sustaining Pharmacy Education, where pharmacists are few. Int Pharm J. 2011;27:29–35. [Google Scholar]
- 50.Mobley-Smith M.A., Boyle C.J., Keresztes J.M., Liles J., Garrelts MacLean L. Report of the 2013-2014 professional Affairs standing committee: advancing the pharmacy profession together through pharmacy technician and pharmacy education partnership. Am J Pharm Educ. 2014;78 doi: 10.5688/ajpe7810S22. Article S22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Manasse H., Menighan T.E. Pharmacy technician education, training, and certification: call for a single national standard and public accountability. J Am Pharm Assoc. 2011;51:326–327. doi: 10.1331/JAPhA.2011.11525. [DOI] [PubMed] [Google Scholar]
- 52.Gilbert L. ‘Re-Engineering the workforce to meet service needs’: exploring ‘Task-Shifting’ in South Africa in the context of Hiv/aids and antiretroviral therapy. S Afr Rev Sociol. 2013;44:54–75. [Google Scholar]
- 53.Boschmans S.A., Fogarty T.L., Schafermeyer K.W., Kevin Mallinson R. Practice analysis for mid-level pharmacy workers in South Africa. Pharm Educ. 2015;15:31–38. [Google Scholar]
- 54.Fogarty T., Boschmans S. An improved pharmacy midlevel worker qualification in South Africa: possibility of coteaching pharmacists and pharmacy technicians. Pharm Educ. 2013;13:107–108. [Google Scholar]
- 55.Draime J., Anderson D., Anderson T. Description of pharmacy technician training programs in the United States. J Am Pharm Assoc. 2015;55:251. doi: 10.1016/j.japh.2015.11.014. [DOI] [PubMed] [Google Scholar]
- 56.Rosado H., John C., Puaar D., Bates I. 2015. An Analysis of the Initial Education and Training Standards for Pharmacy Technicians and Views on Their Fitness for Purpose. A report to the General Pharmaceutical Council. [Google Scholar]
- 57.Schafheutle E., Jee S., Willis S. Fitness for purpose of pharmacy technician education and training in Great Britain. Int J Pharm Pract. 2015;23:20–21. doi: 10.1016/j.sapharm.2015.12.011. [DOI] [PubMed] [Google Scholar]
- 58.Rücker Daniel D.D. Future congress: controversy about PTA training. Pharm Ztg Ver Apoth Ztg. 2015:160. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.