Abstract
OBJECTIVE
To determine whether a link exists between serious hypoglycemia and progression of atherosclerosis in a substudy of the Veterans Affairs Diabetes Trial (VADT) and to examine whether glycemic control during the VADT modified the association between serious hypoglycemia and coronary artery calcium (CAC) progression.
RESEARCH DESIGN AND METHODS
Serious hypoglycemia was defined as severe episodes with loss of consciousness or requiring assistance or documented glucose <50 mg/dL. Progression of CAC was determined in 197 participants with baseline and follow-up computed tomography scans.
RESULTS
During an average follow-up of 4.5 years between scans, 97 participants reported severe hypoglycemia (n = 23) or glucose <50 mg/dL (n = 74). Serious hypoglycemia occurred more frequently in the intensive therapy group than in the standard treatment group (74% vs. 21%, P < 0.01). Serious hypoglycemia was not associated with progression of CAC in the entire cohort, but the interaction between serious hypoglycemia and treatment was significant (P < 0.01). Participants with serious hypoglycemia in the standard therapy group, but not in the intensive therapy group, had ∼50% greater progression of CAC than those without serious hypoglycemia (median 11.15 vs. 5.4 mm3, P = 0.02). Adjustment for all baseline differences, including CAC, or time-varying risk factors during the trial, did not change the results. Examining the effect of serious hypoglycemia by on-trial HbA1c levels (cutoff 7.5%) yielded similar results. In addition, a dose-response relationship was found between serious hypoglycemia and CAC progression in the standard therapy group only.
CONCLUSIONS
Despite a higher frequency of serious hypoglycemia in the intensive therapy group, serious hypoglycemia was associated with progression of CAC in only the standard therapy group.
Introduction
Increasing evidence from longitudinal population-based cohort studies suggests that hypoglycemia is associated with an increased risk of adverse cardiovascular events in patients with type 1 and type 2 diabetes (1–3). Similarly, in randomized controlled trials of intensive versus standard glycemic control for macro- and microvascular complications of diabetes, severe hypoglycemia is associated with a significant risk of cardiovascular events (4–6). Although the risk of hypoglycemia is two- to threefold higher in intensive than in standard glycemic control (4–7), the risk of cardiovascular events appears lower with intensive glycemic control (8–10), raising the possibility that cardiovascular consequences of hypoglycemia with intensive therapy may not be as harmful as they are with standard therapy. Consistent with this notion, annual mortality rates appear higher among patients reporting severe hypoglycemia while receiving standard therapy than among those receiving intensive therapy (4,5).
In both observational studies and randomized controlled trials, cardiovascular events occurred months to years after the documented hypoglycemic event (1–6). The acute effects of severe hypoglycemia (defined as hypoglycemic events requiring assistance), including stimulation of counterregulatory responses and sympathoadrenal activation, abnormal cardiac repolarization, and increased cardiac workload (11,12), are well recognized. However, the long-term effects of hypoglycemia on cardiovascular events are not well understood. In addition to these classic counterregulatory and sympathoadrenal responses, hypoglycemic events have been shown to trigger inflammation (13), induce abnormalities in platelet function and activation of the fibrinolytic system, and result in endothelial dysfunction (12,14), all plausible pathophysiologic mechanisms that may lead to the progression of atherosclerosis. Atherosclerosis is extensive and accelerated in patients with long-standing type 2 diabetes and is a major cause of higher incidence of cardiovascular events in this group (15). However, the association between hypoglycemia and progression of atherosclerosis in type 2 diabetes is not known. In addition, whether the level of glycemic control has an impact on the association between hypoglycemia and progression of atherosclerosis is not clear.
In this substudy of the Veterans Affairs Diabetes Trial (VADT), we determined the association between hypoglycemia and progression of atherosclerosis as assessed by computed tomographic measurement of coronary artery calcification (CAC) over nearly 5 years of follow-up. In addition, we determined whether intensive glycemic control during the VADT modified the association between hypoglycemia and CAC progression.
Research Design and Methods
We analyzed data from the Risk Factors, Atherosclerosis, and Clinical Events in Diabetes (RACED) study (15), a substudy of the VADT (6). The VADT and RACED designs, exclusion/inclusion criteria, and study measures, including laboratory methods and activities, have been described in detail previously (6,16,17). In brief, the primary objective of the VADT during the median follow-up of 5.6 years was to assess the effect of intensive glycemic treatment on cardiovascular events in patients with poorly controlled type 2 diabetes. A median absolute HbA1c separation of 1.5 percentage points (∼16 mmol/mol) between the intensive and standard treatment arms was achieved by ∼6 months, and was maintained throughout the study (6). As part of RACED, 197 participants completed electron beam or multidetector computed tomographic cardiac scanning of CAC at the baseline examination and after 4.6 ± 0.6 years of follow-up (17). Readers blinded to the treatment assignment scored the baseline and follow-up scans in the central reading center while following standardized protocols, as previously described (15,17,18). Protocol and consent forms were approved by the institutional review board at each participating site. All participants provided written informed consent. An independent data and safety monitoring committee whose members were aware of study group assignments monitored safety and efficacy.
Definition of CAC Progression
Volumetric scores were used to calculate the progression of CAC as the difference between the square root transformation of follow-up and baseline scores, as previously described (17).
Definition of Serious Hypoglycemia and Glycemic Variability Indices
Adverse events, including hypoglycemia, were monitored and recorded at each visit. During VADT visits, participants were asked whether they had signs and symptoms of hypoglycemia or blood glucose levels <70 mg/dL (∼3.9 mmol/L) since the last visit. If the answer was yes, they were asked about severe hypoglycemia (episodes with loss of consciousness or episodes requiring medical or other assistance) and episodes with documented blood glucose levels <50 mg/dL (G<50). A plasma glucose level of ∼50 mg/dL (∼2.8 mmol/L) is sufficiently low to induce the full cascade of counterregulatory hormones and cause overt functional brain dysfunction that can progress from measurable cognitive impairment to aberrant behavior, seizure, and coma (19–22). With severe hypoglycemia, plasma glucose levels may or may not be available. However, neurologic recovery attributable to the restoration of plasma glucose levels to normal is considered sufficient evidence that the event was induced by a low plasma glucose concentration, which is usually <50 mg/dL (∼2.8 mmol/L) (23) and accompanied by counterregulatory hormone responses. Thus, for the purpose of this analysis, we included both severe hypoglycemic episodes and G<50 in our definition of serious hypoglycemia.
In addition to the many standard risk factors collected during the VADT, we also calculated visit-to-visit glycemic variability of centrally measured HbA1c and locally measured fasting plasma glucose. The SD and coefficient of variation of each were calculated. Measurements were available every 3 months (16) from 9–21 visits during the follow-up period (average number of visits 15). Glycemic variability measurements during the first 6 months of the trial were excluded to eliminate the effect of the planned rapid reduction in HbA1c.
Statistical Analyses
Participants were initially categorized into two groups based on whether one or more serious hypoglycemic episodes occurred in the time between VADT entry and the follow-up computed tomography scan. Between-group differences in normally distributed continuous variables were assessed with mean ± SD and t tests. Median (25th–75th percentile) and Mann-Whitney U tests were used for variables with skewed distributions, and proportions and χ2 tests were used for dichotomized variables.
To determine the effect of serious hypoglycemia on progression of CAC, we used a robust regression model that limits the influence of outliers and provides stable results in the presence of outliers in both response and covariate variables. To assess the possibility of effect modification by treatment, pairwise interaction terms between treatment and occurrence of hypoglycemia were evaluated. The interaction between treatment and occurrence of hypoglycemia was significant; thus, we performed stratified analyses by treatment arm.
To identify the best parsimonious predictors of CAC progression within each treatment group, we performed a linear regression model with stepwise variable selection (forward in, backward out). All relevant variables from Table 1 were included in the models. Selection criteria required a P < 0.1 for a variable to enter and be retained in models. Serious hypoglycemia as the primary variable of interest was forced into the models. The stepwise analysis indicated that the best predictors of CAC progression differed in each treatment arm. In addition to serious hypoglycemia, prior hypoglycemia in the standard treatment group and baseline CAC and albumin-to-creatinine ratio in the intensive treatment group were retained in the models. We then ran a series of multivariate linear regression models in each treatment arm, with all the variables selected from the parsimonious models for both treatment arms, and adjusted for additional potential confounding effects of other covariates. We assessed the goodness-of-fit of the models with the multivariate coefficient of determination (R2) and residuals. Model fit did not improve with the inclusion of more than seven variables; thus, to avoid overfitting of the regression models, we limited the maximum number of variables in a model to seven.
Table 1.
Baseline characteristics of participants by serious hypoglycemia
| Serious hypoglycemia |
|||
|---|---|---|---|
| No (n = 100) | Yes (n = 97) | P value | |
| Intensive treatment (%) | 21 | 74 | <0.01 |
| Age (years) | 60 ± 9 | 62 ± 9 | 0.1 |
| Non-Hispanic white (%) | 62 | 73 | 0.09 |
| Men (%) | 93 | 93 | 0.95 |
| History of hypertension (%) | 76 | 86 | 0.07 |
| Prior CVD (%) | 35 | 39 | 0.54 |
| Prior hypoglycemia (%) | 8 | 25 | 0.001 |
| Diabetes duration (years) | 11 ± 8 | 14 ± 8 | 0.01 |
| BMI (kg/m2) | 31.8 ± 4.1 | 30.8 ± 4.4 | 0.08 |
| HbA1c (%) | 9.4 ± 1.4 | 9.0 ± 1.3 | 0.05 |
| HbA1c (mmol/mol) | 79 ± 16 | 75 ± 15 | |
| C-peptide (ng/mL) | 0.9 ± 0.6 | 0.6 ± 0.4 | <0.01 |
| Systolic blood pressure (mmHg) | 135 ± 18 | 129 ± 15 | 0.01 |
| Diastolic blood pressure (mmHg) | 77 ± 10 | 74 ± 10 | 0.04 |
| Total cholesterol (mg/dL) | 181 ± 43 | 179 ± 37 | 0.963 |
| LDL cholesterol (mg/dL) | 105 ± 35 | 103 ± 29 | 0.76 |
| HDL cholesterol (mg/dL) | 34 ± 9 | 40 ± 12 | <0.01 |
| Triglycerides (mg/dL) | 183 (135–286) | 150 (113–194) | <0.01 |
| Creatinine (mg/dL) | 0.9 (0.8–1.1) | 1 (0.8–1.2) | 0.05 |
| Albumin-to-creatinine ratio (mg/g) | 18 (7–65) | 14 (4–42) | 0.11 |
| Baseline CAC score | 156 (9–895) | 299 (47–1,120) | 0.05 |
| Medication use (%) | |||
| Insulin | 46 | 69 | <0.01 |
| Antihypertensive | 87 | 93 | 0.17 |
| β-Blocker | 29 | 30 | 0.90 |
| Thiazolidinedione | 9 | 12 | 0.44 |
| Sulfonylurea | 64 | 46 | 0.01 |
| Statin | 56 | 67 | 0.11 |
Data are mean ± SD, median (25th–75th percentile), or percentages. Prior hypoglycemia denotes signs and symptoms of hypoglycemia or blood glucose levels <70 mg/dL (∼3.9 mmol/L) during the last 1.5 months before randomization.
We also performed several sensitivity analyses to examine the robustness of these results and to account for key potential confounders. First, we categorized participants on the basis of the number of reported serious hypoglycemic episodes during follow-up. Because the median number of reported episodes in those with serious hypoglycemia was five, we categorized participants into three groups: 1) those with no hypoglycemic episodes, 2) those with less than five episodes, and 3) those with five or more episodes. Next, we performed stratified analyses by the mean HbA1c value of 7.5% (∼58 mmol/mol) during the study as a level of reasonably good glycemic control and to match HbA1c values used in a prior study of hypoglycemia and CAC (24). We also analyzed the data by severe hypoglycemia and G<50 separately. Finally, we determined CAC progression in a subset of participants matched on baseline CAC (±10%) to further account for differences in baseline CAC. Statistical analyses were performed with SAS release 9.4 software (SAS Institute, Cary, NC).
Results
Participant Characteristics at Baseline
During an average follow-up of 4.6 ± 0.6 years between the two CAC scans, 97 of the 197 participants reported one or more serious hypoglycemic episodes (74 with G<50 only, 23 with severe episodes). The majority of the 97 participants (74%) were in the intensive treatment arm. As shown in Table 1, participants with serious hypoglycemia had a higher prevalence of prior hypoglycemia (P < 0.01), a longer duration of diabetes (P = 0.01), and slightly higher creatinine values (P = 0.05). HbA1c, C-peptide, and triglyceride levels were all lower in those with serious hypoglycemia (P ≤ 0.05), whereas HDL levels and baseline CAC scores were higher (P ≤ 0.05). Baseline insulin use was more common in participants with serious hypoglycemia, whereas sulfonylurea use was less frequent (P ≤ 0.01).
Association Between Serious Hypoglycemia and Progression of CAC
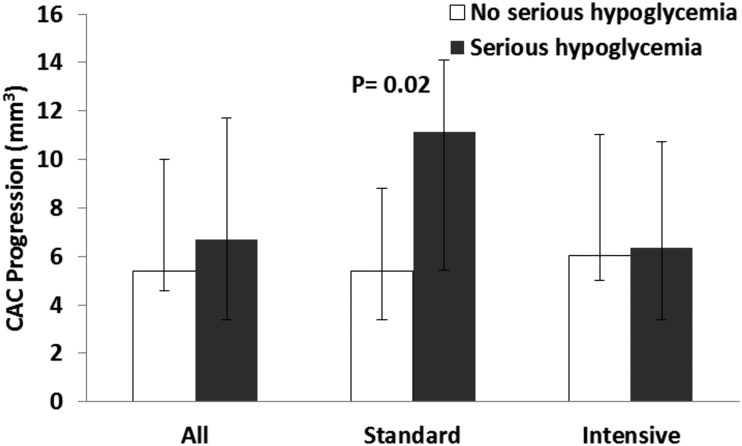
Serious hypoglycemia was not associated with CAC progression in the entire cohort. However, the interaction between serious hypoglycemia and treatment assignment was highly significant (P < 0.01) and persisted after adjustment for all significant differences between participants with and without serious hypoglycemia. Therefore, we performed stratified analysis by treatment arm. As shown in Fig. 1, no significant differences in CAC progression between participants with and without serious hypoglycemia in the entire cohort or in those within the intensive treatment arm were found. However, among participants in the standard treatment arm, those with serious hypoglycemia had significantly greater CAC progression than those with no serious hypoglycemia (P = 0.02).
Figure 1.
Progression of CAC by occurrence of serious hypoglycemia. Median extent of progression of CAC for each group is shown. Error bars represent the 25th–75th percentile. Total number of participants with no serious hypoglycemia was 100, and total number of participants with serious hypoglycemia was 97. The standard treatment group comprised 79 participants with no serious hypoglycemia and 25 with serious hypoglycemia. The intensive treatment group comprised 21 participants with no serious hypoglycemia and 72 participants with serious hypoglycemia. The nonparametric test (Mann-Whitney U test) for the comparison between hypoglycemia categories was not significant for all participants or those in the intensive treatment group.
After adjustment for the variables selected by the stepwise variable selection model (prior hypoglycemia, baseline CAC, and albumin-to-creatinine ratio) in addition to other predictors of CAC progression reported previously (17) (age, duration of diabetes, and race/ethnicity), serious hypoglycemia remained significantly associated with CAC progression in the standard treatment group but not in the intensive treatment group (Table 2, model 1). Additional adjustments for significant differences shown in Table 1, visit-to-visit glycemic variability indices (Table 2), or various combinations of these covariates (not shown) did not change the results appreciably.
Table 2.
Association between serious hypoglycemia and progression of CAC
| Standard treatment (n = 104) |
Intensive treatment (n = 93) |
|||
|---|---|---|---|---|
| Serious hypoglycemia (yes/no) | β ± SE | P value | β ± SE | P value |
| Model 1* | 4.25 ± 1.63 | <0.01 | −1.62 ± 1.36 | 0.23 |
| 1 + HbA1c (%, mmol/mol) | 4.13 ± 1.63 | 0.01 | −1.62 ± 1.38 | 0.24 |
| 1 + triglyceride-to-HDL ratio | 3.71 ± 1.68 | 0.02 | −1.61 ± 1.37 | 0.24 |
| 1 + C-peptide (ng/mL) | 4.58 ± 1.90 | 0.01 | −1.26 ± 1.49 | 0.39 |
| 1 + SBP (mmHg) | 4.72 ± 1.64 | <0.01 | −1.83 ± 1.42 | 0.19 |
| 1 + DBP (mmHg) | 4.43 ± 1.64 | <0.01 | −1.57 ± 1.38 | 0.25 |
| 1 + creatinine (mg/dL) | 4.28 ± 1.65 | <0.01 | −1.52 ± 1.38 | 0.27 |
| 1 + insulin use (yes/no) | 3.81 ± 1.67 | 0.02 | −1.72 ± 1.36 | 0.20 |
| 1 + sulfonylurea use (yes/no) | 3.58 ± 1.66 | 0.03 | −1.74 ± 1.36 | 0.19 |
| 1 + CV HbA1c | 4.47 ± 1.65 | <0.01 | −1.21 ± 1.47 | 0.41 |
| 1 + SD HbA1c (%) | 4.46 ± 1.65 | <0.01 | −1.41 ± 1.47 | 0.33 |
| 1 + CV fasting glucose | 4.00 ± 1.79 | 0.02 | −1.69 ± 1.38 | 0.22 |
| 1 + SD fasting glucose (mg/dL) | 3.94 ± 1.78 | 0.02 | −1.61 ± 1.37 | 0.23 |
CV, coefficient of variation; DBP, diastolic blood pressure; SBP, systolic blood pressure.
*Adjusted for significant predictors of CAC progression in this cohort as previously reported (17) in addition to variables that were selected by parsimonious models from stepwise variable selection model (i.e., age, duration of diabetes, non-Hispanic white ethnicity vs. others, prior hypoglycemia, baseline CAC, and albumin-to-creatinine ratio).
Sensitivity Analyses
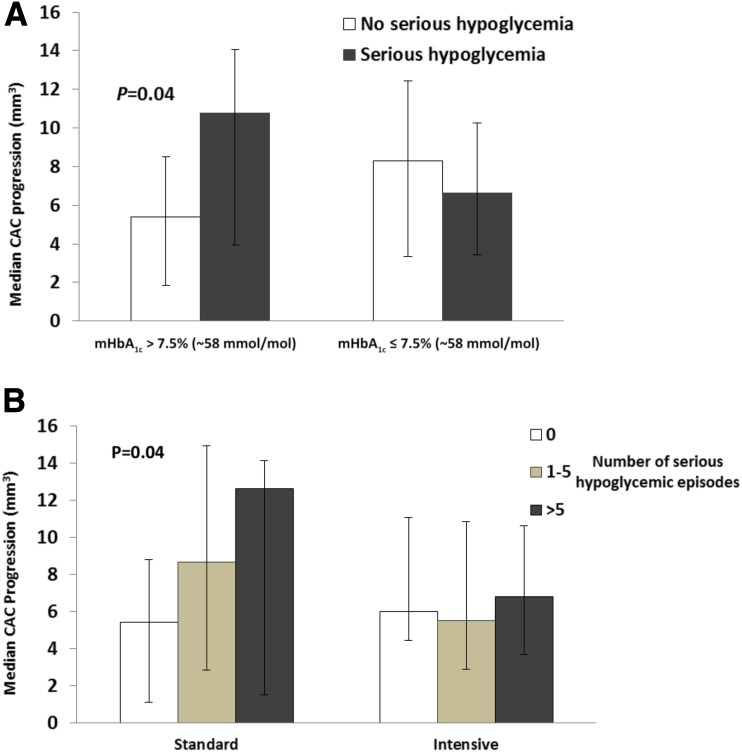
These results were supported by several sensitivity analyses. First, consistent with the association of serious hypoglycemia with CAC progression in the standard treatment arm, serious hypoglycemia was associated with greater CAC progression in participants with a mean HbA1c >7.5% (P = 0.04) but not in those with a mean HbA1c ≤7.5% (Fig. 2A). Of note, CAC progression was associated with increasing mean HbA1c (Supplementary Fig. 1A–B) in participants with serious hypoglycemia (β ± SE 2.69 ± 0.69, P < 0.01) but not in those without serious hypoglycemia (−0.41 ± 0.62, P = 0.51). Second, CAC progression increased with the number of serious hypoglycemic episodes in the standard treatment group (P for overall difference between groups = 0.04) (Fig. 2B) but not in the intensive treatment group. To gain more insight into the potential importance of episodes of G<50 versus severe hypoglycemia, we examined in a separate exploratory analysis the progression of CAC in participants with each of these distinct episodes. Those in the standard group with hypoglycemic episodes defined by having just G<50 had modestly greater progression of CAC than those without hypoglycemia, suggesting that severe hyperglycemia accounts for much of the effect of serious hypoglycemia. However, because the majority (91%) of participants with severe hypoglycemia also reported G<50, examining CAC progression exclusively in those with severe hypoglycemia was not feasible. Finally, to further assess whether differences in baseline CAC might account for the increased CAC progression in participants with serious hypoglycemia in the standard treatment group, we examined a small subset with serious hypoglycemia from the standard group that could be matched based on baseline CAC (within 10%) with participants from the intensive treatment group who also had serious hypoglycemia. Consistent with the aforementioned data, CAC progression trended higher (P = 0.08) in the standard treatment group (median 12.6 mm3) compared with participants in the intensive treatment group (median 7.5 mm3) with similar baseline CAC (Supplementary Fig. 2). Of note, except for the different mean HbA1c between the standard and intensive groups, other cofactors did not differ with hypoglycemia in this subset (data not shown).
Figure 2.
A: Progression of CAC by the occurrence of serious hypoglycemia and categories of mean HbA1c (mHbA1c) during the study. Median extent of progression of CAC for each group is shown. Error bars represent the 25th–75th percentile. The number of participants with mean HbA1c >7.5% (∼58 mmol/mol) with no serious hypoglycemia was 77 and with serious hypoglycemia, 33; participants with mean HbA1c ≤7.5% with no serious hypoglycemia was 23 and with serious hypoglycemia, 64. The nonparametric test (Mann-Whitney U test) for the comparison between hypoglycemia categories was not significant in participants with mean HbA1c ≤7.5%. B: Progression of CAC by the number of serious hypoglycemic episodes. Median extent of progression of CAC for each group is shown. Error bars represent the 25th–75th percentile. Number of participants in the standard treatment group with no serious hypoglycemia was 79; with one to five serious hypoglycemic episodes, 14; and with more than five serious hypoglycemic episodes, 11. The number of participants in the intensive treatment group with no serious hypoglycemia was 21; with one to five serious hypoglycemic episodes, 30; and with more than five serious hypoglycemic episodes, 42. The nonparametric test (Kruskal-Wallis ANOVA) for the overall comparison between categories of frequency of hypoglycemic episodes was not significant in the intensive treatment group.
Conclusions
The study results indicate that serious hypoglycemia in patients undergoing standard therapy but not intensive therapy is associated with increased CAC progression (∼50%) over a nearly 5-year period. Although we previously reported that intensive glycemic control during the VADT did not reduce progression of CAC (17), we did not account for the effect that serious hypoglycemia may play in the cohort. As currently demonstrated, the interaction between treatment assignment and serious hypoglycemia was significant and consistent, persisting even after adjustments for all the significant differences between participants with and without serious hypoglycemia. Thus, the effect of hypoglycemia on CAC progression appears modified by the level of glycemic control, with high glucose levels providing a more permissive environment.
Although patients with serious hypoglycemia seem to have a more advanced stage of type 2 diabetes (based on lower C-peptide levels and higher insulin use at baseline, an indication of greater endogenous insulin deficiency), several key findings indicate that these novel results are not simply a result of patients with serious hypoglycemia being predisposed toward progression of CAC by virtue of their worse cardiovascular risk factor profile or poorer health. First, as shown in Table 1, cardiovascular risk factors were not consistently worse in participants with hypoglycemia (e.g., they had lower HbA1c, higher HDL, lower triglycerides, and lower blood pressure). There was also no difference in prevalence of prior cardiovascular disease (CVD) between treatment groups. Second, after adjustment for all the significant differences between participants with and without serious hypoglycemia (including C-peptide level, insulin use, and creatinine level), serious hypoglycemia remained strongly associated with CAC progression in the standard treatment group only. Third, participants with serious hypoglycemia in the intensive group did not show the same level of CAC progression despite also having more advanced type 2 diabetes and an even higher frequency of hypoglycemic events. The validity of these findings was also supported by several sensitivity analyses (see results).
The major findings of the present study are in line with both the ACCORD (Action to Control Cardiovascular Risk in Diabetes) and the ADVANCE (Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation) trials, which reported higher annual mortality among patients with type 2 diabetes who reported severe hypoglycemia with standard therapy than among those undergoing intensive therapy (4,5). Furthermore, the present results are in keeping with that of the recent VADT follow-up (10), ACCORD (8), and ADVANCE (9) studies, which reported a modest reduction of cardiovascular events with intensive therapy. Although these studies did not directly assess the effect of hypoglycemia on cardiovascular outcomes by treatment, in all, severe hypoglycemia occurred far more frequently with intensive therapy. Of note, the time lag between hypoglycemic events and subsequent cardiovascular and total mortality events in patients with diabetes often has been reported to be years (1–5,8–10), suggesting that hypoglycemia may also have long-term effects on cardiovascular events. The current finding of a greater progression of CAC (a relatively slow process) with serious hypoglycemia in the standard therapy group supports this notion.
In contrast to the present study, the Diabetes Control and Complications Trial/Epidemiology of Diabetes Intervention and Complications study (DCCT/EDIC) (24) reported that the association of severe hypoglycemia with a CAC ≥100 Agatston units was most apparent in patients with type 1 diabetes with better glycemic control (HbA1c <7.5%). Despite this substudy finding, patients in the DCCT receiving intensive therapy demonstrated reduced long-term overall rates of CVD (25). Differences in patient types and other cohort characteristics could have contributed to the different pattern of results from those seen in the present study. In addition, CAC was measured only once in this study, years after the intensive glucose-lowering phase was completed. Thus, potential differences in baseline levels of CAC could not be determined, and progression of CAC was not assessed in the DCCT/EDIC study.
Multiple mechanisms have been proposed to account for the relationship between hypoglycemia and CVD in patients with diabetes. Falling plasma glucose concentrations, beginning at ∼70 mg/dL (∼3.9 mmol/L), is associated with acute activation of counterregulatory defense mechanisms and surges in the sympathoadrenal system, which increase cardiac workload, and provokes abnormal cardiac repolarization, vasospasm, and transient ischemia (11,12,22). If these defenses fail to abort the hypoglycemic episode, lower glucose levels trigger a more intense sympathoadrenal response that causes neurogenic (or autonomic) symptoms and eventually neuroglycopenic symptoms (22). Although, these changes are transient and unlikely to exert any long-term consequences on a healthy circulation, they may be particularly injurious in patients with diabetes whose vasculature is already damaged (26).
Presumably in response to these hormonal and neurologic responses, hypoglycemia can trigger inflammation, abnormalities in platelet function, and activation of the fibrinolytic system and induce oxidative stress and endothelial dysfunction (12,27), all of which may contribute to the progression of atherosclerosis. Evidence also exists that abrupt glucose fluctuations can induce oxidative stress and enhance endothelial cell apoptosis more potently than sustained hyperglycemia in patients with type 2 diabetes (28–30). A similar situation may have existed in the present study in participants who experienced serious hypoglycemic episodes while receiving standard therapy because they had both low glucose episodes as well as a relatively high average HbA1c of 8.4% during the study (6). Abrupt glucose fluctuation during hypoglycemic episodes in the standard treatment group may have contributed to coronary artery injury and to progression of CAC.
Another plausible explanation for greater CAC progression in participants with serious hypoglycemia in the standard therapy group is that these individuals were less ready for hypoglycemic events when they occurred. Because all types of hypoglycemia, even nonserious, occurred more frequently with intensive therapy, participants in this group may have been more prepared to take immediate action to alleviate and shorten the events. Hence, participants in the standard therapy group may have been exposed to relatively more severe and prolonged hypoglycemia, which may have contributed to greater vascular injury and CAC progression. Moreover, vascular tissue in participants in the intensive treatment group may have been preconditioned to hypoglycemia as a result of their more frequent hypoglycemic episodes, resulting in upregulation of antioxidant or other cellular defense systems that could modulate the consequences of severe hypoglycemia. In line with this hypothesis, in the ACCORD trial, the number of preceding hypoglycemic episodes modified the risk of death associated with severe hypoglycemia (31).
The present study has a number of strengths. First, both CAC progression and hypoglycemic episodes were assessed during the VADT during randomized treatment assignment, and episodes of serious hypoglycemia were carefully assessed and recorded at each participant visit; thus, the risk of recall bias and lead time bias was minimal. Another strength of this study is the long interval between scans (nearly 5 years) and the extensive absolute change in calcium that occurred, providing additional confidence in the estimates of the rates of CAC progression. In addition, we were able to investigate the effect of hypoglycemia in a trial where by design, the treatment effect was more directly a function of glucose control than differences in antidiabetic agents used.
An important caveat of this study is that it is a post hoc analysis of a smaller subset of the VADT participants. We have previously shown that this subset of participants is generally reflective of the larger VADT population (17,32). The strong and significant interaction between treatment group and serious hypoglycemia and the consistent results in the more adjusted models and in several sensitivity analyses support the validity of the study findings. However, because the sample size of participants with severe hypoglycemia was small, we cannot rule out the possibility of chance or residual confounding in this relationship. Additionally, participants in the VADT were older, predominantly male veterans with long-standing type 2 diabetes; thus, extrapolation of the study findings to other populations must be done with caution.
In conclusion, this study shows that serious hypoglycemia is associated with increased progression of CAC in patients undergoing standard therapy for glycemic control and in those with higher HbA1c (>7.5%) during the VADT, despite a nearly threefold higher frequency of serious hypoglycemia with intensive therapy. The results may provide additional insights into long-term cardiovascular benefits of intensive glycemic control and support the importance of avoiding hypoglycemia, particularly in elderly patients with long-standing, poorly controlled type 2 diabetes.
Supplementary Material
Article Information
Acknowledgments. The authors thank the VADT participants and staff and the investigators at the Phoenix, San Diego, Long Beach, Hines, Pittsburgh, Tucson, and Miami VA Medical Centers. They also acknowledge the contributions of the Hines VA Cooperative Studies Program Coordinating Center, the Tufts Lipid Metabolism Laboratory, and the Harbor-UCLA Medical Center Computed Tomographic Reading Center.
Funding. This work was supported by the Veterans Affairs Cooperative Studies Program of the U.S. Department of Veterans Affairs Office of Research and Development. Additional support was received from the National Institutes of Health grants R01-067690 and 5R01-094775 to P.D.R. and from the American Diabetes Association to P.D.R.
The contents of this study do not represent the views of the Department of Veterans Affairs or the U.S. Government.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. A.S. and P.D.R. contributed to the study concept and design, data analysis and interpretation, and writing and final approval of the manuscript. G.D.B. contributed to the study design, data acquisition, statistical analysis, data interpretation, and critical review and final approval of the manuscript. A.S. and P.D.R. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. This study was presented in abstract form for a late-breaking poster presentation at the 75th Scientific Sessions of the American Diabetes Association, Boston, MA, 5–9 June 2015.
Footnotes
Clinical trial reg. no. NCT00032487, clinicaltrials.gov.
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc15-2107/-/DC1.
References
- 1.Hsu PF, Sung SH, Cheng HM, et al. . Association of clinical symptomatic hypoglycemia with cardiovascular events and total mortality in type 2 diabetes: a nationwide population-based study. Diabetes Care 2013;36:894–900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khunti K, Davies M, Majeed A, Thorsted BL, Wolden ML, Paul SK. Hypoglycemia and risk of cardiovascular disease and all-cause mortality in insulin-treated people with type 1 and type 2 diabetes: a cohort study. Diabetes Care 2015;38:316–322 [DOI] [PubMed] [Google Scholar]
- 3.Zhao Y, Campbell CR, Fonseca V, Shi L. Impact of hypoglycemia associated with antihyperglycemic medications on vascular risks in veterans with type 2 diabetes. Diabetes Care 2012;35:1126–1132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zoungas S, Patel A, Chalmers J, et al.; ADVANCE Collaborative Group . Severe hypoglycemia and risks of vascular events and death. N Engl J Med 2010;363:1410–1418 [DOI] [PubMed] [Google Scholar]
- 5.Bonds DE, Miller ME, Bergenstal RM, et al. . The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: retrospective epidemiological analysis of the ACCORD study. BMJ 2010;340:b4909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duckworth W, Abraira C, Moritz T, et al.; VADT Investigators . Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 2009;360:129–139 [DOI] [PubMed] [Google Scholar]
- 7.The DCCT Research Group Epidemiology of severe hypoglycemia in the diabetes control and complications trial. Am J Med 1991;90:450–459 [PubMed] [Google Scholar]
- 8.Gerstein HC, Miller ME, Ismail-Beigi F, et al.; ACCORD Study Group . Effects of intensive glycaemic control on ischaemic heart disease: analysis of data from the randomised, controlled ACCORD trial. Lancet 2014;384:1936–1941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel A, MacMahon S, Chalmers J, et al.; ADVANCE Collaborative Group . Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560–2572 [DOI] [PubMed] [Google Scholar]
- 10.Hayward RA, Reaven PD, Wiitala WL, et al.; VADT Investigators . Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2015;372:2197–2206 [DOI] [PubMed] [Google Scholar]
- 11.DeFronzo RA, Hendler R, Christensen N. Stimulation of counterregulatory hormonal responses in diabetic man by a fall in glucose concentration. Diabetes 1980;29:125–131 [DOI] [PubMed] [Google Scholar]
- 12.Desouza CV, Bolli GB, Fonseca V. Hypoglycemia, diabetes, and cardiovascular events. Diabetes Care 2010;33:1389–1394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gogitidze Joy N, Hedrington MS, Briscoe VJ, Tate DB, Ertl AC, Davis SN. Effects of acute hypoglycemia on inflammatory and pro-atherothrombotic biomarkers in individuals with type 1 diabetes and healthy individuals. Diabetes Care 2010;33:1529–1535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Joy NG, Tate DB, Younk LM, Davis SN. Effects of acute and antecedent hypoglycemia on endothelial function and markers of atherothrombotic balance in healthy humans. Diabetes 2015;64:2571–2580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reaven PD, Sacks J; Investigators for the VADT . Coronary artery and abdominal aortic calcification are associated with cardiovascular disease in type 2 diabetes. Diabetologia 2005;48:379–385 [DOI] [PubMed] [Google Scholar]
- 16.Abraira C, Duckworth W, McCarren M, et al.; VA Cooperative Study of Glycemic Control and Complications in Diabetes Mellitus Type 2 . Design of the cooperative study on glycemic control and complications in diabetes mellitus type 2: Veterans Affairs Diabetes Trial. J Diabetes Complications 2003;17:314–322 [DOI] [PubMed] [Google Scholar]
- 17.Saremi A, Moritz TE, Anderson RJ, Abraira C, Duckworth WC, Reaven PD; Veterans Affairs Diabetes Trial (VADT) . Rates and determinants of coronary and abdominal aortic artery calcium progression in the Veterans Affairs Diabetes Trial (VADT). Diabetes Care 2010;33:2642–2647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reaven PD, Sacks J; Investigators for the Veterans Affairs Cooperative Study of Glycemic Control and Complications in Diabetes Mellitus Type 2 . Reduced coronary artery and abdominal aortic calcification in Hispanics with type 2 diabetes. Diabetes Care 2004;27:1115–1120 [DOI] [PubMed] [Google Scholar]
- 19.Boyle PJ, Schwartz NS, Shah SD, Clutter WE, Cryer PE. Plasma glucose concentrations at the onset of hypoglycemic symptoms in patients with poorly controlled diabetes and in nondiabetics. N Engl J Med 1988;318:1487–1492 [DOI] [PubMed] [Google Scholar]
- 20.Mitrakou A, Ryan C, Veneman T, et al. . Hierarchy of glycemic thresholds for counterregulatory hormone secretion, symptoms, and cerebral dysfunction. Am J Physiol 1991;260:E67–E74 [DOI] [PubMed] [Google Scholar]
- 21.Fanelli C, Pampanelli S, Epifano L, et al. . Relative roles of insulin and hypoglycaemia on induction of neuroendocrine responses to, symptoms of, and deterioration of cognitive function in hypoglycaemia in male and female humans. Diabetologia 1994;37:797–807 [DOI] [PubMed] [Google Scholar]
- 22.Cryer PE. Hypoglycemia, functional brain failure, and brain death. J Clin Invest 2007;117:868–870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Workgroup on Hypoglycemia, American Diabetes Association Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care 2005;28:1245–1249 [DOI] [PubMed] [Google Scholar]
- 24.Fährmann ER, Adkins L, Loader CJ, et al. . Severe hypoglycemia and coronary artery calcification during the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) study. Diabetes Res Clin Pract 2015;107:280–289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nathan DM, Cleary PA, Backlund JY, et al.; Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group . Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med 2005;353:2643–2653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wright RJ, Frier BM. Vascular disease and diabetes: is hypoglycaemia an aggravating factor? Diabetes Metab Res Rev 2008;24:353–363 [DOI] [PubMed] [Google Scholar]
- 27.Kemeny SF, Figueroa DS, Clyne AM. Hypo- and hyperglycemia impair endothelial cell actin alignment and nitric oxide synthase activation in response to shear stress. PLoS One 2013;8:e66176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Piconi L, Quagliaro L, Assaloni R, et al. . Constant and intermittent high glucose enhances endothelial cell apoptosis through mitochondrial superoxide overproduction. Diabetes Metab Res Rev 2006;22:198–203 [DOI] [PubMed] [Google Scholar]
- 29.Monnier L, Mas E, Ginet C, et al. . Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA 2006;295:1681–1687 [DOI] [PubMed] [Google Scholar]
- 30.Li W, Liu X, Yanoff M, Cohen S, Ye X. Cultured retinal capillary pericytes die by apoptosis after an abrupt fluctuation from high to low glucose levels: a comparative study with retinal capillary endothelial cells. Diabetologia 1996;39:537–547 [DOI] [PubMed] [Google Scholar]
- 31.Seaquist ER, Miller ME, Bonds DE, et al.; ACCORD Investigators . The impact of frequent and unrecognized hypoglycemia on mortality in the ACCORD study. Diabetes Care 2012;35:409–414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reaven PD, Moritz TE, Schwenke DC, et al.; Veterans Affairs Diabetes Trial . Intensive glucose-lowering therapy reduces cardiovascular disease events in Veterans Affairs Diabetes Trial participants with lower calcified coronary atherosclerosis. Diabetes 2009;58:2642–2648 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.